Copyright © 2015 Bert N. Langford (Images may be subject to copyright. Please send feedback)
Welcome to Our Generation USA!
This Page covers
Addictions
to nicotine, caffeine, alcohol, drugs and other substances (e.g., opioids) -- but also other forms of cultural dependency (e.g., gambling). Also included are recovery programs or groups, e.g. "Alcoholics Anonymous"
Addictions including Compulsive Behaviors (e.g., Gambling)
YouTube Video Intensive Outpatient Addiction Treatment at the Betty Ford Center*
*- The Betty Ford Center
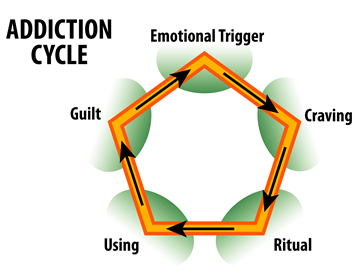
Addiction is a brain disease that is characterized by compulsive engagement in rewarding stimuli, despite adverse consequences.
Despite the involvement of a number of psychosocial factors, a biological process – one which is induced by repeated exposure to an addictive stimulus – is the core pathology that drives the development and maintenance of an addiction.
The two properties that characterize all addictive stimuli are that they are reinforcing (i.e., they increase the likelihood that a person will seek repeated exposure to them) and intrinsically rewarding (i.e., perceived as being positive or desirable).
Addiction is a disorder of the brain's reward system which arises through transcriptional and epigenetic mechanisms and occurs over time from chronically high levels of exposure to an addictive stimulus (e.g., morphine, cocaine, sexual intercourse, gambling, etc.).
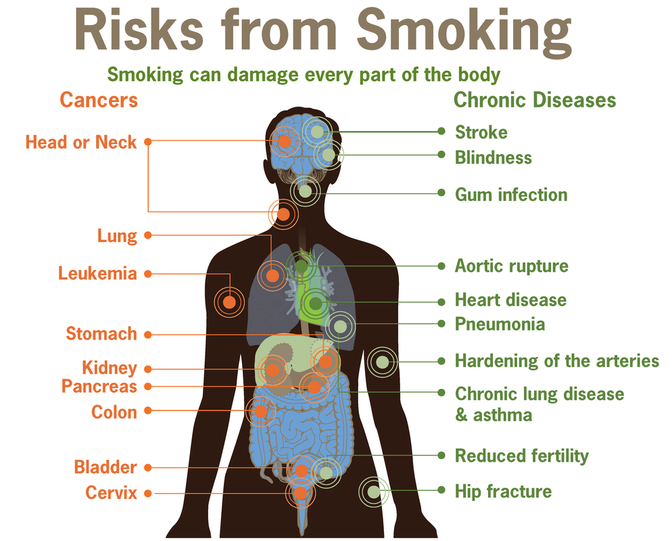
Addiction exacts a high toll on individuals and society as a whole through the direct adverse effects of drugs, associated healthcare costs, long-term complications (e.g., lung cancer with smoking tobacco, liver cirrhosis with drinking alcohol, or meth mouth from intravenous methamphetamine), the functional consequences of altered neural plasticity in the brain, and the consequent loss of productivity.
Classic hallmarks of addiction include impaired control over substances or behavior, preoccupation with substance or behavior, and continued use despite consequences. Habits and patterns associated with addiction are typically characterized by immediate gratification (short-term reward), coupled with delayed deleterious effects (long-term costs).
Examples of drug and behavioral addictions include:
The only behavioral addiction recognized by the DSM-5 is gambling addiction. The term addiction is misused frequently to refer to other compulsive behaviors or disorders, particularly dependence, in news media.
For further amplification, click on any of the following hyperlinks:
Despite the involvement of a number of psychosocial factors, a biological process – one which is induced by repeated exposure to an addictive stimulus – is the core pathology that drives the development and maintenance of an addiction.
The two properties that characterize all addictive stimuli are that they are reinforcing (i.e., they increase the likelihood that a person will seek repeated exposure to them) and intrinsically rewarding (i.e., perceived as being positive or desirable).
Addiction is a disorder of the brain's reward system which arises through transcriptional and epigenetic mechanisms and occurs over time from chronically high levels of exposure to an addictive stimulus (e.g., morphine, cocaine, sexual intercourse, gambling, etc.).
Addiction exacts a high toll on individuals and society as a whole through the direct adverse effects of drugs, associated healthcare costs, long-term complications (e.g., lung cancer with smoking tobacco, liver cirrhosis with drinking alcohol, or meth mouth from intravenous methamphetamine), the functional consequences of altered neural plasticity in the brain, and the consequent loss of productivity.
Classic hallmarks of addiction include impaired control over substances or behavior, preoccupation with substance or behavior, and continued use despite consequences. Habits and patterns associated with addiction are typically characterized by immediate gratification (short-term reward), coupled with delayed deleterious effects (long-term costs).
Examples of drug and behavioral addictions include:
- alcoholism,
- amphetamine addiction,
- cocaine addiction,
- nicotine addiction,
- opiate addiction,
- food addiction,
- gambling addiction,
- and sexual addiction.
The only behavioral addiction recognized by the DSM-5 is gambling addiction. The term addiction is misused frequently to refer to other compulsive behaviors or disorders, particularly dependence, in news media.
For further amplification, click on any of the following hyperlinks:
- Neuropsychology
- Behavioral addiction
- Risk factors
- Mechanisms
- Diagnosis
- Treatment
- Epidemiology
- Personality theories of addiction
- Notes
- References
- External links
Addictive Personality
YouTube Video: 9 Signs of an Addictive Personality
An addictive personality refers to a particular set of personality traits that make an individual predisposed to developing addictions.
This hypothesis states that there are common elements among people with varying addictions that relates to personality traits. People who are substance dependent are characterized by: a physical or psychological dependency that negatively affects their quality of life.
They are frequently connected with substance abuse; however, people with addictive personalities are also highly at risk of becoming addicted to:
Scientists have been better able to understand addictive personalities as researchers delve further into understanding the chemistry of addiction. Alan R. Lang of Florida State University, author of an addiction study prepared for the United States National Academy of Sciences, said, "If we can better identify the personality factors, they can help us devise better treatment and can open up new strategies to intervene and break the patterns of addiction.
Click on any of the following blue hyperlinks for further amplification:
This hypothesis states that there are common elements among people with varying addictions that relates to personality traits. People who are substance dependent are characterized by: a physical or psychological dependency that negatively affects their quality of life.
They are frequently connected with substance abuse; however, people with addictive personalities are also highly at risk of becoming addicted to:
- gambling,
- food,
- pornography,
- exercise,
- work,
- and codependency.
Scientists have been better able to understand addictive personalities as researchers delve further into understanding the chemistry of addiction. Alan R. Lang of Florida State University, author of an addiction study prepared for the United States National Academy of Sciences, said, "If we can better identify the personality factors, they can help us devise better treatment and can open up new strategies to intervene and break the patterns of addiction.
Click on any of the following blue hyperlinks for further amplification:
- Description
- Biopsychosocial causes
- Signs and symptoms
- Personality traits and addiction
- Common forms of addictive behavior include:
- Relation to leadership
- Treatment
- Controversy
Substance Abuse
YouTube Video: 6 Signs of Substance Abuse and Addiction
YouTube Video: Teen Rx Drug Addiction by CBS News
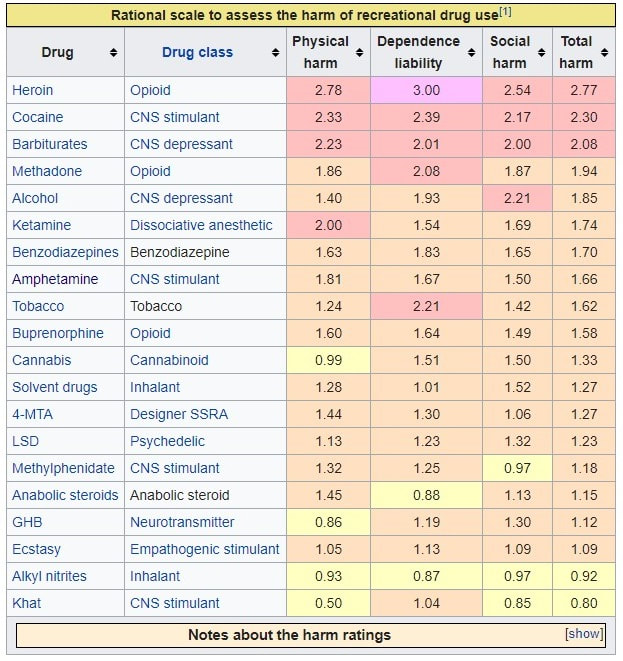
Picture Below: The Physical harm, Dependence liability, and Social harm scores were each computed from the average of three distinct ratings. The highest possible harm rating for each rating scale is 3.0.
Physical harm is the average rating of the scores for acute binge use, chronic use, and intravenous use.
Dependence liability is the average rating of the scores for intensity of pleasure, psychological dependence, and physical dependence.
Social harm is the average rating of the scores for drug intoxication, health-care costs, and other social harms.
Total harm was computed as the average of the Physical harm, Dependence liability, and Social harm scores.
Substance abuse, also known as drug abuse, is a patterned use of a drug in which the user consumes the substance in amounts or with methods which are harmful to themselves or others, and is a form of substance-related disorder.
Widely differing definitions of drug abuse are used in public health, medical and criminal justice contexts. In some cases criminal or anti-social behavior occurs when the person is under the influence of a drug, and long term personality changes in individuals may occur as well.
In addition to possible physical, social, and psychological harm, use of some drugs may also lead to criminal penalties, although these vary widely depending on the local jurisdiction.
Drugs most often associated with this term include the following:
The exact cause of substance abuse is not clear, with the two predominant theories being: either a genetic disposition which is learned from others, or a habit which if addiction develops, manifests itself as a chronic debilitating disease.
In 2010 about 5% of people (230 million) used an illicit substance. Of these 27 million have high-risk drug use otherwise known as recurrent drug use causing harm to their health, psychological problems, or social problems or puts them at risk of those dangers.
In 2015 substance use disorders resulted in 307,400 deaths, up from 165,000 deaths in 1990. Of these, the highest numbers are from the following:
Classifications:
Public health definitions:
Public health practitioners have attempted to look at substance use from a broader perspective than the individual, emphasizing the role of society, culture, and availability. Some health professionals choose to avoid the terms alcohol or drug "abuse" in favor of language they consider more objective, such as "substance and alcohol type problems" or "harmful/problematic use" of drugs.
The Health Officers Council of British Columbia — in their 2005 policy discussion paper, A Public Health Approach to Drug Control in Canada] — has adopted a public health model of psychoactive substance use that challenges the simplistic black-and-white construction of the binary (or complementary) antonyms"use" vs. "abuse". This model explicitly recognizes a spectrum of use, ranging from beneficial use to chronic dependence.
Medical definitions:
'Drug abuse' is no longer a current medical diagnosis in either of the most used diagnostic tools in the world, the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM), and the World Health Organization's International Statistical Classification of Diseases (ICD).
Substance abuse has been adopted by the DSM as a blanket term to include 10 separate classes of drugs, including alcohol; caffeine; cannabis; hallucinogens; inhalants; opioids; sedatives, hypnotics, and anxiolytics; stimulants; tobacco; and other substances.
The ICD uses the term Harmful use to cover physical or psychological harm to the user from use.
Physical dependence, abuse of, and withdrawal from drugs and other miscellaneous substances is outlined in the DSM:
However, other definitions differ; they may entail psychological or physical dependence, and may focus on treatment and prevention in terms of the social consequences of substance uses.
Value Judgment:
Philip Jenkins suggests that there are two issues with the term "drug abuse". First, what constitutes a "drug" is debatable. For instance, GHB, a naturally occurring substance in the central nervous system is considered a drug, and is illegal in many countries, while nicotine is not officially considered a drug in most countries.
Second, the word "abuse" implies a recognized standard of use for any substance. Drinking an occasional glass of wine is considered acceptable in most Western countries, while drinking several bottles is seen as an abuse. Strict temperance advocates, who may or may not be religiously motivated, would see drinking even one glass as an abuse. Some groups even condemn caffeine use in any quantity.
Similarly, adopting the view that any (recreational) use of cannabis or substituted amphetamines constitutes drug abuse implies a decision made that the substance is harmful, even in minute quantities.
In the U.S., drugs have been legally classified into five categories, schedule I, II, III, IV, or V in the Controlled Substances Act. The drugs are classified on their deemed potential for abuse.
Usage of some drugs is strongly correlated. For example, the consumption of seven illicit drugs (amphetamines, cannabis, cocaine, ecstasy, legal highs, LSD, and magic mushrooms) is correlated and the Pearson correlation coefficient r>0.4 in every pair of them; consumption of cannabis is strongly correlated (r>0.5) with usage of nicotine (tobacco), heroin is correlated with cocaine (r>0.4), methadone (r>0.45), and strongly correlated with crack (r>0.5)
Drug Misuse:
Drug misuse is a term used commonly when prescription medication with sedative, anxiolytic, analgesic, or stimulant properties are used for mood alteration or intoxication ignoring the fact that overdose of such medicines can sometimes have serious adverse effects. It sometimes involves drug diversion from the individual for whom it was prescribed.
Prescription misuse has been defined differently and rather inconsistently based on status of drug prescription, the uses without a prescription, intentional use to achieve intoxicating effects, route of administration, co-ingestion with alcohol, and the presence or absence of dependence symptoms.
Chronic use of certain substances leads to a change in the central nervous system known as a 'tolerance' to the medicine such that more of the substance is needed in order to produce desired effects. With some substances, stopping or reducing use can cause withdrawal symptoms to occur, but this is highly dependent on the specific substance in question.
The rate of prescription drug use is fast overtaking illegal drug use in the United States. According to the National Institute of Drug Abuse, 7 million people were taking prescription drugs for non-medical use in 2010. Among 12th graders, non-medical prescription drug use is now second only to cannabis. "Nearly 1 in 12 high school seniors reported non-medical use of Vicodin; 1 in 20 reported such use of OxyContin." Both of these drugs contain opioids.
Avenues of obtaining prescription drugs for misuse are varied: sharing between family and friends, illegally buying medications at school or work, and often "doctor shopping" to find multiple physicians to prescribe the same medication, without knowledge of other prescribers.
Increasingly, law enforcement is holding physicians responsible for prescribing controlled substances without fully establishing patient controls, such as a patient "drug contract." Concerned physicians are educating themselves on how to identify medication-seeking behavior in their patients, and are becoming familiar with "red flags" that would alert them to potential prescription drug abuse.
Click on any of the following blue hyperlinks for more about Substance Abuse:
Widely differing definitions of drug abuse are used in public health, medical and criminal justice contexts. In some cases criminal or anti-social behavior occurs when the person is under the influence of a drug, and long term personality changes in individuals may occur as well.
In addition to possible physical, social, and psychological harm, use of some drugs may also lead to criminal penalties, although these vary widely depending on the local jurisdiction.
Drugs most often associated with this term include the following:
- alcohol,
- cannabis,
- barbiturates,
- benzodiazepines,
- cocaine,
- methaqualone,
- opioids,
- and some substituted amphetamines.
The exact cause of substance abuse is not clear, with the two predominant theories being: either a genetic disposition which is learned from others, or a habit which if addiction develops, manifests itself as a chronic debilitating disease.
In 2010 about 5% of people (230 million) used an illicit substance. Of these 27 million have high-risk drug use otherwise known as recurrent drug use causing harm to their health, psychological problems, or social problems or puts them at risk of those dangers.
In 2015 substance use disorders resulted in 307,400 deaths, up from 165,000 deaths in 1990. Of these, the highest numbers are from the following:
- alcohol use disorders at 137,500 deaths,
- opioid use disorders at 122,100 deaths,
- amphetamine use disorders at 12,200 deaths,
- and cocaine use disorders at 11,100.
Classifications:
Public health definitions:
Public health practitioners have attempted to look at substance use from a broader perspective than the individual, emphasizing the role of society, culture, and availability. Some health professionals choose to avoid the terms alcohol or drug "abuse" in favor of language they consider more objective, such as "substance and alcohol type problems" or "harmful/problematic use" of drugs.
The Health Officers Council of British Columbia — in their 2005 policy discussion paper, A Public Health Approach to Drug Control in Canada] — has adopted a public health model of psychoactive substance use that challenges the simplistic black-and-white construction of the binary (or complementary) antonyms"use" vs. "abuse". This model explicitly recognizes a spectrum of use, ranging from beneficial use to chronic dependence.
Medical definitions:
'Drug abuse' is no longer a current medical diagnosis in either of the most used diagnostic tools in the world, the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM), and the World Health Organization's International Statistical Classification of Diseases (ICD).
Substance abuse has been adopted by the DSM as a blanket term to include 10 separate classes of drugs, including alcohol; caffeine; cannabis; hallucinogens; inhalants; opioids; sedatives, hypnotics, and anxiolytics; stimulants; tobacco; and other substances.
The ICD uses the term Harmful use to cover physical or psychological harm to the user from use.
Physical dependence, abuse of, and withdrawal from drugs and other miscellaneous substances is outlined in the DSM:
- When an individual persists in use of alcohol or other drugs despite problems related to use of the substance, substance dependence may be diagnosed. Compulsive and repetitive use may result in tolerance to the effect of the drug and withdrawal symptoms when use is reduced or stopped.
However, other definitions differ; they may entail psychological or physical dependence, and may focus on treatment and prevention in terms of the social consequences of substance uses.
Value Judgment:
Philip Jenkins suggests that there are two issues with the term "drug abuse". First, what constitutes a "drug" is debatable. For instance, GHB, a naturally occurring substance in the central nervous system is considered a drug, and is illegal in many countries, while nicotine is not officially considered a drug in most countries.
Second, the word "abuse" implies a recognized standard of use for any substance. Drinking an occasional glass of wine is considered acceptable in most Western countries, while drinking several bottles is seen as an abuse. Strict temperance advocates, who may or may not be religiously motivated, would see drinking even one glass as an abuse. Some groups even condemn caffeine use in any quantity.
Similarly, adopting the view that any (recreational) use of cannabis or substituted amphetamines constitutes drug abuse implies a decision made that the substance is harmful, even in minute quantities.
In the U.S., drugs have been legally classified into five categories, schedule I, II, III, IV, or V in the Controlled Substances Act. The drugs are classified on their deemed potential for abuse.
Usage of some drugs is strongly correlated. For example, the consumption of seven illicit drugs (amphetamines, cannabis, cocaine, ecstasy, legal highs, LSD, and magic mushrooms) is correlated and the Pearson correlation coefficient r>0.4 in every pair of them; consumption of cannabis is strongly correlated (r>0.5) with usage of nicotine (tobacco), heroin is correlated with cocaine (r>0.4), methadone (r>0.45), and strongly correlated with crack (r>0.5)
Drug Misuse:
Drug misuse is a term used commonly when prescription medication with sedative, anxiolytic, analgesic, or stimulant properties are used for mood alteration or intoxication ignoring the fact that overdose of such medicines can sometimes have serious adverse effects. It sometimes involves drug diversion from the individual for whom it was prescribed.
Prescription misuse has been defined differently and rather inconsistently based on status of drug prescription, the uses without a prescription, intentional use to achieve intoxicating effects, route of administration, co-ingestion with alcohol, and the presence or absence of dependence symptoms.
Chronic use of certain substances leads to a change in the central nervous system known as a 'tolerance' to the medicine such that more of the substance is needed in order to produce desired effects. With some substances, stopping or reducing use can cause withdrawal symptoms to occur, but this is highly dependent on the specific substance in question.
The rate of prescription drug use is fast overtaking illegal drug use in the United States. According to the National Institute of Drug Abuse, 7 million people were taking prescription drugs for non-medical use in 2010. Among 12th graders, non-medical prescription drug use is now second only to cannabis. "Nearly 1 in 12 high school seniors reported non-medical use of Vicodin; 1 in 20 reported such use of OxyContin." Both of these drugs contain opioids.
Avenues of obtaining prescription drugs for misuse are varied: sharing between family and friends, illegally buying medications at school or work, and often "doctor shopping" to find multiple physicians to prescribe the same medication, without knowledge of other prescribers.
Increasingly, law enforcement is holding physicians responsible for prescribing controlled substances without fully establishing patient controls, such as a patient "drug contract." Concerned physicians are educating themselves on how to identify medication-seeking behavior in their patients, and are becoming familiar with "red flags" that would alert them to potential prescription drug abuse.
Click on any of the following blue hyperlinks for more about Substance Abuse:
- Signs and symptoms
- Treatment Psychological
- Epidemiology
- History
- Society and culture
- Special populations
- See also:
- ΔFosB
- Addictive personality
- Alcohol abuse
- Combined drug intoxication
- Controlled Substances Act
- Drug addiction
- Drug overdose
- List of controlled drugs in the United Kingdom
- List of deaths from drug overdose and intoxication
- Harm reduction
- Low-threshold treatment programs
- Needle-exchange programme
- Poly drug use
- Polysubstance abuse
- Substance use disorder
- Adverse Childhood Experiences: Risk Factors for Substance Misuse and Mental Health Dr. Robert Anda of the U.S. Centers for Disease Control describes the relation between childhood adversity and later ill-health, including substance abuse (video)
- The National Institute on Drug Abuse
The Opioid Epidemic focusing on the United States
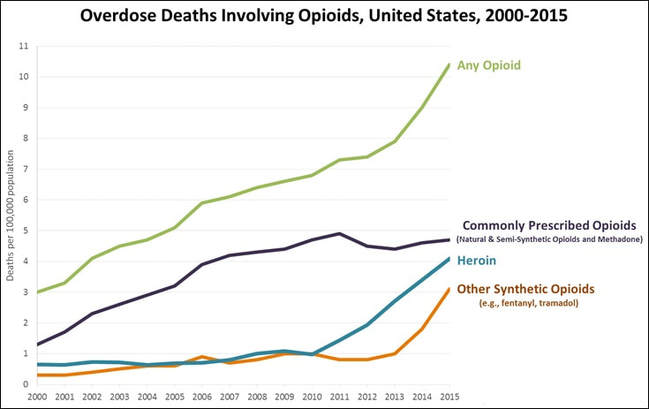
Pictured below: Overdose Deaths Involving Opioids, United States, 2000–2015. Deaths per 100,000 population.
- YouTube Video: The new face of fentanyl addiction: Kati's story
- YouTube Video: One Nation, Overdosed: Documentary On The Deadliest Drug Crisis In American History (Full) by MSNBC
- YouTube Video: Betty Ford's Lecture on Addiction and Recovery*
Pictured below: Overdose Deaths Involving Opioids, United States, 2000–2015. Deaths per 100,000 population.
The opioid epidemic or opioid crisis is the rapid increase in the use of prescription and non-prescription opioid drugs in the United States and Canada beginning in the late 1990s and continuing throughout the first two decades of the 2000s.
Opioids are a diverse class of moderately strong painkillers, including oxycodone (commonly sold under the trade names OxyContin and Percocet), hydrocodone (Vicodin), and a very strong painkiller, fentanyl, which is synthesized to resemble other opiates such as opium-derived morphine and heroin.
The potency and availability of these substances, despite their high risk of addiction and overdose, have made them popular both as formal medical treatments and as recreational drugs. Due to their sedative effects on the part of the brain which regulates breathing, opioids in high doses present the potential for respiratory depression, and may cause respiratory failure and death.
According to the U.S. Drug Enforcement Administration, "overdose deaths, particularly from prescription drugs and heroin, have reached epidemic levels". Nearly half of all opioid overdose deaths in 2016 involved prescription opioids. From 1999 to 2008, overdose death rates, sales, and substance abuse treatment admissions related to opioid pain relievers all increased substantially. By 2015, annual overdose deaths from heroin alone surpassed deaths from both car accidents and guns, with other opioid overdose deaths also on the rise.
Drug overdoses have since become the leading cause of death of Americans under 50, with two-thirds of those deaths from opioids. In 2016, the crisis decreased overall life expectancy of Americans for the second consecutive year.
Overall life expectancy fell from 78.7 to 78.6 years. Men were disproportionally more affected due to higher overdose death rates, with life expectancy declining from 76.3 to 76.1 years. Women’s life expectancy remained stable at 81.1 years.
In 2016, over 64,000 Americans died from overdoses, 21 percent more than the almost 53,000 in 2015. By comparison, the figure was 16,000 in 2010, and 4,000 in 1999.
While death rates varied by state, public health experts estimate that nationwide over 500,000 people could die from the epidemic over the next 10 years. In Canada, half of the overdoses were accidental, while a third was intentional. The remainder were unknown. Many of the deaths are from an extremely potent opioid, fentanyl, which is trafficked from Mexico.
The epidemic cost the United States an estimated $504 billion in 2015.
CDC director Thomas Frieden said that "America is awash in opioids; urgent action is critical." The crisis has changed moral, social, and cultural resistance to street drug alternatives such as heroin.
In March 2017, Larry Hogan, the governor of Maryland, declared a state of emergency to combat the opioid epidemic, and in July 2017 opioid addiction was cited as the "FDA's biggest crisis." On October 26, 2017, President Donald Trump concurred with his Commission's report and declared the country's opioid crisis a "public health emergency."
Click on any of the following blue hyperlinks for more about the Opioid Epidemic:
Opioids are a diverse class of moderately strong painkillers, including oxycodone (commonly sold under the trade names OxyContin and Percocet), hydrocodone (Vicodin), and a very strong painkiller, fentanyl, which is synthesized to resemble other opiates such as opium-derived morphine and heroin.
The potency and availability of these substances, despite their high risk of addiction and overdose, have made them popular both as formal medical treatments and as recreational drugs. Due to their sedative effects on the part of the brain which regulates breathing, opioids in high doses present the potential for respiratory depression, and may cause respiratory failure and death.
According to the U.S. Drug Enforcement Administration, "overdose deaths, particularly from prescription drugs and heroin, have reached epidemic levels". Nearly half of all opioid overdose deaths in 2016 involved prescription opioids. From 1999 to 2008, overdose death rates, sales, and substance abuse treatment admissions related to opioid pain relievers all increased substantially. By 2015, annual overdose deaths from heroin alone surpassed deaths from both car accidents and guns, with other opioid overdose deaths also on the rise.
Drug overdoses have since become the leading cause of death of Americans under 50, with two-thirds of those deaths from opioids. In 2016, the crisis decreased overall life expectancy of Americans for the second consecutive year.
Overall life expectancy fell from 78.7 to 78.6 years. Men were disproportionally more affected due to higher overdose death rates, with life expectancy declining from 76.3 to 76.1 years. Women’s life expectancy remained stable at 81.1 years.
In 2016, over 64,000 Americans died from overdoses, 21 percent more than the almost 53,000 in 2015. By comparison, the figure was 16,000 in 2010, and 4,000 in 1999.
While death rates varied by state, public health experts estimate that nationwide over 500,000 people could die from the epidemic over the next 10 years. In Canada, half of the overdoses were accidental, while a third was intentional. The remainder were unknown. Many of the deaths are from an extremely potent opioid, fentanyl, which is trafficked from Mexico.
The epidemic cost the United States an estimated $504 billion in 2015.
CDC director Thomas Frieden said that "America is awash in opioids; urgent action is critical." The crisis has changed moral, social, and cultural resistance to street drug alternatives such as heroin.
In March 2017, Larry Hogan, the governor of Maryland, declared a state of emergency to combat the opioid epidemic, and in July 2017 opioid addiction was cited as the "FDA's biggest crisis." On October 26, 2017, President Donald Trump concurred with his Commission's report and declared the country's opioid crisis a "public health emergency."
Click on any of the following blue hyperlinks for more about the Opioid Epidemic:
Alcoholism, Alcohol Abuse and Alcohol Dependence
YouTube Video of the Effects of Binge Drinking by CDC
YouTube Video: Why Does Alcoholics Anonymous Work?
Alcoholism:
Alcoholism, also known as alcohol use disorder (AUD), is a broad term for any drinking of alcohol that results in mental or physical health problems. The disorder was previously divided into two types: alcohol abuse and alcohol dependence: see later herein for each.
In a medical context, alcoholism is said to exist when two or more of the following conditions are present: a person drinks large amounts over a long time period, has difficulty cutting down, acquiring and drinking alcohol takes up a great deal of time, alcohol is strongly desired, usage results in not fulfilling responsibilities, usage results in social problems, usage results in health problems, usage results in risky situations, withdrawal occurs when stopping, and alcohol tolerance has occurred with use.
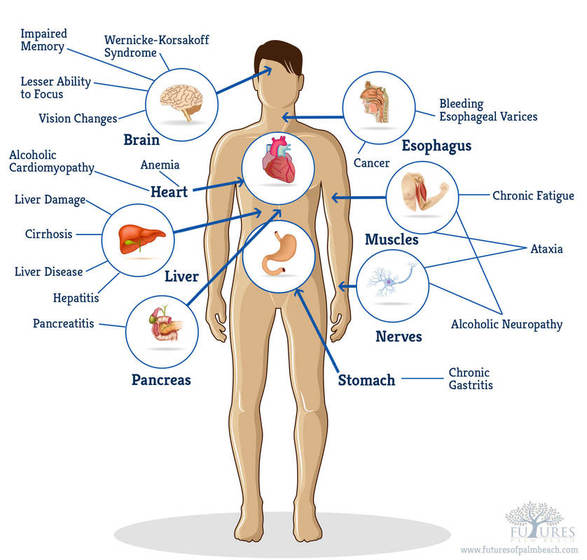
Risky situations include drinking and driving or having unsafe sex, among other things. Alcohol use can affect all parts of the body, but it particularly affects the brain, heart, liver, pancreas and immune system.This can result in mental illness, Wernicke–Korsakoff syndrome, irregular heartbeat, liver cirrhosis and increased cancer risk, among other diseases. Drinking during pregnancy can cause damage to the baby resulting in fetal alcohol spectrum disorders.
Women are generally more sensitive than men to the harmful physical and mental effects of alcohol.
Environmental factors and genetics are two components associated with alcoholism, with about half the risk attributed to each. Someone with a parent or sibling with alcoholism is three to four times more likely to become an alcoholic themselves. Environmental factors include social, cultural and behavioral influences. High stress levels and anxiety, as well as alcohol's inexpensive cost and easy accessibility, increase the risk.
People may continue to drink partly to prevent or improve symptoms of withdrawal. After a person stops drinking alcohol, they may experience a low level of withdrawal lasting for months.
Medically, alcoholism is considered both a physical and mental illness. Questionnaires and certain blood tests may both detect people with possible alcoholism. Further information is then collected to confirm the diagnosis.
Prevention of alcoholism may be attempted by regulating and limiting the sale of alcohol, taxing alcohol to increase its cost, and providing inexpensive treatment. Treatment may take several steps. Due to medical problems that can occur during withdrawal, alcohol detoxification should be carefully controlled.
One common method involves the use of benzodiazepine medications, such as diazepam. These can be either given while admitted to a health care institution or occasionally while a person remains in the community with close supervision.
Mental illness or other addictions may complicate treatment. After detoxification, support such as group therapy or support groups are used to help keep a person from returning to drinking. One commonly used form of support is the group Alcoholics Anonymous.(See above YouTube Video) The medications acamprosate, disulfiram or naltrexone may also be used to help prevent further drinking.
The World Health Organization estimates that as of 2010 there were 208 million people with alcoholism worldwide (4.1% of the population over 15 years of age).
In the United States, about 17 million (7%) of adults and 0.7 million (2.8%) of those age 12 to 17 years of age are affected. It is more common among males and young adults, becoming less common in middle and old age.
It is the least common in Africa, at 1.1%, and has the highest rates in Eastern Europe, at 11%. Alcoholism directly resulted in 139,000 deaths in 2013, up from 112,000 deaths in 1990.
A total of 3.3 million deaths (5.9% of all deaths) are believed to be due to alcohol. It often reduces a person's life expectancy by around ten years.
In the United States, it resulted in economic costs of $224 billion USD in 2006. Many terms, some insulting and others informal, have been used to refer to people affected by alcoholism; the expressions include tippler, drunkard, dipsomaniac and souse. In 1979, the World Health Organization discouraged the use of "alcoholism" due to its inexact meaning, preferring "alcohol dependence syndrome".
Click on any of the following blue hyperlinks for more about alcoholism:
Alcohol abuse encompasses a spectrum of unhealthy alcohol drinking behaviors, ranging from risky drinking to alcohol abuse to alcohol dependence. This includes binge drinking and alcohol dependence. It is a psychiatric diagnosis as classified by DSM-5 (DSM-5).
Globally, alcohol consumption is the seventh leading risk factor for both death and the burden of disease and injury. In short, except for tobacco, alcohol accounts for a higher burden of disease than any other drug.
Alcohol use is a major cause of preventable liver disease worldwide, and alcoholic liver disease is the main alcohol-related chronic medical illness. Millions of men and women of all ages, from adolescents to the elderly, engage in unhealthy drinking in the United States. AUD reportedly most often affects young men (aged 18-24 years) of lower socioeconomic status.
There are two types of alcohol abuse, those who have anti-social and pleasure-seeking tendencies, and those who are anxiety-ridden people who are able to go without drinking for long periods of time but are unable to control themselves once they start.
Alcoholism Definitions:
Main article: Binge drinking
Risky drinking (also called hazardous drinking) is defined by drinking above the recommended limits:
Binge drinking is a pattern of alcohol consumption that brings blood alcohol concentration ≥ 0.08%, usually corresponds to
A patient meets criteria for the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnosis of alcohol use disorder if ≥ 2 of the following behaviors or symptoms have been present within the past 12 months:
Alcohol misuse is a term used by United States Preventive Services Task Force to describe a spectrum of drinking behaviors that encompass risky drinking, alcohol abuse, and alcohol dependence (similar meaning to alcohol use disorder but not a term used in DSM).
In medical care, alcohol abuse and alcohol dependence were used as distinct disorders from 1994 to 2013. After the publication of DSM-5 in 2013, the disorders were all categorized under alcohol use disorder. The DSM-5 combines those two disorders into one alcohol use disorder with sub-classifications of severity. The DSM-IV definition is no longer used. There is no "alcoholism" diagnosis in medical care.
Tolerance is the need for increased amounts of alcohol to achieve the same effect.
A smaller volume of consumed alcohol has a greater impact on the older adult than it does on a younger individual. As a result, the American Geriatrics Society recommends for an older adult with no known risk factors less than one drink a day or fewer than two drinks per occasion regardless of gender.
Signs and Symptoms:
Main article: Long-term effects of alcohol
Individuals with an alcohol use disorder will often complain of difficulty with interpersonal relationships, problems at work or school, and legal problems. Additionally, people may complain of irritability and insomnia. Alcohol abuse is also an important cause of chronic fatigue.
Signs of alcohol abuse are related to alcohol's effects on organ systems. However, while these findings are often present, they are not necessary to make a diagnosis of alcohol abuse. Signs of alcohol abuse show its drastic effects on the central nervous system, including inebriation and poor judgment; chronic anxiety, irritability, and insomnia.
Alcohol's effects on the liver include elevated liver function tests (classically AST is at least twice as high as ALT). Prolonged use leads to cirrhosis and liver failure. With cirrhosis, patients develop an inability to process hormones and toxins.
The skin of a patient with alcoholic cirrhosis can feature cherry angiomas, palmar erythema and — in acute liver failure — jaundice and ascites. The derangements of the endocrine system lead to the enlargement of the male breasts. The inability to process toxins leads to liver disease, such as hepatic encephalopathy.
Alcohol abuse can result in brain damage which causes impairments in executive functioning such as impairments to working memory, visuospatial skills, and can cause an abnormal personality as well as affective disorders to develop.
Binge drinking is associated with individuals reporting fair to poor health compared to non-binge drinking individuals and which may progressively worsen over time. Alcohol also causes impairment in a person's critical thinking.
A person's ability to reason in stressful situations is compromised, and they seem very inattentive to what is going on around them. Social skills are significantly impaired in people suffering from alcoholism due to the neurotoxic effects of alcohol on the brain, especially the prefrontal cortex area of the brain.
The social skills that are impaired by alcohol abuse include impairments in perceiving facial emotions, difficulty with perceiving vocal emotions and theory of mind deficits; the ability to understand humor is also impaired in alcohol abusers. Adolescent binge drinkers are most sensitive to damaging neurocognitive functions especially executive functions and memory.
People who abuse alcohol are less likely to survive critical illness with a higher risk for having sepsis and were more likely to die during hospitalization.
Violence:
Alcohol abuse is significantly associated with suicide and violence. Alcohol is the most significant health concern in Native American communities because of very high rates of alcohol dependence and abuse; up to 80 percent of suicides and 60 percent of violent acts are a result of alcohol abuse in Native American communities.
In the United States alcohol-related violence is related to more severe injuries and chronic cases.
Pregnancy:
Alcohol abuse among pregnant women causes their baby to develop fetal alcohol syndrome. Fetal alcohol syndrome is the pattern of physical abnormalities and the impairment of mental development which is seen with increasing frequency among children with alcoholic mothers.
Alcohol exposure in a developing fetus can result in slowed development of the fetal brain, resulting in severe retardation or death. Surviving infants may suffer severe abnormalities such as abnormal eyes, fissures, lips and incomplete cerebella.
Some infants may develop lung disease. It is even possible that the baby throughout pregnancy will develop heart defects such as ventricular septal defect or atrial septal defect. Experts suggest that pregnant women take no more than one unit of alcohol per day. However, other organizations advise complete abstinence from alcohol while pregnant
Adolescence:
Adolescence and the onset of puberty have both a physiological and social impact on a developing person. About half of grade 12 students have been drunk, and a third binge drink.
About 3% drink every day. One of these social impacts is the increase in risk-taking behaviors, such as the emergence of alcohol use. Children aged 16 and under who consume alcohol heavily display symptoms of conduct disorder. Its symptoms include troublesome behaviour in school, constantly lying, learning disabilities and social impairments.
Alcohol abuse during adolescence greatly increases the risk of developing an alcohol use disorder in adulthood due to changes to neurocircuitry that alcohol abuse causes in the vulnerable adolescent brain. Younger ages of initial consumption among males in recent studies has shown to be associated with increased rates of alcohol abuse within the general population.
Societal inequalities (among other factors) have influenced an adolescents decision to consume alcohol. One study suggests that girls were scrutinized for "drinking like men", whereas magazines that target the male population sent underlying messages to boys and or men that drinking alcohol was "masculine". (Bogren, 2010).
Click on any of the following blue hyperlinks for more about Alcohol Abuse:
Alcohol dependence:
Alcohol dependence is a previous psychiatric diagnosis in which an individual is physically or psychologically dependent upon alcohol (also known formally as ethanol).
In 2013 it was reclassified as alcohol use disorder, or alcoholism along with alcohol abuse in DSM-5.
Click on any of the following blue hyperlinks for more about Alcohol Dependence:
Alcoholism, also known as alcohol use disorder (AUD), is a broad term for any drinking of alcohol that results in mental or physical health problems. The disorder was previously divided into two types: alcohol abuse and alcohol dependence: see later herein for each.
In a medical context, alcoholism is said to exist when two or more of the following conditions are present: a person drinks large amounts over a long time period, has difficulty cutting down, acquiring and drinking alcohol takes up a great deal of time, alcohol is strongly desired, usage results in not fulfilling responsibilities, usage results in social problems, usage results in health problems, usage results in risky situations, withdrawal occurs when stopping, and alcohol tolerance has occurred with use.
Risky situations include drinking and driving or having unsafe sex, among other things. Alcohol use can affect all parts of the body, but it particularly affects the brain, heart, liver, pancreas and immune system.This can result in mental illness, Wernicke–Korsakoff syndrome, irregular heartbeat, liver cirrhosis and increased cancer risk, among other diseases. Drinking during pregnancy can cause damage to the baby resulting in fetal alcohol spectrum disorders.
Women are generally more sensitive than men to the harmful physical and mental effects of alcohol.
Environmental factors and genetics are two components associated with alcoholism, with about half the risk attributed to each. Someone with a parent or sibling with alcoholism is three to four times more likely to become an alcoholic themselves. Environmental factors include social, cultural and behavioral influences. High stress levels and anxiety, as well as alcohol's inexpensive cost and easy accessibility, increase the risk.
People may continue to drink partly to prevent or improve symptoms of withdrawal. After a person stops drinking alcohol, they may experience a low level of withdrawal lasting for months.
Medically, alcoholism is considered both a physical and mental illness. Questionnaires and certain blood tests may both detect people with possible alcoholism. Further information is then collected to confirm the diagnosis.
Prevention of alcoholism may be attempted by regulating and limiting the sale of alcohol, taxing alcohol to increase its cost, and providing inexpensive treatment. Treatment may take several steps. Due to medical problems that can occur during withdrawal, alcohol detoxification should be carefully controlled.
One common method involves the use of benzodiazepine medications, such as diazepam. These can be either given while admitted to a health care institution or occasionally while a person remains in the community with close supervision.
Mental illness or other addictions may complicate treatment. After detoxification, support such as group therapy or support groups are used to help keep a person from returning to drinking. One commonly used form of support is the group Alcoholics Anonymous.(See above YouTube Video) The medications acamprosate, disulfiram or naltrexone may also be used to help prevent further drinking.
The World Health Organization estimates that as of 2010 there were 208 million people with alcoholism worldwide (4.1% of the population over 15 years of age).
In the United States, about 17 million (7%) of adults and 0.7 million (2.8%) of those age 12 to 17 years of age are affected. It is more common among males and young adults, becoming less common in middle and old age.
It is the least common in Africa, at 1.1%, and has the highest rates in Eastern Europe, at 11%. Alcoholism directly resulted in 139,000 deaths in 2013, up from 112,000 deaths in 1990.
A total of 3.3 million deaths (5.9% of all deaths) are believed to be due to alcohol. It often reduces a person's life expectancy by around ten years.
In the United States, it resulted in economic costs of $224 billion USD in 2006. Many terms, some insulting and others informal, have been used to refer to people affected by alcoholism; the expressions include tippler, drunkard, dipsomaniac and souse. In 1979, the World Health Organization discouraged the use of "alcoholism" due to its inexact meaning, preferring "alcohol dependence syndrome".
Click on any of the following blue hyperlinks for more about alcoholism:
- Signs and symptoms
- Causes
- Diagnosis
- Prevention
- Management
- Epidemiology
- Prognosis
- History
- Society and culture
- Research
- See also:
Alcohol abuse encompasses a spectrum of unhealthy alcohol drinking behaviors, ranging from risky drinking to alcohol abuse to alcohol dependence. This includes binge drinking and alcohol dependence. It is a psychiatric diagnosis as classified by DSM-5 (DSM-5).
Globally, alcohol consumption is the seventh leading risk factor for both death and the burden of disease and injury. In short, except for tobacco, alcohol accounts for a higher burden of disease than any other drug.
Alcohol use is a major cause of preventable liver disease worldwide, and alcoholic liver disease is the main alcohol-related chronic medical illness. Millions of men and women of all ages, from adolescents to the elderly, engage in unhealthy drinking in the United States. AUD reportedly most often affects young men (aged 18-24 years) of lower socioeconomic status.
There are two types of alcohol abuse, those who have anti-social and pleasure-seeking tendencies, and those who are anxiety-ridden people who are able to go without drinking for long periods of time but are unable to control themselves once they start.
Alcoholism Definitions:
Main article: Binge drinking
Risky drinking (also called hazardous drinking) is defined by drinking above the recommended limits:
- greater than 14 standard drinks units per week or greater than 4 standard drinks on a single occasion in men
- greater than 7 standard drinks units per week or greater than 3 standard drinks on a single occasion in women
- any drinking in pregnant women or persons < 21 years old
Binge drinking is a pattern of alcohol consumption that brings blood alcohol concentration ≥ 0.08%, usually corresponds to
- ≥ 5 standard drinks on a single occasion in men
- ≥ 4 standard drinks on a single occasion in women
A patient meets criteria for the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) diagnosis of alcohol use disorder if ≥ 2 of the following behaviors or symptoms have been present within the past 12 months:
- drinking more or longer than intended
- more than once wanting to cut down or stop drinking and tried but unsuccessful
- spending a lot of time drinking or being sick/getting over the after-effects
- wanting a drink so badly it precluded all other thoughts
- often having drinking (or after-effects of drinking) interfere with major responsibilities or obligations including those of home, family, job, or school
- continuing to drink despite it causing trouble with family or friends
- giving up or cutting back on important/interesting/pleasurable activities in order to drink
- more than once, drinking in situations in which it was physically hazardous (including swimming, operating machinery, walking in dangerous area, or having unsafe sex)
- continuing to drink despite knowledge of having persistent or recurrent physical or psychological problems exacerbated by alcohol use
- noticing a need for increased amounts of alcohol to achieve intoxication or desired effect, or a diminished effect with continued use of the same amount of alcohol
- noticing withdrawal symptoms while alcohol effects are wearing off, including trouble sleeping, shakiness, restlessness, nausea, sweating, racing heart, seizure, or sensed things that were not there
Alcohol misuse is a term used by United States Preventive Services Task Force to describe a spectrum of drinking behaviors that encompass risky drinking, alcohol abuse, and alcohol dependence (similar meaning to alcohol use disorder but not a term used in DSM).
In medical care, alcohol abuse and alcohol dependence were used as distinct disorders from 1994 to 2013. After the publication of DSM-5 in 2013, the disorders were all categorized under alcohol use disorder. The DSM-5 combines those two disorders into one alcohol use disorder with sub-classifications of severity. The DSM-IV definition is no longer used. There is no "alcoholism" diagnosis in medical care.
Tolerance is the need for increased amounts of alcohol to achieve the same effect.
A smaller volume of consumed alcohol has a greater impact on the older adult than it does on a younger individual. As a result, the American Geriatrics Society recommends for an older adult with no known risk factors less than one drink a day or fewer than two drinks per occasion regardless of gender.
Signs and Symptoms:
Main article: Long-term effects of alcohol
Individuals with an alcohol use disorder will often complain of difficulty with interpersonal relationships, problems at work or school, and legal problems. Additionally, people may complain of irritability and insomnia. Alcohol abuse is also an important cause of chronic fatigue.
Signs of alcohol abuse are related to alcohol's effects on organ systems. However, while these findings are often present, they are not necessary to make a diagnosis of alcohol abuse. Signs of alcohol abuse show its drastic effects on the central nervous system, including inebriation and poor judgment; chronic anxiety, irritability, and insomnia.
Alcohol's effects on the liver include elevated liver function tests (classically AST is at least twice as high as ALT). Prolonged use leads to cirrhosis and liver failure. With cirrhosis, patients develop an inability to process hormones and toxins.
The skin of a patient with alcoholic cirrhosis can feature cherry angiomas, palmar erythema and — in acute liver failure — jaundice and ascites. The derangements of the endocrine system lead to the enlargement of the male breasts. The inability to process toxins leads to liver disease, such as hepatic encephalopathy.
Alcohol abuse can result in brain damage which causes impairments in executive functioning such as impairments to working memory, visuospatial skills, and can cause an abnormal personality as well as affective disorders to develop.
Binge drinking is associated with individuals reporting fair to poor health compared to non-binge drinking individuals and which may progressively worsen over time. Alcohol also causes impairment in a person's critical thinking.
A person's ability to reason in stressful situations is compromised, and they seem very inattentive to what is going on around them. Social skills are significantly impaired in people suffering from alcoholism due to the neurotoxic effects of alcohol on the brain, especially the prefrontal cortex area of the brain.
The social skills that are impaired by alcohol abuse include impairments in perceiving facial emotions, difficulty with perceiving vocal emotions and theory of mind deficits; the ability to understand humor is also impaired in alcohol abusers. Adolescent binge drinkers are most sensitive to damaging neurocognitive functions especially executive functions and memory.
People who abuse alcohol are less likely to survive critical illness with a higher risk for having sepsis and were more likely to die during hospitalization.
Violence:
Alcohol abuse is significantly associated with suicide and violence. Alcohol is the most significant health concern in Native American communities because of very high rates of alcohol dependence and abuse; up to 80 percent of suicides and 60 percent of violent acts are a result of alcohol abuse in Native American communities.
In the United States alcohol-related violence is related to more severe injuries and chronic cases.
Pregnancy:
Alcohol abuse among pregnant women causes their baby to develop fetal alcohol syndrome. Fetal alcohol syndrome is the pattern of physical abnormalities and the impairment of mental development which is seen with increasing frequency among children with alcoholic mothers.
Alcohol exposure in a developing fetus can result in slowed development of the fetal brain, resulting in severe retardation or death. Surviving infants may suffer severe abnormalities such as abnormal eyes, fissures, lips and incomplete cerebella.
Some infants may develop lung disease. It is even possible that the baby throughout pregnancy will develop heart defects such as ventricular septal defect or atrial septal defect. Experts suggest that pregnant women take no more than one unit of alcohol per day. However, other organizations advise complete abstinence from alcohol while pregnant
Adolescence:
Adolescence and the onset of puberty have both a physiological and social impact on a developing person. About half of grade 12 students have been drunk, and a third binge drink.
About 3% drink every day. One of these social impacts is the increase in risk-taking behaviors, such as the emergence of alcohol use. Children aged 16 and under who consume alcohol heavily display symptoms of conduct disorder. Its symptoms include troublesome behaviour in school, constantly lying, learning disabilities and social impairments.
Alcohol abuse during adolescence greatly increases the risk of developing an alcohol use disorder in adulthood due to changes to neurocircuitry that alcohol abuse causes in the vulnerable adolescent brain. Younger ages of initial consumption among males in recent studies has shown to be associated with increased rates of alcohol abuse within the general population.
Societal inequalities (among other factors) have influenced an adolescents decision to consume alcohol. One study suggests that girls were scrutinized for "drinking like men", whereas magazines that target the male population sent underlying messages to boys and or men that drinking alcohol was "masculine". (Bogren, 2010).
Click on any of the following blue hyperlinks for more about Alcohol Abuse:
- Causes
- Mechanisms
- Diagnosis
- Prevention
- Treatment
- Epidemiology
- Prognosis
- Society and culture
- Societal and economic costs
- See also:
- Rethinking Drinking, National Institute on Alcohol Abuse and Alcoholism
- Alcohol and Crime: Data from 2002 to 2008: Bureau of Justice Statistics
- Healthy Youth! Alcohol & Drug Abuse – U.S. Centers for Disease Control (CDC)
Alcohol dependence:
Alcohol dependence is a previous psychiatric diagnosis in which an individual is physically or psychologically dependent upon alcohol (also known formally as ethanol).
In 2013 it was reclassified as alcohol use disorder, or alcoholism along with alcohol abuse in DSM-5.
Click on any of the following blue hyperlinks for more about Alcohol Dependence:
Controlled Substances Act (1970) and the Drug Enforcement Administration (DEA)
YouTube Video: DEA Lecture Series: Who We Are and What We Do - Special Agents
YouTube Video: DEA in action busting drug traffickers
Pictured below: Map of the 21 DEA domestic field divisions: 1. Chicago, 2. Detroit, 3.Atlanta, 4. Dallas, 5. Denver, 6. Boston, 7. El Paso, 8. Houston, 9. Los Angeles, 10. Miami, 11. Newark, 12. New Orleans, 13. New York, 14. Philadelphia, 15. Phoenix, 16. San Diego, 17. San Francisco, 18. Seattle, 19. St. Louis, 20. Caribbean, 21. Washington, D.C.
The Controlled Substances Act (CSA) is the statute establishing federal U.S. drug policy under which the manufacture, importation, possession, use, and distribution of certain substances is regulated. It was passed by the 91st United States Congress as Title II of the Comprehensive Drug Abuse Prevention and Control Act of 1970 and signed into law by President Richard Nixon. The Act also served as the national implementing legislation for the Single Convention on Narcotic Drugs.
The legislation created five Schedules (classifications), with varying qualifications for a substance to be included in each. Two federal agencies, the Drug Enforcement Administration (DEA: below) and the Food and Drug Administration (FDA), determine which substances are added to or removed from the various schedules, although the statute passed by Congress created the initial listing.
Congress has sometimes scheduled other substances through legislation such as the Hillory J. Farias and Samantha Reid Date-Rape Prevention Act of 2000, which placed gamma hydroxybutyrate (GHB) in Schedule I and sodium oxybate (the isolated sodium salt in GHB) in Schedule III.
Classification decisions are required to be made on criteria including potential for abuse (an undefined term), currently accepted medical use in treatment in the United States, and international treaties.
Click here for more about the Controlled Substances Act
___________________________________________________________________________
The Drug Enforcement Administration (DEA) is a United States federal law enforcement agency under the United States Department of Justice, tasked with combating drug smuggling and distribution within the United States.
The DEA is the lead agency for domestic enforcement of the Controlled Substances Act (above), sharing concurrent jurisdiction with the following:
The DEA has sole responsibility for coordinating and pursuing US drug investigations both domestic and abroad.
Click on any of the following blue hyperlinks for more about the Drug Enforcement Administration (DEA):
The legislation created five Schedules (classifications), with varying qualifications for a substance to be included in each. Two federal agencies, the Drug Enforcement Administration (DEA: below) and the Food and Drug Administration (FDA), determine which substances are added to or removed from the various schedules, although the statute passed by Congress created the initial listing.
Congress has sometimes scheduled other substances through legislation such as the Hillory J. Farias and Samantha Reid Date-Rape Prevention Act of 2000, which placed gamma hydroxybutyrate (GHB) in Schedule I and sodium oxybate (the isolated sodium salt in GHB) in Schedule III.
Classification decisions are required to be made on criteria including potential for abuse (an undefined term), currently accepted medical use in treatment in the United States, and international treaties.
Click here for more about the Controlled Substances Act
___________________________________________________________________________
The Drug Enforcement Administration (DEA) is a United States federal law enforcement agency under the United States Department of Justice, tasked with combating drug smuggling and distribution within the United States.
The DEA is the lead agency for domestic enforcement of the Controlled Substances Act (above), sharing concurrent jurisdiction with the following:
- Federal Bureau of Investigation (FBI),
- Immigration and Customs Enforcement (ICE),
- U.S. Customs and Border Protection (CBP),
- and the Department of Homeland Security (DHS).
The DEA has sole responsibility for coordinating and pursuing US drug investigations both domestic and abroad.
Click on any of the following blue hyperlinks for more about the Drug Enforcement Administration (DEA):
- History and mandate
- Organization
- Budget
- Firearms
- Impact on the drug trade
- Criticism
- Raids on medical marijuana dispensaries
- Project Cassandra
- DEA Museum
- See also:
- Official website
- Drug Enforcement Administration in the Federal Register
- List of former DEA Administrators
- Office of Diversion Control
- A response to the DEA web site
- DEA Watch
- DrugEnforcementEdu.org
- Get Smart About Drugs – A DEA Resource for Parents
- DEA Demand Reduction – Street Smart Prevention
- DEA Museum
- Title 21 of the Code of Federal Regulations
- Diplomatic Security Service (DSS), U.S. State Department
- List of United States federal law enforcement agencies
- Operation Panama Express
- Regulation of therapeutic goods in the United States
- U.S. Customs and Border Protection (CBP)
Sexual Addiction
YouTube Video: Sharon Osbourne 'Proud' That Ozzy 'Finally' Admitted to Sex Addiction
Pictured below: This cycle describes what happens inside someone who has a sexual addiction. First a pain agent is triggered; it could be any kind of emotional discomfort (i.e.. pain, fear, shame, anger, etc.), it could be unresolved conflict (inner or outer), it could be stress, or it could be the need to connect with another.
Sexual addiction, also known as sex addiction, is characterized as a state of compulsive participation or engagement in sexual activity, particularly sexual intercourse, despite negative consequences.
Proponents of a diagnostic model for sexual addiction consider it to be one of several sex-related disorders within an umbrella concept known as hypersexual disorder. The term sexual dependence is also used to refer to people who report being unable to control their sexual urges, behaviors, or thoughts.
Related or synonymous models of pathological sexual behavior include hypersexuality (nymphomania and satyriasis), erotomania, Don Juanism (or Don Juanitaism), and paraphilia-related disorders.
The concept of sexual addiction is contentious. There is considerable debate among psychiatrists, psychologists, sexologists, and other specialists whether compulsive sexual behavior constitutes an addiction, and therefore its classification and possible diagnosis.
Animal research has been established that compulsive sexual behavior arises from the same transcriptional and epigenetic mechanisms that mediate drug addiction in laboratory animals; however, as of 2018, sexual addiction is not a clinical diagnosis in either the DSM or ICD medical classifications of diseases and medical disorders.
Some argue that applying such concepts to normal behaviors such as sex, can be problematic, and suggest that applying medical models such as addiction to human sexuality can serve to pathologise normal behavior and cause harm.
Click on any of the following blue hyperlinks for more about Sex Addiction:
Proponents of a diagnostic model for sexual addiction consider it to be one of several sex-related disorders within an umbrella concept known as hypersexual disorder. The term sexual dependence is also used to refer to people who report being unable to control their sexual urges, behaviors, or thoughts.
Related or synonymous models of pathological sexual behavior include hypersexuality (nymphomania and satyriasis), erotomania, Don Juanism (or Don Juanitaism), and paraphilia-related disorders.
The concept of sexual addiction is contentious. There is considerable debate among psychiatrists, psychologists, sexologists, and other specialists whether compulsive sexual behavior constitutes an addiction, and therefore its classification and possible diagnosis.
Animal research has been established that compulsive sexual behavior arises from the same transcriptional and epigenetic mechanisms that mediate drug addiction in laboratory animals; however, as of 2018, sexual addiction is not a clinical diagnosis in either the DSM or ICD medical classifications of diseases and medical disorders.
Some argue that applying such concepts to normal behaviors such as sex, can be problematic, and suggest that applying medical models such as addiction to human sexuality can serve to pathologise normal behavior and cause harm.
Click on any of the following blue hyperlinks for more about Sex Addiction:
Smartphone Addiction
YouTube Video of Crash Shows Dangers of Texting While Driving
Pictured below: Weber State University Students Study Smartphone Addiction
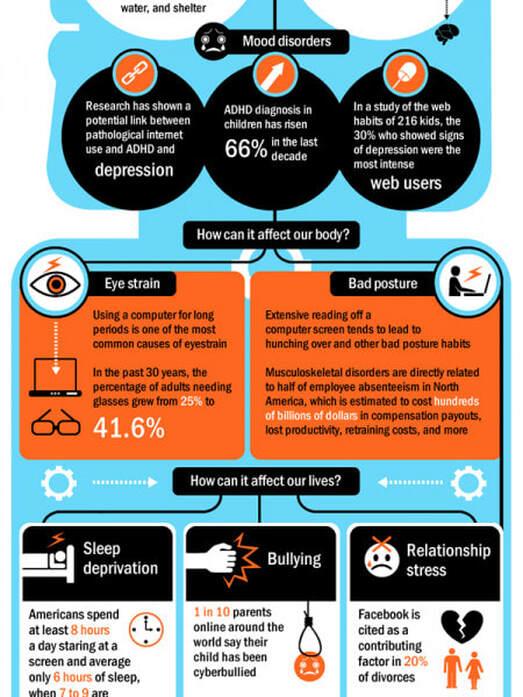
Smartphone addiction is a dependence syndrome seen among mobile phone users. Some mobile phone users exhibit problematic behaviors related to substance use disorders.
These behaviors can include preoccupation with mobile communication, excessive money or time spent on mobile phones, use of mobile phones in socially or physically inappropriate situations such as driving an automobile.
Increased use can also lead to increased time on mobile communication, adverse effects on relationships, and anxiety if separated from a mobile phone or sufficient signal.
Overuse of Smartphones is often defined as a "dependence syndrome", which is the term used by the World Health Organization (WHO Expert Committee, 1964) to replace addiction or habituation. This is categorized either as substance abuse, such as from psychoactive drugs, alcohol and tobacco under ICD-10, or a behavioral addiction, such as a mobile phone addiction.
Substance use disorders can be defined by 11 factors, according to the DSM-5, including:
Smartphone addiction can be compared to substance use disorders in that smartphones provide the drug (entertainment and connection) while acting as the means by which the drug is consumed.
A study conducted at Alabama State University on the effects of smartphones on students, defines the issue by stating that we are not addicted to smartphones themselves, but that we "are addicted to the information, entertainment, and personal connections [that a smartphone] delivers." People have an affinity for constant entertainment, and smartphones provide the quickest, most easily accessible route to it.
Prevalence:
Prevalence of mobile phone overuse depends largely on definition and thus the scales used to quantify a subject's behaviors. Two scales are in use, the 20-item self-reported Problematic Use of Mobile Phones (PUMP) scale, and the Mobile Phone Problem Use Scale (MPPUS), which have been used both with adult and adolescent populations.
There are variations in the age, gender, and percentage of the population affected problematically according to the scales and definitions used.
The prevalence among British adolescents aged 11–14 was 10%.
In India, addiction is stated at 39-44% for this age group. Under different diagnostic criteria, the estimated prevalence ranges from 0 to 38%, with self-attribution of mobile phone addiction exceeding the prevalence estimated in the studies themselves.
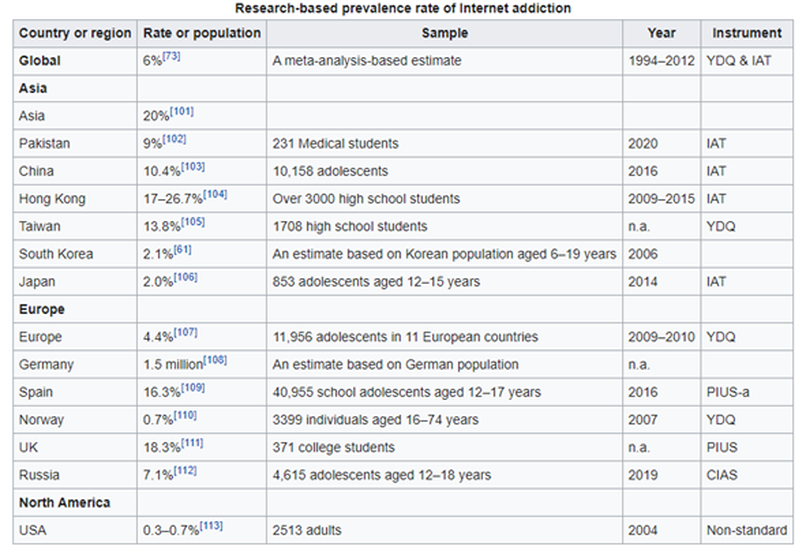
The prevalence of the related problem of Internet addiction was 4.9-10.7% in Korea, and is now regarded as a serious public health issue.
Behaviors associated with mobile-phone addiction differ between genders. Women are more likely to develop addictive mobile phone behavior than men. Men experience less social stress than women and use their mobile phones less for social purposes. Older people are less likely to develop addictive mobile phone behavior because of different social usage, stress, and greater self-regulation.
Click on any of the following blue hyperlinks for more about Smartphone Addiction:
These behaviors can include preoccupation with mobile communication, excessive money or time spent on mobile phones, use of mobile phones in socially or physically inappropriate situations such as driving an automobile.
Increased use can also lead to increased time on mobile communication, adverse effects on relationships, and anxiety if separated from a mobile phone or sufficient signal.
Overuse of Smartphones is often defined as a "dependence syndrome", which is the term used by the World Health Organization (WHO Expert Committee, 1964) to replace addiction or habituation. This is categorized either as substance abuse, such as from psychoactive drugs, alcohol and tobacco under ICD-10, or a behavioral addiction, such as a mobile phone addiction.
Substance use disorders can be defined by 11 factors, according to the DSM-5, including:
- use in larger quantities or for longer than initially intended,
- a desire to cut down or control use,
- spending a great deal of time obtaining, using, or recovering from the substance,
- use in situations in which it is physically hazardous,
- continued use of the substance despite adverse physical or psychological consequences associated with use,
- and withdrawal symptoms.
Smartphone addiction can be compared to substance use disorders in that smartphones provide the drug (entertainment and connection) while acting as the means by which the drug is consumed.
A study conducted at Alabama State University on the effects of smartphones on students, defines the issue by stating that we are not addicted to smartphones themselves, but that we "are addicted to the information, entertainment, and personal connections [that a smartphone] delivers." People have an affinity for constant entertainment, and smartphones provide the quickest, most easily accessible route to it.
Prevalence:
Prevalence of mobile phone overuse depends largely on definition and thus the scales used to quantify a subject's behaviors. Two scales are in use, the 20-item self-reported Problematic Use of Mobile Phones (PUMP) scale, and the Mobile Phone Problem Use Scale (MPPUS), which have been used both with adult and adolescent populations.
There are variations in the age, gender, and percentage of the population affected problematically according to the scales and definitions used.
The prevalence among British adolescents aged 11–14 was 10%.
In India, addiction is stated at 39-44% for this age group. Under different diagnostic criteria, the estimated prevalence ranges from 0 to 38%, with self-attribution of mobile phone addiction exceeding the prevalence estimated in the studies themselves.
The prevalence of the related problem of Internet addiction was 4.9-10.7% in Korea, and is now regarded as a serious public health issue.
Behaviors associated with mobile-phone addiction differ between genders. Women are more likely to develop addictive mobile phone behavior than men. Men experience less social stress than women and use their mobile phones less for social purposes. Older people are less likely to develop addictive mobile phone behavior because of different social usage, stress, and greater self-regulation.
Click on any of the following blue hyperlinks for more about Smartphone Addiction:
- Effects
- Tools
- See also:
- Smartphone
- Smartphone zombie
- Television addiction
- Underearners Anonymous
- Computer addiction
- Internet addiction disorder
- Nomophobia, a proposed name for the fear of being out of cellular phone contact
- Video game overuse
- Mobile phones and driving safety
- De Quervain syndrome
- Mobile phone radiation and health
- Digital detox, a period of time during which a person refrains from using electronic connecting devices
- Mobile phone § Health effects
Celebrities who died due to a Drug or Alcohol Overdose
YouTube Video: Top 10 Musicians Who Tragically Died Due to Drugs and Alcohol by WatchMojo
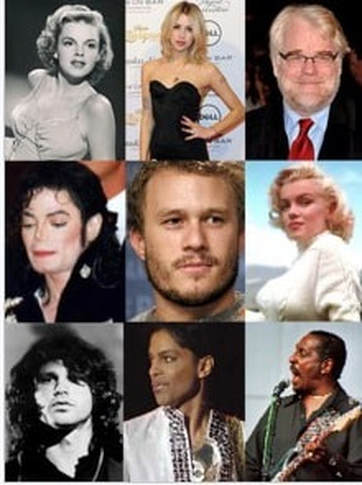
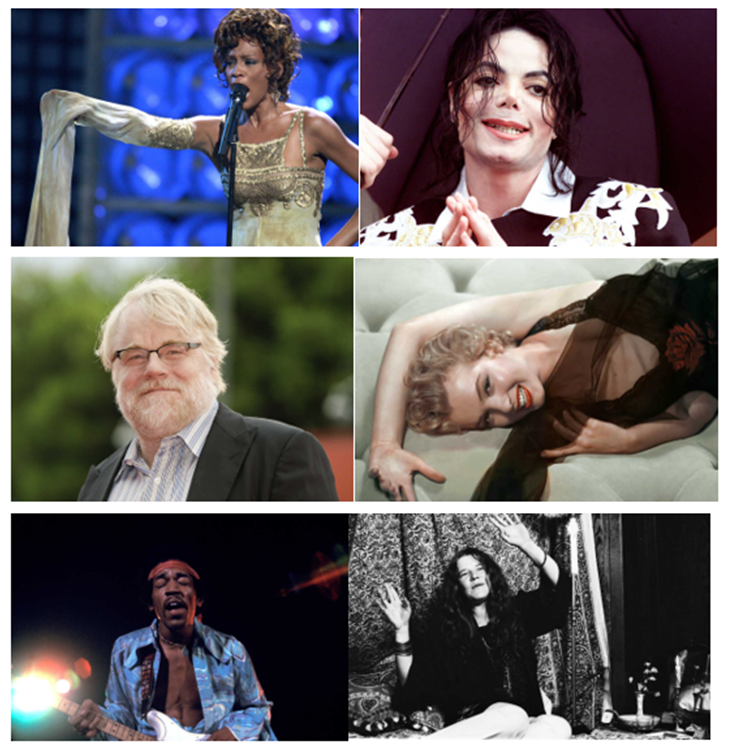
Pictured below: Notable deaths from acute drug use include (L-R):
Top Row: Judy Garland, Peaches Geldof, Philip Seymour Hoffman,
Center Row: Michael Jackson, Heath Ledger, Marilyn Monroe,
Bottom Row: Jim Morrison, Prince, and Ike Turner
For a List of Celebrities who died due to abuse of alcohol and/or drugs, click here.
Drug overdose and intoxication are significant causes of accidental death, and can also be used as a form of suicide.
Death can occur from overdosing on a single or multiple drugs, or from combined drug intoxication (CDI) due to poly drug use.
Poly drug use often carries more risk than use of a single drug, due to an increase in side effects, and drug synergy. For example, the chance of death from overdosing on opiates is greatly increased when they are consumed in conjunction with alcohol.
While they are two distinct phenomena, deaths from CDI are often misreported as overdoses. Drug overdoses and intoxication can also cause indirect deaths. For example, while marijuana does not cause fatal overdoses, being intoxicated by it can increase the chance of fatal traffic collisions.
Drug use and overdoses increased significantly in the 1800s due to the commercialization and availability of certain drugs. For example, while opium and coca had been used for centuries, their active ingredients, morphine and the cocaine alkaloid, were not isolated until 1803 and 1855 respectively.
Cocaine and various opiates were subsequently mass-produced and sold openly and legally in the Western world, resulting in widespread misuse and addiction. Drug use and addiction also increased significantly following the invention of the hypodermic syringe in 1853, with overdose being a leading cause of death among intravenous drug users.
Efforts to prohibit various drugs began to be enacted in the early 20th century, though the effectiveness of such policies is debated. Deaths from drug overdoses are increasing.
Between 2000 and 2014, fatal overdoses rose 137% in the United States, causing nearly half a million deaths in that period, and have also been continually increasing in Australia, Scotland, England, and Wales.
While prohibited drugs are generally viewed as being the most dangerous, the misuse of prescription drugs are linked to more deaths in several countries. Cocaine and heroin combined caused fewer deaths than prescriptions drugs in the United Kingdom in 2013, and fewer deaths than prescription opiates alone in the United States in 2008.
As of 2015 the drug most likely to cause fatal overdose in Australia was diazepam (Valium). While fatal overdoses are highly associated with drugs such as opiates, cocaine and alcohol, deaths from other drugs such as caffeine are extremely rare.
This alphabetical list (see above link) contains 599 notable people whose deaths can be reliably sourced to be the result of drug overdose or acute drug intoxication. Where sources indicate drug overdose or intoxication was only suspected to be the cause of death, this will be specified in the 'notes' column.
Where sources are able to indicate, deaths are specified as 'suicide', 'accidental', 'undetermined', or otherwise in the 'cause' column. Where sources do not explicitly state intent, they will be listed in this column as 'unknown'.
Deaths from accidents or misadventure caused by drug overdoses or intoxication are also included on this list.
Deaths from long-term effects of drugs, such as tobacco-related cancers and cirrhosis from alcohol, are not included, nor are deaths from lethal injection or euthanasia.
See also:
Drug overdose and intoxication are significant causes of accidental death, and can also be used as a form of suicide.
Death can occur from overdosing on a single or multiple drugs, or from combined drug intoxication (CDI) due to poly drug use.
Poly drug use often carries more risk than use of a single drug, due to an increase in side effects, and drug synergy. For example, the chance of death from overdosing on opiates is greatly increased when they are consumed in conjunction with alcohol.
While they are two distinct phenomena, deaths from CDI are often misreported as overdoses. Drug overdoses and intoxication can also cause indirect deaths. For example, while marijuana does not cause fatal overdoses, being intoxicated by it can increase the chance of fatal traffic collisions.
Drug use and overdoses increased significantly in the 1800s due to the commercialization and availability of certain drugs. For example, while opium and coca had been used for centuries, their active ingredients, morphine and the cocaine alkaloid, were not isolated until 1803 and 1855 respectively.
Cocaine and various opiates were subsequently mass-produced and sold openly and legally in the Western world, resulting in widespread misuse and addiction. Drug use and addiction also increased significantly following the invention of the hypodermic syringe in 1853, with overdose being a leading cause of death among intravenous drug users.
Efforts to prohibit various drugs began to be enacted in the early 20th century, though the effectiveness of such policies is debated. Deaths from drug overdoses are increasing.
Between 2000 and 2014, fatal overdoses rose 137% in the United States, causing nearly half a million deaths in that period, and have also been continually increasing in Australia, Scotland, England, and Wales.
While prohibited drugs are generally viewed as being the most dangerous, the misuse of prescription drugs are linked to more deaths in several countries. Cocaine and heroin combined caused fewer deaths than prescriptions drugs in the United Kingdom in 2013, and fewer deaths than prescription opiates alone in the United States in 2008.
As of 2015 the drug most likely to cause fatal overdose in Australia was diazepam (Valium). While fatal overdoses are highly associated with drugs such as opiates, cocaine and alcohol, deaths from other drugs such as caffeine are extremely rare.
This alphabetical list (see above link) contains 599 notable people whose deaths can be reliably sourced to be the result of drug overdose or acute drug intoxication. Where sources indicate drug overdose or intoxication was only suspected to be the cause of death, this will be specified in the 'notes' column.
Where sources are able to indicate, deaths are specified as 'suicide', 'accidental', 'undetermined', or otherwise in the 'cause' column. Where sources do not explicitly state intent, they will be listed in this column as 'unknown'.
Deaths from accidents or misadventure caused by drug overdoses or intoxication are also included on this list.
Deaths from long-term effects of drugs, such as tobacco-related cancers and cirrhosis from alcohol, are not included, nor are deaths from lethal injection or euthanasia.
See also:
- Lists of people by cause of death
- List of deaths from legal euthanasia and assisted suicide
- List of people executed by lethal injection
- Opioid epidemic
Tobacco has a long history in the United States. An estimated 45.3 million people, or 19.3% of all adults (aged 18 years or older), in the United States smoke cigarettes in 2010.
By state, in 2010, smoking prevalence ranged from 9.1% in Utah to 26.8% in West Virginia.
By region, in 2010, smoking prevalence was highest in the Midwest (21.8%) and South (21.0%) and lowest in the West (15.9%). In 2009 46.6 million, or 20.6 percent of adults 18 and older were current smokers. Men tend to smoke more than women. In 2009 23.5 percent of men smoked compared to 17.9 percent women.
Cigarette smoking is the leading cause of preventable death in the United States, accounting for approximately 443,000 deaths, or 1 of every 5 deaths, in the United States each year. Cigarette smoking alone has cost the United States $96 billion in direct medical expenses and $97 billion in lost productivity per year or an average of $4,260 per adult smoker.
Click on any of the following blue hyperlinks for more about Tobacco use in the United States:
Tobacco Political Lobbying:
This sub-topic covers the politics of Tobacco lobbying:
Taxation: See also Cigarette taxes in the United States
Tobacco has been taxed by state governments in the United States for decades. The cumulative revenue of US tobacco taxation exceeded $32 billion in 2010, creating a major source of income for government.
The Contraband Cigarette Trafficking Act of 1978, a law which makes cigarette smuggling a felony punishable by up to 5 years in federal prison, is used to prosecute smugglers who avoid paying the taxes on cigarettes.
The proposed Stop Tobacco Smuggling in the Territories Act of 2013 (H.R. 338; 113th Congress), if it passes during the 113th United States Congress, would update the Contraband Cigarette Trafficking Act to include American Samoa, the Commonwealth of the Northern Mariana Islands, and Guam, which were previously not covered by the law.
Lobby:
In 2010, the tobacco industry spent $16.6 million on lobbyists to represent the industry to Congress.
Major big tobacco lobbying companies include (in order of U.S. market share) Philip Morris, R. J. Reynolds Tobacco Company, and Lorillard Tobacco Co. The tobacco lobby lost a chunk of its support when the U.S. National Association of Attorneys General (NAAG) filed charges against the Tobacco Institute, a tobacco industry advocacy group.
This resulted in the Tobacco Master Settlement Agreement, which forced the organization to disband and place all records on a website.
Litigation:
The lawsuits brought against various tobacco manufacturers, attempting to hold them responsible for wrongful death, injury, or medical expenses related to cigarette smoking and other tobacco use. Cases have been brought both by individual plaintiffs and by government officials, including U.S. State Attorney General. Punitive damages for the plaintiff have often been awarded as a result of a successful litigation. However, the vast majority of court decisions have been in favor of the defendant tobacco companies.
Click on any of the following blue hyperlinks for more about Tobacco Lobbying:
By state, in 2010, smoking prevalence ranged from 9.1% in Utah to 26.8% in West Virginia.
By region, in 2010, smoking prevalence was highest in the Midwest (21.8%) and South (21.0%) and lowest in the West (15.9%). In 2009 46.6 million, or 20.6 percent of adults 18 and older were current smokers. Men tend to smoke more than women. In 2009 23.5 percent of men smoked compared to 17.9 percent women.
Cigarette smoking is the leading cause of preventable death in the United States, accounting for approximately 443,000 deaths, or 1 of every 5 deaths, in the United States each year. Cigarette smoking alone has cost the United States $96 billion in direct medical expenses and $97 billion in lost productivity per year or an average of $4,260 per adult smoker.
Click on any of the following blue hyperlinks for more about Tobacco use in the United States:
- History of commercial tobacco
- Economic impact of the early tobacco industry
- Legislation
- Costs
- Companies and products
- Lobbying and organizations
- Critics
- See also:
- Prevalence of tobacco consumption#United States
- List of smoking bans in the United States
- Smoker Protection Law
- Steven C. Parrish, the Senior Vice President of Philip Morris
- C. C. Little - tobacco researcher
- Tobacco-Free Pharmacies
- Supreme Court Cases on Cigarettes, Smoking and Tobacco
Tobacco Political Lobbying:
This sub-topic covers the politics of Tobacco lobbying:
Taxation: See also Cigarette taxes in the United States
Tobacco has been taxed by state governments in the United States for decades. The cumulative revenue of US tobacco taxation exceeded $32 billion in 2010, creating a major source of income for government.
The Contraband Cigarette Trafficking Act of 1978, a law which makes cigarette smuggling a felony punishable by up to 5 years in federal prison, is used to prosecute smugglers who avoid paying the taxes on cigarettes.
The proposed Stop Tobacco Smuggling in the Territories Act of 2013 (H.R. 338; 113th Congress), if it passes during the 113th United States Congress, would update the Contraband Cigarette Trafficking Act to include American Samoa, the Commonwealth of the Northern Mariana Islands, and Guam, which were previously not covered by the law.
Lobby:
In 2010, the tobacco industry spent $16.6 million on lobbyists to represent the industry to Congress.
Major big tobacco lobbying companies include (in order of U.S. market share) Philip Morris, R. J. Reynolds Tobacco Company, and Lorillard Tobacco Co. The tobacco lobby lost a chunk of its support when the U.S. National Association of Attorneys General (NAAG) filed charges against the Tobacco Institute, a tobacco industry advocacy group.
This resulted in the Tobacco Master Settlement Agreement, which forced the organization to disband and place all records on a website.
Litigation:
The lawsuits brought against various tobacco manufacturers, attempting to hold them responsible for wrongful death, injury, or medical expenses related to cigarette smoking and other tobacco use. Cases have been brought both by individual plaintiffs and by government officials, including U.S. State Attorney General. Punitive damages for the plaintiff have often been awarded as a result of a successful litigation. However, the vast majority of court decisions have been in favor of the defendant tobacco companies.
Click on any of the following blue hyperlinks for more about Tobacco Lobbying:
- History
- See also:
- A Frank Statement
- Operation Berkshire
- Tobacco Master Settlement Agreement
- Tobacco MSA (Alabama)
- Tobacco MSA (Hawaii)
- Tobacco MSA (New York)
- Merchants of Doubt and 2014 film Merchants of Doubt based on the 2010 book.
- No-Smoking.org
- Tobacco Institute Documents-Part of Master Settlement Agreement
- UCSF Tobacco Industry Videos Collection
- UCSF Tobacco Industry Audio Recordings Collection
- State and Local Tax Revenue, Selected Years 1977-2006
Electronic Cigarette (aka "Vaping")
- YouTube Video: Teen was in the fight for her life after vaping a cartridge a day I Nightline
- YouTube Video: Vaping: The Hit Your Brain Takes
- YouTube Video: Vaping: what people are getting wrong | The Economist
An electronic cigarette is an electronic device that simulates tobacco smoking. It consists of an atomizer, a power source such as a battery, and a container such as a cartridge or tank.
Instead of smoke, the user inhales vapor. As such, using an e-cigarette is often called "vaping". The atomizer is a heating element that atomizes a liquid solution called e-liquid. E-cigarettes are activated by taking a puff or pressing a button. Some look like traditional cigarettes, and most versions are reusable.
E-cigarettes create an aerosol, commonly called vapor, made of particulate matter. The vapor typically contains propylene glycol, glycerin, nicotine, flavors, and traces of nitrosamines, other toxicants, carcinogens, heavy metals, and metal nanoparticles. Its exact composition varies, and depends on several factors including user behavior.
The health effects of electronic cigarettes remain uncertain, but they are likely less harmful than smoking tobacco. E-cigarette vapor contains fewer toxic chemicals, in lower concentrations, than cigarette smoke, but also contains harmful chemicals not found in tobacco smoke.
Nicotine is highly addictive. People who vape are more likely to start smoking. For smokers who are unable or unwilling to quit using conventional smoking cessation methods such as nicotine replacement therapy (NRT), vaping has a role in tobacco harm reduction. Research suggests that e‐cigarettes may help people to stop smoking cigarettes.
Construction:
Further information: Construction of electronic cigarettes § E-cigarette liquid
An electronic cigarette consists of an atomizer, a power source such as a battery, and a container for the e-liquid such as a cartridge or tank.
E-cigarettes have evolved over time, and the different designs are classified in generations.
First-generation e-cigarettes tend to look like traditional cigarettes, though there is some variation in size, and so are called "cigalikes".
Second-generation devices are larger overall and look less like traditional cigarettes.
Third-generation devices include mechanical mods and variable voltage devices.
The fourth-generation includes Sub ohm tanks (meaning that they have electrical resistance of less than 1 Ohm) and temperature control devices.
The voltage for first-generation e-cigarettes is about 3.7 and second-generation e-cigarettes can be adjusted from 3 V to 6 V, while more recent devices can go up to 8 V.
There are also pod mod devices that use protonated nicotine, rather than free-base nicotine found in earlier generations, providing higher nicotine yields through the production of aerosolized protonated nicotine.
E-liquid is the mixture used in vapor products such as e-cigarettes. It usually contains propylene glycol, glycerin, nicotine, flavorings, additives, and contaminants. E-liquid formulations vary widely.
A typical e-liquid comprises propylene glycol and glycerin (95%), and flavorings, nicotine, and other additives (5%). Some e-liquids lack propylene glycol, nicotine, or flavors. The flavorings may be natural, artificial, or organic. Over 80 chemicals such as formaldehyde and metallic nanoparticles have been found in the e-liquid. There are many e-liquid manufacturers, and more than 15,000 flavors.
In the US, under Food and Drug Administration (FDA) rules, e-liquids must comply with manufacturing standards. Industry standards are published by the American E-liquid Manufacturing Standards Association (AEMSA). EU standards are in the EU Tobacco Products Directive.
Use:
Popularity:
Main article: Usage of electronic cigarettes
Since their entrance to the market around 2003, e-cigarette use has risen rapidly. In 2011 there were about 7 million adult e-cigarette users globally, rising to 41 million in 2018 and to 68 million in 2020 compared with 1.1 billion cigarette smokers.
E-cigarette use is highest in China, the US, and Europe, with China having the most e-cigarette users. The rise was thought to be due to advertising to young people; their low cost compared to tobacco; and the perception that e-cigarettes are safer than tobacco.
USA:
In 2020, about 20% of US high school students reported using an e-cigarette at least once in the past 30 days. As of 2018, about 3% of US adults use e-cigarettes some days or every day.
UK:
In the UK, current e-cigarette use increased from 1.7% of the adult population in 2012 to 7.1% in 2019 and then decreased to 6.3% in 2020. As of 2020, about 59% of UK adult e-cigarette users are former smokers, 38% currently use both cigarettes and e-cigarettes, and 3% have never smoked a cigarette.
Australia:
According to a 2019 report, approximately 520,000 adult Australians were vaping. That was more than twice as much as in a 2016 survey where only 240,000 Australians were vapers.
Progression:
Historically, many users began with a disposable e-cigarette resembling a tobacco cigarette. They often progress to later-generation devices and may adjust their devices to provide more vapor. Experienced users often prefer rechargeable e-cigarettes. Women prefer disposable e-cigarettes, and young adults pay more attention to modifiability (the ability to change the power of the e-cigarette or change pieces of e-cigarettes).
Modifiability increases the chance of starting vaping among young people.
Most vapers use a refillable tank system, allowing them to mix their own liquid giving control over flavor and strength. Experienced vapers rank customizability as the most important consideration in choosing a device. Users ranked nicotine strength as an important factor for choosing among various e-cigarettes, though such preference could vary by smoking status, e-cigarette use history, and gender.
Non-smokers and inexperienced e-cigarettes users tended to prefer no nicotine or low nicotine e-cigarettes while smokers and experienced e-cigarettes users preferred medium and high nicotine e-cigarettes.
Young people:
Worldwide, increasing numbers of young people in some countries are vaping, and rates were found to be especially high in the US, Poland, and Hungary as of 2013-2015.
With access to e-cigarettes, young people have been using tobacco about a quarter as often. Vaping among adolescents grew every year until 2017. There appears to be an increase of one-time e-cigarette use among young people worldwide.
Most young e-cigarette users have never smoked, but there is a substantial minority who both vape and smoke, which indicates that e-cigarettes may be a starting point for nicotine use. Young people who would not smoke are vaping, and young people who vape are more likely to start smoking.
Twice as many young people vaped in 2014 than also used traditional cigarettes. Young people who smoke tobacco or marijuana, or who drink alcohol, are much more likely to vape. Among young people who have tried vaping, most used a flavored product the first time.
Most young people are not vaping to help them quit tobacco. Vaping correlates with smoking among young people, even in those who would otherwise be unlikely to smoke. Experimenting with vaping encourages young people to continue smoking.
A 2015 study found minors had little resistance to buying e-cigarettes online. Teenagers may not admit using e-cigarettes, but use, for instance, a hookah pen. As a result, self-reporting may be lower in surveys.
Motivation:
There are varied reasons for e-cigarette use. Most users are trying to quit smoking, but a large proportion of use is recreational or as a way to get around smoke-free laws.
Many people who use e-cigarettes still smoke, raising concern that they may be delaying or deterring quitting. Some people say they want to quit smoking by vaping, but others vape to circumvent smoke-free laws and policies, or to cut back on cigarette smoking. Many people vape because they believe vaping is safer than smoking.
Concerns over avoiding stains on teeth or odor from smoke on clothes in some cases prompted interest in or use of e-cigarettes. Some e-cigarettes appeal considerably to people curious in technology who want to customize their devices.
There appears to be a hereditary component to tobacco use, which probably plays a part in transitioning of e-cigarette use from experimentation to routine use.
Many users say they like the choice of flavors and comparatively low price of e-cigarettes compared to cigarettes.
Gateway theory:
In the context of drugs, the gateway hypothesis is that using less harmful drugs can lead to a future risk of using more harmful drugs or crime. Some research suggests vaping is a "gateway" to smoking. A 2020 report of 25 studies and three systematic reviews found that every study examined found that e-cigarette use was associated with increased odds of later smoking.
However, it is also plausible that any favorable relation between vaping and starting smoking is a result of common risk factors. Gateway theories have always been controversial in the field of addictions, and they are difficult to test. Research that controls for confounding factors generally finds that vaping is an "exit ramp" from smoking.
In other words, rather than leading to more cigarette smoking, e-cigarette use may be leading to less smoking.
Because those with mental illness are highly predisposed to nicotine addiction, those who try e-cigarettes may be more likely to become dependent, raising concerns about facilitating a transition to combustible tobacco use. Even if an e-cigarette contains no nicotine, the user mimics the actions of smoking. This may renormalize tobacco use in the general public.
There is a possible risk of re-normalizing of tobacco use in areas where smoking is banned. Government intervention is recommended to keep children safe from the re-normalizing of tobacco, according to a 2017 review.
The "catalyst model" suggests that vaping may proliferate smoking in minors by sensitizing minors to nicotine with the use of a type of nicotine that is more pleasing and without the negative attributes of regular cigarettes.
A 2016 review, based on the catalyst model, "indicate that the perceived health risks, specific product characteristics (such as taste, price, and inconspicuous use), and higher levels of acceptance among peers and others potentially make e-cigarettes initially more attractive to adolescents than tobacco cigarettes. Later, increasing familiarity with nicotine could lead to the reevaluation of both electronic and tobacco cigarettes and subsequently to a potential transition to tobacco smoking."
Health effects:
The benefits and the health risks of e-cigarettes are uncertain, including their long-term effects. There is tentative evidence they may help people quit smoking, but smoking cessation medicine is at least as effective.
Pods contain different doses of nicotine, and these levels are regulated in some countries.
Following the possibility of nicotine addiction from e-cigarette use, there is concern children and young people may start smoking cigarettes. Their part in tobacco harm reduction is unclear, while another review found they appear to have the potential to lower tobacco-related death and disease.
Regulated US Food and Drug Administration (US FDA) nicotine replacement products may be safer than e-cigarettes, but e-cigarettes are generally seen as safer than combusted tobacco products.
The risk of early death may be similar to that of smokeless tobacco. The risk of serious adverse events was reported in 2016 to be low. Less serious adverse effects include abdominal pain, headache, blurry vision, throat and mouth irritation, vomiting, nausea, and coughing.
Nicotine is harmful. In 2019 and 2020, an outbreak of severe vaping lung illness in the US was strongly linked to vitamin E acetate by the CDC. E-cigarettes produce similarly high levels of particulates in the air as do tobacco-cigarettes. There is "only limited evidence showing adverse respiratory and cardiovascular effects in humans", with the authors of a 2020 review calling for more long-term studies on the subject. A 2020 review found e-cigarettes increase the risk of asthma by 40% and chronic obstructive pulmonary disease by 50%.
Pregnancy:
The Royal College of Midwives states, "While vaping devices such as electronic cigarettes (e-cigs) do contain some toxins, they are at far lower levels than found in tobacco smoke. If a pregnant woman who has been smoking chooses to use an e-cig and it helps her to quit smoking and stay smoke-free, she should be supported to do so."
Based on the available evidence on e-cigarette safety, there was also "no reason to believe that use of an e-cig has any adverse effect on breastfeeding." The statement went on to say, "vaping should continue, if it is helpful to quitting smoking and staying smoke-free". The UK National Health Service says: "If using an e-cigarette helps you to stop smoking, it is much safer for you and your baby than continuing to smoke.".
Many women who vape continue to do so during pregnancy because of the perceived safety of e-cigarettes compared to tobacco.
United States:
In one of the few studies identified, a 2015 survey of 316 pregnant women in a Maryland clinic found that the majority had heard of e-cigarettes, 13% had used them, and 0.6% were current daily users. These findings are of concern because the dose of nicotine delivered by e-cigarettes can be as high or higher than that delivered by traditional cigarettes.
Data from two states in the Pregnancy Risk Assessment System (PRAMS) show that in 2015—roughly the mid-point of the study period—10.8% of the sample used e-cigarettes in the three months prior to the pregnancy while 7.0%, 5.8%, and 1.4% used these products at the time of the pregnancy, in the first trimester, and at birth respectively.
According to National Health Interview Survey (NHIS) data from 2014 to 2017, 38.9% of pregnant smokers used e-cigarettes compared to only 13.5% of non-pregnant, reproductive age women smokers. A health economic study found that passing an e-cigarette minimum legal sale age law in the United States increased teenage prenatal smoking by 0.6 percentage points and had no effect on birth outcomes.
Nevertheless, additional research needs to be done on the health effects of electronic cigarette use during pregnancy.
Harm reduction:
Harm reduction refers to any reduction in harm from a prior level. Harm minimization strives to reduce harms to the lowest achievable level. When a person does not want to quit nicotine, harm minimization means striving to eliminate tobacco exposure by replacing it with vaping. E-cigarettes can reduce smokers' exposure to carcinogens and other toxic chemicals found in tobacco.
Tobacco harm reduction has been a controversial area of tobacco control. Health advocates have been slow to support a harm reduction method out of concern that tobacco companies cannot be trusted to sell products that will lower the risks associated with tobacco use. A large number of smokers want to reduce harm from smoking by using e-cigarettes. The argument for harm reduction does not take into account the adverse effects of nicotine.
There cannot be a defensible reason for harm reduction in children who are vaping with a base of nicotine. Quitting smoking is the most effective strategy to tobacco harm reduction.
Tobacco smoke contains 100 known carcinogens and 900 potentially cancer-causing chemicals, but e-cigarette vapor contains less of the potential carcinogens than found in tobacco smoke. A study in 2015 using a third-generation device found levels of formaldehyde were greater than with cigarette smoke when adjusted to a maximum power setting.
E-cigarettes cannot be considered safe because there is no safe level for carcinogens. Due to their similarity to traditional cigarettes, e-cigarettes could play a valuable role in tobacco harm reduction. However, the public health community remains divided concerning the appropriateness of endorsing a device whose safety and efficacy for smoking cessation remain unclear.
Overall, the available evidence supports the cautionary implementation of harm reduction interventions aimed at promoting e-cigarettes as attractive and competitive alternatives to cigarette smoking, while taking measures to protect vulnerable groups and individuals.
The core concern is that smokers who could have quit entirely will develop an alternative nicotine addiction. Dual use may be an increased risk to a smoker who continues to use even a minimal amount of traditional cigarettes, rather than quitting.
The promotion of vaping as a harm reduction aid is premature, while a 2011 review found they appear to have the potential to lower tobacco-related death and disease. Evidence to substantiate the potential of vaping to lower tobacco-related death and disease is unknown.
The health benefits of reducing cigarette use while vaping is unclear. E-cigarettes could have an influential role in tobacco harm reduction. The authors warned against the potential harm of excessive regulation and advised health professionals to consider advising smokers who are reluctant to quit by other methods to switch to e-cigarettes as a safer alternative to smoking.
A 2014 review recommended that regulations for e-cigarettes could be similar to those for dietary supplements or cosmetic products to not limit their potential for harm reduction.
A 2012 review found e-cigarettes could considerably reduce traditional cigarettes use and they likely could be used as a lower risk replacement for traditional cigarettes, but there is not enough data on their safety and efficacy to draw definite conclusions. There is no research available on vaping for reducing harm in high-risk groups such as people with mental disorders.
A 2014 PHE report concluded that hazards associated with products currently on the market are probably low, and apparently much lower than smoking. However, harms could be reduced further through reasonable product standards.
British Medical Association encourages health professionals to recommend conventional nicotine replacement therapies, but for patients unwilling to use or continue using such methods, health professionals may present e-cigarettes as a lower-risk option than tobacco smoking.
The American Association of Public Health Physicians (AAPHP) suggests those who are unwilling to quit tobacco smoking or unable to quit with medical advice and pharmaceutical methods should consider other nicotine-containing products such as e-cigarettes and smokeless tobacco for long-term use instead of smoking.
A 2014 WHO report concluded that some smokers will switch completely to e-cigarettes from traditional tobacco but a "sizeable" number will use both. This report found that such "dual-use" of e-cigarettes and tobacco "will have much smaller beneficial effects on overall survival compared with quitting smoking completely."
Smoking cessation:
The use of e-cigarettes for quitting smoking is controversial. Limited evidence suggests that e‐cigarettes probably do help people to stop smoking. Data regarding their use includes at least 26 randomized controlled trials and a number of user surveys, case reports, and cohort studies.
At least once recent review (2019) found that vaping did not seem to greatly increase the odds of quitting smoking. As a result of the data being confronted with methodological and study design limitations, no firm conclusions can be drawn in respect to their efficacy and safety. A 2016 review found that the combined abstinence rate among smokers using e-cigarettes in prospective studies was 29.1%.
The same review noted that few clinical trials and prospective studies had yet been conducted on their effectiveness, and only one randomized clinical trial had included a group using other quit smoking methods. No long-term trials have been conducted for their use as a smoking cessation aid.
It is still not evident as to whether vaping can adequately assist with quitting smoking at the population level. A 2015 PHE report recommends for smokers who cannot or do not want to quit to use e-cigarettes as one of the main steps to lower smoking-related disease, while a 2015 US PSTF statement found there is not enough evidence to recommend e-cigarettes for quitting smoking in adults, pregnant women, and adolescents.
In 2021 the US PSTF concluded the evidence is still insufficient to recommend e-cigarettes for quitting smoking, finding that the balance of benefits and harms cannot be determined.
As of January 2018, systematic reviews collectively agreed that there is insufficient evidence to unequivocally determine whether vaping helped people abstain from smoking. A 2020 systematic review and meta-analysis of 64 studies found that on the whole as consumer products e-cigarettes do not increase quitting smoking.
A small number of studies have looked at whether using e-cigarettes reduces the number of cigarettes smokers consume. E-cigarette use may decrease the number of cigarettes smoked, but smoking just one to four cigarettes daily greatly increases the risk of cardiovascular disease compared to not smoking. The extent to which decreasing cigarette smoking with vaping leads to quitting is unknown.
It is unclear whether e-cigarettes are only helpful for particular types of smokers. Vaping with nicotine may reduce tobacco use among daily smokers. Whether or not vaping is potentially effective for quitting smoking may rely upon whether it was used as part of making an effort to quit or not.
Comparing e-cigarettes to nicotine replacement therapy, a 2020 review found "moderate-certainty evidence" that e-cigarettes are more effective than nicotine replacement therapy (NRT) for quitting smoking. The difference was minor, indicating that compared to NRT, e-cigarettes might lead to an additional four successful quitters per 100.
However, some studies have people who vaped were not more likely to give up smoking than people who did not vape. and previous reviews have found that e-cigarettes were not been proven to be more effective than smoking cessation medicine and regulated US FDA medicine.
A randomized trial stated 29% of e-cigarette users were still vaping at 6 months, while only 8% of patch users still wore patches at 6 months, suggesting that some people are switching to cigarettes rather than fully quitting all tobacco use. The potential adverse effects such as normalizing smoking have not been adequately studied.
While some surveys reported improved quitting smoking, particularly with intensive e-cigarette users, several studies showed a decline in quitting smoking in dual users of cigarettes and e-cigarettes. Compared to many alternative quitting smoking medicines in early development in clinical trials including e-cigarettes, cytisine may be the most encouraging in efficacy and safety with an inexpensive price.
Other kinds of nicotine replacement products are usually covered by health systems, but because e-cigarettes are not medically licensed they are not covered.
One of the challenges in studying e-cigarettes is that there are hundreds of brands and models of e-cigarettes sold that vary in the design and operation of the devices and composition of the liquid, and the technology continues to change.
E-cigarettes have not been subjected to the same type of efficacy testing as nicotine replacement products. There are also social concerns - use of e-cigarettes may normalize tobacco use and prolong cigarette use for people who could have quit instead, or it could put extra pressure on smokers to stop cigarette smoking because e-cigarettes are a more socially acceptable alternative.
The evidence indicates smokers are more frequently able to completely quit smoking using tank devices compared to cigarette versions , which may be due to their more efficient nicotine delivery. There is low quality evidence that vaping assists smokers to quit smoking in the long-term compared with nicotine-free vaping.
Nicotine-containing e-cigarettes were associated with greater effectiveness for quitting smoking than e-cigarettes without nicotine. A 2013 study in smokers who were not trying to quit, found that vaping, with or without nicotine decreased the number of cigarettes consumed. E-cigarettes without nicotine may reduce tobacco cravings because of the smoking-related physical stimuli.
A 2015 meta-analysis on clinical trials found that e-cigarettes containing nicotine are more effective than nicotine-free ones for quitting smoking. They compared their finding that nicotine-containing e-cigarettes helped 20% of people quit with the results from other studies that found nicotine replacement products helps 10% of people quit.
A 2016 review found low quality evidence of a trend towards benefit of e-cigarettes with nicotine for smoking cessation. In terms of whether flavored e-cigarettes assisted quitting smoking, the evidence is inconclusive. Tentative evidence indicates that health warnings on vaping products may influence users to give up vaping.
As of 2020, the efficacy and safety of vaping for quitting smoking during pregnancy was unknown. No research is available to provide details on the efficacy of vaping for quitting smoking during pregnancy. There is robust evidence that vaping is not effective for quitting smoking among adolescents.
In view of the shortage of evidence, vaping is not recommend for cancer patients, although for all patients vaping is likely less dangerous than smoking cigarettes. The effectiveness of vaping for quitting smoking among vulnerable groups is uncertain.
Safety:
Main articles:
As of 2015, research had not yet provided a consensus on the risks of e-cigarette use.
There is little data about their safety, and a considerable variety of liquids are used as carriers, and thus are present in the aerosol delivered to the user. Reviews of the safety of e-cigarettes have reached quite different conclusions.
A 2014 WHO report cautioned about potential risks of using e-cigarettes. Regulated US FDA products such as nicotine inhalers may be safer than e-cigarettes, but e-cigarettes are generally seen as safer than combusted tobacco products such as cigarettes and cigars. The risk of early death is anticipated to be similar to that of smokeless tobacco.
Since vapor does not contain tobacco and does not involve combustion, users may avoid several harmful constituents usually found in tobacco smoke, such as ash, tar, and carbon monoxide. However, e-cigarette use with or without nicotine cannot be considered risk-free because the long-term effects of e-cigarette use are unknown.
The cytotoxicity of e-liquids varies, and contamination with various chemicals have been detected in the liquid. Metal parts of e-cigarettes in contact with the e-liquid can contaminate it with metal particles. Many chemicals including carbonyl compounds such as formaldehyde can inadvertently be produced when the nichrome wire (heating element) that touches the e-liquid is heated and chemically reacted with the liquid.
Normal usage of e-cigarettes, and reduced voltage (3.0 V) devices generate very low levels of formaldehyde. The later-generation and "tank-style" e-cigarettes with a higher voltage (5.0 V) may generate equal or higher levels of formaldehyde compared to smoking.
A 2015 report by Public Health England found that high levels of formaldehyde only occurred in overheated "dry-puffing". Users detect the "dry puff" (also known as a "dry hit") and avoid it, and they concluded that "There is no indication that EC users are exposed to dangerous levels of aldehydes." However, e-cigarette users may "learn" to overcome the unpleasant taste due to elevated aldehyde formation, when the nicotine craving is high enough.
E-cigarette users who use devices that contain nicotine are exposed to its potentially harmful effects. Nicotine is associated with cardiovascular disease, possible birth defects, and poisoning. In vitro studies of nicotine have associated it with cancer, but carcinogenicity has not been demonstrated in vivo. There is inadequate research to show that nicotine is associated with cancer in humans. The risk is probably low from the inhalation of propylene glycol and glycerin.
No information is available on the long-term effects of the inhalation of flavors.
In 2019-2020, there was an outbreak of vaping-related lung illness in the US and Canada, primarily related to vaping THC with vitamin E acetate.
E-cigarettes create vapor that consists of fine and ultrafine particles of particulate matter, with the majority of particles in the ultrafine range. The vapor have been found to contain propylene glycol, glycerin, nicotine, flavors, small amounts of toxicants, carcinogens, and heavy metals, as well as metal nanoparticles, and other substances.
Exactly what the vapor consists of varies in composition and concentration across and within manufacturers, and depends on the contents of the liquid, the physical and electrical design of the device, and user behavior, among other factors. E-cigarette vapor potentially contains harmful chemicals not found in tobacco smoke. The majority of toxic chemicals found in cigarette smoke are absent in e-cigarette vapor.
E-cigarette vapor contains lower concentrations of potentially toxic chemicals than with cigarette smoke. Those which are present, are mostly below 1% of the corresponding levels permissible by workplace safety standards. But workplace safety standards do not recognize exposure to certain vulnerable groups such as people with medical ailments, children, and infants who may be exposed to second-hand vapor.
Concern exists that some of the mainstream vapor exhaled by e-cigarette users may be inhaled by bystanders, particularly indoors, although e-cigarette pollutant levels are much lower than for cigarettes and likely to pose a much lower risk, if any, compared to cigarettes.
E-cigarette use by a parent might lead to inadvertent health risks to offspring. A 2014 review recommended that e-cigarettes should be regulated for consumer safety. There is limited information available on the environmental issues around production, use, and disposal of e-cigarettes that use cartridges. E-cigarettes that are not reusable may contribute to the problem of electronic waste.
Addiction:
Further information: Effects of electronic cigarettes on human brain development
Nicotine, a key ingredient in most e-liquids, is well-recognized as one of the most addictive substances, as addictive as heroin and cocaine. Addiction is believed to be a disorder of experience-dependent brain plasticity. The reinforcing effects of nicotine play a significant role in the beginning and continuing use of the drug.
First-time nicotine users develop a dependence about 32% of the time. Chronic nicotine use involves both psychological and physical dependence. Nicotine-containing e-cigarette vapor induces addiction-related neurochemical, physiological and behavioral changes.
Nicotine affects neurological, neuromuscular, cardiovascular, respiratory, immunological and gastrointestinal systems. Neuroplasticity within the brain's reward system occurs as a result of long-term nicotine use, leading to nicotine dependence. The neurophysiological activities that are the basis of nicotine dependence are intricate. It includes genetic components, age, gender, and the environment.
Nicotine addiction is a disorder which alters different neural systems such as dopaminergic, glutamatergic, GABAergic, serotoninergic, that take part in reacting to nicotine. Long-term nicotine use affects a broad range of genes associated with neurotransmission, signal transduction, and synaptic architecture. The ability to quitting smoking is affected by genetic factors, including genetically based differences in the way nicotine is metabolized.
Nicotine is a parasympathomimetic stimulant that binds to and activates nicotinic acetylcholine receptors in the brain, which subsequently causes the release of dopamine and other neurotransmitters, such as:
Corticotropin-releasing factor, Neuropeptide Y, orexins, and norepinephrine are involved in nicotine addiction. Continuous exposure to nicotine can cause an increase in the number of nicotinic receptors, which is believed to be a result of receptor desensitization and subsequent receptor upregulation.
Long-term exposure to nicotine can also result in downregulation of glutamate transporter 1. Long-term nicotine exposure upregulates cortical nicotinic receptors, but it also lowers the activity of the nicotinic receptors in the cortical vasodilation region. These effects are not easily understood. With constant use of nicotine, tolerance occurs at least partially as a result of the development of new nicotinic acetylcholine receptors in the brain.
After several months of nicotine abstinence, the number of receptors go back to normal. The extent to which alterations in the brain caused by nicotine use are reversible is not fully understood. Nicotine also stimulates nicotinic acetylcholine receptors in the adrenal medulla, resulting in increased levels of epinephrine and beta-endorphin. Its physiological effects stem from the stimulation of nicotinic acetylcholine receptors, which are located throughout the central and peripheral nervous systems.
When nicotine intake stops, the upregulated nicotinic acetylcholine receptors induce withdrawal symptoms. These symptoms can include cravings for nicotine, anger, irritability, anxiety, depression, impatience, trouble sleeping, restlessness, hunger, weight gain, and difficulty concentrating.
When trying to quit smoking with vaping a base containing nicotine, symptoms of withdrawal can include irritability, restlessness, poor concentration, anxiety, depression, and hunger. The changes in the brain cause a nicotine user to feel abnormal when not using nicotine. In order to feel normal, the user has to keep his or her body supplied with nicotine.
E-cigarettes may reduce cigarette craving and withdrawal symptoms. It is not clear whether e-cigarette use will decrease or increase overall nicotine addiction, but the nicotine content in e-cigarettes is adequate to sustain nicotine dependence. Chronic nicotine use causes a broad range of neuroplastic adaptations, making quitting hard to accomplish.
A 2015 study found that users vaping non-nicotine e-liquid exhibited signs of dependence. Experienced users tend to take longer puffs which may result in higher nicotine intake. It is difficult to assess the impact of nicotine dependence from e-cigarette use because of the wide range of e-cigarette products. The addiction potential of e-cigarettes may have risen because as they have progressed, they delivery nicotine better.
A 2015 American Academy of Pediatrics (AAP) policy statement stressed "the potential for these products to addict a new generation of youth to nicotine and reverse more than 50 years of public health gains in tobacco control."
The World Health Organization (WHO) is concerned about starting nicotine use among non-smokers, and the National Institute on Drug Abuse said e-cigarettes could maintain nicotine addiction in those who are attempting to quit. The limited available data suggests that the likelihood of excessive use of e-cigarettes is smaller than traditional cigarettes.
No long-term studies have been done on the effectiveness of e-cigarettes in treating tobacco addiction, but some evidence suggests that dual use of e-cigarettes and traditional cigarettes may be associated with greater nicotine dependence.
There is concern that children may progress from vaping to smoking. Adolescents are likely to underestimate nicotine's addictiveness. Vulnerability to the brain-modifying effects of nicotine, along with youthful experimentation with e-cigarettes, could lead to a lifelong addiction. A long-term nicotine addiction from using a vape may result in using other tobacco products.
The majority of addiction to nicotine starts during youth and young adulthood. Adolescents are more likely to become nicotine dependent than adults. The adolescent brain seems to be particularly sensitive to neuroplasticity as a result of nicotine.
Minimal exposure could be enough to produce neuroplastic alterations in the very sensitive adolescent brain. A 2014 review found that in studies up to a third of youth who have not tried a traditional cigarette have used e-cigarettes. The degree to which teens are using e-cigarettes in ways the manufacturers did not intend, such as increasing the nicotine delivery, is unknown, as is the extent to which e-cigarette use may lead to addiction or substance dependence in youth.
Positions:
Main article: Positions of medical organizations on electronic cigarettes
Because of overlap with tobacco laws and medical drug policies, e-cigarette legislation is being debated in many countries. The revised EU Tobacco Products Directive came into effect in May 2016, providing stricter regulations for e-cigarettes.
In February 2010 the US District Court ruled against the FDA's seizure of E-Cigarettes as a "drug-device" and in December 2010 the US Court of Appeals confirmed them to be tobacco products which were by then subject to regulation under the 2009 FSPTC Act.
In August 2016, the US FDA extended its regulatory power to include e-cigarettes, cigars, and "all other tobacco products". Large tobacco companies have greatly increased their marketing efforts.
The scientific community in US and Europe are primarily concerned with their possible effect on public health. There is concern among public health experts that e-cigarettes could renormalize smoking, weaken measures to control tobacco. and serve as a gateway for smoking among youth.
The public health community is divided over whether to support e-cigarettes, because their safety and efficacy for quitting smoking is unclear. Many in the public health community acknowledge the potential for their quitting smoking and decreasing harm benefits, but there remains a concern over their long-term safety and potential for a new era of users to get addicted to nicotine and then tobacco.
There is concern among tobacco control academics and advocates that prevalent universal vaping "will bring its own distinct but as yet unknown health risks in the same way tobacco smoking did, as a result of chronic exposure", among other things.
Medical organizations differ in their views about the health implications of vaping There is general agreement that e-cigarettes expose users to fewer toxicants than tobacco cigarettes. Some healthcare groups and policy makers have hesitated to recommend e-cigarettes for quitting smoking, because of limited evidence of effectiveness and safety. Some have advocated bans on e-cigarette sales and others have suggested that e-cigarettes may be regulated as tobacco products but with less nicotine content or be regulated as a medicinal product.
A 2016 World Health Organization (WHO) report found that the scientific evidence for the effectiveness of vaping for quitting smoking is "scant and of low certainty". Healthcare organizations in the UK in 2015 have encouraged smokers to try e-cigarettes to help them quit smoking and also encouraged e-cigarette users to quit smoking tobacco entirely.
In 2016, the US Food and Drug Administration (US FDA) stated that "Although ENDS [electronic nicotine delivery systems] may potentially provide cessation benefits to individual smokers, no ENDS have been approved as effective cessation aids."
In 2019 the European Respiratory Society stated that "The long-term effects of ECIG use are unknown, and there is therefore no evidence that ECIGs are safer than tobacco in the long term." Following hundreds of possible cases of severe lung illness and five confirmed deaths associated with vaping in the US, the Centers for Disease Control and Prevention stated on 6 September 2019 that people should consider not using vaping products while their investigation is ongoing.
Regulation:
Main articles:
Regulation of e-cigarettes varies across countries and states, ranging from no regulation to banning them entirely. For instance, e-cigarettes are illegal in Japan, forcing the market to use heated tobacco products for cigarette alternatives. Others have introduced strict restrictions and some have licensed devices as medicines such as in the UK.
However, as of February 2018, there is no e-cigarette device that has been given a medical license that is commercially sold or available by prescription in the UK. As of 2015, around two thirds of major nations have regulated e-cigarettes in some way.
Because of the potential relationship with tobacco laws and medical drug policies, e-cigarette legislation is being debated in many countries. The companies that make e-cigarettes have been pushing for laws that support their interests.
In 2016 the US Department of Transportation banned the use of e-cigarettes on commercial flights. This regulation applies to all flights to and from the US. In 2018, the Royal College of Physicians asked that a balance is found in regulations over e-cigarettes that ensure product safety while encouraging smokers to use them instead of tobacco, as well as keep an eye on any effects contrary to the control agencies for tobacco.
The legal status of e-cigarettes is currently pending in many countries. Many countries such as Brazil, Singapore, Uruguay, and India have banned e-cigarettes. Canada-wide in 2014, they were technically illegal to sell, as no nicotine-containing e-cigarettes are not regulated by Health Canada, but this is generally unenforced and they are commonly available for sale Canada-wide. In 2016, Health Canada announced plans to regulate vaping products.
In the US and the UK, the use and sale to adults of e-cigarettes are legal.The revised EU Tobacco Products Directive came into effect in May 2016, providing stricter regulations for e-cigarettes. It limits e-cigarette advertising in print, on television and radio, along with reducing the level of nicotine in liquids and reducing the flavors used. It does not ban vaping in public places. It requires the purchaser for e-cigarettes to be at least 18 and does not permit buying them for anyone less than 18 years of age.
The updated Tobacco Products Directive has been disputed by tobacco lobbyists whose businesses could be impacted by these revisions. As of 8 August 2016, the US FDA extended its regulatory power to include e-cigarettes, e-liquid and all related products.
Under this ruling the FDA will evaluate certain issues, including ingredients, product features and health risks, as well their appeal to minors and non-users. The FDA rule also bans access to minors.
A photo ID is now required to buy e-cigarettes, and their sale in all-ages vending machines is not permitted in the US. As of August 2017, regulatory compliance deadlines relating to premarket review requirements for most e-cigarette and e-liquid products have been extended from November 2017 to 8 August 2022, which attracted a lawsuit filed by the American Heart Association, American Academy of Pediatrics, the Campaign for Tobacco-Free Kids, and other plaintiffs.
In May 2016 the US FDA used its authority under the Family Smoking Prevention and Tobacco Control Act to deem e-cigarette devices and e-liquids to be tobacco products, which meant it intended to regulate the marketing, labelling, and manufacture of devices and liquids; vape shops that mix e-liquids or make or modify devices were considered manufacturing sites that needed to register with US FDA and comply with good manufacturing practice regulation.
E-cigarette and tobacco companies have recruited lobbyists in an effort to prevent the US FDA from evaluating e-cigarette products or banning existing products already on the market.
In February 2014 the European Parliament passed regulations requiring standardization and quality control for liquids and vaporizers, disclosure of ingredients in liquids, and child-proofing and tamper-proofing for liquid packaging.
In April 2014 the US FDA published proposed regulations for e-cigarettes. In the US some states tax e-cigarettes as tobacco products, and some state and regional governments have broadened their indoor smoking bans to include e-cigarettes. As of April 2017, 12 US states and 615 localities had prohibited the use of e-cigarettes in venues in which traditional cigarette smoking was prohibited. In 2015, at least 48 states and 2 territories had banned e-cigarette sales to minors.
E-cigarettes containing nicotine have been listed as drug delivery devices in a number of countries, and the marketing of such products has been restricted or put on hold until safety and efficacy clinical trials are conclusive. Since they do not contain tobacco, television advertising in the US is not restricted. Some countries have regulated e-cigarettes as a medical product even though they have not approved them as a smoking cessation aid.
A 2014 review stated the emerging phenomenon of e-cigarettes has raised concerns in the health community, governments, and the general public and recommended that e-cigarettes should be regulated to protect consumers. It added, "heavy regulation by restricting access to e-cigarettes would just encourage continuing use of much unhealthier tobacco smoking." A 2014 review said regulation of the e-cigarette should be considered on the basis of reported adverse health effects.
Product liability:
Multiple reports from the U.S. Fire Administration conclude that electronic cigarettes have been combusting and injuring people and surrounding areas. The composition of a cigarette is the cause of this, as the cartridges that are meant to contain the liquid mixture are in such close proximity to the battery.
A research report by the U.S. Fire Administration supports this, stating that, “Unlike mobile phones, some e-cigarette lithium-ion batteries within e-cigarettes offer no protection to stop the coil overheating”. In 2015 the U.S. Fire Administration noted in their report that electronic cigarettes are not created by Big Tobacco or other tobacco companies, but by independent factories that have little quality control. Because of this low quality control when made, electronic cigarettes have led to numerous incidents in which people are hurt, or in which the surrounding area is damaged.
Most incidents in which electronic cigarettes have been known to explode, occurred when the device itself is charging, usually within 10 minutes. When an e-cigarette combusts, it creates a fire hazard, especially if the electronic cigarette is left on its own with no supervision. Multiple case studies have shown that electronic cigarettes are at risk of this while they are charging.
The U.S. Fire Administration states that “E-cigarettes left charging for a long period, especially when unattended, have led to fires in homes and cars”. This can cause two issues. The first issue would be the device causing a fire while charging and while in use, in which a person may be harmed but they can relatively quickly put out the fire with minimal damage to them and their surroundings.
Some of the incidents that the U.S. Fire Administration looked at portrayed that this scenario only occurred about 8% of the time, leaving 9 people injured and 2 people with serious burns. The second issue would be if the device is left alone charging and the person goes off into another room or leaves the house completely, and the device implodes.
In the cases in which fires were started, 52% of the fires were small-scale or minor. In those cases people were around to stop the fire, but what about the other cases in which a person doesn't notice the fire or if they are not even in the house when the fire starts? 32% of cases showcase a moderate fire and 4% of cases showcase that the fire destroyed the room the device was in and its contents.
Another report from the U.S. Fire Administration states the following, “In 27 incidents, the fire spread was moderate, where the burned area was larger than 6 inches in diameter, but the fire was extinguished by occupants before the fire department arrived. In 10 incidents, the fire spread was major and involved significant portions of a building and required suppression by the fire department,".
The U.S. Fire Administration also notes that in most cases, when the device has combusted, the fire produced spreads to nearby clothing, carpets, drapes, etc. About 66% of explosions led to a fire, because of the contents in the radius of the explosion.
Marketing
Main article: Electronic cigarette and e-cigarette liquid marketing
They are marketed to men, women, and children as being safer than traditional cigarettes. They are also marketed to non-smokers. E-cigarette marketing is common. There are growing concerns that e-cigarette advertising campaigns unjustifiably focus on young adults, adolescents, and women.
Large tobacco companies have greatly increased their marketing efforts. This marketing trend may expand the use of e-cigarettes and contribute to re-glamorizing smoking. Some companies may use e-cigarette advertising to advocate smoking, deliberately, or inadvertently, is an area of concern.
A 2014 review said, "the e-cigarette companies have been rapidly expanding using aggressive marketing messages similar to those used to promote cigarettes in the 1950s and 1960s."
E-cigarette companies are using methods that were once used by the tobacco industry to persuade young people to start using cigarettes. E-cigarettes are promoted to a certain extent to forge a vaping culture that entices non-smokers. Themes in e-cigarette marketing, including sexual content and customer satisfaction, are parallel to themes and techniques that are appealing to youth and young adults in traditional cigarette advertising and promotion
A 2017 review found "The tobacco industry sees a future where ENDS accompany and perpetuate, rather than supplant, tobacco use, especially targeting the youth." E-cigarettes and nicotine are regularly promoted as safe and even healthy in the media and on brand websites, which is an area of concern.
While advertising of tobacco products is banned in most countries, television and radio e-cigarette advertising in several countries may be indirectly encouraging traditional cigarette use E-cigarette advertisements are also in magazines, newspapers, online, and in retail stores. Between 2010 and 2014, e-cigarettes were second only to cigarettes as the top advertised product in magazines.
As cigarette companies have acquired the largest e-cigarette brands, they currently benefit from a dual market of smokers and e-cigarette users while simultaneously presenting themselves as agents of harm reduction.
This raises concerns about the appropriateness of endorsing a product that directly profits the tobacco industry. There is no evidence that the cigarette brands are selling e-cigarettes as part of a plan to phase out traditional cigarettes, despite some stating to want to cooperate in "harm reduction". E-cigarette advertising for using e-cigarettes as a quitting tool have been seen in the US, UK, and China, which have not been supported by regulatory bodies.
In the US, six large e-cigarette businesses spent $59.3 million on promoting e-cigarettes in 2013. In the US and Canada, over $2 million is spent yearly on promoting e-cigarettes online. E-cigarette websites often made unscientific health statements in 2012.
The ease to get past the age verification system at e-cigarette company websites allows underage individuals to access and be exposed to marketing. Around half of e-cigarette company websites have a minimum age notice that prohibited underage individuals from entering.
Celebrity endorsements are used to encourage e-cigarette use. A 2012 national US television advertising campaign for e-cigarettes starred Stephen Dorff exhaling a "thick flume" of what the advertisement describes as "vapor, not tobacco smoke", exhorting smokers with the message "We are all adults here, it's time to take our freedom back."
Opponents of the tobacco industry state that the advertisement, in a context of longstanding prohibition of tobacco advertising on television, seems to have resorted to advertising tactics that got former generations of people in the US addicted to traditional cigarettes.
Cynthia Hallett of Americans for Non-Smokers' Rights described the US advertising campaign as attempting to "re-establish a norm that smoking is okay, that smoking is glamorous and acceptable".
University of Pennsylvania communications professor Joseph Cappella stated that the setting of the advertisement near an ocean was meant to suggest an association of clean air with the nicotine product.
In 2012 and 2013, e-cigarette companies advertised to a large television audience in the US which included 24 million youth. The channels to which e-cigarette advertising reached the largest numbers of youth (ages 12–17) were AMC, Country Music Television, Comedy Central, WGN America, TV Land, and VH1.
E-cigarettes are heavily promoted across all media outlets. They are vigorously advertised, mostly through the Internet, as a safe substitute to traditional cigarettes, among other things. E-cigarette companies promote their e-cigarette products on Facebook, Instagram, YouTube, and Twitter. They are promoted on YouTube by movies with sexual material and music icons, who encourage minors to "take their freedom back." They have partenered with a number of sports and music icons to promote their products.
Tobacco companies intensely market e-cigarettes to youth, with industry strategies including cartoon characters and candy flavors. Fruit flavored e-liquid is the most commonly marketed e-liquid flavor on social media. E-cigarette companies commonly promote that their products contain only water, nicotine, glycerin, propylene glycol, and flavoring but this assertion is misleading as researchers have found differing amounts of heavy metals in the vapor, including chromium, nickel, tin, silver, cadmium, mercury, and aluminum.
The widespread assertion that e-cigarettes emit "only water vapor" is not true because the evidence demonstrates e-cigarette vapor contains possibly harmful chemicals such as nicotine, carbonyls, metals, and volatile organic compounds, in addition to particulate matter.
Massive advertising included the assertion that they would present little risk to non-users. Though, "disadvantages and side effects have been reported in many articles, and the unfavorable effects of its secondhand vapor have been demonstrated in many studies" and evidence indicates that use of e-cigarettes degrades indoor air quality.
Many e-cigarette companies market their products as a smoking cessation aid without evidence of effectiveness. E-cigarette marketing has been found to make unsubstantiated health statements (e.g., that they help one quit smoking) including statements about improving psychiatric symptoms, which may be particularly appealing to smokers with mental illness. E-cigarette marketing advocate weight control and emphasize use of nicotine with many flavors.
These marketing angles could particularly entice overweight people, youth, and vulnerable groups. Some e-cigarette companies state that their products are green without supporting evidence, which may be purely to increase their sales.
Economics:
The number of e-cigarettes sold increased every year from 2003 to 2014. In 2015 a slowdown in the growth in usage occurred in the US. As of January 2018, the growth in usage in the UK has slowed down since 2013. As of 2014 there were at least 466 e-cigarette brands.
Worldwide e-cigarette sales in 2014 were around US$7 billion. Worldwide e-cigarette sales in 2019 were about $19.3 billion. E-cigarette sales could exceed traditional cigarette sales by 2023. Approximately 30–50% of total e-cigarettes sales are handled on the internet. Established tobacco companies have a significant share of the e-cigarette market.
As of 2018, 95% of e-cigarette devices were made in China, mainly in Shenzhen. Chinese companies' market share of e-liquid is low.In 2014, online and offline sales starting increases. Since combustible cigarettes are relatively inexpensive in China a lower price may not be large factor in marketing vaping products over there.
In 2015, 80% of all e-cigarette sales in convenience stores in the US were products made by tobacco companies. According to Nielsen Holdings, convenience store e-cigarette sales in the US went down for the first time during the four-week period ending on 10 May 2014.
Wells Fargo analyst Bonnie Herzog attributes this decline to a shift in consumers' behavior, buying more specialized devices or what she calls "vapors-tanks-mods (VTMs)" that are not tracked by Nielsen. Wells Fargo estimated that VTMs accounted for 57% of the 3.5 billion dollar market in the US for vapor products in 2015.
In 2014, dollar sales of customizable e-cigarettes and e-liquid surpassed sales of cigarette-imitators in the US, even though, overall, these are a less expensive vaping option. In 2014, the Smoke-Free Alternatives Trade Association estimated that there were 35,000 vape shops in the US, more than triple the number a year earlier.
However the 2015 slowdown in market growth affected VTMs as well. Large tobacco retailers are leading the cigalike market. "We saw the market's sudden recognition that the cigarette industry seems to be in serious trouble, disrupted by the rise of vaping," Mad Money's Jim Cramer stated April 2018. "Over the course of three short days, the tobacco stocks were bent, they were spindled and they were mutilated by the realization that electronic cigarettes have become a serious threat to the old-school cigarette makers," he added.
In 2019, a vaping industry organization released a report stating that a possible US ban on e-cigarettes flavors can potentially effect greater than 150,000 jobs around the US.
The leading seller in the e-cigarette market in the US is the Juul e-cigarette, which was introduced in June 2015. As of August 2018, Juul accounts for over 72% of the US e-cigarette market monitored by Nielsen, and its closest competitor--RJ Reynolds' Vuse—makes up less than 10% of the market. Juul rose to popularity quickly, growing by 700% in 2016 alone.
On 17 July 2018 Reynolds announced it will debut in August 2018 a pod mod type device similar Juul. The popularity of the Juul pod system has led to a flood of other pod devices hitting the market.
In Canada, e-cigarettes had an estimated value of 140 million CAD in 2015. There are numerous e-cigarette retail shops in Canada. A 2014 audit of retailers in four Canadian cities found that 94% of grocery stores, convenience stores, and tobacconist shops which sold e-cigarettes sold nicotine-free varieties only, while all vape shops stocked at least one nicotine-containing product.
By 2015 the e-cigarette market had only reached a twentieth of the size of the tobacco market in the UK. In the UK in 2015 the "most prominent brands of cigalikes" were owned by tobacco companies, however, with the exception of one model, all the tank types came from "non-tobacco industry companies". Yet some tobacco industry products, while using prefilled cartridges, resemble tank models.
France's e-cigarette market was estimated by Groupe Xerfi to be €130 million in 2015. Additionally, France's e-liquid market was estimated at €265 million. In December 2015, there were 2,400 vape shops in France, 400 fewer than in March of the same year. Industry organization Fivape said the reduction was due to consolidation, not to reduced demand.
Environmental impact:
Compared to traditional cigarettes, reusable e-cigarettes do not create waste and potential litter from every use in the form of discarded cigarette butts. Traditional cigarettes tend to end up in the ocean where they cause pollution, though once discarded they undergo biodegradation and photodegradation.
Although some brands have begun recycling services for their e-cigarette cartridges and batteries, the prevalence of recycling is unknown. E-cigarettes that are not reusable contribute to the problem of electronic waste, which can create a hazard for people and other organisms.
If improperly disposed of, they can release heavy metals, nicotine, and other chemicals from batteries and unused e-liquid. A July 2018–April 2019 garbology study found e-cigarette products composed 19% of the waste from all traditional and electronic tobacco and cannabis products collected at 12 public high schools in Northern California.
Related technologies:
Other devices to deliver inhaled nicotine have been developed. They aim to mimic the ritual and behavioral aspects of traditional cigarettes.
British American Tobacco, through their subsidiary Nicoventures, licensed a nicotine delivery system based on existing asthma inhaler technology from UK-based healthcare company Kind Consumer. In September 2014 a product based on this named Voke obtained approval from the United Kingdom's Medicines and Healthcare Products Regulatory Agency.
In 2011 Philip Morris International bought the rights to a nicotine pyruvate technology developed by Jed Rose at Duke University. The technology is based on the chemical reaction between pyruvic acid and nicotine, which produces an inhalable nicotine pyruvate vapor.
Morris Products S.A. created a different kind e-cigarette named P3L. The device is supplied with a cartridge that contains nicotine and lactic acid in different cavities. When turned on and heated, the nicotine salt called nicotine lactate forms an aerosol.
The IQOS is a heated tobacco product marketed by Philip Morris International. It heats tobacco at a lower temperature than traditional cigarettes. The tobacco sticks reach a temperature up to 350 °C. It sold first in Japan since November 2014.
On 2 December 2016, the United Tobacco Vapor Group's (UTVG) stated that they have been given a patent for their vaporizing component system. qmos from UTVG does not contain a wick or sponge and the number of components is 5 compared to 20 for traditional e-cigarettes.
Pax Labs has developed vaporizers that heats the leaves of tobacco to deliver nicotine in a vapor. On 1 June 2015, they introduced Juul a type of e-cigarette which delivers 10 times as much nicotine as other e-cigarettes, equivalent to an actual cigarette puff.
Juul was spun off from Pax Labs in June 2017 and is now available by the independent company Juul Labs. The eTron 3T from Vapor Tobacco Manufacturing, launched in December 2014, employs a patented, aqueous system whereby the tobacco is extracted into water. The e-liquid contains organic tobacco, organic glycerin, and water.
In December 2013 Japan Tobacco launched Ploom in Japan. In January 2016 they launched Ploom TECH that produces a vapor from a heated liquid that moves through a capsule of granulated tobacco leaves.
In 2016 British American Tobacco (BAT) released its own version of the heat but not burn technology called glo in Japan and Switzerland. It uses tobacco sticks rather than nicotine liquid, and does not directly heat or burn tobacco.
In 2015 the glo iFuse was released in Romania by BAT. It uses a coil to heat a liquid that produces a vapor that moves through mixed tobacco. Heated tobacco products were first introduced in 1988, but were not a commercial success.
BLOW started selling e-hookahs, an electronic version of the hookah, in 2014. The handle of each hose for the e-hookah contains a heating element and a liquid, which produces vapor.
Gopal Bhatnagar based in Toronto, Canada invented a 3D printed adapter to turn a traditional hookah into an e-hookah. It is used instead of the ceramic bowl that contains shisha tobacco. Rather than the tobacco, users can insert e-cigarettes.
KanaVape is an e-cigarette containing cannabidiol (CBD) and no THC. Several companies including Canada's Eagle Energy Vapor are selling caffeine-based e-cigarettes instead of containing nicotine.
Instead of smoke, the user inhales vapor. As such, using an e-cigarette is often called "vaping". The atomizer is a heating element that atomizes a liquid solution called e-liquid. E-cigarettes are activated by taking a puff or pressing a button. Some look like traditional cigarettes, and most versions are reusable.
E-cigarettes create an aerosol, commonly called vapor, made of particulate matter. The vapor typically contains propylene glycol, glycerin, nicotine, flavors, and traces of nitrosamines, other toxicants, carcinogens, heavy metals, and metal nanoparticles. Its exact composition varies, and depends on several factors including user behavior.
The health effects of electronic cigarettes remain uncertain, but they are likely less harmful than smoking tobacco. E-cigarette vapor contains fewer toxic chemicals, in lower concentrations, than cigarette smoke, but also contains harmful chemicals not found in tobacco smoke.
Nicotine is highly addictive. People who vape are more likely to start smoking. For smokers who are unable or unwilling to quit using conventional smoking cessation methods such as nicotine replacement therapy (NRT), vaping has a role in tobacco harm reduction. Research suggests that e‐cigarettes may help people to stop smoking cigarettes.
Construction:
Further information: Construction of electronic cigarettes § E-cigarette liquid
An electronic cigarette consists of an atomizer, a power source such as a battery, and a container for the e-liquid such as a cartridge or tank.
E-cigarettes have evolved over time, and the different designs are classified in generations.
First-generation e-cigarettes tend to look like traditional cigarettes, though there is some variation in size, and so are called "cigalikes".
Second-generation devices are larger overall and look less like traditional cigarettes.
Third-generation devices include mechanical mods and variable voltage devices.
The fourth-generation includes Sub ohm tanks (meaning that they have electrical resistance of less than 1 Ohm) and temperature control devices.
The voltage for first-generation e-cigarettes is about 3.7 and second-generation e-cigarettes can be adjusted from 3 V to 6 V, while more recent devices can go up to 8 V.
There are also pod mod devices that use protonated nicotine, rather than free-base nicotine found in earlier generations, providing higher nicotine yields through the production of aerosolized protonated nicotine.
E-liquid is the mixture used in vapor products such as e-cigarettes. It usually contains propylene glycol, glycerin, nicotine, flavorings, additives, and contaminants. E-liquid formulations vary widely.
A typical e-liquid comprises propylene glycol and glycerin (95%), and flavorings, nicotine, and other additives (5%). Some e-liquids lack propylene glycol, nicotine, or flavors. The flavorings may be natural, artificial, or organic. Over 80 chemicals such as formaldehyde and metallic nanoparticles have been found in the e-liquid. There are many e-liquid manufacturers, and more than 15,000 flavors.
In the US, under Food and Drug Administration (FDA) rules, e-liquids must comply with manufacturing standards. Industry standards are published by the American E-liquid Manufacturing Standards Association (AEMSA). EU standards are in the EU Tobacco Products Directive.
Use:
Popularity:
Main article: Usage of electronic cigarettes
Since their entrance to the market around 2003, e-cigarette use has risen rapidly. In 2011 there were about 7 million adult e-cigarette users globally, rising to 41 million in 2018 and to 68 million in 2020 compared with 1.1 billion cigarette smokers.
E-cigarette use is highest in China, the US, and Europe, with China having the most e-cigarette users. The rise was thought to be due to advertising to young people; their low cost compared to tobacco; and the perception that e-cigarettes are safer than tobacco.
USA:
In 2020, about 20% of US high school students reported using an e-cigarette at least once in the past 30 days. As of 2018, about 3% of US adults use e-cigarettes some days or every day.
UK:
In the UK, current e-cigarette use increased from 1.7% of the adult population in 2012 to 7.1% in 2019 and then decreased to 6.3% in 2020. As of 2020, about 59% of UK adult e-cigarette users are former smokers, 38% currently use both cigarettes and e-cigarettes, and 3% have never smoked a cigarette.
Australia:
According to a 2019 report, approximately 520,000 adult Australians were vaping. That was more than twice as much as in a 2016 survey where only 240,000 Australians were vapers.
Progression:
Historically, many users began with a disposable e-cigarette resembling a tobacco cigarette. They often progress to later-generation devices and may adjust their devices to provide more vapor. Experienced users often prefer rechargeable e-cigarettes. Women prefer disposable e-cigarettes, and young adults pay more attention to modifiability (the ability to change the power of the e-cigarette or change pieces of e-cigarettes).
Modifiability increases the chance of starting vaping among young people.
Most vapers use a refillable tank system, allowing them to mix their own liquid giving control over flavor and strength. Experienced vapers rank customizability as the most important consideration in choosing a device. Users ranked nicotine strength as an important factor for choosing among various e-cigarettes, though such preference could vary by smoking status, e-cigarette use history, and gender.
Non-smokers and inexperienced e-cigarettes users tended to prefer no nicotine or low nicotine e-cigarettes while smokers and experienced e-cigarettes users preferred medium and high nicotine e-cigarettes.
Young people:
Worldwide, increasing numbers of young people in some countries are vaping, and rates were found to be especially high in the US, Poland, and Hungary as of 2013-2015.
With access to e-cigarettes, young people have been using tobacco about a quarter as often. Vaping among adolescents grew every year until 2017. There appears to be an increase of one-time e-cigarette use among young people worldwide.
Most young e-cigarette users have never smoked, but there is a substantial minority who both vape and smoke, which indicates that e-cigarettes may be a starting point for nicotine use. Young people who would not smoke are vaping, and young people who vape are more likely to start smoking.
Twice as many young people vaped in 2014 than also used traditional cigarettes. Young people who smoke tobacco or marijuana, or who drink alcohol, are much more likely to vape. Among young people who have tried vaping, most used a flavored product the first time.
Most young people are not vaping to help them quit tobacco. Vaping correlates with smoking among young people, even in those who would otherwise be unlikely to smoke. Experimenting with vaping encourages young people to continue smoking.
A 2015 study found minors had little resistance to buying e-cigarettes online. Teenagers may not admit using e-cigarettes, but use, for instance, a hookah pen. As a result, self-reporting may be lower in surveys.
Motivation:
There are varied reasons for e-cigarette use. Most users are trying to quit smoking, but a large proportion of use is recreational or as a way to get around smoke-free laws.
Many people who use e-cigarettes still smoke, raising concern that they may be delaying or deterring quitting. Some people say they want to quit smoking by vaping, but others vape to circumvent smoke-free laws and policies, or to cut back on cigarette smoking. Many people vape because they believe vaping is safer than smoking.
Concerns over avoiding stains on teeth or odor from smoke on clothes in some cases prompted interest in or use of e-cigarettes. Some e-cigarettes appeal considerably to people curious in technology who want to customize their devices.
There appears to be a hereditary component to tobacco use, which probably plays a part in transitioning of e-cigarette use from experimentation to routine use.
Many users say they like the choice of flavors and comparatively low price of e-cigarettes compared to cigarettes.
Gateway theory:
In the context of drugs, the gateway hypothesis is that using less harmful drugs can lead to a future risk of using more harmful drugs or crime. Some research suggests vaping is a "gateway" to smoking. A 2020 report of 25 studies and three systematic reviews found that every study examined found that e-cigarette use was associated with increased odds of later smoking.
However, it is also plausible that any favorable relation between vaping and starting smoking is a result of common risk factors. Gateway theories have always been controversial in the field of addictions, and they are difficult to test. Research that controls for confounding factors generally finds that vaping is an "exit ramp" from smoking.
In other words, rather than leading to more cigarette smoking, e-cigarette use may be leading to less smoking.
Because those with mental illness are highly predisposed to nicotine addiction, those who try e-cigarettes may be more likely to become dependent, raising concerns about facilitating a transition to combustible tobacco use. Even if an e-cigarette contains no nicotine, the user mimics the actions of smoking. This may renormalize tobacco use in the general public.
There is a possible risk of re-normalizing of tobacco use in areas where smoking is banned. Government intervention is recommended to keep children safe from the re-normalizing of tobacco, according to a 2017 review.
The "catalyst model" suggests that vaping may proliferate smoking in minors by sensitizing minors to nicotine with the use of a type of nicotine that is more pleasing and without the negative attributes of regular cigarettes.
A 2016 review, based on the catalyst model, "indicate that the perceived health risks, specific product characteristics (such as taste, price, and inconspicuous use), and higher levels of acceptance among peers and others potentially make e-cigarettes initially more attractive to adolescents than tobacco cigarettes. Later, increasing familiarity with nicotine could lead to the reevaluation of both electronic and tobacco cigarettes and subsequently to a potential transition to tobacco smoking."
Health effects:
The benefits and the health risks of e-cigarettes are uncertain, including their long-term effects. There is tentative evidence they may help people quit smoking, but smoking cessation medicine is at least as effective.
Pods contain different doses of nicotine, and these levels are regulated in some countries.
Following the possibility of nicotine addiction from e-cigarette use, there is concern children and young people may start smoking cigarettes. Their part in tobacco harm reduction is unclear, while another review found they appear to have the potential to lower tobacco-related death and disease.
Regulated US Food and Drug Administration (US FDA) nicotine replacement products may be safer than e-cigarettes, but e-cigarettes are generally seen as safer than combusted tobacco products.
The risk of early death may be similar to that of smokeless tobacco. The risk of serious adverse events was reported in 2016 to be low. Less serious adverse effects include abdominal pain, headache, blurry vision, throat and mouth irritation, vomiting, nausea, and coughing.
Nicotine is harmful. In 2019 and 2020, an outbreak of severe vaping lung illness in the US was strongly linked to vitamin E acetate by the CDC. E-cigarettes produce similarly high levels of particulates in the air as do tobacco-cigarettes. There is "only limited evidence showing adverse respiratory and cardiovascular effects in humans", with the authors of a 2020 review calling for more long-term studies on the subject. A 2020 review found e-cigarettes increase the risk of asthma by 40% and chronic obstructive pulmonary disease by 50%.
Pregnancy:
The Royal College of Midwives states, "While vaping devices such as electronic cigarettes (e-cigs) do contain some toxins, they are at far lower levels than found in tobacco smoke. If a pregnant woman who has been smoking chooses to use an e-cig and it helps her to quit smoking and stay smoke-free, she should be supported to do so."
Based on the available evidence on e-cigarette safety, there was also "no reason to believe that use of an e-cig has any adverse effect on breastfeeding." The statement went on to say, "vaping should continue, if it is helpful to quitting smoking and staying smoke-free". The UK National Health Service says: "If using an e-cigarette helps you to stop smoking, it is much safer for you and your baby than continuing to smoke.".
Many women who vape continue to do so during pregnancy because of the perceived safety of e-cigarettes compared to tobacco.
United States:
In one of the few studies identified, a 2015 survey of 316 pregnant women in a Maryland clinic found that the majority had heard of e-cigarettes, 13% had used them, and 0.6% were current daily users. These findings are of concern because the dose of nicotine delivered by e-cigarettes can be as high or higher than that delivered by traditional cigarettes.
Data from two states in the Pregnancy Risk Assessment System (PRAMS) show that in 2015—roughly the mid-point of the study period—10.8% of the sample used e-cigarettes in the three months prior to the pregnancy while 7.0%, 5.8%, and 1.4% used these products at the time of the pregnancy, in the first trimester, and at birth respectively.
According to National Health Interview Survey (NHIS) data from 2014 to 2017, 38.9% of pregnant smokers used e-cigarettes compared to only 13.5% of non-pregnant, reproductive age women smokers. A health economic study found that passing an e-cigarette minimum legal sale age law in the United States increased teenage prenatal smoking by 0.6 percentage points and had no effect on birth outcomes.
Nevertheless, additional research needs to be done on the health effects of electronic cigarette use during pregnancy.
Harm reduction:
Harm reduction refers to any reduction in harm from a prior level. Harm minimization strives to reduce harms to the lowest achievable level. When a person does not want to quit nicotine, harm minimization means striving to eliminate tobacco exposure by replacing it with vaping. E-cigarettes can reduce smokers' exposure to carcinogens and other toxic chemicals found in tobacco.
Tobacco harm reduction has been a controversial area of tobacco control. Health advocates have been slow to support a harm reduction method out of concern that tobacco companies cannot be trusted to sell products that will lower the risks associated with tobacco use. A large number of smokers want to reduce harm from smoking by using e-cigarettes. The argument for harm reduction does not take into account the adverse effects of nicotine.
There cannot be a defensible reason for harm reduction in children who are vaping with a base of nicotine. Quitting smoking is the most effective strategy to tobacco harm reduction.
Tobacco smoke contains 100 known carcinogens and 900 potentially cancer-causing chemicals, but e-cigarette vapor contains less of the potential carcinogens than found in tobacco smoke. A study in 2015 using a third-generation device found levels of formaldehyde were greater than with cigarette smoke when adjusted to a maximum power setting.
E-cigarettes cannot be considered safe because there is no safe level for carcinogens. Due to their similarity to traditional cigarettes, e-cigarettes could play a valuable role in tobacco harm reduction. However, the public health community remains divided concerning the appropriateness of endorsing a device whose safety and efficacy for smoking cessation remain unclear.
Overall, the available evidence supports the cautionary implementation of harm reduction interventions aimed at promoting e-cigarettes as attractive and competitive alternatives to cigarette smoking, while taking measures to protect vulnerable groups and individuals.
The core concern is that smokers who could have quit entirely will develop an alternative nicotine addiction. Dual use may be an increased risk to a smoker who continues to use even a minimal amount of traditional cigarettes, rather than quitting.
The promotion of vaping as a harm reduction aid is premature, while a 2011 review found they appear to have the potential to lower tobacco-related death and disease. Evidence to substantiate the potential of vaping to lower tobacco-related death and disease is unknown.
The health benefits of reducing cigarette use while vaping is unclear. E-cigarettes could have an influential role in tobacco harm reduction. The authors warned against the potential harm of excessive regulation and advised health professionals to consider advising smokers who are reluctant to quit by other methods to switch to e-cigarettes as a safer alternative to smoking.
A 2014 review recommended that regulations for e-cigarettes could be similar to those for dietary supplements or cosmetic products to not limit their potential for harm reduction.
A 2012 review found e-cigarettes could considerably reduce traditional cigarettes use and they likely could be used as a lower risk replacement for traditional cigarettes, but there is not enough data on their safety and efficacy to draw definite conclusions. There is no research available on vaping for reducing harm in high-risk groups such as people with mental disorders.
A 2014 PHE report concluded that hazards associated with products currently on the market are probably low, and apparently much lower than smoking. However, harms could be reduced further through reasonable product standards.
British Medical Association encourages health professionals to recommend conventional nicotine replacement therapies, but for patients unwilling to use or continue using such methods, health professionals may present e-cigarettes as a lower-risk option than tobacco smoking.
The American Association of Public Health Physicians (AAPHP) suggests those who are unwilling to quit tobacco smoking or unable to quit with medical advice and pharmaceutical methods should consider other nicotine-containing products such as e-cigarettes and smokeless tobacco for long-term use instead of smoking.
A 2014 WHO report concluded that some smokers will switch completely to e-cigarettes from traditional tobacco but a "sizeable" number will use both. This report found that such "dual-use" of e-cigarettes and tobacco "will have much smaller beneficial effects on overall survival compared with quitting smoking completely."
Smoking cessation:
The use of e-cigarettes for quitting smoking is controversial. Limited evidence suggests that e‐cigarettes probably do help people to stop smoking. Data regarding their use includes at least 26 randomized controlled trials and a number of user surveys, case reports, and cohort studies.
At least once recent review (2019) found that vaping did not seem to greatly increase the odds of quitting smoking. As a result of the data being confronted with methodological and study design limitations, no firm conclusions can be drawn in respect to their efficacy and safety. A 2016 review found that the combined abstinence rate among smokers using e-cigarettes in prospective studies was 29.1%.
The same review noted that few clinical trials and prospective studies had yet been conducted on their effectiveness, and only one randomized clinical trial had included a group using other quit smoking methods. No long-term trials have been conducted for their use as a smoking cessation aid.
It is still not evident as to whether vaping can adequately assist with quitting smoking at the population level. A 2015 PHE report recommends for smokers who cannot or do not want to quit to use e-cigarettes as one of the main steps to lower smoking-related disease, while a 2015 US PSTF statement found there is not enough evidence to recommend e-cigarettes for quitting smoking in adults, pregnant women, and adolescents.
In 2021 the US PSTF concluded the evidence is still insufficient to recommend e-cigarettes for quitting smoking, finding that the balance of benefits and harms cannot be determined.
As of January 2018, systematic reviews collectively agreed that there is insufficient evidence to unequivocally determine whether vaping helped people abstain from smoking. A 2020 systematic review and meta-analysis of 64 studies found that on the whole as consumer products e-cigarettes do not increase quitting smoking.
A small number of studies have looked at whether using e-cigarettes reduces the number of cigarettes smokers consume. E-cigarette use may decrease the number of cigarettes smoked, but smoking just one to four cigarettes daily greatly increases the risk of cardiovascular disease compared to not smoking. The extent to which decreasing cigarette smoking with vaping leads to quitting is unknown.
It is unclear whether e-cigarettes are only helpful for particular types of smokers. Vaping with nicotine may reduce tobacco use among daily smokers. Whether or not vaping is potentially effective for quitting smoking may rely upon whether it was used as part of making an effort to quit or not.
Comparing e-cigarettes to nicotine replacement therapy, a 2020 review found "moderate-certainty evidence" that e-cigarettes are more effective than nicotine replacement therapy (NRT) for quitting smoking. The difference was minor, indicating that compared to NRT, e-cigarettes might lead to an additional four successful quitters per 100.
However, some studies have people who vaped were not more likely to give up smoking than people who did not vape. and previous reviews have found that e-cigarettes were not been proven to be more effective than smoking cessation medicine and regulated US FDA medicine.
A randomized trial stated 29% of e-cigarette users were still vaping at 6 months, while only 8% of patch users still wore patches at 6 months, suggesting that some people are switching to cigarettes rather than fully quitting all tobacco use. The potential adverse effects such as normalizing smoking have not been adequately studied.
While some surveys reported improved quitting smoking, particularly with intensive e-cigarette users, several studies showed a decline in quitting smoking in dual users of cigarettes and e-cigarettes. Compared to many alternative quitting smoking medicines in early development in clinical trials including e-cigarettes, cytisine may be the most encouraging in efficacy and safety with an inexpensive price.
Other kinds of nicotine replacement products are usually covered by health systems, but because e-cigarettes are not medically licensed they are not covered.
One of the challenges in studying e-cigarettes is that there are hundreds of brands and models of e-cigarettes sold that vary in the design and operation of the devices and composition of the liquid, and the technology continues to change.
E-cigarettes have not been subjected to the same type of efficacy testing as nicotine replacement products. There are also social concerns - use of e-cigarettes may normalize tobacco use and prolong cigarette use for people who could have quit instead, or it could put extra pressure on smokers to stop cigarette smoking because e-cigarettes are a more socially acceptable alternative.
The evidence indicates smokers are more frequently able to completely quit smoking using tank devices compared to cigarette versions , which may be due to their more efficient nicotine delivery. There is low quality evidence that vaping assists smokers to quit smoking in the long-term compared with nicotine-free vaping.
Nicotine-containing e-cigarettes were associated with greater effectiveness for quitting smoking than e-cigarettes without nicotine. A 2013 study in smokers who were not trying to quit, found that vaping, with or without nicotine decreased the number of cigarettes consumed. E-cigarettes without nicotine may reduce tobacco cravings because of the smoking-related physical stimuli.
A 2015 meta-analysis on clinical trials found that e-cigarettes containing nicotine are more effective than nicotine-free ones for quitting smoking. They compared their finding that nicotine-containing e-cigarettes helped 20% of people quit with the results from other studies that found nicotine replacement products helps 10% of people quit.
A 2016 review found low quality evidence of a trend towards benefit of e-cigarettes with nicotine for smoking cessation. In terms of whether flavored e-cigarettes assisted quitting smoking, the evidence is inconclusive. Tentative evidence indicates that health warnings on vaping products may influence users to give up vaping.
As of 2020, the efficacy and safety of vaping for quitting smoking during pregnancy was unknown. No research is available to provide details on the efficacy of vaping for quitting smoking during pregnancy. There is robust evidence that vaping is not effective for quitting smoking among adolescents.
In view of the shortage of evidence, vaping is not recommend for cancer patients, although for all patients vaping is likely less dangerous than smoking cigarettes. The effectiveness of vaping for quitting smoking among vulnerable groups is uncertain.
Safety:
Main articles:
- Safety of electronic cigarettes,
- Adverse effects of electronic cigarettes,
- and Composition of electronic cigarette aerosol
As of 2015, research had not yet provided a consensus on the risks of e-cigarette use.
There is little data about their safety, and a considerable variety of liquids are used as carriers, and thus are present in the aerosol delivered to the user. Reviews of the safety of e-cigarettes have reached quite different conclusions.
A 2014 WHO report cautioned about potential risks of using e-cigarettes. Regulated US FDA products such as nicotine inhalers may be safer than e-cigarettes, but e-cigarettes are generally seen as safer than combusted tobacco products such as cigarettes and cigars. The risk of early death is anticipated to be similar to that of smokeless tobacco.
Since vapor does not contain tobacco and does not involve combustion, users may avoid several harmful constituents usually found in tobacco smoke, such as ash, tar, and carbon monoxide. However, e-cigarette use with or without nicotine cannot be considered risk-free because the long-term effects of e-cigarette use are unknown.
The cytotoxicity of e-liquids varies, and contamination with various chemicals have been detected in the liquid. Metal parts of e-cigarettes in contact with the e-liquid can contaminate it with metal particles. Many chemicals including carbonyl compounds such as formaldehyde can inadvertently be produced when the nichrome wire (heating element) that touches the e-liquid is heated and chemically reacted with the liquid.
Normal usage of e-cigarettes, and reduced voltage (3.0 V) devices generate very low levels of formaldehyde. The later-generation and "tank-style" e-cigarettes with a higher voltage (5.0 V) may generate equal or higher levels of formaldehyde compared to smoking.
A 2015 report by Public Health England found that high levels of formaldehyde only occurred in overheated "dry-puffing". Users detect the "dry puff" (also known as a "dry hit") and avoid it, and they concluded that "There is no indication that EC users are exposed to dangerous levels of aldehydes." However, e-cigarette users may "learn" to overcome the unpleasant taste due to elevated aldehyde formation, when the nicotine craving is high enough.
E-cigarette users who use devices that contain nicotine are exposed to its potentially harmful effects. Nicotine is associated with cardiovascular disease, possible birth defects, and poisoning. In vitro studies of nicotine have associated it with cancer, but carcinogenicity has not been demonstrated in vivo. There is inadequate research to show that nicotine is associated with cancer in humans. The risk is probably low from the inhalation of propylene glycol and glycerin.
No information is available on the long-term effects of the inhalation of flavors.
In 2019-2020, there was an outbreak of vaping-related lung illness in the US and Canada, primarily related to vaping THC with vitamin E acetate.
E-cigarettes create vapor that consists of fine and ultrafine particles of particulate matter, with the majority of particles in the ultrafine range. The vapor have been found to contain propylene glycol, glycerin, nicotine, flavors, small amounts of toxicants, carcinogens, and heavy metals, as well as metal nanoparticles, and other substances.
Exactly what the vapor consists of varies in composition and concentration across and within manufacturers, and depends on the contents of the liquid, the physical and electrical design of the device, and user behavior, among other factors. E-cigarette vapor potentially contains harmful chemicals not found in tobacco smoke. The majority of toxic chemicals found in cigarette smoke are absent in e-cigarette vapor.
E-cigarette vapor contains lower concentrations of potentially toxic chemicals than with cigarette smoke. Those which are present, are mostly below 1% of the corresponding levels permissible by workplace safety standards. But workplace safety standards do not recognize exposure to certain vulnerable groups such as people with medical ailments, children, and infants who may be exposed to second-hand vapor.
Concern exists that some of the mainstream vapor exhaled by e-cigarette users may be inhaled by bystanders, particularly indoors, although e-cigarette pollutant levels are much lower than for cigarettes and likely to pose a much lower risk, if any, compared to cigarettes.
E-cigarette use by a parent might lead to inadvertent health risks to offspring. A 2014 review recommended that e-cigarettes should be regulated for consumer safety. There is limited information available on the environmental issues around production, use, and disposal of e-cigarettes that use cartridges. E-cigarettes that are not reusable may contribute to the problem of electronic waste.
Addiction:
Further information: Effects of electronic cigarettes on human brain development
Nicotine, a key ingredient in most e-liquids, is well-recognized as one of the most addictive substances, as addictive as heroin and cocaine. Addiction is believed to be a disorder of experience-dependent brain plasticity. The reinforcing effects of nicotine play a significant role in the beginning and continuing use of the drug.
First-time nicotine users develop a dependence about 32% of the time. Chronic nicotine use involves both psychological and physical dependence. Nicotine-containing e-cigarette vapor induces addiction-related neurochemical, physiological and behavioral changes.
Nicotine affects neurological, neuromuscular, cardiovascular, respiratory, immunological and gastrointestinal systems. Neuroplasticity within the brain's reward system occurs as a result of long-term nicotine use, leading to nicotine dependence. The neurophysiological activities that are the basis of nicotine dependence are intricate. It includes genetic components, age, gender, and the environment.
Nicotine addiction is a disorder which alters different neural systems such as dopaminergic, glutamatergic, GABAergic, serotoninergic, that take part in reacting to nicotine. Long-term nicotine use affects a broad range of genes associated with neurotransmission, signal transduction, and synaptic architecture. The ability to quitting smoking is affected by genetic factors, including genetically based differences in the way nicotine is metabolized.
Nicotine is a parasympathomimetic stimulant that binds to and activates nicotinic acetylcholine receptors in the brain, which subsequently causes the release of dopamine and other neurotransmitters, such as:
- norepinephrine,
- acetylcholine,
- serotonin,
- gamma-aminobutyric acid,
- glutamate,
- endorphins,
- and several neuropeptides, including proopiomelanocortin-derived α-MSH and adrenocorticotropic hormone.
Corticotropin-releasing factor, Neuropeptide Y, orexins, and norepinephrine are involved in nicotine addiction. Continuous exposure to nicotine can cause an increase in the number of nicotinic receptors, which is believed to be a result of receptor desensitization and subsequent receptor upregulation.
Long-term exposure to nicotine can also result in downregulation of glutamate transporter 1. Long-term nicotine exposure upregulates cortical nicotinic receptors, but it also lowers the activity of the nicotinic receptors in the cortical vasodilation region. These effects are not easily understood. With constant use of nicotine, tolerance occurs at least partially as a result of the development of new nicotinic acetylcholine receptors in the brain.
After several months of nicotine abstinence, the number of receptors go back to normal. The extent to which alterations in the brain caused by nicotine use are reversible is not fully understood. Nicotine also stimulates nicotinic acetylcholine receptors in the adrenal medulla, resulting in increased levels of epinephrine and beta-endorphin. Its physiological effects stem from the stimulation of nicotinic acetylcholine receptors, which are located throughout the central and peripheral nervous systems.
When nicotine intake stops, the upregulated nicotinic acetylcholine receptors induce withdrawal symptoms. These symptoms can include cravings for nicotine, anger, irritability, anxiety, depression, impatience, trouble sleeping, restlessness, hunger, weight gain, and difficulty concentrating.
When trying to quit smoking with vaping a base containing nicotine, symptoms of withdrawal can include irritability, restlessness, poor concentration, anxiety, depression, and hunger. The changes in the brain cause a nicotine user to feel abnormal when not using nicotine. In order to feel normal, the user has to keep his or her body supplied with nicotine.
E-cigarettes may reduce cigarette craving and withdrawal symptoms. It is not clear whether e-cigarette use will decrease or increase overall nicotine addiction, but the nicotine content in e-cigarettes is adequate to sustain nicotine dependence. Chronic nicotine use causes a broad range of neuroplastic adaptations, making quitting hard to accomplish.
A 2015 study found that users vaping non-nicotine e-liquid exhibited signs of dependence. Experienced users tend to take longer puffs which may result in higher nicotine intake. It is difficult to assess the impact of nicotine dependence from e-cigarette use because of the wide range of e-cigarette products. The addiction potential of e-cigarettes may have risen because as they have progressed, they delivery nicotine better.
A 2015 American Academy of Pediatrics (AAP) policy statement stressed "the potential for these products to addict a new generation of youth to nicotine and reverse more than 50 years of public health gains in tobacco control."
The World Health Organization (WHO) is concerned about starting nicotine use among non-smokers, and the National Institute on Drug Abuse said e-cigarettes could maintain nicotine addiction in those who are attempting to quit. The limited available data suggests that the likelihood of excessive use of e-cigarettes is smaller than traditional cigarettes.
No long-term studies have been done on the effectiveness of e-cigarettes in treating tobacco addiction, but some evidence suggests that dual use of e-cigarettes and traditional cigarettes may be associated with greater nicotine dependence.
There is concern that children may progress from vaping to smoking. Adolescents are likely to underestimate nicotine's addictiveness. Vulnerability to the brain-modifying effects of nicotine, along with youthful experimentation with e-cigarettes, could lead to a lifelong addiction. A long-term nicotine addiction from using a vape may result in using other tobacco products.
The majority of addiction to nicotine starts during youth and young adulthood. Adolescents are more likely to become nicotine dependent than adults. The adolescent brain seems to be particularly sensitive to neuroplasticity as a result of nicotine.
Minimal exposure could be enough to produce neuroplastic alterations in the very sensitive adolescent brain. A 2014 review found that in studies up to a third of youth who have not tried a traditional cigarette have used e-cigarettes. The degree to which teens are using e-cigarettes in ways the manufacturers did not intend, such as increasing the nicotine delivery, is unknown, as is the extent to which e-cigarette use may lead to addiction or substance dependence in youth.
Positions:
Main article: Positions of medical organizations on electronic cigarettes
Because of overlap with tobacco laws and medical drug policies, e-cigarette legislation is being debated in many countries. The revised EU Tobacco Products Directive came into effect in May 2016, providing stricter regulations for e-cigarettes.
In February 2010 the US District Court ruled against the FDA's seizure of E-Cigarettes as a "drug-device" and in December 2010 the US Court of Appeals confirmed them to be tobacco products which were by then subject to regulation under the 2009 FSPTC Act.
In August 2016, the US FDA extended its regulatory power to include e-cigarettes, cigars, and "all other tobacco products". Large tobacco companies have greatly increased their marketing efforts.
The scientific community in US and Europe are primarily concerned with their possible effect on public health. There is concern among public health experts that e-cigarettes could renormalize smoking, weaken measures to control tobacco. and serve as a gateway for smoking among youth.
The public health community is divided over whether to support e-cigarettes, because their safety and efficacy for quitting smoking is unclear. Many in the public health community acknowledge the potential for their quitting smoking and decreasing harm benefits, but there remains a concern over their long-term safety and potential for a new era of users to get addicted to nicotine and then tobacco.
There is concern among tobacco control academics and advocates that prevalent universal vaping "will bring its own distinct but as yet unknown health risks in the same way tobacco smoking did, as a result of chronic exposure", among other things.
Medical organizations differ in their views about the health implications of vaping There is general agreement that e-cigarettes expose users to fewer toxicants than tobacco cigarettes. Some healthcare groups and policy makers have hesitated to recommend e-cigarettes for quitting smoking, because of limited evidence of effectiveness and safety. Some have advocated bans on e-cigarette sales and others have suggested that e-cigarettes may be regulated as tobacco products but with less nicotine content or be regulated as a medicinal product.
A 2016 World Health Organization (WHO) report found that the scientific evidence for the effectiveness of vaping for quitting smoking is "scant and of low certainty". Healthcare organizations in the UK in 2015 have encouraged smokers to try e-cigarettes to help them quit smoking and also encouraged e-cigarette users to quit smoking tobacco entirely.
In 2016, the US Food and Drug Administration (US FDA) stated that "Although ENDS [electronic nicotine delivery systems] may potentially provide cessation benefits to individual smokers, no ENDS have been approved as effective cessation aids."
In 2019 the European Respiratory Society stated that "The long-term effects of ECIG use are unknown, and there is therefore no evidence that ECIGs are safer than tobacco in the long term." Following hundreds of possible cases of severe lung illness and five confirmed deaths associated with vaping in the US, the Centers for Disease Control and Prevention stated on 6 September 2019 that people should consider not using vaping products while their investigation is ongoing.
Regulation:
Main articles:
Regulation of e-cigarettes varies across countries and states, ranging from no regulation to banning them entirely. For instance, e-cigarettes are illegal in Japan, forcing the market to use heated tobacco products for cigarette alternatives. Others have introduced strict restrictions and some have licensed devices as medicines such as in the UK.
However, as of February 2018, there is no e-cigarette device that has been given a medical license that is commercially sold or available by prescription in the UK. As of 2015, around two thirds of major nations have regulated e-cigarettes in some way.
Because of the potential relationship with tobacco laws and medical drug policies, e-cigarette legislation is being debated in many countries. The companies that make e-cigarettes have been pushing for laws that support their interests.
In 2016 the US Department of Transportation banned the use of e-cigarettes on commercial flights. This regulation applies to all flights to and from the US. In 2018, the Royal College of Physicians asked that a balance is found in regulations over e-cigarettes that ensure product safety while encouraging smokers to use them instead of tobacco, as well as keep an eye on any effects contrary to the control agencies for tobacco.
The legal status of e-cigarettes is currently pending in many countries. Many countries such as Brazil, Singapore, Uruguay, and India have banned e-cigarettes. Canada-wide in 2014, they were technically illegal to sell, as no nicotine-containing e-cigarettes are not regulated by Health Canada, but this is generally unenforced and they are commonly available for sale Canada-wide. In 2016, Health Canada announced plans to regulate vaping products.
In the US and the UK, the use and sale to adults of e-cigarettes are legal.The revised EU Tobacco Products Directive came into effect in May 2016, providing stricter regulations for e-cigarettes. It limits e-cigarette advertising in print, on television and radio, along with reducing the level of nicotine in liquids and reducing the flavors used. It does not ban vaping in public places. It requires the purchaser for e-cigarettes to be at least 18 and does not permit buying them for anyone less than 18 years of age.
The updated Tobacco Products Directive has been disputed by tobacco lobbyists whose businesses could be impacted by these revisions. As of 8 August 2016, the US FDA extended its regulatory power to include e-cigarettes, e-liquid and all related products.
Under this ruling the FDA will evaluate certain issues, including ingredients, product features and health risks, as well their appeal to minors and non-users. The FDA rule also bans access to minors.
A photo ID is now required to buy e-cigarettes, and their sale in all-ages vending machines is not permitted in the US. As of August 2017, regulatory compliance deadlines relating to premarket review requirements for most e-cigarette and e-liquid products have been extended from November 2017 to 8 August 2022, which attracted a lawsuit filed by the American Heart Association, American Academy of Pediatrics, the Campaign for Tobacco-Free Kids, and other plaintiffs.
In May 2016 the US FDA used its authority under the Family Smoking Prevention and Tobacco Control Act to deem e-cigarette devices and e-liquids to be tobacco products, which meant it intended to regulate the marketing, labelling, and manufacture of devices and liquids; vape shops that mix e-liquids or make or modify devices were considered manufacturing sites that needed to register with US FDA and comply with good manufacturing practice regulation.
E-cigarette and tobacco companies have recruited lobbyists in an effort to prevent the US FDA from evaluating e-cigarette products or banning existing products already on the market.
In February 2014 the European Parliament passed regulations requiring standardization and quality control for liquids and vaporizers, disclosure of ingredients in liquids, and child-proofing and tamper-proofing for liquid packaging.
In April 2014 the US FDA published proposed regulations for e-cigarettes. In the US some states tax e-cigarettes as tobacco products, and some state and regional governments have broadened their indoor smoking bans to include e-cigarettes. As of April 2017, 12 US states and 615 localities had prohibited the use of e-cigarettes in venues in which traditional cigarette smoking was prohibited. In 2015, at least 48 states and 2 territories had banned e-cigarette sales to minors.
E-cigarettes containing nicotine have been listed as drug delivery devices in a number of countries, and the marketing of such products has been restricted or put on hold until safety and efficacy clinical trials are conclusive. Since they do not contain tobacco, television advertising in the US is not restricted. Some countries have regulated e-cigarettes as a medical product even though they have not approved them as a smoking cessation aid.
A 2014 review stated the emerging phenomenon of e-cigarettes has raised concerns in the health community, governments, and the general public and recommended that e-cigarettes should be regulated to protect consumers. It added, "heavy regulation by restricting access to e-cigarettes would just encourage continuing use of much unhealthier tobacco smoking." A 2014 review said regulation of the e-cigarette should be considered on the basis of reported adverse health effects.
Product liability:
Multiple reports from the U.S. Fire Administration conclude that electronic cigarettes have been combusting and injuring people and surrounding areas. The composition of a cigarette is the cause of this, as the cartridges that are meant to contain the liquid mixture are in such close proximity to the battery.
A research report by the U.S. Fire Administration supports this, stating that, “Unlike mobile phones, some e-cigarette lithium-ion batteries within e-cigarettes offer no protection to stop the coil overheating”. In 2015 the U.S. Fire Administration noted in their report that electronic cigarettes are not created by Big Tobacco or other tobacco companies, but by independent factories that have little quality control. Because of this low quality control when made, electronic cigarettes have led to numerous incidents in which people are hurt, or in which the surrounding area is damaged.
Most incidents in which electronic cigarettes have been known to explode, occurred when the device itself is charging, usually within 10 minutes. When an e-cigarette combusts, it creates a fire hazard, especially if the electronic cigarette is left on its own with no supervision. Multiple case studies have shown that electronic cigarettes are at risk of this while they are charging.
The U.S. Fire Administration states that “E-cigarettes left charging for a long period, especially when unattended, have led to fires in homes and cars”. This can cause two issues. The first issue would be the device causing a fire while charging and while in use, in which a person may be harmed but they can relatively quickly put out the fire with minimal damage to them and their surroundings.
Some of the incidents that the U.S. Fire Administration looked at portrayed that this scenario only occurred about 8% of the time, leaving 9 people injured and 2 people with serious burns. The second issue would be if the device is left alone charging and the person goes off into another room or leaves the house completely, and the device implodes.
In the cases in which fires were started, 52% of the fires were small-scale or minor. In those cases people were around to stop the fire, but what about the other cases in which a person doesn't notice the fire or if they are not even in the house when the fire starts? 32% of cases showcase a moderate fire and 4% of cases showcase that the fire destroyed the room the device was in and its contents.
Another report from the U.S. Fire Administration states the following, “In 27 incidents, the fire spread was moderate, where the burned area was larger than 6 inches in diameter, but the fire was extinguished by occupants before the fire department arrived. In 10 incidents, the fire spread was major and involved significant portions of a building and required suppression by the fire department,".
The U.S. Fire Administration also notes that in most cases, when the device has combusted, the fire produced spreads to nearby clothing, carpets, drapes, etc. About 66% of explosions led to a fire, because of the contents in the radius of the explosion.
Marketing
Main article: Electronic cigarette and e-cigarette liquid marketing
They are marketed to men, women, and children as being safer than traditional cigarettes. They are also marketed to non-smokers. E-cigarette marketing is common. There are growing concerns that e-cigarette advertising campaigns unjustifiably focus on young adults, adolescents, and women.
Large tobacco companies have greatly increased their marketing efforts. This marketing trend may expand the use of e-cigarettes and contribute to re-glamorizing smoking. Some companies may use e-cigarette advertising to advocate smoking, deliberately, or inadvertently, is an area of concern.
A 2014 review said, "the e-cigarette companies have been rapidly expanding using aggressive marketing messages similar to those used to promote cigarettes in the 1950s and 1960s."
E-cigarette companies are using methods that were once used by the tobacco industry to persuade young people to start using cigarettes. E-cigarettes are promoted to a certain extent to forge a vaping culture that entices non-smokers. Themes in e-cigarette marketing, including sexual content and customer satisfaction, are parallel to themes and techniques that are appealing to youth and young adults in traditional cigarette advertising and promotion
A 2017 review found "The tobacco industry sees a future where ENDS accompany and perpetuate, rather than supplant, tobacco use, especially targeting the youth." E-cigarettes and nicotine are regularly promoted as safe and even healthy in the media and on brand websites, which is an area of concern.
While advertising of tobacco products is banned in most countries, television and radio e-cigarette advertising in several countries may be indirectly encouraging traditional cigarette use E-cigarette advertisements are also in magazines, newspapers, online, and in retail stores. Between 2010 and 2014, e-cigarettes were second only to cigarettes as the top advertised product in magazines.
As cigarette companies have acquired the largest e-cigarette brands, they currently benefit from a dual market of smokers and e-cigarette users while simultaneously presenting themselves as agents of harm reduction.
This raises concerns about the appropriateness of endorsing a product that directly profits the tobacco industry. There is no evidence that the cigarette brands are selling e-cigarettes as part of a plan to phase out traditional cigarettes, despite some stating to want to cooperate in "harm reduction". E-cigarette advertising for using e-cigarettes as a quitting tool have been seen in the US, UK, and China, which have not been supported by regulatory bodies.
In the US, six large e-cigarette businesses spent $59.3 million on promoting e-cigarettes in 2013. In the US and Canada, over $2 million is spent yearly on promoting e-cigarettes online. E-cigarette websites often made unscientific health statements in 2012.
The ease to get past the age verification system at e-cigarette company websites allows underage individuals to access and be exposed to marketing. Around half of e-cigarette company websites have a minimum age notice that prohibited underage individuals from entering.
Celebrity endorsements are used to encourage e-cigarette use. A 2012 national US television advertising campaign for e-cigarettes starred Stephen Dorff exhaling a "thick flume" of what the advertisement describes as "vapor, not tobacco smoke", exhorting smokers with the message "We are all adults here, it's time to take our freedom back."
Opponents of the tobacco industry state that the advertisement, in a context of longstanding prohibition of tobacco advertising on television, seems to have resorted to advertising tactics that got former generations of people in the US addicted to traditional cigarettes.
Cynthia Hallett of Americans for Non-Smokers' Rights described the US advertising campaign as attempting to "re-establish a norm that smoking is okay, that smoking is glamorous and acceptable".
University of Pennsylvania communications professor Joseph Cappella stated that the setting of the advertisement near an ocean was meant to suggest an association of clean air with the nicotine product.
In 2012 and 2013, e-cigarette companies advertised to a large television audience in the US which included 24 million youth. The channels to which e-cigarette advertising reached the largest numbers of youth (ages 12–17) were AMC, Country Music Television, Comedy Central, WGN America, TV Land, and VH1.
E-cigarettes are heavily promoted across all media outlets. They are vigorously advertised, mostly through the Internet, as a safe substitute to traditional cigarettes, among other things. E-cigarette companies promote their e-cigarette products on Facebook, Instagram, YouTube, and Twitter. They are promoted on YouTube by movies with sexual material and music icons, who encourage minors to "take their freedom back." They have partenered with a number of sports and music icons to promote their products.
Tobacco companies intensely market e-cigarettes to youth, with industry strategies including cartoon characters and candy flavors. Fruit flavored e-liquid is the most commonly marketed e-liquid flavor on social media. E-cigarette companies commonly promote that their products contain only water, nicotine, glycerin, propylene glycol, and flavoring but this assertion is misleading as researchers have found differing amounts of heavy metals in the vapor, including chromium, nickel, tin, silver, cadmium, mercury, and aluminum.
The widespread assertion that e-cigarettes emit "only water vapor" is not true because the evidence demonstrates e-cigarette vapor contains possibly harmful chemicals such as nicotine, carbonyls, metals, and volatile organic compounds, in addition to particulate matter.
Massive advertising included the assertion that they would present little risk to non-users. Though, "disadvantages and side effects have been reported in many articles, and the unfavorable effects of its secondhand vapor have been demonstrated in many studies" and evidence indicates that use of e-cigarettes degrades indoor air quality.
Many e-cigarette companies market their products as a smoking cessation aid without evidence of effectiveness. E-cigarette marketing has been found to make unsubstantiated health statements (e.g., that they help one quit smoking) including statements about improving psychiatric symptoms, which may be particularly appealing to smokers with mental illness. E-cigarette marketing advocate weight control and emphasize use of nicotine with many flavors.
These marketing angles could particularly entice overweight people, youth, and vulnerable groups. Some e-cigarette companies state that their products are green without supporting evidence, which may be purely to increase their sales.
Economics:
The number of e-cigarettes sold increased every year from 2003 to 2014. In 2015 a slowdown in the growth in usage occurred in the US. As of January 2018, the growth in usage in the UK has slowed down since 2013. As of 2014 there were at least 466 e-cigarette brands.
Worldwide e-cigarette sales in 2014 were around US$7 billion. Worldwide e-cigarette sales in 2019 were about $19.3 billion. E-cigarette sales could exceed traditional cigarette sales by 2023. Approximately 30–50% of total e-cigarettes sales are handled on the internet. Established tobacco companies have a significant share of the e-cigarette market.
As of 2018, 95% of e-cigarette devices were made in China, mainly in Shenzhen. Chinese companies' market share of e-liquid is low.In 2014, online and offline sales starting increases. Since combustible cigarettes are relatively inexpensive in China a lower price may not be large factor in marketing vaping products over there.
In 2015, 80% of all e-cigarette sales in convenience stores in the US were products made by tobacco companies. According to Nielsen Holdings, convenience store e-cigarette sales in the US went down for the first time during the four-week period ending on 10 May 2014.
Wells Fargo analyst Bonnie Herzog attributes this decline to a shift in consumers' behavior, buying more specialized devices or what she calls "vapors-tanks-mods (VTMs)" that are not tracked by Nielsen. Wells Fargo estimated that VTMs accounted for 57% of the 3.5 billion dollar market in the US for vapor products in 2015.
In 2014, dollar sales of customizable e-cigarettes and e-liquid surpassed sales of cigarette-imitators in the US, even though, overall, these are a less expensive vaping option. In 2014, the Smoke-Free Alternatives Trade Association estimated that there were 35,000 vape shops in the US, more than triple the number a year earlier.
However the 2015 slowdown in market growth affected VTMs as well. Large tobacco retailers are leading the cigalike market. "We saw the market's sudden recognition that the cigarette industry seems to be in serious trouble, disrupted by the rise of vaping," Mad Money's Jim Cramer stated April 2018. "Over the course of three short days, the tobacco stocks were bent, they were spindled and they were mutilated by the realization that electronic cigarettes have become a serious threat to the old-school cigarette makers," he added.
In 2019, a vaping industry organization released a report stating that a possible US ban on e-cigarettes flavors can potentially effect greater than 150,000 jobs around the US.
The leading seller in the e-cigarette market in the US is the Juul e-cigarette, which was introduced in June 2015. As of August 2018, Juul accounts for over 72% of the US e-cigarette market monitored by Nielsen, and its closest competitor--RJ Reynolds' Vuse—makes up less than 10% of the market. Juul rose to popularity quickly, growing by 700% in 2016 alone.
On 17 July 2018 Reynolds announced it will debut in August 2018 a pod mod type device similar Juul. The popularity of the Juul pod system has led to a flood of other pod devices hitting the market.
In Canada, e-cigarettes had an estimated value of 140 million CAD in 2015. There are numerous e-cigarette retail shops in Canada. A 2014 audit of retailers in four Canadian cities found that 94% of grocery stores, convenience stores, and tobacconist shops which sold e-cigarettes sold nicotine-free varieties only, while all vape shops stocked at least one nicotine-containing product.
By 2015 the e-cigarette market had only reached a twentieth of the size of the tobacco market in the UK. In the UK in 2015 the "most prominent brands of cigalikes" were owned by tobacco companies, however, with the exception of one model, all the tank types came from "non-tobacco industry companies". Yet some tobacco industry products, while using prefilled cartridges, resemble tank models.
France's e-cigarette market was estimated by Groupe Xerfi to be €130 million in 2015. Additionally, France's e-liquid market was estimated at €265 million. In December 2015, there were 2,400 vape shops in France, 400 fewer than in March of the same year. Industry organization Fivape said the reduction was due to consolidation, not to reduced demand.
Environmental impact:
Compared to traditional cigarettes, reusable e-cigarettes do not create waste and potential litter from every use in the form of discarded cigarette butts. Traditional cigarettes tend to end up in the ocean where they cause pollution, though once discarded they undergo biodegradation and photodegradation.
Although some brands have begun recycling services for their e-cigarette cartridges and batteries, the prevalence of recycling is unknown. E-cigarettes that are not reusable contribute to the problem of electronic waste, which can create a hazard for people and other organisms.
If improperly disposed of, they can release heavy metals, nicotine, and other chemicals from batteries and unused e-liquid. A July 2018–April 2019 garbology study found e-cigarette products composed 19% of the waste from all traditional and electronic tobacco and cannabis products collected at 12 public high schools in Northern California.
Related technologies:
Other devices to deliver inhaled nicotine have been developed. They aim to mimic the ritual and behavioral aspects of traditional cigarettes.
British American Tobacco, through their subsidiary Nicoventures, licensed a nicotine delivery system based on existing asthma inhaler technology from UK-based healthcare company Kind Consumer. In September 2014 a product based on this named Voke obtained approval from the United Kingdom's Medicines and Healthcare Products Regulatory Agency.
In 2011 Philip Morris International bought the rights to a nicotine pyruvate technology developed by Jed Rose at Duke University. The technology is based on the chemical reaction between pyruvic acid and nicotine, which produces an inhalable nicotine pyruvate vapor.
Morris Products S.A. created a different kind e-cigarette named P3L. The device is supplied with a cartridge that contains nicotine and lactic acid in different cavities. When turned on and heated, the nicotine salt called nicotine lactate forms an aerosol.
The IQOS is a heated tobacco product marketed by Philip Morris International. It heats tobacco at a lower temperature than traditional cigarettes. The tobacco sticks reach a temperature up to 350 °C. It sold first in Japan since November 2014.
On 2 December 2016, the United Tobacco Vapor Group's (UTVG) stated that they have been given a patent for their vaporizing component system. qmos from UTVG does not contain a wick or sponge and the number of components is 5 compared to 20 for traditional e-cigarettes.
Pax Labs has developed vaporizers that heats the leaves of tobacco to deliver nicotine in a vapor. On 1 June 2015, they introduced Juul a type of e-cigarette which delivers 10 times as much nicotine as other e-cigarettes, equivalent to an actual cigarette puff.
Juul was spun off from Pax Labs in June 2017 and is now available by the independent company Juul Labs. The eTron 3T from Vapor Tobacco Manufacturing, launched in December 2014, employs a patented, aqueous system whereby the tobacco is extracted into water. The e-liquid contains organic tobacco, organic glycerin, and water.
In December 2013 Japan Tobacco launched Ploom in Japan. In January 2016 they launched Ploom TECH that produces a vapor from a heated liquid that moves through a capsule of granulated tobacco leaves.
In 2016 British American Tobacco (BAT) released its own version of the heat but not burn technology called glo in Japan and Switzerland. It uses tobacco sticks rather than nicotine liquid, and does not directly heat or burn tobacco.
In 2015 the glo iFuse was released in Romania by BAT. It uses a coil to heat a liquid that produces a vapor that moves through mixed tobacco. Heated tobacco products were first introduced in 1988, but were not a commercial success.
BLOW started selling e-hookahs, an electronic version of the hookah, in 2014. The handle of each hose for the e-hookah contains a heating element and a liquid, which produces vapor.
Gopal Bhatnagar based in Toronto, Canada invented a 3D printed adapter to turn a traditional hookah into an e-hookah. It is used instead of the ceramic bowl that contains shisha tobacco. Rather than the tobacco, users can insert e-cigarettes.
KanaVape is an e-cigarette containing cannabidiol (CBD) and no THC. Several companies including Canada's Eagle Energy Vapor are selling caffeine-based e-cigarettes instead of containing nicotine.
Nicotine Addiction Creates Dependency
- YouTube Video: Jeffrey Wigand: The big tobacco whistleblower
- YouTube Video: Long term effects of nicotine
- YouTube Video: BIGGEST Consumer KILLER?: The Seduction of SMOKING | Ep 1 | Science Documentary | Reel Truth Science
[Your WebHost: In this and the related topic below it, we cover the causes of addiction to cigarettes (as well as to vaping in the topic directly above this one). All of these are blamed for the worst health addiction impacting humankind: Smoking. Click here to jump to Smoking below For your information, my wife passed away 2008 due to lung cancer from smoking. Had we known what we know today, she might still be alive: every day she is missed!]
Nicotine is a chiral alkaloid that is naturally produced in the nightshade family of plants (most predominantly in tobacco and Duboisia hopwoodii) and is widely used recreationally as a stimulant and anxiolytic.
As a pharmaceutical drug, it is used for smoking cessation to relieve withdrawal symptoms. Nicotine acts as a receptor agonist at most nicotinic acetylcholine receptors (nAChRs), except at two nicotinic receptor subunits (nAChRα9 and nAChRα10) where it acts as a receptor antagonist.
Nicotine constitutes approximately 0.6–3.0% of the dry weight of tobacco. Nicotine is also present at concentrations of millionths of a percent in the edible family Solanaceae, including potatoes, tomatoes, and eggplants, though sources disagree on whether this has any biological significance to human consumers. It functions as an antiherbivore chemical; consequently, nicotine was widely used as an insecticide in the past, and neonicotinoids, such as imidacloprid, are some of the most effective and widely used insecticides.
Nicotine is highly addictive, unless used in slow-release forms. Animal research suggests that monoamine oxidase inhibitors present in tobacco smoke may enhance nicotine's addictive properties. An average cigarette yields about 2 mg of absorbed nicotine. The estimated lower dose limit for fatal outcomes is 500–1,000 mg of ingested nicotine for an adult (6.5–13 mg/kg). Nicotine addiction involves drug-reinforced behavior, compulsive use, and relapse following abstinence.
Nicotine dependence involves tolerance, sensitization, physical dependence, and psychological dependence. Nicotine dependence causes distress. Nicotine withdrawal symptoms include depressed mood, stress, anxiety, irritability, difficulty concentrating, and sleep disturbances.
Mild nicotine withdrawal symptoms are measurable in unrestricted smokers, who experience normal moods only as their blood nicotine levels peak, with each cigarette. On quitting, withdrawal symptoms worsen sharply, then gradually improve to a normal state.
Nicotine use as a tool for quitting smoking has a good safety history. Animal studies suggest that nicotine may adversely affect cognitive development in adolescence, but the relevance of these findings to human brain development is disputed. At low amounts, it has a mild analgesic effect.
According to the International Agency for Research on Cancer, "nicotine is not generally considered to be a carcinogen." The Surgeon General of the United States indicates that evidence is inadequate to infer the presence or absence of a causal relationship between exposure to nicotine and risk for cancer. [Your WebHost: while nicotine itself does not cause cancer, the cigarette commonly used in smoking does!]
Nicotine has been shown to produce birth defects in some animal species, but not others. It is considered a teratogen in humans. The median lethal dose of nicotine in humans is unknown, but high doses are known to cause nicotine poisoning.
Click on any of the following blue hyperlinks for more about Nicotine:
Nicotine dependence is a state of dependence upon nicotine (see above). Nicotine dependence is a chronic, relapsing disease defined as a compulsive craving to use the drug, despite social consequences, loss of control over drug intake, and emergence of withdrawal symptoms
Tolerance is another component of drug dependence. Nicotine dependence develops over time as a person continues to use nicotine. The most commonly used tobacco product is cigarettes, but all forms of tobacco use and e-cigarette use can cause dependence.
Nicotine dependence is a serious public health problem because it leads to continued tobacco use, which is one of the leading preventable causes of death worldwide, causing more than 8 million deaths per year.
According to the World Health Organization, "Greater nicotine dependence has been shown to be associated with lower motivation to quit, difficulty in trying to quit, and failure to quit, as well as with smoking the first cigarette earlier in the day and smoking more cigarettes per day."
The WHO estimates that there 1.1 billion smokers globally. Of the 34 million smokers in the US in 2018, 74.6% smoked every day, indicating the potential for some level of nicotine dependence. There is an increased frequency of nicotine dependence in people with anxiety disorders.
There are different ways of measuring nicotine dependence. Common dependence assessment scales for cigarette smokers are the Fagerström Test for Nicotine Dependence, the Diagnostic and Statistical Manual of Mental Disorders, the Cigarette Dependence Scale, the Nicotine Dependence Syndrome Scale, and the Wisconsin Inventory of Smoking Dependence Motives (WISDM).
Nicotine is a sympathomimetic stimulant that attaches to nicotinic acetylcholine receptors in the brain. Neuroplasticity within the brain's reward system, including an increase in the number of nicotine receptors, occurs as a result of long-term nicotine use, leading to nicotine dependence.
There are genetic risk factors for developing dependence. For instance, genetic markers for a specific type of nicotinic receptor (the α5-α3-β4 nicotine receptors) have been linked to increased risk for dependence.
Evidence-based treatments, including medications (nicotine replacement therapy, bupropion, varenicline, or cytisine) and behavioral counseling, can double or triple a smoker's chances of quitting successfully.
Click on any of the following blue hyperlinks for more about Nicotine Dependency:
Nicotine is a chiral alkaloid that is naturally produced in the nightshade family of plants (most predominantly in tobacco and Duboisia hopwoodii) and is widely used recreationally as a stimulant and anxiolytic.
As a pharmaceutical drug, it is used for smoking cessation to relieve withdrawal symptoms. Nicotine acts as a receptor agonist at most nicotinic acetylcholine receptors (nAChRs), except at two nicotinic receptor subunits (nAChRα9 and nAChRα10) where it acts as a receptor antagonist.
Nicotine constitutes approximately 0.6–3.0% of the dry weight of tobacco. Nicotine is also present at concentrations of millionths of a percent in the edible family Solanaceae, including potatoes, tomatoes, and eggplants, though sources disagree on whether this has any biological significance to human consumers. It functions as an antiherbivore chemical; consequently, nicotine was widely used as an insecticide in the past, and neonicotinoids, such as imidacloprid, are some of the most effective and widely used insecticides.
Nicotine is highly addictive, unless used in slow-release forms. Animal research suggests that monoamine oxidase inhibitors present in tobacco smoke may enhance nicotine's addictive properties. An average cigarette yields about 2 mg of absorbed nicotine. The estimated lower dose limit for fatal outcomes is 500–1,000 mg of ingested nicotine for an adult (6.5–13 mg/kg). Nicotine addiction involves drug-reinforced behavior, compulsive use, and relapse following abstinence.
Nicotine dependence involves tolerance, sensitization, physical dependence, and psychological dependence. Nicotine dependence causes distress. Nicotine withdrawal symptoms include depressed mood, stress, anxiety, irritability, difficulty concentrating, and sleep disturbances.
Mild nicotine withdrawal symptoms are measurable in unrestricted smokers, who experience normal moods only as their blood nicotine levels peak, with each cigarette. On quitting, withdrawal symptoms worsen sharply, then gradually improve to a normal state.
Nicotine use as a tool for quitting smoking has a good safety history. Animal studies suggest that nicotine may adversely affect cognitive development in adolescence, but the relevance of these findings to human brain development is disputed. At low amounts, it has a mild analgesic effect.
According to the International Agency for Research on Cancer, "nicotine is not generally considered to be a carcinogen." The Surgeon General of the United States indicates that evidence is inadequate to infer the presence or absence of a causal relationship between exposure to nicotine and risk for cancer. [Your WebHost: while nicotine itself does not cause cancer, the cigarette commonly used in smoking does!]
Nicotine has been shown to produce birth defects in some animal species, but not others. It is considered a teratogen in humans. The median lethal dose of nicotine in humans is unknown, but high doses are known to cause nicotine poisoning.
Click on any of the following blue hyperlinks for more about Nicotine:
- Uses
- Contraindications
- Adverse effects
- Overdose
- Drug interactions
- Pharmacology
- Chemistry
- Natural occurrence
- History, society, and culture
- Research
- See also:
Nicotine dependence is a state of dependence upon nicotine (see above). Nicotine dependence is a chronic, relapsing disease defined as a compulsive craving to use the drug, despite social consequences, loss of control over drug intake, and emergence of withdrawal symptoms
Tolerance is another component of drug dependence. Nicotine dependence develops over time as a person continues to use nicotine. The most commonly used tobacco product is cigarettes, but all forms of tobacco use and e-cigarette use can cause dependence.
Nicotine dependence is a serious public health problem because it leads to continued tobacco use, which is one of the leading preventable causes of death worldwide, causing more than 8 million deaths per year.
According to the World Health Organization, "Greater nicotine dependence has been shown to be associated with lower motivation to quit, difficulty in trying to quit, and failure to quit, as well as with smoking the first cigarette earlier in the day and smoking more cigarettes per day."
The WHO estimates that there 1.1 billion smokers globally. Of the 34 million smokers in the US in 2018, 74.6% smoked every day, indicating the potential for some level of nicotine dependence. There is an increased frequency of nicotine dependence in people with anxiety disorders.
There are different ways of measuring nicotine dependence. Common dependence assessment scales for cigarette smokers are the Fagerström Test for Nicotine Dependence, the Diagnostic and Statistical Manual of Mental Disorders, the Cigarette Dependence Scale, the Nicotine Dependence Syndrome Scale, and the Wisconsin Inventory of Smoking Dependence Motives (WISDM).
Nicotine is a sympathomimetic stimulant that attaches to nicotinic acetylcholine receptors in the brain. Neuroplasticity within the brain's reward system, including an increase in the number of nicotine receptors, occurs as a result of long-term nicotine use, leading to nicotine dependence.
There are genetic risk factors for developing dependence. For instance, genetic markers for a specific type of nicotinic receptor (the α5-α3-β4 nicotine receptors) have been linked to increased risk for dependence.
Evidence-based treatments, including medications (nicotine replacement therapy, bupropion, varenicline, or cytisine) and behavioral counseling, can double or triple a smoker's chances of quitting successfully.
Click on any of the following blue hyperlinks for more about Nicotine Dependency:
- Definition
- Diagnosis
- Mechanisms
- Treatment
- Epidemiology
- Concerns
- See also:
- Nicotine poisoning
- Nicotine withdrawal
- Fagerstrom Test of Nicotine Dependence (Heatherton et al., 1991)
- Diagnostic and Statistical Manual of Mental Disorders V (DSM-V)
- Nicotine Dependence Syndrome Scale (NDSS; Shiffman, Waters & Hickcox, 2004)
- Cigarette Dependence Scale (Etter et al., 2003)
- Wisconsin Inventory of Smoking Dependence Motives (Piper et al., 2004)
Smoking Tobacco and its Health Effects
- YouTube Video: Smoking Causes Cancer, Heart Disease, Emphysema
- YouTube Video: The Dangers Of All Forms of Tobacco
- YouTube Video: How to Quit Smoking
Tobacco smoking is the practice of smoking tobacco and inhaling tobacco smoke (consisting of particle and gaseous phases). (A more broad definition may include simply taking tobacco smoke into the mouth, and then releasing it, as is done by some with tobacco pipes and cigars.)
The practice is believed to have begun as early as 5000–3000 BC in Mesoamerica and South America. Tobacco was introduced to Eurasia in the late 17th century by European colonists, where it followed common trade routes.
The practice encountered criticism from its first import into the Western world onwards but embedded itself in certain strata of a number of societies before becoming widespread upon the introduction of automated cigarette-rolling apparatus.
German scientists identified a link between smoking and lung cancer in the late 1920s, leading to the first anti-smoking campaign in modern history, albeit one truncated by the collapse of Nazi Germany at the end of World War II.
In 1950, British researchers demonstrated a clear relationship between smoking and cancer.
Evidence continued to mount in the 1980s, which prompted political action against the practice. Rates of consumption since 1965 in the developed world
have either peaked or declined. However, they continue to climb in the developing world.
Smoking is the most common method of consuming tobacco, and tobacco is the most common substance smoked. The agricultural product is often mixed with additives and then combusted. The resulting smoke is then inhaled and the active substances absorbed through the alveoli in the lungs or the oral mucosa. Combustion was traditionally enhanced by addition of potassium or nitrates.
Many substances in cigarette smoke trigger chemical reactions in nerve endings, which heighten heart rate, alertness and reaction time, among other things. Dopamine and endorphins are released, which are often associated with pleasure.
As of 2008 to 2010, tobacco is used by about 49% of men and 11% of women aged 15 or older in fourteen low-income and middle-income countries (Bangladesh, Brazil, China, Egypt, India, Mexico, Philippines, Poland, Russia, Thailand, Turkey, Ukraine, Uruguay and Vietnam), with about 80% of this usage in the form of smoking. The gender gap tends to be less pronounced in lower age groups.
Many smokers begin during adolescence or early adulthood. During the early stages, a combination of perceived pleasure acting as positive reinforcement and desire to respond to social peer pressure may offset the unpleasant symptoms of initial use, which typically include nausea and coughing.
After an individual has smoked for some years, the avoidance of withdrawal symptoms and negative reinforcement become the key motivations to continue.
A study of first smoking experiences of seventh-grade students found out that the most common factor leading students to smoke is cigarette advertisements. Smoking by parents, siblings and friends also encourages students to smoke.
Click on any of the following blue hyperlinks for more about Tobacco Smoking:
Health Effects of Tobacco:
Tobacco use has predominantly negative effects on human health and concern about health effects of tobacco has a long history. Research has focused primarily on cigarette tobacco smoking.
Tobacco smoke contains more than fifty chemicals that cause cancer. Tobacco also contains nicotine, which is a highly addictive psychoactive drug. When tobacco is smoked, nicotine causes physical and psychological dependency.
Cigarettes sold in underdeveloped countries tend to have higher tar content, and are less likely to be filtered, potentially increasing vulnerability to tobacco smoking related disease in these regions.
Tobacco use is the single greatest cause of preventable death globally. As many as half of people who use tobacco die from complications of tobacco use. The World Health Organization (WHO) estimates that each year tobacco causes about 6 million deaths (about 10% of all deaths) with 600,000 of these occurring in non smokers due to second hand smoke.
In the 20th century tobacco is estimated to have caused 100 million deaths. Similarly, the United States Centers for Disease Control and Prevention describes tobacco use as "the single most important preventable risk to human health in developed countries and an important cause of premature death worldwide."
Currently, the number of premature deaths in the U.S. from tobacco use per year outnumber the number of workers employed in the tobacco industry 4 to 1. According to a 2014 review in the New England Journal of Medicine, tobacco will, if current smoking patterns persist, kill about 1 billion people in the 21st century, half of them before the age of 70.
Tobacco use leads most commonly to diseases affecting the heart, liver and lungs. Smoking is a major risk factor for heart attacks, strokes, chronic obstructive pulmonary disease (COPD) (including emphysema and chronic bronchitis), and several cancers (particularly lung cancer, cancers of the larynx and mouth, bladder cancer, and pancreatic cancer).
It also causes peripheral arterial disease and high blood pressure. The effects depend on the number of years that a person smokes and on how much the person smokes. Starting smoking earlier in life and smoking cigarettes higher in tar increases the risk of these diseases. Also, environmental tobacco smoke, or secondhand smoke, has been shown to cause adverse health effects in people of all ages.
Tobacco use is a significant factor in miscarriages among pregnant smokers, and it contributes to a number of other health problems of the fetus such as premature birth, low birth weight, and increases by 1.4 to 3 times the chance of sudden infant death syndrome (SIDS). Incidence of erectile dysfunction is approximately 85 percent higher in male smokers compared to non-smokers.
Several countries have taken measures to control the consumption of tobacco with usage and sales restrictions as well as warning messages printed on packaging. Additionally, smoke-free laws that ban smoking in public places such as workplaces, theaters, and bars and restaurants reduce exposure to secondhand smoke and help some people who smoke to quit, without negative economic effects on restaurants or bars. Tobacco taxes that increase the price are also effective, especially in developing countries.
The coughing, throat irritation, and shortness of breath caused by smoking have always been obvious. The idea that tobacco use caused some diseases, including mouth cancers, was initially, in the late 1700s and the 1800s, widely accepted by the medical community. In the 1880s, automation slashed the cost of cigarettes, and use expanded.
From the 1890s onwards, associations of tobacco use with cancers and vascular disease were regularly reported; a metaanalysis citing 167 other works was published in 1930, and concluded that tobacco use caused cancer.
Increasingly solid observational evidence was published throughout the 1930s, and in 1938, Science published a paper showing that tobacco users live substantially shorter lives.
Case-control studies were published in Germany in 1939 and 1943, and one in the Netherlands in 1948, but widespread attention was first drawn by five case-control studies published in 1950 by researchers from the US and UK.
These studies were widely criticized as showing correlation, not causality. Follow up prospective cohort studies in the early 1950s clearly found that that smokers died faster, and were more likely to die of lung cancer and cardiovascular disease. These results were first widely accepted in the medical community, and publicized among the general public, in the mid-1960s.
Click on any of the following blue hyperlinks for more about the Health Effects of Tobacco:
The practice is believed to have begun as early as 5000–3000 BC in Mesoamerica and South America. Tobacco was introduced to Eurasia in the late 17th century by European colonists, where it followed common trade routes.
The practice encountered criticism from its first import into the Western world onwards but embedded itself in certain strata of a number of societies before becoming widespread upon the introduction of automated cigarette-rolling apparatus.
German scientists identified a link between smoking and lung cancer in the late 1920s, leading to the first anti-smoking campaign in modern history, albeit one truncated by the collapse of Nazi Germany at the end of World War II.
In 1950, British researchers demonstrated a clear relationship between smoking and cancer.
Evidence continued to mount in the 1980s, which prompted political action against the practice. Rates of consumption since 1965 in the developed world
have either peaked or declined. However, they continue to climb in the developing world.
Smoking is the most common method of consuming tobacco, and tobacco is the most common substance smoked. The agricultural product is often mixed with additives and then combusted. The resulting smoke is then inhaled and the active substances absorbed through the alveoli in the lungs or the oral mucosa. Combustion was traditionally enhanced by addition of potassium or nitrates.
Many substances in cigarette smoke trigger chemical reactions in nerve endings, which heighten heart rate, alertness and reaction time, among other things. Dopamine and endorphins are released, which are often associated with pleasure.
As of 2008 to 2010, tobacco is used by about 49% of men and 11% of women aged 15 or older in fourteen low-income and middle-income countries (Bangladesh, Brazil, China, Egypt, India, Mexico, Philippines, Poland, Russia, Thailand, Turkey, Ukraine, Uruguay and Vietnam), with about 80% of this usage in the form of smoking. The gender gap tends to be less pronounced in lower age groups.
Many smokers begin during adolescence or early adulthood. During the early stages, a combination of perceived pleasure acting as positive reinforcement and desire to respond to social peer pressure may offset the unpleasant symptoms of initial use, which typically include nausea and coughing.
After an individual has smoked for some years, the avoidance of withdrawal symptoms and negative reinforcement become the key motivations to continue.
A study of first smoking experiences of seventh-grade students found out that the most common factor leading students to smoke is cigarette advertisements. Smoking by parents, siblings and friends also encourages students to smoke.
Click on any of the following blue hyperlinks for more about Tobacco Smoking:
- History
- Consumption
- Psychology
- Economic
- Health
- Social
- Incomes
- Public policy
- Gateway drug theory
- Cessation
- See also:
- Cannabis smoking
- Cigarette smoking among college students
- Cigarette smoking for weight loss
- Electronic cigarette
- Herbal cigarette
- List of cigarette smoke carcinogens
- Tobacco advertising
- Tobacco control
- Snuff (tobacco)
- Tobacco History Links – repository from Tobacco.org
- Surgeon General: Tobacco Cessation
- CDC: Smoking & Tobacco Use
- WHO: Tobacco Free Initiative
- The Tobacco Atlas
- Tobacco Viz
- Cigarette smoking prevalence in US counties: 1996–2012
Health Effects of Tobacco:
Tobacco use has predominantly negative effects on human health and concern about health effects of tobacco has a long history. Research has focused primarily on cigarette tobacco smoking.
Tobacco smoke contains more than fifty chemicals that cause cancer. Tobacco also contains nicotine, which is a highly addictive psychoactive drug. When tobacco is smoked, nicotine causes physical and psychological dependency.
Cigarettes sold in underdeveloped countries tend to have higher tar content, and are less likely to be filtered, potentially increasing vulnerability to tobacco smoking related disease in these regions.
Tobacco use is the single greatest cause of preventable death globally. As many as half of people who use tobacco die from complications of tobacco use. The World Health Organization (WHO) estimates that each year tobacco causes about 6 million deaths (about 10% of all deaths) with 600,000 of these occurring in non smokers due to second hand smoke.
In the 20th century tobacco is estimated to have caused 100 million deaths. Similarly, the United States Centers for Disease Control and Prevention describes tobacco use as "the single most important preventable risk to human health in developed countries and an important cause of premature death worldwide."
Currently, the number of premature deaths in the U.S. from tobacco use per year outnumber the number of workers employed in the tobacco industry 4 to 1. According to a 2014 review in the New England Journal of Medicine, tobacco will, if current smoking patterns persist, kill about 1 billion people in the 21st century, half of them before the age of 70.
Tobacco use leads most commonly to diseases affecting the heart, liver and lungs. Smoking is a major risk factor for heart attacks, strokes, chronic obstructive pulmonary disease (COPD) (including emphysema and chronic bronchitis), and several cancers (particularly lung cancer, cancers of the larynx and mouth, bladder cancer, and pancreatic cancer).
It also causes peripheral arterial disease and high blood pressure. The effects depend on the number of years that a person smokes and on how much the person smokes. Starting smoking earlier in life and smoking cigarettes higher in tar increases the risk of these diseases. Also, environmental tobacco smoke, or secondhand smoke, has been shown to cause adverse health effects in people of all ages.
Tobacco use is a significant factor in miscarriages among pregnant smokers, and it contributes to a number of other health problems of the fetus such as premature birth, low birth weight, and increases by 1.4 to 3 times the chance of sudden infant death syndrome (SIDS). Incidence of erectile dysfunction is approximately 85 percent higher in male smokers compared to non-smokers.
Several countries have taken measures to control the consumption of tobacco with usage and sales restrictions as well as warning messages printed on packaging. Additionally, smoke-free laws that ban smoking in public places such as workplaces, theaters, and bars and restaurants reduce exposure to secondhand smoke and help some people who smoke to quit, without negative economic effects on restaurants or bars. Tobacco taxes that increase the price are also effective, especially in developing countries.
The coughing, throat irritation, and shortness of breath caused by smoking have always been obvious. The idea that tobacco use caused some diseases, including mouth cancers, was initially, in the late 1700s and the 1800s, widely accepted by the medical community. In the 1880s, automation slashed the cost of cigarettes, and use expanded.
From the 1890s onwards, associations of tobacco use with cancers and vascular disease were regularly reported; a metaanalysis citing 167 other works was published in 1930, and concluded that tobacco use caused cancer.
Increasingly solid observational evidence was published throughout the 1930s, and in 1938, Science published a paper showing that tobacco users live substantially shorter lives.
Case-control studies were published in Germany in 1939 and 1943, and one in the Netherlands in 1948, but widespread attention was first drawn by five case-control studies published in 1950 by researchers from the US and UK.
These studies were widely criticized as showing correlation, not causality. Follow up prospective cohort studies in the early 1950s clearly found that that smokers died faster, and were more likely to die of lung cancer and cardiovascular disease. These results were first widely accepted in the medical community, and publicized among the general public, in the mid-1960s.
Click on any of the following blue hyperlinks for more about the Health Effects of Tobacco:
The War on Drugs and the Opioid Epidemic in the United States
- YouTube Video: Let's quit abusing drug users (TedMed)
- YouTube Video: Mechanism of Drug Addiction in the Brain, Animation
- YouTube Video: American Epidemic: The Nation's Struggle With Opioid Addiction
The war on drugs is a campaign, led by the U.S. federal government, of drug prohibition, military aid, and military intervention, with the stated aim being to reduce the illegal drug trade in the United States.
The initiative includes a set of drug policies that are intended to discourage the production, distribution, and consumption of psychoactive drugs that the participating governments and the United Nations have made illegal.
The term was popularized by the media shortly after a press conference given on June 18, 1971, by President Richard Nixon—the day after publication of a special message from President Nixon to the Congress on Drug Abuse Prevention and Control—during which he declared drug abuse "public enemy number one". That message to the Congress included text about devoting more federal resources to the "prevention of new addicts, and the rehabilitation of those who are addicted", but that part did not receive the same public attention as the term "war on drugs".
However, two years prior to this, Nixon had formally declared a "war on drugs" that would be directed toward eradication, interdiction, and incarceration. Today, the Drug Policy Alliance, which advocates for an end to the War on Drugs, estimates that the United States spends $51 billion annually on these initiatives.
On May 13, 2009, Gil Kerlikowske—the Director of the Office of National Drug Control Policy (ONDCP)—signaled that the Obama administration did not plan to significantly alter drug enforcement policy, but also that the administration would not use the term "War on Drugs", because Kerlikowske considers the term to be "counter-productive".
ONDCP's view is that "drug addiction is a disease that can be successfully prevented and treated... making drugs more available will make it harder to keep our communities healthy and safe".
In June 2011, the Global Commission on Drug Policy released a critical report on the War on Drugs, declaring: "The global war on drugs has failed, with devastating consequences for individuals and societies around the world.
Fifty years after the initiation of the UN Single Convention on Narcotic Drugs, and years after President Nixon launched the US government's war on drugs, fundamental reforms in national and global drug control policies are urgently needed." The report was criticized by organizations that oppose a general legalization of drugs.
Click on any of the following blue hyperlinks for more about the War on Drugs:
Opioid epidemic in the United States:
The opioid epidemic or opioid crisis is a term that generally refers to the rapid increase in the use of prescription and nonprescription opioid drugs, in the United States, beginning in the late 1990s. The increase in opioid overdose deaths has been dramatic, and opioids were responsible for 47,600 of the 70,200 drug overdose deaths overall in the US in 2017. The rate of prolonged opioid use is increasing globally.
Drug overdoses have become the leading cause of death of Americans under 50, with two-thirds of those deaths from opioids. In 2016, the crisis decreased overall life expectancy of Americans for the second consecutive year.
Overall life expectancy fell from 78.7 to 78.6 years. Men were disproportionately more affected due to higher overdose death rates, with life expectancy declining from 76.3 to 76.1 years.
Women's life expectancy remained stable at 81.1 years. However, white women, the demographic of women most affected by the crisis, did experience a decline in life expectancy related to the opioid epidemic.
Click on any of the following blue hyperlinks for more about the Opioid Epidemic in the United States:
The initiative includes a set of drug policies that are intended to discourage the production, distribution, and consumption of psychoactive drugs that the participating governments and the United Nations have made illegal.
The term was popularized by the media shortly after a press conference given on June 18, 1971, by President Richard Nixon—the day after publication of a special message from President Nixon to the Congress on Drug Abuse Prevention and Control—during which he declared drug abuse "public enemy number one". That message to the Congress included text about devoting more federal resources to the "prevention of new addicts, and the rehabilitation of those who are addicted", but that part did not receive the same public attention as the term "war on drugs".
However, two years prior to this, Nixon had formally declared a "war on drugs" that would be directed toward eradication, interdiction, and incarceration. Today, the Drug Policy Alliance, which advocates for an end to the War on Drugs, estimates that the United States spends $51 billion annually on these initiatives.
On May 13, 2009, Gil Kerlikowske—the Director of the Office of National Drug Control Policy (ONDCP)—signaled that the Obama administration did not plan to significantly alter drug enforcement policy, but also that the administration would not use the term "War on Drugs", because Kerlikowske considers the term to be "counter-productive".
ONDCP's view is that "drug addiction is a disease that can be successfully prevented and treated... making drugs more available will make it harder to keep our communities healthy and safe".
In June 2011, the Global Commission on Drug Policy released a critical report on the War on Drugs, declaring: "The global war on drugs has failed, with devastating consequences for individuals and societies around the world.
Fifty years after the initiation of the UN Single Convention on Narcotic Drugs, and years after President Nixon launched the US government's war on drugs, fundamental reforms in national and global drug control policies are urgently needed." The report was criticized by organizations that oppose a general legalization of drugs.
Click on any of the following blue hyperlinks for more about the War on Drugs:
- History
- United States domestic policy
- Commonly used illegal drugs
- United States foreign policy and covert military activities
- Public support and opposition in the United States and Mexico
- Socio-economic effects
- Allegations of U.S. government assistance in drug trafficking
- Efficacy of the United States war on drugs
- Legality
- Alternatives
- See also:
- Baker, a series of counter-narcotics training exercises conducted by the United States Army and several Asian countries
- Civil forfeiture in the United States
- Class war
- Cognitive liberty
- Crack epidemic
- Drugs in the United States
- Latin American drug legalization
- Mexican Drug War
- Philippine Drug War
- Prison-industrial complex
- Race war
- Recreational use of drugs
- War on Gangs
- Covert activities and foreign policy
- Government agencies and laws
- Organizations opposing prohibition
- Organizations opposing drug legalization
- Government and NGO reports
- National Drug Threat Assessment 2009 from the United States Department of Justice
- War On Drugs: Legislation in the 108th Congress and Related Developments, a 2003 report from the Congressional Research Service via the State Department website
- The Report of the Canadian Government Commission of Inquiry into the Non-Medical Use of Drugs—1972
- Drug Enforcement Administration (2017), Drugs of abuse: A DEA resource guide (PDF) (2017 ed.), Washington, DC: Author
- Narco News — news site focusing on drug war in Latin America
- Drug War Facts
- Drug War Distortions
- Major Studies of Drugs and Drug Policy Full text of major government commission reports on the drug laws from around the world over the last 100 years
- Historical Research on the Drug War Full text of numerous full histories of the drug war and thousands of original historical documents
- Cato Institute Drug Prohibition Research
- Drug War Victims
- Videos:
- The War on Drugs is the subject of the 2007 documentary film The War on Drugs
- The War on Drugs is covered in the 2006 documentary film Cocaine Cowboys
- The House I Live In—documentary film, Grand Jury Prize SUNDANCE Film Festival 2012
- How to Make Money Selling Drugs—documentary film
Opioid epidemic in the United States:
The opioid epidemic or opioid crisis is a term that generally refers to the rapid increase in the use of prescription and nonprescription opioid drugs, in the United States, beginning in the late 1990s. The increase in opioid overdose deaths has been dramatic, and opioids were responsible for 47,600 of the 70,200 drug overdose deaths overall in the US in 2017. The rate of prolonged opioid use is increasing globally.
Drug overdoses have become the leading cause of death of Americans under 50, with two-thirds of those deaths from opioids. In 2016, the crisis decreased overall life expectancy of Americans for the second consecutive year.
Overall life expectancy fell from 78.7 to 78.6 years. Men were disproportionately more affected due to higher overdose death rates, with life expectancy declining from 76.3 to 76.1 years.
Women's life expectancy remained stable at 81.1 years. However, white women, the demographic of women most affected by the crisis, did experience a decline in life expectancy related to the opioid epidemic.
Click on any of the following blue hyperlinks for more about the Opioid Epidemic in the United States:
- Background
- Causes
- Effects
- Demographics
- Countermeasures
- History
- See also:
- Diseases of despair – including opioid overdose
- Johnson & Johnson
- Opium in Iran, world's highest per capita rate of opiate addiction
- List of deaths from drug overdose and intoxication
- List of countries by prevalence of opiates use
- Teva Pharmaceutical Industries
- Alexander GC, Frattaroli S, Gielen AC, eds. (2017). The Opioid Epidemic: From Evidence to Impact (PDF). Baltimore, Maryland: Johns Hopkins Bloomberg School of Public Health.
- "CDC Guideline for Prescribing Opioids for Chronic Pain". U.S. Centers for Disease Control and Prevention (CDC). April 17, 2019.
- Montgomery, Philip (October 30, 2017). "Faces of an Epidemic". The New Yorker.
- Emily Witt, "A Blizzard of Prescriptions" (review of Beth Macy, Dopesick, Head of Zeus, 2019; Chris McGreal, American Overdose: The Opioid Tragedy in Three Acts, Faber, 2018; Sam Quinones, Dreamland: The True Tale of America's Opiate Epidemic, Bloomsbury, 2016), London Review of Books, vol. 41, no. 7 (April 4, 2019), pp. 23–26. "OxyContin['s] lamentable [market] success was owed to a confluence of factors particular to the US. They include, but are not limited to: the country's dysfunctional privatised healthcare system, which makes it possible for addicts to accumulate doctors willing to prescribe painkillers in a way they can't in the UK; a corrupt regulatory agency [the Food and Drug Administration] beholden to the [pharmaceutical] industry it was tasked with regulating; a punitive legal paradigm that criminalises drug users instead of helping them; an abstinence-only approach to treating drug addiction that impedes evidence-based medication-assisted treatment; corporate greed; a political class that takes marching orders from the lobbyists of said corporations; entrenched poverty, joblessness and hopelessness; and a general epistemological failure when it comes to ideas about what 'drugs' are, which psychoactive chemicals are safe and which are dangerous, and what a drug dealer is supposed to look like. [This] prepared a consumer market for heroin. Hundreds of thousands of lives have been lost, each one of them a world." (Emily Witt, p. 23.)
- "The Opioid Files: Follow The Post's investigation of the opioid epidemic". The Washington Post. July 20, 2019. Retrieved July 23, 2019.
Nicotine Replacement Therapy to quit smoking and reduce the risk of Lung Cancer
- YouTube Video: What is the Single Best Thing You Can Do to Quit Smoking?
- YouTube Video: Comparison of Nicotine Replacement Therapy Products
- YouTube Video: Nicotine Replacement Therapy - Frequently asked questions
Nicotine replacement therapy (NRT) is a medically approved way to treat people with tobacco use disorder by taking nicotine by means other than tobacco. It is used to help with quitting smoking or stopping chewing tobacco. It increases the chance of quitting tobacco smoking by about 55%.
Often it is used along with other behavioral techniques. NRT has also been used to treat ulcerative colitis. Types of NRT include:
The use of multiple types of NRT at a time may increase effectiveness.
Common side effects depend on the formulation of nicotine. Common side effects with the gum include nausea, hiccups, and irritation of the mouth. Common side effects with the patch include skin irritation and a dry mouth while the inhaler commonly results in a cough, runny nose, or headaches.
Serious risks include nicotine poisoning and continued addiction. They do not appear to increase the risk of heart attacks There are possible harms to the baby if used during pregnancy. Nicotine replacement therapy works by reducing cravings caused by nicotine addiction.
They were first approved for use in 1984, in the United States. Nicotine replacement products are on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system. They are available as generic medication.
Click on any of the following blue hyperlinks for more about Nicotine Replacement Therapy:
Often it is used along with other behavioral techniques. NRT has also been used to treat ulcerative colitis. Types of NRT include:
- the adhesive patch,
- chewing gum,
- lozenges,
- nose spray,
- and inhaler.
The use of multiple types of NRT at a time may increase effectiveness.
Common side effects depend on the formulation of nicotine. Common side effects with the gum include nausea, hiccups, and irritation of the mouth. Common side effects with the patch include skin irritation and a dry mouth while the inhaler commonly results in a cough, runny nose, or headaches.
Serious risks include nicotine poisoning and continued addiction. They do not appear to increase the risk of heart attacks There are possible harms to the baby if used during pregnancy. Nicotine replacement therapy works by reducing cravings caused by nicotine addiction.
They were first approved for use in 1984, in the United States. Nicotine replacement products are on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system. They are available as generic medication.
Click on any of the following blue hyperlinks for more about Nicotine Replacement Therapy:
- Medical uses
- Side effects
- Mechanism of action
- Society and culture
- See also:
- Tobacco cessation clinic
- Tobacco harm reduction
- American Legacy Foundation
- Opioid replacement therapy
- "Nicotine". Drug Information Portal. U.S. National Library of Medicine.
- University of Wisconsin Center for Tobacco Research and Intervention
- Recommendations for special populations
- "Nicotine Lozenges". MedlinePlus. 2018-08-15.
- "Nicotine Nasal Spray". MedlinePlus. 2016-07-15.
- "Nicotine Oral Inhalation". MedlinePlus. 2016-07-15.
- "Nicotine Gum". MedlinePlus. 2017-10-15.
Cannabis Use Disorder
- YouTube Video: Is Marijuana Addictive?
- YouTube Video: Understanding Cannabinoids: Your Complete Cannabis Guide / Samantha Miller / Green Flower
- YouTube Video: Cannabis and its effect on mental health
Cannabis use disorder (CUD), also known as cannabis addiction or marijuana addiction, is defined in the fifth revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and ICD-10 as the continued use of cannabis despite clinically significant impairment.
Signs and symptoms:
Cannabis use is associated with comorbid mental health problems, such as mood and anxiety disorders, and discontinuing cannabis use is difficult for some users. Psychiatric comorbidities are often present in dependent cannabis users including a range of personality disorders.
Based on annual survey data, some high school seniors who report smoking daily (nearly 7%, according to one study) may function at a lower rate in school than students that do not. The sedating and anxiolytic properties of tetrahydrocannabinol (THC) in some users might make the use of cannabis an attempt to self-medicate personality or psychiatric disorders.
Dependency:
Prolonged cannabis use produces both pharmacokinetic changes (how the drug is absorbed, distributed, metabolized, and excreted) and pharmacodynamic changes (how the drug interacts with target cells) to the body. These changes require the user to consume higher doses of the drug to achieve a common desirable effect (known as a higher tolerance), reinforcing the body's metabolic systems for eliminating the drug more efficiently and further down-regulating cannabinoid receptors in the brain.
Cannabis users have shown decreased reactivity to dopamine, suggesting a possible link to a dampening of the reward system of the brain and an increase in negative emotion and addiction severity.
Cannabis users can develop tolerance to the effects of THC. Tolerance to the behavioral and psychological effects of THC has been demonstrated in adolescent humans and animals. The mechanisms that create this tolerance to THC are thought to involve changes in cannabinoid receptor function.
One study has shown that between 2001–2002 and 2012–2013, the use of marijuana in the US doubled.
Cannabis dependence develops in about 9% of users, significantly less than that of heroin, cocaine, alcohol, and prescribed anxiolytics, but slightly higher than that for psilocybin, mescaline, or LSD. Of those who use cannabis daily, 10–20% develop dependence.
Withdrawal:
annabis withdrawal symptoms occur in one-half of people in treatment for cannabis use disorders. Symptoms may include any of the following:
It is often paired with rhythmic movement disorder. Most symptoms begin during the first week of abstinence and resolve after a few weeks. About 12% of heavy cannabis users showed cannabis withdrawal as defined by the DSM-5, and this was associated with significant disability as well as mood, anxiety and personality disorders.
Cause:
Cannabis addiction is often due to prolonged and increasing use of the drug. Increasing the strength of the cannabis taken and an increasing use of more effective methods of delivery often increase the progression of cannabis dependency. It can also be caused by being prone to becoming addicted to substances, which can either be genetically or environmentally acquired.
Risk factors:
Certain factors are considered to heighten the risk of developing cannabis dependence and longitudinal studies over a number of years have enabled researchers to track aspects of social and psychological development concurrently with cannabis use.
Increasing evidence is being shown for the elevation of associated problems by the frequency and age at which cannabis is used, with young and frequent users being at most risk.
The main factors in Australia, for example, related to a heightened risk for developing problems with cannabis use include frequent use at a young age; personal maladjustment; emotional distress; poor parenting; school drop-out; affiliation with drug-using peers; moving away from home at an early age; daily cigarette smoking; and ready access to cannabis.
The researchers concluded there is emerging evidence that positive experiences to early cannabis use are a significant predictor of late dependence and that genetic predisposition plays a role in the development of problematic use.
High risk groups:
A number of groups have been identified as being at greater risk of developing cannabis dependence and, in Australia, for example, have been found to include adolescent populations, Aboriginal and Torres Strait Islanders and people suffering from mental health conditions.
Adolescents:
The endocannabinoid system is directly involved in adolescent brain development. Adolescent cannabis users are therefore particularly vulnerable to the potential adverse effects of cannabis use. Adolescent cannabis use is associated with increased cannabis misuse as an adult, issues with memory and concentration, long-term cognitive complications, and poor psychiatric outcomes including social anxiety, suicidality and addiction.
There are a lot of reasons why adolescents start a smoking habit. According to a study completed by Bill Sanders, friends influence, difficult household problems, and experimentation are some of the reasons why this population starts to smoke marijuana.
This segment of population seems to be one of the most influenceable group there is. They want to follow the group and look "cool", "hip" and accepted by their friends. This fear of rejection plays a big role in their decision to smoke pot. However it does not seem to be the most important factor. According to a study from Canada, the lack of knowledge about cannabis seems to be the main reason why adolescents start to smoke.
The authors observed a high correlation between adolescents that knew about the mental and physical harms of cannabis and their consumption. Of the 1045 young participants in the study, those who could name the least number of negative effects about this drug were usually the ones who were consuming it. They were not isolated cases either. Actually, the study showed that the proportion of teenagers who saw cannabis as a high-risk drug and the ones who thought the contrary was about the same.
Pregnancy:
There is an association between smoking cannabis during pregnancy and low birth weight. Smoking cannabis during pregnancy can lower the amount of oxygen delivered to the developing fetus, which can restrict fetal growth.
The active ingredient in cannabis (D9-tetrahydrocannabinol, THC) is fat soluble and can enter into breastmilk during lactation. THC in breastmilk can then subsequently be taken up by a breastfeeding infant, as shown by the presence of THC in the infant's feces. However, the evidence for long-term effects of exposure to THC through breastmilk is unclear.
Diagnosis:
Cannabis use disorder is recognized in the fifth version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which also added cannabis withdrawal as a new condition.
In the 2013 revision for the DSM-5, DSM-IV abuse and dependence were combined into cannabis use disorder. The legal problems criterion (from cannabis abuse) has been removed, and the craving criterion was newly added, resulting in a total of eleven criteria: hazardous use, social/interpersonal problems, neglected major roles, withdrawal, tolerance, used larger amounts/longer, repeated attempts to quit/control use, much time spent using, physical/psychological problems related to use, activities given up and craving.
For a diagnosis of DSM-5 cannabis use disorder, at least two of these criteria need to be present in the last twelve-month period. Additionally, three severity levels have been defined: mild (two or three criteria), moderate (four or five criteria) and severe (six or more criteria) cannabis use disorder.
Cannabis use disorder is also recognized in the eleventh revision of the International Classification of Diseases (ICD-11), adding more subdivisions including time intervals of pattern of use (episodic, continuous, or unspecified) and dependence (current, early full remission, sustained partial remission, sustained full remission, or unspecified) compared to the 10th revision.
A 2019 meta-analysis found that 34% of people with cannabis-induced psychosis transitioned to schizophrenia. This was found to be comparatively higher than hallucinogens (26%) and amphetamines (22%).
To screen for cannabis-related problems, several methods are used. Scales specific to cannabis, which provides the benefit of being cost efficient compared to extensive diagnostic interviews, include the Cannabis Abuse Screening Test (CAST), Cannabis Use Identification Test (CUDIT), and Cannabis Use Problems Identification Test (CUPIT). Scales for general drug use disorders are also used, including the Severity Dependence Scale (SDS), Drug Use Disorder Identification Test (DUDIT), and Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST).
However, there are no gold standard and both older and newer scales are still in use.[43] To quantify cannabis use, methods such as Timeline Follow-Back (TLFB) and Cannabis Use Daily (CUD) are used. These methods measure general consumption and not grams of psychoactive substance as the concentration of THC may vary among drug users.
Treatment:
Clinicians differentiate between casual users who have difficulty with drug screens, and daily heavy users, to a chronic user who uses multiple times a day. In the US, as of 2013, cannabis is the most commonly identified illicit substance used by people admitted to treatment facilities.
Demand for treatment for cannabis use disorder increased internationally between 1995 and 2002. In the United States, the average adult who seeks treatment has consumed cannabis for over 10 years almost daily and has attempted to quit six or more times.
Treatment options for cannabis dependence are far fewer than for opiate or alcohol dependence. Most treatment falls into the categories of psychological or psychotherapeutic, intervention, pharmacological intervention or treatment through peer support and environmental approaches.
No medications have been found effective for cannabis dependence, but psychotherapeutic models hold promise. Screening and brief intervention sessions can be given in a variety of settings, particularly at doctor's offices, which is of importance as most cannabis users seeking help will do so from their general practitioner rather than a drug treatment service agency.
The most commonly accessed forms of treatment in Australia are 12-step programmes, physicians, rehabilitation programs, and detox services, with inpatient and outpatient services equally accessed. In the EU approximately 20% of all primary admissions and 29% of all new drug clients in 2005, had primary cannabis problems. And in all countries that reported data between 1999 and 2005 the number of people seeking treatment for cannabis use increased.
Psychological:
Psychological intervention includes cognitive behavioral therapy (CBT), motivational enhancement therapy (MET), contingency management (CM), supportive-expressive psychotherapy (SEP), family and systems interventions, and twelve-step programs.
Evaluations of Marijuana Anonymous programs, modelled on the 12-step lines of Alcoholics Anonymous and Narcotics Anonymous, have shown small beneficial effects for general drug use reduction. In 2006, the Wisconsin Initiative to Promote Healthy Lifestyles implemented a program that helps primary care physicians identify and address marijuana use problems in patients.
Medication:
As of 2020, there is no single medication that has been proven effective for treating cannabis use disorder; research is focused on three treatment approaches: agonist substitution, antagonist, and modulation of other neurotransmitter systems. More broadly, the goal of medication therapy for cannabis use disorder centers around targeting the stages of the addiction: acute intoxication/binge, withdrawal/negative affect, and preoccupation/anticipation.
For the treatment of the withdrawal/negative affect symptom domain of cannabis use disorder, medications may work by alleviating restlessness, irritable or depressed mood, anxiety, and insomnia. Bupropion, which is a norepinephrine–dopamine reuptake inhibitor, has been studied for the treatment of withdrawal with largely poor results. Atomoxetine has also shown poor results, and is as a norepinephrine reuptake inhibitor, though it does increase the release of dopamine through downstream effects in the prefrontal cortex (an area of the brain responsible for planning complex tasks and behavior).
Venlafaxine, a serotonin–norepinephrine reuptake inhibitor, has also been studied for cannabis use disorder, with the thought that the serotonergic component may be useful for the depressed mood or anxious dimensions of the withdrawal symptom domain. While venlafaxine has been shown to improve mood for people with cannabis use disorder, a clinical trial in this population actually found worse cannabis abstinence rates compared to placebo.
It is worth noting that venlafaxine is sometimes poorly tolerated, and infrequent use or abrupt discontinuation of its use can lead to withdrawal symptoms from the medication itself, including irritability, dysphoria, and insomnia. It is possible that venlafaxine use actually exacerbated cannabis withdrawal symptoms, leading people to use more cannabis than placebo to alleviate their discomfort. Mirtazapine, which increases serotonin and norepinephrine, has also failed to improve abstinence rates in people with cannabis use disorder.
People sometimes use cannabis to cope with their anxiety, and cannabis withdrawal can lead to symptoms of anxiety. Buspirone, a serotonin 1A receptor (5-HT1A) agonist, has shown limited efficacy for treating anxiety in people with cannabis use disorder, though there may be better efficacy in males than in females. Fluoxetine, a selective serotonin reuptake inhibitor, has failed to show efficacy in adolescents with both cannabis use disorder and depression.
SSRIs are a class of antidepressant drugs that are also used for the treatment of anxiety disorders, such as generalized anxiety disorder. Vilazodone, which has both SSRI and 5-HT1A agonism properties, also failed to increase abstinence rates in people with cannabis use disorder.
Studies of divalproex have found no significant benefit, though some studies have found mixed results. Baclofen, a GABA-B receptor agonist and antispasmodic medication, has been found to reduce cravings but without a significant benefit towards preventing relapse or improving sleep. Zolpidem, a GABA-A receptor agonist and "Z-hypnotic" medication, has shown some efficacy in treating insomnia due to cannabis withdrawal, though there is a potential for misuse.
Entacapone was well tolerated and decreased cannabis cravings in a trial on a small number of patients. Topiramate, an antiepileptic drug, has shown mixed results in adolescents, reducing the volume of cannabis consumption without significantly increasing abstinence, with somewhat poor tolerability. Gabapentin, an indirect GABA modulator, has shown some preliminary benefit for reducing cravings and cannabis use.
The agonist substitution approach is one that draws upon the analogy of the success of nicotine replacement therapy for nicotine addiction. Dronabinol, which is synthetic THC, has shown benefit in reducing cravings and other symptoms of withdrawal, though without preventing relapse or promoting abstinence.
Combination therapy with dronabinol and the alpha 2 adrenergic receptor agonist lofexidine have shown mixed results, with possible benefits towards reducing withdrawal symptoms. However, overall, the combination of dronabinol and lofexidine is likely not effective for the treatment of cannabis use disorder. Nabilone, a synthetic THC analogue, has shown benefits in reducing symptoms of withdrawal such as difficulty sleeping, and decreased overall cannabis use.
Despite its psychoactive effects, the slower onset of action and longer duration of action of nabilone make it less likely to be abused than cannabis itself, which makes nabilone a promising harm reduction strategy for the treatment of cannabis use disorder. The combination of nabilone and zolpidem has been shown to decrease sleep-related and mood-related symptoms of cannabis withdrawal, in addition to decreasing cannabis use.
Nabiximols, a combined THC and cannabidiol (CBD) product that is formulated as an oral (buccal) spray, has been shown to improve withdrawal symptoms without improving abstinence rates. Oral CBD has not shown efficacy in reducing the signs or symptoms of cannabis use, and likely has no benefit in cannabis use withdrawal symptoms. The CB-1 receptor antagonist rimonabant has shown efficacy in reducing the effects of cannabis in users, but with a risk for serious psychiatric side effects.
Naltrexone, a mu opioid receptor antagonist, has shown mixed results for cannabis use disorder—both increasing the subjective effects of cannabis when given acutely, but potentially decreasing the overall use of cannabis with chronic administration. N-acetylcysteine (NAC) has shown some limited benefit in decreasing cannabis use in adolescents, though not with adults. Lithium, a mood stabilizer, has shown mixed results for treating symptoms of cannabis withdrawal, but is likely ineffective.
Quetiapine, a second-generation antipsychotic, has been shown to treat cannabis withdrawal related insomnia and decreased appetite at the expense of exacerbating cravings.
Oxytocin, a neuropeptide that the body produces, has shown some benefit in reducing the use of cannabis when administered intranasally in combination with motivational enhancement therapy sessions, though the treatment effect did not persist between sessions.
Over-the-counter sedating Antihistamines such as Doxylamine have sedating and anti-emetic effects and may provide short term relief but should only be used within advised dosages.
Barriers to treatment:
Research that looks at barriers to cannabis treatment frequently cites a lack of interest in treatment, lack of motivation and knowledge of treatment facilities, an overall lack of facilities, costs associated with treatment, difficulty meeting program eligibility criteria and transport difficulties.
Epidemiology:
Cannabis is one of the most widely used drugs in the world. In the United States, between 42% and 49% of people have used cannabis, an estimated 9% of those who use cannabis develop dependence.
Of Australians aged 14 years and over 34.8% have used cannabis one or more times in their life. In the U.S., cannabis is the most commonly identified illicit substance used by people admitted to treatment facilities. Most of these people were referred there by the criminal justice system. Of admittents 16% either went on their own, or were referred by family or friends.
In the European Union (data as available in 2018, information for individual countries was collected between 2012 and 2017), 26.3% of adults aged 15–64 used cannabis at least once in their lives, and 7.2% used cannabis in the last year. The highest prevalence of cannabis use among 15 to 64 years old in the EU was reported in France, with 41.4% having used cannabis at least once in their life, and 2.17% used cannabis daily or almost daily.
Among young adults (15–34 years old), 14.1% used cannabis in the last year.
Among adolescents (15–16 years old) in a European school based study (ESPAD), 16% of students have used cannabis at least once in their life, and 7% (boys: 8%, girls: 5%) of students had used cannabis in the last 30 days.
Globally, 22.1 million people (0.3% of the worlds population) were estimated to suffer from cannabis dependence.
Research:
Medications such as SSRI antidepressants, mixed action antidepressants, bupropion, buspirone and atomoxetine may not be helpful to treat cannabis use disorder, but the evidence is very weak and further research is required. THC preparations, gabapentin, oxytocin, and N-acetylcysteine also require more research to determine if they are effective as the evidence base is weak.
Heavy cannabis use has been associated with impaired cognitive functioning, however, its specific details are difficult to elucidate due to the potential use of additional substances of users, and lack of longitudinal studies.
See also:
Signs and symptoms:
Cannabis use is associated with comorbid mental health problems, such as mood and anxiety disorders, and discontinuing cannabis use is difficult for some users. Psychiatric comorbidities are often present in dependent cannabis users including a range of personality disorders.
Based on annual survey data, some high school seniors who report smoking daily (nearly 7%, according to one study) may function at a lower rate in school than students that do not. The sedating and anxiolytic properties of tetrahydrocannabinol (THC) in some users might make the use of cannabis an attempt to self-medicate personality or psychiatric disorders.
Dependency:
Prolonged cannabis use produces both pharmacokinetic changes (how the drug is absorbed, distributed, metabolized, and excreted) and pharmacodynamic changes (how the drug interacts with target cells) to the body. These changes require the user to consume higher doses of the drug to achieve a common desirable effect (known as a higher tolerance), reinforcing the body's metabolic systems for eliminating the drug more efficiently and further down-regulating cannabinoid receptors in the brain.
Cannabis users have shown decreased reactivity to dopamine, suggesting a possible link to a dampening of the reward system of the brain and an increase in negative emotion and addiction severity.
Cannabis users can develop tolerance to the effects of THC. Tolerance to the behavioral and psychological effects of THC has been demonstrated in adolescent humans and animals. The mechanisms that create this tolerance to THC are thought to involve changes in cannabinoid receptor function.
One study has shown that between 2001–2002 and 2012–2013, the use of marijuana in the US doubled.
Cannabis dependence develops in about 9% of users, significantly less than that of heroin, cocaine, alcohol, and prescribed anxiolytics, but slightly higher than that for psilocybin, mescaline, or LSD. Of those who use cannabis daily, 10–20% develop dependence.
Withdrawal:
annabis withdrawal symptoms occur in one-half of people in treatment for cannabis use disorders. Symptoms may include any of the following:
- dysphoria (anxiety, irritability, depression, restlessness),
- disturbed sleep,
- gastrointestinal symptoms,
- and decreased appetite.
It is often paired with rhythmic movement disorder. Most symptoms begin during the first week of abstinence and resolve after a few weeks. About 12% of heavy cannabis users showed cannabis withdrawal as defined by the DSM-5, and this was associated with significant disability as well as mood, anxiety and personality disorders.
Cause:
Cannabis addiction is often due to prolonged and increasing use of the drug. Increasing the strength of the cannabis taken and an increasing use of more effective methods of delivery often increase the progression of cannabis dependency. It can also be caused by being prone to becoming addicted to substances, which can either be genetically or environmentally acquired.
Risk factors:
Certain factors are considered to heighten the risk of developing cannabis dependence and longitudinal studies over a number of years have enabled researchers to track aspects of social and psychological development concurrently with cannabis use.
Increasing evidence is being shown for the elevation of associated problems by the frequency and age at which cannabis is used, with young and frequent users being at most risk.
The main factors in Australia, for example, related to a heightened risk for developing problems with cannabis use include frequent use at a young age; personal maladjustment; emotional distress; poor parenting; school drop-out; affiliation with drug-using peers; moving away from home at an early age; daily cigarette smoking; and ready access to cannabis.
The researchers concluded there is emerging evidence that positive experiences to early cannabis use are a significant predictor of late dependence and that genetic predisposition plays a role in the development of problematic use.
High risk groups:
A number of groups have been identified as being at greater risk of developing cannabis dependence and, in Australia, for example, have been found to include adolescent populations, Aboriginal and Torres Strait Islanders and people suffering from mental health conditions.
Adolescents:
The endocannabinoid system is directly involved in adolescent brain development. Adolescent cannabis users are therefore particularly vulnerable to the potential adverse effects of cannabis use. Adolescent cannabis use is associated with increased cannabis misuse as an adult, issues with memory and concentration, long-term cognitive complications, and poor psychiatric outcomes including social anxiety, suicidality and addiction.
There are a lot of reasons why adolescents start a smoking habit. According to a study completed by Bill Sanders, friends influence, difficult household problems, and experimentation are some of the reasons why this population starts to smoke marijuana.
This segment of population seems to be one of the most influenceable group there is. They want to follow the group and look "cool", "hip" and accepted by their friends. This fear of rejection plays a big role in their decision to smoke pot. However it does not seem to be the most important factor. According to a study from Canada, the lack of knowledge about cannabis seems to be the main reason why adolescents start to smoke.
The authors observed a high correlation between adolescents that knew about the mental and physical harms of cannabis and their consumption. Of the 1045 young participants in the study, those who could name the least number of negative effects about this drug were usually the ones who were consuming it. They were not isolated cases either. Actually, the study showed that the proportion of teenagers who saw cannabis as a high-risk drug and the ones who thought the contrary was about the same.
Pregnancy:
There is an association between smoking cannabis during pregnancy and low birth weight. Smoking cannabis during pregnancy can lower the amount of oxygen delivered to the developing fetus, which can restrict fetal growth.
The active ingredient in cannabis (D9-tetrahydrocannabinol, THC) is fat soluble and can enter into breastmilk during lactation. THC in breastmilk can then subsequently be taken up by a breastfeeding infant, as shown by the presence of THC in the infant's feces. However, the evidence for long-term effects of exposure to THC through breastmilk is unclear.
Diagnosis:
Cannabis use disorder is recognized in the fifth version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which also added cannabis withdrawal as a new condition.
In the 2013 revision for the DSM-5, DSM-IV abuse and dependence were combined into cannabis use disorder. The legal problems criterion (from cannabis abuse) has been removed, and the craving criterion was newly added, resulting in a total of eleven criteria: hazardous use, social/interpersonal problems, neglected major roles, withdrawal, tolerance, used larger amounts/longer, repeated attempts to quit/control use, much time spent using, physical/psychological problems related to use, activities given up and craving.
For a diagnosis of DSM-5 cannabis use disorder, at least two of these criteria need to be present in the last twelve-month period. Additionally, three severity levels have been defined: mild (two or three criteria), moderate (four or five criteria) and severe (six or more criteria) cannabis use disorder.
Cannabis use disorder is also recognized in the eleventh revision of the International Classification of Diseases (ICD-11), adding more subdivisions including time intervals of pattern of use (episodic, continuous, or unspecified) and dependence (current, early full remission, sustained partial remission, sustained full remission, or unspecified) compared to the 10th revision.
A 2019 meta-analysis found that 34% of people with cannabis-induced psychosis transitioned to schizophrenia. This was found to be comparatively higher than hallucinogens (26%) and amphetamines (22%).
To screen for cannabis-related problems, several methods are used. Scales specific to cannabis, which provides the benefit of being cost efficient compared to extensive diagnostic interviews, include the Cannabis Abuse Screening Test (CAST), Cannabis Use Identification Test (CUDIT), and Cannabis Use Problems Identification Test (CUPIT). Scales for general drug use disorders are also used, including the Severity Dependence Scale (SDS), Drug Use Disorder Identification Test (DUDIT), and Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST).
However, there are no gold standard and both older and newer scales are still in use.[43] To quantify cannabis use, methods such as Timeline Follow-Back (TLFB) and Cannabis Use Daily (CUD) are used. These methods measure general consumption and not grams of psychoactive substance as the concentration of THC may vary among drug users.
Treatment:
Clinicians differentiate between casual users who have difficulty with drug screens, and daily heavy users, to a chronic user who uses multiple times a day. In the US, as of 2013, cannabis is the most commonly identified illicit substance used by people admitted to treatment facilities.
Demand for treatment for cannabis use disorder increased internationally between 1995 and 2002. In the United States, the average adult who seeks treatment has consumed cannabis for over 10 years almost daily and has attempted to quit six or more times.
Treatment options for cannabis dependence are far fewer than for opiate or alcohol dependence. Most treatment falls into the categories of psychological or psychotherapeutic, intervention, pharmacological intervention or treatment through peer support and environmental approaches.
No medications have been found effective for cannabis dependence, but psychotherapeutic models hold promise. Screening and brief intervention sessions can be given in a variety of settings, particularly at doctor's offices, which is of importance as most cannabis users seeking help will do so from their general practitioner rather than a drug treatment service agency.
The most commonly accessed forms of treatment in Australia are 12-step programmes, physicians, rehabilitation programs, and detox services, with inpatient and outpatient services equally accessed. In the EU approximately 20% of all primary admissions and 29% of all new drug clients in 2005, had primary cannabis problems. And in all countries that reported data between 1999 and 2005 the number of people seeking treatment for cannabis use increased.
Psychological:
Psychological intervention includes cognitive behavioral therapy (CBT), motivational enhancement therapy (MET), contingency management (CM), supportive-expressive psychotherapy (SEP), family and systems interventions, and twelve-step programs.
Evaluations of Marijuana Anonymous programs, modelled on the 12-step lines of Alcoholics Anonymous and Narcotics Anonymous, have shown small beneficial effects for general drug use reduction. In 2006, the Wisconsin Initiative to Promote Healthy Lifestyles implemented a program that helps primary care physicians identify and address marijuana use problems in patients.
Medication:
As of 2020, there is no single medication that has been proven effective for treating cannabis use disorder; research is focused on three treatment approaches: agonist substitution, antagonist, and modulation of other neurotransmitter systems. More broadly, the goal of medication therapy for cannabis use disorder centers around targeting the stages of the addiction: acute intoxication/binge, withdrawal/negative affect, and preoccupation/anticipation.
For the treatment of the withdrawal/negative affect symptom domain of cannabis use disorder, medications may work by alleviating restlessness, irritable or depressed mood, anxiety, and insomnia. Bupropion, which is a norepinephrine–dopamine reuptake inhibitor, has been studied for the treatment of withdrawal with largely poor results. Atomoxetine has also shown poor results, and is as a norepinephrine reuptake inhibitor, though it does increase the release of dopamine through downstream effects in the prefrontal cortex (an area of the brain responsible for planning complex tasks and behavior).
Venlafaxine, a serotonin–norepinephrine reuptake inhibitor, has also been studied for cannabis use disorder, with the thought that the serotonergic component may be useful for the depressed mood or anxious dimensions of the withdrawal symptom domain. While venlafaxine has been shown to improve mood for people with cannabis use disorder, a clinical trial in this population actually found worse cannabis abstinence rates compared to placebo.
It is worth noting that venlafaxine is sometimes poorly tolerated, and infrequent use or abrupt discontinuation of its use can lead to withdrawal symptoms from the medication itself, including irritability, dysphoria, and insomnia. It is possible that venlafaxine use actually exacerbated cannabis withdrawal symptoms, leading people to use more cannabis than placebo to alleviate their discomfort. Mirtazapine, which increases serotonin and norepinephrine, has also failed to improve abstinence rates in people with cannabis use disorder.
People sometimes use cannabis to cope with their anxiety, and cannabis withdrawal can lead to symptoms of anxiety. Buspirone, a serotonin 1A receptor (5-HT1A) agonist, has shown limited efficacy for treating anxiety in people with cannabis use disorder, though there may be better efficacy in males than in females. Fluoxetine, a selective serotonin reuptake inhibitor, has failed to show efficacy in adolescents with both cannabis use disorder and depression.
SSRIs are a class of antidepressant drugs that are also used for the treatment of anxiety disorders, such as generalized anxiety disorder. Vilazodone, which has both SSRI and 5-HT1A agonism properties, also failed to increase abstinence rates in people with cannabis use disorder.
Studies of divalproex have found no significant benefit, though some studies have found mixed results. Baclofen, a GABA-B receptor agonist and antispasmodic medication, has been found to reduce cravings but without a significant benefit towards preventing relapse or improving sleep. Zolpidem, a GABA-A receptor agonist and "Z-hypnotic" medication, has shown some efficacy in treating insomnia due to cannabis withdrawal, though there is a potential for misuse.
Entacapone was well tolerated and decreased cannabis cravings in a trial on a small number of patients. Topiramate, an antiepileptic drug, has shown mixed results in adolescents, reducing the volume of cannabis consumption without significantly increasing abstinence, with somewhat poor tolerability. Gabapentin, an indirect GABA modulator, has shown some preliminary benefit for reducing cravings and cannabis use.
The agonist substitution approach is one that draws upon the analogy of the success of nicotine replacement therapy for nicotine addiction. Dronabinol, which is synthetic THC, has shown benefit in reducing cravings and other symptoms of withdrawal, though without preventing relapse or promoting abstinence.
Combination therapy with dronabinol and the alpha 2 adrenergic receptor agonist lofexidine have shown mixed results, with possible benefits towards reducing withdrawal symptoms. However, overall, the combination of dronabinol and lofexidine is likely not effective for the treatment of cannabis use disorder. Nabilone, a synthetic THC analogue, has shown benefits in reducing symptoms of withdrawal such as difficulty sleeping, and decreased overall cannabis use.
Despite its psychoactive effects, the slower onset of action and longer duration of action of nabilone make it less likely to be abused than cannabis itself, which makes nabilone a promising harm reduction strategy for the treatment of cannabis use disorder. The combination of nabilone and zolpidem has been shown to decrease sleep-related and mood-related symptoms of cannabis withdrawal, in addition to decreasing cannabis use.
Nabiximols, a combined THC and cannabidiol (CBD) product that is formulated as an oral (buccal) spray, has been shown to improve withdrawal symptoms without improving abstinence rates. Oral CBD has not shown efficacy in reducing the signs or symptoms of cannabis use, and likely has no benefit in cannabis use withdrawal symptoms. The CB-1 receptor antagonist rimonabant has shown efficacy in reducing the effects of cannabis in users, but with a risk for serious psychiatric side effects.
Naltrexone, a mu opioid receptor antagonist, has shown mixed results for cannabis use disorder—both increasing the subjective effects of cannabis when given acutely, but potentially decreasing the overall use of cannabis with chronic administration. N-acetylcysteine (NAC) has shown some limited benefit in decreasing cannabis use in adolescents, though not with adults. Lithium, a mood stabilizer, has shown mixed results for treating symptoms of cannabis withdrawal, but is likely ineffective.
Quetiapine, a second-generation antipsychotic, has been shown to treat cannabis withdrawal related insomnia and decreased appetite at the expense of exacerbating cravings.
Oxytocin, a neuropeptide that the body produces, has shown some benefit in reducing the use of cannabis when administered intranasally in combination with motivational enhancement therapy sessions, though the treatment effect did not persist between sessions.
Over-the-counter sedating Antihistamines such as Doxylamine have sedating and anti-emetic effects and may provide short term relief but should only be used within advised dosages.
Barriers to treatment:
Research that looks at barriers to cannabis treatment frequently cites a lack of interest in treatment, lack of motivation and knowledge of treatment facilities, an overall lack of facilities, costs associated with treatment, difficulty meeting program eligibility criteria and transport difficulties.
Epidemiology:
Cannabis is one of the most widely used drugs in the world. In the United States, between 42% and 49% of people have used cannabis, an estimated 9% of those who use cannabis develop dependence.
Of Australians aged 14 years and over 34.8% have used cannabis one or more times in their life. In the U.S., cannabis is the most commonly identified illicit substance used by people admitted to treatment facilities. Most of these people were referred there by the criminal justice system. Of admittents 16% either went on their own, or were referred by family or friends.
In the European Union (data as available in 2018, information for individual countries was collected between 2012 and 2017), 26.3% of adults aged 15–64 used cannabis at least once in their lives, and 7.2% used cannabis in the last year. The highest prevalence of cannabis use among 15 to 64 years old in the EU was reported in France, with 41.4% having used cannabis at least once in their life, and 2.17% used cannabis daily or almost daily.
Among young adults (15–34 years old), 14.1% used cannabis in the last year.
Among adolescents (15–16 years old) in a European school based study (ESPAD), 16% of students have used cannabis at least once in their life, and 7% (boys: 8%, girls: 5%) of students had used cannabis in the last 30 days.
Globally, 22.1 million people (0.3% of the worlds population) were estimated to suffer from cannabis dependence.
Research:
Medications such as SSRI antidepressants, mixed action antidepressants, bupropion, buspirone and atomoxetine may not be helpful to treat cannabis use disorder, but the evidence is very weak and further research is required. THC preparations, gabapentin, oxytocin, and N-acetylcysteine also require more research to determine if they are effective as the evidence base is weak.
Heavy cannabis use has been associated with impaired cognitive functioning, however, its specific details are difficult to elucidate due to the potential use of additional substances of users, and lack of longitudinal studies.
See also:
- La Guardia Committee, the first in-depth study into the effects of cannabis.
- Medical cannabis
Video Game Addiction
- YouTube Video: Am I Addicted to Video Games? 9 Warning Signs
- YouTube Video: How To Overcome Video Game Addiction
- YouTube Video: Your brain on video games | Daphne Bavelier TED.x
Video game addiction, also known as gaming disorder or internet gaming disorder, is generally defined as the problematic, compulsive use of video games that results in significant impairment to an individual's ability to function in various life domains over a prolonged period of time.
This and associated concepts have been the subject of considerable research, debate, and discussion among experts in several disciplines and has generated controversy within the medical, scientific, and gaming communities. Such disorders can be diagnosed when an individual engages in gaming activities at the cost of fulfilling daily responsibilities or pursuing other interests without regard for the negative consequences. As defined by the ICD-11, the main criterion for this disorder is a lack of self control over gaming.
The World Health Organization included gaming disorder in the 11th revision of its International Classification of Diseases (ICD). The American Psychiatric Association (APA), while stating there is insufficient evidence for the inclusion of Internet gaming disorder in the Diagnostic and Statistical Manual of Mental Disorders in 2013, considered it worthy of further study.
Controversy around the diagnosis includes whether the disorder is a separate clinical entity or a manifestation of underlying psychiatric disorders. Research has approached the question from a variety of viewpoints, with no universally standardized or agreed definitions, leading to difficulties in developing evidence-based recommendations.
Definition and diagnosis:
In its report, the Council on Science and Public Health to the American Medical Association (AMA) used this two-hour-per-day limit to define "gaming overuse", citing the American Academy of Pediatrics guideline of no more than one to two hours per day of "screen time". However, the ESA document cited in the Council report does not contain the two-hour-per-day data.
American Psychiatric Association:
While the American Psychiatric Association (APA) does not recognize video game addiction as a disorder, in light of existing evidence, the organisation included video game addiction as a "condition requiring further study" in the DSM-5 as Internet gaming disorder. Video game addiction is a broader concept than internet gaming addiction, but most video game addiction is associated with internet gaming.
APA suggests, like Khan, the effects (or symptoms) of video game addiction may be similar to those of other proposed psychological addictions. Video game addiction may be an impulse control disorder, similar to compulsive gambling The APA explains why Internet Gaming Disorder has been proposed as a disorder:
This decision was based upon the large number of studies of this condition and the severity of its consequences. ... Because of the distinguishing features and increased risks of clinically significant problems associated with gaming in particular, the Workgroup recommended the inclusion of only internet gaming disorder in Section 3 of the DSM-5.
Some players become more concerned with their interactions in the game than in their broader lives. Players may play many hours per day, neglect personal hygiene, gain or lose significant weight, disrupt sleep patterns resulting in sleep deprivation, play at work, avoid phone calls from friends, or lie about how much time they spend playing video games.
The APA has developed nine criteria for characterising the proposed Internet Gaming Disorder:
One of the most commonly used instruments for the measurement of addiction, the PVP Questionnaire (Problem Video Game Playing Questionnaire), was presented as a quantitative measure, not as a diagnostic tool. According to Griffiths, "all addictions (whether chemical or behavioral) are essentially about constant rewards and reinforcement". He proposes that addiction has six components: salience, mood modification, tolerance, withdrawal, conflict, and relapse.
But the APA's nine criteria for diagnosing Internet Gaming Disorder were made by taking point of departure in eight different diagnostic/measuring tools proposed in other studies. Thus, the APA's criteria attempt to condense the scientific work on diagnosing Internet Gaming Disorder.
World Health Organization:
The World Health Organization (WHO) had proposed and later included "gaming disorder" in the 11th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-11), released in June 2018, which was approved by the World Health Assembly in May 2019. the use and enforcement of ICD-11 is expected to start on 1 January 2022.
Screening tools:
The first psychometric test to assess IGD was the Internet Gaming Disorder Test (IGD-20). This test includes 20 questions designed to assess the extent of problems caused by disordered gaming and the degree of symptoms experienced by gamers. The test was first published in a journal article published in the PLoS ONE journal on 14 October 2014.
The Internet Gaming Disorder Scale–Short-Form (IGDS9-SF)[ is a short psychometric test to assess video game addiction according to the American Psychiatric Association framework for IGD. Recent review studies suggest that the IGDS9-SF presents with robust empirical and clinical evidence and is an effective tool to assess IGD. Moreover, the scale was adapted in several languages as Spanish, Chinese, Czech, German, and so many more.
On 3 June 2019, a screening tool for Gaming Disorder, specifically as defined by the World Health Organization, called the "Gaming Disorder Test" was published in a journal article.[4]
Risk factors:
The Internet can foster various addictions including addiction to gameplaying.
Addictive playing of MMORPGs is associated with negative effects, whereas normal play is not.
Younger people and men are more likely to experience a gaming disorder than older people and women respectively. Adolescents are at a higher risk of sustaining video game disorder over time than adults.
An international meta-analysis over 34 jurisdictions quantified the effect size of gender as small, with most effect in Asia, lesser in Europe and Africa, and null in North America, and further finding that economic factors, internet availability, social norms and addiction-related health factors mediate the effect of gender, with nations with a greater GDP per capita having less differences in video game addiction between genders.
Comorbid psychiatric disorders act as both risk factors and consequences. Indeed, there is a strong association between video game addiction and anxiety, depression, ADHD, social phobia, and poor psycho-social support. ADHD and its symptoms, such as impulsivity and conduct problems, also increase risks of developing video game disorder.
Although internet gaming disorder has a strong relationship with obsessive-compulsive disorder, it is not specific and internet gaming disorder is both phenomenologically and neurobiologically distinct, which indicates that internet gaming disorder is more characterized by impulsivity than compulsivity. Familial factors appear to play an important role, although not well understood.
Some personality traits, such as high neuroticism, high impulsivity, and high aggressiveness are consistently significant predictors of internet gaming disorder, and combination of personality traits seem to play a pivotal role in the acquisition, maintenance and development of the disorder.
Mechanisms:
Although there is much research since the 1980s on problematic online gaming use, the mechanisms are not well understood, due to inconsistent definitions used in studies.
Video game structure:
Some theories focus on the presumed built-in reward systems of video games, such as compulsion loops, to explain their potentially addictive nature. The anticipation of such rewards can create a neurological reaction that releases dopamine into the body, so that once the reward is obtained, the person will remember it as a pleasurable feeling. This has been found to be similar to the neurological reaction of other behavioral addictions such as substance abuse and gambling disorder, although not to the same magnitude and with some differences.
Mark Griffiths has proposed another reason online video games are potentially addictive is because they "can be played all day every day." The fact there is no end to the game can feel rewarding for some, and hence players are further engaged in the game.
Addiction circuits in the brain:
Long-term internet video/mobile game playing affects brain regions responsible for reward, impulse control and sensory-motor coordination. Structural analyses shown modifications in the volume of the ventral striatum, possibly as result of changes in rewards, and video game addicts had faulty inhibitory control and reward mechanisms.
Video game playing is associated with dopamine release similar in magnitude to that of drug abuse, and the presentation of gaming pictures activates brain regions similarly to drug pictures for drug addicts. Treatment studies which used fMRI to monitor the brain connectivity changes found a decrease in the activity of the regions associated with cravings.
Although there are evidences that video game addiction may be supported by similar neural mechanisms underlying drug abuse, as video game and internet addictions reduce the sensitivity of the dopaminergic reward system, it is still premature to conclude that this addiction is equivalent to substance addictions, as the research is in its early stages.
There is evidence of a dual processing model of digital technology addictions characterized by an imbalance between the reactive and the reflective reward systems. Other studies shown increased difficulties in decision making in specific contexts, such as risky situations but not in ambiguous situations, and an increased preference for short-term rewards.
Although the number of neuroimaging studies on internet gaming disorder is rising, there are several methodological shortcomings, particularly in the inconsistency of psychometric assessments. Furthermore, the conclusions on reduced inhibition should be moderated, as only one study included a functional control, which then showed no difference in inhibition.
A meta-analytic review of the research concluded the evidence suggests video game addiction arises out of other mental health problems, rather than causing them. Thus it is unclear whether video game addiction should be considered a unique diagnosis.
Management:
As concern over video game addiction grows, the use of psychopharmacology, psychotherapy, twelve-step programs, and use of continuing developing treatment enhancements have been proposed to treat this disorder. Empirical studies indeed indicate that internet gaming disorder is associated with detrimental health-related outcomes.
However, the clinical trials of potential treatments remain of low quality, except for cognitive-behavioral therapies, which shows efficacy to reduce gaming disorder and depressive symptoms but not total time spent.
Although there is a scientific consensus that cognitive-behavioral therapy is preferable to pharmacological treatment, it remains difficult to make definitive statements about its benefits and efficiency due to methodological inconsistencies and lack of follow-up.
Since efficacious treatments have not been well established, prevention of video gaming disorder is crucial. Some evidence suggest that up to 50% of people affected by the internet gaming disorder may recover naturally.
Some countries, such as South Korea, China, the Netherlands, Canada, and the United States, have responded to the perceived threat of video game addiction by opening treatment centers.
Outcomes:
Mental health:
Internet gaming disorder is associated with increased anxiety, social phobia and depression, with adults and young adults being more affected than adolescents.
Physical health:
The most frequent physical health-related outcome are alterations in physical functioning such as somatisation and sleep disturbances. Preliminary evidence suggest that internet gaming disorder and the induced sedentarity may contribute to a lack of physical exercise, even though the relationship is not causal.
Epidemiology:
The prevalence of internet gaming disorder range from 0.7% to 25.5% worldwide, or 1.0% to 26.8% worldwide, and 3.5% to 17% in China, and is higher among males than females and among younger than older people, with geographical region being an insignificant contributor.
A longer time spent on video games predicts a tendency towards pathological gaming in the future. The studies, however, used various methodologies and definitions, which renders consensus difficult to achieve and may explain the wide range of prevalence.
Research:
Debates on the classification:
A meta-analytic review of pathological gaming studies concluded that about 3% of gamers may experience some symptoms of pathological gaming. The report noted problems in the field with defining and measuring pathological gaming and concluded that pathological gaming behaviors were more likely the product of underlying mental health problems rather than the inverse.
Barnett and Coulson expressed concern that much of the debate on the issue of addiction may be a knee jerk response stimulated by poor understanding of games and game players.
Such issues may lead both society and scholars to exaggerate the prevalence and nature of problematic gaming, and over-focus on games specifically, while ignoring underlying mental health issues.
Other scholars have cautioned that comparing the symptoms of problematic gaming with problematic gambling is flawed, and that such comparisons may introduce research artifacts and artificially inflate prevalence estimates.
For instance, Richard Wood has observed that behaviors which are problematic in regards to gambling may not be as problematic when put into the context of other behaviors that are rewarding such as gaming. Similarly, Barnett and Coulson have cautioned that discussions of problematic gaming have moved forward prematurely without proper understanding of the symptoms, proper assessment and consequences.
Rather than video gaming disorder being a subtype of gambling disorder, a majority of researchers support the idea of video game addiction being a part of a more comprehensive framework of impulse control disorders with "pathological technology use" with similar characteristics, including the pathological use of video games, internet, computers and other interactive medias.
Although internet and video game addictions are generally considered different from gambling disorder and substance abuse, there is a growing body of evidence indicating they share common features, including behavioral and neural features. Indeed, it is suggested that while behavioral addiction may differ with drug addictions in magnitude, they share several characteristics, with Hellman et al. proposing that the concept of addiction should be de-medicalized.
On the contrary, a literature review found that as the video game addiction develops, online gaming addicts spend increasing amounts of time not only playing but also preparing for and organizing their playing sessions, suggesting this addiction may be behavioral rather than a disorder of impulse control. There is recent evidence suggesting that internet gaming disorder can cause two distinct types of dysfunctions: cognitive and metacognitive.
Griffiths has suggested that psycho-social dependence may revolve around the intermittent reinforcements in the game and the need to belong. Hagedorn & Young have suggested that social dependence may arise due to video games occurring online where players interact with others and the relationships "often become more important for gamers than real-life relationships".
Controversy and alternative viewpoints:
Common challenges involve the reliability of the methodology and validity of the results in some studies. Many rely on self-surveys from university students and also lack time frames making it difficult to study the impact, if any, of addiction on a long term scale. Other concerns also address the definition of addiction and how to measure it, questioning whether or not time is a proper unit to determine how addicted someone is to gaming.
Daria Joanna Kuss and Mark D. Griffiths have argued the current scientific knowledge on internet gaming addiction is copious in scope and complexity. They state that instead, a simple framework should be provided to allow all current and future studies to be categorized, as internet gaming addiction lies on a continuum beginning with etiology and risk factors all the way through the development of "full-blown" addiction and ending with ramifications and potential treatment.
In addition, they caution the deployment of the label "addiction" since it heavily denotes the use of substances or engagement in certain behaviors. Finally, the researcher promotes other researchers to assess the validity and reliability of existing measures instead of developing additional measurement instruments.
Other challenges include the lack of context of the participant's life and the negative portrayal of gaming addicts. Some state that gamers sometimes use video games to either escape from an uncomfortable environment or alleviate their already existing mental issues—both possibly important aspects in determining the psychological impact of gaming.
Negative portrayal also deals with the lack of consistency in measuring addictive gaming. This leads to discussions that sometimes exaggerate the issue and create a misconception in some that they, themselves, may be addicted when they are not.
The evidence of video game addiction to create withdrawal symptoms is very limited and thus debated, due to different definitions and low quality trials.
The concept of video game disorder is itself being debated, with the overlap of its symptoms with other mental disorders, the unclear consensus on a definition and thresholds, and the lack of evidence raising doubts on whether or not this qualifies as a mental disorder of its own.
Despite the lack of a unified definition, there is an emerging consensus among studies that Internet gaming disorder is mainly defined by three features: 1) withdrawal, 2) loss of control, and 3) conflict. Although the DSM-5 definition of video game disorder has a good fit to current methodological definitions used in trials and studies, there are still debates on the clinical pertinence.
Michael Brody, M.D., head of the TV and Media Committee of the American Academy of Child and Adolescent Psychiatry, stated in a 2007 press release that "... there is not enough research on whether or not video games are addictive." However, Brody also cautioned that for some children and adolescents, "... it displaces physical activity and time spent on studies, with friends, and even with family."
A major issue concerns the lack of consistent measures and definitions and of acquisition of follow-up data. Furthermore, the study design quality has not greatly improved between the 2000s and 2017.
For instance, most studies measured internet gaming behaviors in terms of frequency of use (total time spent), without considering the type of game (e.g., MMORPG), the social context (e.g., physically or virtually with friends), nor the motivations (e.g., competitive, achievement-oriented "grinding").
Although the amount of time spent was postulated by Johanssonn and Götestam in 2004 to lead to pathological behaviors, it is unclear whether the time spent is a cause or a consequence of pathological use. These criticisms, however, mostly pertain to Western research since there is more data of higher quality available in Asian regions, where the Internet gaming disorder is more prevalent.
A survey conducted in 2019 of 214 scholars shown that 60.8% agreed that pathological video game use could be a mental health problems, whereas 30.4% were skeptical. However, only 49.7% agreed with the DSM-5 definition of Internet gaming disorder, and 56.5% to the definition of the World Health Organization.
Most scholars were worried that WHO's and DSM-5's inclusion of Internet gaming disorder was "over-pathologizing normal youth" and "precipitated moral panic over video games". This indicates a lack of consensus on the issue as of 2019.
Society and culture:
Parental concerns:
According to ABC News, parents have many concerns about their children playing video games, including concerns about age appropriateness, the amount of time spent playing games, physical health, and aggressive behavior.
Governmental concerns:
The first video game to attract political controversy was the 1978 arcade game Space Invaders. In 1981, a political bill called the Control of Space Invaders (and other Electronic Games) Bill was drafted by British Labour Party MP George Foulkes in an attempt to ban the game for its "addictive properties" and for causing "deviancy". The bill was debated and only narrowly defeated in parliament by 114 votes to 94 votes.
In August 2005, the government of the People's Republic of China, where more than 20 million people play online games, introduced an online gaming restriction limiting playing time to three hours, after which the player would be expelled from whichever game they were playing.
In 2006, it relaxed the rule so only citizens under the age of 18 would face the limitation. Reports indicate underage gamers found ways to circumvent the measure. In July 2007, the rule was relaxed yet again. Internet games operating in China must require users identify themselves by resident identity numbers.
After three hours, players under 18 are prompted to stop and "do suitable physical exercise". If they continue, their in-game points are "slashed in half". After five hours, all their points are automatically erased.
In 2008, one of the five Federal Communications Commission (FCC) Commissioners, Deborah Taylor Tate, stated that online gaming addiction was "one of the top reasons for college drop-outs". However, she did not mention a source for the statement nor identify its position in relation to other top reasons.
In 2011, the South Korean government implemented a law, known as the Shutdown law or the Cinderella Law, which prohibits children under the age of 16 from playing online video games between the hours of 12:00 a.m. to 6:00 a.m. However, as of 2014, the law was amended and now children under the age of 16 can play after midnight if they have permission from their parents.
A systematic review identified in 2017 three types of currently attempted governmental policies: 1) limiting the availability of video games (shutdown, fatigue system, parental controls), 2) reduce the risks and harm (warning messages), 3) provide addiction help services to gamers.
Most of these policies were either not as efficient as intended or not yet evaluated for efficiency, which lead some researchers to prompt for a global public health approach to prevent the onset and progression of this disorder. Some researchers suggest that the video game industry should itself place preventive measures against video game addiction.
Deaths:
There have been at least a few deaths caused directly by exhaustion from playing games for excessive periods of time.
China:
In 2005, thirteen-year-old Zhang XiaoYi committed suicide by jumping from the top of a 24-story tower block in his home province Tianjin. After previously having spent two straight days playing online role-playing games in an Internet cafe, Zhang had told his parents that he had "been poisoned by games and could no longer control himself".
The head of a software association said to gaming website Play.tm that same year: "In the hypothetical world created by such games, [players] become confident and gain satisfaction, which they cannot get in the real world."
In 2007, a 26-year-old man identified only as "Zhang" died of a heart attack due to lack of physical activity following a seven-day gaming binge, while a 30-year-old man died in a Guangzhou Internet cafe after playing online games for three straight days.
South Korea:
In 2005, 28-year old industrial repairman Seungseob Lee (Hangul: 이승섭) visited an Internet cafe in the city of Daegu and played StarCraft almost continuously for fifty hours. He went into cardiac arrest and died at a local hospital. A friend reported: "... he was a game addict. We all knew about it. He couldn't stop himself." About six weeks before his death, his girlfriend, also an avid gamer, broke up with him. In addition, he was fired from his job.
In 2009, Kim Sa-rang, a 3-month-old Korean girl, starved to death after both her parents spent hours each day in an Internet cafe, rearing a virtual child in an online game, Prius Online. The death is covered in the 2014 documentary Love Child.
United States:
In November 2001, Shawn Woolley committed suicide; it has been inferred that his death was related to the popular computer game EverQuest. Shawn's mother said the suicide was due to a rejection or betrayal in the game from a character Shawn called "iluvyou".
Ohio teenager Daniel Petric shot his parents, killing his mother, after they took away his copy of Halo 3 in October 2007. In a sentencing hearing after the teen was found guilty of aggravated murder, the judge said, "I firmly believe that Daniel Petric had no idea at the time he hatched this plot that if he killed his parents they would be dead forever."
On 16 June 2009, Petric was sentenced to 23 years to life in prison.
Click on any of the following blue hyperlinks for more about Video Game Addictions:
This and associated concepts have been the subject of considerable research, debate, and discussion among experts in several disciplines and has generated controversy within the medical, scientific, and gaming communities. Such disorders can be diagnosed when an individual engages in gaming activities at the cost of fulfilling daily responsibilities or pursuing other interests without regard for the negative consequences. As defined by the ICD-11, the main criterion for this disorder is a lack of self control over gaming.
The World Health Organization included gaming disorder in the 11th revision of its International Classification of Diseases (ICD). The American Psychiatric Association (APA), while stating there is insufficient evidence for the inclusion of Internet gaming disorder in the Diagnostic and Statistical Manual of Mental Disorders in 2013, considered it worthy of further study.
Controversy around the diagnosis includes whether the disorder is a separate clinical entity or a manifestation of underlying psychiatric disorders. Research has approached the question from a variety of viewpoints, with no universally standardized or agreed definitions, leading to difficulties in developing evidence-based recommendations.
Definition and diagnosis:
In its report, the Council on Science and Public Health to the American Medical Association (AMA) used this two-hour-per-day limit to define "gaming overuse", citing the American Academy of Pediatrics guideline of no more than one to two hours per day of "screen time". However, the ESA document cited in the Council report does not contain the two-hour-per-day data.
American Psychiatric Association:
While the American Psychiatric Association (APA) does not recognize video game addiction as a disorder, in light of existing evidence, the organisation included video game addiction as a "condition requiring further study" in the DSM-5 as Internet gaming disorder. Video game addiction is a broader concept than internet gaming addiction, but most video game addiction is associated with internet gaming.
APA suggests, like Khan, the effects (or symptoms) of video game addiction may be similar to those of other proposed psychological addictions. Video game addiction may be an impulse control disorder, similar to compulsive gambling The APA explains why Internet Gaming Disorder has been proposed as a disorder:
This decision was based upon the large number of studies of this condition and the severity of its consequences. ... Because of the distinguishing features and increased risks of clinically significant problems associated with gaming in particular, the Workgroup recommended the inclusion of only internet gaming disorder in Section 3 of the DSM-5.
Some players become more concerned with their interactions in the game than in their broader lives. Players may play many hours per day, neglect personal hygiene, gain or lose significant weight, disrupt sleep patterns resulting in sleep deprivation, play at work, avoid phone calls from friends, or lie about how much time they spend playing video games.
The APA has developed nine criteria for characterising the proposed Internet Gaming Disorder:
- Pre-occupation. Do you spend a lot of time thinking about games even when you are not playing, or planning when you can play next?
- Withdrawal. Do you feel restless, irritable, moody, angry, anxious or sad when attempting to cut down or stop gaming, or when you are unable to play?
- Tolerance. Do you feel the need to play for increasing amounts of time, play more exciting games, or use more powerful equipment to get the same amount of excitement you used to get?
- Reduce/stop. Do you feel that you should play less, but are unable to cut back on the amount of time you spend playing games?
- Give up other activities. Do you lose interest in or reduce participation in other recreational activities due to gaming?
- Continue despite problems. Do you continue to play games even though you are aware of negative consequences, such as not getting enough sleep, being late to school/work, spending too much money, having arguments with others, or neglecting important duties?
- Deceive/cover up. Do you lie to family, friends or others about how much you game, or try to keep your family or friends from knowing how much you game?
- Escape adverse moods. Do you game to escape from or forget about personal problems, or to relieve uncomfortable feelings such as guilt, anxiety, helplessness or depression?
- Risk/lose relationships/opportunities. Do you risk or lose significant relationships, or job, educational or career opportunities because of gaming?
One of the most commonly used instruments for the measurement of addiction, the PVP Questionnaire (Problem Video Game Playing Questionnaire), was presented as a quantitative measure, not as a diagnostic tool. According to Griffiths, "all addictions (whether chemical or behavioral) are essentially about constant rewards and reinforcement". He proposes that addiction has six components: salience, mood modification, tolerance, withdrawal, conflict, and relapse.
But the APA's nine criteria for diagnosing Internet Gaming Disorder were made by taking point of departure in eight different diagnostic/measuring tools proposed in other studies. Thus, the APA's criteria attempt to condense the scientific work on diagnosing Internet Gaming Disorder.
World Health Organization:
The World Health Organization (WHO) had proposed and later included "gaming disorder" in the 11th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-11), released in June 2018, which was approved by the World Health Assembly in May 2019. the use and enforcement of ICD-11 is expected to start on 1 January 2022.
Screening tools:
The first psychometric test to assess IGD was the Internet Gaming Disorder Test (IGD-20). This test includes 20 questions designed to assess the extent of problems caused by disordered gaming and the degree of symptoms experienced by gamers. The test was first published in a journal article published in the PLoS ONE journal on 14 October 2014.
The Internet Gaming Disorder Scale–Short-Form (IGDS9-SF)[ is a short psychometric test to assess video game addiction according to the American Psychiatric Association framework for IGD. Recent review studies suggest that the IGDS9-SF presents with robust empirical and clinical evidence and is an effective tool to assess IGD. Moreover, the scale was adapted in several languages as Spanish, Chinese, Czech, German, and so many more.
On 3 June 2019, a screening tool for Gaming Disorder, specifically as defined by the World Health Organization, called the "Gaming Disorder Test" was published in a journal article.[4]
Risk factors:
The Internet can foster various addictions including addiction to gameplaying.
Addictive playing of MMORPGs is associated with negative effects, whereas normal play is not.
Younger people and men are more likely to experience a gaming disorder than older people and women respectively. Adolescents are at a higher risk of sustaining video game disorder over time than adults.
An international meta-analysis over 34 jurisdictions quantified the effect size of gender as small, with most effect in Asia, lesser in Europe and Africa, and null in North America, and further finding that economic factors, internet availability, social norms and addiction-related health factors mediate the effect of gender, with nations with a greater GDP per capita having less differences in video game addiction between genders.
Comorbid psychiatric disorders act as both risk factors and consequences. Indeed, there is a strong association between video game addiction and anxiety, depression, ADHD, social phobia, and poor psycho-social support. ADHD and its symptoms, such as impulsivity and conduct problems, also increase risks of developing video game disorder.
Although internet gaming disorder has a strong relationship with obsessive-compulsive disorder, it is not specific and internet gaming disorder is both phenomenologically and neurobiologically distinct, which indicates that internet gaming disorder is more characterized by impulsivity than compulsivity. Familial factors appear to play an important role, although not well understood.
Some personality traits, such as high neuroticism, high impulsivity, and high aggressiveness are consistently significant predictors of internet gaming disorder, and combination of personality traits seem to play a pivotal role in the acquisition, maintenance and development of the disorder.
Mechanisms:
Although there is much research since the 1980s on problematic online gaming use, the mechanisms are not well understood, due to inconsistent definitions used in studies.
Video game structure:
Some theories focus on the presumed built-in reward systems of video games, such as compulsion loops, to explain their potentially addictive nature. The anticipation of such rewards can create a neurological reaction that releases dopamine into the body, so that once the reward is obtained, the person will remember it as a pleasurable feeling. This has been found to be similar to the neurological reaction of other behavioral addictions such as substance abuse and gambling disorder, although not to the same magnitude and with some differences.
Mark Griffiths has proposed another reason online video games are potentially addictive is because they "can be played all day every day." The fact there is no end to the game can feel rewarding for some, and hence players are further engaged in the game.
Addiction circuits in the brain:
Long-term internet video/mobile game playing affects brain regions responsible for reward, impulse control and sensory-motor coordination. Structural analyses shown modifications in the volume of the ventral striatum, possibly as result of changes in rewards, and video game addicts had faulty inhibitory control and reward mechanisms.
Video game playing is associated with dopamine release similar in magnitude to that of drug abuse, and the presentation of gaming pictures activates brain regions similarly to drug pictures for drug addicts. Treatment studies which used fMRI to monitor the brain connectivity changes found a decrease in the activity of the regions associated with cravings.
Although there are evidences that video game addiction may be supported by similar neural mechanisms underlying drug abuse, as video game and internet addictions reduce the sensitivity of the dopaminergic reward system, it is still premature to conclude that this addiction is equivalent to substance addictions, as the research is in its early stages.
There is evidence of a dual processing model of digital technology addictions characterized by an imbalance between the reactive and the reflective reward systems. Other studies shown increased difficulties in decision making in specific contexts, such as risky situations but not in ambiguous situations, and an increased preference for short-term rewards.
Although the number of neuroimaging studies on internet gaming disorder is rising, there are several methodological shortcomings, particularly in the inconsistency of psychometric assessments. Furthermore, the conclusions on reduced inhibition should be moderated, as only one study included a functional control, which then showed no difference in inhibition.
A meta-analytic review of the research concluded the evidence suggests video game addiction arises out of other mental health problems, rather than causing them. Thus it is unclear whether video game addiction should be considered a unique diagnosis.
Management:
As concern over video game addiction grows, the use of psychopharmacology, psychotherapy, twelve-step programs, and use of continuing developing treatment enhancements have been proposed to treat this disorder. Empirical studies indeed indicate that internet gaming disorder is associated with detrimental health-related outcomes.
However, the clinical trials of potential treatments remain of low quality, except for cognitive-behavioral therapies, which shows efficacy to reduce gaming disorder and depressive symptoms but not total time spent.
Although there is a scientific consensus that cognitive-behavioral therapy is preferable to pharmacological treatment, it remains difficult to make definitive statements about its benefits and efficiency due to methodological inconsistencies and lack of follow-up.
Since efficacious treatments have not been well established, prevention of video gaming disorder is crucial. Some evidence suggest that up to 50% of people affected by the internet gaming disorder may recover naturally.
Some countries, such as South Korea, China, the Netherlands, Canada, and the United States, have responded to the perceived threat of video game addiction by opening treatment centers.
Outcomes:
Mental health:
Internet gaming disorder is associated with increased anxiety, social phobia and depression, with adults and young adults being more affected than adolescents.
Physical health:
The most frequent physical health-related outcome are alterations in physical functioning such as somatisation and sleep disturbances. Preliminary evidence suggest that internet gaming disorder and the induced sedentarity may contribute to a lack of physical exercise, even though the relationship is not causal.
Epidemiology:
The prevalence of internet gaming disorder range from 0.7% to 25.5% worldwide, or 1.0% to 26.8% worldwide, and 3.5% to 17% in China, and is higher among males than females and among younger than older people, with geographical region being an insignificant contributor.
A longer time spent on video games predicts a tendency towards pathological gaming in the future. The studies, however, used various methodologies and definitions, which renders consensus difficult to achieve and may explain the wide range of prevalence.
Research:
Debates on the classification:
A meta-analytic review of pathological gaming studies concluded that about 3% of gamers may experience some symptoms of pathological gaming. The report noted problems in the field with defining and measuring pathological gaming and concluded that pathological gaming behaviors were more likely the product of underlying mental health problems rather than the inverse.
Barnett and Coulson expressed concern that much of the debate on the issue of addiction may be a knee jerk response stimulated by poor understanding of games and game players.
Such issues may lead both society and scholars to exaggerate the prevalence and nature of problematic gaming, and over-focus on games specifically, while ignoring underlying mental health issues.
Other scholars have cautioned that comparing the symptoms of problematic gaming with problematic gambling is flawed, and that such comparisons may introduce research artifacts and artificially inflate prevalence estimates.
For instance, Richard Wood has observed that behaviors which are problematic in regards to gambling may not be as problematic when put into the context of other behaviors that are rewarding such as gaming. Similarly, Barnett and Coulson have cautioned that discussions of problematic gaming have moved forward prematurely without proper understanding of the symptoms, proper assessment and consequences.
Rather than video gaming disorder being a subtype of gambling disorder, a majority of researchers support the idea of video game addiction being a part of a more comprehensive framework of impulse control disorders with "pathological technology use" with similar characteristics, including the pathological use of video games, internet, computers and other interactive medias.
Although internet and video game addictions are generally considered different from gambling disorder and substance abuse, there is a growing body of evidence indicating they share common features, including behavioral and neural features. Indeed, it is suggested that while behavioral addiction may differ with drug addictions in magnitude, they share several characteristics, with Hellman et al. proposing that the concept of addiction should be de-medicalized.
On the contrary, a literature review found that as the video game addiction develops, online gaming addicts spend increasing amounts of time not only playing but also preparing for and organizing their playing sessions, suggesting this addiction may be behavioral rather than a disorder of impulse control. There is recent evidence suggesting that internet gaming disorder can cause two distinct types of dysfunctions: cognitive and metacognitive.
Griffiths has suggested that psycho-social dependence may revolve around the intermittent reinforcements in the game and the need to belong. Hagedorn & Young have suggested that social dependence may arise due to video games occurring online where players interact with others and the relationships "often become more important for gamers than real-life relationships".
Controversy and alternative viewpoints:
Common challenges involve the reliability of the methodology and validity of the results in some studies. Many rely on self-surveys from university students and also lack time frames making it difficult to study the impact, if any, of addiction on a long term scale. Other concerns also address the definition of addiction and how to measure it, questioning whether or not time is a proper unit to determine how addicted someone is to gaming.
Daria Joanna Kuss and Mark D. Griffiths have argued the current scientific knowledge on internet gaming addiction is copious in scope and complexity. They state that instead, a simple framework should be provided to allow all current and future studies to be categorized, as internet gaming addiction lies on a continuum beginning with etiology and risk factors all the way through the development of "full-blown" addiction and ending with ramifications and potential treatment.
In addition, they caution the deployment of the label "addiction" since it heavily denotes the use of substances or engagement in certain behaviors. Finally, the researcher promotes other researchers to assess the validity and reliability of existing measures instead of developing additional measurement instruments.
Other challenges include the lack of context of the participant's life and the negative portrayal of gaming addicts. Some state that gamers sometimes use video games to either escape from an uncomfortable environment or alleviate their already existing mental issues—both possibly important aspects in determining the psychological impact of gaming.
Negative portrayal also deals with the lack of consistency in measuring addictive gaming. This leads to discussions that sometimes exaggerate the issue and create a misconception in some that they, themselves, may be addicted when they are not.
The evidence of video game addiction to create withdrawal symptoms is very limited and thus debated, due to different definitions and low quality trials.
The concept of video game disorder is itself being debated, with the overlap of its symptoms with other mental disorders, the unclear consensus on a definition and thresholds, and the lack of evidence raising doubts on whether or not this qualifies as a mental disorder of its own.
Despite the lack of a unified definition, there is an emerging consensus among studies that Internet gaming disorder is mainly defined by three features: 1) withdrawal, 2) loss of control, and 3) conflict. Although the DSM-5 definition of video game disorder has a good fit to current methodological definitions used in trials and studies, there are still debates on the clinical pertinence.
Michael Brody, M.D., head of the TV and Media Committee of the American Academy of Child and Adolescent Psychiatry, stated in a 2007 press release that "... there is not enough research on whether or not video games are addictive." However, Brody also cautioned that for some children and adolescents, "... it displaces physical activity and time spent on studies, with friends, and even with family."
A major issue concerns the lack of consistent measures and definitions and of acquisition of follow-up data. Furthermore, the study design quality has not greatly improved between the 2000s and 2017.
For instance, most studies measured internet gaming behaviors in terms of frequency of use (total time spent), without considering the type of game (e.g., MMORPG), the social context (e.g., physically or virtually with friends), nor the motivations (e.g., competitive, achievement-oriented "grinding").
Although the amount of time spent was postulated by Johanssonn and Götestam in 2004 to lead to pathological behaviors, it is unclear whether the time spent is a cause or a consequence of pathological use. These criticisms, however, mostly pertain to Western research since there is more data of higher quality available in Asian regions, where the Internet gaming disorder is more prevalent.
A survey conducted in 2019 of 214 scholars shown that 60.8% agreed that pathological video game use could be a mental health problems, whereas 30.4% were skeptical. However, only 49.7% agreed with the DSM-5 definition of Internet gaming disorder, and 56.5% to the definition of the World Health Organization.
Most scholars were worried that WHO's and DSM-5's inclusion of Internet gaming disorder was "over-pathologizing normal youth" and "precipitated moral panic over video games". This indicates a lack of consensus on the issue as of 2019.
Society and culture:
Parental concerns:
According to ABC News, parents have many concerns about their children playing video games, including concerns about age appropriateness, the amount of time spent playing games, physical health, and aggressive behavior.
Governmental concerns:
The first video game to attract political controversy was the 1978 arcade game Space Invaders. In 1981, a political bill called the Control of Space Invaders (and other Electronic Games) Bill was drafted by British Labour Party MP George Foulkes in an attempt to ban the game for its "addictive properties" and for causing "deviancy". The bill was debated and only narrowly defeated in parliament by 114 votes to 94 votes.
In August 2005, the government of the People's Republic of China, where more than 20 million people play online games, introduced an online gaming restriction limiting playing time to three hours, after which the player would be expelled from whichever game they were playing.
In 2006, it relaxed the rule so only citizens under the age of 18 would face the limitation. Reports indicate underage gamers found ways to circumvent the measure. In July 2007, the rule was relaxed yet again. Internet games operating in China must require users identify themselves by resident identity numbers.
After three hours, players under 18 are prompted to stop and "do suitable physical exercise". If they continue, their in-game points are "slashed in half". After five hours, all their points are automatically erased.
In 2008, one of the five Federal Communications Commission (FCC) Commissioners, Deborah Taylor Tate, stated that online gaming addiction was "one of the top reasons for college drop-outs". However, she did not mention a source for the statement nor identify its position in relation to other top reasons.
In 2011, the South Korean government implemented a law, known as the Shutdown law or the Cinderella Law, which prohibits children under the age of 16 from playing online video games between the hours of 12:00 a.m. to 6:00 a.m. However, as of 2014, the law was amended and now children under the age of 16 can play after midnight if they have permission from their parents.
A systematic review identified in 2017 three types of currently attempted governmental policies: 1) limiting the availability of video games (shutdown, fatigue system, parental controls), 2) reduce the risks and harm (warning messages), 3) provide addiction help services to gamers.
Most of these policies were either not as efficient as intended or not yet evaluated for efficiency, which lead some researchers to prompt for a global public health approach to prevent the onset and progression of this disorder. Some researchers suggest that the video game industry should itself place preventive measures against video game addiction.
Deaths:
There have been at least a few deaths caused directly by exhaustion from playing games for excessive periods of time.
China:
In 2005, thirteen-year-old Zhang XiaoYi committed suicide by jumping from the top of a 24-story tower block in his home province Tianjin. After previously having spent two straight days playing online role-playing games in an Internet cafe, Zhang had told his parents that he had "been poisoned by games and could no longer control himself".
The head of a software association said to gaming website Play.tm that same year: "In the hypothetical world created by such games, [players] become confident and gain satisfaction, which they cannot get in the real world."
In 2007, a 26-year-old man identified only as "Zhang" died of a heart attack due to lack of physical activity following a seven-day gaming binge, while a 30-year-old man died in a Guangzhou Internet cafe after playing online games for three straight days.
South Korea:
In 2005, 28-year old industrial repairman Seungseob Lee (Hangul: 이승섭) visited an Internet cafe in the city of Daegu and played StarCraft almost continuously for fifty hours. He went into cardiac arrest and died at a local hospital. A friend reported: "... he was a game addict. We all knew about it. He couldn't stop himself." About six weeks before his death, his girlfriend, also an avid gamer, broke up with him. In addition, he was fired from his job.
In 2009, Kim Sa-rang, a 3-month-old Korean girl, starved to death after both her parents spent hours each day in an Internet cafe, rearing a virtual child in an online game, Prius Online. The death is covered in the 2014 documentary Love Child.
United States:
In November 2001, Shawn Woolley committed suicide; it has been inferred that his death was related to the popular computer game EverQuest. Shawn's mother said the suicide was due to a rejection or betrayal in the game from a character Shawn called "iluvyou".
Ohio teenager Daniel Petric shot his parents, killing his mother, after they took away his copy of Halo 3 in October 2007. In a sentencing hearing after the teen was found guilty of aggravated murder, the judge said, "I firmly believe that Daniel Petric had no idea at the time he hatched this plot that if he killed his parents they would be dead forever."
On 16 June 2009, Petric was sentenced to 23 years to life in prison.
Click on any of the following blue hyperlinks for more about Video Game Addictions:
- History
- See also:
Heroin Addiction
- YouTube Video: Mechanism of Drug Addiction in the Brain, Animation.
- YouTube Video: What Does Heroin Do To Your Body?
- YouTube Video: The New Face of Heroin Addiction | 20/20 | ABC News
Heroin, also known as diacetylmorphine and diamorphine among other names, is an opioid used as a recreational drug for its euphoric effects.
Medical grade diamorphine is used as a pure hydrochloride salt which is distinguished from black tar heroin, a variable admixture of morphine derivatives—predominantly 6-MAM (6-monoacetylmorphine), which is the result of crude acetylation during clandestine production of street heroin.
Diamorphine is used medically in several countries to relieve pain, such as during childbirth or a heart attack, as well as in opioid replacement therapy.
It is typically injected, usually into a vein, but it can also be smoked, snorted, or inhaled. In a clinical context the route of administration is most commonly intravenous injection; it may also be given by intramuscular or subcutaneous injection, as well as orally in the form of tablets. The onset of effects is usually rapid and lasts for a few hours.
Common side effects include respiratory depression (decreased breathing), dry mouth, drowsiness, impaired mental function, constipation, and addiction. Side effects of use by injection can include abscesses, infected heart valves, blood-borne infections, and pneumonia.
After a history of long-term use, opioid withdrawal symptoms can begin within hours of the last use. When given by injection into a vein, heroin has two to three times the effect of a similar dose of morphine. It typically appears in the form of a white or brown powder.
Treatment of heroin addiction often includes behavioral therapy and medications. Medications can include buprenorphine, methadone, or naltrexone. A heroin overdose may be treated with naloxone.
An estimated 17 million people as of 2015 use opiates, of which heroin is the most common, and opioid use resulted in 122,000 deaths. The total number of heroin users worldwide as of 2015 is believed to have increased in Africa, the Americas, and Asia since 2000.
In the United States, approximately 1.6 percent of people have used heroin at some point, with 950,000 using it in the last year. When people die from overdosing on a drug, the drug is usually an opioid and often heroin.
Heroin was first made by C. R. Alder Wright in 1874 from morphine, a natural product of the opium poppy. Internationally, heroin is controlled under Schedules I and IV of the Single Convention on Narcotic Drugs, and it is generally illegal to make, possess, or sell without a license.
About 448 tons of heroin were made in 2016. In 2015,Afghanistan produced about 66% of the world's opium. Illegal heroin is often mixed with other substances such as sugar, starch, caffeine, quinine, or other opioids like fentanyl.
Click on any of the following blue hyperlinks for more about Heroin Addiction:
Medical grade diamorphine is used as a pure hydrochloride salt which is distinguished from black tar heroin, a variable admixture of morphine derivatives—predominantly 6-MAM (6-monoacetylmorphine), which is the result of crude acetylation during clandestine production of street heroin.
Diamorphine is used medically in several countries to relieve pain, such as during childbirth or a heart attack, as well as in opioid replacement therapy.
It is typically injected, usually into a vein, but it can also be smoked, snorted, or inhaled. In a clinical context the route of administration is most commonly intravenous injection; it may also be given by intramuscular or subcutaneous injection, as well as orally in the form of tablets. The onset of effects is usually rapid and lasts for a few hours.
Common side effects include respiratory depression (decreased breathing), dry mouth, drowsiness, impaired mental function, constipation, and addiction. Side effects of use by injection can include abscesses, infected heart valves, blood-borne infections, and pneumonia.
After a history of long-term use, opioid withdrawal symptoms can begin within hours of the last use. When given by injection into a vein, heroin has two to three times the effect of a similar dose of morphine. It typically appears in the form of a white or brown powder.
Treatment of heroin addiction often includes behavioral therapy and medications. Medications can include buprenorphine, methadone, or naltrexone. A heroin overdose may be treated with naloxone.
An estimated 17 million people as of 2015 use opiates, of which heroin is the most common, and opioid use resulted in 122,000 deaths. The total number of heroin users worldwide as of 2015 is believed to have increased in Africa, the Americas, and Asia since 2000.
In the United States, approximately 1.6 percent of people have used heroin at some point, with 950,000 using it in the last year. When people die from overdosing on a drug, the drug is usually an opioid and often heroin.
Heroin was first made by C. R. Alder Wright in 1874 from morphine, a natural product of the opium poppy. Internationally, heroin is controlled under Schedules I and IV of the Single Convention on Narcotic Drugs, and it is generally illegal to make, possess, or sell without a license.
About 448 tons of heroin were made in 2016. In 2015,Afghanistan produced about 66% of the world's opium. Illegal heroin is often mixed with other substances such as sugar, starch, caffeine, quinine, or other opioids like fentanyl.
Click on any of the following blue hyperlinks for more about Heroin Addiction:
- Uses
- Routes of administration
- Adverse effects
- Overdose
- Pharmacology
- Chemistry
- History
- Society and culture
- Research
- See also;
- Allegations of CIA drug trafficking
- Cheese (recreational drug)
- The Politics of Heroin in Southeast Asia
- Heroin at Curlie
- NIDA InfoFacts on Heroin
- ONDCP Drug Facts
- U.S. National Library of Medicine: Drug Information Portal – Heroin
- BBC Article entitled 'When Heroin Was Legal'. References to the United Kingdom and the United States
- Drug-poisoning Deaths Involving Heroin: United States, 2000–2013 U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
- Heroin Trafficking in the United States (2016) by Kristin Finklea, Congressional Research Service.
Opium and Opiates, including Opium Production in Afghanistan
- YouTube Video: The battle to stop Afghanistan's opium trade
- YouTube Video: Opium trade fueling the Taliban
- YouTube Video: The Reality of the US Withdrawal From Afghanistan
Opium (or poppy tears, scientific name: Lachryma papaveris) is dried latex obtained from the seed capsules of the opium poppy Papaver somniferum. Approximately 12 percent of opium is made up of the analgesic alkaloid morphine, which is processed chemically to produce heroin and other synthetic opioids for medicinal use and for the illegal drug trade.
The latex also contains the closely related opiates codeine and thebaine, and non-analgesic alkaloids such as papaverine and noscapine. The traditional, labor-intensive method of obtaining the latex is to scratch ("score") the immature seed pods (fruits) by hand; the latex leaks out and dries to a sticky yellowish residue that is later scraped off and dehydrated.
The word "meconium" (derived from the Greek for "opium-like", but now used to refer to newborn stools) historically referred to related, weaker preparations made from other parts of the opium poppy or different species of poppies.
The production methods have not significantly changed since ancient times. Through selective breeding of the Papaver somniferum plant, the content of the phenanthrene alkaloids morphine, codeine, and to a lesser extent thebaine has been greatly increased.
In modern times, much of the thebaine, which often serves as the raw material for the synthesis for oxycodone, hydrocodone, hydromorphone, and other semisynthetic opiates, originates from extracting Papaver orientale or Papaver bracteatum.
For the illegal drug trade, the morphine is extracted from the opium latex, reducing the bulk weight by 88%. It is then converted to heroin (see above topic) which is almost twice as potent and increases the value by a similar factor. The reduced weight and bulk make it easier to smuggle.
Click on any of the following blue hyperlinks for more about Opium:
Opiate is a term classically used in pharmacology to mean a substance derived from opium (above). Opioid, a more modern term, is used to designate all substances, both natural and synthetic, that bind to opioid receptors in the brain (including antagonists).
Opiates are alkaloid compounds naturally found in the opium poppy plant Papaver somniferum. The psychoactive compounds found in the opium plant include morphine, codeine, and thebaine.
Opiates have long been used for a variety of medical conditions with evidence of opiate trade and use for pain relief as early as the eighth century AD. Opiates are considered drugs with moderate to high abuse potential and are listed on various "Substance-Control Schedules" under the Uniform Controlled Substances Act of the United States of America.
In 2014, between 13 and 20 million people used opiates recreationally (0.3% to 0.4% of the global population between the ages of 15 and 65). According to the CDC, from this population, there has been a recorded 47,000 deaths with a total of a half a million deaths from 2000–2014.
In 2016, the World Health Organization reported that 27 million people suffer from opioid abuse disorder. They also reported that in 2015, 450,000 people died as a result of drug use, with between a third and a half of that number being attributed to opioids.
Click on any of the following blue hyperlinks for more about Opiates:
Opium production in Afghanistan
Afghanistan has been the world's leading illicit drug producer since 2001. Afghanistan's opium poppy harvest produces more than 90% of illicit heroin globally, and more than 95% of the European supply.
More land is used for opium in Afghanistan than is used for coca cultivation in Latin America. In 2007, 93% of the non-pharmaceutical-grade opiates on the world market originated in Afghanistan. This amounts to an export value of about US$4 billion, with a quarter being earned by opium farmers and the rest going to district officials, insurgents, warlords, and drug traffickers.
In the seven years (1994–2000) prior to a Taliban opium ban, the Afghan farmers' share of gross income from opium was divided among 200,000 families. As of 2017, opium production provides about 400,000 jobs in Afghanistan, more than the Afghan National Security Forces.
The opium trade spiked in 2006 after the Taliban lost control of local warlords. In addition to opium, Afghanistan is also the world's leading producer of hashish
Click on any of the following blue hyperlinks for more about Opioid Production in Afghanistan:
The latex also contains the closely related opiates codeine and thebaine, and non-analgesic alkaloids such as papaverine and noscapine. The traditional, labor-intensive method of obtaining the latex is to scratch ("score") the immature seed pods (fruits) by hand; the latex leaks out and dries to a sticky yellowish residue that is later scraped off and dehydrated.
The word "meconium" (derived from the Greek for "opium-like", but now used to refer to newborn stools) historically referred to related, weaker preparations made from other parts of the opium poppy or different species of poppies.
The production methods have not significantly changed since ancient times. Through selective breeding of the Papaver somniferum plant, the content of the phenanthrene alkaloids morphine, codeine, and to a lesser extent thebaine has been greatly increased.
In modern times, much of the thebaine, which often serves as the raw material for the synthesis for oxycodone, hydrocodone, hydromorphone, and other semisynthetic opiates, originates from extracting Papaver orientale or Papaver bracteatum.
For the illegal drug trade, the morphine is extracted from the opium latex, reducing the bulk weight by 88%. It is then converted to heroin (see above topic) which is almost twice as potent and increases the value by a similar factor. The reduced weight and bulk make it easier to smuggle.
Click on any of the following blue hyperlinks for more about Opium:
- History
- Modern production and use
- Chemical and physiological properties
- Slang terms
- See also:
- Golden Crescent
- Golden Triangle
- History of Jardine, Matheson & Co.
- Illegal drug trade in Colombia
- Mexican Drug War
- Nabidh
- Opium replacement
- Protocol for Limiting and Regulating the Cultivation of the Poppy Plant, the Production of, International and Wholesale Trade in, and Use of Opium
- Psychoactive drug
- Society for the Suppression of the Opium Trade
- Morphine
- A fleet of opium clippers on the River Ganges
- Confessions of a Poppy Tea addict
- DEA drug information: Opium, morphine, and heroin
- Erowid: Opium
- Opium in India
- Opium Made Easy by Michael Pollan (originally appeared in Harper's.)
- Opium Museum: Opium paraphernalia and historical photos of opium smokers
- BLTC Research: Speculations on the future of opioids
- Thailex photo: Traditional method of using opium in Thailand
- Tsur Shezaf, Witer, The Opium Growers of Sinai Archived November 20, 2009, at the Wayback Machine
- UNODC – United Nations Office on Drugs and Crime – Afghan Opium Survey 2009
Opiate is a term classically used in pharmacology to mean a substance derived from opium (above). Opioid, a more modern term, is used to designate all substances, both natural and synthetic, that bind to opioid receptors in the brain (including antagonists).
Opiates are alkaloid compounds naturally found in the opium poppy plant Papaver somniferum. The psychoactive compounds found in the opium plant include morphine, codeine, and thebaine.
Opiates have long been used for a variety of medical conditions with evidence of opiate trade and use for pain relief as early as the eighth century AD. Opiates are considered drugs with moderate to high abuse potential and are listed on various "Substance-Control Schedules" under the Uniform Controlled Substances Act of the United States of America.
In 2014, between 13 and 20 million people used opiates recreationally (0.3% to 0.4% of the global population between the ages of 15 and 65). According to the CDC, from this population, there has been a recorded 47,000 deaths with a total of a half a million deaths from 2000–2014.
In 2016, the World Health Organization reported that 27 million people suffer from opioid abuse disorder. They also reported that in 2015, 450,000 people died as a result of drug use, with between a third and a half of that number being attributed to opioids.
Click on any of the following blue hyperlinks for more about Opiates:
- Overview
- Synthesis
- Pharmacokinetics
- Indication
- Complications and side effects
- Pharmacology in pain
- Absolute contraindications
- Risk factors for prescription abuse
- See also:
Opium production in Afghanistan
Afghanistan has been the world's leading illicit drug producer since 2001. Afghanistan's opium poppy harvest produces more than 90% of illicit heroin globally, and more than 95% of the European supply.
More land is used for opium in Afghanistan than is used for coca cultivation in Latin America. In 2007, 93% of the non-pharmaceutical-grade opiates on the world market originated in Afghanistan. This amounts to an export value of about US$4 billion, with a quarter being earned by opium farmers and the rest going to district officials, insurgents, warlords, and drug traffickers.
In the seven years (1994–2000) prior to a Taliban opium ban, the Afghan farmers' share of gross income from opium was divided among 200,000 families. As of 2017, opium production provides about 400,000 jobs in Afghanistan, more than the Afghan National Security Forces.
The opium trade spiked in 2006 after the Taliban lost control of local warlords. In addition to opium, Afghanistan is also the world's leading producer of hashish
Click on any of the following blue hyperlinks for more about Opioid Production in Afghanistan:
- History
- Production and distribution
- Worldwide impact
- Medical production
- Opium addiction within Afghan society
- The Afghan economy and opium
- Production and Afghan governance
- Opium smuggling into Iran
- Counter-narcotics policy
- See also:
- Afghan morphine
- Crime in Afghanistan
- Economy of Afghanistan
- Golden Crescent
- Haji Bagcho
- Haji Bashar
- Illegal drug trade
- Jundallah
- Opium in Iran
- The Senlis Council
- Opium Season, the true story of a young American in Afghanistan running an aid program to counter the opium trade
Methamphetamine ("Meth")
- YouTube Video: What Are Signs Of A Meth Lab In Your Neighborhood?
- YouTube Video: Meth Lab Baby: a child's fight for life
- YouTube Video: 'Backpack Meth Labs' On The Rise
Methamphetamine (known as "Meth" and contracted from N-methylamphetamine) is a potent central nervous system (CNS) stimulant that is mainly used as a recreational drug and less commonly as a second-line treatment for attention deficit hyperactivity disorder and obesity.
Methamphetamine was discovered in 1893 and exists as two enantiomers: levo-methamphetamine and dextro-methamphetamine. Methamphetamine properly refers to a specific chemical, the racemic free base, which is an equal mixture of levomethamphetamine and dextromethamphetamine in their pure amine forms.
It is rarely prescribed over concerns involving human neurotoxicity and potential for recreational use as an aphrodisiac and euphoriant, among other concerns, as well as the availability of safer substitute drugs with comparable treatment efficacy.
Dextromethamphetamine is a stronger CNS stimulant than levomethamphetamine.
Both methamphetamine and dextromethamphetamine are illicitly trafficked and sold owing to their potential for recreational use. The highest prevalence of illegal methamphetamine use occurs in parts of Asia, Oceania, and in the United States, where racemic methamphetamine and dextromethamphetamine are classified as schedule II controlled substances.
Levomethamphetamine is available as an over-the-counter (OTC) drug for use as an inhaled nasal decongestant in the United States. Internationally, the production, distribution, sale, and possession of methamphetamine is restricted or banned in many countries, due to its placement in schedule II of the United Nations Convention on Psychotropic Substances treaty.
While dextromethamphetamine is a more potent drug, racemic methamphetamine is sometimes illicitly produced due to the relative ease of synthesis and limited availability of chemical precursors.
In low to moderate doses, methamphetamine can elevate mood, increase alertness, concentration and energy in fatigued individuals, reduce appetite, and promote weight loss.
At very high doses, it can induce psychosis, breakdown of skeletal muscle, seizures and bleeding in the brain. Chronic high-dose use can precipitate unpredictable and rapid mood swings, stimulant psychosis (e.g., paranoia, hallucinations, delirium, and delusions) and violent behavior.
Recreationally, methamphetamine's ability to increase energy has been reported to lift mood and increase sexual desire to such an extent that users are able to engage in sexual activity continuously for several days.
Methamphetamine is known to possess a high addiction liability (i.e., a high likelihood that long-term or high dose use will lead to compulsive drug use) and high dependence liability (i.e. a high likelihood that withdrawal symptoms will occur when methamphetamine use ceases).
Withdrawal off of methamphetamine after heavy use may lead to a post-acute-withdrawal syndrome, which can persist for months beyond the typical withdrawal period.
Methamphetamine is neurotoxic to human midbrain dopaminergic neurons at high doses. Methamphetamine has been shown to have a higher affinity and, as a result, higher toxicity toward serotonergic neurons than amphetamine. Methamphetamine neurotoxicity causes adverse changes in brain structure and function, such as reductions in grey matter volume in several brain regions, as well as adverse changes in markers of metabolic integrity.
Methamphetamine belongs to the substituted phenethylamine and substituted amphetamine chemical classes. It is related to the other dimethylphenethylamines as a positional isomer of these compounds, which share the common chemical formula: C10H15N1.
Click on any of the following blue hyperlinks for more abou Meth:
Methamphetamine was discovered in 1893 and exists as two enantiomers: levo-methamphetamine and dextro-methamphetamine. Methamphetamine properly refers to a specific chemical, the racemic free base, which is an equal mixture of levomethamphetamine and dextromethamphetamine in their pure amine forms.
It is rarely prescribed over concerns involving human neurotoxicity and potential for recreational use as an aphrodisiac and euphoriant, among other concerns, as well as the availability of safer substitute drugs with comparable treatment efficacy.
Dextromethamphetamine is a stronger CNS stimulant than levomethamphetamine.
Both methamphetamine and dextromethamphetamine are illicitly trafficked and sold owing to their potential for recreational use. The highest prevalence of illegal methamphetamine use occurs in parts of Asia, Oceania, and in the United States, where racemic methamphetamine and dextromethamphetamine are classified as schedule II controlled substances.
Levomethamphetamine is available as an over-the-counter (OTC) drug for use as an inhaled nasal decongestant in the United States. Internationally, the production, distribution, sale, and possession of methamphetamine is restricted or banned in many countries, due to its placement in schedule II of the United Nations Convention on Psychotropic Substances treaty.
While dextromethamphetamine is a more potent drug, racemic methamphetamine is sometimes illicitly produced due to the relative ease of synthesis and limited availability of chemical precursors.
In low to moderate doses, methamphetamine can elevate mood, increase alertness, concentration and energy in fatigued individuals, reduce appetite, and promote weight loss.
At very high doses, it can induce psychosis, breakdown of skeletal muscle, seizures and bleeding in the brain. Chronic high-dose use can precipitate unpredictable and rapid mood swings, stimulant psychosis (e.g., paranoia, hallucinations, delirium, and delusions) and violent behavior.
Recreationally, methamphetamine's ability to increase energy has been reported to lift mood and increase sexual desire to such an extent that users are able to engage in sexual activity continuously for several days.
Methamphetamine is known to possess a high addiction liability (i.e., a high likelihood that long-term or high dose use will lead to compulsive drug use) and high dependence liability (i.e. a high likelihood that withdrawal symptoms will occur when methamphetamine use ceases).
Withdrawal off of methamphetamine after heavy use may lead to a post-acute-withdrawal syndrome, which can persist for months beyond the typical withdrawal period.
Methamphetamine is neurotoxic to human midbrain dopaminergic neurons at high doses. Methamphetamine has been shown to have a higher affinity and, as a result, higher toxicity toward serotonergic neurons than amphetamine. Methamphetamine neurotoxicity causes adverse changes in brain structure and function, such as reductions in grey matter volume in several brain regions, as well as adverse changes in markers of metabolic integrity.
Methamphetamine belongs to the substituted phenethylamine and substituted amphetamine chemical classes. It is related to the other dimethylphenethylamines as a positional isomer of these compounds, which share the common chemical formula: C10H15N1.
Click on any of the following blue hyperlinks for more abou Meth:
- Uses
- Contraindications
- Adverse effects
- Overdose
- Interactions
- Pharmacology
- Chemistry
- History, society, and culture
- Trafficking
- Legal status
- Research
- See also:
- 18-MC
- Breaking Bad, a TV series centered on illicit methamphetamine synthesis
- Faces of Meth, a drug prevention project
- Methamphetamine in the United States
- Montana Meth Project, a Montana-based organization aiming to reduce meth use among teenagers
- Rolling meth lab, a transportable laboratory that is used to illegally produce methamphetamine
Psychological effects of Internet use including Internet addiction disorder
- YouTube Video: Internet addiction disorder affecting toddlers | 60 Minutes Australia
- YouTube Video: Meet The Kid Addicted To The Internet
- YouTube Video: Are You Addicted to the Internet?
Psychological effects of Internet use:
Various researchers have undertaken efforts to examine the psychological effects of Internet use. Some research employs studying brain functions in Internet users. Some studies assert that these changes are harmful, while others argue that asserted changes are beneficial.
Assertions:
American writer Nicholas Carr asserts that Internet use reduces the deep thinking that leads to true creativity. He also says that hyperlinks and overstimulation mean that the brain must give most of its attention to short-term decisions. Carr also states that the vast availability of information on the World Wide Web overwhelms the brain and hurts long-term memory. He says that the availability of stimuli leads to a very large cognitive load, which makes it difficult to remember anything.
Computer scientist Ramesh Sitaraman has asserted that Internet users are impatient and are likely to get more impatient with time. In a large-scale research study that completed in 2012 involving millions of users watching videos on the Internet, Krishnan and Sitaraman show that users start to abandon online videos if they do not start playing within two seconds.
In addition, users with faster Internet connections (such as FTTH) showed less patience and abandoned videos at a faster rate than users with slower Internet connections. Many commentators have since argued that these results provide a glimpse into the future: as Internet services become faster and provide more instant gratification, people become less patient and less able to delay gratification and work towards longer-term rewards.
Psychologist Steven Pinker, however, argues that people have control over what they do, and that research and reasoning never came naturally to people. He says that "experience does not revamp the basic information-processing capacities of the brain" and asserts that the Internet is actually making people smarter.
MRI studies:
The BBC describes the research published in the peer-reviewed science journal PLoS ONE:
"A research team led by Hao Lei of the Chinese Academy of Sciences in Wuhan carried out brain scans of 35 men and women aged between 14 and 21. Seventeen of them were classed as having Internet addiction disorder (IAD: see next topic) on the basis of answering yes to questions such as, "Have you repeatedly made unsuccessful efforts to control, cut back or stop Internet use?”
Specialized MRI brain scans showed changes in the white matter of the brain—the part that contains nerve fibres—in those classed as being web addicts, compared with non-addicts.
Furthermore, the study says, "We provided evidence demonstrating the multiple structural changes of the brain in IAD subjects. VBM results indicated the decreased gray matter volume in the bilateral dorsolateral prefrontal cortex (DLPFC), the supplementary motor area (SMA), the orbitofrontal cortex (OFC), the cerebellum and the left rostral ACC (rACC)."
UCLA professor of psychiatry Gary Small studied brain activity in experienced web surfers versus casual web surfers. He used MRI scans on both groups to evaluate brain activity. The study showed that when Internet surfing, the brain activity of the experienced Internet users was far more extensive than that of the novices, particularly in areas of the prefrontal cortex associated with problem-solving and decision making.
However, the two groups had no significant differences in brain activity when reading blocks of text. This evidence suggested that the distinctive neural pathways of experienced Web users had developed because of their Web use. Dr. Small concluded that "The current explosion of digital technology not only is changing the way we live and communicate, but is rapidly and profoundly altering our brains."
Effect on traditional reading:
In an August 2008 article in The Atlantic ("Is Google Making Us Stupid?"), Nicholas Carr experientially asserts that using the Internet can lead to lower attention span and make it more difficult to read in the traditional sense (that is, read a book at length without mental interruptions).
He says that he and his friends have found it more difficult to concentrate and read whole books, even though they read a great deal when they were younger (that is, when they did not have access to the Internet). This assertion is based on anecdotal evidence, not controlled research.
Researchers from the University College London have done a 5-year study on Internet habits, and have found that people using the sites exhibited "a form of skimming activity," hopping from one source to another and rarely returning to any source they’d already visited.
The 2008 report says, "It is clear that users are not reading online in the traditional sense; indeed there are signs that new forms of "reading" are emerging as users "power browse" horizontally through titles, contents pages and abstracts going for quick wins. It almost seems that they go online to avoid reading in the traditional sense."
Brain power:
Research suggests that using the Internet helps boost brain power for middle-aged and older people (research on younger people has not been done). The study compares brain activity when the subjects were reading and when the subjects were surfing the Internet. It found that Internet surfing uses much more brain activity than reading does.
Lead researcher Professor Gary Small said: "The study results are encouraging, that emerging computerized technologies may have physiological effects and potential benefits for middle-aged and older adults. Internet searching engages complicated brain activity, which may help exercise and improve brain function."
Productivity:
One of the most widely debated effects of social networking has been its influence on productivity. In many schools and workplaces, social media sites are blocked because employers believe their employees will be distracted and unfocused on the sites. It seems, at least from one study, that employers do, indeed, have reason to be concerned.
A survey from Hearst Communications found that productivity levels of people that used social networking sites were 1.5% lower than those that did not. Logically, people cannot get work done when they are performing other tasks. If the employees suffer from degrading self-control, it will be even harder for them to get back to work and maintain productivity.
Effects of social networking and behavior:
Evgeny Morozov has said that social networking could be potentially harmful to people. He writes that they can destroy privacy, and notes that "Insurance companies have accessed their patients' Facebook accounts to try to disprove they have hard-to-verify health problems like depression; employers have checked social networking sites to vet future employees; university authorities have searched the web for photos of their students' drinking or smoking pot."
He also said that the Internet also makes people more complacent and risk averse. He said that because much of the ubiquity of modern technology—cameras, recorders, and such—people may not want to act in unusual ways for fear of getting a bad name. People can see pictures and videos of you on the Internet, and this may make you act differently.
Attention span:
According to the New York Times, many scientists say that "people's ability to focus is being undermined by bursts of information".
From 53,573 page views taken from various users, 17% of the views lasted less than 4 seconds while 4% lasted more than 10 minutes. In regards to page content, users will only read 49% of a site that contains 111 words or fewer while users will opt to read 28% of an average website (approximately 593 words). For each additional 100 words on a site, users will spend 4.4 seconds longer on the site.
It is found that those who read articles online go through the article more thoroughly than those who read from print-based materials. Upon choosing their reading material, online readers read 77% of the content, which can be compared to broadsheet newspaper where the corresponding number is 62%.
Effects of anonymity:
See also: Internet anonymity and Anonymous post
Interacting on the Internet mostly does not involve "physical" interactions with another person (i.e. face-to-face conversation), and therefore easily leads to a person feeling free to act differently online, as well as unrestraint in civility and minimization of authority, etc.
People who are socially anxious are more likely to use electronic communication as their only means of communication. This, in turn, makes them more likely to disclose personal information to strangers online that they normally wouldn't give out face-to-face. The phenomenon is a likely cause for the prevalence of cyberbullying, especially for children who do not understand "social networking etiquette."
Internet anonymity can lead to online disinhibition, in which people do and say things online that they normally wouldn't do or say in person. Psychology researcher John Suler differentiates between benign disinhibition in which people can grow psychologically by revealing secret emotions, fears, and wishes and showing unusual acts of kindness and generosity and toxic disinhibition, in which people use rude language, harsh criticisms, anger, hatred and threats or visit pornographic or violent sites that they wouldn't in the 'real world.'
Escapism:
Ease of access to the Internet can increase escapism in which a user uses the Internet as an "escape" from the perceived unpleasant or banal aspects of daily/real life. Because the internet and virtual realities easily satisfy social needs and drives, according to Jim Blascovich and Jeremy Bailensen, "sometimes [they are] so satisfying that addicted users will withdraw physically from society."
Stanford psychiatrist Dr. Elias Aboujaoude believes that advances in virtual reality and immersive 3-D have led us to "where we can have a 'full life' [online] that can be quite removed from our own." Eventually, virtual reality may drastically change a person's social and emotional needs. "We may stop 'needing' or craving real social interactions because they may become foreign to us," Aboujaoude says.
Effects on children:
Internet has its impact on all age groups from elders to children. According to the article 'Digital power: exploring the effects of social media on children's spirituality', children consider the Internet as their third place after home and school.
One of the main effects social media has had on children is the effect of cyber bullying. A study carried out by 177 students in Canada found that "15% of the students admitted that they cyberbullied others" while "40% of the cyber victims had no idea who the bullies were".
The psychological harm cyber bullying can cause is reflected in low self-esteem, depression and anxiety. It also opens up avenues for manipulation and control. Cyber bullying has ultimately led to depression, anxiety and in severe cases suicide.
Suicide is the third leading cause of death for youth between the ages of 10 and 24. Cyber bullying is rapidly increasing. Some writers have suggested monitoring and educating children from a young age about the risks associated with cyber bullying.
Children use, on average, 27 hours of internet a week and it is on the increase. This leads to an increased risk of insomnia.
Screen time is affecting children in many ways, not only are children at an increased risk of insomnia but they are also at risk of having eye and health developing problems. A study done in 2018 showed that young children are experiencing Computer Vision Syndrome, also referred to as Digital Eye Strain symptoms which include blurred or double vision, headaches, eye fatigue, and more. Many kids are having to wear glasses at a younger age due to excessive amount of screentime.
Health problems are also a big effect of the internet. The National Longitudinal Study of Adolescent Health did a study on adolescents ranging from 7-12 grade and they found that the more screen time you have the higher the risk of obesity. Reducing the amount of time children spend on the internet can prevent getting diseases like obesity and diabetes.
Effects on parenting:
"A psychologist, Aric Sigman, warned of the perils of "passive parenting” and "benign neglect” caused by parent's reliance on gadgets". In some cases, parents' internet addictions can have drastic effects on their children.
In 2009, a three-year-old girl from New Mexico died of malnutrition and dehydration on the same day that her mother was said to have spent 15 hours playing World of Warcraft online.
In another case in 2014, a Korean couple became so immersed in a video game that allowed them to raise a virtual child online that they let their real baby die. The effects of the Internet on parenting can be observed in a how parents utilize the Internet, the response to their child's Internet consumption, as well as the effects and influences that the Internet has on the relationship between parent and child.
Parental Internet use and opinions towards family impact:
Overall, parents are seen to do simple tasks such as sending e-mails and keep up with current events whereas social networking sites are less frequented. In regard to researching parental material, a study conducted in January 2012 by the University of Minnesota found that 75% of questioned parents have stated that the Internet improves their method of obtaining parenting related information, 19.7% found parenting websites too complex to navigate, and 13.1% of the group did not find any useful parenting information on any website.
Many studies have shown that parents view the Internet as a hub of information especially in their children's education. They feel that it is a valuable commodity that can enhance their learning experience and when used in this manner it does not contribute to any family tension or conflicts.
However, when the Internet is used as a social medium (either online gaming or social networking sites) there is a positive correlation between the use of the Internet and family conflicts. In conjunction with using the Internet for social means, there is a risk of exposing familial information to strangers, which is perceived to parents as a threat and can ultimately weaken family boundaries.
Parental response to child online consumption:
A report released in October 2012 by Ofcom focused on the amount of online consumption done by children aged 5–15 and how the parents react to their child's consumption. Of the parents interviewed, 85% use a form of online mediation ranging from face-to-face talks with their children about online surfing to cellphone browser filters. The remaining 15% of parents do not take active measures to adequately inform their children of safe Internet browsing; these parents have either spoken only briefly to their children about cautious surfing or do not do anything at all.
Parents are active in monitoring their child's online use by using methods such as investigating the browsing history and by regulating Internet usage. However, since parents are less versed in Internet usage than their children they are more concerned with the Internet interfering with family life than online matters such as child grooming or cyber-bullying.
When addressing those with lack of parental control over the Internet, parents state that their child is rarely alone (defined for children from 5–11 years old) or that they trust their children when they are online (for children 12–15 years old).
Approximately 80% of parents ensure that their child has been taught Internet safety from school and 70% of parents feel that the benefits of using the Internet are greater than the risks that come along with it.
Conversely an American study, conducted by Pew Internet released on 20 November 2012, reveal that parents are highly concerned about the problems the Internet can impose on their teenage children. 47% of parents are tend to worry about their children being exposed to inappropriate material on the Internet and 45% of the parents are concerned about their children's behavior towards each other both online offline. Only 31% of parents showed concern about the Internet taking away social time from the family.
Effects of Internet use on parent-child relationships:
Researcher Sanford Grossbart and others explores the relationship between the mother and child and how Internet use affects this relationship. This study forms its basis around Marvin Sussman and Suzanne Steinmetz's idea that the relationship between parent and child is highly influenced by the changing experiences and events of each generation.
"Parental warmth" is a factor in how receptive a parent is to being taught the nuances of the Internet by their child versus the traditional method of the parent influencing the child. If the parent displayed "warm" tendencies she was more open to learning how to use the Internet from their child even if the parent happened to be more knowledgeable on the subject.
This fosters teaching in a positive environment, which sustains a strong relationship between mother and child, encourages education, and promotes mature behavior. "Cooler" mothers only allowed themselves to be taught if they thought that their child held the same amount of knowledge or greater and would dismiss the teaching otherwise suggesting a relationship that stems from the majority of influence coming from the parent.
However, despite warm and cool parenting methods, parents who encounter a language barrier rely more heavily on their children to utilize the Internet. Vikki Katz of Rutgers University has studied the interaction between immigrant parents and children and how they use technology. Katz notes that the majority resources that immigrants find helpful are located online, however the search algorithms currently in place do not direct languages other than English appropriately.
Because of this shortcoming, parents strongly encourage their bilingual children to bridge the gap between the Internet and language.
The Internet is increasingly being used as a virtual babysitter when parents actively download applications specifically for their children with intentions to keep them calm. A survey conducted by Ipsos has found that half of the interviewed parents believe children ages 8–13 are old enough to own or carry smartphones thus increasing online content consumption in younger generations.
See also:
Internet addiction disorder
Problematic internet use or pathological internet use, is generally defined as problematic, compulsive use of the internet, that results in significant impairment in an individual's function in various life domains over a prolonged period of time.
Young people are at particular risk of developing internet addiction disorder, with case studies highlighting students whose academic performance plummets as they spend more and more time online. Some also suffer health consequences from loss of sleep, as they stay up later and later to chat online, check for social network status updates or to reach the next game levels.
Excessive Internet use has not been recognized as a disorder by the World Health Organization, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) or the International Classification of Diseases (ICD-11). However, the diagnosis of gaming disorder has been included in the ICD-11.
Controversy around the diagnosis includes whether the disorder is a separate clinical entity, or a manifestation of underlying psychiatric disorders. Research has approached the question from a variety of viewpoints, with no universally standardised or agreed definitions, leading to difficulties in developing evidence based recommendations.
As adolescents (12–19 years) and emerging adults (20–29 years) access the Internet more than any other age groups and undertake a higher risk of overuse of the Internet, the problem of Internet behavior disorder is most relevant to young people.
Consequences:
Mental health consequences:
A longitudinal study of Chinese high school students (2010) suggests that individuals with moderate to severe risk of Internet addiction are 2.5 times more likely to develop depressive symptoms than their IAD-free counterparts.
Another longitudinal study of high school students from Helsinki found that problematic internet usage and depressive symptoms may produce a positive feedback loop. Problematic internet usage is also associated with increased risk of substance abuse.
Social consequences:
The best-documented evidence of Internet addiction so far is time-disruption, which subsequently results in interference with regular social life, including academic, professional performance and daily routines. Some studies also reveal that IAD can lead to disruption of social relationships in Europe and Taiwan. It is, however, also noted by others that IAD is beneficial for peer relations in Taiwan.
Dr. Keith W. Beard (2005) states that "an individual is addicted when an individual's psychological state, which includes both mental and emotional states, as well as their scholastic, occupational and social interactions, is impaired by the overuse of [Internet]".
As a result of its complex nature, some scholars do not provide a definition of Internet addiction disorder and throughout time, different terms are used to describe the same phenomenon of excessive Internet use. Internet addiction disorder is used interchangeably with problematic Internet use, pathological Internet use, and Internet addictive disorder.
In some cases, this behavior is also referred to as Internet overuse, problematic computer use, compulsive Internet use, Internet abuse, harmful use of the Internet, and Internet dependency.
Signs and symptoms:
Physical symptoms:
Physical symptoms include a weakened immune system due to lack of sleep, loss of exercise, and increased risk for carpal tunnel syndrome and eye and back strain.
Symptoms of withdrawal might include agitation, depression, anger and anxiety when the person is away from technology. These psychological symptoms might even turn into physical symptoms such as rapid heartbeat, tense shoulders and shortness of breath.
Related disorders:
Online gambling addiction:
According to David Hodgins, a professor of psychology at the University of Calgary, online gambling is considered to be as serious as pathological gambling. It is known as an "isolated disorder" which means that those who have a gambling problem prefer to separate themselves from interruptions and distractions.
Because gambling is available online, it increases the opportunity for problem gamblers to indulge in gambling without social influences swaying their decisions. This is why this disorder has become more a problem at this date in time and is why it is so difficult to overcome. The opportunity to gamble online is almost always available in this century opposed to only having the opportunity in a public forum at casinos for example.
Online gambling has become quite popular especially with today's adolescents. Today's youth has a greater knowledge of modern software and search engines along with a greater need for extra money. So not only is it easier for them to find opportunities to gamble over any subject, but the incentive to be granted this money is desperately desired.
Online gaming addiction: (Internet gaming disorder)
Main article: Video game addiction
Video game addiction is a known issue around the world. Incidence and severity grew in the 2000s, with the advent of broadband technology, games allowing for the creation of avatars, 'second life' games, and MMORPGs (massive multiplayer online role playing games). World of Warcraft has the largest MMORPG community online and there have been a number of studies about the addictive qualities of the game.
Addicts of the game range from children to mature adults. A well-known example is Ryan van Cleave, a university professor whose life declined as he became involved in online gaming. Andrew Doan, a physician with a research background in neuroscience, battled his own addictions with video games, investing over 20,000 hours of playing games over a period of nine years.
Online gaming addiction may be considered in terms of B.F. Skinner's theory of operant conditioning, which claims that the frequency of a given behavior is directly linked to rewarding and punishment of that behavior. If a behavior is rewarded, it is more likely to be repeated. If it is punished, it becomes suppressed.
Orzack, a clinical psychologist at McLean Hospital in Massachusetts claims that 40 percent of World of Warcraft (WoW) players are addicted. Orzack says that the best way to optimize the desired behavior in the subject is to provide rewards for correct behavior, and then adjust the number of times the subject is required to exhibit that behavior before a reward is provided.
For instance, if a rat must press a bar to receive food, then it will press faster and more often if it does not know how many times it needs to press the bar. An equivalent in World of Warcraft would be purple (epic) loot drops.
Players in World of Warcraft will often spend weeks hunting for a special item which is based on a chance system, sometimes with only a 0.01% chance of it being dropped by a slain monster. The rarity of the item and difficulty of acquiring the item gives the player a status amongst their peers once they obtain the item.
Jim Rossignol, a finance journalist who reports on Internet gaming has described how he overcame his own addiction and channeled his compulsion into a desirable direction as a reporter of Internet gaming and gaming culture.
Pornography addiction (problematic Internet pornography use):
Main article: Pornography addiction
See also: Effects of pornography
Universally accepted diagnostic criteria do not exist for pornography addiction or problematic Internet pornography viewing. Pornography addiction is often defined operationally by the frequency of pornography viewing and negative consequences.
The only diagnostic criteria for a behavioral addiction in the current Diagnostic and Statistical Manual of Mental Disorders are for pathological gambling, and they are similar to those for substance abuse and dependence, such as preoccupation with the behavior, diminished ability to control the behavior, tolerance, withdrawal, and adverse psychosocial consequences.
Diagnostic criteria have been proposed for other behavioral addictions, and these are usually also based on established diagnoses for substance abuse and dependence.
A proposed diagnosis for hypersexual disorder includes pornography as a subtype of this disorder. It included such criteria as time consumed by sexual activity interfering with obligations, repetitive engagement in sexual activity in response to stress, repeated failed attempts to reduce these behaviors, and distress or impairment of life functioning.
A study on problematic Internet pornography viewing used the criteria of viewing Internet pornography more than three times a week during some weeks, and viewing causing difficulty in general life functioning.
According to the American Society of Addiction Medicine, some psychological and behavioral changes characteristic of addiction brain changes include addictive cravings, impulsiveness, weakened executive function, desensitization, and dysphoria. BOLD fMRI results have shown that individuals diagnosed with compulsive sexual behavior (CSB) show enhanced cue reactivity in brain regions associated traditionally with drug-cue reactivity.
These regions include the amygdala and the ventral striatum. Men without CSB who had a long history of viewing pornography exhibited a less intense response to pornographic images in the left ventral putamen, possibly suggestive of desensitization. ASAMs position is inconsistent with the American Association of Sex Educators, Counselors, and Therapists, who cite lack of strong evidence for such classification, describing ASAM as not informed by "accurate human sexuality knowledge".
Neuropsychopharmacological and psychological researches on pornography addiction conducted between 2015 and 2021 have concluded that most studies have been focused entirely or almost exclusively on men in anonymous settings, and the findings are contradicting.
Some researches support the idea that pornography addiction qualifies as a form of behavioral addiction into the umbrella construct of hypersexual behavior and/or a subset of compulsive sexual behavior (CSB), and should be treated as such, whereas others have detected the increased activation of ventral striatal reactivity in men for cues predicting erotic but not monetary rewards and cues signaling erotic pictures, therefore suggesting similarities between pornography addiction and conventional addiction disorders.
Some clinicians and support organizations recommend voluntary use of Internet content-control software, internet monitoring, or both, to manage problematic online pornography use.
Sex researcher Alvin Cooper and colleagues suggested several reasons for using filters as a therapeutic measure, including curbing accessibility that facilitates problematic behavior and encouraging clients to develop coping and relapse prevention strategies. Cognitive therapist Mary Anne Layden suggested that filters may be useful in maintaining environmental control.
Internet behavior researcher David Delmonico stated that, despite their limitations, filters may serve as a "frontline of protection."
Despite the fact that pornography is being indicted as a public health crisis in the United States and elsewhere, with problematic Internet and online pornography use reported to constitute an increasing burden in public mental health since the 2000s, psychopathological models and diagnostic criteria have lacked consensus, and the body of evidence on the effectiveness of therapeutic approaches is still scarce.
In consequence of the COVID-19 pandemic (2020-2021), problematic Internet pornography use and Internet addiction disorder have become difficult to cope for individuals who have adopted this lifestyle and have developed a dependence on these activities as an essential part of their lives, owing to elongated periods of staying at home due to self-isolation.
Communication addiction disorder (compulsive talking):
Main article: Communication addiction disorder
Communication addiction disorder (CAD) is a supposed behavioral disorder related to the necessity of being in constant communication with other people, even when there is no practical necessity for such communication. CAD has been linked to Internet addiction.
Users become addicted to the social elements of the Internet, such as Facebook and YouTube. Users become addicted to one-on-one or group communication in the form of social support, relationships, and entertainment. However, interference with these activities can result in conflict and guilt. This kind of addiction is called problematic social media use.
Social network addiction is a dependence of people by connection, updating, and control of their and their friend's social network page. For some people, in fact, the only important thing is to have a lot of friends in the network regardless if they are offline or only virtual; this is particularly true for teenagers as a reinforcement of egos.
Sometimes teenagers use social networks to show their idealized image to the others. However, other studies claim that people are using social networks to communicate their real personality and not to promote their idealized identity.
Virtual reality addiction:
Main article: Virtual reality addiction
Virtual-reality addiction is an addiction to the use of virtual reality or virtual, immersive environments. Currently, interactive virtual media (such as social networks) are referred to as virtual reality, whereas future virtual reality refers to computer-simulated, immersive environments or worlds.
Experts warn about the dangers of virtual reality, and compare the use of virtual reality (both in its current and future form) to the use of drugs, bringing with these comparisons the concern that, like drugs, users could possibly become addicted to virtual reality.
Video streaming addiction:
Main article: Television addiction
Video streaming addiction is an addiction to watching video content online. This can include TV shows, movies, short video clips and other content. Each person's experience is unique but people who have this addiction may also display addictive relationship with offline video content too (such as television, DVDs, VHS tapes, etc.) Addicts often display binge behavior.
With more development of binging sites such as Netflix, Stan, and Foxtel, more people start binging movies and TV shows everyday, only contributing to this addiction.
Risk factors:
Interpersonal difficulties:
It is argued that interpersonal difficulties such as introversion, social problems, and poor face-to-face communication skills often lead to internet addiction. Internet-based relationships offer a safe alternative for people with aforementioned difficulties to escape from the potential rejections and anxieties of interpersonal real-life contact.
Social support
Individuals who lack sufficient social connection and social support are found to run a higher risk of Internet addiction. They resort to virtual relationships and support to alleviate their loneliness. As a matter of fact, the most prevalent applications among Internet addicts are chat rooms, interactive games, instant messaging, or social media.
Some empirical studies reveal that conflict between parents and children and not living with mother significantly associated with IA after one year. Protective factors such as quality communication between parents and children and positive youth development are demonstrated, in turn, to reduce the risk of IA.
Psychological factors:
Prior addictive or psychiatric history are found to influence the likelihood of being addicted to the Internet. Some individuals with prior psychiatric problems such as depression and anxiety turn to compulsive behaviors to avoid the unpleasant emotions and situation of their psychiatric problems and regard being addicted to the Internet a safer alternative to substance addictive tendency.
But it is generally unclear from existing research which is the cause and which is the effect partially due to the fact that comorbidity is common among Internet addicts.
The most common co-morbidities that have been linked to IAD are major depression and attention deficit hyperactivity disorder (ADHD). The rate of ADHD and IAD associating is as high as 51.6%.
Internet addicts with no previous significant addictive or psychiatric history are argued to develop an addiction to some of the features of Internet use: anonymity, easy accessibility, and its interactive nature.
Neurobiological factors:
Like most other psychopathological conditions, Internet addiction belongs to the group of multifactorial polygenic disorders. For each specific case, there is a unique combination of inherited characteristics (nervous tissue structure, secretion, degradation, and reception of neuromediators), and many are extra-environment factors (family-related, social, and ethnic-cultural).
One of the main challenges in the development of the bio-psychosocial model of Internet addiction is to determine which genes and neuromediators are responsible for increased addiction susceptibility. This article incorporates text by Sergey Tereshchenko and Edward Kasparov available under the CC BY 4.0 license.
Other factors:
Parental educational level, age at first use of the Internet, and the frequency of using social networking sites and gaming sites are found to be positively associated with excessive Internet use among adolescents in some European countries, as well as in the USA.
Diagnosis:
Diagnosis of Internet addiction disorder is empirically difficult. Various screening instruments have been employed to detect Internet addiction disorder. Current diagnoses are faced with multiple obstacles.
Difficulties:
Given the newness of the Internet and the inconsistent definition of Internet addiction disorder, practical diagnosis is far from clear-cut. With the first research initiated by Kimberly S. Young in 1996, the scientific study of Internet addiction has merely existed for more than 20 years.
A few obstacles are present in creating an applicable diagnostic method for Internet addiction disorder.
Despite the advocacy of categorizing Internet addiction as an established illness, neither DSM-IV (1995) nor DSM-5 (2013) considers Internet addiction as a mental disorder.
A subcategory of IAD, Internet gaming disorder is listed in DSM-5 as a condition that requires more research in order to be considered as a full disorder in May 2013. The WHO's draft 11th Revision of the International Classification of Diseases (ICD-11) scheduled for publication in 2018 also include gaming disorder. There is still considerable controversy over whether IAD should be included in the DSM-5 and recognized as a mental disease in general.
Screening instruments:
DSM-based instruments: Most of the criteria utilized by research are adaptations of listed mental disorders (e.g., pathological gambling) in the Statistical Manual of Mental Disorders (DSM) handbook.
Dr. Ivan K. Goldberg, who first broached the concept of Internet addiction, adopted a few criteria for IAD on the basis of DSM-IV, including “hoping to increase time on the network” and “dreaming about the network.”
By adapting the DSM-IV criteria for pathological gambling, Dr. Kimberly S. Young (1998) proposed one of the first integrated sets of criteria, Diagnostic Questionnaire (YDQ), to detect Internet addiction. A person who fulfills any five of the eight adapted criteria would be regarded as Internet addicted: Preoccupation with the Internet;
While Young's YDQ assessment for IA has the advantage of simplicity and ease of use, Keith W. Beard and Eve M. Wolf (2001) further asserted that all of the first five (in the order above) and at least one of the final three criteria (in the order above) be met to delineate Internet addiction in order for a more appropriate and objective assessment.
Young further extended her eight-question YDQ assessment to the now most widely used Internet Addiction Test (IAT), which consists of 20 items with each on a five-point Likert scale.
Questions included on the IAT expand upon Young's earlier eight-question assessment in greater detail and include questions such as "Do you become defensive or secretive when anyone asks you what you do online?" and "Do you find yourself anticipating when you go online again?".
A complete list of questions can be found in Dr. Kimberly S. Young's 1998 book Caught in the Net: How to Recognize the Signs of Internet Addiction and A Winning Strategy for Recovery and Drs. Laura Widyanto and Mary McMurran's 2004 article titled The Psychometric Properties of the Internet Addiction Test.
The Test score ranges from 20 to 100 and a higher value indicates a more problematic use of the Internet:
Over time, a considerable number of screening instruments have been developed to diagnose Internet addiction, including:
Although the various screening methods are developed from diverse contexts, four dimensions manifest themselves across all instruments:
More recently, researchers Mark D. Griffiths (2000) and Dr. Jason C. Northrup and colleagues (2015) claim that Internet per se is simply the medium and that the people are in effect addicted to processes facilitated by the Internet.
Based on Young's Internet Addiction Test (IAT), Northrup and associates further decompose the internet addiction measure into four addictive processes:
The Internet Process Addiction Test (IPAT) is created to measure the processes to which individuals are addicted.
Screening methods that heavily rely on DSM criteria have been accused of lacking consensus by some studies, finding that screening results generated from prior measures rooted in DSM criteria are inconsistent with each other. As a consequence of studies being conducted in divergent contexts, studies constantly modify scales for their own purposes, thereby imposing a further challenge to the standardization in assessing Internet addiction disorder.
Single-question instruments:
Some scholars and practitioners also attempt to define Internet addiction by a single question, typically the time-use of the Internet. The extent to which Internet use can cause negative health consequences is, however, not clear from such a measure. The latter of which is critical to whether IAD should be defined as a mental disorder.
Neuroimaging techniques:
Emergent neuroscience studies investigated the influence of problematic, compulsive use of the internet on the human brain.
Following anecdotal reports and the conclusion by Dr. Kimberly S. Young (1998), neuroimaging studies revealed that IAD contributes to structural and functional abnormalities in the human brain, similar to other behavioral and substance additions.
Therefore, objective non-invasive neuroimaging can contribute to the preliminary diagnosis and treatment of IAD.
Electroencephalography-based diagnosis:
Using Electroencephalography (EEG) readings allows identifying abnormalities in the electrical activity of the human brain caused by IAD.
Studies revealed that individuals suffering from IAD predominantly demonstrate increased activity in the theta and gamma band and decreased delta, alpha, and beta activity. Following these findings, studies identified a correlation between the differences in the EEG readings and the severity of IAD, as well as the extent of impulsivity and inattention.
Classification:
As many scholars have pointed out, the Internet serves merely as a medium through which tasks of divergent nature can be accomplished. Treating disparate addictive behaviors under the same umbrella term is highly problematic.
Dr. Kimberly S. Young (1999) asserts that Internet addiction is a broad term which can be decomposed into several subtypes of behavior and impulse control problems, namely, Cybersexual addiction: compulsive use of adult websites for cybersex and cyberporn (see Internet sex addiction)
For a more detailed description of related disorders please refer to the related disorders section above.
Treatment:
Current interventions and strategies used as treatments for Internet addiction stem from those practiced in substance abuse disorder. In the absence of "methodologically adequate research", treatment programs are not well corroborated. Psychosocial treatment is the approach most often applied. In practice, rehab centers usually devise a combination of multiple therapies.
Psychosocial treatment:
Cognitive behavioral therapy
The cognitive behavioral therapy with Internet addicts (CBT-IA) is developed in analogy to therapies for impulse control disorder.
Several key aspects are embedded in this therapy:
Three phases are implemented in the CBT-IA therapy:
Symptom management of CBT-IA treatment has been found to sustain six months post-treatment.
Motivational interviewing:
The motivational interviewing approach is developed based on therapies for alcohol abusers. This therapy is a directive, patient-centered counseling style for eliciting behavior change through helping patients explore and resolve ambivalence with a respectful therapeutic manner. It does not, however, provide patients with solutions or problem solving until patients' decision to change behaviors.
Several key elements are embedded in this therapy:
Asking open-ended questions;
Other psychosocial treatment therapies include reality therapy, Naikan cognitive psychotherapy, group therapy, family therapy, and multimodal psychotherapy.
Medication:
IAD may be associated with a co-morbidity, so treating a related disorder may also help in the treatment of IAD. When individuals with IAD were treated with certain antidepressants, the time online was reduced by 65% and cravings of being online also decreased. The antidepressants that have been most successful are selective serotonin reuptake inhibitors (SSRIs) such as escitalopram and the atypical antidepressant bupropion.
A psychostimulant, methylphenidate, was also found to have beneficial effects. However, the available evidence on treatment of IAD is of very low quality at this time and well-designed trials are needed.
Prevalence:
Various researchers have undertaken efforts to examine the psychological effects of Internet use. Some research employs studying brain functions in Internet users. Some studies assert that these changes are harmful, while others argue that asserted changes are beneficial.
Assertions:
American writer Nicholas Carr asserts that Internet use reduces the deep thinking that leads to true creativity. He also says that hyperlinks and overstimulation mean that the brain must give most of its attention to short-term decisions. Carr also states that the vast availability of information on the World Wide Web overwhelms the brain and hurts long-term memory. He says that the availability of stimuli leads to a very large cognitive load, which makes it difficult to remember anything.
Computer scientist Ramesh Sitaraman has asserted that Internet users are impatient and are likely to get more impatient with time. In a large-scale research study that completed in 2012 involving millions of users watching videos on the Internet, Krishnan and Sitaraman show that users start to abandon online videos if they do not start playing within two seconds.
In addition, users with faster Internet connections (such as FTTH) showed less patience and abandoned videos at a faster rate than users with slower Internet connections. Many commentators have since argued that these results provide a glimpse into the future: as Internet services become faster and provide more instant gratification, people become less patient and less able to delay gratification and work towards longer-term rewards.
Psychologist Steven Pinker, however, argues that people have control over what they do, and that research and reasoning never came naturally to people. He says that "experience does not revamp the basic information-processing capacities of the brain" and asserts that the Internet is actually making people smarter.
MRI studies:
The BBC describes the research published in the peer-reviewed science journal PLoS ONE:
"A research team led by Hao Lei of the Chinese Academy of Sciences in Wuhan carried out brain scans of 35 men and women aged between 14 and 21. Seventeen of them were classed as having Internet addiction disorder (IAD: see next topic) on the basis of answering yes to questions such as, "Have you repeatedly made unsuccessful efforts to control, cut back or stop Internet use?”
Specialized MRI brain scans showed changes in the white matter of the brain—the part that contains nerve fibres—in those classed as being web addicts, compared with non-addicts.
Furthermore, the study says, "We provided evidence demonstrating the multiple structural changes of the brain in IAD subjects. VBM results indicated the decreased gray matter volume in the bilateral dorsolateral prefrontal cortex (DLPFC), the supplementary motor area (SMA), the orbitofrontal cortex (OFC), the cerebellum and the left rostral ACC (rACC)."
UCLA professor of psychiatry Gary Small studied brain activity in experienced web surfers versus casual web surfers. He used MRI scans on both groups to evaluate brain activity. The study showed that when Internet surfing, the brain activity of the experienced Internet users was far more extensive than that of the novices, particularly in areas of the prefrontal cortex associated with problem-solving and decision making.
However, the two groups had no significant differences in brain activity when reading blocks of text. This evidence suggested that the distinctive neural pathways of experienced Web users had developed because of their Web use. Dr. Small concluded that "The current explosion of digital technology not only is changing the way we live and communicate, but is rapidly and profoundly altering our brains."
Effect on traditional reading:
In an August 2008 article in The Atlantic ("Is Google Making Us Stupid?"), Nicholas Carr experientially asserts that using the Internet can lead to lower attention span and make it more difficult to read in the traditional sense (that is, read a book at length without mental interruptions).
He says that he and his friends have found it more difficult to concentrate and read whole books, even though they read a great deal when they were younger (that is, when they did not have access to the Internet). This assertion is based on anecdotal evidence, not controlled research.
Researchers from the University College London have done a 5-year study on Internet habits, and have found that people using the sites exhibited "a form of skimming activity," hopping from one source to another and rarely returning to any source they’d already visited.
The 2008 report says, "It is clear that users are not reading online in the traditional sense; indeed there are signs that new forms of "reading" are emerging as users "power browse" horizontally through titles, contents pages and abstracts going for quick wins. It almost seems that they go online to avoid reading in the traditional sense."
Brain power:
Research suggests that using the Internet helps boost brain power for middle-aged and older people (research on younger people has not been done). The study compares brain activity when the subjects were reading and when the subjects were surfing the Internet. It found that Internet surfing uses much more brain activity than reading does.
Lead researcher Professor Gary Small said: "The study results are encouraging, that emerging computerized technologies may have physiological effects and potential benefits for middle-aged and older adults. Internet searching engages complicated brain activity, which may help exercise and improve brain function."
Productivity:
One of the most widely debated effects of social networking has been its influence on productivity. In many schools and workplaces, social media sites are blocked because employers believe their employees will be distracted and unfocused on the sites. It seems, at least from one study, that employers do, indeed, have reason to be concerned.
A survey from Hearst Communications found that productivity levels of people that used social networking sites were 1.5% lower than those that did not. Logically, people cannot get work done when they are performing other tasks. If the employees suffer from degrading self-control, it will be even harder for them to get back to work and maintain productivity.
Effects of social networking and behavior:
Evgeny Morozov has said that social networking could be potentially harmful to people. He writes that they can destroy privacy, and notes that "Insurance companies have accessed their patients' Facebook accounts to try to disprove they have hard-to-verify health problems like depression; employers have checked social networking sites to vet future employees; university authorities have searched the web for photos of their students' drinking or smoking pot."
He also said that the Internet also makes people more complacent and risk averse. He said that because much of the ubiquity of modern technology—cameras, recorders, and such—people may not want to act in unusual ways for fear of getting a bad name. People can see pictures and videos of you on the Internet, and this may make you act differently.
Attention span:
According to the New York Times, many scientists say that "people's ability to focus is being undermined by bursts of information".
From 53,573 page views taken from various users, 17% of the views lasted less than 4 seconds while 4% lasted more than 10 minutes. In regards to page content, users will only read 49% of a site that contains 111 words or fewer while users will opt to read 28% of an average website (approximately 593 words). For each additional 100 words on a site, users will spend 4.4 seconds longer on the site.
It is found that those who read articles online go through the article more thoroughly than those who read from print-based materials. Upon choosing their reading material, online readers read 77% of the content, which can be compared to broadsheet newspaper where the corresponding number is 62%.
Effects of anonymity:
See also: Internet anonymity and Anonymous post
Interacting on the Internet mostly does not involve "physical" interactions with another person (i.e. face-to-face conversation), and therefore easily leads to a person feeling free to act differently online, as well as unrestraint in civility and minimization of authority, etc.
People who are socially anxious are more likely to use electronic communication as their only means of communication. This, in turn, makes them more likely to disclose personal information to strangers online that they normally wouldn't give out face-to-face. The phenomenon is a likely cause for the prevalence of cyberbullying, especially for children who do not understand "social networking etiquette."
Internet anonymity can lead to online disinhibition, in which people do and say things online that they normally wouldn't do or say in person. Psychology researcher John Suler differentiates between benign disinhibition in which people can grow psychologically by revealing secret emotions, fears, and wishes and showing unusual acts of kindness and generosity and toxic disinhibition, in which people use rude language, harsh criticisms, anger, hatred and threats or visit pornographic or violent sites that they wouldn't in the 'real world.'
Escapism:
Ease of access to the Internet can increase escapism in which a user uses the Internet as an "escape" from the perceived unpleasant or banal aspects of daily/real life. Because the internet and virtual realities easily satisfy social needs and drives, according to Jim Blascovich and Jeremy Bailensen, "sometimes [they are] so satisfying that addicted users will withdraw physically from society."
Stanford psychiatrist Dr. Elias Aboujaoude believes that advances in virtual reality and immersive 3-D have led us to "where we can have a 'full life' [online] that can be quite removed from our own." Eventually, virtual reality may drastically change a person's social and emotional needs. "We may stop 'needing' or craving real social interactions because they may become foreign to us," Aboujaoude says.
Effects on children:
Internet has its impact on all age groups from elders to children. According to the article 'Digital power: exploring the effects of social media on children's spirituality', children consider the Internet as their third place after home and school.
One of the main effects social media has had on children is the effect of cyber bullying. A study carried out by 177 students in Canada found that "15% of the students admitted that they cyberbullied others" while "40% of the cyber victims had no idea who the bullies were".
The psychological harm cyber bullying can cause is reflected in low self-esteem, depression and anxiety. It also opens up avenues for manipulation and control. Cyber bullying has ultimately led to depression, anxiety and in severe cases suicide.
Suicide is the third leading cause of death for youth between the ages of 10 and 24. Cyber bullying is rapidly increasing. Some writers have suggested monitoring and educating children from a young age about the risks associated with cyber bullying.
Children use, on average, 27 hours of internet a week and it is on the increase. This leads to an increased risk of insomnia.
Screen time is affecting children in many ways, not only are children at an increased risk of insomnia but they are also at risk of having eye and health developing problems. A study done in 2018 showed that young children are experiencing Computer Vision Syndrome, also referred to as Digital Eye Strain symptoms which include blurred or double vision, headaches, eye fatigue, and more. Many kids are having to wear glasses at a younger age due to excessive amount of screentime.
Health problems are also a big effect of the internet. The National Longitudinal Study of Adolescent Health did a study on adolescents ranging from 7-12 grade and they found that the more screen time you have the higher the risk of obesity. Reducing the amount of time children spend on the internet can prevent getting diseases like obesity and diabetes.
Effects on parenting:
"A psychologist, Aric Sigman, warned of the perils of "passive parenting” and "benign neglect” caused by parent's reliance on gadgets". In some cases, parents' internet addictions can have drastic effects on their children.
In 2009, a three-year-old girl from New Mexico died of malnutrition and dehydration on the same day that her mother was said to have spent 15 hours playing World of Warcraft online.
In another case in 2014, a Korean couple became so immersed in a video game that allowed them to raise a virtual child online that they let their real baby die. The effects of the Internet on parenting can be observed in a how parents utilize the Internet, the response to their child's Internet consumption, as well as the effects and influences that the Internet has on the relationship between parent and child.
Parental Internet use and opinions towards family impact:
Overall, parents are seen to do simple tasks such as sending e-mails and keep up with current events whereas social networking sites are less frequented. In regard to researching parental material, a study conducted in January 2012 by the University of Minnesota found that 75% of questioned parents have stated that the Internet improves their method of obtaining parenting related information, 19.7% found parenting websites too complex to navigate, and 13.1% of the group did not find any useful parenting information on any website.
Many studies have shown that parents view the Internet as a hub of information especially in their children's education. They feel that it is a valuable commodity that can enhance their learning experience and when used in this manner it does not contribute to any family tension or conflicts.
However, when the Internet is used as a social medium (either online gaming or social networking sites) there is a positive correlation between the use of the Internet and family conflicts. In conjunction with using the Internet for social means, there is a risk of exposing familial information to strangers, which is perceived to parents as a threat and can ultimately weaken family boundaries.
Parental response to child online consumption:
A report released in October 2012 by Ofcom focused on the amount of online consumption done by children aged 5–15 and how the parents react to their child's consumption. Of the parents interviewed, 85% use a form of online mediation ranging from face-to-face talks with their children about online surfing to cellphone browser filters. The remaining 15% of parents do not take active measures to adequately inform their children of safe Internet browsing; these parents have either spoken only briefly to their children about cautious surfing or do not do anything at all.
Parents are active in monitoring their child's online use by using methods such as investigating the browsing history and by regulating Internet usage. However, since parents are less versed in Internet usage than their children they are more concerned with the Internet interfering with family life than online matters such as child grooming or cyber-bullying.
When addressing those with lack of parental control over the Internet, parents state that their child is rarely alone (defined for children from 5–11 years old) or that they trust their children when they are online (for children 12–15 years old).
Approximately 80% of parents ensure that their child has been taught Internet safety from school and 70% of parents feel that the benefits of using the Internet are greater than the risks that come along with it.
Conversely an American study, conducted by Pew Internet released on 20 November 2012, reveal that parents are highly concerned about the problems the Internet can impose on their teenage children. 47% of parents are tend to worry about their children being exposed to inappropriate material on the Internet and 45% of the parents are concerned about their children's behavior towards each other both online offline. Only 31% of parents showed concern about the Internet taking away social time from the family.
Effects of Internet use on parent-child relationships:
Researcher Sanford Grossbart and others explores the relationship between the mother and child and how Internet use affects this relationship. This study forms its basis around Marvin Sussman and Suzanne Steinmetz's idea that the relationship between parent and child is highly influenced by the changing experiences and events of each generation.
"Parental warmth" is a factor in how receptive a parent is to being taught the nuances of the Internet by their child versus the traditional method of the parent influencing the child. If the parent displayed "warm" tendencies she was more open to learning how to use the Internet from their child even if the parent happened to be more knowledgeable on the subject.
This fosters teaching in a positive environment, which sustains a strong relationship between mother and child, encourages education, and promotes mature behavior. "Cooler" mothers only allowed themselves to be taught if they thought that their child held the same amount of knowledge or greater and would dismiss the teaching otherwise suggesting a relationship that stems from the majority of influence coming from the parent.
However, despite warm and cool parenting methods, parents who encounter a language barrier rely more heavily on their children to utilize the Internet. Vikki Katz of Rutgers University has studied the interaction between immigrant parents and children and how they use technology. Katz notes that the majority resources that immigrants find helpful are located online, however the search algorithms currently in place do not direct languages other than English appropriately.
Because of this shortcoming, parents strongly encourage their bilingual children to bridge the gap between the Internet and language.
The Internet is increasingly being used as a virtual babysitter when parents actively download applications specifically for their children with intentions to keep them calm. A survey conducted by Ipsos has found that half of the interviewed parents believe children ages 8–13 are old enough to own or carry smartphones thus increasing online content consumption in younger generations.
See also:
- Cyberpsychology
- Digital media use and mental health
- Millennials
- "50 things that are being killed by the internet", Matthew Moore, The Telegraph, 4 September 2009
- "Attached to Technology and Paying a Price", Matt Richtel, New York Times, 6 June 2010
- "How is internet affecting our intelligence", Moeez Lodhi, "A Different Version", 16 December 2019
Internet addiction disorder
Problematic internet use or pathological internet use, is generally defined as problematic, compulsive use of the internet, that results in significant impairment in an individual's function in various life domains over a prolonged period of time.
Young people are at particular risk of developing internet addiction disorder, with case studies highlighting students whose academic performance plummets as they spend more and more time online. Some also suffer health consequences from loss of sleep, as they stay up later and later to chat online, check for social network status updates or to reach the next game levels.
Excessive Internet use has not been recognized as a disorder by the World Health Organization, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) or the International Classification of Diseases (ICD-11). However, the diagnosis of gaming disorder has been included in the ICD-11.
Controversy around the diagnosis includes whether the disorder is a separate clinical entity, or a manifestation of underlying psychiatric disorders. Research has approached the question from a variety of viewpoints, with no universally standardised or agreed definitions, leading to difficulties in developing evidence based recommendations.
As adolescents (12–19 years) and emerging adults (20–29 years) access the Internet more than any other age groups and undertake a higher risk of overuse of the Internet, the problem of Internet behavior disorder is most relevant to young people.
Consequences:
Mental health consequences:
A longitudinal study of Chinese high school students (2010) suggests that individuals with moderate to severe risk of Internet addiction are 2.5 times more likely to develop depressive symptoms than their IAD-free counterparts.
Another longitudinal study of high school students from Helsinki found that problematic internet usage and depressive symptoms may produce a positive feedback loop. Problematic internet usage is also associated with increased risk of substance abuse.
Social consequences:
The best-documented evidence of Internet addiction so far is time-disruption, which subsequently results in interference with regular social life, including academic, professional performance and daily routines. Some studies also reveal that IAD can lead to disruption of social relationships in Europe and Taiwan. It is, however, also noted by others that IAD is beneficial for peer relations in Taiwan.
Dr. Keith W. Beard (2005) states that "an individual is addicted when an individual's psychological state, which includes both mental and emotional states, as well as their scholastic, occupational and social interactions, is impaired by the overuse of [Internet]".
As a result of its complex nature, some scholars do not provide a definition of Internet addiction disorder and throughout time, different terms are used to describe the same phenomenon of excessive Internet use. Internet addiction disorder is used interchangeably with problematic Internet use, pathological Internet use, and Internet addictive disorder.
In some cases, this behavior is also referred to as Internet overuse, problematic computer use, compulsive Internet use, Internet abuse, harmful use of the Internet, and Internet dependency.
Signs and symptoms:
Physical symptoms:
Physical symptoms include a weakened immune system due to lack of sleep, loss of exercise, and increased risk for carpal tunnel syndrome and eye and back strain.
Symptoms of withdrawal might include agitation, depression, anger and anxiety when the person is away from technology. These psychological symptoms might even turn into physical symptoms such as rapid heartbeat, tense shoulders and shortness of breath.
Related disorders:
Online gambling addiction:
According to David Hodgins, a professor of psychology at the University of Calgary, online gambling is considered to be as serious as pathological gambling. It is known as an "isolated disorder" which means that those who have a gambling problem prefer to separate themselves from interruptions and distractions.
Because gambling is available online, it increases the opportunity for problem gamblers to indulge in gambling without social influences swaying their decisions. This is why this disorder has become more a problem at this date in time and is why it is so difficult to overcome. The opportunity to gamble online is almost always available in this century opposed to only having the opportunity in a public forum at casinos for example.
Online gambling has become quite popular especially with today's adolescents. Today's youth has a greater knowledge of modern software and search engines along with a greater need for extra money. So not only is it easier for them to find opportunities to gamble over any subject, but the incentive to be granted this money is desperately desired.
Online gaming addiction: (Internet gaming disorder)
Main article: Video game addiction
Video game addiction is a known issue around the world. Incidence and severity grew in the 2000s, with the advent of broadband technology, games allowing for the creation of avatars, 'second life' games, and MMORPGs (massive multiplayer online role playing games). World of Warcraft has the largest MMORPG community online and there have been a number of studies about the addictive qualities of the game.
Addicts of the game range from children to mature adults. A well-known example is Ryan van Cleave, a university professor whose life declined as he became involved in online gaming. Andrew Doan, a physician with a research background in neuroscience, battled his own addictions with video games, investing over 20,000 hours of playing games over a period of nine years.
Online gaming addiction may be considered in terms of B.F. Skinner's theory of operant conditioning, which claims that the frequency of a given behavior is directly linked to rewarding and punishment of that behavior. If a behavior is rewarded, it is more likely to be repeated. If it is punished, it becomes suppressed.
Orzack, a clinical psychologist at McLean Hospital in Massachusetts claims that 40 percent of World of Warcraft (WoW) players are addicted. Orzack says that the best way to optimize the desired behavior in the subject is to provide rewards for correct behavior, and then adjust the number of times the subject is required to exhibit that behavior before a reward is provided.
For instance, if a rat must press a bar to receive food, then it will press faster and more often if it does not know how many times it needs to press the bar. An equivalent in World of Warcraft would be purple (epic) loot drops.
Players in World of Warcraft will often spend weeks hunting for a special item which is based on a chance system, sometimes with only a 0.01% chance of it being dropped by a slain monster. The rarity of the item and difficulty of acquiring the item gives the player a status amongst their peers once they obtain the item.
Jim Rossignol, a finance journalist who reports on Internet gaming has described how he overcame his own addiction and channeled his compulsion into a desirable direction as a reporter of Internet gaming and gaming culture.
Pornography addiction (problematic Internet pornography use):
Main article: Pornography addiction
See also: Effects of pornography
Universally accepted diagnostic criteria do not exist for pornography addiction or problematic Internet pornography viewing. Pornography addiction is often defined operationally by the frequency of pornography viewing and negative consequences.
The only diagnostic criteria for a behavioral addiction in the current Diagnostic and Statistical Manual of Mental Disorders are for pathological gambling, and they are similar to those for substance abuse and dependence, such as preoccupation with the behavior, diminished ability to control the behavior, tolerance, withdrawal, and adverse psychosocial consequences.
Diagnostic criteria have been proposed for other behavioral addictions, and these are usually also based on established diagnoses for substance abuse and dependence.
A proposed diagnosis for hypersexual disorder includes pornography as a subtype of this disorder. It included such criteria as time consumed by sexual activity interfering with obligations, repetitive engagement in sexual activity in response to stress, repeated failed attempts to reduce these behaviors, and distress or impairment of life functioning.
A study on problematic Internet pornography viewing used the criteria of viewing Internet pornography more than three times a week during some weeks, and viewing causing difficulty in general life functioning.
According to the American Society of Addiction Medicine, some psychological and behavioral changes characteristic of addiction brain changes include addictive cravings, impulsiveness, weakened executive function, desensitization, and dysphoria. BOLD fMRI results have shown that individuals diagnosed with compulsive sexual behavior (CSB) show enhanced cue reactivity in brain regions associated traditionally with drug-cue reactivity.
These regions include the amygdala and the ventral striatum. Men without CSB who had a long history of viewing pornography exhibited a less intense response to pornographic images in the left ventral putamen, possibly suggestive of desensitization. ASAMs position is inconsistent with the American Association of Sex Educators, Counselors, and Therapists, who cite lack of strong evidence for such classification, describing ASAM as not informed by "accurate human sexuality knowledge".
Neuropsychopharmacological and psychological researches on pornography addiction conducted between 2015 and 2021 have concluded that most studies have been focused entirely or almost exclusively on men in anonymous settings, and the findings are contradicting.
Some researches support the idea that pornography addiction qualifies as a form of behavioral addiction into the umbrella construct of hypersexual behavior and/or a subset of compulsive sexual behavior (CSB), and should be treated as such, whereas others have detected the increased activation of ventral striatal reactivity in men for cues predicting erotic but not monetary rewards and cues signaling erotic pictures, therefore suggesting similarities between pornography addiction and conventional addiction disorders.
Some clinicians and support organizations recommend voluntary use of Internet content-control software, internet monitoring, or both, to manage problematic online pornography use.
Sex researcher Alvin Cooper and colleagues suggested several reasons for using filters as a therapeutic measure, including curbing accessibility that facilitates problematic behavior and encouraging clients to develop coping and relapse prevention strategies. Cognitive therapist Mary Anne Layden suggested that filters may be useful in maintaining environmental control.
Internet behavior researcher David Delmonico stated that, despite their limitations, filters may serve as a "frontline of protection."
Despite the fact that pornography is being indicted as a public health crisis in the United States and elsewhere, with problematic Internet and online pornography use reported to constitute an increasing burden in public mental health since the 2000s, psychopathological models and diagnostic criteria have lacked consensus, and the body of evidence on the effectiveness of therapeutic approaches is still scarce.
In consequence of the COVID-19 pandemic (2020-2021), problematic Internet pornography use and Internet addiction disorder have become difficult to cope for individuals who have adopted this lifestyle and have developed a dependence on these activities as an essential part of their lives, owing to elongated periods of staying at home due to self-isolation.
Communication addiction disorder (compulsive talking):
Main article: Communication addiction disorder
Communication addiction disorder (CAD) is a supposed behavioral disorder related to the necessity of being in constant communication with other people, even when there is no practical necessity for such communication. CAD has been linked to Internet addiction.
Users become addicted to the social elements of the Internet, such as Facebook and YouTube. Users become addicted to one-on-one or group communication in the form of social support, relationships, and entertainment. However, interference with these activities can result in conflict and guilt. This kind of addiction is called problematic social media use.
Social network addiction is a dependence of people by connection, updating, and control of their and their friend's social network page. For some people, in fact, the only important thing is to have a lot of friends in the network regardless if they are offline or only virtual; this is particularly true for teenagers as a reinforcement of egos.
Sometimes teenagers use social networks to show their idealized image to the others. However, other studies claim that people are using social networks to communicate their real personality and not to promote their idealized identity.
Virtual reality addiction:
Main article: Virtual reality addiction
Virtual-reality addiction is an addiction to the use of virtual reality or virtual, immersive environments. Currently, interactive virtual media (such as social networks) are referred to as virtual reality, whereas future virtual reality refers to computer-simulated, immersive environments or worlds.
Experts warn about the dangers of virtual reality, and compare the use of virtual reality (both in its current and future form) to the use of drugs, bringing with these comparisons the concern that, like drugs, users could possibly become addicted to virtual reality.
Video streaming addiction:
Main article: Television addiction
Video streaming addiction is an addiction to watching video content online. This can include TV shows, movies, short video clips and other content. Each person's experience is unique but people who have this addiction may also display addictive relationship with offline video content too (such as television, DVDs, VHS tapes, etc.) Addicts often display binge behavior.
With more development of binging sites such as Netflix, Stan, and Foxtel, more people start binging movies and TV shows everyday, only contributing to this addiction.
Risk factors:
Interpersonal difficulties:
It is argued that interpersonal difficulties such as introversion, social problems, and poor face-to-face communication skills often lead to internet addiction. Internet-based relationships offer a safe alternative for people with aforementioned difficulties to escape from the potential rejections and anxieties of interpersonal real-life contact.
Social support
Individuals who lack sufficient social connection and social support are found to run a higher risk of Internet addiction. They resort to virtual relationships and support to alleviate their loneliness. As a matter of fact, the most prevalent applications among Internet addicts are chat rooms, interactive games, instant messaging, or social media.
Some empirical studies reveal that conflict between parents and children and not living with mother significantly associated with IA after one year. Protective factors such as quality communication between parents and children and positive youth development are demonstrated, in turn, to reduce the risk of IA.
Psychological factors:
Prior addictive or psychiatric history are found to influence the likelihood of being addicted to the Internet. Some individuals with prior psychiatric problems such as depression and anxiety turn to compulsive behaviors to avoid the unpleasant emotions and situation of their psychiatric problems and regard being addicted to the Internet a safer alternative to substance addictive tendency.
But it is generally unclear from existing research which is the cause and which is the effect partially due to the fact that comorbidity is common among Internet addicts.
The most common co-morbidities that have been linked to IAD are major depression and attention deficit hyperactivity disorder (ADHD). The rate of ADHD and IAD associating is as high as 51.6%.
Internet addicts with no previous significant addictive or psychiatric history are argued to develop an addiction to some of the features of Internet use: anonymity, easy accessibility, and its interactive nature.
Neurobiological factors:
Like most other psychopathological conditions, Internet addiction belongs to the group of multifactorial polygenic disorders. For each specific case, there is a unique combination of inherited characteristics (nervous tissue structure, secretion, degradation, and reception of neuromediators), and many are extra-environment factors (family-related, social, and ethnic-cultural).
One of the main challenges in the development of the bio-psychosocial model of Internet addiction is to determine which genes and neuromediators are responsible for increased addiction susceptibility. This article incorporates text by Sergey Tereshchenko and Edward Kasparov available under the CC BY 4.0 license.
Other factors:
Parental educational level, age at first use of the Internet, and the frequency of using social networking sites and gaming sites are found to be positively associated with excessive Internet use among adolescents in some European countries, as well as in the USA.
Diagnosis:
Diagnosis of Internet addiction disorder is empirically difficult. Various screening instruments have been employed to detect Internet addiction disorder. Current diagnoses are faced with multiple obstacles.
Difficulties:
Given the newness of the Internet and the inconsistent definition of Internet addiction disorder, practical diagnosis is far from clear-cut. With the first research initiated by Kimberly S. Young in 1996, the scientific study of Internet addiction has merely existed for more than 20 years.
A few obstacles are present in creating an applicable diagnostic method for Internet addiction disorder.
- Wide and extensive use of the Internet: Diagnosing Internet addiction is often more complex than substance addiction as internet use has largely evolved into being an integral or necessary part of human lives. The addictive or problematic use of the internet is thus easily masked or justified. Also, the Internet is largely a pro-social, interactive, and information-driven medium, while other established addiction behaviors such as gambling are often seen as a single, antisocial behavior that has very little socially redeeming value. Many so-called Internet addicts do not suffer from the same damage to health and relationships that are common to established addictions.
- High comorbidity: Internet addiction is often accompanied by other psychiatric disorders such as personality disorder and intellectual disability. It is found that Internet addiction is accompanied by other DSM-IV diagnosis 86% of the time. In one study conducted in South Korea, 30% of the identified Internet addicts have accompanying symptoms such as anxiety or depression and another 30% have a second disorder such as attention deficit hyperactivity disorder (ADHD). Another study in South Korea found an average of 1.5 other diagnoses among adolescent internet addicts. Further, it is noted in the United States that many patients only resort to medical help when experiencing difficulties they attribute to other disorders. For many individuals, overuse or inappropriate use of the Internet is a manifestation of their depression, social anxiety disorders, impulse control disorders, or pathological gambling. It generally remains unclear from existing literature whether other psychiatric disorders is the cause or manifest of Internet addiction.
Despite the advocacy of categorizing Internet addiction as an established illness, neither DSM-IV (1995) nor DSM-5 (2013) considers Internet addiction as a mental disorder.
A subcategory of IAD, Internet gaming disorder is listed in DSM-5 as a condition that requires more research in order to be considered as a full disorder in May 2013. The WHO's draft 11th Revision of the International Classification of Diseases (ICD-11) scheduled for publication in 2018 also include gaming disorder. There is still considerable controversy over whether IAD should be included in the DSM-5 and recognized as a mental disease in general.
Screening instruments:
DSM-based instruments: Most of the criteria utilized by research are adaptations of listed mental disorders (e.g., pathological gambling) in the Statistical Manual of Mental Disorders (DSM) handbook.
Dr. Ivan K. Goldberg, who first broached the concept of Internet addiction, adopted a few criteria for IAD on the basis of DSM-IV, including “hoping to increase time on the network” and “dreaming about the network.”
By adapting the DSM-IV criteria for pathological gambling, Dr. Kimberly S. Young (1998) proposed one of the first integrated sets of criteria, Diagnostic Questionnaire (YDQ), to detect Internet addiction. A person who fulfills any five of the eight adapted criteria would be regarded as Internet addicted: Preoccupation with the Internet;
- A need for increased time spent online to achieve the same amount of satisfaction;
- Repeated efforts to curtail Internet use;
- Irritability, depression, or mood lability when Internet use is limited;
- Staying online longer than anticipated;
- Putting a job or relationship in jeopardy to use the Internet;
- Lying to others about how much time is spent online; and
- Using the Internet as a means of regulating mood.
While Young's YDQ assessment for IA has the advantage of simplicity and ease of use, Keith W. Beard and Eve M. Wolf (2001) further asserted that all of the first five (in the order above) and at least one of the final three criteria (in the order above) be met to delineate Internet addiction in order for a more appropriate and objective assessment.
Young further extended her eight-question YDQ assessment to the now most widely used Internet Addiction Test (IAT), which consists of 20 items with each on a five-point Likert scale.
Questions included on the IAT expand upon Young's earlier eight-question assessment in greater detail and include questions such as "Do you become defensive or secretive when anyone asks you what you do online?" and "Do you find yourself anticipating when you go online again?".
A complete list of questions can be found in Dr. Kimberly S. Young's 1998 book Caught in the Net: How to Recognize the Signs of Internet Addiction and A Winning Strategy for Recovery and Drs. Laura Widyanto and Mary McMurran's 2004 article titled The Psychometric Properties of the Internet Addiction Test.
The Test score ranges from 20 to 100 and a higher value indicates a more problematic use of the Internet:
- 20–39 = average Internet users,
- 40–69 = potentially problematic Internet users, and
- 70–100 = problematic Internet users.
Over time, a considerable number of screening instruments have been developed to diagnose Internet addiction, including:
- the Internet Addiction Test (IAT),
- the Internet-Related Addictive Behavior Inventory (IRABI),
- the Chinese Internet Addiction Inventory (CIAI),
- the Korean Internet Addiction Self-Assessment Scale (KS Scale),
- the Compulsive Internet Use Scale (CIUS),
- the Generalized Problematic Internet Use Scale (GPIUS),
- the Internet Consequences Scale (ICONS),
- and the Problematic Internet Use Scale (PIUS).
- Among others, the Internet Addiction Test (IAT) by Young (1998) exhibits good internal reliability and validity and has been used and validated worldwide as a screening instrument.
Although the various screening methods are developed from diverse contexts, four dimensions manifest themselves across all instruments:
- Excessive use: compulsive Internet use and excessive online time-use;
- Withdrawal symptoms: withdrawal symptoms including feelings such as depression and anger, given restricted Internet use;
- Tolerance: the need for better equipment, increased internet use, and more applications/software;
- Negative repercussions: Internet use caused negative consequences in various aspects, including problematic performance in social, academic, or work domains.
More recently, researchers Mark D. Griffiths (2000) and Dr. Jason C. Northrup and colleagues (2015) claim that Internet per se is simply the medium and that the people are in effect addicted to processes facilitated by the Internet.
Based on Young's Internet Addiction Test (IAT), Northrup and associates further decompose the internet addiction measure into four addictive processes:
- Online video game playing,
- online social networking,
- online sexual activity,
- and web surfing.
The Internet Process Addiction Test (IPAT) is created to measure the processes to which individuals are addicted.
Screening methods that heavily rely on DSM criteria have been accused of lacking consensus by some studies, finding that screening results generated from prior measures rooted in DSM criteria are inconsistent with each other. As a consequence of studies being conducted in divergent contexts, studies constantly modify scales for their own purposes, thereby imposing a further challenge to the standardization in assessing Internet addiction disorder.
Single-question instruments:
Some scholars and practitioners also attempt to define Internet addiction by a single question, typically the time-use of the Internet. The extent to which Internet use can cause negative health consequences is, however, not clear from such a measure. The latter of which is critical to whether IAD should be defined as a mental disorder.
Neuroimaging techniques:
Emergent neuroscience studies investigated the influence of problematic, compulsive use of the internet on the human brain.
Following anecdotal reports and the conclusion by Dr. Kimberly S. Young (1998), neuroimaging studies revealed that IAD contributes to structural and functional abnormalities in the human brain, similar to other behavioral and substance additions.
Therefore, objective non-invasive neuroimaging can contribute to the preliminary diagnosis and treatment of IAD.
Electroencephalography-based diagnosis:
Using Electroencephalography (EEG) readings allows identifying abnormalities in the electrical activity of the human brain caused by IAD.
Studies revealed that individuals suffering from IAD predominantly demonstrate increased activity in the theta and gamma band and decreased delta, alpha, and beta activity. Following these findings, studies identified a correlation between the differences in the EEG readings and the severity of IAD, as well as the extent of impulsivity and inattention.
Classification:
As many scholars have pointed out, the Internet serves merely as a medium through which tasks of divergent nature can be accomplished. Treating disparate addictive behaviors under the same umbrella term is highly problematic.
Dr. Kimberly S. Young (1999) asserts that Internet addiction is a broad term which can be decomposed into several subtypes of behavior and impulse control problems, namely, Cybersexual addiction: compulsive use of adult websites for cybersex and cyberporn (see Internet sex addiction)
- Cyber-relationship addiction: Over-involvement in online relationships
- Net compulsions: Obsessive online gambling, shopping or day-trading
- Information overload: Compulsive web surfing or database searches
- Computer addiction: Obsessive computer game playing (see Video game addiction)
For a more detailed description of related disorders please refer to the related disorders section above.
Treatment:
Current interventions and strategies used as treatments for Internet addiction stem from those practiced in substance abuse disorder. In the absence of "methodologically adequate research", treatment programs are not well corroborated. Psychosocial treatment is the approach most often applied. In practice, rehab centers usually devise a combination of multiple therapies.
Psychosocial treatment:
Cognitive behavioral therapy
The cognitive behavioral therapy with Internet addicts (CBT-IA) is developed in analogy to therapies for impulse control disorder.
Several key aspects are embedded in this therapy:
- Learning time management strategies;
- Recognizing the benefits and potential harms of the Internet;
- Increasing self-awareness and awareness of others and one's surroundings;
- Identifying "triggers" of Internet "binge behavior", such as particular Internet applications, emotional states, maladaptive cognitions, and life events;
- Learning to manage emotions and control impulses related to accessing the Internet, such as muscles or breathing relaxation training;
- Improving interpersonal communication and interaction skills;
- Improving coping styles;
- Cultivating interests in alternative activities.
Three phases are implemented in the CBT-IA therapy:
- Behavior modification to control Internet use: Examine both computer behavior and non-computer behavior and manage Internet addicts' time online and offline;
- Cognitive restructuring to challenge and modify cognitive distortions: Identify, challenge, and modify the rationalizations that justify excessive Internet use;
- Harm reduction therapy to address co-morbid issues: Address any co-morbid factors associated with Internet addiction, sustain recovery, and prevent relapse.
Symptom management of CBT-IA treatment has been found to sustain six months post-treatment.
Motivational interviewing:
The motivational interviewing approach is developed based on therapies for alcohol abusers. This therapy is a directive, patient-centered counseling style for eliciting behavior change through helping patients explore and resolve ambivalence with a respectful therapeutic manner. It does not, however, provide patients with solutions or problem solving until patients' decision to change behaviors.
Several key elements are embedded in this therapy:
Asking open-ended questions;
- Giving affirmations;
- Reflective listening
Other psychosocial treatment therapies include reality therapy, Naikan cognitive psychotherapy, group therapy, family therapy, and multimodal psychotherapy.
Medication:
IAD may be associated with a co-morbidity, so treating a related disorder may also help in the treatment of IAD. When individuals with IAD were treated with certain antidepressants, the time online was reduced by 65% and cravings of being online also decreased. The antidepressants that have been most successful are selective serotonin reuptake inhibitors (SSRIs) such as escitalopram and the atypical antidepressant bupropion.
A psychostimulant, methylphenidate, was also found to have beneficial effects. However, the available evidence on treatment of IAD is of very low quality at this time and well-designed trials are needed.
Prevalence:
Above: Different samples, methodologies, and screening instruments are employed across studies.
Terminology:
The notion of "Internet addictive disorder" was initially conjured up by Ivan K. Goldberg in 1995 as a joke to parody the complexity and rigidity of the American Psychiatric Association's (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM). In his first narration, Internet addictive disorder was described as having the symptoms of "important social or occupational activities that are given up or reduced because of Internet use", "fantasies or dreams about the Internet," and "voluntary or involuntary typing movements of the fingers."
The definition of Internet addiction disorder has troubled researchers ever since its inception. In general, no standardized definition has been provided despite that the phenomenon has received extensive public and scholar recognition. Below are some of the commonly used definitions.
In 1998, Jonathan J. Kandell defined Internet addiction as "a psychological dependence on the Internet, regardless of the type of activity once logged on."
English psychologist Mark D. Griffiths (1998) conceived Internet addiction as a subtype of broader technology addiction, and also a subtype of behavioral addictions.
Society:
Internet and Technology Addicts Anonymous:
Internet and Technology Addicts Anonymous (ITAA), founded in 2017, is a 12-step program supporting users coping with the problems resulting from compulsive internet and technology use.
Some common sub-addictions include smartphone addiction, binge watching addiction, and social media addiction. There are face to face meetings in some cities. Telephone / online meetings take place every day of the week, at various times (and in various languages) that allow people worldwide to attend.
Similar to 12-step fellowships such as Overeaters Anonymous, Workaholics Anonymous, or Sex and Love Addicts Anonymous, most members do not define sobriety as avoiding all technology use altogether. Instead, most ITAA members come up with their own definitions of abstinence or problem behaviors, such as not using the computer or internet at certain hours or locations or not going to certain websites or categories of websites that have proven problematic in the past.
Meetings provide a source of live support for people, to share struggles and victories, and to learn to better function in life once less of it is spent on problematic technology use.
NoSurf:
The NoSurf Reddit community maintains a list of resources and strategies helpful for people trying to decrease their internet usage. This includes lists of software programs that people use to control which sites they visit and when, as well as a discussion group that takes place on Discord.
Public concern:
Internet addiction has raised great public concern in Asia and some countries consider Internet addiction as one of the major issues that threatens public health, in particular among adolescents.
China:
Internet addiction is commonly referred to as "electronic opium" or "electronic heroin" in China. The government of the People's Republic of China was the first country to formally classify Internet addiction a clinical disorder by recognizing "Clinical Diagnostic Criteria for Internet Addiction" in 2008. The government has enacted several policies to regulate adolescents' Internet use, including limiting daily gaming time to 3 hours and requiring users' identification in online video games.
Mistreatment and abuse in China: In the absence of guidance from China's Health Ministry and a clear definition of Internet addiction, dubious treatment clinics have sprouted up in the country. As part of the treatment, some clinics and camps impose corporal punishment upon patients of Internet addiction and some conducted electroconvulsive therapy (ECT) against patients, the latter of which has caused wide public concern and controversy.
Several forms of mistreatment have been well-documented by news reports.
One of the most commonly used treatments for Internet-addicted adolescents in China is inpatient care, either in a legal or illegal camp. It is reported that children were sent to these camps against their will. Some are seized and bound by staff of the camp, some are drugged by their parents, and some are tricked into treatment.
In many camps and clinics, corporal punishment is frequently used in the treatment of Internet addiction disorder. The types of corporal punishment practiced include, but not limited to, kilometers-long hikes, intense squats, standing, starving, and confinement.
After physical abuse caused the death of an adolescent at a treatment camp in 2009, the Chinese government officially prohibited the use physical violence in such places. However, multiple cases of abuse and deaths at such facilities continue to be reported.
Among Internet addiction rehab centers that use corporal punishment in treatment, Yuzhang Academy in Nanchang, Jiangxi Province, is the most notorious. In 2017, the Academy was accused of using severe corporal punishment against students, the majority of which are Internet addicts. Former students claimed that the Academy hit problematic students with iron rulers, "whip them with finger-thick steel cables", and lock students in small cells week long. Several suicidal cases emerged under the great pressure.
In November 2017, the Academy stopped operating after extensive media exposure and police intervention.
Electroconvulsive therapy: In China, electroconvulsive therapy (ECT) is legally used for schizophrenia and mood disorders. Its use in treating adolescent Internet addicts has raised great public concern and stigmatized the legal use of ECT.
The most reported and controversial clinic treating Internet addiction disorder is perhaps the Linyi Psychiatric Hospital in Shandong Province. Its center for Internet addiction treatment was established in 2006 by Yang Yongxin.
Various interviews of Yongxin Yang confirm that Yang has created a special therapy, xingnao ("brain-waking") therapy, to treat Internet addiction. As part of the therapy, electroconvulsive therapy is implemented with currents of 1–5 milliampere. As Yang put it, the electroconvulsive therapy only involves sending a small current through the brain and will not harm the recipient.
As a psychiatric hospital, patients are deprived of personal liberty and are subject to electroconvulsive treatment at the will of hospital staffs. And before admission, parents have to sign contracts in which they deliver their guardianship of kids partially to the hospital and acknowledge that their kids will receive ECT.
Frequently, ECT is employed as a punishment method upon patients who breaks any of the center's rules, including "eating chocolate, locking the bathroom door, taking pills before a meal and sitting on Yang's chair without permission".
It is reported in a CCTV-12 segment that a DX-IIA electroconvulsive therapy machine is utilized to correct Internet addiction. The machine was, later on, revealed to be illegal, inapplicable to minor and can cause great pain and muscle spasm to recipients. Many former patients in the hospital later on stood out and reported that the ECT they received in the hospital was extremely painful, tore up their head, and even caused incontinence.
An Interview of the Internet addiction treatment center in Linyi Psychiatric Hospital is accessible via the following link. Since neither the safety nor the effectiveness of the method was clear, the Chinese Ministry of Health banned electroconvulsive therapy in treating Internet addiction disorder in 2009.
Drug: In Yang's clinic, patients are forced to take psychiatric medication[125] in addition to Jiewangyin, a type of medication invented by himself. Neither the effectiveness nor applicability of the medication has been assessed, however.
Physical abuse and death: At clinics and rehab centers, at least 12 cases of physical abuse have been revealed by media in the recent years including seven deaths.
In 2009, a 15-year-old, Senshan Deng, was found dead eight hours after being sent to an Internet-addiction center in Nanning, Guangxi Province. It is reported that the teenager was beaten by his trainers during his stay in the center.
In 2009, another 14-year-old teenager, Liang Pu, was taken to hospital with water in the lungs and kidney failure after a similar attack in Sichuan Province.
In 2014, a 19-year-old, Lingling Guo, died in an Internet-addiction center with multiple injuries on head and neck in Zhengzhou, Henan Province.
In 2016, after escaping from an Internet addiction rehab center, a 16-year-old girl tied and starved her mother to death in revenge of the being sent to treatment in Heilongjiang Province.
In August 2017, an 18-year-old boy, Li Ao, was found dead with 20 external scars and bruises two days after his parents sent him to a military-style boot camp in Fuyang city, Anhui Province.
South Korea:
Being almost universally connected to the Internet and boasting online gaming as a professional sport, South Korea deems Internet addiction one of the most serious social issues and describes it as a "national crisis". Nearly 80% of the South Korean population have smartphones.
According to government data, about two million of the country's population (less than 50 million) have Internet addiction problem, and approximately 68,000 10–19-year-old teenagers are addicted to the Internet, accounting for roughly 10% of the teenage population.
Even the very young generation are faced with the same problem: Approximately 40% of South Korean children between age three to five are using smartphones over three times per week. According to experts, if children are constantly stimulated by smartphones during infancy period, their brain will struggle to balance growth and the risk of Internet addiction.
It is believed that due to Internet addiction, many tragic events have happened in South Korea: A mother, tired of playing online games, killed her three-year-old son. A couple, obsessed with online child-raising games, left their young daughter die of malnutrition. A 15-year-old teenager killed his mother for not letting himself play online games and then committed suicide. One Internet gaming addict stabbed his sister after playing violent games.
Another addict killed one and injured seven others.
In response, the South Korea government has launched the first Internet prevention center in the world, the Jump Up Internet Rescue School, where the most severely addicted teens are treated with full governmental financial aid. As of 2007, the government has built a network of 140 Internet-addiction counseling centers besides treatment programs at around 100 hospitals.
Typically, counselor- and instructor-led music therapy and equine therapy and other real-life group activities including military-style obstacle courses and therapeutic workshops on pottery and drumming are used to divert IAs' attention and interest from screens.
In 2011, the Korean government introduced the "Shutdown law", also known as the "Cinderella Act", to prevent children under 16 years old from playing online games from midnight (12:00) to 6 a.m.
Japan:
In Japan, internet addiction disorder has manifested into the citizens primarily affecting the youth and adolescent population. In the male youth the internet addiction shows a trend in increased time in gaming on their devices while the female youth shows trends in social media use.
The smartphone and internet addiction in Japan has become detrimental to the society by affecting social interactions between people and their communication. They become used to interacting over the internet and their phones that it deteriorates some of their social skills over time.
Many cases of social withdrawal have been occurring in Japan since the late 1990's which inclines people to stay indoors most of the time. The term used for this is hikikomori, and it primarily affects the youth of Japan in that they are less inclined to leave their residences. Internet addiction can contribute to this effect because of how it diminishes social interactions and gives young people another reason to stay at home for longer.
Many of the hikikomori people in Japan are reported to have friends in their online games, so they will experience a different kind of social interaction which happens in a virtual space.
See also:
Terminology:
The notion of "Internet addictive disorder" was initially conjured up by Ivan K. Goldberg in 1995 as a joke to parody the complexity and rigidity of the American Psychiatric Association's (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM). In his first narration, Internet addictive disorder was described as having the symptoms of "important social or occupational activities that are given up or reduced because of Internet use", "fantasies or dreams about the Internet," and "voluntary or involuntary typing movements of the fingers."
The definition of Internet addiction disorder has troubled researchers ever since its inception. In general, no standardized definition has been provided despite that the phenomenon has received extensive public and scholar recognition. Below are some of the commonly used definitions.
In 1998, Jonathan J. Kandell defined Internet addiction as "a psychological dependence on the Internet, regardless of the type of activity once logged on."
English psychologist Mark D. Griffiths (1998) conceived Internet addiction as a subtype of broader technology addiction, and also a subtype of behavioral addictions.
Society:
Internet and Technology Addicts Anonymous:
Internet and Technology Addicts Anonymous (ITAA), founded in 2017, is a 12-step program supporting users coping with the problems resulting from compulsive internet and technology use.
Some common sub-addictions include smartphone addiction, binge watching addiction, and social media addiction. There are face to face meetings in some cities. Telephone / online meetings take place every day of the week, at various times (and in various languages) that allow people worldwide to attend.
Similar to 12-step fellowships such as Overeaters Anonymous, Workaholics Anonymous, or Sex and Love Addicts Anonymous, most members do not define sobriety as avoiding all technology use altogether. Instead, most ITAA members come up with their own definitions of abstinence or problem behaviors, such as not using the computer or internet at certain hours or locations or not going to certain websites or categories of websites that have proven problematic in the past.
Meetings provide a source of live support for people, to share struggles and victories, and to learn to better function in life once less of it is spent on problematic technology use.
NoSurf:
The NoSurf Reddit community maintains a list of resources and strategies helpful for people trying to decrease their internet usage. This includes lists of software programs that people use to control which sites they visit and when, as well as a discussion group that takes place on Discord.
Public concern:
Internet addiction has raised great public concern in Asia and some countries consider Internet addiction as one of the major issues that threatens public health, in particular among adolescents.
China:
Internet addiction is commonly referred to as "electronic opium" or "electronic heroin" in China. The government of the People's Republic of China was the first country to formally classify Internet addiction a clinical disorder by recognizing "Clinical Diagnostic Criteria for Internet Addiction" in 2008. The government has enacted several policies to regulate adolescents' Internet use, including limiting daily gaming time to 3 hours and requiring users' identification in online video games.
Mistreatment and abuse in China: In the absence of guidance from China's Health Ministry and a clear definition of Internet addiction, dubious treatment clinics have sprouted up in the country. As part of the treatment, some clinics and camps impose corporal punishment upon patients of Internet addiction and some conducted electroconvulsive therapy (ECT) against patients, the latter of which has caused wide public concern and controversy.
Several forms of mistreatment have been well-documented by news reports.
One of the most commonly used treatments for Internet-addicted adolescents in China is inpatient care, either in a legal or illegal camp. It is reported that children were sent to these camps against their will. Some are seized and bound by staff of the camp, some are drugged by their parents, and some are tricked into treatment.
In many camps and clinics, corporal punishment is frequently used in the treatment of Internet addiction disorder. The types of corporal punishment practiced include, but not limited to, kilometers-long hikes, intense squats, standing, starving, and confinement.
After physical abuse caused the death of an adolescent at a treatment camp in 2009, the Chinese government officially prohibited the use physical violence in such places. However, multiple cases of abuse and deaths at such facilities continue to be reported.
Among Internet addiction rehab centers that use corporal punishment in treatment, Yuzhang Academy in Nanchang, Jiangxi Province, is the most notorious. In 2017, the Academy was accused of using severe corporal punishment against students, the majority of which are Internet addicts. Former students claimed that the Academy hit problematic students with iron rulers, "whip them with finger-thick steel cables", and lock students in small cells week long. Several suicidal cases emerged under the great pressure.
In November 2017, the Academy stopped operating after extensive media exposure and police intervention.
Electroconvulsive therapy: In China, electroconvulsive therapy (ECT) is legally used for schizophrenia and mood disorders. Its use in treating adolescent Internet addicts has raised great public concern and stigmatized the legal use of ECT.
The most reported and controversial clinic treating Internet addiction disorder is perhaps the Linyi Psychiatric Hospital in Shandong Province. Its center for Internet addiction treatment was established in 2006 by Yang Yongxin.
Various interviews of Yongxin Yang confirm that Yang has created a special therapy, xingnao ("brain-waking") therapy, to treat Internet addiction. As part of the therapy, electroconvulsive therapy is implemented with currents of 1–5 milliampere. As Yang put it, the electroconvulsive therapy only involves sending a small current through the brain and will not harm the recipient.
As a psychiatric hospital, patients are deprived of personal liberty and are subject to electroconvulsive treatment at the will of hospital staffs. And before admission, parents have to sign contracts in which they deliver their guardianship of kids partially to the hospital and acknowledge that their kids will receive ECT.
Frequently, ECT is employed as a punishment method upon patients who breaks any of the center's rules, including "eating chocolate, locking the bathroom door, taking pills before a meal and sitting on Yang's chair without permission".
It is reported in a CCTV-12 segment that a DX-IIA electroconvulsive therapy machine is utilized to correct Internet addiction. The machine was, later on, revealed to be illegal, inapplicable to minor and can cause great pain and muscle spasm to recipients. Many former patients in the hospital later on stood out and reported that the ECT they received in the hospital was extremely painful, tore up their head, and even caused incontinence.
An Interview of the Internet addiction treatment center in Linyi Psychiatric Hospital is accessible via the following link. Since neither the safety nor the effectiveness of the method was clear, the Chinese Ministry of Health banned electroconvulsive therapy in treating Internet addiction disorder in 2009.
Drug: In Yang's clinic, patients are forced to take psychiatric medication[125] in addition to Jiewangyin, a type of medication invented by himself. Neither the effectiveness nor applicability of the medication has been assessed, however.
Physical abuse and death: At clinics and rehab centers, at least 12 cases of physical abuse have been revealed by media in the recent years including seven deaths.
In 2009, a 15-year-old, Senshan Deng, was found dead eight hours after being sent to an Internet-addiction center in Nanning, Guangxi Province. It is reported that the teenager was beaten by his trainers during his stay in the center.
In 2009, another 14-year-old teenager, Liang Pu, was taken to hospital with water in the lungs and kidney failure after a similar attack in Sichuan Province.
In 2014, a 19-year-old, Lingling Guo, died in an Internet-addiction center with multiple injuries on head and neck in Zhengzhou, Henan Province.
In 2016, after escaping from an Internet addiction rehab center, a 16-year-old girl tied and starved her mother to death in revenge of the being sent to treatment in Heilongjiang Province.
In August 2017, an 18-year-old boy, Li Ao, was found dead with 20 external scars and bruises two days after his parents sent him to a military-style boot camp in Fuyang city, Anhui Province.
South Korea:
Being almost universally connected to the Internet and boasting online gaming as a professional sport, South Korea deems Internet addiction one of the most serious social issues and describes it as a "national crisis". Nearly 80% of the South Korean population have smartphones.
According to government data, about two million of the country's population (less than 50 million) have Internet addiction problem, and approximately 68,000 10–19-year-old teenagers are addicted to the Internet, accounting for roughly 10% of the teenage population.
Even the very young generation are faced with the same problem: Approximately 40% of South Korean children between age three to five are using smartphones over three times per week. According to experts, if children are constantly stimulated by smartphones during infancy period, their brain will struggle to balance growth and the risk of Internet addiction.
It is believed that due to Internet addiction, many tragic events have happened in South Korea: A mother, tired of playing online games, killed her three-year-old son. A couple, obsessed with online child-raising games, left their young daughter die of malnutrition. A 15-year-old teenager killed his mother for not letting himself play online games and then committed suicide. One Internet gaming addict stabbed his sister after playing violent games.
Another addict killed one and injured seven others.
In response, the South Korea government has launched the first Internet prevention center in the world, the Jump Up Internet Rescue School, where the most severely addicted teens are treated with full governmental financial aid. As of 2007, the government has built a network of 140 Internet-addiction counseling centers besides treatment programs at around 100 hospitals.
Typically, counselor- and instructor-led music therapy and equine therapy and other real-life group activities including military-style obstacle courses and therapeutic workshops on pottery and drumming are used to divert IAs' attention and interest from screens.
In 2011, the Korean government introduced the "Shutdown law", also known as the "Cinderella Act", to prevent children under 16 years old from playing online games from midnight (12:00) to 6 a.m.
Japan:
In Japan, internet addiction disorder has manifested into the citizens primarily affecting the youth and adolescent population. In the male youth the internet addiction shows a trend in increased time in gaming on their devices while the female youth shows trends in social media use.
The smartphone and internet addiction in Japan has become detrimental to the society by affecting social interactions between people and their communication. They become used to interacting over the internet and their phones that it deteriorates some of their social skills over time.
Many cases of social withdrawal have been occurring in Japan since the late 1990's which inclines people to stay indoors most of the time. The term used for this is hikikomori, and it primarily affects the youth of Japan in that they are less inclined to leave their residences. Internet addiction can contribute to this effect because of how it diminishes social interactions and gives young people another reason to stay at home for longer.
Many of the hikikomori people in Japan are reported to have friends in their online games, so they will experience a different kind of social interaction which happens in a virtual space.
See also:
- Addictive personality
- Cyberslacking
- Criticism of Facebook
- Digital addict
- Digital detox
- Digital media use and mental health
- Gaming disorder
- Instagram's impact on people
- List of repetitive strain injury software (i.e. break reminders)
- Media multitasking
- Pornography addiction
- Procrastination
- Soft addiction
- Underearners Anonymous
- Workaholic
Alcoholics Anonymous and the Betty Ford Center
- YouTube Video: Does Alcoholics Anonymous Work? (Stanford Study)
- YouTube Video: What are the 12 Steps of AA?
- YouTube Video: Betty Ford's Lecture on Addiction and Recovery (Dec 13, 2019: Mrs. Betty Ford shares her story of drug and alcohol recovery with patients at the Betty Ford Center.)
Alcoholics Anonymous:
Alcoholics Anonymous (AA) is an international mutual aid fellowship of alcoholics dedicated to abstinence-based recovery from alcoholism through its spiritually-inclined Twelve Step program.
Following its Twelve Traditions, AA is non-professional, non-denominational, as well as apolitical and unaffiliated. In 2020 AA estimated its worldwide membership to be over two million with 75% of those in the U.S. and Canada.
AA has maintained neutrality towards the disease model of alcoholism though its program is sympathetic to it, but its wider acceptance has been partly due to many AA members independently promulgating it.
Regarding its effectiveness, a recent scientific review has shown that AA does as well or better than clinical interventions or no treatment at all; in particular, AA produces better abstinence rates at lower medical costs.
1935 is marked by AA as its starting year when a newly sober Bill Wilson (Bill W.) first commiserated with the alcoholic Bob Smith (Dr. Bob) and brought him into AA’s precursor the Christian revivalist Oxford Group.
Leaving the Oxford Group to form a fellowship of alcoholics only, Wilson and Smith, along with other early members, wrote Alcoholics Anonymous: The Story of How More Than One Hundred Men Have Recovered From Alcoholism, from which AA acquired its name.
Published in 1939 and commonly called "the Big Book", it contains AA's Twelve Step recovery program. Later editions included the Twelve Traditions, first adopted in 1946 to formalize and unify the fellowship as a benign anarchy.
The Twelve Steps are presented as a suggested self-improvement program of initially admitting powerlessness over alcohol and acknowledging its damage, the listing of and striving to correct personal failings and the making of amends for past misdeeds. To stay recovered, they suggest maintained spiritual development and the taking of other alcoholics through the Steps.
Though not explicitly suggested, the latter is often done by sponsoring other alcoholics. The Steps do urge submission to the will of God—"as we understood Him"—but are accepting and accommodating to the practices and convictions of other spiritual persuasions as well as those of non-theist members.
The Twelve Traditions are AA's guidelines for members, groups and its non-governing upper echelons. Besides making a desire to stop drinking as the only requirement for membership, the Traditions advise against dogma, hierarchies and involvement in public controversies while mindful that helping others recover from alcoholism is AA’s primary purpose.
Without threat of retribution or means of enforcement, the Traditions urge members to remain anonymous in public media. They also wish that members or groups to not use AA to gain wealth, property or prestige. Within AA, groups are autonomous, self-supporting through members’ voluntary contributions and obliged to reject outside contributions.
Externally, no AA entity can represent AA as affiliated with or in support of other organizations or causes.
With AA's permission, subsequent fellowships such as Narcotics Anonymous and Gamblers Anonymous have adopted and adapted the Twelve Steps and the Twelve Traditions to their addiction recovery programs.
Click on any of the following blue hyperlinks for more about Alcoholics Anonymou:
The Betty Ford Center:
The Betty Ford Center (BFC) is a non-profit, residential treatment center for persons with substance dependence in Rancho Mirage, California. It offers inpatient, outpatient, and residential day treatment for alcohol and other drug addictions, as well as prevention and education programs for family and children.
The Betty Ford Center, which is adjacent to Eisenhower Medical Center but is under a separate license to practice, has 100 inpatient beds available on their campus and additional lodging for 84 clients in the Residential Day Treatment program. The Betty Ford Center opened on October 4, 1982.
History:
The center was co-founded by former U.S. First Lady Betty Ford, Leonard Firestone and Dr. James West in 1982. West also served as the Betty Ford Center's first medical director from 1982 until 1989. He left that position to become the Betty Ford Center's director of outpatient services.
Betty Ford's decision to undertake such a project followed on the heels of her own battle with alcohol dependence and diazepam addiction and release from the Long Beach Naval Hospital.
The Betty Ford Center merged with Hazelden Foundation on February 10, 2014, to create the Hazelden Betty Ford Foundation.
In 2015, the Betty Ford Center opened an outpatient addiction treatment clinic in West Los Angeles.
See also:
More about Betty Ford:
Elizabeth Anne Ford (Bloomer; formerly Warren; April 8, 1918 – July 8, 2011) was the first lady of the United States from 1974 to 1977, as the wife of President Gerald Ford. As first lady, she was active in social policy and set a precedent as a politically active presidential spouse. Ford also served as the second lady of the United States from 1973 to 1974 when her husband was vice president.
Throughout her husband's term in office, she maintained high approval ratings and was considered to be an influential first lady. Ford was noted for raising breast cancer awareness following her 1974 mastectomy. In addition, she was a passionate supporter of the Equal Rights Amendment (ERA).
As a supporter of abortion rights and a leader in the women's rights movement, she gained fame as one of the most candid first ladies in history, commenting on the hot-button issues of the time, such as feminism, equal pay, the Equal Rights Amendment, sex, drugs, abortion, and gun control. Surveys of historians conducted by the Siena College Research Institute have shown that historians regard Ford to be among the best and most courageous American first ladies.
Following her White House years, she continued to lobby for the ERA and remained active in the feminist movement. Soon after leaving office, she raised awareness of addiction when she sought help for and publicly disclosed her long-running struggle with alcoholism and substance abuse.
After recovering, she founded and served as the first chair of the board of directors of the Betty Ford Center for substance abuse and addiction (see preceding topic about the Betty Ford Center).
Ford also became involved in causes related to HIV/AIDS. For years after leaving the White House, Ford continued to enjoy great influence and popularity, continuing to rank in the top-ten of Gallup's annual most admired woman poll every year through 1991.
Ford was awarded the Presidential Medal of Freedom by George H. W. Bush in 1991. She was also awarded the Congressional Gold Medal as a co-recipient with President Ford in 1998.
Click here for more about Betty Ford
Alcoholics Anonymous (AA) is an international mutual aid fellowship of alcoholics dedicated to abstinence-based recovery from alcoholism through its spiritually-inclined Twelve Step program.
Following its Twelve Traditions, AA is non-professional, non-denominational, as well as apolitical and unaffiliated. In 2020 AA estimated its worldwide membership to be over two million with 75% of those in the U.S. and Canada.
AA has maintained neutrality towards the disease model of alcoholism though its program is sympathetic to it, but its wider acceptance has been partly due to many AA members independently promulgating it.
Regarding its effectiveness, a recent scientific review has shown that AA does as well or better than clinical interventions or no treatment at all; in particular, AA produces better abstinence rates at lower medical costs.
1935 is marked by AA as its starting year when a newly sober Bill Wilson (Bill W.) first commiserated with the alcoholic Bob Smith (Dr. Bob) and brought him into AA’s precursor the Christian revivalist Oxford Group.
Leaving the Oxford Group to form a fellowship of alcoholics only, Wilson and Smith, along with other early members, wrote Alcoholics Anonymous: The Story of How More Than One Hundred Men Have Recovered From Alcoholism, from which AA acquired its name.
Published in 1939 and commonly called "the Big Book", it contains AA's Twelve Step recovery program. Later editions included the Twelve Traditions, first adopted in 1946 to formalize and unify the fellowship as a benign anarchy.
The Twelve Steps are presented as a suggested self-improvement program of initially admitting powerlessness over alcohol and acknowledging its damage, the listing of and striving to correct personal failings and the making of amends for past misdeeds. To stay recovered, they suggest maintained spiritual development and the taking of other alcoholics through the Steps.
Though not explicitly suggested, the latter is often done by sponsoring other alcoholics. The Steps do urge submission to the will of God—"as we understood Him"—but are accepting and accommodating to the practices and convictions of other spiritual persuasions as well as those of non-theist members.
The Twelve Traditions are AA's guidelines for members, groups and its non-governing upper echelons. Besides making a desire to stop drinking as the only requirement for membership, the Traditions advise against dogma, hierarchies and involvement in public controversies while mindful that helping others recover from alcoholism is AA’s primary purpose.
Without threat of retribution or means of enforcement, the Traditions urge members to remain anonymous in public media. They also wish that members or groups to not use AA to gain wealth, property or prestige. Within AA, groups are autonomous, self-supporting through members’ voluntary contributions and obliged to reject outside contributions.
Externally, no AA entity can represent AA as affiliated with or in support of other organizations or causes.
With AA's permission, subsequent fellowships such as Narcotics Anonymous and Gamblers Anonymous have adopted and adapted the Twelve Steps and the Twelve Traditions to their addiction recovery programs.
Click on any of the following blue hyperlinks for more about Alcoholics Anonymou:
- History
- The Big Book, the Twelve Steps, and the Twelve Traditions
- Organization and finances
- Program
- Spirituality
- Disease concept of alcoholism
- Canadian and United States demographics
- Relationship with institutions
- Effectiveness
- Criticism
- Literature
- AA in media
- See also:
- Adult Children of Alcoholics
- Al-Anon/Alateen
- Calix Society
- Community reinforcement approach and family training (CRAFT)
- Drug addiction recovery groups
- Drug rehabilitation
- Group psychotherapy
- List of twelve-step groups
- Long-term effects of alcohol
- Recovery approach
- Short-term effects of alcohol consumption
- Stepping Stones (house), home of Bill W.
- Washingtonian movement
- German Lopez (2 January 2018). "Why some people swear by Alcoholics Anonymous — and others despise it".
- Scott Alexander (24 October 2014). "Alcoholics Anonymous: Much More Than You Wanted To Know". Archived from the original on 24 June 2020.
- Official website
- A History of Agnostic Groups in AA
- Reproduction of the 1938 Original Manuscript of Alcoholics Anonymous
The Betty Ford Center:
The Betty Ford Center (BFC) is a non-profit, residential treatment center for persons with substance dependence in Rancho Mirage, California. It offers inpatient, outpatient, and residential day treatment for alcohol and other drug addictions, as well as prevention and education programs for family and children.
The Betty Ford Center, which is adjacent to Eisenhower Medical Center but is under a separate license to practice, has 100 inpatient beds available on their campus and additional lodging for 84 clients in the Residential Day Treatment program. The Betty Ford Center opened on October 4, 1982.
History:
The center was co-founded by former U.S. First Lady Betty Ford, Leonard Firestone and Dr. James West in 1982. West also served as the Betty Ford Center's first medical director from 1982 until 1989. He left that position to become the Betty Ford Center's director of outpatient services.
Betty Ford's decision to undertake such a project followed on the heels of her own battle with alcohol dependence and diazepam addiction and release from the Long Beach Naval Hospital.
The Betty Ford Center merged with Hazelden Foundation on February 10, 2014, to create the Hazelden Betty Ford Foundation.
In 2015, the Betty Ford Center opened an outpatient addiction treatment clinic in West Los Angeles.
See also:
- Hazelden Betty Ford Foundation official website
- U.S. Geological Survey Geographic Names Information System: Betty Ford Center at Eisenhower
More about Betty Ford:
Elizabeth Anne Ford (Bloomer; formerly Warren; April 8, 1918 – July 8, 2011) was the first lady of the United States from 1974 to 1977, as the wife of President Gerald Ford. As first lady, she was active in social policy and set a precedent as a politically active presidential spouse. Ford also served as the second lady of the United States from 1973 to 1974 when her husband was vice president.
Throughout her husband's term in office, she maintained high approval ratings and was considered to be an influential first lady. Ford was noted for raising breast cancer awareness following her 1974 mastectomy. In addition, she was a passionate supporter of the Equal Rights Amendment (ERA).
As a supporter of abortion rights and a leader in the women's rights movement, she gained fame as one of the most candid first ladies in history, commenting on the hot-button issues of the time, such as feminism, equal pay, the Equal Rights Amendment, sex, drugs, abortion, and gun control. Surveys of historians conducted by the Siena College Research Institute have shown that historians regard Ford to be among the best and most courageous American first ladies.
Following her White House years, she continued to lobby for the ERA and remained active in the feminist movement. Soon after leaving office, she raised awareness of addiction when she sought help for and publicly disclosed her long-running struggle with alcoholism and substance abuse.
After recovering, she founded and served as the first chair of the board of directors of the Betty Ford Center for substance abuse and addiction (see preceding topic about the Betty Ford Center).
Ford also became involved in causes related to HIV/AIDS. For years after leaving the White House, Ford continued to enjoy great influence and popularity, continuing to rank in the top-ten of Gallup's annual most admired woman poll every year through 1991.
Ford was awarded the Presidential Medal of Freedom by George H. W. Bush in 1991. She was also awarded the Congressional Gold Medal as a co-recipient with President Ford in 1998.
Click here for more about Betty Ford
Recreational Drug Use
- YouTube Video: 90's "This is Your Brain on Drugs" Commercial – Extended Cut
- YouTube Video: Defining Psychedelic Drugs
- YouTube Video: Psychedelics: The scientific renaissance of mind-altering drugs | Sam Harris, Michael Pollan & more
[Your WebHost: the following topic is comprehensive, perhaps to the point that some readers interpret parts to be encouraging drug and/or alcohol use. That is not the case. Just as an example of the harm done to celebrities you might know, click here.]
Recreational drug use indicates the use of one or more psychoactive drugs to induce an altered state of consciousness either for pleasure or for some other casual purpose or pastime by modifying the perceptions, feelings, and emotions of the user.
When a psychoactive drug enters the user's body, it induces an intoxicating effect.
Generally, recreational drugs are divided into three categories:
In popular practice, recreational drug use generally is a tolerated social behaviour,[ rather than perceived as the medical condition of self-medication. However, heavy use of some drugs is socially stigmatized.
Many people also use prescribed and controlled depressants such as opioids, as well as opiates and benzodiazepines.
Common recreational drugs include:
What controlled substances are considered generally unlawful to possess varies by country, but usually includes:
In 2015, it was estimated that about 5% of people worldwide aged 15 to 65 (158 million to 351 million) had used controlled drugs at least once.
Reasons for use:
Further information:
Many researchers have explored the etiology of recreational drug use. Some of the most common theories are:
There has not been agreement around any one single cause. Instead, experts tend to apply the biopsychosocial model. Any number of these factors are likely to influence an individual's drug use as they are not mutually exclusive.
Regardless of genetics, mental health, or traumatic experiences, social factors play a large role in exposure to and availability of certain types of drugs and patterns of drug use.
According to addiction researcher Martin A. Plant, many people go through a period of self-redefinition before initiating recreational drug use. They tend to view using drugs as part of a general lifestyle that involves belonging to a subculture that they associate with heightened status and the challenging of social norms.
Plant states: "From the user's point of view there are many positive reasons to become part of the milieu of drug taking. The reasons for drug use appear to have as much to do with needs for friendship, pleasure and status as they do with unhappiness or poverty. Becoming a drug taker, to many people, is a positive affirmation rather than a negative experience".
Evolution:
Main article: Evolutionary models of human drug use
Anthropological research has suggested that humans "may have evolved to counter-exploit plant neurotoxins". The ability to use botanical chemicals to serve the function of endogenous neurotransmitters may have improved survival rates, conferring an evolutionary advantage.
A typically restrictive prehistoric diet may have emphasised the apparent benefit of consuming psychoactive drugs, which had themselves evolved to imitate neurotransmitters.
Chemical–ecological adaptations, and the genetics of hepatic enzymes, particularly cytochrome P450, have led researchers to propose that "humans have shared a co-evolutionary relationship with psychotropic plant substances that is millions of years old."
Health risks:
Main articles: Further information:
Severity and type of risks that come with recreational drug use vary widely with the drug in question and the amount being used. There are many factors in the environment and within the user that interact with each drug differently.
Overall, some studies suggest that alcohol is one of the most dangerous of all recreational drugs; only heroin, crack cocaine, and methamphetamine are judged to be more harmful. Alcoholic drinks, tobacco products and other nicotine-based products (e.g., electronic cigarettes), and cannabis are regarded by various medical professionals to be the most common and widespread gateway drugs.
In the United States, Australia, and New Zealand, the general onset of drinking alcohol, tobacco smoking, cannabis smoking, and consumption of multiple drugs among young people most frequently occurs during adolescence and within school settings (middle school and secondary school).
Scientific studies which focus on a low–moderate level of alcohol consumption, particularly of red wine, have concluded that there can be substantial health benefits from its use, such as decreased risk of cardiovascular diseases, stroke, and cognitive decline. This claim has been disputed.
Researcher David Nutt stated that these studies showing benefits for "moderate" alcohol consumption lacked control for the variable of what the subjects were drinking, beforehand.
Experts in the United Kingdom have suggested that some psychoactive drugs that may be causing less harm to fewer users (although they are also used less frequently in the first place) include cannabis, psilocybin mushrooms, LSD, and MDMA. However, these drugs are not without their own particular risks and side effects.
Drug harmfulness:
Drug harmfulness is defined as the degree to which a psychoactive drug is harmful to a user and is measured in various ways, such as by addictiveness and the potential for physical harm.
More harmful drugs are called "hard drugs", and less harmful drugs are called "soft drugs". The term "soft drug" is considered controversial by its critics as it may imply that soft drugs cause no or insignificant harm.
Responsible use:
Main article: Responsible drug use
The concept of "responsible drug use" is that a person can use drugs recreationally or otherwise with reduced or eliminated risk of negatively affecting other aspects of one's life or other people's lives. Advocates of this philosophy point to the many well-known artists and intellectuals who have used drugs, experimentally or otherwise, with few detrimental effects on their lives. Responsible drug use becomes problematic only when the use of the substance significantly interferes with the user's daily life.
Responsible drug use advocates that users should not take drugs at the same time as activities such as driving, swimming, operating machinery, or other activities that are unsafe without a sober state. Responsible drug use is emphasized as a primary prevention technique in harm-reduction drug policies.
Harm-reduction policies were popularized in the late 1980s, although they began in the 1970s counter-culture, when cartoons explaining responsible drug use and the consequences of irresponsible drug use were distributed to users.
Another issue is that the illegality of drugs in itself also causes social and economic consequences for those using them—the drugs may be "cut" with adulterants and the purity varies wildly, making overdoses more likely—and legalization of drug production and distribution would reduce these and other dangers of illegal drug use.
Harm reduction seeks to minimize the harm that can occur through the use of various drugs, whether legal (e.g., alcohol and nicotine), or illegal (e.g., heroin and cocaine). For example, people who take drugs intravenously (cocaine, heroin) can minimize harm to both themself and members of the community through proper injecting technique, using new needles and syringes each time, and proper disposal of all injecting equipment.
Prevention:
Main articles: Harm reduction and Preventive healthcare
In efforts to curtail recreational drug use, governments worldwide introduced several laws prohibiting the possession of almost all varieties of recreational drugs during the 20th century. The West's "War on Drugs" however, is now facing increasing criticism. Evidence is insufficient to tell if behavioral interventions help prevent recreational drug use in children.
One in four adolescents has used an illegal drug and one in ten of those adolescents who need addiction treatment get some type of care. School-based programs are the most commonly used method for drug use education; however, the success rates of these intervention programs is highly dependent on the commitment of participants and is limited in general. Studies have also shown that home intervention is also effective in decreasing the appeal of drugs.
Demographics:
Further information: Illegal drug trade, Opioid epidemic, and Prohibition of drugs
Australia:
Further information: Alcoholism in rural Australia
Alcohol is the most widely used drug in Australia. 86.2% of Australians aged 12 years and over have consumed alcohol at least once in their lifetime, compared to 34.8% of Australians aged 12 years and over who have used cannabis at least once in their lifetime.
United States:
Further information:
From the mid-19th century to the 1930s, American physicians prescribed Cannabis sativa as a prescription drug for various medical conditions.
In the 1960s, the counterculture movement introduced the use of psychoactive drugs, including cannabis. Young adults and college students reported the recreational prevalence of cannabis, among other drugs, at 20-25% while the cultural mindset of using was open and curious.
In 1969, the FBI reported that between the years 1966 and 1968, the number of arrests for marijuana possession, which had been outlawed throughout the United States under Marijuana Tax Act of 1937, had increased by 98%.
Despite acknowledgement that drug use was greatly growing among America's youth during the late 1960s, surveys have suggested that only as much as 4% of the American population had ever smoked marijuana by 1969. By 1972, however, that number would increase to 12%. That number would then double by 1977.
The Controlled Substances Act of 1970 classified marijuana along with heroin and LSD as a Schedule I drug, i.e., having the relatively highest abuse potential and no accepted medical use.
Most marijuana at that time came from Mexico, but in 1975 the Mexican government agreed to eradicate the crop by spraying it with the herbicide paraquat, raising fears of toxic side effects. Colombia then became the main supplier.
The "zero tolerance" climate of the Reagan and Bush administrations (1981–93) resulted in passage of strict laws and mandatory sentences for possession of marijuana. The "War on Drugs" thus brought with it a shift from reliance on imported supplies to domestic cultivation (particularly in Hawaii and California).
Beginning in 1982, the Drug Enforcement Administration turned increased attention to marijuana farms in the United States, and there was a shift to the indoor growing of plants specially developed for small size and high yield.
After over a decade of decreasing use, marijuana smoking began an upward trend once more in the early 1990s, especially among teenagers, but by the end of the decade this upswing had leveled off well below former peaks of use.
Society and culture:
Main articles: Further information:
Many movements and organizations are advocating for or against the liberalization of the use of recreational drugs, most notably regarding the legalization of marijuana and cannabinoids for medical and/or recreational use.
Subcultures have emerged among users of recreational drugs, as well as alternative lifestyles and social movements among those who abstain from them, such as teetotalism and "straight edge".
Since the early 2000s, medical professionals have acknowledged and addressed the problem of the increasing consumption of alcoholic drinks and club drugs (such as:
Studies have shown that adolescents are more likely than young adults to use multiple drugs, and the consumption of club drugs is highly associated with the presence of criminal behaviors and recent alcohol abuse or dependence.
The prevalence of recreational drugs in human societies is widely reflected in fiction, entertainment, and the arts, subject to prevailing laws and social conventions.
For instance, in the music industry, the musical genres hip hop, hardcore rap, and trap, alongside their derivative subgenres and subcultures, are most notorious for having continuously celebrated and promoted drug trafficking, gangster lifestyle, and consumption of drugs and alcohol since their inception in the United States during the late 1980s–early 1990s.
In video games, for example, drugs are portrayed in a variety of ways: including power-ups , e.g.,
In 1997's Fallout, drugs ("chems" in the game) can fill the role of any above mentioned. Drug trafficking, gang rivalries, and their related criminal underworld also play a big part in the best-selling Grand Theft Auto video game franchise.
Common recreational drugs:
The following substances are commonly used recreationally:
Routes of administration:
Drugs are often associated with a particular route of administration. Many drugs can be consumed in more than one way. For example, marijuana can be swallowed like food or smoked, and cocaine can be "sniffed" in the nostrils, injected, or, with various modifications, smoked.
Many drugs are taken through various routes. Intravenous route is the most efficient, but also one of the most dangerous. Nasal, rectal, inhalation and smoking are safer. The oral route is one of the safest and most comfortable, but of little bioavailability.
Types:
Depressants:
Further information: Depressant
Depressants are psychoactive drugs that temporarily diminish the function or activity of a specific part of the body or mind.
Colloquially, depressants are known as "downers", and users generally take them to feel more relaxed and less tense. Examples of these kinds of effects may include anxiolysis, sedation, and hypotension.
Depressants are widely used throughout the world as prescription medicines and as illicit substances. When these are used, effects may include:
Depressants exert their effects through a number of different pharmacological mechanisms, the most prominent of which include potentiation of GABA or opioid activity, and inhibition of adrenergic, histamine or acetylcholine activity. Some are also capable of inducing feelings of euphoria. The most widely used depressant by far is alcohol (i.e. ethanol).
Stimulants or "uppers", such as amphetamines or cocaine, which increase mental or physical function, have an opposite effect to depressants.
Depressants, in particular alcohol, can precipitate psychosis. A 2019 systematic review and meta-analysis by Murrie et al. found that the rate of transition from opioid, alcohol and sedative induced psychosis to schizophrenia was 12%, 10% and 9% respectively.
Antihistamines:
Further information: Antihistamine
Antihistamines (or "histamine antagonists") inhibit the release or action of histamine. "Antihistamine" can be used to describe any histamine antagonist, but the term is usually reserved for the classical antihistamines that act upon the H1 histamine receptor.
Antihistamines are used as treatment for allergies. Allergies are caused by an excessive response of the body to allergens, such as the pollen released by grasses and trees. An allergic reaction causes release of histamine by the body. Other uses of antihistamines are to help with normal symptoms of insect stings even if there is no allergic reaction.
Their recreational appeal exists mainly due to their anticholinergic properties, that induce anxiolysis and, in some cases such as diphenhydramine, chlorpheniramine, and orphenadrine, a characteristic euphoria at moderate doses. High dosages taken to induce recreational drug effects may lead to overdoses.
Antihistamines are also consumed in combination with alcohol, particularly by youth who find it hard to obtain alcohol. The combination of the two drugs can cause intoxication with lower alcohol doses.
Hallucinations and possibly delirium resembling the effects of Datura stramonium can result if the drug is taken in much higher than therapeutic doses. Antihistamines are widely available over the counter at drug stores (without a prescription), in the form of allergy medication and some cough medicines. They are sometimes used in combination with other substances such as alcohol.
The most common unsupervised use of antihistamines in terms of volume and percentage of the total is perhaps in parallel to the medicinal use of some antihistamines to extend and intensify the effects of opioids and depressants.
The most commonly used are hydroxyzine, mainly to extend a supply of other drugs, as in medical use, and the above-mentioned ethanolamine and alkylamine-class first-generation antihistamines, which are – once again as in the 1950s – the subject of medical research into their anti-depressant properties.
For all of the above reasons, the use of medicinal scopolamine for recreational uses is also observed.
Analgesics:
Further information: Analgesic
Analgesics (also known as "painkillers") are used to relieve pain (achieve analgesia). The word analgesic derives from Greek "αν-" (an-, "without") and "άλγος" (álgos, "pain").
Analgesic drugs act in various ways on the peripheral and central nervous systems; they include paracetamol (also known in the US as acetaminophen), the nonsteroidal anti-inflammatory drugs (NSAIDs) such as the salicylates (e.g. aspirin), and opioid drugs such as hydrocodone, codeine, heroin and oxycodone.
Some further examples of the brand name prescription opiates and opioid analgesics that may be used recreationally include:
Tranquilizers:
Further information: Tranquilizer
The following are examples of tranquilizers (GABAergics):
Stimulants:
Further information: Stimulant
Stimulants, also known as "psychostimulants", induce euphoria with improvements in mental and physical function, such as enhanced alertness, wakefulness, and locomotion.
Stimulants are also occasionally called "uppers". Depressants or "downers", which decrease mental or physical function, are in stark contrast to stimulants and are considered to be their functional opposites.
Stimulants enhance the activity of the central and peripheral nervous systems. Common effects may include increased:
Use of stimulants may cause the body to significantly reduce its production of endogenous compounds that fulfill similar functions. Once the effect of the ingested stimulant has worn off the user may feel depressed, lethargic, confused, and dysphoric. This is colloquially termed a "crash" and may promote reuse of the stimulant.
Amphetamines are a significant cause of drug-induced psychosis. Importantly, a 2019 meta-analysis found that 22% of people with amphetamine-induced psychosis transition to a later diagnosis of schizophrenia.
Examples of stimulants include:
Euphoriants:
Further information: Euphoriant
Hallucinogens:
Further information: Hallucinogen
See also: List of psychedelic drugs
Hallucinogens can be divided into three broad categories: psychedelics, dissociatives, and deliriants. They can cause subjective changes in perception, thought, emotion and consciousness. Unlike other psychoactive drugs such as stimulants and opioids, hallucinogens do not merely amplify familiar states of mind but also induce experiences that differ from those of ordinary consciousness, often compared to non-ordinary forms of consciousness such as trance, meditation, conversion experiences, and dreams.
Psychedelics, dissociatives, and deliriants have a long worldwide history of use within medicinal and religious traditions. They are used in shamanic forms of ritual healing and divination, in initiation rites, and in the religious rituals of syncretistic movements such as:
When used in religious practice, psychedelic drugs, as well as other substances like tobacco, are referred to as entheogens.
Hallucinogen-induced psychosis occurs when psychosis persists despite no longer being intoxicated with the drug. It is estimated that 26% of people with hallucinogen-induced psychosis will transition to a diagnosis of schizophrenia. This percentage is less than the psychosis transition rate for cannabis (34%) but higher than that of amphetamines (22%).
Starting in the mid-20th century, psychedelic drugs have been the object of extensive attention in the Western world. They have been and are being explored as potential therapeutic agents in treating:
Yet the most popular, and at the same time most stigmatized, use of psychedelics in Western culture has been associated with the search for direct religious experience, enhanced creativity, personal development, and "mind expansion".
The use of psychedelic drugs was a major element of the 1960s counterculture, where it became associated with various social movements and a general atmosphere of rebellion and strife between generations.
Inhalants:
Further information: Inhalant
Inhalants are gases, aerosols, or solvents that are breathed in and absorbed through the lungs.
While some "inhalant" drugs are used for medical purposes, as in the case of nitrous oxide, a dental anesthetic, inhalants are used as recreational drugs for their intoxicating effect.
Most inhalant drugs that are used non-medically are ingredients in household or industrial chemical products that are not intended to be concentrated and inhaled, including organic solvents (found in cleaning products, fast-drying glues, and nail polish removers), fuels (gasoline (petrol) and kerosene), and propellant gases such as Freon and compressed hydrofluorocarbons that are used in aerosol cans such as hairspray, whipped cream, and non-stick cooking spray.
A small number of recreational inhalant drugs are pharmaceutical products that are used illicitly, such as anesthetics (ether and nitrous oxide) and volatile anti-angina drugs (alkyl nitrites, more commonly known as "poppers").
The most serious inhalant abuse occurs among children and teens who "[...] live on the streets completely without family ties". Inhalant users inhale vapor or aerosol propellant gases using plastic bags held over the mouth or by breathing from a solvent-soaked rag or an open container.
The effects of inhalants range from an alcohol-like intoxication and intense euphoria to vivid hallucinations, depending on the substance and the dosage. Some inhalant users are injured due to the harmful effects of the solvents or gases, or due to other chemicals used in the products inhaled. As with any recreational drug, users can be injured due to dangerous behavior while they are intoxicated, such as driving under the influence.
Computer cleaning dusters are dangerous to inhale, because the gases expand and cool rapidly upon being sprayed. In many cases, users have died from hypoxia (lack of oxygen), pneumonia, cardiac failure or arrest, or aspiration of vomit.
Examples include:
List of drugs which can be smoked:
See also: Smoking and List of plants used for smoking
Plants:
Substances (also not necessarily psychoactive plants smoked within them):
List of psychoactive plants, fungi, and animals:
See also: List of psychoactive plants
Minimally psychoactive plants which contain mainly caffeine and theobromine:
Most known psychoactive plants:
Solanaceae plants—contain atropine, hyoscyamine, and scopolamine
Cacti with mescaline:
Other plants:
Fungi:
Psychoactive animals:
See also:
Drug-related literature:
Recreational drug use indicates the use of one or more psychoactive drugs to induce an altered state of consciousness either for pleasure or for some other casual purpose or pastime by modifying the perceptions, feelings, and emotions of the user.
When a psychoactive drug enters the user's body, it induces an intoxicating effect.
Generally, recreational drugs are divided into three categories:
- depressants (drugs that induce a feeling of relaxation and calmness);
- stimulants (drugs that induce a sense of energy and alertness);
- and hallucinogens (drugs that induce perceptual distortions such as hallucination).
In popular practice, recreational drug use generally is a tolerated social behaviour,[ rather than perceived as the medical condition of self-medication. However, heavy use of some drugs is socially stigmatized.
Many people also use prescribed and controlled depressants such as opioids, as well as opiates and benzodiazepines.
Common recreational drugs include:
- caffeine, commonly found in
- alcohol, commonly found in
- beer,
- wine,
- and distilled spirits;
- nicotine, commonly found in
- cannabis and hashish (with legality of possession varying inter/intra-nationally);
- and the controlled substances listed as controlled drugs in
- the Single Convention on Narcotic Drugs (1961)
- and the Convention on Psychotropic Substances (1971) of the United Nations.
What controlled substances are considered generally unlawful to possess varies by country, but usually includes:
- cannabis,
- cocaine,
- opiates,
- MDMA,
- amphetamine,
- methamphetamine,
- LSD,
- psilocybin,
- mescaline,
- and benzodiazepines.
In 2015, it was estimated that about 5% of people worldwide aged 15 to 65 (158 million to 351 million) had used controlled drugs at least once.
Reasons for use:
Further information:
- Epigenetics of cocaine addiction,
- History of drinking,
- History of smoking,
- and Molecular and epigenetic mechanisms of alcoholism
Many researchers have explored the etiology of recreational drug use. Some of the most common theories are:
- genetics,
- personality type,
- psychological problems,
- self-medication,
- sex,
- age,
- instant gratification,
- basic human need,
- curiosity, rebelliousness,
- a sense of belonging to a group,
- family and attachment issues,
- history of trauma,
- failure at school or work,
- socioeconomic stressors,
- peer pressure,
- juvenile delinquency,
- availability,
- historical factors,
- or socio-cultural influences.
There has not been agreement around any one single cause. Instead, experts tend to apply the biopsychosocial model. Any number of these factors are likely to influence an individual's drug use as they are not mutually exclusive.
Regardless of genetics, mental health, or traumatic experiences, social factors play a large role in exposure to and availability of certain types of drugs and patterns of drug use.
According to addiction researcher Martin A. Plant, many people go through a period of self-redefinition before initiating recreational drug use. They tend to view using drugs as part of a general lifestyle that involves belonging to a subculture that they associate with heightened status and the challenging of social norms.
Plant states: "From the user's point of view there are many positive reasons to become part of the milieu of drug taking. The reasons for drug use appear to have as much to do with needs for friendship, pleasure and status as they do with unhappiness or poverty. Becoming a drug taker, to many people, is a positive affirmation rather than a negative experience".
Evolution:
Main article: Evolutionary models of human drug use
Anthropological research has suggested that humans "may have evolved to counter-exploit plant neurotoxins". The ability to use botanical chemicals to serve the function of endogenous neurotransmitters may have improved survival rates, conferring an evolutionary advantage.
A typically restrictive prehistoric diet may have emphasised the apparent benefit of consuming psychoactive drugs, which had themselves evolved to imitate neurotransmitters.
Chemical–ecological adaptations, and the genetics of hepatic enzymes, particularly cytochrome P450, have led researchers to propose that "humans have shared a co-evolutionary relationship with psychotropic plant substances that is millions of years old."
Health risks:
Main articles: Further information:
Severity and type of risks that come with recreational drug use vary widely with the drug in question and the amount being used. There are many factors in the environment and within the user that interact with each drug differently.
Overall, some studies suggest that alcohol is one of the most dangerous of all recreational drugs; only heroin, crack cocaine, and methamphetamine are judged to be more harmful. Alcoholic drinks, tobacco products and other nicotine-based products (e.g., electronic cigarettes), and cannabis are regarded by various medical professionals to be the most common and widespread gateway drugs.
In the United States, Australia, and New Zealand, the general onset of drinking alcohol, tobacco smoking, cannabis smoking, and consumption of multiple drugs among young people most frequently occurs during adolescence and within school settings (middle school and secondary school).
Scientific studies which focus on a low–moderate level of alcohol consumption, particularly of red wine, have concluded that there can be substantial health benefits from its use, such as decreased risk of cardiovascular diseases, stroke, and cognitive decline. This claim has been disputed.
Researcher David Nutt stated that these studies showing benefits for "moderate" alcohol consumption lacked control for the variable of what the subjects were drinking, beforehand.
Experts in the United Kingdom have suggested that some psychoactive drugs that may be causing less harm to fewer users (although they are also used less frequently in the first place) include cannabis, psilocybin mushrooms, LSD, and MDMA. However, these drugs are not without their own particular risks and side effects.
Drug harmfulness:
Drug harmfulness is defined as the degree to which a psychoactive drug is harmful to a user and is measured in various ways, such as by addictiveness and the potential for physical harm.
More harmful drugs are called "hard drugs", and less harmful drugs are called "soft drugs". The term "soft drug" is considered controversial by its critics as it may imply that soft drugs cause no or insignificant harm.
Responsible use:
Main article: Responsible drug use
The concept of "responsible drug use" is that a person can use drugs recreationally or otherwise with reduced or eliminated risk of negatively affecting other aspects of one's life or other people's lives. Advocates of this philosophy point to the many well-known artists and intellectuals who have used drugs, experimentally or otherwise, with few detrimental effects on their lives. Responsible drug use becomes problematic only when the use of the substance significantly interferes with the user's daily life.
Responsible drug use advocates that users should not take drugs at the same time as activities such as driving, swimming, operating machinery, or other activities that are unsafe without a sober state. Responsible drug use is emphasized as a primary prevention technique in harm-reduction drug policies.
Harm-reduction policies were popularized in the late 1980s, although they began in the 1970s counter-culture, when cartoons explaining responsible drug use and the consequences of irresponsible drug use were distributed to users.
Another issue is that the illegality of drugs in itself also causes social and economic consequences for those using them—the drugs may be "cut" with adulterants and the purity varies wildly, making overdoses more likely—and legalization of drug production and distribution would reduce these and other dangers of illegal drug use.
Harm reduction seeks to minimize the harm that can occur through the use of various drugs, whether legal (e.g., alcohol and nicotine), or illegal (e.g., heroin and cocaine). For example, people who take drugs intravenously (cocaine, heroin) can minimize harm to both themself and members of the community through proper injecting technique, using new needles and syringes each time, and proper disposal of all injecting equipment.
Prevention:
Main articles: Harm reduction and Preventive healthcare
In efforts to curtail recreational drug use, governments worldwide introduced several laws prohibiting the possession of almost all varieties of recreational drugs during the 20th century. The West's "War on Drugs" however, is now facing increasing criticism. Evidence is insufficient to tell if behavioral interventions help prevent recreational drug use in children.
One in four adolescents has used an illegal drug and one in ten of those adolescents who need addiction treatment get some type of care. School-based programs are the most commonly used method for drug use education; however, the success rates of these intervention programs is highly dependent on the commitment of participants and is limited in general. Studies have also shown that home intervention is also effective in decreasing the appeal of drugs.
Demographics:
Further information: Illegal drug trade, Opioid epidemic, and Prohibition of drugs
Australia:
Further information: Alcoholism in rural Australia
Alcohol is the most widely used drug in Australia. 86.2% of Australians aged 12 years and over have consumed alcohol at least once in their lifetime, compared to 34.8% of Australians aged 12 years and over who have used cannabis at least once in their lifetime.
United States:
Further information:
- Cocaine in the United States,
- Crack epidemic in the United States,
- and Opioid epidemic in the United States
From the mid-19th century to the 1930s, American physicians prescribed Cannabis sativa as a prescription drug for various medical conditions.
In the 1960s, the counterculture movement introduced the use of psychoactive drugs, including cannabis. Young adults and college students reported the recreational prevalence of cannabis, among other drugs, at 20-25% while the cultural mindset of using was open and curious.
In 1969, the FBI reported that between the years 1966 and 1968, the number of arrests for marijuana possession, which had been outlawed throughout the United States under Marijuana Tax Act of 1937, had increased by 98%.
Despite acknowledgement that drug use was greatly growing among America's youth during the late 1960s, surveys have suggested that only as much as 4% of the American population had ever smoked marijuana by 1969. By 1972, however, that number would increase to 12%. That number would then double by 1977.
The Controlled Substances Act of 1970 classified marijuana along with heroin and LSD as a Schedule I drug, i.e., having the relatively highest abuse potential and no accepted medical use.
Most marijuana at that time came from Mexico, but in 1975 the Mexican government agreed to eradicate the crop by spraying it with the herbicide paraquat, raising fears of toxic side effects. Colombia then became the main supplier.
The "zero tolerance" climate of the Reagan and Bush administrations (1981–93) resulted in passage of strict laws and mandatory sentences for possession of marijuana. The "War on Drugs" thus brought with it a shift from reliance on imported supplies to domestic cultivation (particularly in Hawaii and California).
Beginning in 1982, the Drug Enforcement Administration turned increased attention to marijuana farms in the United States, and there was a shift to the indoor growing of plants specially developed for small size and high yield.
After over a decade of decreasing use, marijuana smoking began an upward trend once more in the early 1990s, especially among teenagers, but by the end of the decade this upswing had leveled off well below former peaks of use.
Society and culture:
Main articles: Further information:
- Alcohol abuse among college students,
- Benzodiazepine drug misuse,
- Binge drinking,
- and Drug-facilitated sexual assault
Many movements and organizations are advocating for or against the liberalization of the use of recreational drugs, most notably regarding the legalization of marijuana and cannabinoids for medical and/or recreational use.
Subcultures have emerged among users of recreational drugs, as well as alternative lifestyles and social movements among those who abstain from them, such as teetotalism and "straight edge".
Since the early 2000s, medical professionals have acknowledged and addressed the problem of the increasing consumption of alcoholic drinks and club drugs (such as:
- MDMA,
- cocaine,
- rohypnol,
- GHB,
- ketamine,
- PCP,
- LSD,
- and methamphetamine
- associated with rave culture among adolescents and young adults in the Western world.
Studies have shown that adolescents are more likely than young adults to use multiple drugs, and the consumption of club drugs is highly associated with the presence of criminal behaviors and recent alcohol abuse or dependence.
The prevalence of recreational drugs in human societies is widely reflected in fiction, entertainment, and the arts, subject to prevailing laws and social conventions.
For instance, in the music industry, the musical genres hip hop, hardcore rap, and trap, alongside their derivative subgenres and subcultures, are most notorious for having continuously celebrated and promoted drug trafficking, gangster lifestyle, and consumption of drugs and alcohol since their inception in the United States during the late 1980s–early 1990s.
In video games, for example, drugs are portrayed in a variety of ways: including power-ups , e.g.,
- cocaine gum replenishes stamina in Red Dead Redemption 2),
- obstacles to be avoided (such as the Fuzzies in Super Mario World 2: Yoshi's Island that distort the player's view when accidentally consumed),
- items to be bought and sold for in-game currency (coke dealing is a big part of Scarface: The World Is Yours).
In 1997's Fallout, drugs ("chems" in the game) can fill the role of any above mentioned. Drug trafficking, gang rivalries, and their related criminal underworld also play a big part in the best-selling Grand Theft Auto video game franchise.
Common recreational drugs:
The following substances are commonly used recreationally:
- Alcohol: Most drinking alcohol is ethanol, CH
3CH
2OH. Drinking alcohol creates intoxication, relaxation and lowered inhibitions. It is produced by the fermentation of sugars by yeasts to create wine, beer, and distilled liquor (e.g., vodka, rum, gin, etc.). In most areas of the world, it is legal for those over a certain age (18 in most countries). It is an IARC Group 1 carcinogen and a teratogen. Alcohol withdrawal can be life-threatening. - Amphetamines: Used recreationally to provide alertness and a sense of energy. Prescribed for ADHD, narcolepsy, depression and weight loss. A potent central nervous system stimulant, in the 1940s and 50s methamphetamine was used by Axis and Allied troops in World War II, and, later on, other armies, and by Japanese factory workers. It increases muscle strength and fatigue resistance and improves reaction time. Methamphetamine use can be neurotoxic, which means it damages dopamine neurons. As a result of this brain damage, chronic use can lead to post acute withdrawal syndrome.
- Caffeine: Often found in coffee, black tea, energy drinks, some soft drinks (e.g., Coca-Cola, Pepsi and Mountain Dew, among others), and chocolate. It is the world's most widely consumed psychoactive drug, but has only mild dependence liability for long-term users.
- Cannabis: Its common forms include marijuana and hashish, which are smoked or eaten. It contains at least 85 cannabinoids. The primary psychoactive component is THC, which mimics the neurotransmitter anandamide, named after the Hindu ananda, "joy, bliss, delight".
- Cocaine: It is available as a white powder, which is insufflated ("sniffed" into the nostrils) or converted into a solution with water and injected. A popular derivative, crack cocaine is typically smoked. When transformed into its freebase form, crack, the cocaine vapor may be inhaled directly. This is thought to increase bioavailability, but has also been found to be toxic, due to the production of methylecgonidine during pyrolysis.
- MDMA: Commonly known as ecstasy, it is a common club drug in the rave scene.
- Electronic cigarette: A large proportion of e-cigarette use is recreational. Most e-cigarette liquids contain nicotine, but the level of nicotine varies depending on user-preference and manufacturers. Nicotine is highly addictive, comparable to heroin or cocaine. E-cigarettes are being used to inhale MDMA, cocaine powder, crack cocaine, synthetic cathinones, mephedrone, α-PVP, synthetic cannabinoids, opioids, heroin, fentanyl, tryptamines, and ketamine.
- Ketamine: An anesthetic used legally by paramedics and doctors in emergency situations for its dissociative and analgesic qualities; but illegally in the club drug scene.
- Lean: A liquid drug mixture made when mixing cough syrup, sweets, soft drinks and codeine. It originated in the 1990s in Houston. Ever since then, this drug usage has grown and is often used at parties and in the trap music scene. Many people would get a drowsy feeling when consuming this drug.
- LSD: A popular ergoline derivative, that was first synthesized in 1938 by Albert Hofmann. However, he failed to notice its psychedelic effects until 1943. In the 1950s, it was used in psychological therapy, and, covertly, by the CIA in Project MKULTRA, in which the drug was administered to unwitting US and Canadian citizens. It played a central role in 1960s 'counter-culture', and was banned in October 1968 by US President Lyndon B Johnson.
- Nitrous oxide: legally used by dentists as an anxiolytic and anaesthetic, it is also used recreationally by users who obtain it from whipped cream canisters (whippets or whip-its) (see inhalant), as it causes perceptual effects, a "high" and at higher doses, hallucinations.
- Opiates and opioids: Available by prescription for pain relief. Commonly used opioids include oxycodone, hydrocodone, codeine, fentanyl, heroin, methadone, and morphine. Opioids have a high potential for addiction and have the ability to induce severe physical withdrawal symptoms upon cessation of frequent use. Heroin can be smoked, insufflated or turned into a solution with water and injected. Percocet is a prescription opioid containing oxycodone and acetaminophen.
- Psilocybin mushrooms: This hallucinogenic drug was an important drug in the psychedelic scene. Until 1963, when it was chemically analyzed by Albert Hofmann, it was completely unknown to modern science that Psilocybe semilanceata ("Liberty Cap", common throughout Europe) contains psilocybin, a hallucinogen previously identified only in species native to Mexico, Asia, and North America.
- Tobacco: Nicotiana tabacum. Nicotine is the key drug contained in tobacco leaves, which are either smoked, chewed or snuffed. It contains nicotine, which crosses the blood–brain barrier in 10–20 seconds. It mimics the action of the neurotransmitter acetylcholine at nicotinic acetylcholine receptors in the brain and the neuromuscular junction. The neuronal forms of the receptor are present both post-synaptically (involved in classical neurotransmission) and pre-synaptically, where they can influence the release of multiple neurotransmitters.
- Tranquilizers: barbiturates, benzodiazepines (e.g. alprazolam, diazepam, etc.)(commonly prescribed for anxiety disorders; known to cause dementia and post acute withdrawal syndrome)
- "Bath salts": slang term that generally refers to substituted cathinones such as Mephedrone and Methylenedioxypyrovalerone (MDPV), but not always
- DMT – primary ingredient in ayahuasca, can also be smoked (inhalation causes a brief effect lasting usually 5 to 15 minutes).
- Peyote: This hallucinogen contains mescaline, native to southwestern Texas and Mexico
- Salvia divinorum: This hallucinogenic Mexican herb in the mint family; not considered recreational, most likely due to the nature of the hallucinations (legal in some jurisdictions)
- Synthetic cannabis: "Spice", "K2", JWH-018, AM-2201
- Quaaludes: A popular club drug in the 1970s. No longer prescribed or manufactured in many countries but remains popular in South Africa.
Routes of administration:
Drugs are often associated with a particular route of administration. Many drugs can be consumed in more than one way. For example, marijuana can be swallowed like food or smoked, and cocaine can be "sniffed" in the nostrils, injected, or, with various modifications, smoked.
- inhalation: all intoxicative inhalants (see below) that are gases or solvent vapours that are inhaled through the trachea, as the name suggests
- insufflation: also known as "snorting", or "sniffing", this method involves the user placing a powder in the nostrils and breathing in through the nose, so that the drug is absorbed by the mucous membranes. Drugs that are "snorted", or "sniffed", include powdered amphetamines, cocaine, heroin, ketamine, MDMA, snuff tobacco
- Subcutaneous injection: also known as Skin popping. Injection of drug into the third lowest layer of skin.
- Intramuscular injection: injection of drug into a muscle.
- intravenous injection (see also the article Drug injection): the user injects a solution of water and the drug into a vein, or less commonly, into the tissue. Drugs that are injected include morphine and heroin, less commonly other opioids. Stimulants like cocaine or methamphetamine may also be injected. In rare cases, users inject other drugs.
- oral intake:
- caffeine,
- ethanol,
- cannabis edibles,
- psilocybin mushrooms,
- coca tea,
- poppy tea,
- laudanum,
- GHB,
- ecstasy pills with MDMA or various other substances (mainly stimulants and psychedelics),
- prescription and over-the-counter drugs
- (ADHD and narcolepsy medications,
- benzodiazepines,
- anxiolytics,
- sedatives,
- cough suppressants,
- morphine,
- codeine,
- opioids
- and others)
- sublingual: substances diffuse into the blood through tissues under the tongue. Many psychoactive drugs can be or have been specifically designed for sublingual administration, including
- arbiturates,
- benzodiazepines,
- opioid analgesics with poor gastrointestinal bioavailability,
- LSD blotters,
- coca leaves,
- some hallucinogens.
- This route of administration is activated when chewing some forms of smokeless tobacco (e.g. dipping tobacco, snus).
- intrarectal: administering into the rectum, most water-soluble drugs can be used this way.
- smoking (see also the section below):
- tobacco,
- cannabis,
- opium,
- crystal meth,
- phencyclidine,
- crack cocaine and heroin (diamorphine as freebase) known as chasing the dragon.
- transdermal patches with prescription drugs: e.g.
- methylphenidate (Daytrana)
- and fentanyl.
Many drugs are taken through various routes. Intravenous route is the most efficient, but also one of the most dangerous. Nasal, rectal, inhalation and smoking are safer. The oral route is one of the safest and most comfortable, but of little bioavailability.
Types:
Depressants:
Further information: Depressant
Depressants are psychoactive drugs that temporarily diminish the function or activity of a specific part of the body or mind.
Colloquially, depressants are known as "downers", and users generally take them to feel more relaxed and less tense. Examples of these kinds of effects may include anxiolysis, sedation, and hypotension.
Depressants are widely used throughout the world as prescription medicines and as illicit substances. When these are used, effects may include:
- anxiolysis (reduction of anxiety),
- analgesia (pain relief), sedation, somnolence,
- cognitive/memory impairment,
- dissociation,
- muscle relaxation,
- lowered blood pressure/heart rate,
- respiratory depression,
- anesthesia,
- and anticonvulsant effects.
Depressants exert their effects through a number of different pharmacological mechanisms, the most prominent of which include potentiation of GABA or opioid activity, and inhibition of adrenergic, histamine or acetylcholine activity. Some are also capable of inducing feelings of euphoria. The most widely used depressant by far is alcohol (i.e. ethanol).
Stimulants or "uppers", such as amphetamines or cocaine, which increase mental or physical function, have an opposite effect to depressants.
Depressants, in particular alcohol, can precipitate psychosis. A 2019 systematic review and meta-analysis by Murrie et al. found that the rate of transition from opioid, alcohol and sedative induced psychosis to schizophrenia was 12%, 10% and 9% respectively.
Antihistamines:
Further information: Antihistamine
Antihistamines (or "histamine antagonists") inhibit the release or action of histamine. "Antihistamine" can be used to describe any histamine antagonist, but the term is usually reserved for the classical antihistamines that act upon the H1 histamine receptor.
Antihistamines are used as treatment for allergies. Allergies are caused by an excessive response of the body to allergens, such as the pollen released by grasses and trees. An allergic reaction causes release of histamine by the body. Other uses of antihistamines are to help with normal symptoms of insect stings even if there is no allergic reaction.
Their recreational appeal exists mainly due to their anticholinergic properties, that induce anxiolysis and, in some cases such as diphenhydramine, chlorpheniramine, and orphenadrine, a characteristic euphoria at moderate doses. High dosages taken to induce recreational drug effects may lead to overdoses.
Antihistamines are also consumed in combination with alcohol, particularly by youth who find it hard to obtain alcohol. The combination of the two drugs can cause intoxication with lower alcohol doses.
Hallucinations and possibly delirium resembling the effects of Datura stramonium can result if the drug is taken in much higher than therapeutic doses. Antihistamines are widely available over the counter at drug stores (without a prescription), in the form of allergy medication and some cough medicines. They are sometimes used in combination with other substances such as alcohol.
The most common unsupervised use of antihistamines in terms of volume and percentage of the total is perhaps in parallel to the medicinal use of some antihistamines to extend and intensify the effects of opioids and depressants.
The most commonly used are hydroxyzine, mainly to extend a supply of other drugs, as in medical use, and the above-mentioned ethanolamine and alkylamine-class first-generation antihistamines, which are – once again as in the 1950s – the subject of medical research into their anti-depressant properties.
For all of the above reasons, the use of medicinal scopolamine for recreational uses is also observed.
Analgesics:
Further information: Analgesic
Analgesics (also known as "painkillers") are used to relieve pain (achieve analgesia). The word analgesic derives from Greek "αν-" (an-, "without") and "άλγος" (álgos, "pain").
Analgesic drugs act in various ways on the peripheral and central nervous systems; they include paracetamol (also known in the US as acetaminophen), the nonsteroidal anti-inflammatory drugs (NSAIDs) such as the salicylates (e.g. aspirin), and opioid drugs such as hydrocodone, codeine, heroin and oxycodone.
Some further examples of the brand name prescription opiates and opioid analgesics that may be used recreationally include:
- Vicodin,
- Lortab,
- Norco (hydrocodone),
- Avinza,
- Kapanol (morphine),
- Opana,
- Paramorphan (oxymorphone),
- Dilaudid,
- Palladone (hydromorphone),
- and OxyContin (oxycodone).
Tranquilizers:
Further information: Tranquilizer
The following are examples of tranquilizers (GABAergics):
- Barbiturates
- Benzodiazepines
- Ethanol (drinking alcohol; ethyl alcohol)
- Nonbenzodiazepines
- Others:
- carisoprodol (Soma)
- chloral hydrate
- diethyl ether
- ethchlorvynol (Placidyl; "jelly-bellies")
- gamma-butyrolactone (GBL, a prodrug to GHB)
- gamma-hydroxybutyrate (GHB; G; Xyrem; "Liquid Ecstasy", "Fantasy")
- glutethimide (Doriden)
- kava (from Piper methysticum; contains kavalactones)
- ketamine, a phencyclidine (PCP) analog
- meprobamate (Miltown)
- methaqualone (Sopor, Mandrax; "Quaaludes")
- phenibut
- propofol (Diprivan), a general anesthetic
- theanine (found in Camellia sinensis, the tea plant)
- valerian (from Valeriana officinalis)
Stimulants:
Further information: Stimulant
Stimulants, also known as "psychostimulants", induce euphoria with improvements in mental and physical function, such as enhanced alertness, wakefulness, and locomotion.
Stimulants are also occasionally called "uppers". Depressants or "downers", which decrease mental or physical function, are in stark contrast to stimulants and are considered to be their functional opposites.
Stimulants enhance the activity of the central and peripheral nervous systems. Common effects may include increased:
- alertness,
- awareness,
- wakefulness,
- endurance,
- productivity and motivation,
- arousal,
- locomotion,
- heart rate,
- and blood pressure,
- and a diminished desire for food and sleep.
Use of stimulants may cause the body to significantly reduce its production of endogenous compounds that fulfill similar functions. Once the effect of the ingested stimulant has worn off the user may feel depressed, lethargic, confused, and dysphoric. This is colloquially termed a "crash" and may promote reuse of the stimulant.
Amphetamines are a significant cause of drug-induced psychosis. Importantly, a 2019 meta-analysis found that 22% of people with amphetamine-induced psychosis transition to a later diagnosis of schizophrenia.
Examples of stimulants include:
- Sympathomimetics (catecholaminergics)—e.g. amphetamine, methamphetamine, cocaine, methylphenidate, ephedrine, pseudoephedrine
- Entactogens (serotonergics, primarily phenethylamines)—e.g. MDMA (which is also an amphetamine)
- Eugeroics, e.g. modafinil
- Others:
- arecoline (found in Areca catechu)
- caffeine (found in Coffea spp.)
- nicotine (found in Nicotiana spp.)
- rauwolscine (found in Rauvolfia serpentina)
- yohimbine (Procomil; a tryptamine alkaloid found in Pausinystalia johimbe)
Euphoriants:
Further information: Euphoriant
- Alcohol: "Euphoria, the feeling of well-being, has been reported during the early (10–15 min) phase of alcohol consumption" (e.g., beer, wine or spirits)
- Cannabis: Tetrahydrocannabinol, the main psychoactive ingredient in this plant, can have sedative and euphoric properties.
- Catnip: Catnip contains a sedative known as nepetalactone that activates opioid receptors. In cats it elicits sniffing, licking, chewing, head shaking, rolling, and rubbing which are indicators of pleasure. In humans, however, catnip does not act as a euphoriant.
- Stimulants: "Psychomotor stimulants produce locomotor activity (the subject becomes hyperactive), euphoria, (often expressed by excessive talking and garrulous behaviour), and anorexia. The amphetamines are the best known drugs in this category..."
- MDMA: The "euphoriant drugs such as MDMA ('ecstasy') and MDEA ('eve')" are popular among young adults. MDMA "users experience short-term feelings of euphoria, rushes of energy and increased tactility" as well as interpersonal connectedness.
- Opium: This "drug derived from the unripe seed-pods of the opium poppy…produces drowsiness and euphoria and reduces pain. Morphine and codeine are opium derivatives." Opioids have led to many deaths in the United States, particularly by causing respiratory depression.
Hallucinogens:
Further information: Hallucinogen
See also: List of psychedelic drugs
Hallucinogens can be divided into three broad categories: psychedelics, dissociatives, and deliriants. They can cause subjective changes in perception, thought, emotion and consciousness. Unlike other psychoactive drugs such as stimulants and opioids, hallucinogens do not merely amplify familiar states of mind but also induce experiences that differ from those of ordinary consciousness, often compared to non-ordinary forms of consciousness such as trance, meditation, conversion experiences, and dreams.
Psychedelics, dissociatives, and deliriants have a long worldwide history of use within medicinal and religious traditions. They are used in shamanic forms of ritual healing and divination, in initiation rites, and in the religious rituals of syncretistic movements such as:
When used in religious practice, psychedelic drugs, as well as other substances like tobacco, are referred to as entheogens.
Hallucinogen-induced psychosis occurs when psychosis persists despite no longer being intoxicated with the drug. It is estimated that 26% of people with hallucinogen-induced psychosis will transition to a diagnosis of schizophrenia. This percentage is less than the psychosis transition rate for cannabis (34%) but higher than that of amphetamines (22%).
Starting in the mid-20th century, psychedelic drugs have been the object of extensive attention in the Western world. They have been and are being explored as potential therapeutic agents in treating:
- depression,
- post-traumatic stress disorder (PTSD),
- obsessive-compulsive disorder,
- alcoholism,
- and opioid addiction.
Yet the most popular, and at the same time most stigmatized, use of psychedelics in Western culture has been associated with the search for direct religious experience, enhanced creativity, personal development, and "mind expansion".
The use of psychedelic drugs was a major element of the 1960s counterculture, where it became associated with various social movements and a general atmosphere of rebellion and strife between generations.
- Deliriants
- atropine (alkaloid found in plants of the family Solanaceae, including datura, deadly nightshade, henbane and mandrake)
- dimenhydrinate (Dramamine, an antihistamine)
- diphenhydramine (Benadryl, Unisom, Nytol)
- hyoscyamine (alkaloid also found in the Solanaceae)
- hyoscine hydrobromide (another Solanaceae alkaloid)
- myristicin found in Myristica fragrans ("Nutmeg")
- ibotenic acid (found in Amanita muscaria ("Fly Agaric"); prodrug to muscimol)
- muscimol (also found in Amanita muscaria, a GABAergic)
- Dissociatives
- dextromethorphan (DXM; Robitussin, Delsym, etc.; "Dex", "Robo", "Cough Syrup", "DXM")
- "Triple C's, Coricidin, Skittles" refer to a potentially fatal formulation containing both dextromethorphan and chlorpheniramine.
- ketamine (K; Ketalar, Ketaset, Ketanest; "Ket", "Kit Kat", "Special-K", "Vitamin K", "Jet Fuel", "Horse Tranquilizer")
- methoxetamine (Mex, Mket, Mexi)
- phencyclidine (PCP; Sernyl; "Angel Dust", "Rocket Fuel", "Sherm", "Killer Weed", "Super Grass")
- nitrous oxide (N2O; "NOS", "Laughing Gas", "Whippets", "Balloons")
- dextromethorphan (DXM; Robitussin, Delsym, etc.; "Dex", "Robo", "Cough Syrup", "DXM")
- Psychedelics
- Phenethylamines
- 2C-B ("Nexus", "Venus", "Eros", "Bees")
- 2C-E ("Eternity", "Hummingbird")
- 2C-I ("Infinity")
- 2C-T-2 ("Rosy")
- 2C-T-7 ("Blue Mystic", "Lucky 7")
- DOB
- DOC
- DOI
- DOM ("Serenity, Tranquility, and Peace" ("STP"))
- MDMA ("Ecstasy", "E", "Molly", "Mandy", "MD", "Crystal Love")
- mescaline (found in peyote, Peruvian torch cactus and San Pedro cactus)
- Tryptamines (including ergolines and lysergamides)
- 5-MeO-DiPT ("Foxy", "Foxy Methoxy")
- 5-MeO-DMT (found in various plants like chacruna, jurema, vilca, and yopo)
- alpha-methyltryptamine (αMT; Indopan; "Spirals")
- bufotenin (secreted by Bufo alvarius, also found in various Amanita mushrooms)
- N,N-dimethyltryptamine (N,N-DMT; DMT; "Dimitri", "Disneyland", "Spice"; found in large amounts in Psychotria and in D. cabrerana)
- lysergic acid amide (LSA; ergine; found in morning glory and Hawaiian baby woodrose seeds)
- lysergic acid diethylamide (LSD; L; Delysid; "Acid", "Sid". "Cid", "Lucy", "Sidney", "Blotters", "Droppers", "Sugar Cubes")
- O-Acetylpsilocin (believed to be a prodrug of psilocin)
- psilocin (found in psilocybin mushrooms)
- psilocybin (also found in psilocybin mushrooms; prodrug to psilocin)
- ibogaine (found in Tabernanthe iboga ("Iboga"))
- Phenethylamines
- Atypicals:
- salvinorin A (found in Salvia divinorum, a trans-neoclerodane diterpenoid ("Diviner's Sage", "Lady Salvia", "Salvinorin"))
Inhalants:
Further information: Inhalant
Inhalants are gases, aerosols, or solvents that are breathed in and absorbed through the lungs.
While some "inhalant" drugs are used for medical purposes, as in the case of nitrous oxide, a dental anesthetic, inhalants are used as recreational drugs for their intoxicating effect.
Most inhalant drugs that are used non-medically are ingredients in household or industrial chemical products that are not intended to be concentrated and inhaled, including organic solvents (found in cleaning products, fast-drying glues, and nail polish removers), fuels (gasoline (petrol) and kerosene), and propellant gases such as Freon and compressed hydrofluorocarbons that are used in aerosol cans such as hairspray, whipped cream, and non-stick cooking spray.
A small number of recreational inhalant drugs are pharmaceutical products that are used illicitly, such as anesthetics (ether and nitrous oxide) and volatile anti-angina drugs (alkyl nitrites, more commonly known as "poppers").
The most serious inhalant abuse occurs among children and teens who "[...] live on the streets completely without family ties". Inhalant users inhale vapor or aerosol propellant gases using plastic bags held over the mouth or by breathing from a solvent-soaked rag or an open container.
The effects of inhalants range from an alcohol-like intoxication and intense euphoria to vivid hallucinations, depending on the substance and the dosage. Some inhalant users are injured due to the harmful effects of the solvents or gases, or due to other chemicals used in the products inhaled. As with any recreational drug, users can be injured due to dangerous behavior while they are intoxicated, such as driving under the influence.
Computer cleaning dusters are dangerous to inhale, because the gases expand and cool rapidly upon being sprayed. In many cases, users have died from hypoxia (lack of oxygen), pneumonia, cardiac failure or arrest, or aspiration of vomit.
Examples include:
- Chloroform
- Ethyl chloride
- Diethyl ether
- Ethane and ethylene
- Laughing gas (nitrous oxide)
- Poppers (alkyl nitrites)
- Solvents and propellants (including propane, butane, freon, gasoline, kerosene, toluene) along with the fumes of glues containing them
List of drugs which can be smoked:
See also: Smoking and List of plants used for smoking
Plants:
- tobacco
- cannabis
- salvia divinorum
- opium
- datura and other Solanaceae (formerly smoked to treat asthma)
- possibly other plants (see the section below)
Substances (also not necessarily psychoactive plants smoked within them):
- methamphetamine
- crack cocaine
- black tar heroin
- phencyclidine (PCP)
- synthetic cannabinoids (see also: synthetic cannabis)
- dimethyltryptamine (DMT)
- 5-MeO-DMT
- Bufotenine
- DiPT
- Methaqualone
- Ethanol (alcohol)
- Ketamine
- Heroin
- many others, including some prescription drugs
List of psychoactive plants, fungi, and animals:
See also: List of psychoactive plants
Minimally psychoactive plants which contain mainly caffeine and theobromine:
- coffee
- tea (caffeine in tea is sometimes called theine) – also contains theanine
- guarana (caffeine in guarana is sometimes called guaranine)
- yerba mate (caffeine in yerba mate is sometimes called mateine)
- cocoa
- kola
Most known psychoactive plants:
- cannabis: cannabinoids
- tobacco: nicotine and beta-carboline alkaloids
- coca: cocaine
- opium poppy: morphine, codeine, and other opiates
- salvia divinorum: salvinorin A
- khat: cathine and cathinone
- kava: kavalactones
- nutmeg: myristicin and elemicin
Solanaceae plants—contain atropine, hyoscyamine, and scopolamine
- datura
- deadly nightshade Atropa belladonna
- henbane
- mandrake (mandragora)
- other Solanaceae
Cacti with mescaline:
Other plants:
- kratom:
- ephedra: ephedrine
- damiana
- Calea zacatechichi
- Silene capensis
- valerian: valerian (the chemical with the same name)
- various plants like chacruna, jurema, vilca, and yopo – 5-MeO-DMT
- Morning glory and Hawaiian Baby Woodrose – lysergic acid amide (LSA, ergine)
- Ayahuasca (for DMT)
- Tabernanthe iboga ("Iboga")--ibogaine
- Areca catechu (see: betel and paan)--arecoline
- Rauvolfia serpentina: rauwolscine
- yohimbe (Pausinystalia johimbe): yohimbine and corynanthine
- many others
Fungi:
- psilocybin mushrooms: psilocybin and psilocin
- various Amanita mushrooms: muscimol
- Amanita muscaria: ibotenic acid and muscimol
- Claviceps purpurea and other Clavicipitaceae: ergotamine (not psychoactive itself but used in synthesis of LSD)
Psychoactive animals:
- hallucinogenic fish
- psychoactive toads: bufotenin, Bufo alvarius (Colorado River toad or Sonoran Desert toad) also contains 5-MeO-DMT
See also:
- "The Science of Drug Use: A Resource for the Justice Sector". www.drugabuse.gov. North Bethesda, Maryland: National Institute on Drug Abuse. 26 May 2020. Retrieved 23 December 2021.
- School-Based Drug Abuse Prevention: Promising and Successful Programs (PDF). www.publicsafety.gc.ca. Ottawa, Ontario: Public Safety Canada. 31 January 2018. ISBN 978-1-100-12181-9. Archived (PDF) from the original on 19 May 2021. Retrieved 23 December 2021.
- Sacco LN, Finklea K (3 May 2016). "Synthetic Drugs: Overview and Issues for Congress" (PDF). Washington, D.C.: Congressional Research Service. Archived (PDF) from the original on 8 December 2021. Retrieved 23 December 2021.
- Alcohol licensing laws of the United Kingdom
- Ban on caffeinated alcoholic drinks in the United States
- Cigarette packets in Australia
- Counterfeit drug
- Demand reduction
- Designer drug
- Drug discovery
- Drug policy:
- Effective dose
- Effects of cannabis
- Flavored tobacco
- Gateway drug theory
- Harm reduction
- Illegal drug trade
- LD50
- Legalization of non-medical cannabis in the United States
- Over the counter drug
- Pharmacology
- Polysubstance use and abuse
- Prevalence of tobacco consumption
- Project MKUltra
- Psychedelic experience
- Psychopharmacology
- Psychotomimetism
- Purple drank
- Recreational use of dextromethorphan
- Recreational use of ketamine
- Regulation of therapeutic goods
- Tobacco marketing targeting African Americans
- Tobacco packaging warning messages
- Toxicology
- Usage of electronic cigarettes
Drug-related literature:
- Licit and Illicit Drugs
- Marihuana: The First Twelve Thousand Years
- Methland
- Smoke and Mirrors: The War on Drugs and the Politics of Failure
- The Doors of Perception
- The Rhetoric of Drugs
- This Is Your Country On Drugs
List of Celebrity Deaths from Drug Overdose and Alcohol Intoxication
- YouTube Video Celebrity Drugs and Death in the Spotlight
- YouTube Video: Famous People Whose Parents Committed Suicide
- YouTube Video: Tragic Details About Robin Williams Revealed
- Top (L) Whitney Houston: It was the night before the Grammys, February 11, 2012, when this pop diva checked into room 434 of the Beverly Hilton. She was scheduled to appear at Clive Davis's pre-Grammy party, but the star never made it. Houston was found in the bathtub of her hotel room, prescription bottles littering the room. The vocalist ingested cocaine, Flexeril, marijuana, and Xanax and fell into a deep sleep in the bathtub. Sadly, her daughter, Bobbi Kristina, also was found unconscious in a bathtub, and has since passed away.
- Top (R): Michael Jackson: Known as the King of Pop, Jackson was reportedly introverted, odd and quiet. Alas the icon kept his prescription drug habit well hidden. He left a nation mourning when he died of cardiac arrest due to an acute propofol and benzodiazepines intoxication.
- Center (L): Philip Seymour Hoffman: This Oscar-winning actor was tragically found dead with a needle in his arm in February 2014. A combination of heroin, cocaine and other drugs took the Capote star's life in his Manhattan apartment. The actor had three children with his partner, Mimi O'Donnell.
- Center (R): Marilyn Monroe: Born Norma Jean, Monroe was the ultimate sex symbol of her time. The Some Like It Hot and How To Marry A Millionaire star died in 1962 of a prescription drug overdose. Cryptic letters and personal relationships with both John and Robert Kennedy led many to wonder if the overdose was indeed accidental.
- Bottom (L): Jimi Hendrix: One of the best known electric guitarists in the world, Hendrix and his Fender guitar revolutionized the music scene in the 1960s, but his drug addiction was no secret. Hendrix died on September 18, 1970, at the age of 27 in London after a deadly dose of alcohol and drugs. The musician passed out and reportedly choked to death on his own vomit.
- Bottom (R) Janis Joplin: This original wild child was only 27 when she died of a heroin overdose on October 4, 1970, at the Hollywood Landmark Hotel. Pearl was her last and most successful album. While she struggled outwardly with addiction, the "First Lady of Rock and Roll" was known for her sultry vocals and is considered a music legend.
Drug overdose and intoxication are significant causes of accidental death; and can also be used as a form of suicide. Death can occur from overdosing on a single or multiple drugs, or from combined drug intoxication (CDI) due to poly drug use.
Poly drug use often carries more risk than use of a single drug, due to an increase in side effects, and drug synergy. For example, the chance of death from overdosing on opiates is greatly increased when they are consumed in conjunction with alcohol.
While they are two distinct phenomena, deaths from CDI are often misreported as overdoses. Drug overdoses and intoxication can also cause indirect deaths. For example, while marijuana does not cause fatal overdoses, being intoxicated by it can increase the chance of fatal traffic collisions.
Drug use and overdoses increased significantly in the 1800s due to the commercialization and availability of certain drugs. For example, while opium and coca had been used for centuries, their active ingredients, morphine and the cocaine alkaloid, were not isolated until 1803 and 1855 respectively.
Cocaine and various opiates were subsequently mass-produced and sold openly and legally in the Western world, resulting in widespread misuse and addiction. Drug use and addiction also increased significantly following the invention of the hypodermic syringe in 1853, with overdose being a leading cause of death among intravenous drug users.
Efforts to prohibit various drugs began to be enacted in the early 20th century, though the effectiveness of such policies is debated. Deaths from drug overdoses are increasing.
Between 2000 and 2014, fatal overdoses rose 137% in the United States, causing nearly half a million deaths in that period, and have also been continually increasing in Australia, Scotland, England, and Wales.
While prohibited drugs are generally viewed as being the most dangerous, the misuse of prescription drugs is linked to more deaths in several countries. Cocaine and heroin combined caused fewer deaths than prescriptions drugs in the United Kingdom in 2013, and fewer deaths than prescription opiates alone in the United States in 2008.
As of 2015, the drug most likely to cause fatal overdose in Australia was diazepam (Valium). While fatal overdoses are highly associated with drugs such as opiates, cocaine and alcohol, deaths from other drugs such as caffeine are extremely rare.
This alphabetical list below contains 621 notable people whose deaths can be reliably sourced to be the result of drug overdose or acute drug intoxication. Where sources indicate drug overdose or intoxication was only suspected to be the cause of death, this will be specified in the 'notes' column.
Where sources are able to indicate, deaths are specified as 'suicide', 'accidental', 'undetermined', or otherwise in the 'cause' column. Where sources do not explicitly state intent, they will be listed in this column as 'unknown'.
Deaths from accidents or misadventure caused by drug overdoses or intoxication are also included on this list.
Deaths from long-term effects of drugs, such as tobacco-related cancers and cirrhosis from alcohol, are not included, nor are deaths from lethal injection or legal euthana.
Click here for a List of Deaths due to alcohol or drugs.
See also:
Poly drug use often carries more risk than use of a single drug, due to an increase in side effects, and drug synergy. For example, the chance of death from overdosing on opiates is greatly increased when they are consumed in conjunction with alcohol.
While they are two distinct phenomena, deaths from CDI are often misreported as overdoses. Drug overdoses and intoxication can also cause indirect deaths. For example, while marijuana does not cause fatal overdoses, being intoxicated by it can increase the chance of fatal traffic collisions.
Drug use and overdoses increased significantly in the 1800s due to the commercialization and availability of certain drugs. For example, while opium and coca had been used for centuries, their active ingredients, morphine and the cocaine alkaloid, were not isolated until 1803 and 1855 respectively.
Cocaine and various opiates were subsequently mass-produced and sold openly and legally in the Western world, resulting in widespread misuse and addiction. Drug use and addiction also increased significantly following the invention of the hypodermic syringe in 1853, with overdose being a leading cause of death among intravenous drug users.
Efforts to prohibit various drugs began to be enacted in the early 20th century, though the effectiveness of such policies is debated. Deaths from drug overdoses are increasing.
Between 2000 and 2014, fatal overdoses rose 137% in the United States, causing nearly half a million deaths in that period, and have also been continually increasing in Australia, Scotland, England, and Wales.
While prohibited drugs are generally viewed as being the most dangerous, the misuse of prescription drugs is linked to more deaths in several countries. Cocaine and heroin combined caused fewer deaths than prescriptions drugs in the United Kingdom in 2013, and fewer deaths than prescription opiates alone in the United States in 2008.
As of 2015, the drug most likely to cause fatal overdose in Australia was diazepam (Valium). While fatal overdoses are highly associated with drugs such as opiates, cocaine and alcohol, deaths from other drugs such as caffeine are extremely rare.
This alphabetical list below contains 621 notable people whose deaths can be reliably sourced to be the result of drug overdose or acute drug intoxication. Where sources indicate drug overdose or intoxication was only suspected to be the cause of death, this will be specified in the 'notes' column.
Where sources are able to indicate, deaths are specified as 'suicide', 'accidental', 'undetermined', or otherwise in the 'cause' column. Where sources do not explicitly state intent, they will be listed in this column as 'unknown'.
Deaths from accidents or misadventure caused by drug overdoses or intoxication are also included on this list.
Deaths from long-term effects of drugs, such as tobacco-related cancers and cirrhosis from alcohol, are not included, nor are deaths from lethal injection or legal euthana.
Click here for a List of Deaths due to alcohol or drugs.
See also:
- List of deaths through alcohol
- Lists of people by cause of death
- List of deaths from legal euthanasia and assisted suicide
- List of people executed by lethal injection
- Opioid epidemic
- United States drug overdose death rates and totals over time