Copyright © 2015 Bert N. Langford (Images may be subject to copyright. Please send feedback)
Welcome to Our Generation USA!
Health and Fitness
covers mental and physical health along with the means for prolonging one's life and quality of life, including health insurance.
Click Here for the Web Page "Modern Medicine"
Click Here for the Web Page "Sports"
Click Here for the Web Page "Civilization"
Health and Fitness including a Healthy Diet along with Physical Workouts
YouTube Video: Fat-Burning Cardio Dance Workout: Jane Fonda* - Doo-Wop
*-Jane Fonda
Pictured: L-R: A Gym and Healthy Vegetables and Fruit
Health is the ability to adapt and manage physical, mental and social challenges throughout life.
Since the late 1970s, the Federal Healthy People Initiative has been a visible component of the United States’ approach to improving population health. In each decade, a new version of Healthy People is issued (see history of healthy people), featuring updated goals and identifying topic areas and quantifiable objectives for health improvement during the succeeding ten years, with assessment at that point of progress or lack thereof.
Progress has been limited for many objectives, leading to concerns about the effectiveness of Healthy People in shaping outcomes in the context of a decentralized and uncoordinated US health system. Healthy People 2020 gives more prominence to health promotion and preventive approaches, and adds a substantive focus on the importance of addressing societal determinants of health.
A new expanded digital interface facilitates use and dissemination rather than bulky printed books as produced in the past. The impact of these changes to Healthy People will be determined in the coming years.
Systematic activities to prevent or cure health problems and promote good health in humans are undertaken by health care providers. The term "healthy" is also widely used in the context of many types of non-living organizations and their impacts for the benefit of humans, such as in the sense of healthy communities, healthy cities or healthy environments.
In addition to health care interventions and a person's surroundings, a number of other factors are known to influence the health status of individuals, including their background, lifestyle, and economic, social conditions, and spirituality; these are referred to as "determinants of health." Studies have shown that high levels of stress can affect human health.
Click on any of the following blue hyperlinks for further amplification on Health: ___________________________________________________________________________
A healthy diet provides the body with essential nutrition: fluid, adequate essential amino acids from protein, essential fatty acids, vitamins, minerals, and adequate calories. The requirements for a healthy diet can be met from a variety of plant-based and animal-based foods.
A healthy diet supports energy needs and provides for human nutrition without exposure to toxicity or excessive weight gain from consuming excessive amounts. Where lack of calories is not an issue, a properly balanced diet (in addition to exercise) is also thought to be important for lowering health risks, such as obesity, heart disease, type 2 diabetes, hypertension and cancer.
Various nutrition guides are published by medical and governmental institutions to educate the public on what they should be eating to promote health. Nutrition facts labels are also mandatory in some countries to allow consumers to choose between foods based on the components relevant to health.
Click on any of the following blue hyperlinks for further amplification:
Physical fitness is a general state of health and well-being and, more specifically, the ability to perform aspects of sports, occupations and daily activities. Physical fitness is generally achieved through proper nutrition, moderate-vigorous physical exercise, physical activity, and sufficient rest.
With automation and changes in lifestyles physical fitness is considered as a measure of the body's ability to function efficiently and effectively in work and leisure activities, to be healthy, to resist hypokinetic diseases, and to meet emergency situations.
Click on any of the following blue hyperlinks for further amplification: ____________________________________________________________
Physical exercise is any bodily activity that enhances or maintains physical fitness and overall health and wellness. It is performed for various reasons, including increasing growth and development, preventing aging, strengthening muscles and the cardiovascular system, honing athletic skills, weight loss or maintenance, and merely enjoyment.
Frequent and regular physical exercise boosts the immune system and helps prevent "diseases of affluence" such as cardiovascular disease, type 2 diabetes, and obesity.
It may also help prevent stress and depression, increase quality of sleep and act as a non-pharmaceutical sleep aid to treat diseases such as insomnia, help promote or maintain positive self-esteem, improve mental health, maintain steady digestion and treat constipation and gas, regulate fertility health, and augment an individual's sex appeal or body image, which has been found to be linked with higher levels of self-esteem.
Some care providers call exercise the "miracle" or "wonder" drug—alluding to the wide variety of benefits that it can provide for many individuals. Aside from the health advantages, these benefits may include different social rewards for staying active while enjoying the environment of one’s culture. Many individuals choose to exercise publicly outdoors where they can congregate in groups, socialize, and appreciate life.
In the United States, the CDC/ACSM consensus statement and the Surgeon General's report states that every adult should participate in moderate exercise, such as walking, swimming, and household tasks, for a minimum of 30 minutes daily.
Click on any of the following blue hyperlinks for further amplification:
Since the late 1970s, the Federal Healthy People Initiative has been a visible component of the United States’ approach to improving population health. In each decade, a new version of Healthy People is issued (see history of healthy people), featuring updated goals and identifying topic areas and quantifiable objectives for health improvement during the succeeding ten years, with assessment at that point of progress or lack thereof.
Progress has been limited for many objectives, leading to concerns about the effectiveness of Healthy People in shaping outcomes in the context of a decentralized and uncoordinated US health system. Healthy People 2020 gives more prominence to health promotion and preventive approaches, and adds a substantive focus on the importance of addressing societal determinants of health.
A new expanded digital interface facilitates use and dissemination rather than bulky printed books as produced in the past. The impact of these changes to Healthy People will be determined in the coming years.
Systematic activities to prevent or cure health problems and promote good health in humans are undertaken by health care providers. The term "healthy" is also widely used in the context of many types of non-living organizations and their impacts for the benefit of humans, such as in the sense of healthy communities, healthy cities or healthy environments.
In addition to health care interventions and a person's surroundings, a number of other factors are known to influence the health status of individuals, including their background, lifestyle, and economic, social conditions, and spirituality; these are referred to as "determinants of health." Studies have shown that high levels of stress can affect human health.
Click on any of the following blue hyperlinks for further amplification on Health: ___________________________________________________________________________
A healthy diet provides the body with essential nutrition: fluid, adequate essential amino acids from protein, essential fatty acids, vitamins, minerals, and adequate calories. The requirements for a healthy diet can be met from a variety of plant-based and animal-based foods.
A healthy diet supports energy needs and provides for human nutrition without exposure to toxicity or excessive weight gain from consuming excessive amounts. Where lack of calories is not an issue, a properly balanced diet (in addition to exercise) is also thought to be important for lowering health risks, such as obesity, heart disease, type 2 diabetes, hypertension and cancer.
Various nutrition guides are published by medical and governmental institutions to educate the public on what they should be eating to promote health. Nutrition facts labels are also mandatory in some countries to allow consumers to choose between foods based on the components relevant to health.
Click on any of the following blue hyperlinks for further amplification:
- Mainstream science
- Recommendations
- For specific conditions
- Reduced disease risk
- Unhealthy diets
- Popular diets
- Public health
- Cultural and psychological factors
- See also:
Physical fitness is a general state of health and well-being and, more specifically, the ability to perform aspects of sports, occupations and daily activities. Physical fitness is generally achieved through proper nutrition, moderate-vigorous physical exercise, physical activity, and sufficient rest.
With automation and changes in lifestyles physical fitness is considered as a measure of the body's ability to function efficiently and effectively in work and leisure activities, to be healthy, to resist hypokinetic diseases, and to meet emergency situations.
Click on any of the following blue hyperlinks for further amplification: ____________________________________________________________
Physical exercise is any bodily activity that enhances or maintains physical fitness and overall health and wellness. It is performed for various reasons, including increasing growth and development, preventing aging, strengthening muscles and the cardiovascular system, honing athletic skills, weight loss or maintenance, and merely enjoyment.
Frequent and regular physical exercise boosts the immune system and helps prevent "diseases of affluence" such as cardiovascular disease, type 2 diabetes, and obesity.
It may also help prevent stress and depression, increase quality of sleep and act as a non-pharmaceutical sleep aid to treat diseases such as insomnia, help promote or maintain positive self-esteem, improve mental health, maintain steady digestion and treat constipation and gas, regulate fertility health, and augment an individual's sex appeal or body image, which has been found to be linked with higher levels of self-esteem.
Some care providers call exercise the "miracle" or "wonder" drug—alluding to the wide variety of benefits that it can provide for many individuals. Aside from the health advantages, these benefits may include different social rewards for staying active while enjoying the environment of one’s culture. Many individuals choose to exercise publicly outdoors where they can congregate in groups, socialize, and appreciate life.
In the United States, the CDC/ACSM consensus statement and the Surgeon General's report states that every adult should participate in moderate exercise, such as walking, swimming, and household tasks, for a minimum of 30 minutes daily.
Click on any of the following blue hyperlinks for further amplification:
- Classification
- Health effects
- Mechanism of effects
- Public health measures
- Exercise trends
- Nutrition and recovery
- See also:
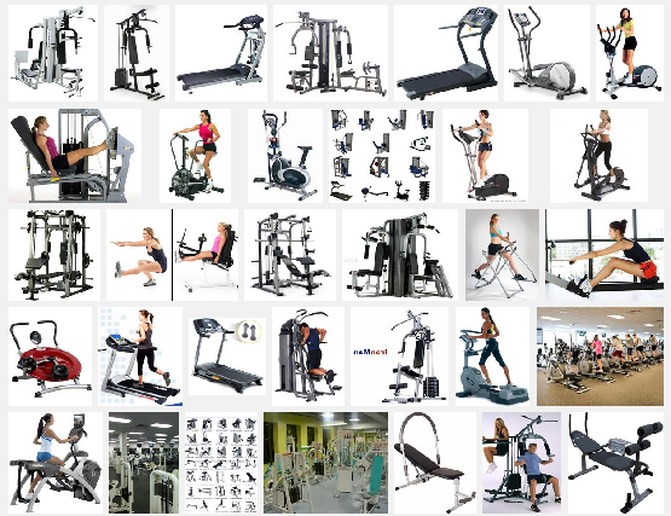
Gyms and Health Clubs in the United States
YouTube Video: Planet Fitness 30 Minute Circuit
YouTube Video: Join a Full Body with Cardio Workout with PF Trainer Teddy
Pictured below: Planet Fitness Gym Franchise (Click here for Planet Fitness Website)
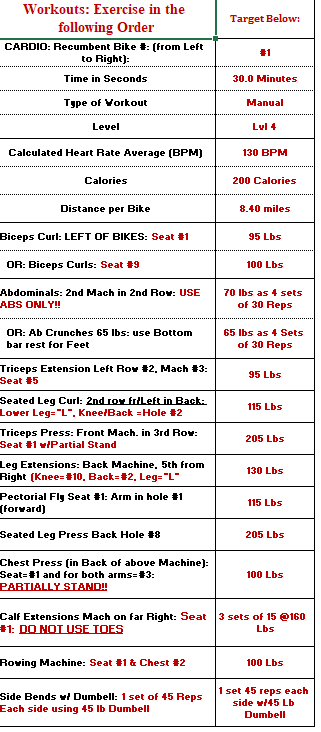
[Your Web Host: in order to overcome the heart disease my father's side of the family had suffered, I started working out at gyms primarily for cardio fitness during my freshman year at College (1961). I have kept up the practice still today, 60+ years later.
In my youth, I had a mixed exercise routine of jogging (25+ miles a week, even jogged around Central Park in NYC while in New York for business!), and free weights (in the 1990s I bench-pressed 345 pounds, which was twice my body weight then: today, a short cardio workout + machines to keep my heart and body tuned: it has worked!)
At 79+ years a day, I still go to the gym three times a week. For the past few years I have attended Planet Fitness at Mid-Rivers Mall, in Missouri. I have to say it is the best gym I've ever belonged to (and there have been dozens over the years!) The care and maintenance of their equipment is incredible and the staff is very friendly and supportive.
And, with oversize ceiling fans supplementing their air conditioning, there are not hot spots in the summer like other gyms! The floor covering is non-skid and durable. Many machines are duplicated, minimizing wait time.
First, I perform a 30+ minute cardio workout on a recumbent bike, a necessity due to left hip replacement surgery a few years back that prevents me from using treadmills or elliptical machines.
After finishing cardio, I then work out on machines for an additional 45-50 minutes.
I go to the gym in the afternoons on (minimally) Tuesday, Thursday and Saturday.
I decided to add Planet Fitness to this website after watching the New Year Eve celebration in Times Square last night on ABC: in many of the TV shots of the crowds, I saw those Purple and Yellow hats that some of my gym's staff had been wearing earlier: I found out from this Wikipedia description (below) that, since December 2014, Planet Fitness has been the official fitness sponsor of Dick Clark’s New Year’s Rockin’ Eve on ABC!]
___________________________________________________________________________
A gymnasium, also known as a gym, is a covered location for gymnastics, athletics, and gymnastic services. The word is derived from the ancient Greek gymnasium. They are commonly found in athletic and fitness centers. "Gym" is also slang for "fitness center", which is often an area for indoor recreation.
Gym apparatus such as barbells, parallel bars, jumping board, running path, tennis-balls, cricket field, fencing area, and so forth are used as exercises. In safe weather, outdoor locations are the most conducive to health.
See also:
Click on any of the following blue hyperlinks for additional information about a specific gym or health club in the United States:
In my youth, I had a mixed exercise routine of jogging (25+ miles a week, even jogged around Central Park in NYC while in New York for business!), and free weights (in the 1990s I bench-pressed 345 pounds, which was twice my body weight then: today, a short cardio workout + machines to keep my heart and body tuned: it has worked!)
At 79+ years a day, I still go to the gym three times a week. For the past few years I have attended Planet Fitness at Mid-Rivers Mall, in Missouri. I have to say it is the best gym I've ever belonged to (and there have been dozens over the years!) The care and maintenance of their equipment is incredible and the staff is very friendly and supportive.
And, with oversize ceiling fans supplementing their air conditioning, there are not hot spots in the summer like other gyms! The floor covering is non-skid and durable. Many machines are duplicated, minimizing wait time.
First, I perform a 30+ minute cardio workout on a recumbent bike, a necessity due to left hip replacement surgery a few years back that prevents me from using treadmills or elliptical machines.
After finishing cardio, I then work out on machines for an additional 45-50 minutes.
I go to the gym in the afternoons on (minimally) Tuesday, Thursday and Saturday.
I decided to add Planet Fitness to this website after watching the New Year Eve celebration in Times Square last night on ABC: in many of the TV shots of the crowds, I saw those Purple and Yellow hats that some of my gym's staff had been wearing earlier: I found out from this Wikipedia description (below) that, since December 2014, Planet Fitness has been the official fitness sponsor of Dick Clark’s New Year’s Rockin’ Eve on ABC!]
___________________________________________________________________________
A gymnasium, also known as a gym, is a covered location for gymnastics, athletics, and gymnastic services. The word is derived from the ancient Greek gymnasium. They are commonly found in athletic and fitness centers. "Gym" is also slang for "fitness center", which is often an area for indoor recreation.
Gym apparatus such as barbells, parallel bars, jumping board, running path, tennis-balls, cricket field, fencing area, and so forth are used as exercises. In safe weather, outdoor locations are the most conducive to health.
See also:
- Exercise trends
- Gym floor cover
- Gymkhana
- Largest high school gyms in the United States
- Outdoor gym
- Bodybuilding
- Physical exercise
- Physical fitness
Click on any of the following blue hyperlinks for additional information about a specific gym or health club in the United States:
- Club Fitness
- Club One
- Crunch Fitness
- Curves International
- Equinox Fitness
- Orangetheory Fitness
- 24 Hour Fitness
- Planet Fitness
- Gold's Gym
- Snap Fitness
- Anytime Fitness 2000 locations
- LA Fitness
- Youfit
- Town Sports International DBA NYSC, BSC, WSC and PSC
Dieting, including a List of Diets as well as the Best Commercial Diets according to U.S. News and World Report
- YouTube Video: How to Lose Weight on Weight Watchers | Diet Plan
- YouTube: The BEST DIETS For Weight Loss I've Used
- YouTube Video: Losing Weight on the South Beach Diet
Click here for a List of Diets.
Dieting is the practice of eating food in a regulated and supervised fashion to decrease, maintain, or increase body weight, or to prevent and treat diseases, such as diabetes.
A restricted diet is often used by those who are overweight or obese, sometimes in combination with physical exercise, to reduce body weight. Some people follow a diet to gain weight (usually in the form of muscle). Diets can also be used to maintain a stable body weight and improve health.
Diets to promote weight loss can be categorized as:
A meta-analysis of six randomized controlled trials found no difference between low-calorie, low-carbohydrate, and low-fat diets, with a 2–4 kilogram weight loss over 12–18 months in all studies.
At two years, all calorie-reduced diet types cause equal weight loss irrespective of the macro-nutrients emphasized. In general, the most effective diet is any which reduces calorie consumption.
A study published in American Psychologist found that short-term dieting involving "severe restriction of calorie intake" does not lead to "sustained improvements in weight and health for the majority of individuals". Other studies have found that the average individual maintains some weight loss after dieting. Weight loss by dieting, while of benefit to those classified as unhealthy, may slightly increase the mortality rate for individuals who are otherwise healthy.
The first popular diet was "Banting", named after William Banting. In his 1863 pamphlet, Letter on Corpulence, Addressed to the Public, he outlined the details of a particular low-carbohydrate, low-calorie diet that had led to his own dramatic weight loss.
Click on any of the following blue hyperlinks for more about Dieting:
Best Commercial Diet Plans by U.S. News and World Report (1/2/2019)
Brand-name diet programs might come to mind when choosing a diet that's the right fit for you. Health experts who rated the diet plans below found wide differences in effectiveness.
Among the qualities considered by the panelists were each diet's ability to deliver weight loss, provide good nutrition and safety, and be relatively easy to follow. Topping the Best Commercial Diet Plans ranking list are Weight Watchers, Jenny Craig and the Nutritarian diet.
Read the Best Diets methodology
Listed below are the top 4 diet plans (of the 13 covered under this article):
Weight Watchers Ranked #1 in Best Commercial Diet Plans:
What is WW (Weight Watchers) Diet? This diet has been reviewed by U.S. News' team of expert panelists. Learn more »
Although still used to shed pounds, WW (formerly Weight Watchers) is also focused on inspiring healthy living and improving overall well-being. That includes taking a holistic approach to help members eat healthier and move more.
Its WW Freestyle program, launched in late 2017, builds on its SmartPoints system, which assigns every food and beverage a point value, based on its nutrition. The program expands dietary options that are 0 points from only fruits and vegetables to more than 200 foods, including eggs, seafood and corn.
A backbone of the plan is multi-model access (via in-person workshops, online chat or phone) to support from people who lost weight using WW, kept it off and have been trained in behavioral weight management techniques.
Balanced Diet:
These diets fall within accepted ranges for the amount of protein, carbs, fat and other nutrients they provide.
Pros & Cons
U.S. News Best Diet Rankings:
WW (Weight Watchers) Diet ranked #4 in Best Diets Overall. 41 diets were evaluated with input from a panel of health experts. See how we rank diets here.
WW (Weight Watchers) Diet is ranked:
Overall
How does WW (Weight Watchers) Diet work?:
For those who join WW via a Digital, Workshop or Personal Coaching membership, there’s no fixed membership period. But you can continue with the program after you’ve shed unwanted pounds to receive continued guidance on eating and healthy living. WW also recently rolled out a program specifically for those who want to build healthy habits without focusing on weight loss.
The SmartPoints system guides members toward an overall eating pattern that is lower in calories, saturated fat and sugar, and higher in protein, and the WW Freestyle program offers participants even more freedom and flexibility, with 200 foods to choose from that are 0 points, including eggs, corn, fish, seafood, skinless chicken or turkey breast, non-fat plain yogurt, beans, peas, lentils and tofu.
These foods help lay a foundation for healthier pattern of eating and there’s a low risk for overeating them, WW says. However, you can eat whatever you want – provided you stick to your daily SmartPoints target, a number based on your gender, weight, height and age.
The company offers thousands of recipes, each with a SmartPoints value, to show how it fits into your eating plan, and you can find the points values for more than 285,000 foods on the mobile app or desktop food database. If you’re preparing a dish that’s not listed in the database, you can calculate the points value ingredient by ingredient, using your mobile app or through the company’s website.
Click here for full article on Weight Watchers Commercial Diet Plan.
___________________________________________________________________________
Jenny Craig Diet Ranked #2 in Best Commercial Diet Plans
What is Jenny Craig Diet?This diet has been reviewed by U.S. News' team of expert panelists. Learn more »
Losing weight is as simple as managing calories, fat and portions on Jenny Craig. Jenny's prepackaged meals and recipes do all three, plus emphasize healthy eating, an active lifestyle and behavior modification. Personal consultants guide members through their journeys from day one.
You'll gain support and motivation, and learn how much you should be eating, what a balanced meal looks like and how to use that knowledge to achieve weight maintenance. By following the plan, you’re expected to drop up to 2 pounds a week.
Jenny Craig offers three programs: its standard “Classic” program, Rapid Results and Jenny Craig for Type 2, which is designed for people with Type 2 diabetes by including a lower-carb menu, reinforcement of self-monitoring of blood sugar levels, consistent meals and snacks, and other self-management strategies for weight loss and support for diabetes control.
Jenny Craig’s DNA Decoder Plan, which will match members’ genetic markers to their optimal nutritional program and action plan, will be launched in late November 2019.
Balanced Diet:
These diets fall within accepted ranges for the amount of protein, carbs, fat and other nutrients they provide.
Pros & Cons
U.S. News Best Diet Rankings:
Jenny Craig Diet ranked #11 in Best Diets Overall. 41 diets were evaluated with input from a panel of health experts. See how we rank diets here.
Jenny Craig Diet is ranked:
Overall
How does Jenny Craig Diet work?
To get started on Jenny Craig, you’ll just need to sign up and walk through your individual plan. For the first half of your weight loss program, you eat three prepackaged Jenny meals and one snack a day – options like cinnamon rolls and homestyle beef pot roast – in addition to five servings of fresh fruits and vegetables and at least two nonfat dairy product equivalents.
You'll get a personalized meal and exercise plan, plus weekly one-on-one counseling sessions with a Jenny Craig consultant. Note: These are not nutrition professionals – anyone who is "health-oriented and customer-focused" can attend a training course and get certified – but they're trained in the basics of nutrition, exercise and behavior modification through a curriculum developed by registered dietitians in consultation with a science advisory board.
Many consultants are former Jenny Craig members. Your diet, which ranges from 1,200 to 2,300 calories a day, is designed around your current weight, age, gender, height, goal weight and fitness habits.
The diet lasts as long as you need it to, be it three months or two years. Once you're halfway to your goal weight, the Jenny Craig consultant begins working with you to cook some meals for yourself again, using Jenny's recipes and low-fat food prep strategies.
After reaching your goal weight, you'll spend four weeks transitioning back to making only your own meals, while adjusting to a slightly higher number of daily calories. In monthly consultations, you learn weight regain prevention strategies such as nutritional label reading, exercise and stress management.
One-on-one support plays a big role, although Jenny participants don't get together for group meetings, which is a part of some commercial diets. Instead, you'll typically talk with your personal consultant once a week, either in person at a center or through the Jenny Craig Anywhere program, which offers consultations by phone or via video chat.
No matter how you connect with your consultant, you'll discuss how well you did the previous week, and whether you had trouble sticking to the plan. You'll also choose the next week's meals and order your food. On-the-go members who opt for "Jenny Craig Anywhere" have access to the same meals as those who pick up their meals in a center.
In 2018, Jenny Craig launched its Rapid Results plan, which is based on science involving the body clock’s circadian rhythms. The difference is in the timing – you eat during a 12-hour nourishment period, then take a break for a 12-hour rejuvenation period (which includes sleep).
Click here for full article about the Jenny Craig Diet.
___________________________________________________________________________
Click here for Nutritarian Diet: Rated #3 in Best Commercial Diet
___________________________________________________________________________
Click here for South Beach Diet: Rated #4 in Best Commercial Diet.
___________________________________________________________________________
Click here for Remaining Diets considered as Best Commercial Diets as ranked by U.S. News World Report.
Dieting is the practice of eating food in a regulated and supervised fashion to decrease, maintain, or increase body weight, or to prevent and treat diseases, such as diabetes.
A restricted diet is often used by those who are overweight or obese, sometimes in combination with physical exercise, to reduce body weight. Some people follow a diet to gain weight (usually in the form of muscle). Diets can also be used to maintain a stable body weight and improve health.
Diets to promote weight loss can be categorized as:
- low-fat,
- low-carbohydrate,
- low-calorie,
- very low calorie
- and more recently flexible dieting.
A meta-analysis of six randomized controlled trials found no difference between low-calorie, low-carbohydrate, and low-fat diets, with a 2–4 kilogram weight loss over 12–18 months in all studies.
At two years, all calorie-reduced diet types cause equal weight loss irrespective of the macro-nutrients emphasized. In general, the most effective diet is any which reduces calorie consumption.
A study published in American Psychologist found that short-term dieting involving "severe restriction of calorie intake" does not lead to "sustained improvements in weight and health for the majority of individuals". Other studies have found that the average individual maintains some weight loss after dieting. Weight loss by dieting, while of benefit to those classified as unhealthy, may slightly increase the mortality rate for individuals who are otherwise healthy.
The first popular diet was "Banting", named after William Banting. In his 1863 pamphlet, Letter on Corpulence, Addressed to the Public, he outlined the details of a particular low-carbohydrate, low-calorie diet that had led to his own dramatic weight loss.
Click on any of the following blue hyperlinks for more about Dieting:
- History
- Types
- Nutrition
- How the body eliminates fat
- Weight loss groups
- Food diary
- Possible weight loss effects of drinking water prior to meals
- Fasting
- Crash Dieting
- Side effects
- Low carbohydrate versus low fat
- Low glycemic index
- See also:
- Body image
- Carbon footprint
- Eating disorder
- Food faddism
- High residue diet
- National Weight Control Registry
- Nutrigenomics
- Nutrition psychology
- Nutrition scale
- Nutritional rating systems
- Online weight loss plans
- Superfood
- Table of food nutrients
- Underweight
- Dieting at Curlie
- A PBS Frontline interview with Prof. Walter Willett, Chair of Harvard's nutrition department (2004)
- "Not All Calories Are Created Equal, Author Says". Excerpt from Good Calories, Bad Calories and NPR interview with Gary Taubes and Dr. Ronald Krauss (2 November 2007).
Best Commercial Diet Plans by U.S. News and World Report (1/2/2019)
Brand-name diet programs might come to mind when choosing a diet that's the right fit for you. Health experts who rated the diet plans below found wide differences in effectiveness.
Among the qualities considered by the panelists were each diet's ability to deliver weight loss, provide good nutrition and safety, and be relatively easy to follow. Topping the Best Commercial Diet Plans ranking list are Weight Watchers, Jenny Craig and the Nutritarian diet.
Read the Best Diets methodology
Listed below are the top 4 diet plans (of the 13 covered under this article):
Weight Watchers Ranked #1 in Best Commercial Diet Plans:
What is WW (Weight Watchers) Diet? This diet has been reviewed by U.S. News' team of expert panelists. Learn more »
Although still used to shed pounds, WW (formerly Weight Watchers) is also focused on inspiring healthy living and improving overall well-being. That includes taking a holistic approach to help members eat healthier and move more.
Its WW Freestyle program, launched in late 2017, builds on its SmartPoints system, which assigns every food and beverage a point value, based on its nutrition. The program expands dietary options that are 0 points from only fruits and vegetables to more than 200 foods, including eggs, seafood and corn.
A backbone of the plan is multi-model access (via in-person workshops, online chat or phone) to support from people who lost weight using WW, kept it off and have been trained in behavioral weight management techniques.
Balanced Diet:
These diets fall within accepted ranges for the amount of protein, carbs, fat and other nutrients they provide.
Pros & Cons
- Eat what you want; no foods off-limits
- Flexibility to shape your own diet
- Participation can be pricey, though often deemed a good value, depending on the program you choose
U.S. News Best Diet Rankings:
WW (Weight Watchers) Diet ranked #4 in Best Diets Overall. 41 diets were evaluated with input from a panel of health experts. See how we rank diets here.
WW (Weight Watchers) Diet is ranked:
- #4 (tie) in
Best Diets Overall - #1 in
Best Weight-Loss Diets - #1 in
Best Commercial Diet Plans - #6 (tie) in
Best Diabetes Diets - #6 (tie) in
Best Diets for Healthy Eating - #2 (tie) in
Best Fast Weight-Loss Diets - #13 (tie) in
Best Heart-Healthy Diets - #2 (tie) in
Easiest Diets to Follow
Overall
How does WW (Weight Watchers) Diet work?:
For those who join WW via a Digital, Workshop or Personal Coaching membership, there’s no fixed membership period. But you can continue with the program after you’ve shed unwanted pounds to receive continued guidance on eating and healthy living. WW also recently rolled out a program specifically for those who want to build healthy habits without focusing on weight loss.
The SmartPoints system guides members toward an overall eating pattern that is lower in calories, saturated fat and sugar, and higher in protein, and the WW Freestyle program offers participants even more freedom and flexibility, with 200 foods to choose from that are 0 points, including eggs, corn, fish, seafood, skinless chicken or turkey breast, non-fat plain yogurt, beans, peas, lentils and tofu.
These foods help lay a foundation for healthier pattern of eating and there’s a low risk for overeating them, WW says. However, you can eat whatever you want – provided you stick to your daily SmartPoints target, a number based on your gender, weight, height and age.
The company offers thousands of recipes, each with a SmartPoints value, to show how it fits into your eating plan, and you can find the points values for more than 285,000 foods on the mobile app or desktop food database. If you’re preparing a dish that’s not listed in the database, you can calculate the points value ingredient by ingredient, using your mobile app or through the company’s website.
Click here for full article on Weight Watchers Commercial Diet Plan.
___________________________________________________________________________
Jenny Craig Diet Ranked #2 in Best Commercial Diet Plans
What is Jenny Craig Diet?This diet has been reviewed by U.S. News' team of expert panelists. Learn more »
Losing weight is as simple as managing calories, fat and portions on Jenny Craig. Jenny's prepackaged meals and recipes do all three, plus emphasize healthy eating, an active lifestyle and behavior modification. Personal consultants guide members through their journeys from day one.
You'll gain support and motivation, and learn how much you should be eating, what a balanced meal looks like and how to use that knowledge to achieve weight maintenance. By following the plan, you’re expected to drop up to 2 pounds a week.
Jenny Craig offers three programs: its standard “Classic” program, Rapid Results and Jenny Craig for Type 2, which is designed for people with Type 2 diabetes by including a lower-carb menu, reinforcement of self-monitoring of blood sugar levels, consistent meals and snacks, and other self-management strategies for weight loss and support for diabetes control.
Jenny Craig’s DNA Decoder Plan, which will match members’ genetic markers to their optimal nutritional program and action plan, will be launched in late November 2019.
Balanced Diet:
These diets fall within accepted ranges for the amount of protein, carbs, fat and other nutrients they provide.
Pros & Cons
- No guesswork
- Prepackaged meals, delivered
- Home-cooked and restaurant meals largely off-limits
- Budget-buster
U.S. News Best Diet Rankings:
Jenny Craig Diet ranked #11 in Best Diets Overall. 41 diets were evaluated with input from a panel of health experts. See how we rank diets here.
Jenny Craig Diet is ranked:
- #11 (tie) in
Best Diets Overall - #3 (tie) in
Best Weight-Loss Diets - #2 in
Best Commercial Diet Plans - #6 (tie) in
Best Diabetes Diets - #15 (tie) in
Best Diets for Healthy Eating - #6 (tie) in
Best Fast Weight-Loss Diets - #19 (tie) in
Best Heart-Healthy Diets - #7 in
Easiest Diets to Follow
Overall
How does Jenny Craig Diet work?
To get started on Jenny Craig, you’ll just need to sign up and walk through your individual plan. For the first half of your weight loss program, you eat three prepackaged Jenny meals and one snack a day – options like cinnamon rolls and homestyle beef pot roast – in addition to five servings of fresh fruits and vegetables and at least two nonfat dairy product equivalents.
You'll get a personalized meal and exercise plan, plus weekly one-on-one counseling sessions with a Jenny Craig consultant. Note: These are not nutrition professionals – anyone who is "health-oriented and customer-focused" can attend a training course and get certified – but they're trained in the basics of nutrition, exercise and behavior modification through a curriculum developed by registered dietitians in consultation with a science advisory board.
Many consultants are former Jenny Craig members. Your diet, which ranges from 1,200 to 2,300 calories a day, is designed around your current weight, age, gender, height, goal weight and fitness habits.
The diet lasts as long as you need it to, be it three months or two years. Once you're halfway to your goal weight, the Jenny Craig consultant begins working with you to cook some meals for yourself again, using Jenny's recipes and low-fat food prep strategies.
After reaching your goal weight, you'll spend four weeks transitioning back to making only your own meals, while adjusting to a slightly higher number of daily calories. In monthly consultations, you learn weight regain prevention strategies such as nutritional label reading, exercise and stress management.
One-on-one support plays a big role, although Jenny participants don't get together for group meetings, which is a part of some commercial diets. Instead, you'll typically talk with your personal consultant once a week, either in person at a center or through the Jenny Craig Anywhere program, which offers consultations by phone or via video chat.
No matter how you connect with your consultant, you'll discuss how well you did the previous week, and whether you had trouble sticking to the plan. You'll also choose the next week's meals and order your food. On-the-go members who opt for "Jenny Craig Anywhere" have access to the same meals as those who pick up their meals in a center.
In 2018, Jenny Craig launched its Rapid Results plan, which is based on science involving the body clock’s circadian rhythms. The difference is in the timing – you eat during a 12-hour nourishment period, then take a break for a 12-hour rejuvenation period (which includes sleep).
Click here for full article about the Jenny Craig Diet.
___________________________________________________________________________
Click here for Nutritarian Diet: Rated #3 in Best Commercial Diet
___________________________________________________________________________
Click here for South Beach Diet: Rated #4 in Best Commercial Diet.
___________________________________________________________________________
Click here for Remaining Diets considered as Best Commercial Diets as ranked by U.S. News World Report.
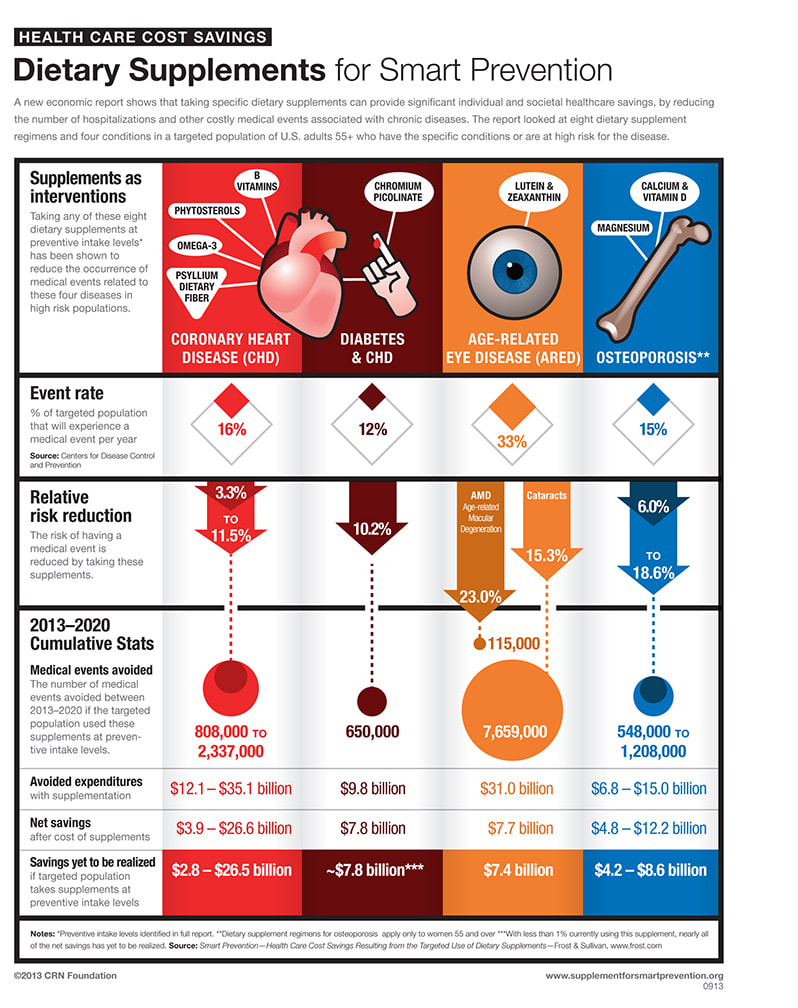
Dietary Supplements
- YouTube Video: Vitamins, Supplements and Heart Disease
- YouTube Video: Making Heart Attacks History: Caldwell Esselstyn at TEDxCambridge 2011
- YouTube Video: 6 Supplements That Might Actually Help You
A dietary supplement is a manufactured product intended to supplement the diet when taken by mouth as a pill, capsule, tablet, or liquid. A supplement can provide nutrients either extracted from food sources or synthetic, individually or in combination, in order to increase the quantity of their consumption.
The class of nutrient compounds includes vitamins, minerals, fiber, fatty acids and amino acids. Dietary supplements can also contain substances that have not been confirmed as being essential to life, but are marketed as having a beneficial biological effect, such as plant pigments or polyphenols. Animals can also be a source of supplement ingredients, as for example collagen from chickens or fish. These are also sold individually and in combination, and may be combined with nutrient ingredients.
In the United States and Canada, dietary supplements are considered a subset of foods, and are regulated accordingly. The European Commission has also established harmonized rules to help insure that food supplements are safe and properly labeled.
Creating an industry estimated to have a 2015 value of $37 billion, there are more than 50,000 dietary supplement products marketed just in the United States, where about 50% of the American adult population consumes dietary supplements. Multivitamins are the most commonly used product.
For those who fail to consume a balanced diet, the United States National Institutes of Health states that certain supplements "may have value."
In the United States, it is against federal regulations for supplement manufacturers to claim that these products prevent or treat any disease. Companies are allowed to use what is referred to as "Structure/Function" wording if there is substantiation of scientific evidence for a supplement providing a potential health effect.
An example would be "_____ helps maintain healthy joints", but the label must bear a disclaimer that the Food and Drug Administration (FDA) "has not evaluated the claim and that the dietary supplement product is not intended to "diagnose, treat, cure or prevent any disease," because only a drug can legally make such a claim.
The FDA enforces these regulations, and also prohibits the sale of supplements and supplement ingredients that are dangerous, or supplements not made according to standardized good manufacturing practices (GMPs).
Click on any of the following blue hyperlinks for more about Dietary Supplements:
The class of nutrient compounds includes vitamins, minerals, fiber, fatty acids and amino acids. Dietary supplements can also contain substances that have not been confirmed as being essential to life, but are marketed as having a beneficial biological effect, such as plant pigments or polyphenols. Animals can also be a source of supplement ingredients, as for example collagen from chickens or fish. These are also sold individually and in combination, and may be combined with nutrient ingredients.
In the United States and Canada, dietary supplements are considered a subset of foods, and are regulated accordingly. The European Commission has also established harmonized rules to help insure that food supplements are safe and properly labeled.
Creating an industry estimated to have a 2015 value of $37 billion, there are more than 50,000 dietary supplement products marketed just in the United States, where about 50% of the American adult population consumes dietary supplements. Multivitamins are the most commonly used product.
For those who fail to consume a balanced diet, the United States National Institutes of Health states that certain supplements "may have value."
In the United States, it is against federal regulations for supplement manufacturers to claim that these products prevent or treat any disease. Companies are allowed to use what is referred to as "Structure/Function" wording if there is substantiation of scientific evidence for a supplement providing a potential health effect.
An example would be "_____ helps maintain healthy joints", but the label must bear a disclaimer that the Food and Drug Administration (FDA) "has not evaluated the claim and that the dietary supplement product is not intended to "diagnose, treat, cure or prevent any disease," because only a drug can legally make such a claim.
The FDA enforces these regulations, and also prohibits the sale of supplements and supplement ingredients that are dangerous, or supplements not made according to standardized good manufacturing practices (GMPs).
Click on any of the following blue hyperlinks for more about Dietary Supplements:
- Definition
- Types
- Industry
- Controversy
- Adverse effects
- Society and culture
- Research
- See also:
- Bodybuilding supplement
- Nutrient
- Food fortification
- Megavitamin therapy
- Nutraceutical
- Dietary Supplement Health and Education Act of 1994
- Multivitamin
- Dietary Supplements (database) (PubMed)
- Alternative Medicine
- ConsumerLab.com
- Examine.com
- Natural Standard
- MedlinePlus, Herbs and Supplements, United States National Library of Medicine
- Using Dietary Supplements Wisely, U.S. National Center for Complementary and Integrative Health
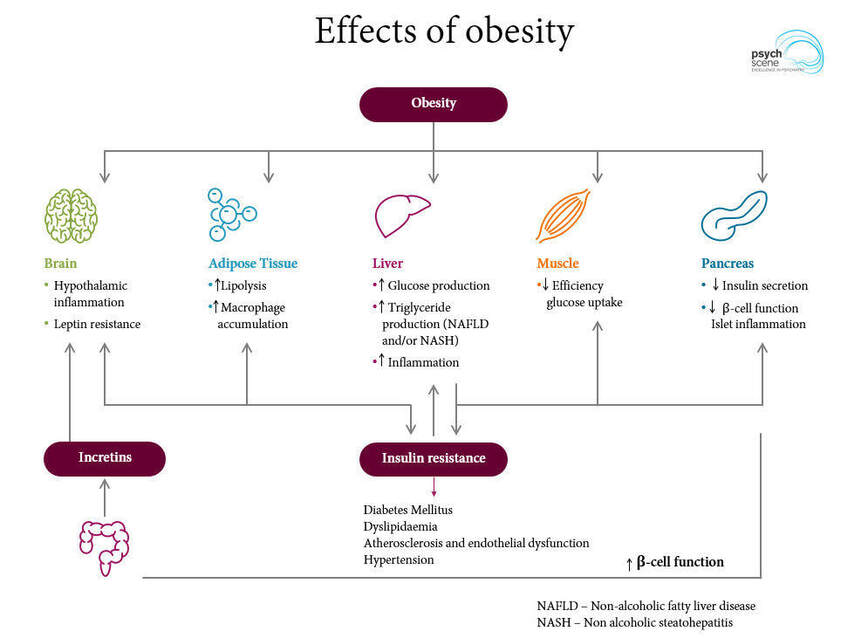
Obesity in the United States based on Body Mass Index (BMI)
- YouTube Video: Huge rise in child and teen obesity, says WHO
- YouTube Video: Obesity in America by ABC News
- YouTube Video: How to Speed Up Your Metabolism
Obesity in the United States is a major health issue, resulting in numerous diseases, specifically increased risk of certain types of cancer, coronary artery disease, type 2 diabetes, stroke, as well as significant increases in early mortality and economic costs. While many industrialized countries have experienced similar increases, obesity rates in the United States are the highest in the world.
An obese person in the United States incurs an average of $1,429 more in medical expenses annually. Approximately $147 billion is spent in added medical expenses per year within the United States. This number is expected to increase approximately $1.24 billion per year until the year 2030.
The United States had the highest rate of obesity within the OECD grouping of large trading economies. From 23% obesity in 1962, estimates have steadily increased. 2014 figures from the CDC found that more than one-third (36.5%) of U.S. adults age 20 and older and 17% of children and adolescents aged 2–19 years were obese.
A second study from the National Center for Health Statistics at the CDC showed that 39.6% of US adults age 20 and older were obese as of 2015-2016 (37.9% for men and 41.1% for women).
Obesity in an adult is defined as a BMI of 30 and above. Overweight in an adult is defined as a BMI of greater than 25 and less than 30, (so 25.01-29.9999). For children, obesity is defined as BMI 95th percentile or greater for gender/age on a growth chart and overweight is defined as BMI 85th percentile to 94.999th%.
Overweight or obese: For the following statistics, adults is defined as age 20 and over. The overweight + obese percentages for the overall US population are higher reaching:
In 2010 65.7% of American adults and 17% of American children are overweight or obese, and 63% of teenage girls become overweight by age 11.
In 2013 the Organisation for Economic Co-operation and Development (OECD) found that 57.6% of American citizens were overweight or obese. The organization estimates that 3/4 of the American population will likely be overweight or obese by 2020. A forecast based on early long-term trends suggests that more than 85% of adults will be overweight or obese in the U.S. by 2030.
Obesity has been cited as a contributing factor to approximately 100,000–400,000 deaths in the United States per year and has increased health care use and expenditures, costing society an estimated $117 billion in direct (preventive, diagnostic, and treatment services related to weight) and indirect (absenteeism, loss of future earnings due to premature death) costs. This exceeds health care costs associated with smoking and accounts for 6% to 12% of national health care expenditures in the United States.
Click on any of the following blue hyperlinks for more about Obesity in the United States:
Body mass index (BMI) is a value derived from the mass (weight) and height of a person. The BMI is defined as the body mass divided by the square of the body height, and is universally expressed in units of kg/m2, resulting from mass in kilograms and height in metres.
The BMI may also be determined using a table or chart which displays BMI as a function of mass and height using contour lines or colours for different BMI categories, and which may use other units of measurement (converted to metric units for the calculation).
The BMI is a convenient rule of thumb used to broadly categorize a person as underweight, normal weight, overweight, or obese based on tissue mass (muscle, fat, and bone) and height. That categorization is the subject of some debate about where on the BMI scale the dividing lines between categories should be placed. Commonly accepted BMI ranges are underweight: under 18.5 kg/m2, normal weight: 18.5 to 25, overweight: 25 to 30, obese: over 30.
BMIs under 20.0 and over 25.0 have been associated with higher all-cause mortality, increasing risk with distance from the 20.0–25.0 range. The prevalence of overweight and obesity is the highest in the Americas and lowest in Southeast Asia. The prevalence of overweight and obesity in high income and upper middle income countries is more than double that of low and lower middle income countries.
Click on any of the following blue hyperlinks for more about Body Mass Index:
An obese person in the United States incurs an average of $1,429 more in medical expenses annually. Approximately $147 billion is spent in added medical expenses per year within the United States. This number is expected to increase approximately $1.24 billion per year until the year 2030.
The United States had the highest rate of obesity within the OECD grouping of large trading economies. From 23% obesity in 1962, estimates have steadily increased. 2014 figures from the CDC found that more than one-third (36.5%) of U.S. adults age 20 and older and 17% of children and adolescents aged 2–19 years were obese.
A second study from the National Center for Health Statistics at the CDC showed that 39.6% of US adults age 20 and older were obese as of 2015-2016 (37.9% for men and 41.1% for women).
Obesity in an adult is defined as a BMI of 30 and above. Overweight in an adult is defined as a BMI of greater than 25 and less than 30, (so 25.01-29.9999). For children, obesity is defined as BMI 95th percentile or greater for gender/age on a growth chart and overweight is defined as BMI 85th percentile to 94.999th%.
Overweight or obese: For the following statistics, adults is defined as age 20 and over. The overweight + obese percentages for the overall US population are higher reaching:
- 39.4% in 1997,
- 44.5% in 2004,
- 56.6% in 2007,
- 63.8% (adults) and 17% (children) in 2008.
In 2010 65.7% of American adults and 17% of American children are overweight or obese, and 63% of teenage girls become overweight by age 11.
In 2013 the Organisation for Economic Co-operation and Development (OECD) found that 57.6% of American citizens were overweight or obese. The organization estimates that 3/4 of the American population will likely be overweight or obese by 2020. A forecast based on early long-term trends suggests that more than 85% of adults will be overweight or obese in the U.S. by 2030.
Obesity has been cited as a contributing factor to approximately 100,000–400,000 deaths in the United States per year and has increased health care use and expenditures, costing society an estimated $117 billion in direct (preventive, diagnostic, and treatment services related to weight) and indirect (absenteeism, loss of future earnings due to premature death) costs. This exceeds health care costs associated with smoking and accounts for 6% to 12% of national health care expenditures in the United States.
Click on any of the following blue hyperlinks for more about Obesity in the United States:
- Prevalence
- Epidemiology
- Contributing factors
- Total costs to the US
- Effects on life expectancy
- Anti-obesity efforts
- Accommodations
- See also
- Centers for Disease Control: Obesity Data and Statistics
- American Obesity Treatment Association: Obesity Education and Statistics
- Contributors to Obesity | Tableau Public (infographic for the United States)
- List of countries by Body Mass Index (BMI)
- Obesogen
- Hunger in the United States
- EPODE International Network, the world's largest obesity-prevention network
- World Fit, a program of the United States Olympic Committee
- Fat acceptance movement
- Documentaries:
Body mass index (BMI) is a value derived from the mass (weight) and height of a person. The BMI is defined as the body mass divided by the square of the body height, and is universally expressed in units of kg/m2, resulting from mass in kilograms and height in metres.
The BMI may also be determined using a table or chart which displays BMI as a function of mass and height using contour lines or colours for different BMI categories, and which may use other units of measurement (converted to metric units for the calculation).
The BMI is a convenient rule of thumb used to broadly categorize a person as underweight, normal weight, overweight, or obese based on tissue mass (muscle, fat, and bone) and height. That categorization is the subject of some debate about where on the BMI scale the dividing lines between categories should be placed. Commonly accepted BMI ranges are underweight: under 18.5 kg/m2, normal weight: 18.5 to 25, overweight: 25 to 30, obese: over 30.
BMIs under 20.0 and over 25.0 have been associated with higher all-cause mortality, increasing risk with distance from the 20.0–25.0 range. The prevalence of overweight and obesity is the highest in the Americas and lowest in Southeast Asia. The prevalence of overweight and obesity in high income and upper middle income countries is more than double that of low and lower middle income countries.
Click on any of the following blue hyperlinks for more about Body Mass Index:
- History
- Scalability
- Categories
- Consequences of elevated level in adults
- Applications
- Limitations
- Alternatives
- See also:
- Allometry
- Body fat percentage (BFP)
- Relative Fat Mass (RFM)
- Body water
- Corpulence index
- History of anthropometry
- List of countries by Body Mass Index (BMI)
- Obesity paradox
- Somatotype and constitutional psychology
- U.S. National Center for Health Statistics:
Alcohol Consumption and its Impact on Health as well as Alcoholics Anonymous (AA) in overcoming Alcoholism
- YouTube Video: Your Brain on Alcohol
- YouTube Video: How I overcame alcoholism | Claudia Christian | TEDxLondonBusinessSchool
- YouTube Video: Best AA speech ever
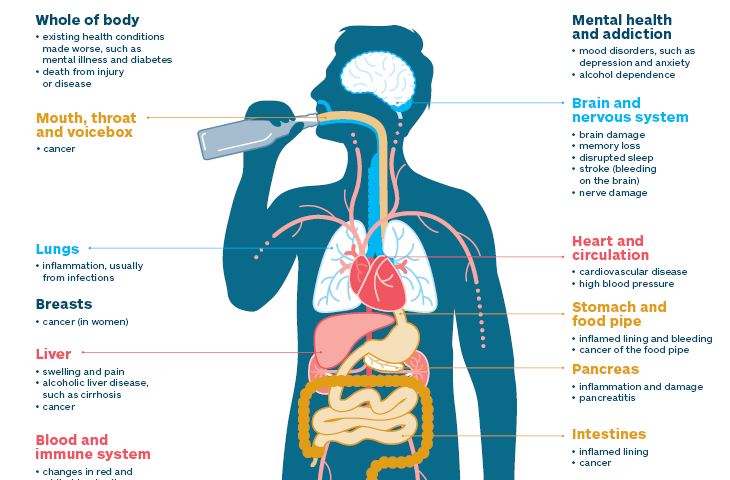
Alcohol (also known as ethanol) has a number of effects on health.
Short-term effects of alcohol consumption include intoxication and dehydration.
Long-term effects of alcohol consumption include changes in the metabolism of the liver and brain and alcoholism.
Alcohol intoxication affects the brain, causing slurred speech, clumsiness, and delayed reflexes. Alcohol stimulates insulin production, which speeds up glucose metabolism and can result in low blood sugar, causing irritability and possibly death for diabetics.
Even light and moderate alcohol consumption increases cancer risk in individuals. A 2014 World Health Organization report found that harmful alcohol consumption caused about 3.3 million deaths annually worldwide. Negative efforts are related to the amount consumed with no safe lower limit seen. Some nations have introduced alcohol packaging warning messages that inform consumers about alcohol and cancer, as well as foetal alcohol syndrome.
The median lethal dose of alcohol in test animals is a blood alcohol content of 0.45%. This is about six times the level of ordinary intoxication (0.08%), but vomiting or unconsciousness may occur much sooner in people who have a low tolerance for alcohol. The high tolerance of chronic heavy drinkers may allow some of them to remain conscious at levels above 0.40%, although serious health hazards are incurred at this level.
Alcohol also limits the production of vasopressin (ADH) from the hypothalamus and the secretion of this hormone from the posterior pituitary gland. This is what causes severe dehydration when alcohol is consumed in large amounts. It also causes a high concentration of water in the urine and vomit and the intense thirst that goes along with a hangover.
Stress, hangovers, and the oral contraceptive pill may increase the desire for alcohol because these things will lower the level of testosterone and alcohol will acutely elevate it. Tobacco has the same effect of increasing the craving for alcohol.
Short Term Effects:
Main article: Short-term effects of alcohol
The short-term effects of alcohol consumption range from a decrease in anxiety and motor skills at lower doses to unconsciousness, anterograde amnesia, and central nervous system depression at higher doses. Cell membranes are highly permeable to alcohol, so once alcohol is in the bloodstream it can diffuse into nearly every cell in the body.
The concentration of alcohol in blood is measured via blood alcohol content (BAC). The amount and circumstances of consumption play a large part in determining the extent of intoxication; for example, eating a heavy meal before alcohol consumption causes alcohol to absorb more slowly. Hydration also plays a role, especially in determining the extent of hangovers.
After excessive drinking, unconsciousness can occur and extreme levels of consumption can lead to alcohol poisoning and death (a concentration in the blood stream of 0.40% will kill half of those affected). Alcohol may also cause death indirectly, by asphyxiation from vomit.
Alcohol can greatly exacerbate sleep problems. During abstinence, residual disruptions in sleep regularity and sleep patterns are the greatest predictors of relapse.
Long Term Effects:
Main article: Long-term effects of alcohol
According to the World Health Organization's 2018 Global Status Report on Alcohol and Health, there are more than 3 million people who die from the harmful effects of alcohol each year, which amounts to more than 5% of the burden of disease world-wide.
The US National Institutes of Health similarly estimates that 3.3 million deaths (5.9% of all deaths) were believed to be due to alcohol each year.
Guidelines in the US and the UK advise that if people choose to drink, they should drink moderately.
Even light and moderate alcohol consumption increases cancer risk in individuals, especially with respect to squamous cell carcinoma of the esophagus, oropharyngeal cancer, and breast cancer.
A systematic analysis of data from the Global Burden of Disease Study, which was an observational study, found that long term consumption of any amount of alcohol is associated with an increased of risk of death in all people, and that even moderate consumption appears to be risky.
Similar to prior analyses, it found an apparent benefit for older women in reducing the risks of death from ischemic heart disease and from diabetes, but unlike prior studies it found those risks cancelled by an apparent increased risk of death from breast cancer and other causes.
A 2016 systematic review and meta-analysis found that moderate ethanol consumption brought no mortality benefit compared with lifetime abstention from ethanol consumption. Risk is greater in younger people due to binge drinking which may result in violence or accidents.
Long-term heavy use of alcohol damages nearly every organ and system in the body. Risks include alcoholism, malnutrition, chronic pancreatitis, alcoholic liver disease and cancer. In addition, damage to the central nervous system and peripheral nervous system can occur from chronic alcohol abuse.
The developing adolescent brain is particularly vulnerable to the toxic effects of alcohol.
Click on any of the following blue hyperlinks for more about the effects of drinking alcohol on health:
Alcoholics Anonymous (AA) is an international mutual aid fellowship with the stated purpose of enabling its members to "stay sober and help other alcoholics achieve sobriety."
AA is nonprofessional, self-supporting, and apolitical. Its only membership requirement is a desire to stop drinking. The AA program of recovery is set forth in the Twelve Steps.
AA was founded in Akron, Ohio when in 1935 one alcoholic, Bill Wilson, talked to another alcoholic, Bob Smith, about the nature of alcoholism and a possible solution. With the help of other early members, the book Alcoholics Anonymous: The Story of How More Than One Hundred Men Have Recovered From Alcoholism was written in 1939. Its title became the name of the organization and is now usually referred to as "The Big Book".
AA's initial Twelve Traditions were introduced in 1946 to help the fellowship be stable and unified while disengaged from "outside issues" and influences.
The Traditions recommend that members remain anonymous in public media, altruistically help other alcoholics, and that AA groups avoid official affiliations with other organizations. They also advise against dogma and coercive hierarchies. Subsequent fellowships such as Narcotics Anonymous have adapted the Twelve Steps and the Twelve Traditions to their respective primary purposes.
AA membership has since spread internationally "across diverse cultures holding different beliefs and values", including geopolitical areas resistant to grassroots movements. Close to two million people worldwide are estimated to be members of AA as of 2016.
Click on any of the following blue hyperlinks for more about Alcoholics Anonymous (AA):
Short-term effects of alcohol consumption include intoxication and dehydration.
Long-term effects of alcohol consumption include changes in the metabolism of the liver and brain and alcoholism.
Alcohol intoxication affects the brain, causing slurred speech, clumsiness, and delayed reflexes. Alcohol stimulates insulin production, which speeds up glucose metabolism and can result in low blood sugar, causing irritability and possibly death for diabetics.
Even light and moderate alcohol consumption increases cancer risk in individuals. A 2014 World Health Organization report found that harmful alcohol consumption caused about 3.3 million deaths annually worldwide. Negative efforts are related to the amount consumed with no safe lower limit seen. Some nations have introduced alcohol packaging warning messages that inform consumers about alcohol and cancer, as well as foetal alcohol syndrome.
The median lethal dose of alcohol in test animals is a blood alcohol content of 0.45%. This is about six times the level of ordinary intoxication (0.08%), but vomiting or unconsciousness may occur much sooner in people who have a low tolerance for alcohol. The high tolerance of chronic heavy drinkers may allow some of them to remain conscious at levels above 0.40%, although serious health hazards are incurred at this level.
Alcohol also limits the production of vasopressin (ADH) from the hypothalamus and the secretion of this hormone from the posterior pituitary gland. This is what causes severe dehydration when alcohol is consumed in large amounts. It also causes a high concentration of water in the urine and vomit and the intense thirst that goes along with a hangover.
Stress, hangovers, and the oral contraceptive pill may increase the desire for alcohol because these things will lower the level of testosterone and alcohol will acutely elevate it. Tobacco has the same effect of increasing the craving for alcohol.
Short Term Effects:
Main article: Short-term effects of alcohol
The short-term effects of alcohol consumption range from a decrease in anxiety and motor skills at lower doses to unconsciousness, anterograde amnesia, and central nervous system depression at higher doses. Cell membranes are highly permeable to alcohol, so once alcohol is in the bloodstream it can diffuse into nearly every cell in the body.
The concentration of alcohol in blood is measured via blood alcohol content (BAC). The amount and circumstances of consumption play a large part in determining the extent of intoxication; for example, eating a heavy meal before alcohol consumption causes alcohol to absorb more slowly. Hydration also plays a role, especially in determining the extent of hangovers.
After excessive drinking, unconsciousness can occur and extreme levels of consumption can lead to alcohol poisoning and death (a concentration in the blood stream of 0.40% will kill half of those affected). Alcohol may also cause death indirectly, by asphyxiation from vomit.
Alcohol can greatly exacerbate sleep problems. During abstinence, residual disruptions in sleep regularity and sleep patterns are the greatest predictors of relapse.
Long Term Effects:
Main article: Long-term effects of alcohol
According to the World Health Organization's 2018 Global Status Report on Alcohol and Health, there are more than 3 million people who die from the harmful effects of alcohol each year, which amounts to more than 5% of the burden of disease world-wide.
The US National Institutes of Health similarly estimates that 3.3 million deaths (5.9% of all deaths) were believed to be due to alcohol each year.
Guidelines in the US and the UK advise that if people choose to drink, they should drink moderately.
Even light and moderate alcohol consumption increases cancer risk in individuals, especially with respect to squamous cell carcinoma of the esophagus, oropharyngeal cancer, and breast cancer.
A systematic analysis of data from the Global Burden of Disease Study, which was an observational study, found that long term consumption of any amount of alcohol is associated with an increased of risk of death in all people, and that even moderate consumption appears to be risky.
Similar to prior analyses, it found an apparent benefit for older women in reducing the risks of death from ischemic heart disease and from diabetes, but unlike prior studies it found those risks cancelled by an apparent increased risk of death from breast cancer and other causes.
A 2016 systematic review and meta-analysis found that moderate ethanol consumption brought no mortality benefit compared with lifetime abstention from ethanol consumption. Risk is greater in younger people due to binge drinking which may result in violence or accidents.
Long-term heavy use of alcohol damages nearly every organ and system in the body. Risks include alcoholism, malnutrition, chronic pancreatitis, alcoholic liver disease and cancer. In addition, damage to the central nervous system and peripheral nervous system can occur from chronic alcohol abuse.
The developing adolescent brain is particularly vulnerable to the toxic effects of alcohol.
Click on any of the following blue hyperlinks for more about the effects of drinking alcohol on health:
- Pregnancy
- Cardiovascular disease
- Breastfeeding
- Alcohol education
- Alcohol expectations
- Alcohol abuse
- Injury and deaths
- Genetic differences
- Gender differences
- See also:
Alcoholics Anonymous (AA) is an international mutual aid fellowship with the stated purpose of enabling its members to "stay sober and help other alcoholics achieve sobriety."
AA is nonprofessional, self-supporting, and apolitical. Its only membership requirement is a desire to stop drinking. The AA program of recovery is set forth in the Twelve Steps.
AA was founded in Akron, Ohio when in 1935 one alcoholic, Bill Wilson, talked to another alcoholic, Bob Smith, about the nature of alcoholism and a possible solution. With the help of other early members, the book Alcoholics Anonymous: The Story of How More Than One Hundred Men Have Recovered From Alcoholism was written in 1939. Its title became the name of the organization and is now usually referred to as "The Big Book".
AA's initial Twelve Traditions were introduced in 1946 to help the fellowship be stable and unified while disengaged from "outside issues" and influences.
The Traditions recommend that members remain anonymous in public media, altruistically help other alcoholics, and that AA groups avoid official affiliations with other organizations. They also advise against dogma and coercive hierarchies. Subsequent fellowships such as Narcotics Anonymous have adapted the Twelve Steps and the Twelve Traditions to their respective primary purposes.
AA membership has since spread internationally "across diverse cultures holding different beliefs and values", including geopolitical areas resistant to grassroots movements. Close to two million people worldwide are estimated to be members of AA as of 2016.
Click on any of the following blue hyperlinks for more about Alcoholics Anonymous (AA):
- History
- The Big Book, the Twelve Steps and the Twelve Traditions
- Organization and finances
- Program
- Spirituality
- Disease concept of alcoholism
- Canadian and United States demographics
- Effectiveness
- Relationship with institutions
- Criticism
- Literature
- AA in film
- AA in television
- See also:
- AA official website
- A History of Agnostic Groups in AA
- Addiction recovery groups
- Al-Anon/Alateen
- Calix Society
- Community reinforcement approach and family training (CRAFT)
- Drug rehabilitation
- Group psychotherapy
- Intervention counseling
- List of twelve-step groups
- Recovery model
- Self-help groups for mental health
- Stepping Stones (home)
- Substance abuse
- Washingtonian movement
Tobacco Smoking including Health Effects of Tobacco, e.g., Chronic Obstructive Pulmonary Disease (COPD) and Tobacco Politics
- YouTube Video: CDC: Tips From Former Smokers - Becky: It Goes With Me
- YouTube Video: How to Quit Smoking
- YouTube Video: Mayo Clinic Minute: Are e-cigarettes safe?
Tobacco smoking is the practice of smoking tobacco and inhaling tobacco smoke (consisting of particle and gaseous phases). A broader definition may include simply taking tobacco smoke into the mouth, and then releasing it, as is done by some with tobacco pipes and cigars.
The practice is believed to have begun as early as 5000–3000 BC in Mesoamerica and South America. Tobacco was introduced to Eurasia in the late 17th century by European colonists, where it followed common trade routes.
The practice encountered criticism from its first import into the Western world onwards but embedded itself in certain strata of a number of societies before becoming widespread upon the introduction of automated cigarette-rolling apparatus.
German scientists identified a link between smoking and lung cancer in the late 1920s, leading to the first anti-smoking campaign in modern history, albeit one truncated by the collapse of Nazi Germany at the end of World War II.
In 1950, British researchers demonstrated a clear relationship between smoking and cancer. Evidence continued to mount in the 1980s, which prompted political action against the practice.
Rates of consumption since 1965 in the developed world have either peaked or declined. However, they continue to climb in the developing world.
Smoking is the most common method of consuming tobacco, and tobacco is the most common substance smoked. The agricultural product is often mixed with additives and then combusted. The resulting smoke is then inhaled and the active substances absorbed through the alveoli in the lungs or the oral mucosa.
Combustion was traditionally enhanced by addition of potassium or nitrates. Many substances in cigarette smoke trigger chemical reactions in nerve endings, which heighten heart rate, alertness and reaction time, among other things.
Dopamine and endorphins are released, which are often associated with pleasure. As of 2008 to 2010, tobacco is used by about 49% of men and 11% of women aged 15 or older in fourteen low-income and middle-income countries (Bangladesh, Brazil, China, Egypt, India, Mexico, Philippines, Poland, Russia, Thailand, Turkey, Ukraine, Uruguay and Vietnam), with about 80% of this usage in the form of smoking. The gender gap tends to be less pronounced in lower age groups.
Many smokers begin during adolescence or early adulthood. During the early stages, a combination of perceived pleasure acting as positive reinforcement and desire to respond to social peer pressure may offset the unpleasant symptoms of initial use, which typically include nausea and coughing. After an individual has smoked for some years, the avoidance of withdrawal symptoms and negative reinforcement become the key motivations to continue.
A study of first smoking experiences of seventh-grade students found out that the most common factor leading students to smoke is cigarette advertisements. Smoking by parents, siblings and friends also encourages students to smoke.
Click on any of the following blue hyperlinks for more about Tobacco Smoking:
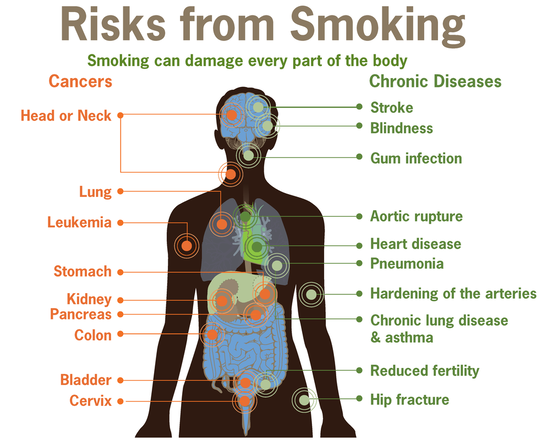
Health Effects of Tobacco
Tobacco use has predominantly negative effects on human health and concern about health effects of tobacco has a long history. Research has focused primarily on cigarette tobacco smoking (above).
Tobacco smoke contains more than 70 chemicals that cause cancer. Tobacco also contains nicotine, which is a highly addictive psychoactive drug. When tobacco is smoked, nicotine causes physical and psychological dependency. Cigarettes sold in underdeveloped countries tend to have higher tar content, and are less likely to be filtered, potentially increasing vulnerability to tobacco smoking related disease in these regions.
Tobacco use is the single greatest cause of preventable death globally. As many as half of people who use tobacco die from complications of tobacco use. The World Health Organization (WHO) estimates that each year tobacco causes about 6 million deaths (about 10% of all deaths) with 600,000 of these occurring in non smokers due to second hand smoke.
In the 20th century tobacco is estimated to have caused 100 million deaths. Similarly, the United States Centers for Disease Control and Prevention describes tobacco use as "the single most important preventable risk to human health in developed countries and an important cause of premature death worldwide."
Currently, the number of premature deaths in the U.S. from tobacco use per year outnumber the number of workers employed in the tobacco industry 4 to 1. According to a 2014 review in the New England Journal of Medicine, tobacco will, if current smoking patterns persist, kill about 1 billion people in the 21st century, half of them before the age of 70.
Tobacco use leads most commonly to diseases affecting the heart, liver and lungs. Smoking is a major risk factor for the following:
Tobacco also causes peripheral arterial disease and high blood pressure. The effects depend on the number of years that a person smokes and on how much the person smokes.
Starting smoking earlier in life and smoking cigarettes higher in tar increases the risk of these diseases. Also, environmental tobacco smoke, or secondhand smoke, has been shown to cause adverse health effects in people of all ages.
Tobacco use is a significant factor in miscarriages among pregnant smokers, and it contributes to a number of other health problems of the fetus such as premature birth, low birth weight, and increases by 1.4 to 3 times the chance of sudden infant death syndrome (SIDS). Incidence of erectile dysfunction is approximately 85 percent higher in male smokers compared to non-smokers.
Several countries have taken measures to control the consumption of tobacco with usage and sales restrictions as well as warning messages printed on packaging. Additionally, smoke-free laws that ban smoking in public places such as workplaces, theaters, and bars and restaurants reduce exposure to secondhand smoke and help some people who smoke to quit, without negative economic effects on restaurants or bars. Tobacco taxes that increase the price are also effective, especially in developing countries.
The idea that tobacco use caused some diseases, including mouth cancers, was initially, in the late 1700s and the 1800s, widely accepted by the medical community. In the 1880s, automation slashed the cost of cigarettes, and use expanded. From the 1890s onwards, associations of tobacco use with cancers and vascular disease were regularly reported; a meta-analysis citing 167 other works was published in 1930, and concluded that tobacco use caused cancer.
Increasingly solid observational evidence was published throughout the 1930s, and in 1938, Science published a paper showing that tobacco users live substantially shorter lives. Case-control studies were published in Germany in 1939 and 1943, and one in the Netherlands in 1948, but widespread attention was first drawn by five case-control studies published in 1950 by researchers from the US and UK.
These studies were widely criticized as showing correlation, not causality. Follow up prospective cohort studies in the early 1950s clearly found that that smokers died faster, and were more likely to die of lung cancer and cardiovascular disease. These results were first widely accepted in the medical community, and publicized among the general public, in the mid-1960s.
Click on any of the following blue hyperlinks for more about the Health Effects of Tobacco Smoking: ___________________________________________________________________________
Chronic Obstructive Pulmonary Disease (COPD):
Chronic obstructive pulmonary disease (COPD) is a type of obstructive lung disease characterized by long-term breathing problems and poor airflow. The main symptoms include shortness of breath and cough with sputum production. COPD is a progressive disease, meaning it typically worsens over time. Eventually, everyday activities such as walking or getting dressed become difficult.
Chronic bronchitis and emphysema are older terms used for different types of COPD. The term "chronic bronchitis" is still used to define a productive cough that is present for at least three months each year for two years. Those with such a cough are at a greater risk of developing COPD. The term "emphysema" is also used for the abnormal presence of air or other gas within tissues.
Tobacco smoking (above) is the most common cause of COPD, with factors such as air pollution and genetics playing a smaller role. In the developing world, one of the common sources of air pollution is poorly vented heating and cooking fires. Long-term exposure to these irritants causes an inflammatory response in the lungs, resulting in narrowing of the small airways and breakdown of lung tissue. The diagnosis is based on poor airflow as measured by lung function tests. In contrast to asthma, the airflow reduction does not improve much with the use of a bronchodilator.
Most cases of COPD can be prevented by reducing exposure to risk factors. This includes decreasing rates of smoking and improving indoor and outdoor air quality. While treatment can slow worsening, no cure is known.
COPD treatments include smoking cessation, vaccinations, respiratory rehabilitation, and often inhaled bronchodilators and steroids. Some people may benefit from long-term oxygen therapy or lung transplantation. In those who have periods of acute worsening, increased use of medications and hospitalization may be needed.
As of 2015, COPD affected about 174.5 million people (2.4% of the global population). It typically occurs in people over the age of 40. Males and females are affected equally commonly. In 2015, it resulted in 3.2 million deaths, up from 2.4 million deaths in 1990.
More than 90% of these deaths occur in the developing world. The number of deaths is projected to increase further because of higher smoking rates in the developing world, and an aging population in many countries. It resulted in an estimated economic cost of $2.1 trillion in 2010.
Click on any of the following blue hyperlinks to learn more about COPD:
Tobacco Politics:
Tobacco politics refers to the politics surrounding the use and distribution of tobacco.
In the United States, from the 1950s until the 1990s, tobacco industries wielded great influence in shaping public opinion on the health risks of tobacco. Despite the efforts of public health advocates, scientists, and those affected by smoking, both Congress and courts favored the tobacco industry in policy and litigation.
It was not until the 1990s when public health advocates had more success in litigating against tobacco industries, including the 1998 Master Settlement Agreement between major tobacco companies and 46 state attorneys general. Although public opinion in the United States on cigarette smoking is more unfavorable, many large tobacco companies continue to find success internationally.
As of 2018, 169 states have signed the World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC), which governs international tobacco control. However, many nations have had difficulty complying with the FCTC, with higher rates of smoking especially in developing nations. There are currently close to one billion smokers worldwide.
Click on any of the following blue hyperlinks for more about Tobacco Politics:
The practice is believed to have begun as early as 5000–3000 BC in Mesoamerica and South America. Tobacco was introduced to Eurasia in the late 17th century by European colonists, where it followed common trade routes.
The practice encountered criticism from its first import into the Western world onwards but embedded itself in certain strata of a number of societies before becoming widespread upon the introduction of automated cigarette-rolling apparatus.
German scientists identified a link between smoking and lung cancer in the late 1920s, leading to the first anti-smoking campaign in modern history, albeit one truncated by the collapse of Nazi Germany at the end of World War II.
In 1950, British researchers demonstrated a clear relationship between smoking and cancer. Evidence continued to mount in the 1980s, which prompted political action against the practice.
Rates of consumption since 1965 in the developed world have either peaked or declined. However, they continue to climb in the developing world.
Smoking is the most common method of consuming tobacco, and tobacco is the most common substance smoked. The agricultural product is often mixed with additives and then combusted. The resulting smoke is then inhaled and the active substances absorbed through the alveoli in the lungs or the oral mucosa.
Combustion was traditionally enhanced by addition of potassium or nitrates. Many substances in cigarette smoke trigger chemical reactions in nerve endings, which heighten heart rate, alertness and reaction time, among other things.
Dopamine and endorphins are released, which are often associated with pleasure. As of 2008 to 2010, tobacco is used by about 49% of men and 11% of women aged 15 or older in fourteen low-income and middle-income countries (Bangladesh, Brazil, China, Egypt, India, Mexico, Philippines, Poland, Russia, Thailand, Turkey, Ukraine, Uruguay and Vietnam), with about 80% of this usage in the form of smoking. The gender gap tends to be less pronounced in lower age groups.
Many smokers begin during adolescence or early adulthood. During the early stages, a combination of perceived pleasure acting as positive reinforcement and desire to respond to social peer pressure may offset the unpleasant symptoms of initial use, which typically include nausea and coughing. After an individual has smoked for some years, the avoidance of withdrawal symptoms and negative reinforcement become the key motivations to continue.
A study of first smoking experiences of seventh-grade students found out that the most common factor leading students to smoke is cigarette advertisements. Smoking by parents, siblings and friends also encourages students to smoke.
Click on any of the following blue hyperlinks for more about Tobacco Smoking:
- History
- Consumption
- Psychology
- Economic
- Health
- Social
- Incomes
- Public policy
- Gateway drug theory
- Cessation
- See also:
- Cannabis smoking
- Cigarette smoking among college students
- Cigarette smoking for weight loss
- Electronic cigarette
- Herbal cigarette
- List of cigarette smoke carcinogens
- Tobacco advertising
- Tobacco control
- Snuff (tobacco)
- Tobacco History Links – repository from Tobacco.org
- Surgeon General: Tobacco Cessation
- CDC: Smoking & Tobacco Use
- WHO: Tobacco Free Initiative
- The Tobacco Atlas
- Tobacco Viz
- Cigarette smoking prevalence in US counties: 1996–2012
Health Effects of Tobacco
Tobacco use has predominantly negative effects on human health and concern about health effects of tobacco has a long history. Research has focused primarily on cigarette tobacco smoking (above).
Tobacco smoke contains more than 70 chemicals that cause cancer. Tobacco also contains nicotine, which is a highly addictive psychoactive drug. When tobacco is smoked, nicotine causes physical and psychological dependency. Cigarettes sold in underdeveloped countries tend to have higher tar content, and are less likely to be filtered, potentially increasing vulnerability to tobacco smoking related disease in these regions.
Tobacco use is the single greatest cause of preventable death globally. As many as half of people who use tobacco die from complications of tobacco use. The World Health Organization (WHO) estimates that each year tobacco causes about 6 million deaths (about 10% of all deaths) with 600,000 of these occurring in non smokers due to second hand smoke.
In the 20th century tobacco is estimated to have caused 100 million deaths. Similarly, the United States Centers for Disease Control and Prevention describes tobacco use as "the single most important preventable risk to human health in developed countries and an important cause of premature death worldwide."
Currently, the number of premature deaths in the U.S. from tobacco use per year outnumber the number of workers employed in the tobacco industry 4 to 1. According to a 2014 review in the New England Journal of Medicine, tobacco will, if current smoking patterns persist, kill about 1 billion people in the 21st century, half of them before the age of 70.
Tobacco use leads most commonly to diseases affecting the heart, liver and lungs. Smoking is a major risk factor for the following:
- heart attacks,
- strokes,
- chronic obstructive pulmonary disease (COPD) (including emphysema and chronic bronchitis),
- and several cancers, particularly the following:
Tobacco also causes peripheral arterial disease and high blood pressure. The effects depend on the number of years that a person smokes and on how much the person smokes.
Starting smoking earlier in life and smoking cigarettes higher in tar increases the risk of these diseases. Also, environmental tobacco smoke, or secondhand smoke, has been shown to cause adverse health effects in people of all ages.
Tobacco use is a significant factor in miscarriages among pregnant smokers, and it contributes to a number of other health problems of the fetus such as premature birth, low birth weight, and increases by 1.4 to 3 times the chance of sudden infant death syndrome (SIDS). Incidence of erectile dysfunction is approximately 85 percent higher in male smokers compared to non-smokers.
Several countries have taken measures to control the consumption of tobacco with usage and sales restrictions as well as warning messages printed on packaging. Additionally, smoke-free laws that ban smoking in public places such as workplaces, theaters, and bars and restaurants reduce exposure to secondhand smoke and help some people who smoke to quit, without negative economic effects on restaurants or bars. Tobacco taxes that increase the price are also effective, especially in developing countries.
The idea that tobacco use caused some diseases, including mouth cancers, was initially, in the late 1700s and the 1800s, widely accepted by the medical community. In the 1880s, automation slashed the cost of cigarettes, and use expanded. From the 1890s onwards, associations of tobacco use with cancers and vascular disease were regularly reported; a meta-analysis citing 167 other works was published in 1930, and concluded that tobacco use caused cancer.
Increasingly solid observational evidence was published throughout the 1930s, and in 1938, Science published a paper showing that tobacco users live substantially shorter lives. Case-control studies were published in Germany in 1939 and 1943, and one in the Netherlands in 1948, but widespread attention was first drawn by five case-control studies published in 1950 by researchers from the US and UK.
These studies were widely criticized as showing correlation, not causality. Follow up prospective cohort studies in the early 1950s clearly found that that smokers died faster, and were more likely to die of lung cancer and cardiovascular disease. These results were first widely accepted in the medical community, and publicized among the general public, in the mid-1960s.
Click on any of the following blue hyperlinks for more about the Health Effects of Tobacco Smoking: ___________________________________________________________________________
Chronic Obstructive Pulmonary Disease (COPD):
Chronic obstructive pulmonary disease (COPD) is a type of obstructive lung disease characterized by long-term breathing problems and poor airflow. The main symptoms include shortness of breath and cough with sputum production. COPD is a progressive disease, meaning it typically worsens over time. Eventually, everyday activities such as walking or getting dressed become difficult.
Chronic bronchitis and emphysema are older terms used for different types of COPD. The term "chronic bronchitis" is still used to define a productive cough that is present for at least three months each year for two years. Those with such a cough are at a greater risk of developing COPD. The term "emphysema" is also used for the abnormal presence of air or other gas within tissues.
Tobacco smoking (above) is the most common cause of COPD, with factors such as air pollution and genetics playing a smaller role. In the developing world, one of the common sources of air pollution is poorly vented heating and cooking fires. Long-term exposure to these irritants causes an inflammatory response in the lungs, resulting in narrowing of the small airways and breakdown of lung tissue. The diagnosis is based on poor airflow as measured by lung function tests. In contrast to asthma, the airflow reduction does not improve much with the use of a bronchodilator.
Most cases of COPD can be prevented by reducing exposure to risk factors. This includes decreasing rates of smoking and improving indoor and outdoor air quality. While treatment can slow worsening, no cure is known.
COPD treatments include smoking cessation, vaccinations, respiratory rehabilitation, and often inhaled bronchodilators and steroids. Some people may benefit from long-term oxygen therapy or lung transplantation. In those who have periods of acute worsening, increased use of medications and hospitalization may be needed.
As of 2015, COPD affected about 174.5 million people (2.4% of the global population). It typically occurs in people over the age of 40. Males and females are affected equally commonly. In 2015, it resulted in 3.2 million deaths, up from 2.4 million deaths in 1990.
More than 90% of these deaths occur in the developing world. The number of deaths is projected to increase further because of higher smoking rates in the developing world, and an aging population in many countries. It resulted in an estimated economic cost of $2.1 trillion in 2010.
Click on any of the following blue hyperlinks to learn more about COPD:
- Signs and symptoms
- Cause
- Pathophysiology
- Diagnosis
- Prevention
- Management
- Prognosis
- Epidemiology
- History
- Society and culture
- Research
- Other animals
- See also:
Tobacco Politics:
Tobacco politics refers to the politics surrounding the use and distribution of tobacco.
In the United States, from the 1950s until the 1990s, tobacco industries wielded great influence in shaping public opinion on the health risks of tobacco. Despite the efforts of public health advocates, scientists, and those affected by smoking, both Congress and courts favored the tobacco industry in policy and litigation.
It was not until the 1990s when public health advocates had more success in litigating against tobacco industries, including the 1998 Master Settlement Agreement between major tobacco companies and 46 state attorneys general. Although public opinion in the United States on cigarette smoking is more unfavorable, many large tobacco companies continue to find success internationally.
As of 2018, 169 states have signed the World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC), which governs international tobacco control. However, many nations have had difficulty complying with the FCTC, with higher rates of smoking especially in developing nations. There are currently close to one billion smokers worldwide.
Click on any of the following blue hyperlinks for more about Tobacco Politics:
- Taxation
- Lobby
- Litigation
- Tobacco politics and litigation outside of the United States
- See also:
- No-Smoking.org
- Smoking Lobby Group
- Tobacco Institute Documents-Part of Master Settlement Agreement
- UCSF Tobacco Industry Videos Collection
- UCSF Tobacco Industry Audio Recordings Collection
- State and Local Tax Revenue, Selected Years 1977-2006
- A Frank Statement
- Operation Berkshire
- Tobacco Master Settlement Agreement
- Tobacco MSA (Alabama)
- Tobacco MSA (Hawaii)
- Tobacco MSA (New York)
- Merchants of Doubt and 2014 film Merchants of Doubt based on the 2010 book
Exercise including Equipment, and a List of Equipment Manufacturers
- YouTube Video: How to Get the Most Out of Elliptical Gym Workout
- YouTube Video of Beginner's Guide to Recumbent Bike Cardio by Silver Sneakers
- YouTube Video: I Did Peloton For Two Weeks Straight And Here’s What Happened
Exercise is any bodily activity that enhances or maintains physical fitness and overall health and wellness. It is performed for various reasons, to aid growth and improve strength, preventing aging, developing muscles and the cardiovascular system, honing athletic skills, weight loss or maintenance, improving health and also for enjoyment. Many individuals choose to exercise outdoors where they can congregate in groups, socialize, and enhance well-being.
Physical exercises are generally grouped into three types, depending on the overall effect they have on the human body:
Physical exercise can also include training that focuses on accuracy, agility, power, and speed.
Sometimes the terms 'dynamic' and 'static' are used. 'Dynamic' exercises such as steady running, tend to produce a lowering of the diastolic blood pressure during exercise, due to the improved blood flow. Conversely, static exercise (such as weight-lifting) can cause the systolic pressure to rise significantly, albeit transiently, during the performance of the exercise.
Click on any of the following blue hyperlinks for more about Exercise:
Exercise equipment is any apparatus or device used during physical activity to enhance the strength or conditioning effects of that exercise by providing either fixed or adjustable amounts of resistance, or to otherwise enhance the experience or outcome of an exercise routine.
Exercise equipment may also include such wearable items as proper footgear, gloves, and hydration packs.
General strength training equipment:
A broad range of different types of exercise equipment are available, including
Exercise equipment companies:
C: E: F: I: J: K: L: M: N: P: R: T:
Physical exercises are generally grouped into three types, depending on the overall effect they have on the human body:
- Aerobic exercise is any physical activity that uses large muscle groups and causes the body to use more oxygen than it would while resting. The goal of aerobic exercise is to increase cardiovascular endurance. Examples of aerobic exercise include:
- running,
- cycling,
- swimming,
- brisk walking,
- skipping rope,
- rowing,
- hiking,
- dancing,
- playing tennis,
- continuous training,
- and long distance running.
- Anaerobic exercise, which includes strength and resistance training, can firm, strengthen, and increase muscle mass, as well as improve bone density, balance, and coordination. Examples of strength exercises are:
- push-ups,
- pull-ups,
- lunges,
- squats,
- bench press,
- weight training,
- functional training,
- eccentric training,
- interval training,
- sprinting,
- and high-intensity interval training that increases short-term muscle strength.
- Flexibility exercises stretch and lengthen muscles. Activities such as stretching help to improve joint flexibility and keep muscles limber. The goal is to improve the range of motion which can reduce the chance of injury.
Physical exercise can also include training that focuses on accuracy, agility, power, and speed.
Sometimes the terms 'dynamic' and 'static' are used. 'Dynamic' exercises such as steady running, tend to produce a lowering of the diastolic blood pressure during exercise, due to the improved blood flow. Conversely, static exercise (such as weight-lifting) can cause the systolic pressure to rise significantly, albeit transiently, during the performance of the exercise.
Click on any of the following blue hyperlinks for more about Exercise:
- Health effects
- Mechanism of effects
- Public health measures
- Exercise trends
- Nutrition and recovery
- History
- Other animals
- See also:
- Main article: Outline of exercise
- Active living
- Behavioural change theories
- Bodybuilding
- Exercise hypertension
- Exercise-induced nausea
- Exercise intensity
- Exercise intolerance
- Exercise-induced anaphylaxis
- Exercise-induced asthma
- Kinesiology
- Metabolic equivalent
- Non-exercise associated thermogenesis
- Supercompensation
- Warming up
- Adult Compendium of Physical Activities – a website containing lists of Metabolic Equivalent of Task (MET) values for a number of physical activities, based upon PMID 8292105, 10993420 and 21681120
- Physical activity and the environment – guidance on the promotion and creation of physical environments that support increased levels of physical activity.
- MedLinePlus Topic on Exercise and Physical Fitness
- Science Daily's reference on physical exercise
Exercise equipment is any apparatus or device used during physical activity to enhance the strength or conditioning effects of that exercise by providing either fixed or adjustable amounts of resistance, or to otherwise enhance the experience or outcome of an exercise routine.
Exercise equipment may also include such wearable items as proper footgear, gloves, and hydration packs.
General strength training equipment:
A broad range of different types of exercise equipment are available, including
- Free-weight training:
- Preloaded dumbbells and conventional dumbbells
- Kettlebells
- Preloaded barbells and conventional barbells
- Weight plates: bumper plates, steel plates, micro-plates
- Collars
- Weight machines
- Cables
- Rowers
- Head/neck harness
- Variable resistance training:
- Elastic bands (resistance bands): monster bands, hip circles, floss bands, mini bands
- Chain accommodation training: chains
- Lifting accessories:
- Straps, wraps and sleeves:
- Lifting wrist straps
- Wrist wraps
- Elbow sleeves
- Knee wraps
- Knee sleeves
- Hand care: Gym chalk, gloves
- Sling shots
- Shoes (specifically made for Olympic weightlifting, squats, deadlifts, overhead press, etc.)
- Belts (10 mm, 13 mm; small, medium, large; prong belts, lever belts)
- Straps, wraps and sleeves:
- kBox
- Yokes
- Training sleds: sleds, push sleds, pull sleds
- Logs
- Axles
- Farmer's walk handles
- Stones: Atlas stones, stones of steel
- Kegs
- General grip strength: Captains of Crush Grippers, wrist rollers, Fat Gripz, pinch blocks, pull-up spheres
- Power pins, loading pins
- Hammers, slammers, maces, clubs
- Sandbags
- Bulgarian bags
- Parallel bars (P-bars): high P-bars, low P-bars
- Pulling-related:
- Pull-up/dip belts
- Peg boards
- Pull-up bars:
- Doorway (use leverage around door frame)
- Extending door frame (extends out to fit between door frame)
- Wall-mounted
- Ceiling-mounted
- Free standing bar
- Suspension training/trainer:
- TRX Suspension Trainer
- Jungle Gym XT
- Flying
- AirFit Trainer Pro
- Gymnastic rings
- Weighted vests
- Limb weights: ankle weights, wrist weights
- Paralletes or push-up handles
- Medicine balls
- Swiss balls
- Ropes: jump ropes, climbing ropes, conditioning ropes
- Training Sleds
- Rolling: foam roller, RumbleRoller, GRID STK foam roller
- Balls: Lacrosse ball, spiky, dimple, rad roller or peanuts
- Elliptical trainer
StreetStrider, an elliptical trainer on wheels - Stepper, also known as mini stepper or stair stepper
- Stair machine, also known as stair stepper
- Training masks
- Treadmill
- Wall bars
- Exercise machine
- Fitness (biology)
- Hojo undō, conditioning exercises used in martial arts
- Physical exercise
- Weight training
Exercise equipment companies:
C: E: F: I: J: K: L: M: N: P: R: T:
Performance-enhancing drugs: Know the risks:
By Mayo Clinic Staff
Hoping to gain a competitive edge by taking performance-enhancing drugs? Learn how these drugs work and how they can affect your health.
Most serious athletes will tell you that the drive to win is fierce. Besides the satisfaction of personal accomplishment, athletes often pursue dreams of winning a medal for their country or securing a spot on a professional team. In such an environment, the use of performance-enhancing drugs has become increasingly common.
But using performance-enhancing drugs (doping) has risks. Take the time to learn about the potential benefits, the health risks and the many unknowns regarding so-called performance-enhancing drugs such as anabolic steroids, androstenedione, human growth hormone, erythropoietin, diuretics, creatine and stimulants. You may decide that the benefits aren't worth the risks.
Anabolic steroids: What are they?
Some athletes take a form of steroids — known as anabolic-androgenic steroids or just anabolic steroids — to increase their muscle mass and strength. The main anabolic steroid hormone produced by your body is testosterone.
Testosterone has two main effects on your body:
Some athletes take straight testosterone to boost their performance. The anabolic steroids used by athletes are often synthetic modifications of testosterone.
These hormones have approved medical uses. But improving athletic performance isn't one of them.
Why are these drugs so appealing to athletes? Besides making muscles bigger, anabolic steroids may reduce the muscle damage that occurs during a hard workout, helping athletes recover from the session more quickly and enabling them to work out harder and more frequently. Some athletes, as well as non-athletes, may like the muscular appearance they get when they take the drugs.
Designer steroids:
A particularly dangerous class of anabolic steroids are the so-called designer drugs — synthetic steroids that have been illicitly created to be undetectable by current drug tests.
They are made specifically for athletes and have no approved medical use. Because of this, they haven't been tested or approved by the Food and Drug Administration (FDA) and represent a particular health threat to athletes.
Risks:
Many athletes take anabolic steroids at doses that are much higher than those prescribed for medical reasons. Anabolic steroids have serious physical side effects.
Men may develop:
Women may develop:
Both men and women might experience:
Taking anabolic-androgenic steroids to enhance athletic performance is prohibited by most sports organizations — and it's illegal. In the past 20 years, more-effective law enforcement in the United States has pushed much of the illegal steroid industry into the black market.
This poses additional health risks because the drugs are either made in other countries and smuggled in or made in clandestine labs in the United States. Either way, they aren't subject to government safety standards and could be impure or mislabeled.
Androstenedione: What is it?
Androstenedione (andro) is a hormone produced by the adrenal glands, ovaries and testes. It's a hormone that's normally converted to testosterone and a form of estrogen (estradiol) in both men and women.
Andro is available legally only by prescription and is a controlled substance. Its use as a performance-enhancing drug is illegal in the United States.
Manufacturers and bodybuilding magazines tout andro's ability to allow athletes to train harder and recover more quickly. Scientific studies that refute these claims show that supplemental androstenedione doesn't increase testosterone and that your muscles don't get stronger with andro use.
RisksSide effects of andro in men include:
In women, side effects include:
In both men and women, andro can damage the heart and blood vessels, increasing the risk of heart attack and stroke.
Human growth hormone: What is it?
Human growth hormone is a hormone that has an anabolic effect. Athletes take it to improve muscle mass and performance. However, it hasn't been shown conclusively to improve either strength or endurance.
Human growth hormone is available only by prescription and is administered by injection.
RisksAdverse effects related to human growth hormone range in severity and may include:
Erythropoietin: What is it?
Erythropoietin is a type of hormone used to treat anemia in people with severe kidney disease. It increases production of red blood cells and hemoglobin — the protein that carries oxygen to your body's organs.
Taking erythropoietin improves the movement of oxygen to the muscles. Epoetin, a synthetic form of erythropoietin, is commonly used by endurance athletes.
Risks:
Erythropoietin use among competitive cyclists was common in the 1990s and allegedly contributed to at least 18 deaths. Inappropriate use of erythropoietin may increase the risk of stroke, heart attack and blockage in an artery in the lung (pulmonary embolism).
Diuretics: What are they?
Diuretics are drugs that change your body's natural balance of fluids and salts (electrolytes), which can lead to dehydration. This loss of water can decrease an athlete's weight, which many athletes prefer. Diuretics may also help athletes pass drug tests by diluting their urine and are sometimes referred to as a "masking" agent.
Risks:
Diuretics taken at any dose, even medically recommended doses, predispose athletes to adverse effects such as:
Creatine: What is it?
Many athletes take nutritional supplements instead of or in addition to performance-enhancing drugs. Supplements are available over-the-counter as powders or pills. Creatine monohydrate is a supplement that's popular among athletes.
Creatine is a naturally occurring compound produced by your body that helps your muscles release energy. Scientific research indicates that creatine may have some athletic benefit by producing small gains in short-term bursts of power.
Creatine appears to help muscles make more adenosine triphosphate (ATP), which stores and transports energy in cells, and is used for quick bursts of activity, such as weightlifting or sprinting. But there's no evidence that creatine enhances performance in aerobic or endurance sports.
Risks:
Possible side effects of creatine that can decrease athletic performance include:
Weight gain is sought by athletes who want to increase their size. But with prolonged creatine use, weight gain is more likely the result of water retention than an increase in muscle mass. Water is drawn into your muscle tissue, away from other parts of your body, putting you at risk of dehydration.
It appears safe for adults to use creatine at the doses recommended by manufacturers. But there are no studies investigating the long-term benefits and risks of creatine supplementation.
Stimulants: What are they?
Some athletes use stimulants to stimulate the central nervous system and increase heart rate and blood pressure.
Stimulants can:
Common stimulants include caffeine and amphetamines. Cold remedies often contain the stimulants ephedrine or pseudoephedrine hydrochloride.
Energy drinks, which are popular among many athletes, often contain high doses of caffeine and other stimulants. The street drugs cocaine and methamphetamine also are stimulants.
Risks:
Although stimulants can boost physical performance and promote aggressiveness on the field, they have side effects that can impair athletic performance, including:
Other side effects include:
The bottom line
Do performance-enhancing drugs boost performance? Some athletes may appear to achieve physical gains from such drugs, but at what cost?
The long-term effects of performance-enhancing drugs haven't been rigorously studied. And short-term benefits are tempered by many risks. Not to mention that doping is prohibited by most sports organizations.
No matter how you look at it, using performance-enhancing drugs is risky business.
[End of Mayo Clinic Article]
___________________________________________________________________________
Wikipedia: Anabolic Steroids
Anabolic steroids, also known more properly as anabolic–androgenic steroids (AAS), are steroidal androgens that include natural androgens like testosterone as well as synthetic androgens that are structurally related and have similar effects to testosterone.
They are anabolic and increase protein within cells, especially in skeletal muscles, and also have varying degrees of androgenic and virilizing effects, including induction of the development and maintenance of masculine secondary sexual characteristics such as the growth of facial and body hair.
The word anabolic, referring to anabolism, comes from the Greek ἀναβολή anabole, "that which is thrown up, mound". Androgens or AAS are one of three types of sex hormone agonists, the others being estrogens like estradiol and progestogens like progesterone.
AAS were synthesized in the 1930s, and are now used therapeutically in medicine to stimulate muscle growth and appetite, induce male puberty and treat chronic wasting conditions, such as cancer and AIDS.
The American College of Sports Medicine acknowledges that AAS, in the presence of adequate diet, can contribute to increases in body weight, often as lean mass increases and that the gains in muscular strength achieved through high-intensity exercise and proper diet can be additionally increased by the use of AAS in some individuals.
Health risks can be produced by long-term use or excessive doses of AAS. These effects include harmful changes in cholesterol levels (increased low-density lipoprotein and decreased high-density lipoprotein), acne, high blood pressure, liver damage (mainly with most oral AAS), and dangerous changes in the structure of the left ventricle of the heart.
These risks are only increased when, as they often do, athletes take steroids alongside other drugs, causing significantly more damage to their bodies. The effect of anabolic steroids on the heart can cause myocardial infarction and strokes. Conditions pertaining to hormonal imbalances such as gynecomastia and testicular size reduction may also be caused by AAS.
In women and children, AAS can cause irreversible masculinization.
Ergogenic uses for AAS in sports, racing, and bodybuilding as performance-enhancing drugs are controversial because of their adverse effects and the potential to gain unfair advantage in physical competitions. Their use is referred to as doping and banned by most major sporting bodies.
Athletes have been looking for drugs to enhance their athletic abilities since the Olympics started in Ancient Greece. For many years, AAS have been by far the most detected doping substances in IOC-accredited laboratories. In countries where AAS are controlled substances, there is often a black market in which smuggled, clandestinely manufactured or even counterfeit drugs are sold to users.
Click on any of the following blue hyperlinks for more about Anabolic Steroids:
By Mayo Clinic Staff
Hoping to gain a competitive edge by taking performance-enhancing drugs? Learn how these drugs work and how they can affect your health.
Most serious athletes will tell you that the drive to win is fierce. Besides the satisfaction of personal accomplishment, athletes often pursue dreams of winning a medal for their country or securing a spot on a professional team. In such an environment, the use of performance-enhancing drugs has become increasingly common.
But using performance-enhancing drugs (doping) has risks. Take the time to learn about the potential benefits, the health risks and the many unknowns regarding so-called performance-enhancing drugs such as anabolic steroids, androstenedione, human growth hormone, erythropoietin, diuretics, creatine and stimulants. You may decide that the benefits aren't worth the risks.
Anabolic steroids: What are they?
Some athletes take a form of steroids — known as anabolic-androgenic steroids or just anabolic steroids — to increase their muscle mass and strength. The main anabolic steroid hormone produced by your body is testosterone.
Testosterone has two main effects on your body:
- Anabolic effects promote muscle building.
- Androgenic effects are responsible for male traits, such as facial hair and a deeper voice.
Some athletes take straight testosterone to boost their performance. The anabolic steroids used by athletes are often synthetic modifications of testosterone.
These hormones have approved medical uses. But improving athletic performance isn't one of them.
Why are these drugs so appealing to athletes? Besides making muscles bigger, anabolic steroids may reduce the muscle damage that occurs during a hard workout, helping athletes recover from the session more quickly and enabling them to work out harder and more frequently. Some athletes, as well as non-athletes, may like the muscular appearance they get when they take the drugs.
Designer steroids:
A particularly dangerous class of anabolic steroids are the so-called designer drugs — synthetic steroids that have been illicitly created to be undetectable by current drug tests.
They are made specifically for athletes and have no approved medical use. Because of this, they haven't been tested or approved by the Food and Drug Administration (FDA) and represent a particular health threat to athletes.
Risks:
Many athletes take anabolic steroids at doses that are much higher than those prescribed for medical reasons. Anabolic steroids have serious physical side effects.
Men may develop:
- Prominent breasts
- Shrunken testicles
- Infertility
- Prostate gland enlargement
Women may develop:
- A deeper voice, which may be irreversible
- An enlarged clitoris, which may be irreversible
- Increased body hair
- Baldness, which may be irreversible
- Infrequent or absent periods
Both men and women might experience:
- Severe acne
- Increased risk of tendinitis and tendon rupture
- Liver abnormalities and tumors
- Increased low-density lipoprotein (LDL) cholesterol (the "bad" cholesterol)
- Decreased high-density lipoprotein (HDL) cholesterol (the "good" cholesterol
- High blood pressure (hypertension)
- Heart and blood circulation problems
- Aggressive behaviors, rage or violence
- Psychiatric disorders, such as depression
- Drug dependence
- Infections or diseases such as HIV or hepatitis if you're injecting the drugs
- Inhibited growth and development, and risk of future health problems in teenagers
Taking anabolic-androgenic steroids to enhance athletic performance is prohibited by most sports organizations — and it's illegal. In the past 20 years, more-effective law enforcement in the United States has pushed much of the illegal steroid industry into the black market.
This poses additional health risks because the drugs are either made in other countries and smuggled in or made in clandestine labs in the United States. Either way, they aren't subject to government safety standards and could be impure or mislabeled.
Androstenedione: What is it?
Androstenedione (andro) is a hormone produced by the adrenal glands, ovaries and testes. It's a hormone that's normally converted to testosterone and a form of estrogen (estradiol) in both men and women.
Andro is available legally only by prescription and is a controlled substance. Its use as a performance-enhancing drug is illegal in the United States.
Manufacturers and bodybuilding magazines tout andro's ability to allow athletes to train harder and recover more quickly. Scientific studies that refute these claims show that supplemental androstenedione doesn't increase testosterone and that your muscles don't get stronger with andro use.
RisksSide effects of andro in men include:
- Acne
- Diminished sperm production
- Shrinking of the testicles
- Enlargement of the breasts
In women, side effects include:
- Acne
- Masculinization, such as deepening of the voice and male-pattern baldness
In both men and women, andro can damage the heart and blood vessels, increasing the risk of heart attack and stroke.
Human growth hormone: What is it?
Human growth hormone is a hormone that has an anabolic effect. Athletes take it to improve muscle mass and performance. However, it hasn't been shown conclusively to improve either strength or endurance.
Human growth hormone is available only by prescription and is administered by injection.
RisksAdverse effects related to human growth hormone range in severity and may include:
- Joint pain
- Muscle weakness
- Fluid retention
- Diabetes
- Vision problems
- Carpal tunnel syndrome
- Impaired glucose regulation
- Enlarged heart (cardiomegaly)
- High blood pressure (hypertension)
Erythropoietin: What is it?
Erythropoietin is a type of hormone used to treat anemia in people with severe kidney disease. It increases production of red blood cells and hemoglobin — the protein that carries oxygen to your body's organs.
Taking erythropoietin improves the movement of oxygen to the muscles. Epoetin, a synthetic form of erythropoietin, is commonly used by endurance athletes.
Risks:
Erythropoietin use among competitive cyclists was common in the 1990s and allegedly contributed to at least 18 deaths. Inappropriate use of erythropoietin may increase the risk of stroke, heart attack and blockage in an artery in the lung (pulmonary embolism).
Diuretics: What are they?
Diuretics are drugs that change your body's natural balance of fluids and salts (electrolytes), which can lead to dehydration. This loss of water can decrease an athlete's weight, which many athletes prefer. Diuretics may also help athletes pass drug tests by diluting their urine and are sometimes referred to as a "masking" agent.
Risks:
Diuretics taken at any dose, even medically recommended doses, predispose athletes to adverse effects such as:
- Dehydration
- Muscle cramps
- Dizziness
- Potassium deficiency
- Drop in blood pressure
- Loss of coordination and balance
- Death
Creatine: What is it?
Many athletes take nutritional supplements instead of or in addition to performance-enhancing drugs. Supplements are available over-the-counter as powders or pills. Creatine monohydrate is a supplement that's popular among athletes.
Creatine is a naturally occurring compound produced by your body that helps your muscles release energy. Scientific research indicates that creatine may have some athletic benefit by producing small gains in short-term bursts of power.
Creatine appears to help muscles make more adenosine triphosphate (ATP), which stores and transports energy in cells, and is used for quick bursts of activity, such as weightlifting or sprinting. But there's no evidence that creatine enhances performance in aerobic or endurance sports.
Risks:
Possible side effects of creatine that can decrease athletic performance include:
- Stomach cramps
- Muscle cramps
- Weight gain
Weight gain is sought by athletes who want to increase their size. But with prolonged creatine use, weight gain is more likely the result of water retention than an increase in muscle mass. Water is drawn into your muscle tissue, away from other parts of your body, putting you at risk of dehydration.
It appears safe for adults to use creatine at the doses recommended by manufacturers. But there are no studies investigating the long-term benefits and risks of creatine supplementation.
Stimulants: What are they?
Some athletes use stimulants to stimulate the central nervous system and increase heart rate and blood pressure.
Stimulants can:
- Improve endurance
- Reduce fatigue
- Suppress appetite
- Increase alertness and aggressiveness
Common stimulants include caffeine and amphetamines. Cold remedies often contain the stimulants ephedrine or pseudoephedrine hydrochloride.
Energy drinks, which are popular among many athletes, often contain high doses of caffeine and other stimulants. The street drugs cocaine and methamphetamine also are stimulants.
Risks:
Although stimulants can boost physical performance and promote aggressiveness on the field, they have side effects that can impair athletic performance, including:
- Nervousness and irritability, which make it hard to concentrate on the game
- Insomnia, which can prevent an athlete from getting needed sleep
- Dehydration
- Heatstroke
- Addiction or tolerance, meaning that athletes need greater amounts to achieve the desired effect, so they'll take doses that are much higher than the intended medical dose
Other side effects include:
- Heart palpitations
- Heart rhythm abnormalities
- Weight loss
- Tremors
- Mild high blood pressure (hypertension)
- Hallucinations
- Stroke
- Heart attack and other circulatory problems
The bottom line
Do performance-enhancing drugs boost performance? Some athletes may appear to achieve physical gains from such drugs, but at what cost?
The long-term effects of performance-enhancing drugs haven't been rigorously studied. And short-term benefits are tempered by many risks. Not to mention that doping is prohibited by most sports organizations.
No matter how you look at it, using performance-enhancing drugs is risky business.
[End of Mayo Clinic Article]
___________________________________________________________________________
Wikipedia: Anabolic Steroids
Anabolic steroids, also known more properly as anabolic–androgenic steroids (AAS), are steroidal androgens that include natural androgens like testosterone as well as synthetic androgens that are structurally related and have similar effects to testosterone.
They are anabolic and increase protein within cells, especially in skeletal muscles, and also have varying degrees of androgenic and virilizing effects, including induction of the development and maintenance of masculine secondary sexual characteristics such as the growth of facial and body hair.
The word anabolic, referring to anabolism, comes from the Greek ἀναβολή anabole, "that which is thrown up, mound". Androgens or AAS are one of three types of sex hormone agonists, the others being estrogens like estradiol and progestogens like progesterone.
AAS were synthesized in the 1930s, and are now used therapeutically in medicine to stimulate muscle growth and appetite, induce male puberty and treat chronic wasting conditions, such as cancer and AIDS.
The American College of Sports Medicine acknowledges that AAS, in the presence of adequate diet, can contribute to increases in body weight, often as lean mass increases and that the gains in muscular strength achieved through high-intensity exercise and proper diet can be additionally increased by the use of AAS in some individuals.
Health risks can be produced by long-term use or excessive doses of AAS. These effects include harmful changes in cholesterol levels (increased low-density lipoprotein and decreased high-density lipoprotein), acne, high blood pressure, liver damage (mainly with most oral AAS), and dangerous changes in the structure of the left ventricle of the heart.
These risks are only increased when, as they often do, athletes take steroids alongside other drugs, causing significantly more damage to their bodies. The effect of anabolic steroids on the heart can cause myocardial infarction and strokes. Conditions pertaining to hormonal imbalances such as gynecomastia and testicular size reduction may also be caused by AAS.
In women and children, AAS can cause irreversible masculinization.
Ergogenic uses for AAS in sports, racing, and bodybuilding as performance-enhancing drugs are controversial because of their adverse effects and the potential to gain unfair advantage in physical competitions. Their use is referred to as doping and banned by most major sporting bodies.
Athletes have been looking for drugs to enhance their athletic abilities since the Olympics started in Ancient Greece. For many years, AAS have been by far the most detected doping substances in IOC-accredited laboratories. In countries where AAS are controlled substances, there is often a black market in which smuggled, clandestinely manufactured or even counterfeit drugs are sold to users.
Click on any of the following blue hyperlinks for more about Anabolic Steroids:
- Uses
- Adverse effects
- Pharmacology
- Chemistry
- History
- Society and culture
- Research
- See also:
- Selective androgen receptor modulator
- Antiandrogen
- Mossman-Pacey paradox
- Steroid rosacea
- Steroid use in Bollywood
- Bigger, Stronger, Faster
- Juiced: Wild Times, Rampant 'Roids, Smash Hits & How Baseball Got Big
- List of androgens/anabolic steroids available in the United States
- Media related to Anabolic-androgenic steroids at Wikimedia Commons
Calculating Heart Rate during a Cardio Workout Pictured below: my Weekly Workout Routine at Planet Fitness @ 76 years of age. Note that exercises are alternated between upper and lower body exercises. I used the recumbent bike for my 30 minute cardio workout at the beginning, then 50 minutes on other strength/endurance machines of my overall 80 minute workout day.
Know Your Target Heart Rates for Exercise, Losing Weight and Health
What should your heart rate be when working out, and how can you keep track of it? Our simple chart will help keep you in the target training zone, whether you want to lose weight or just maximize your workout.
Find out what normal resting and maximum heart rates are for your age and how exercise intensity and other factors affect heart rate.
How do you get your heart rate in the target zone?When you work out, are you doing too much or not enough? There’s a simple way to know: Your target heart rate helps you hit the bulls eye so you can get max benefit from every step, swing and squat. Even if you’re not a gym rat or elite athlete, knowing your heart rate (or pulse) can help you track your health and fitness level.
First Things First: Resting Heart Rate
Your resting heart rate is the number of times your heart beats per minute when you’re at rest. A good time to check it is in the morning after you’ve had a good night’s sleep, before you get out of bed or grab that first cup of java!
For most of us, between 60 and 100 beats per minute (bpm) is normal.1 The rate can be affected by factors like stress, anxiety, hormones, medication, and how physically active you are. An athlete or more active person may have a resting heart rate as low as 40 beats per minute. Now that’s chill!
When it comes to resting heart rate, lower is better. It usually means your heart muscle is in better condition and doesn’t have to work as hard to maintain a steady beat. Studies have found that a higher resting heart rate is linked with lower physical fitness and higher blood pressure and body weight.
Know Your Numbers: Maximum and Target Heart Rate:
The below table shows target heart rate zones for different ages. Your maximum heart rate is about 220 minus your age.
In the age category closest to yours, read across to find your target heart rates. Target heart rate during moderate intensity activities is about 50-70% of maximum heart rate, while during vigorous physical activity it’s about 70-85% of maximum.
The figures below are averages, so use them as a general guide:
What should your heart rate be when working out, and how can you keep track of it? Our simple chart will help keep you in the target training zone, whether you want to lose weight or just maximize your workout.
Find out what normal resting and maximum heart rates are for your age and how exercise intensity and other factors affect heart rate.
How do you get your heart rate in the target zone?When you work out, are you doing too much or not enough? There’s a simple way to know: Your target heart rate helps you hit the bulls eye so you can get max benefit from every step, swing and squat. Even if you’re not a gym rat or elite athlete, knowing your heart rate (or pulse) can help you track your health and fitness level.
First Things First: Resting Heart Rate
Your resting heart rate is the number of times your heart beats per minute when you’re at rest. A good time to check it is in the morning after you’ve had a good night’s sleep, before you get out of bed or grab that first cup of java!
For most of us, between 60 and 100 beats per minute (bpm) is normal.1 The rate can be affected by factors like stress, anxiety, hormones, medication, and how physically active you are. An athlete or more active person may have a resting heart rate as low as 40 beats per minute. Now that’s chill!
When it comes to resting heart rate, lower is better. It usually means your heart muscle is in better condition and doesn’t have to work as hard to maintain a steady beat. Studies have found that a higher resting heart rate is linked with lower physical fitness and higher blood pressure and body weight.
Know Your Numbers: Maximum and Target Heart Rate:
The below table shows target heart rate zones for different ages. Your maximum heart rate is about 220 minus your age.
In the age category closest to yours, read across to find your target heart rates. Target heart rate during moderate intensity activities is about 50-70% of maximum heart rate, while during vigorous physical activity it’s about 70-85% of maximum.
The figures below are averages, so use them as a general guide:
Hit the Target: Find Your Heart Rate from the above table.
Now that you have a target, you can monitor your heart rate to make sure you’re in the zone. As you exercise, periodically check your heart rate. A wearable activity tracker makes it super easy, but if you don’t use one you can also find it manually:
Important Note: Some drugs and medications affect heart rate, meaning you may have a lower maximum heart rate and target zone. If you have a heart condition or take medication, ask your healthcare provider what your heart rate should be.
So what’s in a number?
If your heart rate is too high, you’re straining. Slow your roll! If it’s too low, and the intensity feels “light” to “moderate,” you may want to push yourself to exercise a little harder, especially if you’re trying to lose weight.
If you’re just starting out, aim for the lower range of your target zone (50 percent) and gradually build up. In time, you’ll be able to exercise comfortably at up to 85 percent of your maximum heart rate!
[End of Article]
___________________________________________________________________________
Aerobic exercise (also known as cardio) is physical exercise of low to high intensity that depends primarily on the aerobic energy-generating process.
"Aerobic" means "relating to, involving, or requiring free oxygen", and refers to the use of oxygen to adequately meet energy demands during exercise via aerobic metabolism.
Generally, light-to-moderate intensity activities that are sufficiently supported by aerobic metabolism can be performed for extended periods of time.
What is generally called aerobic exercise might be better termed "solely aerobic", because it is designed to be low-intensity enough so that all carbohydrates are aerobically turned into energy.
When practiced in this way, examples of cardiovascular or aerobic exercise are medium to long distance running or jogging, swimming, cycling, and walking.
What qualifies as aerobic exercise:
Main article: Bioenergetic systems
Aerobic exercise comprises innumerable forms. In general, it is performed at a moderate level of intensity over a relatively long period of time. For example, running a long distance at a moderate pace is an aerobic exercise, but sprinting is not.
Playing singles tennis, with near-continuous motion, is generally considered aerobic activity, while golf or two person team tennis, with brief bursts of activity punctuated by more frequent breaks, may not be predominantly aerobic.
Some sports are thus inherently "aerobic", while other aerobic exercises, such as fartlek training or aerobic dance classes, are designed specifically to improve aerobic capacity and fitness. It is most common for aerobic exercises to involve the leg muscles, primarily or exclusively.
There are some exceptions. For example, rowing to distances of 2,000 meters or more is an aerobic sport that exercises several major muscle groups, including those of the legs, abdominals, chest, and arms.
Aerobic versus anaerobic exercise:
Aerobic exercise and fitness can be contrasted with anaerobic exercise, of which strength training and short-distance running are the most salient examples. The two types of exercise differ by the duration and intensity of muscular contractions involved, as well as by how energy is generated within the muscle.
New research on the endocrine functions of contracting muscles has shown that both aerobic and anaerobic exercise promote the secretion of myokines, with attendant benefits including growth of new tissue, tissue repair, and various anti-inflammatory functions, which in turn reduce the risk of developing various inflammatory diseases.
Myokine secretion in turn is dependent on the amount of muscle contracted, and the duration and intensity of contraction. As such, both types of exercise produce endocrine benefits.
In almost all conditions, anaerobic exercise is accompanied by aerobic exercises because the less efficient anaerobic metabolism must supplement the aerobic system due to energy demands that exceed the aerobic system's capacity. Common kettlebell exercises combine aerobic and anaerobic aspects.
Benefits:
Cooper himself defines aerobic exercise as the ability to use the maximum amount of oxygen during exhaustive work. Cooper describes some of the major health benefits of aerobic exercise, such as gaining more efficient lungs by maximizing breathing capacity, thereby increasing ability to ventilate more air in a shorter period of time. As breathing capacity increases, one is able to extract oxygen more quickly into the blood stream, increasing elimination of carbon dioxide.
With aerobic exercise the heart becomes more efficient at functioning, and blood volume, hemoglobin and red blood cells increase, enhancing the ability of the body to transport oxygen from the lungs into the blood and muscles.
Metabolism will change and enable consumption of more calories without putting on weight. Aerobic exercise can delay osteoporosis as there is an increase in muscle mass, a loss of fat and an increase in bone density. With these variables increasing, there is a decrease in likelihood of diabetes as muscles use sugars better than fat.
One of the major benefits of aerobic exercise is that body weight may decrease slowly; it will only decrease at a rapid pace if there is a calorie restriction, therefore reducing obesity rates.
Health benefits:
Among the recognized health benefits of doing regular aerobic exercise are:
High-impact aerobic activities (such as jogging or using a skipping rope) can:
Body performance benefits:
In addition to the health benefits of aerobic exercise, there are numerous performance benefits:
Disadvantages:
Some drawbacks of aerobic exercise include:
Both the health benefits and the performance benefits, or "training effect", require that the duration and the frequency of exercise both exceed a certain minimum. Most authorities suggest at least twenty minutes performed at least three times per week.
Success in aerobic exercise businesses:
Aerobic exercise has long been a popular approach to achieving weight loss and physical fitness, often taking a commercial form.
Click on any of the following blue hyperlinks for more about Aerobic Exercise:
Now that you have a target, you can monitor your heart rate to make sure you’re in the zone. As you exercise, periodically check your heart rate. A wearable activity tracker makes it super easy, but if you don’t use one you can also find it manually:
- Take your pulse on the inside of your wrist, on the thumb side.
- Use the tips of your first two fingers (not your thumb) and press lightly over the artery.
- Count your pulse for 30 seconds and multiply by 2 to find your beats per minute.
Important Note: Some drugs and medications affect heart rate, meaning you may have a lower maximum heart rate and target zone. If you have a heart condition or take medication, ask your healthcare provider what your heart rate should be.
So what’s in a number?
If your heart rate is too high, you’re straining. Slow your roll! If it’s too low, and the intensity feels “light” to “moderate,” you may want to push yourself to exercise a little harder, especially if you’re trying to lose weight.
If you’re just starting out, aim for the lower range of your target zone (50 percent) and gradually build up. In time, you’ll be able to exercise comfortably at up to 85 percent of your maximum heart rate!
[End of Article]
___________________________________________________________________________
Aerobic exercise (also known as cardio) is physical exercise of low to high intensity that depends primarily on the aerobic energy-generating process.
"Aerobic" means "relating to, involving, or requiring free oxygen", and refers to the use of oxygen to adequately meet energy demands during exercise via aerobic metabolism.
Generally, light-to-moderate intensity activities that are sufficiently supported by aerobic metabolism can be performed for extended periods of time.
What is generally called aerobic exercise might be better termed "solely aerobic", because it is designed to be low-intensity enough so that all carbohydrates are aerobically turned into energy.
When practiced in this way, examples of cardiovascular or aerobic exercise are medium to long distance running or jogging, swimming, cycling, and walking.
What qualifies as aerobic exercise:
Main article: Bioenergetic systems
Aerobic exercise comprises innumerable forms. In general, it is performed at a moderate level of intensity over a relatively long period of time. For example, running a long distance at a moderate pace is an aerobic exercise, but sprinting is not.
Playing singles tennis, with near-continuous motion, is generally considered aerobic activity, while golf or two person team tennis, with brief bursts of activity punctuated by more frequent breaks, may not be predominantly aerobic.
Some sports are thus inherently "aerobic", while other aerobic exercises, such as fartlek training or aerobic dance classes, are designed specifically to improve aerobic capacity and fitness. It is most common for aerobic exercises to involve the leg muscles, primarily or exclusively.
There are some exceptions. For example, rowing to distances of 2,000 meters or more is an aerobic sport that exercises several major muscle groups, including those of the legs, abdominals, chest, and arms.
Aerobic versus anaerobic exercise:
Aerobic exercise and fitness can be contrasted with anaerobic exercise, of which strength training and short-distance running are the most salient examples. The two types of exercise differ by the duration and intensity of muscular contractions involved, as well as by how energy is generated within the muscle.
New research on the endocrine functions of contracting muscles has shown that both aerobic and anaerobic exercise promote the secretion of myokines, with attendant benefits including growth of new tissue, tissue repair, and various anti-inflammatory functions, which in turn reduce the risk of developing various inflammatory diseases.
Myokine secretion in turn is dependent on the amount of muscle contracted, and the duration and intensity of contraction. As such, both types of exercise produce endocrine benefits.
In almost all conditions, anaerobic exercise is accompanied by aerobic exercises because the less efficient anaerobic metabolism must supplement the aerobic system due to energy demands that exceed the aerobic system's capacity. Common kettlebell exercises combine aerobic and anaerobic aspects.
Benefits:
Cooper himself defines aerobic exercise as the ability to use the maximum amount of oxygen during exhaustive work. Cooper describes some of the major health benefits of aerobic exercise, such as gaining more efficient lungs by maximizing breathing capacity, thereby increasing ability to ventilate more air in a shorter period of time. As breathing capacity increases, one is able to extract oxygen more quickly into the blood stream, increasing elimination of carbon dioxide.
With aerobic exercise the heart becomes more efficient at functioning, and blood volume, hemoglobin and red blood cells increase, enhancing the ability of the body to transport oxygen from the lungs into the blood and muscles.
Metabolism will change and enable consumption of more calories without putting on weight. Aerobic exercise can delay osteoporosis as there is an increase in muscle mass, a loss of fat and an increase in bone density. With these variables increasing, there is a decrease in likelihood of diabetes as muscles use sugars better than fat.
One of the major benefits of aerobic exercise is that body weight may decrease slowly; it will only decrease at a rapid pace if there is a calorie restriction, therefore reducing obesity rates.
Health benefits:
Among the recognized health benefits of doing regular aerobic exercise are:
- Strengthening the muscles involved in respiration, to facilitate the flow of air in and out of the lungs
- Strengthening and enlarging the heart muscle, to improve its pumping efficiency and reduce the resting heart rate, known as aerobic conditioning
- Improving circulation efficiency and reducing blood pressure
- Increasing the total number of red blood cells in the body, facilitating transport of oxygen
- Improving mental health, including reducing stress and lowering the incidence of depression, as well as increased cognitive capacity.
- Reducing the risk for diabetes (One meta-analysis has shown, from multiple conducted studies, that aerobic exercise does help lower Hb A1Clevels for type 2 diabetics.)
- Reducing the risk of death due to cardiovascular problems
High-impact aerobic activities (such as jogging or using a skipping rope) can:
- Stimulate bone growth
- Reduce the risk of osteoporosis for both men and women
Body performance benefits:
In addition to the health benefits of aerobic exercise, there are numerous performance benefits:
- Increasing storage of energy molecules such as fats and carbohydrates within the muscles, allowing for increased endurance
- Neovascularization of the muscle sarcomeres to increase blood flow through the muscles
- Increasing speed at which aerobic metabolism is activated within muscles, allowing a greater portion of energy for intense exercise to be generated aerobically
- Improving the ability of muscles to use fats during exercise, preserving intramuscular glycogen
- Enhancing the speed at which muscles recover from high intensity exercise
- Improvement in brain structural connections
- Increase in gray matter density
- New neuron growth
- Improvement in cognitive function (cognitive control and various forms of memory)
- Improvement or maintenance of mental health
Disadvantages:
Some drawbacks of aerobic exercise include:
- Overuse injuries because of repetitive, high-impact exercise such as distance running
- Is not an effective approach to building muscle
- Not an effective form of fat loss, unless used consistently
Both the health benefits and the performance benefits, or "training effect", require that the duration and the frequency of exercise both exceed a certain minimum. Most authorities suggest at least twenty minutes performed at least three times per week.
Success in aerobic exercise businesses:
Aerobic exercise has long been a popular approach to achieving weight loss and physical fitness, often taking a commercial form.
- In the 1970s, Judi Sheppard Missett helped create the market for commercial aerobics with her Jazzercise program
- In the 1980s, Richard Simmons hosted an aerobic exercise show on television, and also released a series of exercise videos
- In the 1990s, Billy Blanks's Tae Bo helped popularize cardio-boxing workouts that incorporated martial arts movements
Click on any of the following blue hyperlinks for more about Aerobic Exercise:
- History
- Types of aerobic exercise
- See also:
Health Care Reform in the United States including Exploring the Next Phase of Healthcare Reform by Harvard School of Public Health Pictured below:
Exploring the Next Phase of Health Care Reform: How Health Care Leaders Can Position Their Organizations for Success by Harvard School of Public Health
These are uncertain times in American health care. The Republican Congress and President Trump have vowed to repeal and replace the Patient Protection and Affordable Care Act (ACA), commonly called Obamacare. They recently unveiled the American Health Care Act, the replacement plan, which has met with substantial resistance from all parts of the political spectrum.
The current political and policy environment has left many health care leaders and other stakeholders wondering what to expect and how best to position their organizations for the next phase of health care reform.
The Potential Effects of Proposed Changes:
House Republicans recently introduced legislation intended to create a new health plan, retaining some provisions of Obamacare and eliminating or scaling back others.
While the exact details may continue to change in the coming weeks as the bill moves through Congress, there are some specific themes that can be expected in the final version that becomes law, according to John E. McDonough, DrPH, MPA, Program Director of Preparing for What’s Next in U.S. Health Reform and Director of the Center for Executive and Continuing Professional Education at the Harvard T.H. Chan School of Public Health.
McDonough, who served as a Senior Advisor on National Health Reform to the U.S. Senate Committee on Health, Education, Labor, and Pensions, explains that there are two major components of the ACA that will be affected by whatever legislation is passed. These are access and value.
Two Main Themes: Access and Value:
The first area, access, refers to insurance coverage for uninsured and underinsured Americans. While a significant impact of the ACA was that it expanded its Medicaid offerings to states to cover vulnerable residents, a number of Americans are now at risk of losing this support under whatever new plan is ultimately passed.
There are two major components of the ACA that will be affected by whatever legislation is passed. These are access and value.
“Many, many individuals have gotten health insurance coverage from ACA and [some of them] are quite concerned about whether they will still have coverage in three months, six months, or a year,” McDonough says.
The second area, value, refers to a focus started by the ACA to improve the quality, efficiency, and effectiveness of medical care in the United States. “The evidence shows Americans get care from our medical system that is not as high quality as we have a right to expect because of high costs,” McDonough says.
The ACA established a number of initiatives to address this fact, including creating Accountable Care Organizations (ACOs), providing bundled payment plans, and imposing penalties on hospitals with very high rates of readmissions and hospital-acquired infections.
These types of efforts, which are part of a broader push to transform the health care delivery system to ensure a greater focus on value, are receiving widespread support from both Republicans and Democrats, which means that they should continue, and even grow, under any new health care law, McDonough stresses.
“There seems to be a growing sense in the health care community that [the move to value-based payment and population health management] pushed forward under ACA should continue and expand,” McDonough says, adding that this is one piece of good news in the sea of uncertainty that exists.
Preparing for New Developments:
Ashish Jha, MD, MPH, Professor of International Health and Health Policy at the Harvard T.H. Chan School of Public Health, Director of the Harvard Global Health Institute, and a practicing general internist at the VA, agrees with this assessment. “The journey we began with ACA to move to value-based health care is going to continue,” he says. “But what form it will take, how we will do it, and how much is voluntary verses mandatory” remain to be seen moving forward.
He points out that this means that professionals need to know the range of options in order to be prepared for whatever way the field goes. “They need to ask, ‘What is the range and how do I prepare, so I will be in good shape?’’’ he explains.
Trends to Watch:
Jha, who is also faculty on Preparing for What’s Next in U.S. Health Reform, points to a number of other changes also started under the ACA that, regardless of the final health plan passed, will continue to affect organizations over the next few years.
For instance, people today are responsible for a growing portion of their own health care costs. This changes the way that organizations collect their money, meaning organizations need to find new ways of operating.
There will be many moral and ethical dilemmas for organizations as access shrinks and many patients lose coverage under the new plan. “I think health care leaders are very used to a world where they provide services to patients and get paid by insurers, or the government/Medicare or Medicaid. But now they’re waking up to a new model where they are getting a larger chunk from patients. They’re not used to collecting money from patients themselves and that will change their relationships,” Jha says.
With customers footing more of the bill, they now have higher expectations from providers. “The customer is changing, and what will customers want in return now that they’re writing the check? That becomes a really important issue for providers to focus on. It’s part of patient-centered care. Now patients are in the driver’s seat,” he stresses.
Another issue worth paying attention to on the value side of the equation is that participation in some Medicare bundled payment programs will be voluntary for now, but is ultimately expected to become mandatory in the not-too-distant future. This raises some interesting questions for organizations, as they grapple with whether to use the voluntary program to get acclimated. Organizations that don’t participate now could end up having a lot of catching up to do in the future, which could “have very serious consequences three to five years down the road,” Jha says.
Issues to Watch:
On the access side of things, Jha points out that there will also be many moral and ethical dilemmas for organizations as access shrinks and many patients lose coverage under the new plan.
Five years ago, many people were uninsured and had no contact with the health care system. “Now, these people have been covered and have become part of the organizations [that serve them]. They have developed relationships with their doctors, so it’s a big difference now when they lose coverage,” he says. “Are organizations really going to walk away from these patients? [And if not], how will health systems manage the financial debt they will incur to care for the uninsured?”
Another important trend that will impact many health organizations moving forward revolves around consolidation. “Doctors are being bought out by big hospitals. We have no idea how the Trump Administration will feel about that. Consolidation is a strategy that provider organizations have used to survive, getting bigger. But that gravy train for providers is coming to an end. Now, with more people uninsured, and more focus on value, there are broader market issues around consolidation and integration that will be challenging for providers,” Jha says.
Other Trends Worth Following:
Other trends that will continue to impact organizations include the growing push for providers to use interconnected Electronic Health Records (EHR). This is an important tool to help track and achieve key benchmarks of value-based care and improve coordination among providers for increased efficiency and better outcomes.
“While everyone thinks this is a good thing, and most organizations have made the leap into EHRs, people, especially frontline doctors and nurses, are very frustrated with these systems. How organizations will manage the transition between simply adopting the EHR and using it in ways that lead to meaningfully better care is the challenge ahead,” Jha says.
In addition, Jha says that the Trump Administration’s tougher restrictions on immigration may have a real effect on health systems that needs to be addressed up front. “Twenty-five percent of doctors in our country are foreign medical graduates, as are a large population of our nurses and other health professionals,” he says.
“As immigration gets tighter, there’s a question as to whether we will have a harder time attracting the best and brightest in the world. So health care will have a hard time building their ranks” in the future. With an aging population, this means that health systems may have challenges creating a good workforce to care for them.
The Importance of Staying Up-to-Date:
With so many fluctuations expected in how the health care system will do business in the coming months and years, both Jha and McDonough say that it is crucial for health care leaders to stay abreast of the latest developments as they progress.
One of the most important things is for health care leaders to stay in touch with what is happening out there and pay attention to the coverage in the media. “One of the most important things is for health care leaders to stay in touch with what is happening out there and pay attention to the coverage in the media,” McDonough says. “If you work in a hospital, [you will need to] follow the national organizations, such as the American Hospital Association, and stay alert to the opinions of experts as to what might happen,” he says.
But that alone will not be enough, says Jha. Understanding the nuances of policy changes will be critical for leaders to stay on top of the shifting requirements—and opportunities—that exist in the current environment so they can strategically position their organizations for success.
Harvard T.H. Chan School of Public Health offers Preparing for What’s Next in U.S. Health Reform, which offers key lessons involving health reform from the nation’s leading policy experts under the new federal administration. To learn more about this opportunity, click here.
[End of Article]
___________________________________________________________________________
Healthcare reform in the United States has a long history. Reforms have often been proposed but have rarely been accomplished.
In 2010, landmark reform was passed through two federal statutes enacted in 2010: the Patient Protection and Affordable Care Act (PPACA), signed March 23, 2010, and the Health Care and Education Reconciliation Act of 2010 (H.R. 4872), which amended the PPACA and became law on March 30, 2010.
Future reforms of the American health care system continue to be proposed, with notable proposals including a single-payer system and a reduction in fee-for-service medical care. The PPACA includes a new agency, the Center for Medicare and Medicaid Innovation (CMS Innovation Center), which is intended to research reform ideas through pilot projects.
History of national reform efforts:
Main article: History of health care reform in the United States
Motivation:
Main article: Healthcare reform debate in the United States
International comparisons of healthcare have found that the United States spends more per-capita than other similarly developed nations but falls below similar countries in various health metrics, suggesting inefficiency and waste.
In addition, the United States has significant underinsurance and significant impending unfunded liabilities from its aging demographic and its social insurance programs Medicare and Medicaid (Medicaid provides free long-term care to the elderly poor). The fiscal and human impact of these issues have motivated reform proposals.
U.S. healthcare costs were approximately $3.2 trillion or nearly $10,000 per person on average in 2015. Major categories of expense include hospital care (32%), physician and clinical services (20%), and prescription drugs (10%). U.S. costs in 2016 were substantially higher than other OECD countries, at 17.2% GDP versus 12.4% GDP for the next most expensive country (Switzerland). For scale, a 5% GDP difference represents about $1 trillion or $3,000 per person.
Some of the many reasons cited for the cost differential with other countries include: Higher administrative costs of a private system with multiple payment processes; higher costs for the same products and services; more expensive volume/mix of services with higher usage of more expensive specialists; aggressive treatment of very sick elderly versus palliative care; less use of government intervention in pricing; and higher income levels driving greater demand for healthcare. Healthcare costs are a fundamental driver of health insurance costs, which leads to coverage affordability challenges for millions of families.
There is ongoing debate whether the current law (ACA/Obamacare) and the Republican alternatives (AHCA and BCRA) do enough to address the cost challenge.
According to 2009 World Bank statistics, the U.S. had the highest health care costs relative to the size of the economy (GDP) in the world, even though estimated 50 million citizens (approximately 16% of the September 2011 estimated population of 312 million) lacked insurance. In March 2010, billionaire Warren Buffett commented that the high costs paid by U.S. companies for their employees' health care put them at a competitive disadvantage.
Life expectancy compared to healthcare spending from 1970 to 2008, in the US and the next 19 most wealthy countries by total GDP. Further, an estimated 77 million Baby Boomers are reaching retirement age, which combined with significant annual increases in healthcare costs per person will place enormous budgetary strain on U.S. state and federal governments, particularly through Medicare and Medicaid spending (Medicaid provides long-term care for the elderly poor). Maintaining the long-term fiscal health of the U.S. federal government is significantly dependent on healthcare costs being controlled.
Insurance cost and availability:
Further information: Health insurance coverage in the United States
In addition, the number of employers who offer health insurance has declined and costs for employer-paid health insurance are rising: from 2001 to 2007, premiums for family coverage increased 78%, while wages rose 19% and prices rose 17%, according to the Kaiser Family Foundation.
Even for those who are employed, the private insurance in the US varies greatly in its coverage; one study by the Commonwealth Fund published in Health Affairs estimated that 16 million U.S. adults were underinsured in 2003. The underinsured were significantly more likely than those with adequate insurance to forgo health care, report financial stress because of medical bills, and experience coverage gaps for such items as prescription drugs.
The study found that underinsurance disproportionately affects those with lower incomes—73% of the underinsured in the study population had annual incomes below 200% of the federal poverty level.
However, a study published by the Kaiser Family Foundation in 2008 found that the typical large employer preferred provider organization (PPO) plan in 2007 was more generous than either Medicare or the Federal Employees Health Benefits Program Standard Option.
One indicator of the consequences of Americans' inconsistent health care coverage is a study in Health Affairs that concluded that half of personal bankruptcys involved medical bills, although other sources dispute this.
There are health losses from insufficient health insurance. A 2009 Harvard study published in the American Journal of Public Health found more than 44,800 excess deaths annually in the United States due to Americans lacking health insurance.
More broadly, estimates of the total number of people in the United States, whether insured or uninsured, who die because of lack of medical care were estimated in a 1997 analysis to be nearly 100,000 per year. A study of the effects of the Massachusetts universal health care law (which took effect in 2006) found a 3% drop in mortality among people 20–64 years old—1 death per 830 people with insurance.
Other studies, just as those examining the randomized distribution of Medicaid insurance to low-income people in Oregon in 2008, found no change in death rate.
The cost of insurance has been a primary motivation in the reform of the US healthcare system, and many different explanations have been proposed in the reasons for high insurance costs and how to remedy them. One critique and motivation for healthcare reform has been the development of the medical–industrial complex. This relates to moral arguments for health care reform, framing healthcare as a social good, one that is fundamentally immoral to deny to people based on economic status.
The motivation behind healthcare reform in response to the medical-industrial complex also stems from issues of social inequity, promotion of medicine over preventative care. The medical-industrial complex, defined as a network of health insurance companies, pharmaceutical companies, and the like, plays a role in the complexity of the US insurance market and a fine line between government and industry within it.
Likewise, critiques of insurance markets being conducted under a capitalistic, free-market model also include that medical solutions, as opposed to preventative healthcare measures, are promoted to maintain this medical-industrial complex. Arguments for a market-based approach to health insurance include the Grossman model, which is based on an ideal competitive model, but others have critiqued this, arguing that fundamentally, this means that people in higher socioeconomic levels will receive a better quality of healthcare.
Uninsured rate:
With the implementation of the ACA, the level of uninsured rates severely decreased in the U.S. . This is due to the expansion of qualifications for access to medicaid, subsidizing insurance, prevention of insurance companies from underwriting, as well as enforcing the individual mandate which requires citizens to purchase health insurance or pay a fee.
In a research study which was conducted comparing the effects of the ACA before and after it was fully implemented in 2014, it was discovered that racial and ethnic minorities benefited more than whites with many gaining insurance coverage which they lacked before allowing for many to seek treatment improving their overall health.
In June 2014, Gallup–Healthways Well–Being conducted a survey and found that the uninsured rate is decreasing with 13 percent of U.S. adults uninsured in 2014 compared to 17 percent in January 2014 and translates to roughly 10 million to 11 million individuals who gained coverage.
The survey also looked at the major demographic groups and found each is making progress towards getting health insurance. However, Hispanics, who have the highest uninsured rate of any racial or ethnic group, are lagging in their progress. Under the new health care reform, Latinos were expected to be major beneficiaries of the new health care law. Gallup found that the biggest drop in the uninsured rate (3 percentage points) was among households making less than $36,000 a year.
Waste and fraud:
In December 2011 the outgoing Administrator of the Centers for Medicare & Medicaid Services, Donald Berwick, asserted that 20% to 30% of health care spending is waste. He listed five causes for the waste: (1) overtreatment of patients, (2) the failure to coordinate care, (3) the administrative complexity of the health care system, (4) burdensome rules and (5) fraud.
An estimated 3–10% of all health care expenditures in the U.S. are fraudulent. In 2011, Medicare and Medicaid made $65 billion in improper payments (including both error and fraud). Government efforts to reduce fraud include $4 billion in fraudulent payments recovered by the Department of Justice and the FBI in 2012, longer jail sentences specified by the Affordable Care Act, and Senior Medicare Patrols—volunteers trained to identify and report fraud.
In 2007, the Department of Justice and Health and Human Services formed the Medicare Fraud Strike Force to combat fraud through data analysis and increased community policing.
As of May 2013, the Strike Force has charged more than 1,500 people for false billings of more than $5 billion. Medicare fraud often takes the form of kickbacks and money-laundering. Fraud schemes often take the form of billing for medically unnecessary services or services not rendered.
Quality of care:
There is significant debate regarding the quality of the U.S. healthcare system relative to those of other countries. Although there are advancements in the quality of care in America due to the acknowledgement of various health related topics such as how insurance plans are now mandated to include coverage for those with mental health and substance abuse disorders as well with the inability to deny a person who has preexisting conditions through the ACA, there is still much that needs to be improved.
Within the U.S., those who are a racial/ethnic minority along with those who poses a lower income have higher chances of experiencing a lower quality of care at higher cost. Despite the advancements with the ACA, this may discourage a person from seeking medical treatment.
Physicians for a National Health Program, a pro-universal single-payer system of health care advocacy group, has claimed that a free market solution to health care provides a lower quality of care, with higher mortality rates, than publicly funded systems. The quality of health maintenance organizations and managed care have also been criticized by this same group.
According to a 2000 study of the World Health Organization, publicly funded systems of industrial nations spend less on health care, both as a percentage of their GDP and per capita, and enjoy superior population-based health care outcomes.
However, conservative commentator David Gratzer and the Cato Institute, a libertarian think tank, have both criticized the WHO's comparison method for being biased; the WHO study marked down countries for having private or fee-paying health treatment and rated countries by comparison to their expected health care performance, rather than objectively comparing quality of care.
Some medical researchers say that patient satisfaction surveys are a poor way to evaluate medical care. Researchers at the RAND Corporation and the Department of Veterans Affairs asked 236 elderly patients in two different managed care plans to rate their care, then examined care in medical records, as reported in Annals of Internal Medicine. There was no correlation. "Patient ratings of health care are easy to obtain and report, but do not accurately measure the technical quality of medical care," said John T. Chang, UCLA, lead author.
Public opinion:
Public opinion polls have shown a majority of the public supports various levels of government involvement in health care in the United States, with stated preferences depending on how the question is asked.
Polls from Harvard University in 1988, the Los Angeles Times in 1990, and the Wall Street Journal in 1991 all showed strong support for a health care system compared to the system in Canada.
More recently, however, polling support has declined for that sort of health care system, with a 2007 Yahoo/AP poll showing 54% of respondents considered themselves supporters of "single-payer health care," a majority in favor of a number of reforms according to a joint poll with the Los Angeles Times and Bloomberg, and a plurality of respondents in a 2009 poll for Time Magazine showed support for "a national single-payer plan similar to Medicare for all."
Polls by Rasmussen Reports in 2011 and 2012 showed pluralities opposed to single-payer health care. Many other polls show support for various levels of government involvement in health care, including polls from New York Times/CBS News and Washington Post/ABC News, showing favorability for a form of national health insurance.
The Kaiser Family Foundation showed 58% in favor of a national health plan such as Medicare-for-all in 2009, with support around the same level from 2017 to April 2019, when 56% said they supported it. A Quinnipiac poll in three states in 2008 found majority support for the government ensuring "that everyone in the United States has adequate health-care" among likely Democratic primary voters.
A 2001 article in the public health journal Health Affairs studied fifty years of American public opinion of various health care plans and concluded that, while there appears to be general support of a "national health care plan," poll respondents "remain satisfied with their current medical arrangements, do not trust the federal government to do what is right, and do not favor a single-payer type of national health plan."
Politifact rated a 2009 statement by Michael Moore "false" when he stated that "[t]he majority actually want single-payer health care." According to Politifact, responses on these polls largely depend on the wording. For example, people respond more favorably when they are asked if they want a system "like Medicare".
Alternatives and research directions:
There are alternatives to the exchange-based market system which was enacted by the Patient Protection and Affordable Care Act which have been proposed in the past and continue to be proposed, such as a single-payer system and allowing health insurance to be regulated at the federal level.
In addition, the Patient Protection and Affordable Health Care Act of 2010 contained provisions which allows the Centers for Medicare and Medicaid Services (CMS) to undertake pilot projects which, if they are successful could be implemented in future.
Single-payer health care:
Further information: Single-payer healthcare § United States
A number of proposals have been made for a universal single-payer healthcare system in the United States, most recently the United States National Health Care Act, (popularly known as H.R. 676 or "Medicare for All") but none have achieved more political support than 20% congressional co-sponsorship.
Advocates argue that preventative health care expenditures can save several hundreds of billions of dollars per year because publicly funded universal health care would benefit employers and consumers, that employers would benefit from a bigger pool of potential customers and that employers would likely pay less, and would be spared administrative costs of health care benefits.
It is also argued that inequities between employers would be reduced. Also, for example, cancer patients are more likely to be diagnosed at Stage I where curative treatment is typically a few outpatient visits, instead of at Stage III or later in an emergency room where treatment can involve years of hospitalization and is often terminal.
Others have estimated a long-term savings amounting to 40% of all national health expenditures due to preventative health care, although estimates from the Congressional Budget Office and The New England Journal of Medicine have found that preventative care is more expensive.
Any national system would be paid for in part through taxes replacing insurance premiums, but advocates also believe savings would be realized through preventative care and the elimination of insurance company overhead and hospital billing costs. An analysis of a single-payer bill by the Physicians for a National Health Program estimated the immediate savings at $350 billion per year.
The Commonwealth Fund believes that, if the United States adopted a universal health care system, the mortality rate would improve and the country would save approximately $570 billion a year.
Recent enactments of single-payer systems within individual states, such as in Vermont in 2011, may serve as living models supporting federal single-payer coverage. The plan in Vermont, however, has failed.
On June 1, 2017, in light of the recent Trump Administration’s efforts to repeal the Affordable Care Act, California Democratic Senator Ricardo Lara proposed a bill to establish single-payer healthcare within the state of California (SB 562), calling on fellow senators to act quickly in defense of healthcare.
The legislation would implement “Medicare for All,” placing all levels of healthcare in the hands of the state. The bill proposed to the California Senate by Senator Lara lacked a method of funding required to finance the $400 billion-dollar policy. Despite this lack of foresight, the bill gained approval from the senate and will move on to await approval by the state assembly.
In wake of the Affordable Care Act, the state of California has experienced the greatest rise in newly insured people compared to other states. Subsequently, the number of physicians under MediCal are not enough to meet the demand, therefore 25% of physicians care for 80% of patients who are covered through MediCal.
In the past, California has struggled to maintain healthcare effectiveness, due in part to its unstable budget and complex regulations. The state has a policy in place known as the Gann Limit, otherwise entitled proposition 98, which ensures that a portion of state funds are directed towards the education system.
This limit would be exceeded if California raises taxes to fund the new system which would require $100 billion in tax revenue. In order to avoid legal dispute, voters would be required to amend proposition 98 and exempt healthcare funding from required educational contributions.
The state announced on August 1, 2017 that coverage for health insurance will increase by 12.5% in next year, threatening the coverage of 1.5 million people.
Public option:
Main article: Public health insurance option
In January 2013, Representative Jan Schakowsky and 44 other U.S. House of Representatives Democrats introduced H.R. 261, the "Public Option Deficit Reduction Act" which would amend the 2010 Affordable Care Act to create a public option. The bill would set up a government-run health insurance plan with premiums 5% to 7% percent lower than private insurance. The Congressional Budget Office estimated it would reduce the United States public debt by $104 billion over 10 years.
Balancing doctor supply and demand:
The Medicare Graduate Medical Education program regulates the supply of medical doctors in the U.S. By adjusting the reimbursement rates to establish more income equality among the medical professions, the effective cost of medical care can be lowered.
Bundled payments:
A key project is one that could radically change the way the medical profession is paid for services under Medicare and Medicaid. The current system, which is also the prime system used by medical insurers is known as fee-for-service because the medical practitioner is paid only for the performance of medical procedures which, it is argued means that doctors have a financial incentive to do more tests (which generates more income) which may not be in the patients' best long-term interest.
The current system encourages medical interventions such as surgeries and prescribed medicines (all of which carry some risk for the patient but increase revenues for the medical care industry) and does not reward other activities such as encouraging behavioral changes such as modifying dietary habits and quitting smoking, or follow-ups regarding prescribed regimes which could have better outcomes for the patient at a lower cost.
The current fee-for-service system also rewards bad hospitals for bad service. Some have noted that the best hospitals have fewer re-admission rates than others, which benefits patients, but some of the worst hospitals have high re-admission rates which is bad for patients but is perversely rewarded under the fee-for-service system.
Projects at CMS are examining the possibility of rewarding health care providers through a process known as "bundled payments" by which local doctors and hospitals in an area would be paid not on a fee for service basis but on a capitation system linked to outcomes.
The areas with the best outcomes would get more. This system, it is argued, makes medical practitioners much more concerned to focus on activities that deliver real health benefits at a lower cost to the system by removing the perversities inherent in the fee-for-service system.
Though aimed as a model for health care funded by CMS, if the project is successful it is thought that the model could be followed by the commercial health insurance industry also.
Centers for Medicare and Medicaid Innovation. With the ACA improving the health of many by increasing the number of people who are insured, this is not the final stage for the ACA due to the push for a medicaid expansion reform.
With the Democrats supporting the expansion and the Republicans against it, it was denied in the Supreme Court in the trial of NFIB vs Sebelius. The Court ruled that implementing taxes in order to pay for health insurance for all citizens was an unconstitutional exercise of Congress’s power under Article I.
If the expansion eventually succeeds, Medicaid would become a fully federal program with new federal eligibility standards. This would alleviate the responsibility of state governments to fund Medicaid.
In addition to the reform for the medicaid expansion, there are additional reforms focused on addressing social determinants in the healthcare system through various programs and initiatives in order to reduce healthcare expenditures and improve health outcomes.
Programs and initiatives recognizing and addressing non-medical social needs have sprung from various sectors within healthcare, with emerging efforts made by multi-payer federal and state initiatives, medicaid initiatives led by states, or by health plans, as well as provider level actions.State and federal initiatives, primarily sponsored CMMI (Center for Medicare and Medicaid Innovation) a division of CMS, seek to address basic social needs within the context of the healthcare delivery system.
CMMI initiatives like the 2016 "Accountable Health Communities" (AHC) model have been created to focus on connecting Medicare and Medicaid beneficiaries with community services to address health-related social needs, while providing funds to organizations so that they can systematically identify and address the health-related social needs of Medicare and Medicaid recipients through screening, referral, and community navigation services.
The model was officially implemented in 2017 and will be evaluated for its ability to affect cost of healthcare spending and reduce inpatient/outpatient utilization in 2022. Under the AHC model, funds have been allocated towards developing a 10-item screening tool to identify 5 different patient need domains that can be addressed through community resources (housing instability, food insecurity, transportation difficulties, utility assistance needs, and interpersonal safety).
Increasing bodies of evidence suggest that addressing social needs can help stop their damaging health effects, but screening for social needs is not yet standard clinical practice. Applying this tool in the AHC model will help CMS evaluate the impact of local partnerships between healthcare providers and community organizations in advancing the aims of addressing the cost and quality of health care across all settings.
National recommendations around multi-dimension screening for social risk are not yet available since the evidence base to support such recommendations is highly under-developed at present.
More research is still needed in this area to be able to demonstrate whether screening for social risk, and especially for multiple domains of social risk, will succeed in meeting the Wilson and Jungner screening criteria.
Health plan specific initiatives:
Due to how new CMMI initiatives are, evidence supporting the effectiveness of its various initiatives of reducing healthcare spending and improving health outcomes of patients is relatively small, but is expected to grow within the coming years as many of CMMI's programs and initiatives will be due for their programmatic performance evaluation.
However, it remains that there is more evidence of smaller scale initiatives in individual health plans/hospitals/clinics, as several health plans, hospitals, and clinics have sought out to address social determinants of health within their scope of care.
Transportation:
Transportation is a key social determinant impacting patient outcomes with approximately 3.6 million individuals unable to receive the necessary medical care due to transportation barrier, according to recent study.
In addition, these 3.6 million experience multiple conditions at a much higher rate than those who have stable access to transportation. Many conditions that they face, however, can be managed if appropriate care is made available.
For some conditions, this care is cost-effective and results in health care cost savings that outweigh added transportation costs. without access to reliable, affordable, and convenient transportation, patients miss appointments and end up costing clinics money.
According to a cross-study analysis, missed appointments and care delays cost the healthcare industry $150 billion each year. Patients without transportation are also less likely to take medications as directed. One study found that 65 percent of patients felt transportation assistance would enable them to fill prescriptions as directed after discharge.
According to a recent article published in the Journal of the American Medical Association, ride-sharing services such as Lyft and Uber can improve that healthcare disparity and cut down on the $2.7 million the federal government spends each year on non-emergency medical transportation services.
To recover revenue and improve care quality, some health systems like MedStar Health and Denver Health Medical Center are teaming up with Uber, Lyft, and other ride-sharing companies to connect patients with transportation.
Housing:
The University of Illinois Hospital, part of the University of Illinois Hospital & Health Sciences System, identified that large portion of the individuals with high rates of emergency department were also chronically homeless, and that these individuals were in the 10th decile for patient cost, with annual per patient expenses ranging from $51,000 to $533,000.
The University of Illinois partnered with a community group called the Center for Housing and Health to initiate the Better Health Through Housing initiative in 2015, an initiative that connected chronically homeless individuals with transitional housing and case managers. In partnering with the Center for Housing and Health, the University of Illinois Hospital saw participant healthcare costs fall 42 percent, and more recent studies have found that costs dropped by 61 percent. The hospital's emergency department reported a 35% reduction in use.
Malnutrition:
Some health plans have chosen to address some SDOH within their own means by establishing programs that directly deal with a single risk factor. Studies show that malnutrition can lead to higher costs of care and extended hospital states with the average hospital stay costing nearly $2,000 per day.
Advocate Health Care, an accountable care organization in Chicago, Illinois, implemented a nutrition care program at four of its Chicago area hospitals, an initiative that resulted in more than $4.8 million in cost savings within 6 months due to shorter hospital states and lower readmission rates (reduced 30 day readmission rates by 27% and the average hospital stay by nearly two days).
Trump administration efforts:
Donald Trump was elected president on a platform that included a pledge to "repeal and replace" the Patient Protection and Affordable Care Act (commonly called the Affordable Care Act or Obamacare). Rather than making adjustments to the Affordable Care Act, President Trump is proposing the American Health Care Act (AHCA), which was developed by the House of Representatives.
If passed, this new health care act would cause insurance and healthcare to return to the market potentially causing for 18 million Americans to become uninsured.
In addition to this, President Trump is pushing for a change in policies regarding "public charge" which would cause the public benefits such as health, nutrition, and housing programs that were previously excluded to count towards considering a person a public charge.
By doing this, immigrants who use these resources would have their ability to obtain legal permanent resident status affected increasing their chance of being denied citizenship.
The administration has suggested that the AHCA is only part of its reform efforts. Other proposals include allowing interstate competition in the health insurance market.
Incentivizing health reimbursement arrangements is another goal.
See also:
These are uncertain times in American health care. The Republican Congress and President Trump have vowed to repeal and replace the Patient Protection and Affordable Care Act (ACA), commonly called Obamacare. They recently unveiled the American Health Care Act, the replacement plan, which has met with substantial resistance from all parts of the political spectrum.
The current political and policy environment has left many health care leaders and other stakeholders wondering what to expect and how best to position their organizations for the next phase of health care reform.
The Potential Effects of Proposed Changes:
House Republicans recently introduced legislation intended to create a new health plan, retaining some provisions of Obamacare and eliminating or scaling back others.
While the exact details may continue to change in the coming weeks as the bill moves through Congress, there are some specific themes that can be expected in the final version that becomes law, according to John E. McDonough, DrPH, MPA, Program Director of Preparing for What’s Next in U.S. Health Reform and Director of the Center for Executive and Continuing Professional Education at the Harvard T.H. Chan School of Public Health.
McDonough, who served as a Senior Advisor on National Health Reform to the U.S. Senate Committee on Health, Education, Labor, and Pensions, explains that there are two major components of the ACA that will be affected by whatever legislation is passed. These are access and value.
Two Main Themes: Access and Value:
The first area, access, refers to insurance coverage for uninsured and underinsured Americans. While a significant impact of the ACA was that it expanded its Medicaid offerings to states to cover vulnerable residents, a number of Americans are now at risk of losing this support under whatever new plan is ultimately passed.
There are two major components of the ACA that will be affected by whatever legislation is passed. These are access and value.
“Many, many individuals have gotten health insurance coverage from ACA and [some of them] are quite concerned about whether they will still have coverage in three months, six months, or a year,” McDonough says.
The second area, value, refers to a focus started by the ACA to improve the quality, efficiency, and effectiveness of medical care in the United States. “The evidence shows Americans get care from our medical system that is not as high quality as we have a right to expect because of high costs,” McDonough says.
The ACA established a number of initiatives to address this fact, including creating Accountable Care Organizations (ACOs), providing bundled payment plans, and imposing penalties on hospitals with very high rates of readmissions and hospital-acquired infections.
These types of efforts, which are part of a broader push to transform the health care delivery system to ensure a greater focus on value, are receiving widespread support from both Republicans and Democrats, which means that they should continue, and even grow, under any new health care law, McDonough stresses.
“There seems to be a growing sense in the health care community that [the move to value-based payment and population health management] pushed forward under ACA should continue and expand,” McDonough says, adding that this is one piece of good news in the sea of uncertainty that exists.
Preparing for New Developments:
Ashish Jha, MD, MPH, Professor of International Health and Health Policy at the Harvard T.H. Chan School of Public Health, Director of the Harvard Global Health Institute, and a practicing general internist at the VA, agrees with this assessment. “The journey we began with ACA to move to value-based health care is going to continue,” he says. “But what form it will take, how we will do it, and how much is voluntary verses mandatory” remain to be seen moving forward.
He points out that this means that professionals need to know the range of options in order to be prepared for whatever way the field goes. “They need to ask, ‘What is the range and how do I prepare, so I will be in good shape?’’’ he explains.
Trends to Watch:
Jha, who is also faculty on Preparing for What’s Next in U.S. Health Reform, points to a number of other changes also started under the ACA that, regardless of the final health plan passed, will continue to affect organizations over the next few years.
For instance, people today are responsible for a growing portion of their own health care costs. This changes the way that organizations collect their money, meaning organizations need to find new ways of operating.
There will be many moral and ethical dilemmas for organizations as access shrinks and many patients lose coverage under the new plan. “I think health care leaders are very used to a world where they provide services to patients and get paid by insurers, or the government/Medicare or Medicaid. But now they’re waking up to a new model where they are getting a larger chunk from patients. They’re not used to collecting money from patients themselves and that will change their relationships,” Jha says.
With customers footing more of the bill, they now have higher expectations from providers. “The customer is changing, and what will customers want in return now that they’re writing the check? That becomes a really important issue for providers to focus on. It’s part of patient-centered care. Now patients are in the driver’s seat,” he stresses.
Another issue worth paying attention to on the value side of the equation is that participation in some Medicare bundled payment programs will be voluntary for now, but is ultimately expected to become mandatory in the not-too-distant future. This raises some interesting questions for organizations, as they grapple with whether to use the voluntary program to get acclimated. Organizations that don’t participate now could end up having a lot of catching up to do in the future, which could “have very serious consequences three to five years down the road,” Jha says.
Issues to Watch:
On the access side of things, Jha points out that there will also be many moral and ethical dilemmas for organizations as access shrinks and many patients lose coverage under the new plan.
Five years ago, many people were uninsured and had no contact with the health care system. “Now, these people have been covered and have become part of the organizations [that serve them]. They have developed relationships with their doctors, so it’s a big difference now when they lose coverage,” he says. “Are organizations really going to walk away from these patients? [And if not], how will health systems manage the financial debt they will incur to care for the uninsured?”
Another important trend that will impact many health organizations moving forward revolves around consolidation. “Doctors are being bought out by big hospitals. We have no idea how the Trump Administration will feel about that. Consolidation is a strategy that provider organizations have used to survive, getting bigger. But that gravy train for providers is coming to an end. Now, with more people uninsured, and more focus on value, there are broader market issues around consolidation and integration that will be challenging for providers,” Jha says.
Other Trends Worth Following:
Other trends that will continue to impact organizations include the growing push for providers to use interconnected Electronic Health Records (EHR). This is an important tool to help track and achieve key benchmarks of value-based care and improve coordination among providers for increased efficiency and better outcomes.
“While everyone thinks this is a good thing, and most organizations have made the leap into EHRs, people, especially frontline doctors and nurses, are very frustrated with these systems. How organizations will manage the transition between simply adopting the EHR and using it in ways that lead to meaningfully better care is the challenge ahead,” Jha says.
In addition, Jha says that the Trump Administration’s tougher restrictions on immigration may have a real effect on health systems that needs to be addressed up front. “Twenty-five percent of doctors in our country are foreign medical graduates, as are a large population of our nurses and other health professionals,” he says.
“As immigration gets tighter, there’s a question as to whether we will have a harder time attracting the best and brightest in the world. So health care will have a hard time building their ranks” in the future. With an aging population, this means that health systems may have challenges creating a good workforce to care for them.
The Importance of Staying Up-to-Date:
With so many fluctuations expected in how the health care system will do business in the coming months and years, both Jha and McDonough say that it is crucial for health care leaders to stay abreast of the latest developments as they progress.
One of the most important things is for health care leaders to stay in touch with what is happening out there and pay attention to the coverage in the media. “One of the most important things is for health care leaders to stay in touch with what is happening out there and pay attention to the coverage in the media,” McDonough says. “If you work in a hospital, [you will need to] follow the national organizations, such as the American Hospital Association, and stay alert to the opinions of experts as to what might happen,” he says.
But that alone will not be enough, says Jha. Understanding the nuances of policy changes will be critical for leaders to stay on top of the shifting requirements—and opportunities—that exist in the current environment so they can strategically position their organizations for success.
Harvard T.H. Chan School of Public Health offers Preparing for What’s Next in U.S. Health Reform, which offers key lessons involving health reform from the nation’s leading policy experts under the new federal administration. To learn more about this opportunity, click here.
[End of Article]
___________________________________________________________________________
Healthcare reform in the United States has a long history. Reforms have often been proposed but have rarely been accomplished.
In 2010, landmark reform was passed through two federal statutes enacted in 2010: the Patient Protection and Affordable Care Act (PPACA), signed March 23, 2010, and the Health Care and Education Reconciliation Act of 2010 (H.R. 4872), which amended the PPACA and became law on March 30, 2010.
Future reforms of the American health care system continue to be proposed, with notable proposals including a single-payer system and a reduction in fee-for-service medical care. The PPACA includes a new agency, the Center for Medicare and Medicaid Innovation (CMS Innovation Center), which is intended to research reform ideas through pilot projects.
History of national reform efforts:
Main article: History of health care reform in the United States
Motivation:
Main article: Healthcare reform debate in the United States
International comparisons of healthcare have found that the United States spends more per-capita than other similarly developed nations but falls below similar countries in various health metrics, suggesting inefficiency and waste.
In addition, the United States has significant underinsurance and significant impending unfunded liabilities from its aging demographic and its social insurance programs Medicare and Medicaid (Medicaid provides free long-term care to the elderly poor). The fiscal and human impact of these issues have motivated reform proposals.
U.S. healthcare costs were approximately $3.2 trillion or nearly $10,000 per person on average in 2015. Major categories of expense include hospital care (32%), physician and clinical services (20%), and prescription drugs (10%). U.S. costs in 2016 were substantially higher than other OECD countries, at 17.2% GDP versus 12.4% GDP for the next most expensive country (Switzerland). For scale, a 5% GDP difference represents about $1 trillion or $3,000 per person.
Some of the many reasons cited for the cost differential with other countries include: Higher administrative costs of a private system with multiple payment processes; higher costs for the same products and services; more expensive volume/mix of services with higher usage of more expensive specialists; aggressive treatment of very sick elderly versus palliative care; less use of government intervention in pricing; and higher income levels driving greater demand for healthcare. Healthcare costs are a fundamental driver of health insurance costs, which leads to coverage affordability challenges for millions of families.
There is ongoing debate whether the current law (ACA/Obamacare) and the Republican alternatives (AHCA and BCRA) do enough to address the cost challenge.
According to 2009 World Bank statistics, the U.S. had the highest health care costs relative to the size of the economy (GDP) in the world, even though estimated 50 million citizens (approximately 16% of the September 2011 estimated population of 312 million) lacked insurance. In March 2010, billionaire Warren Buffett commented that the high costs paid by U.S. companies for their employees' health care put them at a competitive disadvantage.
Life expectancy compared to healthcare spending from 1970 to 2008, in the US and the next 19 most wealthy countries by total GDP. Further, an estimated 77 million Baby Boomers are reaching retirement age, which combined with significant annual increases in healthcare costs per person will place enormous budgetary strain on U.S. state and federal governments, particularly through Medicare and Medicaid spending (Medicaid provides long-term care for the elderly poor). Maintaining the long-term fiscal health of the U.S. federal government is significantly dependent on healthcare costs being controlled.
Insurance cost and availability:
Further information: Health insurance coverage in the United States
In addition, the number of employers who offer health insurance has declined and costs for employer-paid health insurance are rising: from 2001 to 2007, premiums for family coverage increased 78%, while wages rose 19% and prices rose 17%, according to the Kaiser Family Foundation.
Even for those who are employed, the private insurance in the US varies greatly in its coverage; one study by the Commonwealth Fund published in Health Affairs estimated that 16 million U.S. adults were underinsured in 2003. The underinsured were significantly more likely than those with adequate insurance to forgo health care, report financial stress because of medical bills, and experience coverage gaps for such items as prescription drugs.
The study found that underinsurance disproportionately affects those with lower incomes—73% of the underinsured in the study population had annual incomes below 200% of the federal poverty level.
However, a study published by the Kaiser Family Foundation in 2008 found that the typical large employer preferred provider organization (PPO) plan in 2007 was more generous than either Medicare or the Federal Employees Health Benefits Program Standard Option.
One indicator of the consequences of Americans' inconsistent health care coverage is a study in Health Affairs that concluded that half of personal bankruptcys involved medical bills, although other sources dispute this.
There are health losses from insufficient health insurance. A 2009 Harvard study published in the American Journal of Public Health found more than 44,800 excess deaths annually in the United States due to Americans lacking health insurance.
More broadly, estimates of the total number of people in the United States, whether insured or uninsured, who die because of lack of medical care were estimated in a 1997 analysis to be nearly 100,000 per year. A study of the effects of the Massachusetts universal health care law (which took effect in 2006) found a 3% drop in mortality among people 20–64 years old—1 death per 830 people with insurance.
Other studies, just as those examining the randomized distribution of Medicaid insurance to low-income people in Oregon in 2008, found no change in death rate.
The cost of insurance has been a primary motivation in the reform of the US healthcare system, and many different explanations have been proposed in the reasons for high insurance costs and how to remedy them. One critique and motivation for healthcare reform has been the development of the medical–industrial complex. This relates to moral arguments for health care reform, framing healthcare as a social good, one that is fundamentally immoral to deny to people based on economic status.
The motivation behind healthcare reform in response to the medical-industrial complex also stems from issues of social inequity, promotion of medicine over preventative care. The medical-industrial complex, defined as a network of health insurance companies, pharmaceutical companies, and the like, plays a role in the complexity of the US insurance market and a fine line between government and industry within it.
Likewise, critiques of insurance markets being conducted under a capitalistic, free-market model also include that medical solutions, as opposed to preventative healthcare measures, are promoted to maintain this medical-industrial complex. Arguments for a market-based approach to health insurance include the Grossman model, which is based on an ideal competitive model, but others have critiqued this, arguing that fundamentally, this means that people in higher socioeconomic levels will receive a better quality of healthcare.
Uninsured rate:
With the implementation of the ACA, the level of uninsured rates severely decreased in the U.S. . This is due to the expansion of qualifications for access to medicaid, subsidizing insurance, prevention of insurance companies from underwriting, as well as enforcing the individual mandate which requires citizens to purchase health insurance or pay a fee.
In a research study which was conducted comparing the effects of the ACA before and after it was fully implemented in 2014, it was discovered that racial and ethnic minorities benefited more than whites with many gaining insurance coverage which they lacked before allowing for many to seek treatment improving their overall health.
In June 2014, Gallup–Healthways Well–Being conducted a survey and found that the uninsured rate is decreasing with 13 percent of U.S. adults uninsured in 2014 compared to 17 percent in January 2014 and translates to roughly 10 million to 11 million individuals who gained coverage.
The survey also looked at the major demographic groups and found each is making progress towards getting health insurance. However, Hispanics, who have the highest uninsured rate of any racial or ethnic group, are lagging in their progress. Under the new health care reform, Latinos were expected to be major beneficiaries of the new health care law. Gallup found that the biggest drop in the uninsured rate (3 percentage points) was among households making less than $36,000 a year.
Waste and fraud:
In December 2011 the outgoing Administrator of the Centers for Medicare & Medicaid Services, Donald Berwick, asserted that 20% to 30% of health care spending is waste. He listed five causes for the waste: (1) overtreatment of patients, (2) the failure to coordinate care, (3) the administrative complexity of the health care system, (4) burdensome rules and (5) fraud.
An estimated 3–10% of all health care expenditures in the U.S. are fraudulent. In 2011, Medicare and Medicaid made $65 billion in improper payments (including both error and fraud). Government efforts to reduce fraud include $4 billion in fraudulent payments recovered by the Department of Justice and the FBI in 2012, longer jail sentences specified by the Affordable Care Act, and Senior Medicare Patrols—volunteers trained to identify and report fraud.
In 2007, the Department of Justice and Health and Human Services formed the Medicare Fraud Strike Force to combat fraud through data analysis and increased community policing.
As of May 2013, the Strike Force has charged more than 1,500 people for false billings of more than $5 billion. Medicare fraud often takes the form of kickbacks and money-laundering. Fraud schemes often take the form of billing for medically unnecessary services or services not rendered.
Quality of care:
There is significant debate regarding the quality of the U.S. healthcare system relative to those of other countries. Although there are advancements in the quality of care in America due to the acknowledgement of various health related topics such as how insurance plans are now mandated to include coverage for those with mental health and substance abuse disorders as well with the inability to deny a person who has preexisting conditions through the ACA, there is still much that needs to be improved.
Within the U.S., those who are a racial/ethnic minority along with those who poses a lower income have higher chances of experiencing a lower quality of care at higher cost. Despite the advancements with the ACA, this may discourage a person from seeking medical treatment.
Physicians for a National Health Program, a pro-universal single-payer system of health care advocacy group, has claimed that a free market solution to health care provides a lower quality of care, with higher mortality rates, than publicly funded systems. The quality of health maintenance organizations and managed care have also been criticized by this same group.
According to a 2000 study of the World Health Organization, publicly funded systems of industrial nations spend less on health care, both as a percentage of their GDP and per capita, and enjoy superior population-based health care outcomes.
However, conservative commentator David Gratzer and the Cato Institute, a libertarian think tank, have both criticized the WHO's comparison method for being biased; the WHO study marked down countries for having private or fee-paying health treatment and rated countries by comparison to their expected health care performance, rather than objectively comparing quality of care.
Some medical researchers say that patient satisfaction surveys are a poor way to evaluate medical care. Researchers at the RAND Corporation and the Department of Veterans Affairs asked 236 elderly patients in two different managed care plans to rate their care, then examined care in medical records, as reported in Annals of Internal Medicine. There was no correlation. "Patient ratings of health care are easy to obtain and report, but do not accurately measure the technical quality of medical care," said John T. Chang, UCLA, lead author.
Public opinion:
Public opinion polls have shown a majority of the public supports various levels of government involvement in health care in the United States, with stated preferences depending on how the question is asked.
Polls from Harvard University in 1988, the Los Angeles Times in 1990, and the Wall Street Journal in 1991 all showed strong support for a health care system compared to the system in Canada.
More recently, however, polling support has declined for that sort of health care system, with a 2007 Yahoo/AP poll showing 54% of respondents considered themselves supporters of "single-payer health care," a majority in favor of a number of reforms according to a joint poll with the Los Angeles Times and Bloomberg, and a plurality of respondents in a 2009 poll for Time Magazine showed support for "a national single-payer plan similar to Medicare for all."
Polls by Rasmussen Reports in 2011 and 2012 showed pluralities opposed to single-payer health care. Many other polls show support for various levels of government involvement in health care, including polls from New York Times/CBS News and Washington Post/ABC News, showing favorability for a form of national health insurance.
The Kaiser Family Foundation showed 58% in favor of a national health plan such as Medicare-for-all in 2009, with support around the same level from 2017 to April 2019, when 56% said they supported it. A Quinnipiac poll in three states in 2008 found majority support for the government ensuring "that everyone in the United States has adequate health-care" among likely Democratic primary voters.
A 2001 article in the public health journal Health Affairs studied fifty years of American public opinion of various health care plans and concluded that, while there appears to be general support of a "national health care plan," poll respondents "remain satisfied with their current medical arrangements, do not trust the federal government to do what is right, and do not favor a single-payer type of national health plan."
Politifact rated a 2009 statement by Michael Moore "false" when he stated that "[t]he majority actually want single-payer health care." According to Politifact, responses on these polls largely depend on the wording. For example, people respond more favorably when they are asked if they want a system "like Medicare".
Alternatives and research directions:
There are alternatives to the exchange-based market system which was enacted by the Patient Protection and Affordable Care Act which have been proposed in the past and continue to be proposed, such as a single-payer system and allowing health insurance to be regulated at the federal level.
In addition, the Patient Protection and Affordable Health Care Act of 2010 contained provisions which allows the Centers for Medicare and Medicaid Services (CMS) to undertake pilot projects which, if they are successful could be implemented in future.
Single-payer health care:
Further information: Single-payer healthcare § United States
A number of proposals have been made for a universal single-payer healthcare system in the United States, most recently the United States National Health Care Act, (popularly known as H.R. 676 or "Medicare for All") but none have achieved more political support than 20% congressional co-sponsorship.
Advocates argue that preventative health care expenditures can save several hundreds of billions of dollars per year because publicly funded universal health care would benefit employers and consumers, that employers would benefit from a bigger pool of potential customers and that employers would likely pay less, and would be spared administrative costs of health care benefits.
It is also argued that inequities between employers would be reduced. Also, for example, cancer patients are more likely to be diagnosed at Stage I where curative treatment is typically a few outpatient visits, instead of at Stage III or later in an emergency room where treatment can involve years of hospitalization and is often terminal.
Others have estimated a long-term savings amounting to 40% of all national health expenditures due to preventative health care, although estimates from the Congressional Budget Office and The New England Journal of Medicine have found that preventative care is more expensive.
Any national system would be paid for in part through taxes replacing insurance premiums, but advocates also believe savings would be realized through preventative care and the elimination of insurance company overhead and hospital billing costs. An analysis of a single-payer bill by the Physicians for a National Health Program estimated the immediate savings at $350 billion per year.
The Commonwealth Fund believes that, if the United States adopted a universal health care system, the mortality rate would improve and the country would save approximately $570 billion a year.
Recent enactments of single-payer systems within individual states, such as in Vermont in 2011, may serve as living models supporting federal single-payer coverage. The plan in Vermont, however, has failed.
On June 1, 2017, in light of the recent Trump Administration’s efforts to repeal the Affordable Care Act, California Democratic Senator Ricardo Lara proposed a bill to establish single-payer healthcare within the state of California (SB 562), calling on fellow senators to act quickly in defense of healthcare.
The legislation would implement “Medicare for All,” placing all levels of healthcare in the hands of the state. The bill proposed to the California Senate by Senator Lara lacked a method of funding required to finance the $400 billion-dollar policy. Despite this lack of foresight, the bill gained approval from the senate and will move on to await approval by the state assembly.
In wake of the Affordable Care Act, the state of California has experienced the greatest rise in newly insured people compared to other states. Subsequently, the number of physicians under MediCal are not enough to meet the demand, therefore 25% of physicians care for 80% of patients who are covered through MediCal.
In the past, California has struggled to maintain healthcare effectiveness, due in part to its unstable budget and complex regulations. The state has a policy in place known as the Gann Limit, otherwise entitled proposition 98, which ensures that a portion of state funds are directed towards the education system.
This limit would be exceeded if California raises taxes to fund the new system which would require $100 billion in tax revenue. In order to avoid legal dispute, voters would be required to amend proposition 98 and exempt healthcare funding from required educational contributions.
The state announced on August 1, 2017 that coverage for health insurance will increase by 12.5% in next year, threatening the coverage of 1.5 million people.
Public option:
Main article: Public health insurance option
In January 2013, Representative Jan Schakowsky and 44 other U.S. House of Representatives Democrats introduced H.R. 261, the "Public Option Deficit Reduction Act" which would amend the 2010 Affordable Care Act to create a public option. The bill would set up a government-run health insurance plan with premiums 5% to 7% percent lower than private insurance. The Congressional Budget Office estimated it would reduce the United States public debt by $104 billion over 10 years.
Balancing doctor supply and demand:
The Medicare Graduate Medical Education program regulates the supply of medical doctors in the U.S. By adjusting the reimbursement rates to establish more income equality among the medical professions, the effective cost of medical care can be lowered.
Bundled payments:
A key project is one that could radically change the way the medical profession is paid for services under Medicare and Medicaid. The current system, which is also the prime system used by medical insurers is known as fee-for-service because the medical practitioner is paid only for the performance of medical procedures which, it is argued means that doctors have a financial incentive to do more tests (which generates more income) which may not be in the patients' best long-term interest.
The current system encourages medical interventions such as surgeries and prescribed medicines (all of which carry some risk for the patient but increase revenues for the medical care industry) and does not reward other activities such as encouraging behavioral changes such as modifying dietary habits and quitting smoking, or follow-ups regarding prescribed regimes which could have better outcomes for the patient at a lower cost.
The current fee-for-service system also rewards bad hospitals for bad service. Some have noted that the best hospitals have fewer re-admission rates than others, which benefits patients, but some of the worst hospitals have high re-admission rates which is bad for patients but is perversely rewarded under the fee-for-service system.
Projects at CMS are examining the possibility of rewarding health care providers through a process known as "bundled payments" by which local doctors and hospitals in an area would be paid not on a fee for service basis but on a capitation system linked to outcomes.
The areas with the best outcomes would get more. This system, it is argued, makes medical practitioners much more concerned to focus on activities that deliver real health benefits at a lower cost to the system by removing the perversities inherent in the fee-for-service system.
Though aimed as a model for health care funded by CMS, if the project is successful it is thought that the model could be followed by the commercial health insurance industry also.
Centers for Medicare and Medicaid Innovation. With the ACA improving the health of many by increasing the number of people who are insured, this is not the final stage for the ACA due to the push for a medicaid expansion reform.
With the Democrats supporting the expansion and the Republicans against it, it was denied in the Supreme Court in the trial of NFIB vs Sebelius. The Court ruled that implementing taxes in order to pay for health insurance for all citizens was an unconstitutional exercise of Congress’s power under Article I.
If the expansion eventually succeeds, Medicaid would become a fully federal program with new federal eligibility standards. This would alleviate the responsibility of state governments to fund Medicaid.
In addition to the reform for the medicaid expansion, there are additional reforms focused on addressing social determinants in the healthcare system through various programs and initiatives in order to reduce healthcare expenditures and improve health outcomes.
Programs and initiatives recognizing and addressing non-medical social needs have sprung from various sectors within healthcare, with emerging efforts made by multi-payer federal and state initiatives, medicaid initiatives led by states, or by health plans, as well as provider level actions.State and federal initiatives, primarily sponsored CMMI (Center for Medicare and Medicaid Innovation) a division of CMS, seek to address basic social needs within the context of the healthcare delivery system.
CMMI initiatives like the 2016 "Accountable Health Communities" (AHC) model have been created to focus on connecting Medicare and Medicaid beneficiaries with community services to address health-related social needs, while providing funds to organizations so that they can systematically identify and address the health-related social needs of Medicare and Medicaid recipients through screening, referral, and community navigation services.
The model was officially implemented in 2017 and will be evaluated for its ability to affect cost of healthcare spending and reduce inpatient/outpatient utilization in 2022. Under the AHC model, funds have been allocated towards developing a 10-item screening tool to identify 5 different patient need domains that can be addressed through community resources (housing instability, food insecurity, transportation difficulties, utility assistance needs, and interpersonal safety).
Increasing bodies of evidence suggest that addressing social needs can help stop their damaging health effects, but screening for social needs is not yet standard clinical practice. Applying this tool in the AHC model will help CMS evaluate the impact of local partnerships between healthcare providers and community organizations in advancing the aims of addressing the cost and quality of health care across all settings.
National recommendations around multi-dimension screening for social risk are not yet available since the evidence base to support such recommendations is highly under-developed at present.
More research is still needed in this area to be able to demonstrate whether screening for social risk, and especially for multiple domains of social risk, will succeed in meeting the Wilson and Jungner screening criteria.
Health plan specific initiatives:
Due to how new CMMI initiatives are, evidence supporting the effectiveness of its various initiatives of reducing healthcare spending and improving health outcomes of patients is relatively small, but is expected to grow within the coming years as many of CMMI's programs and initiatives will be due for their programmatic performance evaluation.
However, it remains that there is more evidence of smaller scale initiatives in individual health plans/hospitals/clinics, as several health plans, hospitals, and clinics have sought out to address social determinants of health within their scope of care.
Transportation:
Transportation is a key social determinant impacting patient outcomes with approximately 3.6 million individuals unable to receive the necessary medical care due to transportation barrier, according to recent study.
In addition, these 3.6 million experience multiple conditions at a much higher rate than those who have stable access to transportation. Many conditions that they face, however, can be managed if appropriate care is made available.
For some conditions, this care is cost-effective and results in health care cost savings that outweigh added transportation costs. without access to reliable, affordable, and convenient transportation, patients miss appointments and end up costing clinics money.
According to a cross-study analysis, missed appointments and care delays cost the healthcare industry $150 billion each year. Patients without transportation are also less likely to take medications as directed. One study found that 65 percent of patients felt transportation assistance would enable them to fill prescriptions as directed after discharge.
According to a recent article published in the Journal of the American Medical Association, ride-sharing services such as Lyft and Uber can improve that healthcare disparity and cut down on the $2.7 million the federal government spends each year on non-emergency medical transportation services.
To recover revenue and improve care quality, some health systems like MedStar Health and Denver Health Medical Center are teaming up with Uber, Lyft, and other ride-sharing companies to connect patients with transportation.
Housing:
The University of Illinois Hospital, part of the University of Illinois Hospital & Health Sciences System, identified that large portion of the individuals with high rates of emergency department were also chronically homeless, and that these individuals were in the 10th decile for patient cost, with annual per patient expenses ranging from $51,000 to $533,000.
The University of Illinois partnered with a community group called the Center for Housing and Health to initiate the Better Health Through Housing initiative in 2015, an initiative that connected chronically homeless individuals with transitional housing and case managers. In partnering with the Center for Housing and Health, the University of Illinois Hospital saw participant healthcare costs fall 42 percent, and more recent studies have found that costs dropped by 61 percent. The hospital's emergency department reported a 35% reduction in use.
Malnutrition:
Some health plans have chosen to address some SDOH within their own means by establishing programs that directly deal with a single risk factor. Studies show that malnutrition can lead to higher costs of care and extended hospital states with the average hospital stay costing nearly $2,000 per day.
Advocate Health Care, an accountable care organization in Chicago, Illinois, implemented a nutrition care program at four of its Chicago area hospitals, an initiative that resulted in more than $4.8 million in cost savings within 6 months due to shorter hospital states and lower readmission rates (reduced 30 day readmission rates by 27% and the average hospital stay by nearly two days).
Trump administration efforts:
Donald Trump was elected president on a platform that included a pledge to "repeal and replace" the Patient Protection and Affordable Care Act (commonly called the Affordable Care Act or Obamacare). Rather than making adjustments to the Affordable Care Act, President Trump is proposing the American Health Care Act (AHCA), which was developed by the House of Representatives.
If passed, this new health care act would cause insurance and healthcare to return to the market potentially causing for 18 million Americans to become uninsured.
In addition to this, President Trump is pushing for a change in policies regarding "public charge" which would cause the public benefits such as health, nutrition, and housing programs that were previously excluded to count towards considering a person a public charge.
By doing this, immigrants who use these resources would have their ability to obtain legal permanent resident status affected increasing their chance of being denied citizenship.
The administration has suggested that the AHCA is only part of its reform efforts. Other proposals include allowing interstate competition in the health insurance market.
Incentivizing health reimbursement arrangements is another goal.
See also:
- Comparison of the healthcare systems in Canada and the United States
- Health care reform
- Health care reforms proposed during the Obama administration
- Health care system § International comparisons
- Health economics
- Health policy
- List of healthcare reform advocacy groups in the United States
- McCarran–Ferguson Act
- Medicare Sustainable Growth Rate
- Healthcare reform in the United States at Curlie
Vital Signs
- YouTube Video: Blood Pressure: How High is Too High and How Do I Lower it Safely?
- YouTube Video: How to: Measure Resting Heart Rate
- YouTube Video: How to Take a Temperature: Under Arm, Oral, Ear, Rectum, Skin, Temporal
Vital signs (also known as vitals) are a group of the four to six most important medical signs that indicate the status of the body’s vital (life-sustaining) functions. These measurements are taken to help assess the general physical health of a person, give clues to possible diseases, and show progress toward recovery.
The normal ranges for a person’s vital signs vary with age, weight, gender, and overall health.
There are four primary vital signs:
The above are often notated as BT, BP, HR, and RR.
However, depending on the clinical setting, the vital signs may include other measurements called the "fifth vital sign" or "sixth vital sign". Vital signs are recorded using the LOINC internationally accepted standard coding system.
Early warning scores have been proposed that combine the individual values of vital signs into a single score. This was done in recognition that deteriorating vital signs often precede cardiac arrest and/or admission to the intensive care unit. Used appropriately, a rapid response team can assess and treat a deteriorating patient and prevent adverse outcomes
Primary vital signs:
There are four primary vital signs which are standard in most medical settings:
The equipment needed is a thermometer, a sphygmomanometer, and a watch. Although a pulse can be taken by hand, a stethoscope may be required for a patient with a very weak pulse.
Temperature:
Temperature recording gives an indication of core body temperature which is normally tightly controlled (thermoregulation) as it affects the rate of chemical reactions.
Body temperature is maintained through a balance of the heat produced by the body and the heat lost from the body.
Temperature can be recorded in order to establish a baseline for the individual's normal body temperature for the site and measuring conditions.
Temperature can be measured from the mouth, rectum, axilla (armpit), ear, or skin. Oral, rectal, and axillary temperature can be measured with either a glass or electronic thermometer.
Note that rectal temperature measures approximately 1°F greater than oral temperature, and axillary temperature measures about 1°F less than oral temperature. Aural and skin temperature measurements require special devices designed to measure temperature from these locations.
While 98.6 °F/ 37°C is considered "normal" body temperature, there is some variance between individuals. Most have a normal body temperature set point that falls within the range of 36.0°C to 37.5°C (96.5–99.5°F).
The main reason for checking body temperature is to solicit any signs of systemic infection or inflammation in the presence of a fever. Fever is considered oral temperature of >99.5°F or rectal temperature of >100.5°F. Other causes of elevated temperature include hyperthermia, which results from unregulated heat generation or abnormalities in the body's heat exchange mechanisms.
Temperature depression (hypothermia) also needs to be evaluated. Hypothermia is classified as temperature below 35 °C/95 °F .
It is also recommended to review the trend of the patient's temperature over time. A fever of 38 °C does not necessarily indicate an ominous sign if the patient's previous temperature has been higher.
Pulse:
Main article: Pulse
The pulse is the rate at which the heart beats while pumping blood through the arteries, recorded as beats per minute (bpm). It may also be called "heart rate". In addition to providing the heart rate, the pulse should also be evaluated for strength and obvious rhythm abnormalities.
The pulse is commonly taken at the wrist (radial artery). Alternative sites include the elbow (brachial artery), the neck (carotid artery), behind the knee (popliteal artery), or in the foot (dorsalis pedis or posterior tibial arteries). The pulse is taken with the index finger and middle finger by pushing with firm yet gentle pressure at the locations described above, and counting the beats felt per 60 seconds (or per 30 seconds and multiplying by two).
The pulse rate can also be measured by listening directly to the heartbeat using a stethoscope. The pulse may vary due to exercise, fitness level, disease, emotions, and medications.
The pulse also varies with age:
Respiratory rate:
Main article: Respiratory rate
Average respiratory rates vary between ages, but the normal reference range for people age 18 to 65 is 16–20 breaths per minute. The value of respiratory rate as an indicator of potential respiratory dysfunction has been investigated but findings suggest it is of limited value. Respiratory rate is a clear indicator of acidotic states, as the main function of respiration is removal of CO2 leaving bicarbonate base in circulation.
Blood pressure:
Main article: Blood pressure § Measurement
Blood pressure is recorded as two readings: a higher systolic pressure, which occurs during the maximal contraction of the heart, and the lower diastolic or resting pressure.
In adults, a normal blood pressure is 120/80, with 120 being the systolic and 80 being the diastolic reading. Usually, the blood pressure is read from the left arm unless there is some damage to the arm. The difference between the systolic and diastolic pressure is called the pulse pressure.
The measurement of these pressures is now usually done with an aneroid or electronic sphygmomanometer. The classic measurement device is a mercury sphygmomanometer, using a column of mercury measured off in millimeters.
In the United States and UK, the common form is millimeters of mercury, while elsewhere SI units of pressure are used. There is no natural 'normal' value for blood pressure, but rather a range of values that on increasing are associated with increased risks. The guideline acceptable reading also takes into account other co-factors for disease.
Therefore, elevated blood pressure (hypertension) is variously defined when the systolic number is persistently over 140–160 mmHg. Low blood pressure is hypotension. Blood pressures are also taken at other portions of the extremities. These pressures are called segmental blood pressures and are used to evaluate blockage or arterial occlusion in a limb (see Ankle brachial pressure index).
Other signs:
In the U.S., in addition to the above four, many providers are required or encouraged by government technology-in-medicine laws to record the patient's height, weight, and body mass index.
In contrast to the traditional vital signs, these measurements are not useful for assessing acute changes in state because of the rate at which they change; however, they are useful for assessing the impact of prolonged illness or chronic health problems.
The definition of vital signs may also vary with the setting of the assessment. Emergency medical technicians (EMTs), in particular, are taught to measure the vital signs of respiration, pulse, skin, pupils, and blood pressure as "the 5 vital signs" in a non-hospital setting.
Fifth vital signs:
The "fifth vital sign" may refer to a few different parameters.
Sixth vital signs:
There is no standard "sixth vital sign"; its use is more informal and discipline-dependent.
Click on any of the following blue hyperlinks for more about Vital Signs:
The normal ranges for a person’s vital signs vary with age, weight, gender, and overall health.
There are four primary vital signs:
- body temperature,
- blood pressure,
- pulse (heart rate),
- and breathing rate (respiratory rate),
The above are often notated as BT, BP, HR, and RR.
However, depending on the clinical setting, the vital signs may include other measurements called the "fifth vital sign" or "sixth vital sign". Vital signs are recorded using the LOINC internationally accepted standard coding system.
Early warning scores have been proposed that combine the individual values of vital signs into a single score. This was done in recognition that deteriorating vital signs often precede cardiac arrest and/or admission to the intensive care unit. Used appropriately, a rapid response team can assess and treat a deteriorating patient and prevent adverse outcomes
Primary vital signs:
There are four primary vital signs which are standard in most medical settings:
The equipment needed is a thermometer, a sphygmomanometer, and a watch. Although a pulse can be taken by hand, a stethoscope may be required for a patient with a very weak pulse.
Temperature:
Temperature recording gives an indication of core body temperature which is normally tightly controlled (thermoregulation) as it affects the rate of chemical reactions.
Body temperature is maintained through a balance of the heat produced by the body and the heat lost from the body.
Temperature can be recorded in order to establish a baseline for the individual's normal body temperature for the site and measuring conditions.
Temperature can be measured from the mouth, rectum, axilla (armpit), ear, or skin. Oral, rectal, and axillary temperature can be measured with either a glass or electronic thermometer.
Note that rectal temperature measures approximately 1°F greater than oral temperature, and axillary temperature measures about 1°F less than oral temperature. Aural and skin temperature measurements require special devices designed to measure temperature from these locations.
While 98.6 °F/ 37°C is considered "normal" body temperature, there is some variance between individuals. Most have a normal body temperature set point that falls within the range of 36.0°C to 37.5°C (96.5–99.5°F).
The main reason for checking body temperature is to solicit any signs of systemic infection or inflammation in the presence of a fever. Fever is considered oral temperature of >99.5°F or rectal temperature of >100.5°F. Other causes of elevated temperature include hyperthermia, which results from unregulated heat generation or abnormalities in the body's heat exchange mechanisms.
Temperature depression (hypothermia) also needs to be evaluated. Hypothermia is classified as temperature below 35 °C/95 °F .
It is also recommended to review the trend of the patient's temperature over time. A fever of 38 °C does not necessarily indicate an ominous sign if the patient's previous temperature has been higher.
Pulse:
Main article: Pulse
The pulse is the rate at which the heart beats while pumping blood through the arteries, recorded as beats per minute (bpm). It may also be called "heart rate". In addition to providing the heart rate, the pulse should also be evaluated for strength and obvious rhythm abnormalities.
The pulse is commonly taken at the wrist (radial artery). Alternative sites include the elbow (brachial artery), the neck (carotid artery), behind the knee (popliteal artery), or in the foot (dorsalis pedis or posterior tibial arteries). The pulse is taken with the index finger and middle finger by pushing with firm yet gentle pressure at the locations described above, and counting the beats felt per 60 seconds (or per 30 seconds and multiplying by two).
The pulse rate can also be measured by listening directly to the heartbeat using a stethoscope. The pulse may vary due to exercise, fitness level, disease, emotions, and medications.
The pulse also varies with age:
- A newborn can have a heart rate of 100-160 bpm,
- an infant (0-5 months old) a heart rate of 90–150 bpm,
- and a toddler (6-12 months old) a heart rate of 80–140 bpm.
- A child aged 1-3 years old can have a heart rate of 80-130 bpm,
- a child aged 3-5 years old a heart rate of 80-120 bpm,
- an older child (age of 6-10) a heart rate of 70-110 bpm,
- and an adolescent (age 11-14) a heart rate of 60–105 bpm.
- An adult (age 15+) can have a heart rate of 60–100 bpm.
Respiratory rate:
Main article: Respiratory rate
Average respiratory rates vary between ages, but the normal reference range for people age 18 to 65 is 16–20 breaths per minute. The value of respiratory rate as an indicator of potential respiratory dysfunction has been investigated but findings suggest it is of limited value. Respiratory rate is a clear indicator of acidotic states, as the main function of respiration is removal of CO2 leaving bicarbonate base in circulation.
Blood pressure:
Main article: Blood pressure § Measurement
Blood pressure is recorded as two readings: a higher systolic pressure, which occurs during the maximal contraction of the heart, and the lower diastolic or resting pressure.
In adults, a normal blood pressure is 120/80, with 120 being the systolic and 80 being the diastolic reading. Usually, the blood pressure is read from the left arm unless there is some damage to the arm. The difference between the systolic and diastolic pressure is called the pulse pressure.
The measurement of these pressures is now usually done with an aneroid or electronic sphygmomanometer. The classic measurement device is a mercury sphygmomanometer, using a column of mercury measured off in millimeters.
In the United States and UK, the common form is millimeters of mercury, while elsewhere SI units of pressure are used. There is no natural 'normal' value for blood pressure, but rather a range of values that on increasing are associated with increased risks. The guideline acceptable reading also takes into account other co-factors for disease.
Therefore, elevated blood pressure (hypertension) is variously defined when the systolic number is persistently over 140–160 mmHg. Low blood pressure is hypotension. Blood pressures are also taken at other portions of the extremities. These pressures are called segmental blood pressures and are used to evaluate blockage or arterial occlusion in a limb (see Ankle brachial pressure index).
Other signs:
In the U.S., in addition to the above four, many providers are required or encouraged by government technology-in-medicine laws to record the patient's height, weight, and body mass index.
In contrast to the traditional vital signs, these measurements are not useful for assessing acute changes in state because of the rate at which they change; however, they are useful for assessing the impact of prolonged illness or chronic health problems.
The definition of vital signs may also vary with the setting of the assessment. Emergency medical technicians (EMTs), in particular, are taught to measure the vital signs of respiration, pulse, skin, pupils, and blood pressure as "the 5 vital signs" in a non-hospital setting.
Fifth vital signs:
The "fifth vital sign" may refer to a few different parameters.
- Pain is considered a standard fifth vital sign in some organizations, such as the U.S. Veterans Affairs. Pain is measured on a 0-10 pain scale based on subjective patient reporting and may be unreliable. Some studies show that recording pain routinely may not change management.
- Menstrual cycle
- Oxygen saturation (as measured by pulse oximetry)
- Blood Glucose level.
Sixth vital signs:
There is no standard "sixth vital sign"; its use is more informal and discipline-dependent.
- End-tidal CO2.
- Functional status
- Shortness of breath
- Gait speed
- Delirium
Click on any of the following blue hyperlinks for more about Vital Signs:
Cardiopulmonary resuscitation (CPR) is an emergency procedure that combines chest compressions often with artificial ventilation in an effort to manually preserve intact brain function until further measures are taken to restore spontaneous blood circulation and breathing in a person who is in cardiac arrest.
It is recommended in those who are unresponsive with no breathing or abnormal breathing, for example, agonal respirations.
CPR involves chest compressions for adults between 5 cm (2.0 in) and 6 cm (2.4 in) deep and at a rate of at least 100 to 120 per minute.
The rescuer may also provide artificial ventilation by either exhaling air into the subject's mouth or nose (mouth-to-mouth resuscitation) or using a device that pushes air into the subject's lungs (mechanical ventilation).
Current recommendations place emphasis on early and high-quality chest compressions over artificial ventilation; a simplified CPR method involving chest compressions, is only recommended for untrained rescuers. In children, however, only doing compressions may result in worse outcomes, because in children the problem normally arises from a respiratory, rather than cardiac problem.
Chest compression to breathing ratios is set at 30 to 2 in adults.
CPR alone is unlikely to restart the heart. Its main purpose is to restore partial flow of oxygenated blood to the brain and heart. The objective is to delay tissue death and to extend the brief window of opportunity for a successful resuscitation without permanent brain damage.
Administration of an electric shock to the subject's heart, termed defibrillation, is usually needed in order to restore a viable or "perfusing" heart rhythm. Defibrillation is effective only for certain heart rhythms, namely ventricular fibrillation or pulseless ventricular tachycardia, rather than asystole or pulseless electrical activity.
Early shock when appropriate is recommended. CPR may succeed in inducing a heart rhythm that may be shockable. In general, CPR is continued until the person has a return of spontaneous circulation (ROSC) or is declared dead.
Click on any of the following blue hyperlinks for more about administering CPR:
It is recommended in those who are unresponsive with no breathing or abnormal breathing, for example, agonal respirations.
CPR involves chest compressions for adults between 5 cm (2.0 in) and 6 cm (2.4 in) deep and at a rate of at least 100 to 120 per minute.
The rescuer may also provide artificial ventilation by either exhaling air into the subject's mouth or nose (mouth-to-mouth resuscitation) or using a device that pushes air into the subject's lungs (mechanical ventilation).
Current recommendations place emphasis on early and high-quality chest compressions over artificial ventilation; a simplified CPR method involving chest compressions, is only recommended for untrained rescuers. In children, however, only doing compressions may result in worse outcomes, because in children the problem normally arises from a respiratory, rather than cardiac problem.
Chest compression to breathing ratios is set at 30 to 2 in adults.
CPR alone is unlikely to restart the heart. Its main purpose is to restore partial flow of oxygenated blood to the brain and heart. The objective is to delay tissue death and to extend the brief window of opportunity for a successful resuscitation without permanent brain damage.
Administration of an electric shock to the subject's heart, termed defibrillation, is usually needed in order to restore a viable or "perfusing" heart rhythm. Defibrillation is effective only for certain heart rhythms, namely ventricular fibrillation or pulseless ventricular tachycardia, rather than asystole or pulseless electrical activity.
Early shock when appropriate is recommended. CPR may succeed in inducing a heart rhythm that may be shockable. In general, CPR is continued until the person has a return of spontaneous circulation (ROSC) or is declared dead.
Click on any of the following blue hyperlinks for more about administering CPR:
- Medical uses
- Consequences
- Methods
- Pathophysiology
- Additional devices
- Prevalence
- Society and culture
- History
- Other animals
- Research
- See also:
- Slow code
- Lazarus syndrome, spontaneous auto-resuscitation where attempts at artificial resuscitation have failed
- Automated external defibrillator (AED)
- 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care
- ERC European Resuscitation Council
- CPR: NHS Choices
- How to resuscitate a child: NHS Choices
- 5 Components of High-Quality CPR: AED Philippines
Locating Health Information on the Internet Pictured below: Checklist of questions for evaluating Health Information found on the Internet (by the National Library of Medicine).
Health information on the Internet refers to all health-related information communicated through or available on the Internet.
Description:
The Internet is widely used by the general public as a tool for finding health information. In the late 1990s, researchers noted an increase in Internet users' access to health-related content despite the variation in the quality of information, level of accessibility, and overall health literacy. Access to health information does not guarantee understanding, as health literacy of individuals vary.
It is believed patients who know their medical history may learn and interpret this information in a way that benefits them. This, however, is not always the case because online health information is not always peer reviewed. Physicians worry that patients who conduct Internet research on their medical history are at a risk of being misinformed.
In 2013, the opinions about the relationship between health care providers and online health information were still being established. According to a 2014 study, "The flow of information has fundamentally changed, and physicians have less control over health information relayed to patients. Not surprisingly, this paradigm shift has elicited varied and sometimes conflicting views about the value of the Internet as a tool to improve health care."
Importance of the physician-patient relationship:
In cases in which a physician has difficulty explaining complicated medical concepts to a patient, that patient may be inclined to seek information on the internet. A consensus exists that patients should have shared decision making, meaning that patients should be able to make informed decisions about the direction of their medical treatment in collaboration with their physician. Rich, educated, and socially advantaged patients may enjoy the benefits of the shared decision-making approach more than those with a lower socioeconomic class or minority status.
Patients' naive understanding of their health contributes to a range of issues, including the tendency to deviate from the physician's medical advice or to miss medical appointments.
Patients with limited access to health information are more likely to use complementary and alternative medicine, and fail to inform their physician about it. Complementary and alternative medicine may not be evidence-based medicine.
While physicians can work on improving their doctor-patient communication skills, individuals can become more knowledgeable about their health through patient education programs. A study by Lorig in 2002 suggested healthcare processes can be efficiently improved with patients' behavior.
Social media:
Social forums in which anyone can have conversations about health with their peers exist; these are especially popular among patients who want to talk about shared medical concerns with others. Those who participate in online communities that discuss health issues report feeling relieved about their health worries, perceiving they have more control over their health and medical condition, gaining more medical knowledge, and having more personal agency overall.
Some research studies have failed to find evidence to validate the physicians' concerns about patients receiving misinformation online or using online health information to conduct self-diagnosis. Patients with chronic diseases who use the Internet to get health-related information often acquire good skills to judge the quality of information that they find.
Social media platforms are considered channels physicians can use to acquire insight on their patients' thoughts. Patients have increasingly turned to social media for health information, sometimes of dubious quality. Several studies have used social media to gather data on patients' adverse drug reactions (ADRs) with generally promising results.
Some commercial organizations use health information gathered from the Internet, raising serious ethical and privacy concerns, including the risk of accidental violations of the patient privacy by healthcare providers.
Academic medical literature:
The written record of peer-reviewed medical consensus is stored in scientific journals. There has been an academic journal publishing reform since the advent of electronic publishing.
Although some journals have adopted an open access template for online users, other journals are opposed to a widening of open access publishing. The open-access policy has significantly increased the accessibility of professional health information to researchers, physicians, and the public through the Internet. Some of the academic medical literature, however, may not be peer-reviewed and users are advised to exercise caution when reading health-related articles from such websites.
Quality:
The nature of health-related information available on the Internet is complex and its quality varies greatly by source. The standards for ensuring quality control on the Internet have been criticized and no single standard is universally accepted.
Many researchers have investigated this issue in detail, resulting in a wide range of theories from different disciplines.
Personal health information:
For many applications, people wish to use health information on the Internet to gain further insight about a personal health concern. Because of this, the goal is often to use the Internet to find information as it is described in a person's medical record. Since the advent of electronic media, medical records have been increasingly kept as electronic medical records.
More healthcare professionals rely on electronic medical records because it is a favorable means for patients to access their personal health information. These comprehensive systems allow patients to easily access their records without a doctor's visit, view interactive patient education materials, and use a greater range of health services such as renewing a medical prescription or making an appointment online.
All medical records are protected health information because sharing personal health information exposes an individual to a range of harm that may result from a violation of their expectation of privacy. Some privacy risks include an increased likelihood of medical identity theft, termination of disability coverage and unauthorized use of advanced medical research by third parties.
As of 2000, there is a broad international debate about ways to balance patient and commercial medicine demands for personal health information with an individual's needs for safety and respect.
Electronic medical records:
Main article: Electronic medical record
An electronic medical record is a medical record stored on electronic media, for example, computer servers or hard-drives.
De-identification:
Main article: De-identification
De-identification is an attempt to remove patients' identifiable information from their medical records with the intent of making the information transferable without compromising patients' identities. The closer the data is to anonymization, the lesser its value to those who want it.
Research companies and digital advertising companies are among the third parties that use such information in a variety of ways, which include using these patient datasets to reach their target audiences, formulate new medications or collect genetic data for government surveillance. Patients' data is rarely fully anonymized. Many controversies regarding the de-identification of patient's data exist.
Research using personal health information:
There is a high commercial demand for accessing extensive collections of various types of personal health care information.
Distribution of collections of personal health information:
In 2014 National Health Service (NHS) in the United Kingdom proposed selling patients' personal health information. In 2013, however, various groups had expressed worries over dangers resulting from the distribution of patients' identifiable information along with their medical history.
Major providers of health information on the Internet:
PubMed:
Main article: PubMed
PubMed is a free search engine that primarily lists the MEDLINE database of peer-reviewed references and abstracts on life sciences and biomedical topics maintained by the United States National Library of Medicine at the National Institutes of Health. When readers search and try to access a manuscript of interest, they are directed to the website of the respective journal where the document was originally published.
Wikis:
Main articles: Health information on Wikipedia and List of medical wikis
In 2014, Wikipedia was described as "the leading single source of healthcare information for patients and healthcare professionals". The information available on Wikipedia may not be peer-reviewed. Other wiki-style website exist to promulgate medical and heath-related information.
Regulation:
In the United States, the Food and Drug Administration offers guidance for health industry organizations that share information online.
See also:
Description:
The Internet is widely used by the general public as a tool for finding health information. In the late 1990s, researchers noted an increase in Internet users' access to health-related content despite the variation in the quality of information, level of accessibility, and overall health literacy. Access to health information does not guarantee understanding, as health literacy of individuals vary.
It is believed patients who know their medical history may learn and interpret this information in a way that benefits them. This, however, is not always the case because online health information is not always peer reviewed. Physicians worry that patients who conduct Internet research on their medical history are at a risk of being misinformed.
In 2013, the opinions about the relationship between health care providers and online health information were still being established. According to a 2014 study, "The flow of information has fundamentally changed, and physicians have less control over health information relayed to patients. Not surprisingly, this paradigm shift has elicited varied and sometimes conflicting views about the value of the Internet as a tool to improve health care."
Importance of the physician-patient relationship:
In cases in which a physician has difficulty explaining complicated medical concepts to a patient, that patient may be inclined to seek information on the internet. A consensus exists that patients should have shared decision making, meaning that patients should be able to make informed decisions about the direction of their medical treatment in collaboration with their physician. Rich, educated, and socially advantaged patients may enjoy the benefits of the shared decision-making approach more than those with a lower socioeconomic class or minority status.
Patients' naive understanding of their health contributes to a range of issues, including the tendency to deviate from the physician's medical advice or to miss medical appointments.
Patients with limited access to health information are more likely to use complementary and alternative medicine, and fail to inform their physician about it. Complementary and alternative medicine may not be evidence-based medicine.
While physicians can work on improving their doctor-patient communication skills, individuals can become more knowledgeable about their health through patient education programs. A study by Lorig in 2002 suggested healthcare processes can be efficiently improved with patients' behavior.
Social media:
Social forums in which anyone can have conversations about health with their peers exist; these are especially popular among patients who want to talk about shared medical concerns with others. Those who participate in online communities that discuss health issues report feeling relieved about their health worries, perceiving they have more control over their health and medical condition, gaining more medical knowledge, and having more personal agency overall.
Some research studies have failed to find evidence to validate the physicians' concerns about patients receiving misinformation online or using online health information to conduct self-diagnosis. Patients with chronic diseases who use the Internet to get health-related information often acquire good skills to judge the quality of information that they find.
Social media platforms are considered channels physicians can use to acquire insight on their patients' thoughts. Patients have increasingly turned to social media for health information, sometimes of dubious quality. Several studies have used social media to gather data on patients' adverse drug reactions (ADRs) with generally promising results.
Some commercial organizations use health information gathered from the Internet, raising serious ethical and privacy concerns, including the risk of accidental violations of the patient privacy by healthcare providers.
Academic medical literature:
The written record of peer-reviewed medical consensus is stored in scientific journals. There has been an academic journal publishing reform since the advent of electronic publishing.
Although some journals have adopted an open access template for online users, other journals are opposed to a widening of open access publishing. The open-access policy has significantly increased the accessibility of professional health information to researchers, physicians, and the public through the Internet. Some of the academic medical literature, however, may not be peer-reviewed and users are advised to exercise caution when reading health-related articles from such websites.
Quality:
The nature of health-related information available on the Internet is complex and its quality varies greatly by source. The standards for ensuring quality control on the Internet have been criticized and no single standard is universally accepted.
Many researchers have investigated this issue in detail, resulting in a wide range of theories from different disciplines.
Personal health information:
For many applications, people wish to use health information on the Internet to gain further insight about a personal health concern. Because of this, the goal is often to use the Internet to find information as it is described in a person's medical record. Since the advent of electronic media, medical records have been increasingly kept as electronic medical records.
More healthcare professionals rely on electronic medical records because it is a favorable means for patients to access their personal health information. These comprehensive systems allow patients to easily access their records without a doctor's visit, view interactive patient education materials, and use a greater range of health services such as renewing a medical prescription or making an appointment online.
All medical records are protected health information because sharing personal health information exposes an individual to a range of harm that may result from a violation of their expectation of privacy. Some privacy risks include an increased likelihood of medical identity theft, termination of disability coverage and unauthorized use of advanced medical research by third parties.
As of 2000, there is a broad international debate about ways to balance patient and commercial medicine demands for personal health information with an individual's needs for safety and respect.
Electronic medical records:
Main article: Electronic medical record
An electronic medical record is a medical record stored on electronic media, for example, computer servers or hard-drives.
De-identification:
Main article: De-identification
De-identification is an attempt to remove patients' identifiable information from their medical records with the intent of making the information transferable without compromising patients' identities. The closer the data is to anonymization, the lesser its value to those who want it.
Research companies and digital advertising companies are among the third parties that use such information in a variety of ways, which include using these patient datasets to reach their target audiences, formulate new medications or collect genetic data for government surveillance. Patients' data is rarely fully anonymized. Many controversies regarding the de-identification of patient's data exist.
Research using personal health information:
There is a high commercial demand for accessing extensive collections of various types of personal health care information.
Distribution of collections of personal health information:
In 2014 National Health Service (NHS) in the United Kingdom proposed selling patients' personal health information. In 2013, however, various groups had expressed worries over dangers resulting from the distribution of patients' identifiable information along with their medical history.
Major providers of health information on the Internet:
PubMed:
Main article: PubMed
PubMed is a free search engine that primarily lists the MEDLINE database of peer-reviewed references and abstracts on life sciences and biomedical topics maintained by the United States National Library of Medicine at the National Institutes of Health. When readers search and try to access a manuscript of interest, they are directed to the website of the respective journal where the document was originally published.
Wikis:
Main articles: Health information on Wikipedia and List of medical wikis
In 2014, Wikipedia was described as "the leading single source of healthcare information for patients and healthcare professionals". The information available on Wikipedia may not be peer-reviewed. Other wiki-style website exist to promulgate medical and heath-related information.
Regulation:
In the United States, the Food and Drug Administration offers guidance for health industry organizations that share information online.
See also:
- WebMD
- Evaluating Health Information by MedlinePlus
- How to Evaluate Health Information on the Internet by the Food and Drug Administration
How Wikipedia Prevents the Spread of Coronavirus Misinformation (Wired Magazine 03/15/2020)Pictured below: Pie chart of Wikipedia content by subject as of January 2008
[Your WebHost: I am both happy and relieved that, as an encyclopedic source, Wikipedia has only gotten better as time has enabled it to. Likely 70 percent of the content of this website originates with Wikipedia, starting in 2014!]
How Wikipedia Prevents the Spread of Coronavirus Misinformation
A group of hawk-eyed experts operate on a special track to monitor medical information on the site.
“This edit was VERY poor,” wrote James Heilman, an emergency room doctor in British Columbia, to a Wikipedia contributor who had made a couple of changes toward the end of the article on the new coronavirus outbreak.
Those edits recommended a special type of mask for blocking the transmission of the virus from those who have it, and Heilman, a prominent figure in reviewing medical Wikipedia articles, wanted to inform the editor that this advice was too sweeping and based on insufficient evidence. More than that, he aimed to send a warning. “Please do not make edits like this again,” he wrote.
Wikipedia’s reputation is generally on the ascent. Just last month, no less a publication than WIRED deemed it “the last best place on the internet.” What was once considered the site’s greatest vulnerability—that anyone can edit it—has been revealed to be its greatest strength. In the place of experts, there are enthusiasts who are thrilled to share their knowledge of a little part of the world with all of humanity.
As Richard Cooke, who wrote the WIRED essay, observed: “It’s assembled grain by grain, like a termite mound. The smallness of the grains, and of the workers carrying them, makes the project’s scale seem impossible. But it is exactly this incrementalism that puts immensity within reach.”
Read all of our coronavirus coverage here.
His point, and it’s really indisputable, is that this mammoth online project has developed a personality, a purpose, a soul. Now, as the new coronavirus outbreak plays out across its many pages, we can see that Wikipedia has also developed a conscience.
The coronavirus articles on English Wikipedia are part of WikiProject Medicine, a collection of some 35,000 articles that are watched over by nearly 150 editors with interest and expertise in medicine and public health. (A survey for a paper co-written by Heilman in 2015 concluded that roughly half of the core editors had an advanced degree.)
Readers of Wikipedia wouldn’t know that an article is part of the project—the designation appears on a separate talk page and really serves as a head’s up to interested editors to look carefully at the entries.
Once an article has been flagged as relating to medicine, the editors scrutinize the article with an exceptional ferocity. While typically an article in The New York Times or The Wall Street Journal would be a reliable source for Wikipedia, the medical editors insist on peer-reviewed papers, textbooks or reports from prominent centers and institutes.
On these subjects, Wikipedia doesn’t seem like the encyclopedia anyone can edit, striving to be welcoming to newcomers; it certainly doesn’t profess a laid-back philosophy that articles improve over time and can start off a bit unevenly. The editor chastised by Heilman hasn’t returned to the article and instead is improving articles about sound-recording equipment.
By having these different standards within its pages, Wikipedia can be a guide to the big commercial platforms that have become way stations for fake cures, bogus comparisons to past outbreaks, and political spin. Twitter, Amazon, YouTube, and Facebook have all promised to cleanse their sites of this dangerous disinformation, but they are doing so in fits and starts and by relying in part on familiar, passive tools like acting when others flag dangerous content.
Here is how Facebook's Mark Zuckerberg put it in a post on March 3: “It’s important that everyone has a place to share their experiences and talk about the outbreak, but as our community standards make clear, it’s not okay to share something that puts people in danger.
So we’re removing false claims and conspiracy theories that have been flagged by leading global health organizations. We’re also blocking people from running ads that try to exploit the situation—for example, claiming that their product can cure the disease.”
Wikipedia shows, however, that extreme circumstances, especially when related to public health, require different, more stringent rules, not better application of existing rules. The stakes are simply too high.
I spoke this week with the Wikipedia editor who guided the article about the new coronavirus from a one-sentence item in early January to a substantial article with charts of infections around the world. She goes by the handle Whispyhistory, and is a doctor in South London; she spoke via Skype from her office, which she proudly noted had a new thermometer that looks like a laser gun.
Whispyhistory has only been contributing for three years; she was recruited through an edit-a-thon at a medical library. While at first she was open with her colleagues about her side project, now she prefers to remain anonymous. “You start getting hounded by people about what you are writing,” she said. “It’s just so much easier to not use your real name.”
WikiProject Medicine welcomed her, she said, but she’s had to build a reputation for accuracy and responsibility. “You have to know what you are saying,” she said, and even so it can be intimidating. “You’ve got so many people watching you.” The picture she paints of the project’s contributors is akin to the staff of a demanding teaching hospital. The editors confer on a talk page she calls “the doctors’ mess” where they perform “triage” to assess which articles require attention immediately. Science and data reign; and above all else, the pledge is to do no harm.
On January 6, she said, a colleague asked her if she had heard of an outbreak of atypical pneumonia in China. She hadn’t, but “being someone who writes for Wikipedia, the first thing you do is see if it’s on Wikipedia. Someone had written the article the day before.” The article was thin, but Whispyhistory had the sense that “this might be something big,” so she added the WikiProject Medicine tag to the article and wrote a note informing her colleagues to pay attention to the outbreak, which they did.
Like a young resident, she pulled all-nighters before showing up at the office at 6 am, keeping a watch over the article as the virus spread. In those early days, for instance, she saw a note on the doctors’ mess that linked to a news report claiming that the new coronavirus could survive on surfaces for nine hours.
The author wanted to add that information to the Wikipedia page immediately. “That already sends an alert since there is nothing that’s really so important that you’ve got to add something straight away,” she recalled. She went from the news article to the paper that it cited, and discovered that it was looking at the SARS virus, not the (very similar) one that causes Covid-19. She decided not to include the research.
As Heilman put it in an email, “Keeping Wikipedia reliable and up-to-date involves deleting material just as much as adding it.” I asked both him and Whispyhistory how the article on the new coronavirus managed to exclude the arguments that were being made (at least until recently) by President Trump and his supporters—that the disease is being hyped by Democrats and that it’s comparable to the flu. Don’t they have angry wannabe contributors accusing Wikipedia of bias? “That’s really easy to answer. ... You have to cite everything you write,” Whispyhistory said. Heilman agreed that a requirement for legitimate sourcing filters out unfounded notions.
Bogus claims about the pandemic do show up on Wikipedia, but in a separate article: “Misinformation related to the 2019–20 coronavirus pandemic,” under the heading “Misinformation by governments/United States.” Heilman noted that Wikipedia has a structural advantage over the big social networks: “It takes more time and effort to disrupt Wikipedia than it does to restore Wikipedia to a reliable level. It’s the exact opposite on Twitter and Facebook, where it takes a second to spread false news,” while getting those lies removed will take a lot of time and effort.
Unless Twitter, Facebook and the others can learn to address misinformation more effectively, Wikipedia will remain the last best place on the Internet.
WIRED is providing free access to stories about public health and how to protect yourself during the coronavirus pandemic. Sign up for our Coronavirus Update newsletter for the latest updates, and subscribe to support our journalism.
More From WIRED on Covid-19:
How Wikipedia Prevents the Spread of Coronavirus Misinformation
A group of hawk-eyed experts operate on a special track to monitor medical information on the site.
“This edit was VERY poor,” wrote James Heilman, an emergency room doctor in British Columbia, to a Wikipedia contributor who had made a couple of changes toward the end of the article on the new coronavirus outbreak.
Those edits recommended a special type of mask for blocking the transmission of the virus from those who have it, and Heilman, a prominent figure in reviewing medical Wikipedia articles, wanted to inform the editor that this advice was too sweeping and based on insufficient evidence. More than that, he aimed to send a warning. “Please do not make edits like this again,” he wrote.
Wikipedia’s reputation is generally on the ascent. Just last month, no less a publication than WIRED deemed it “the last best place on the internet.” What was once considered the site’s greatest vulnerability—that anyone can edit it—has been revealed to be its greatest strength. In the place of experts, there are enthusiasts who are thrilled to share their knowledge of a little part of the world with all of humanity.
As Richard Cooke, who wrote the WIRED essay, observed: “It’s assembled grain by grain, like a termite mound. The smallness of the grains, and of the workers carrying them, makes the project’s scale seem impossible. But it is exactly this incrementalism that puts immensity within reach.”
Read all of our coronavirus coverage here.
His point, and it’s really indisputable, is that this mammoth online project has developed a personality, a purpose, a soul. Now, as the new coronavirus outbreak plays out across its many pages, we can see that Wikipedia has also developed a conscience.
The coronavirus articles on English Wikipedia are part of WikiProject Medicine, a collection of some 35,000 articles that are watched over by nearly 150 editors with interest and expertise in medicine and public health. (A survey for a paper co-written by Heilman in 2015 concluded that roughly half of the core editors had an advanced degree.)
Readers of Wikipedia wouldn’t know that an article is part of the project—the designation appears on a separate talk page and really serves as a head’s up to interested editors to look carefully at the entries.
Once an article has been flagged as relating to medicine, the editors scrutinize the article with an exceptional ferocity. While typically an article in The New York Times or The Wall Street Journal would be a reliable source for Wikipedia, the medical editors insist on peer-reviewed papers, textbooks or reports from prominent centers and institutes.
On these subjects, Wikipedia doesn’t seem like the encyclopedia anyone can edit, striving to be welcoming to newcomers; it certainly doesn’t profess a laid-back philosophy that articles improve over time and can start off a bit unevenly. The editor chastised by Heilman hasn’t returned to the article and instead is improving articles about sound-recording equipment.
By having these different standards within its pages, Wikipedia can be a guide to the big commercial platforms that have become way stations for fake cures, bogus comparisons to past outbreaks, and political spin. Twitter, Amazon, YouTube, and Facebook have all promised to cleanse their sites of this dangerous disinformation, but they are doing so in fits and starts and by relying in part on familiar, passive tools like acting when others flag dangerous content.
Here is how Facebook's Mark Zuckerberg put it in a post on March 3: “It’s important that everyone has a place to share their experiences and talk about the outbreak, but as our community standards make clear, it’s not okay to share something that puts people in danger.
So we’re removing false claims and conspiracy theories that have been flagged by leading global health organizations. We’re also blocking people from running ads that try to exploit the situation—for example, claiming that their product can cure the disease.”
Wikipedia shows, however, that extreme circumstances, especially when related to public health, require different, more stringent rules, not better application of existing rules. The stakes are simply too high.
I spoke this week with the Wikipedia editor who guided the article about the new coronavirus from a one-sentence item in early January to a substantial article with charts of infections around the world. She goes by the handle Whispyhistory, and is a doctor in South London; she spoke via Skype from her office, which she proudly noted had a new thermometer that looks like a laser gun.
Whispyhistory has only been contributing for three years; she was recruited through an edit-a-thon at a medical library. While at first she was open with her colleagues about her side project, now she prefers to remain anonymous. “You start getting hounded by people about what you are writing,” she said. “It’s just so much easier to not use your real name.”
WikiProject Medicine welcomed her, she said, but she’s had to build a reputation for accuracy and responsibility. “You have to know what you are saying,” she said, and even so it can be intimidating. “You’ve got so many people watching you.” The picture she paints of the project’s contributors is akin to the staff of a demanding teaching hospital. The editors confer on a talk page she calls “the doctors’ mess” where they perform “triage” to assess which articles require attention immediately. Science and data reign; and above all else, the pledge is to do no harm.
On January 6, she said, a colleague asked her if she had heard of an outbreak of atypical pneumonia in China. She hadn’t, but “being someone who writes for Wikipedia, the first thing you do is see if it’s on Wikipedia. Someone had written the article the day before.” The article was thin, but Whispyhistory had the sense that “this might be something big,” so she added the WikiProject Medicine tag to the article and wrote a note informing her colleagues to pay attention to the outbreak, which they did.
Like a young resident, she pulled all-nighters before showing up at the office at 6 am, keeping a watch over the article as the virus spread. In those early days, for instance, she saw a note on the doctors’ mess that linked to a news report claiming that the new coronavirus could survive on surfaces for nine hours.
The author wanted to add that information to the Wikipedia page immediately. “That already sends an alert since there is nothing that’s really so important that you’ve got to add something straight away,” she recalled. She went from the news article to the paper that it cited, and discovered that it was looking at the SARS virus, not the (very similar) one that causes Covid-19. She decided not to include the research.
As Heilman put it in an email, “Keeping Wikipedia reliable and up-to-date involves deleting material just as much as adding it.” I asked both him and Whispyhistory how the article on the new coronavirus managed to exclude the arguments that were being made (at least until recently) by President Trump and his supporters—that the disease is being hyped by Democrats and that it’s comparable to the flu. Don’t they have angry wannabe contributors accusing Wikipedia of bias? “That’s really easy to answer. ... You have to cite everything you write,” Whispyhistory said. Heilman agreed that a requirement for legitimate sourcing filters out unfounded notions.
Bogus claims about the pandemic do show up on Wikipedia, but in a separate article: “Misinformation related to the 2019–20 coronavirus pandemic,” under the heading “Misinformation by governments/United States.” Heilman noted that Wikipedia has a structural advantage over the big social networks: “It takes more time and effort to disrupt Wikipedia than it does to restore Wikipedia to a reliable level. It’s the exact opposite on Twitter and Facebook, where it takes a second to spread false news,” while getting those lies removed will take a lot of time and effort.
Unless Twitter, Facebook and the others can learn to address misinformation more effectively, Wikipedia will remain the last best place on the Internet.
WIRED is providing free access to stories about public health and how to protect yourself during the coronavirus pandemic. Sign up for our Coronavirus Update newsletter for the latest updates, and subscribe to support our journalism.
More From WIRED on Covid-19:
- How to make your own hand sanitizer
- Singapore was ready for Covid-19--other countries, take note
- Is it ethical to order delivery during a pandemic?
- Can't stop touching your face? Science has some theories why
- Tips for working from home without losing your mind
- Read all of our coronavirus coverage here
The Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) is a law passed by the U.S. Congress on a reconciliation basis and signed by President Ronald Reagan that, among other things, mandates an insurance program which gives some employees the ability to continue health insurance coverage after leaving employment.
COBRA includes amendments to the Employee Retirement Income Security Act of 1974 (ERISA). The law deals with a great variety of subjects, such as:
However, it is perhaps best known for Title X, which amends the Internal Revenue Code and the Public Health Service Act to deny income tax deductions to employers (generally those with 20 or more full-time equivalent employees) for contributions to a group health plan unless such plan meets certain continuing coverage requirements. The violation for failing to meet those criteria was subsequently changed to an excise tax.
Although this statute became law on April 7, 1986, its official name is the Consolidated Omnibus Budget Reconciliation Act of 1985 (Pub.L. 99–272, 100 Stat. 82). Because of the discrepancy between the official name of the Act and the year in which it was enacted, some government publications refer to the Act as the Consolidated Omnibus Budget Reconciliation Act of 1986.
Provisions:
As originally enacted, Title X of the Act provided that a qualifying employer will not be permitted to take a tax deduction for its health insurance costs unless its health insurance plan allows employees of the employer and the employee's immediate family members who had been covered by a health care plan to maintain their coverage if a "qualifying event" causes them to lose coverage.
However, the legislation was subsequently amended to instead impose an excise tax upon an employer whose health plan fails to satisfy the applicable rules. A qualifying employer is generally an employer with 20 or more full-time-equivalent employees.
Among the "qualifying events" listed in the statute are loss of benefits coverage due to
See DOL.GOV's FAQs For Employers About COBRA Continuation Health Coverage
COBRA also allows for coverage for up to 18 months in most cases. If the individual is deemed disabled by the Social Security Administration, coverage may continue for up to 29 months.
In the case of divorce from the former employee, the former spouse's coverage may continue for up to 36 months. In the case of death of the former employee, the widow's coverage may continue for up to 36 months.
COBRA does not apply, on the other hand, if employees lose their benefits coverage because the employer has terminated the plan altogether or if the employer has gone out of business.
In cases where COBRA does not apply, some states have stepped in with state health insurance continuation laws, usually called "mini-COBRA" laws, which help employees continue their health insurance when federal COBRA does not apply.
COBRA does not, unlike other federal statutes such as the Family and Medical Leave Act (FMLA), require the employer to pay for the cost of providing continuation coverage. Instead it allows employees and their dependents to maintain coverage at their own expense by paying the full cost of the premium the employer and the employee previously paid, plus up to a 2% administrative charge (50% for the latter 11 months under the disability extension).
According to the U.S. Department of Labor:
"...the coverage you are given must be identical to the coverage that is currently available under the plan to similarly situated active employees and their families (generally, this is the same coverage that you had immediately before the qualifying event).
You will also be entitled, while receiving continuation coverage, to the same benefits, choices, and services that a similarly situated participant or beneficiary is currently receiving under the plan, such as the right during an open enrollment season to choose among available coverage options. You will also be subject to the same rules and limits that would apply to a similarly situated participant or beneficiary, such as co-payment requirements, deductibles, and coverage limits.
Employees and dependents can also opt for a lesser form of coverage, e.g., to choose continuation coverage under a plan that only covers the employee, but not his or her dependents, or that only provides medical and hospitalization coverage and does not pay for dental work, if those options are available to covered employees.
Employees and dependents lose coverage if they fail to make timely payments of these premiums. Employers are required to inform employees and dependents upon loss of coverage, in writing, by at least fifteen days before the coverage ceases."
Coordination of coverage:
An individual covered under COBRA may also be covered by another group health plan or Medicare as long as either of two conditions is met:
Subsidy under federal stimulus:
Only 10% of Americans eligible for COBRA insurance in 2006 used it, many because they were unable to afford to pay the full premium after their job loss. While some employers may voluntarily help subsidize or fully cover the cost of COBRA insurance as part of a termination or exit package, it is more common for the ex-employee to cover the entire cost.
The American Recovery and Reinvestment Act of 2009 as signed by President Barack Obama includes a 65% subsidy to employees for COBRA-enabled insurance for up to 9 months after an involuntary termination (this has since been expanded to 15 months). An employee is eligible for this subsidy if:
If the employee has an adjusted gross income in 2009 over $125,000 if filing as single ($250,000 if filing jointly), then the subsidy will be recaptured in a phased manner from the employee through the tax system.
Termination of employment must have occurred between September 1, 2008 and December 31, 2009 (later expanded to February 28, 2010, expanded again to March 31, 2010, and then expanded again to June 2, 2010).
Specific provisions and responsibilities may differ in the state specific mini-COBRA plans for employers with fewer than 20 employees throughout half of the previous calendar year.
Those employees who are eligible for the ultimate benefits of this subsidy are referred to as Assistance Eligible Individuals (or AEIs).
Employers subject to Federal COBRA are required to:
This Act was signed into law by President Barack Obama on February 17, 2009.
On December 19, 2009, President Obama signed into law the Department of Defense Appropriations Act, 2010, which made several amendments to the COBRA provisions of the American Recovery and Reinvestment Act of 2009 (ARRA). The Act extends COBRA subsidy eligibility to employees who lost their jobs due to no fault of their own between January 1 and February 28, 2010. The nine-month subsidy period was also expanded to fifteen months.
On March 3, 2010, President Obama signed into law the Temporary Extension Act of 2010. The Act extends COBRA subsidy eligibility to employees who lost their jobs due to no fault of their own between March 1 and 31, 2010. In addition, employees who lost group health insurance due to reduced work hours on or after Sept. 1, 2008, followed by involuntary termination between March 2 and March 31, 2010, will now be eligible for the COBRA subsidy.
The Continuing Extension Act of 2010 extends premium assistance for COBRA benefits through May 31, 2010.
As of June 2010, an extension of COBRA's premium assistance has not materialized, and attempts by congressional members to include such provisions have been dropped.
As of June 1, 2010, all newly unemployed workers must pay full coverage costs as determined by their respective plans. This is due in part to conservative Democrats in Congress who have expressed concerns about treating some unemployed workers differently from others, such as people priced out of the private insurance market.
A number of Senate Democrats expressed concern about this situation and have introduced legislation to expand COBRA coverage to people who become unemployed through November 2010, but such legislation did not pass in 2010.
Similar state and local legislation:
Forty-one states have legislation similar to federal COBRA requiring employers to allow employees and their dependents to continue their group health insurance coverage following certain qualifying events. The district of Columbia also has laws covering COBRA.
California:
California's legislation only applies to non-government employers with a group health insurance plan with fewer than twenty employees.
District of Columbia:
The District of Columbia's Continuation of Health Coverage Act of 2001 applies to employers with a group health insurance plan with a situs in the District of Columbia and with fewer than twenty employees. Coverage must be offered to be extended for a period of three months following the date that coverage would have ended.
Maryland:
Maryland's legislation only applies to employers with a group health insurance plan with a situs in Maryland and with fewer than twenty employees that continuation coverage must be offered to an employee who lives in Maryland, who had coverage from the employer for at least three months, and who either resigns or loses employment due to no fault of their own.
Continuation coverage must also be offered to the former spouse and dependent children of an employee after a divorce. One exception to the eighteen-month rule is that coverage may end for the former spouse upon the former spouse's remarriage.
Continuation coverage must also be offered to the surviving spouse and dependent children of an employee who dies. The employee must have resided in Maryland and had coverage with the employer for at least three months prior to death. In all cases, continuation coverage must be offered for eighteen months, with the exception that a former spouse's continuation coverage ends upon remarriage.
Virginia:
Virginia's legislation applies to employers with a group health insurance plan, other than an HMO plan, and with twenty or fewer employees. Employers must offer continuation coverage to employees for twelve months. The legislation does not apply to employees who did not have coverage from the employer for at least three months prior to the qualifying event.
See also:
Private Websites:
COBRA includes amendments to the Employee Retirement Income Security Act of 1974 (ERISA). The law deals with a great variety of subjects, such as:
- tobacco price supports,
- railroads,
- private pension plans,
- emergency department treatment,
- disability insurance,
- and the postal service.
However, it is perhaps best known for Title X, which amends the Internal Revenue Code and the Public Health Service Act to deny income tax deductions to employers (generally those with 20 or more full-time equivalent employees) for contributions to a group health plan unless such plan meets certain continuing coverage requirements. The violation for failing to meet those criteria was subsequently changed to an excise tax.
Although this statute became law on April 7, 1986, its official name is the Consolidated Omnibus Budget Reconciliation Act of 1985 (Pub.L. 99–272, 100 Stat. 82). Because of the discrepancy between the official name of the Act and the year in which it was enacted, some government publications refer to the Act as the Consolidated Omnibus Budget Reconciliation Act of 1986.
Provisions:
As originally enacted, Title X of the Act provided that a qualifying employer will not be permitted to take a tax deduction for its health insurance costs unless its health insurance plan allows employees of the employer and the employee's immediate family members who had been covered by a health care plan to maintain their coverage if a "qualifying event" causes them to lose coverage.
However, the legislation was subsequently amended to instead impose an excise tax upon an employer whose health plan fails to satisfy the applicable rules. A qualifying employer is generally an employer with 20 or more full-time-equivalent employees.
Among the "qualifying events" listed in the statute are loss of benefits coverage due to
- the death of the covered employee;
- an employee loses eligibility for coverage due to voluntary or involuntary termination or a reduction in hours as a result of resignation, discharge (except for "gross misconduct"), layoff, strike or lockout, medical leave, or slowdown in business operations;
- divorce or legal separation that terminates the ex-spouse's eligibility for benefits;
- or a dependent child reaching the age at which he or she is no longer covered. COBRA imposes different notice requirements on participants and beneficiaries, depending on the particular qualifying event that triggers COBRA rights.
See DOL.GOV's FAQs For Employers About COBRA Continuation Health Coverage
COBRA also allows for coverage for up to 18 months in most cases. If the individual is deemed disabled by the Social Security Administration, coverage may continue for up to 29 months.
In the case of divorce from the former employee, the former spouse's coverage may continue for up to 36 months. In the case of death of the former employee, the widow's coverage may continue for up to 36 months.
COBRA does not apply, on the other hand, if employees lose their benefits coverage because the employer has terminated the plan altogether or if the employer has gone out of business.
In cases where COBRA does not apply, some states have stepped in with state health insurance continuation laws, usually called "mini-COBRA" laws, which help employees continue their health insurance when federal COBRA does not apply.
COBRA does not, unlike other federal statutes such as the Family and Medical Leave Act (FMLA), require the employer to pay for the cost of providing continuation coverage. Instead it allows employees and their dependents to maintain coverage at their own expense by paying the full cost of the premium the employer and the employee previously paid, plus up to a 2% administrative charge (50% for the latter 11 months under the disability extension).
According to the U.S. Department of Labor:
"...the coverage you are given must be identical to the coverage that is currently available under the plan to similarly situated active employees and their families (generally, this is the same coverage that you had immediately before the qualifying event).
You will also be entitled, while receiving continuation coverage, to the same benefits, choices, and services that a similarly situated participant or beneficiary is currently receiving under the plan, such as the right during an open enrollment season to choose among available coverage options. You will also be subject to the same rules and limits that would apply to a similarly situated participant or beneficiary, such as co-payment requirements, deductibles, and coverage limits.
Employees and dependents can also opt for a lesser form of coverage, e.g., to choose continuation coverage under a plan that only covers the employee, but not his or her dependents, or that only provides medical and hospitalization coverage and does not pay for dental work, if those options are available to covered employees.
Employees and dependents lose coverage if they fail to make timely payments of these premiums. Employers are required to inform employees and dependents upon loss of coverage, in writing, by at least fifteen days before the coverage ceases."
Coordination of coverage:
An individual covered under COBRA may also be covered by another group health plan or Medicare as long as either of two conditions is met:
- The other coverage was in force as of or prior to the coverage under COBRA.
- The other coverage is subject to pre-existing conditions exclusions or limitations.
Subsidy under federal stimulus:
Only 10% of Americans eligible for COBRA insurance in 2006 used it, many because they were unable to afford to pay the full premium after their job loss. While some employers may voluntarily help subsidize or fully cover the cost of COBRA insurance as part of a termination or exit package, it is more common for the ex-employee to cover the entire cost.
The American Recovery and Reinvestment Act of 2009 as signed by President Barack Obama includes a 65% subsidy to employees for COBRA-enabled insurance for up to 9 months after an involuntary termination (this has since been expanded to 15 months). An employee is eligible for this subsidy if:
- the termination of employment was involuntary,
- the terminated employee has no other group sponsored health insurance option, and
- the terminated employee is otherwise eligible to enroll in COBRA.
If the employee has an adjusted gross income in 2009 over $125,000 if filing as single ($250,000 if filing jointly), then the subsidy will be recaptured in a phased manner from the employee through the tax system.
Termination of employment must have occurred between September 1, 2008 and December 31, 2009 (later expanded to February 28, 2010, expanded again to March 31, 2010, and then expanded again to June 2, 2010).
Specific provisions and responsibilities may differ in the state specific mini-COBRA plans for employers with fewer than 20 employees throughout half of the previous calendar year.
Those employees who are eligible for the ultimate benefits of this subsidy are referred to as Assistance Eligible Individuals (or AEIs).
Employers subject to Federal COBRA are required to:
- Notify terminated employees of their potential rights under ARRA by sending a series of notices
- Provide a method for qualified AEIs to enroll
- Pay the full amount of the premiums and seek reimbursement of the 65% subsidy by including it in the Employer's Quarterly Federal Tax Return (Form 941)
This Act was signed into law by President Barack Obama on February 17, 2009.
On December 19, 2009, President Obama signed into law the Department of Defense Appropriations Act, 2010, which made several amendments to the COBRA provisions of the American Recovery and Reinvestment Act of 2009 (ARRA). The Act extends COBRA subsidy eligibility to employees who lost their jobs due to no fault of their own between January 1 and February 28, 2010. The nine-month subsidy period was also expanded to fifteen months.
On March 3, 2010, President Obama signed into law the Temporary Extension Act of 2010. The Act extends COBRA subsidy eligibility to employees who lost their jobs due to no fault of their own between March 1 and 31, 2010. In addition, employees who lost group health insurance due to reduced work hours on or after Sept. 1, 2008, followed by involuntary termination between March 2 and March 31, 2010, will now be eligible for the COBRA subsidy.
The Continuing Extension Act of 2010 extends premium assistance for COBRA benefits through May 31, 2010.
As of June 2010, an extension of COBRA's premium assistance has not materialized, and attempts by congressional members to include such provisions have been dropped.
As of June 1, 2010, all newly unemployed workers must pay full coverage costs as determined by their respective plans. This is due in part to conservative Democrats in Congress who have expressed concerns about treating some unemployed workers differently from others, such as people priced out of the private insurance market.
A number of Senate Democrats expressed concern about this situation and have introduced legislation to expand COBRA coverage to people who become unemployed through November 2010, but such legislation did not pass in 2010.
Similar state and local legislation:
Forty-one states have legislation similar to federal COBRA requiring employers to allow employees and their dependents to continue their group health insurance coverage following certain qualifying events. The district of Columbia also has laws covering COBRA.
California:
California's legislation only applies to non-government employers with a group health insurance plan with fewer than twenty employees.
District of Columbia:
The District of Columbia's Continuation of Health Coverage Act of 2001 applies to employers with a group health insurance plan with a situs in the District of Columbia and with fewer than twenty employees. Coverage must be offered to be extended for a period of three months following the date that coverage would have ended.
Maryland:
Maryland's legislation only applies to employers with a group health insurance plan with a situs in Maryland and with fewer than twenty employees that continuation coverage must be offered to an employee who lives in Maryland, who had coverage from the employer for at least three months, and who either resigns or loses employment due to no fault of their own.
Continuation coverage must also be offered to the former spouse and dependent children of an employee after a divorce. One exception to the eighteen-month rule is that coverage may end for the former spouse upon the former spouse's remarriage.
Continuation coverage must also be offered to the surviving spouse and dependent children of an employee who dies. The employee must have resided in Maryland and had coverage with the employer for at least three months prior to death. In all cases, continuation coverage must be offered for eighteen months, with the exception that a former spouse's continuation coverage ends upon remarriage.
Virginia:
Virginia's legislation applies to employers with a group health insurance plan, other than an HMO plan, and with twenty or fewer employees. Employers must offer continuation coverage to employees for twelve months. The legislation does not apply to employees who did not have coverage from the employer for at least three months prior to the qualifying event.
See also:
- Other Resources, Department of Labor
- Library of Congress THOMAS summary of the Act.
- General information from the Centers for Medicare and Medicaid Services (CMS) (2006, archived)
Private Websites:
- COBRA insurance guide Information about COBRA (cobrainsurance.com, private website)
- COBRA insurance information (cobrainsurancebenefits.org, private website)
- Understanding COBRA (cobrainsurancedirect.com, private website)
- COBRA Insurance Direct Learn more about COBRA Insurance (cobrainsurancedirect.com, private website)
- All About COBRA Health Insurance (Investopedia, private website)
Health Insurance Portability and Accountability Act ("HIPAA") 1996
- YouTube Video: Why HIPAA?
- YouTube Video: Common HIPAA Mistakes
- YouTube Video: HIPAA Training: The HIPAA Privacy Rule
The Health Insurance Portability and Accountability Act of 1996 (HIPAA or the Kennedy–Kassebaum Act) was enacted by the 104th United States Congress and signed by President Bill Clinton in 1996.
HiPAA was created primarily to modernize the flow of healthcare information, stipulate how personally identifiable information maintained by the healthcare and healthcare insurance industries should be protected from fraud and theft, and address limitations on healthcare insurance coverage.
The act consists of five titles:
Click on any of the following blue hyperlinks for more about HIPAA:
HiPAA was created primarily to modernize the flow of healthcare information, stipulate how personally identifiable information maintained by the healthcare and healthcare insurance industries should be protected from fraud and theft, and address limitations on healthcare insurance coverage.
The act consists of five titles:
- Title I of HIPAA protects health insurance coverage for workers and their families when they change or lose their jobs.
- Title II of HIPAA, known as the Administrative Simplification (AS) provisions, requires the establishment of national standards for electronic health care transactions and national identifiers for providers, health insurance plans, and employers.
- Title III sets guidelines for pre-tax medical spending accounts,
- Title IV sets guidelines for group health plans,
- and Title V governs company-owned life insurance policies.
Click on any of the following blue hyperlinks for more about HIPAA:
- Titles
- Title I: Health Care Access, Portability, and Renewability
- Title II: Preventing Health Care Fraud and Abuse; Administrative Simplification; Medical Liability Reform
- Title III: Tax-related health provisions governing medical savings accounts
- Title IV: Application and enforcement of group health insurance requirements
- Title V: Revenue offset governing tax deductions for employers
- Effects on research and clinical care
- HIPAA acronym
- Violations
- Legislative information
- See also:
- California Office of HIPAA Implementation (CalOHI)
- "HIPAA", Centers for Medicare and Medicaid Services
- Congressional Research Service (CRS) reports regarding HIPAA, University of North Texas Libraries
- Full text of the Health Insurance Portability and Accountability Act (PDF/TXT) U.S. Government Printing Office
- Office for Civil Rights page on HIPAA
Patient Protection and Affordable Care Act, including Pre-existing Condition Coverage (2010)
- YouTube Video: Understanding the Affordable Care Act
- YouTube Video: ObamaCare: Real reason Republicans hate it
- YouTube Video: The Affordable Care Act Saves Lives
The Affordable Care Act (ACA), formally known as the Patient Protection and Affordable Care Act, and commonly known as Obamacare, is a United States federal statute enacted by the 111th United States Congress and signed into law by President Barack Obama on March 23, 2010.
Together with the Health Care and Education Reconciliation Act of 2010 amendment, it represents the U.S. healthcare system's most significant regulatory overhaul and expansion of coverage since the passage of Medicare and Mediacid in 1965.
ACA's major provisions came into force in 2014. By 2016, the uninsured share of the population had roughly halved, with estimates ranging from 20 to 24 million additional people covered. The law also enacted a host of delivery system reforms intended to constrain healthcare costs and improve quality. After the law went into effect, increases in overall healthcare spending slowed, including premiums for employer-based insurance plans.
The increased coverage was due, roughly equally, to an expansion of Medicaid eligibility and to changes to individual insurance markets. Both received new spending, funded through a combination of new taxes and cuts to Medicare provider rates and Medicare Advantage.
Several Congressional Budget Office reports said that overall these provisions reduced the budget deficit, that repealing ACA would increase the deficit, and that the law reduced income inequality by taxing primarily the top 1% to fund roughly $600 in benefits on average to families in the bottom 40% of the income distribution.
The act largely retained the existing structure of Medicare, Medicaid and the employer market, but individual markets were radically overhauled. Insurers were made to accept all applicants without charging based on pre-existing conditions (see next topic below) or demographic status (except age). To combat the resultant adverse selection, the act mandated that individuals buy insurance (or pay a fine/tax) and that insurers cover a list of "essential health benefits".
Before and after enactment ACA faced strong political opposition, calls for repeal and legal challenges. In National Federation of Independent Business v. Sebelius, the Supreme Court ruled that states could choose not to participate in ACA's Medicaid expansion, although it upheld the law as a whole.
The federal health exchange, HealthCare.gov, faced major technical problems at the beginning of its rollout in 2013. Polls initially found that a plurality of Americans opposed the act, although its individual provisions were generally more popular and the law gained majority support by 2017.
The federal tax penalty for violating the individual mandate of the ACA was rescinded by President Donald Trump through the Tax Cuts and Jobs Act of 2017, starting in 2019. This raised questions about whether the Affordable Care Act was still constitutional.
Click on any of the following blue hyperlinks for more about the Affordable Care Act:
Pre-existing condition:
In the context of healthcare in the United States, a pre-existing condition is a medical condition that started before a person's health insurance went into effect.
Before 2014 some insurance policies would not cover expenses due to pre-existing conditions. These exclusions by the insurance industry were meant to cope with adverse selection by potential customers.
Such exclusions have been prohibited since January 1, 2014, by the Patient Protection and Affordable Care Act.
According to the Kaiser Family Foundation, more than a quarter of adults below the age of 65 (approximately 52 million people) had pre-existing conditions in 2016.
Definitions:
The University of Pittsburgh Medical Center defines a pre-existing condition as a "medical condition that occurred before a program of health benefits went into effect".
James Rohack, president of the American Medical Association, has stated on a Fox News Sunday interview that exclusions, based upon these conditions, function as a form of "rationing" of health care.
Conditions can be broken down into two further categories, according to Lisa Smith of Investopedia: Most insurance companies use one of two definitions to identify such conditions.
Which definition may be used was sometimes regulated by state laws. Some states required insurance companies to use the objective standard, while others required the prudent person standard. 10 states did not specify either definition, 21 required the "prudent person" standard, and 18 required the "objective" standard.
According to the Kaiser Family Foundation, more than a quarter of adults below the age of 65 (approximately 52 million people) had pre-existing conditions in 2016.
Current U.S. federal regulation:
Patient Protection and Affordable Care Act (Pub.L. 111-148) enacted March 23, 2010
Click on any of the following blue hyperlinks for more about Pre-existing Conditions:
Together with the Health Care and Education Reconciliation Act of 2010 amendment, it represents the U.S. healthcare system's most significant regulatory overhaul and expansion of coverage since the passage of Medicare and Mediacid in 1965.
ACA's major provisions came into force in 2014. By 2016, the uninsured share of the population had roughly halved, with estimates ranging from 20 to 24 million additional people covered. The law also enacted a host of delivery system reforms intended to constrain healthcare costs and improve quality. After the law went into effect, increases in overall healthcare spending slowed, including premiums for employer-based insurance plans.
The increased coverage was due, roughly equally, to an expansion of Medicaid eligibility and to changes to individual insurance markets. Both received new spending, funded through a combination of new taxes and cuts to Medicare provider rates and Medicare Advantage.
Several Congressional Budget Office reports said that overall these provisions reduced the budget deficit, that repealing ACA would increase the deficit, and that the law reduced income inequality by taxing primarily the top 1% to fund roughly $600 in benefits on average to families in the bottom 40% of the income distribution.
The act largely retained the existing structure of Medicare, Medicaid and the employer market, but individual markets were radically overhauled. Insurers were made to accept all applicants without charging based on pre-existing conditions (see next topic below) or demographic status (except age). To combat the resultant adverse selection, the act mandated that individuals buy insurance (or pay a fine/tax) and that insurers cover a list of "essential health benefits".
Before and after enactment ACA faced strong political opposition, calls for repeal and legal challenges. In National Federation of Independent Business v. Sebelius, the Supreme Court ruled that states could choose not to participate in ACA's Medicaid expansion, although it upheld the law as a whole.
The federal health exchange, HealthCare.gov, faced major technical problems at the beginning of its rollout in 2013. Polls initially found that a plurality of Americans opposed the act, although its individual provisions were generally more popular and the law gained majority support by 2017.
The federal tax penalty for violating the individual mandate of the ACA was rescinded by President Donald Trump through the Tax Cuts and Jobs Act of 2017, starting in 2019. This raised questions about whether the Affordable Care Act was still constitutional.
Click on any of the following blue hyperlinks for more about the Affordable Care Act:
- Provisions
- Insurance regulations: individual policies
- Individual mandate
- Premium subsidies
- Exchanges
- Cost-sharing reduction subsidies
- Risk management
- Medicaid expansion
- Medicare savings
- Taxes
- SCHIP
- Dependents
- Employer mandate
- Delivery system reforms
- Medicare drug benefit (Part D)
- State waivers
- Other insurance provisions
- Nutrition labeling requirements
- Legislative history
- Impact
- Attempted repeals
- Public opinion
- Political aspects
- Criticism and opposition
- Implementation
- See also:
- Comparison of the health care systems in Canada and the United States
- Individual shared responsibility provision
- Massachusetts health care reform (sometimes called "Romneycare")
- Medicaid
- Medicare Access and CHIP Reauthorization Act of 2015 (Reform to the American Health Care system signed into law by President Obama)
- Universal health care
- Universal health coverage by country
- U.S. health care compared with eight other countries (tabular form)
- ACA text:
- Codification in U.S. Code is generally at 42 U.S.C. 18001 et sqq. To read it, start at GPO FDsys by selecting, in the Year menu, the most recent year that lists Title 42. In Title 42, seek section 18001 and subsequent sections.
- Public Law 111–148 after consolidating the amendments made by PPACA Title X and by HCERA.
- Full text, summary, background, provisions and more, via Democratic Policy Committee (Senate.gov)
- Public Law 111–148 U.S. Government Printing Office
Pre-existing condition:
In the context of healthcare in the United States, a pre-existing condition is a medical condition that started before a person's health insurance went into effect.
Before 2014 some insurance policies would not cover expenses due to pre-existing conditions. These exclusions by the insurance industry were meant to cope with adverse selection by potential customers.
Such exclusions have been prohibited since January 1, 2014, by the Patient Protection and Affordable Care Act.
According to the Kaiser Family Foundation, more than a quarter of adults below the age of 65 (approximately 52 million people) had pre-existing conditions in 2016.
Definitions:
The University of Pittsburgh Medical Center defines a pre-existing condition as a "medical condition that occurred before a program of health benefits went into effect".
James Rohack, president of the American Medical Association, has stated on a Fox News Sunday interview that exclusions, based upon these conditions, function as a form of "rationing" of health care.
Conditions can be broken down into two further categories, according to Lisa Smith of Investopedia: Most insurance companies use one of two definitions to identify such conditions.
- Under the "objective standard" definition, a pre-existing condition is any condition for which the patient has already received medical advice or treatment prior to enrollment in a new medical insurance plan.
- Under the broader, "prudent person" definition, a pre-existing condition is anything for which symptoms were present and a prudent person would have sought treatment.
Which definition may be used was sometimes regulated by state laws. Some states required insurance companies to use the objective standard, while others required the prudent person standard. 10 states did not specify either definition, 21 required the "prudent person" standard, and 18 required the "objective" standard.
According to the Kaiser Family Foundation, more than a quarter of adults below the age of 65 (approximately 52 million people) had pre-existing conditions in 2016.
Current U.S. federal regulation:
Patient Protection and Affordable Care Act (Pub.L. 111-148) enacted March 23, 2010
- Immediate reform: effective June 21, 2010 (90 days after enactment)
- National high-risk pool for individuals with a pre-existing condition who have been uninsured for the prior 6 months
- Premium to be set at a standard rate for a standard population
- Premium for older individuals allowed to be up to 4 times the premium for younger individuals
- Premium for tobacco users allowed to be up to 1.5 times the premium for non-tobacco users
- National high-risk pool for individuals with a pre-existing condition who have been uninsured for the prior 6 months
- Immediate reform: effective September 23, 2010 (6 months after enactment)
- Group health insurance plans and new (non-grandfathered) individual health insurance plans
- Pre-existing condition exclusions prohibited for children under age 19
- Group health insurance plans and new (non-grandfathered) individual health insurance plans
- Reform delayed for 4 years: effective January 1, 2014
- Individual and group health insurance plans
- Pre-existing condition exclusions prohibited in all health insurance plans
- Prohibit treating acts of domestic violence as a pre-existing condition
- Waiting period for enrollment in new health insurance plans limited to 90 days
- Grandfathered existing health insurance plans must prohibit pre-existing condition exclusions by January 1, 2014
- Individual and group health insurance plans
Click on any of the following blue hyperlinks for more about Pre-existing Conditions:
- Former regulation
- Practice and effect
- Commentary by lawmakers
- Public opinion
- Pre-existing Condition Insurance Plan
Single-payer Health Care
- YouTube Video: What is Single-payer Health Care?
- YouTube Video: Why Medical Bills In The US Are So Expensive
- YouTube Video: How Germany's Universal Health-Care System Works
Single-payer healthcare is a type of universal healthcare in which the costs of essential healthcare for all residents are covered by a single public system (hence 'single-payer').
Single-payer systems may contract for healthcare services from private organizations (as is the case in Canada) or may own and employ healthcare resources and personnel (as is the case in the United Kingdom). "Single-payer" describes the mechanism by which healthcare is paid for by a single public authority, not a private authority, nor a mix of both.
Description:
Within single-payer healthcare systems, a single government or government-related source pays for all covered healthcare services. Governments use this strategy to achieve several goals, including universal healthcare, decreased economic burden of health care, and improved health outcomes for the population.
In 2010, the World Health Organization's member countries adopted universal healthcare as a goal; this goal was also adopted by the United Nations General Assembly in 2015 as part of the 2030 Agenda for Sustainable Development.
A single-payer health system establishes a single risk pool, consisting of the entire population of a geographic or political region. It also establishes a single set of rules for services offered, reimbursement rates, drug prices, and minimum standards for required services.
In wealthy nations, single-payer health insurance is typically available to all citizens and legal residents. Examples include the United Kingdom's National Health Service, Australia's Medicare, Canada's Medicare, and Taiwan's National Health Insurance.
History of the term:
The term was coined in the 1990s to characterize the differences between the Canadian healthcare system with those such as the United Kingdom's NHS. In the Canadian healthcare system, the government pays private agencies to provide healthcare for qualifying individuals. In other systems, the government both funds and delivers care.
Typically, "single-payer healthcare" refers to health insurance provided as a public service and offered to citizens and legal residents; it does not usually refer to delivery of healthcare services. The fund can be managed by the government directly or as a publicly owned and regulated agency.
Single-payer contrasts with other funding mechanisms like 'multi-payer' (multiple public and/or private sources), 'two-tiered' (defined either as a public source with the option to use qualifying private coverage as a substitute, or as a public source for catastrophic care backed by private insurance for common medical care), and 'insurance mandate' (citizens are required to buy private insurance which meets a national standard and which is generally subsidized). Some systems combine elements of these four funding mechanisms.
In contrast to the standard usage of the term, some writers describe all publicly administered systems as "single-payer plans," and others have described any system of healthcare which intends to cover the entire population, such as voucher plans, as "single-payer plans," although these usages generally don't meet strict definitions of the term.
Click on any of the following blue hyperlinks for more about Single Payer Health Insurance:
Single-payer systems may contract for healthcare services from private organizations (as is the case in Canada) or may own and employ healthcare resources and personnel (as is the case in the United Kingdom). "Single-payer" describes the mechanism by which healthcare is paid for by a single public authority, not a private authority, nor a mix of both.
Description:
Within single-payer healthcare systems, a single government or government-related source pays for all covered healthcare services. Governments use this strategy to achieve several goals, including universal healthcare, decreased economic burden of health care, and improved health outcomes for the population.
In 2010, the World Health Organization's member countries adopted universal healthcare as a goal; this goal was also adopted by the United Nations General Assembly in 2015 as part of the 2030 Agenda for Sustainable Development.
A single-payer health system establishes a single risk pool, consisting of the entire population of a geographic or political region. It also establishes a single set of rules for services offered, reimbursement rates, drug prices, and minimum standards for required services.
In wealthy nations, single-payer health insurance is typically available to all citizens and legal residents. Examples include the United Kingdom's National Health Service, Australia's Medicare, Canada's Medicare, and Taiwan's National Health Insurance.
History of the term:
The term was coined in the 1990s to characterize the differences between the Canadian healthcare system with those such as the United Kingdom's NHS. In the Canadian healthcare system, the government pays private agencies to provide healthcare for qualifying individuals. In other systems, the government both funds and delivers care.
Typically, "single-payer healthcare" refers to health insurance provided as a public service and offered to citizens and legal residents; it does not usually refer to delivery of healthcare services. The fund can be managed by the government directly or as a publicly owned and regulated agency.
Single-payer contrasts with other funding mechanisms like 'multi-payer' (multiple public and/or private sources), 'two-tiered' (defined either as a public source with the option to use qualifying private coverage as a substitute, or as a public source for catastrophic care backed by private insurance for common medical care), and 'insurance mandate' (citizens are required to buy private insurance which meets a national standard and which is generally subsidized). Some systems combine elements of these four funding mechanisms.
In contrast to the standard usage of the term, some writers describe all publicly administered systems as "single-payer plans," and others have described any system of healthcare which intends to cover the entire population, such as voucher plans, as "single-payer plans," although these usages generally don't meet strict definitions of the term.
Click on any of the following blue hyperlinks for more about Single Payer Health Insurance:
- Countries with single-payer systems
- Regions with 'Beveridge Model' systems
- Regions with hybrid single-payer/private insurance systems
- See also:
- All-payer rate setting
- Health care reform debate in the United States
- International comparisons of health care systems – tabular comparisons of the US, Canada, and other countries not shown above.
- National health insurance
- Public health insurance option ("the public option")
- Medical Deserts in the United States
Preventive Health Care
- YouTube Video: Keeping Healthy People Healthy: Practice Preventive Medicine
- YouTube Video: Quality Improvement in Healthcare
- YouTube Video: Improving Healthcare: Straight from the Heart | Sanjay Saint | TEDxUofM
Preventive healthcare, or prophylaxis, consists of measures taken for disease prevention. Disease and disability are affected by environmental factors, genetic predisposition, disease agents, and lifestyle choices and are dynamic processes which begin before individuals realize they are affected.
Disease prevention relies on anticipatory actions that can be categorized as primal, primary, secondary, and tertiary prevention.
Each year, millions of people die of preventable deaths. A 2004 study showed that about half of all deaths in the United States in 2000 were due to preventable behaviors and exposures.
Leading causes included cardiovascular disease, chronic respiratory disease, unintentional injuries, diabetes, and certain infectious diseases. This same study estimates that 400,000 people die each year in the United States due to poor diet and a sedentary lifestyle.
According to estimates made by the World Health Organization (WHO), about 55 million people died worldwide in 2011, two thirds of this group from non-communicable diseases, including cancer, diabetes, and chronic cardiovascular and lung diseases. This is an increase from the year 2000, during which 60% of deaths were attributed to these diseases.
Preventive healthcare is especially important given the worldwide rise in prevalence of chronic diseases and deaths from these diseases.
There are many methods for prevention of disease. One of them is prevention of teenage smoking through information giving.
It is recommended that adults and children aim to visit their doctor for regular check-ups, even if they feel healthy, to perform disease screening, identify risk factors for disease, discuss tips for a healthy and balanced lifestyle, stay up to date with immunizations and boosters, and maintain a good relationship with a healthcare provider.
Some common disease screenings include checking for :
Genetic testing can also be performed to screen for mutations that cause genetic disorders or predisposition to certain diseases such as breast or ovarian cancer. However, these measures are not affordable for every individual and the cost effectiveness of preventive healthcare is still a topic of debate.
Levels of prevention:
Preventive healthcare strategies are described as taking place at the primal, primary, secondary, and tertiary prevention levels.
Although advocated as preventive medicine in the early twentieth century by Sara Josephine Baker, in the 1940s, Hugh R. Leavell and E. Gurney Clark coined the term primary prevention.
They worked at the Harvard and Columbia University Schools of Public Health, respectively, and later expanded the levels to include secondary and tertiary prevention. Goldston (1987) notes that these levels might be better described as "prevention, treatment, and rehabilitation", although the terms primary, secondary, and tertiary prevention are still in use today.
The concept of primal prevention has been created much more recently, in relation to the new developments in molecular biology over the last fifty years, more particularly in epigenetics, which point to the paramount importance of environmental conditions - both physical and affective - on the organism during its fetal and newborn life (or so-called primal period of life). The last of which has often ignored potential negative impacts on human rights and quality of lifez'
Primal and primordial prevention:
Primal prevention has been propounded as a separate category of health promotion. This health promotion par excellence is based on knowledge in molecular biology, in particular on epigenetics, which points to how much affective as well as physical environment during fetal and newborn life may determine adult health.
This way of promoting health consists mainly in providing future parents with pertinent, unbiased information on primal health and supporting them during their child's primal period of life (i.e., "from conception to first anniversary" according to definition by the Primal Health Research Centre, London). This includes adequate parental leave ideally for both parents with kin caregiving and financial help where needed.
Primordial prevention refers to all measures designed to prevent the development of risk factors in the first place, early in life, and even preconception, as Ruth Etzel has described it "all population-level actions and measures that inhibit the emergence and establishment of adverse environmental, economic, and social conditions". This could be reducing air pollution or prohibiting endocrine-disrupting chemicals in food-handling equipment and food contact materials.
Primary prevention:
Primary prevention consists of traditional health promotion and "specific protection." Health promotion activities are current, non-clinical life choices such as, eating nutritious meals and exercising daily, that both prevent disease and create a sense of overall well-being. Preventing disease and creating overall well-being, prolongs life expectancy.
Health-promotional activities do not target a specific disease or condition but rather promote health and well-being on a very general level. On the other hand, specific protection targets a type or group of diseases and complements the goals of health promotion.
Food is the most basic tool in preventive health care. The 2011 National Health Interview Survey performed by the Centers for Disease Control was the first national survey to include questions about ability to pay for food. Difficulty with paying for food, medicine, or both is a problem facing 1 out of 3 Americans. If better food options were available through food banks, soup kitchens, and other resources for low-income people, obesity and the chronic conditions that come along with it would be better controlled.
A food desert is an area with restricted access to healthy foods due to a lack of supermarkets within a reasonable distance. These are often low-income neighborhoods with the majority of residents lacking transportation. There have been several grassroots movements since 1995 to encourage urban gardening, using vacant lots to grow food cultivated by local residents. Mobile fresh markets are another resource for residents in a "food desert", which are specially outfitted buses bringing affordable fresh fruits and vegetables to low-income neighborhoods.
Scientific advancements in genetics have contributed to the knowledge of hereditary diseases and have facilitated progress in specific protective measures in individuals who are carriers of a disease gene or have an increased predisposition to a specific disease.
Genetic testing has allowed physicians to make quicker and more accurate diagnoses and has allowed for tailored treatments or personalized medicine. Similarly, specific protective measures such as water purification, sewage treatment, and the development of personal hygienic routines (such as regular hand-washing, safe sex to prevent sexually transmitted infections) became mainstream upon the discovery of infectious disease agents and have decreased the rates of communicable diseases which are spread in unsanitary conditions.
Secondary prevention:
Secondary prevention deals with latent diseases and attempts to prevent an asymptomatic disease from progressing to symptomatic disease. Certain diseases can be classified as primary or secondary. This depends on definitions of what constitutes a disease, though, in general, primary prevention addresses the root cause of a disease or injury whereas secondary prevention aims to detect and treat a disease early on.
Secondary prevention consists of "early diagnosis and prompt treatment" to contain the disease and prevent its spread to other individuals, and "disability limitation" to prevent potential future complications and disabilities from the disease. For example, early diagnosis and prompt treatment for a syphilis patient would include a course of antibiotics to destroy the pathogen and screening and treatment of any infants born to syphilitic mothers.
Disability limitation for syphilitic patients includes continued check-ups on the heart, cerebrospinal fluid, and central nervous system of patients to curb any damaging effects such as blindness or paralysis.
Tertiary prevention:
Finally, tertiary prevention attempts to reduce the damage caused by symptomatic disease by focusing on mental, physical, and social rehabilitation. Unlike secondary prevention, which aims to prevent disability, the objective of tertiary prevention is to maximize the remaining capabilities and functions of an already disabled patient.
Goals of tertiary prevention include: preventing pain and damage, halting progression and complications from disease, and restoring the health and functions of the individuals affected by disease.
For syphilitic patients, rehabilitation includes measures to prevent complete disability from the disease, such as implementing work-place adjustments for the blind and paralyzed or providing counseling to restore normal daily functions to the greatest extent possible.
Leading causes of preventable death:
United States:
The leading cause of death in the United States was tobacco. However, poor diet and lack of exercise may soon surpass tobacco as a leading cause of death. These behaviors are modifiable and public health and prevention efforts could make a difference to reduce these deaths.
Leading causes of preventable deaths in the United States in the year 2000:
Worldwide:
The leading causes of preventable death worldwide share similar trends to the United States. There are a few differences between the two, such as malnutrition, pollution, and unsafe sanitation, that reflect health disparities between the developing and developed world.
Leading causes of preventable death worldwide as of the year 2001:
Deaths caused (in millions per year):
Click on any of the following blue hyperlinks for more about Preventive Healthcare:
Disease prevention relies on anticipatory actions that can be categorized as primal, primary, secondary, and tertiary prevention.
Each year, millions of people die of preventable deaths. A 2004 study showed that about half of all deaths in the United States in 2000 were due to preventable behaviors and exposures.
Leading causes included cardiovascular disease, chronic respiratory disease, unintentional injuries, diabetes, and certain infectious diseases. This same study estimates that 400,000 people die each year in the United States due to poor diet and a sedentary lifestyle.
According to estimates made by the World Health Organization (WHO), about 55 million people died worldwide in 2011, two thirds of this group from non-communicable diseases, including cancer, diabetes, and chronic cardiovascular and lung diseases. This is an increase from the year 2000, during which 60% of deaths were attributed to these diseases.
Preventive healthcare is especially important given the worldwide rise in prevalence of chronic diseases and deaths from these diseases.
There are many methods for prevention of disease. One of them is prevention of teenage smoking through information giving.
It is recommended that adults and children aim to visit their doctor for regular check-ups, even if they feel healthy, to perform disease screening, identify risk factors for disease, discuss tips for a healthy and balanced lifestyle, stay up to date with immunizations and boosters, and maintain a good relationship with a healthcare provider.
Some common disease screenings include checking for :
- hypertension (high blood pressure),
- hyperglycemia (high blood sugar, a risk factor for diabetes mellitus),
- hypercholesterolemia (high blood cholesterol),
- screening for:
- colon cancer,
- depression,
- HIV
- and other common types of sexually transmitted disease such as chlamydia, syphilis, and gonorrhea,
- mammography (to screen for breast cancer),
- colorectal cancer screening,
- a Pap test (to check for cervical cancer),
- and screening for osteoporosis.
Genetic testing can also be performed to screen for mutations that cause genetic disorders or predisposition to certain diseases such as breast or ovarian cancer. However, these measures are not affordable for every individual and the cost effectiveness of preventive healthcare is still a topic of debate.
Levels of prevention:
Preventive healthcare strategies are described as taking place at the primal, primary, secondary, and tertiary prevention levels.
Although advocated as preventive medicine in the early twentieth century by Sara Josephine Baker, in the 1940s, Hugh R. Leavell and E. Gurney Clark coined the term primary prevention.
They worked at the Harvard and Columbia University Schools of Public Health, respectively, and later expanded the levels to include secondary and tertiary prevention. Goldston (1987) notes that these levels might be better described as "prevention, treatment, and rehabilitation", although the terms primary, secondary, and tertiary prevention are still in use today.
The concept of primal prevention has been created much more recently, in relation to the new developments in molecular biology over the last fifty years, more particularly in epigenetics, which point to the paramount importance of environmental conditions - both physical and affective - on the organism during its fetal and newborn life (or so-called primal period of life). The last of which has often ignored potential negative impacts on human rights and quality of lifez'
Primal and primordial prevention:
Primal prevention has been propounded as a separate category of health promotion. This health promotion par excellence is based on knowledge in molecular biology, in particular on epigenetics, which points to how much affective as well as physical environment during fetal and newborn life may determine adult health.
This way of promoting health consists mainly in providing future parents with pertinent, unbiased information on primal health and supporting them during their child's primal period of life (i.e., "from conception to first anniversary" according to definition by the Primal Health Research Centre, London). This includes adequate parental leave ideally for both parents with kin caregiving and financial help where needed.
Primordial prevention refers to all measures designed to prevent the development of risk factors in the first place, early in life, and even preconception, as Ruth Etzel has described it "all population-level actions and measures that inhibit the emergence and establishment of adverse environmental, economic, and social conditions". This could be reducing air pollution or prohibiting endocrine-disrupting chemicals in food-handling equipment and food contact materials.
Primary prevention:
Primary prevention consists of traditional health promotion and "specific protection." Health promotion activities are current, non-clinical life choices such as, eating nutritious meals and exercising daily, that both prevent disease and create a sense of overall well-being. Preventing disease and creating overall well-being, prolongs life expectancy.
Health-promotional activities do not target a specific disease or condition but rather promote health and well-being on a very general level. On the other hand, specific protection targets a type or group of diseases and complements the goals of health promotion.
Food is the most basic tool in preventive health care. The 2011 National Health Interview Survey performed by the Centers for Disease Control was the first national survey to include questions about ability to pay for food. Difficulty with paying for food, medicine, or both is a problem facing 1 out of 3 Americans. If better food options were available through food banks, soup kitchens, and other resources for low-income people, obesity and the chronic conditions that come along with it would be better controlled.
A food desert is an area with restricted access to healthy foods due to a lack of supermarkets within a reasonable distance. These are often low-income neighborhoods with the majority of residents lacking transportation. There have been several grassroots movements since 1995 to encourage urban gardening, using vacant lots to grow food cultivated by local residents. Mobile fresh markets are another resource for residents in a "food desert", which are specially outfitted buses bringing affordable fresh fruits and vegetables to low-income neighborhoods.
Scientific advancements in genetics have contributed to the knowledge of hereditary diseases and have facilitated progress in specific protective measures in individuals who are carriers of a disease gene or have an increased predisposition to a specific disease.
Genetic testing has allowed physicians to make quicker and more accurate diagnoses and has allowed for tailored treatments or personalized medicine. Similarly, specific protective measures such as water purification, sewage treatment, and the development of personal hygienic routines (such as regular hand-washing, safe sex to prevent sexually transmitted infections) became mainstream upon the discovery of infectious disease agents and have decreased the rates of communicable diseases which are spread in unsanitary conditions.
Secondary prevention:
Secondary prevention deals with latent diseases and attempts to prevent an asymptomatic disease from progressing to symptomatic disease. Certain diseases can be classified as primary or secondary. This depends on definitions of what constitutes a disease, though, in general, primary prevention addresses the root cause of a disease or injury whereas secondary prevention aims to detect and treat a disease early on.
Secondary prevention consists of "early diagnosis and prompt treatment" to contain the disease and prevent its spread to other individuals, and "disability limitation" to prevent potential future complications and disabilities from the disease. For example, early diagnosis and prompt treatment for a syphilis patient would include a course of antibiotics to destroy the pathogen and screening and treatment of any infants born to syphilitic mothers.
Disability limitation for syphilitic patients includes continued check-ups on the heart, cerebrospinal fluid, and central nervous system of patients to curb any damaging effects such as blindness or paralysis.
Tertiary prevention:
Finally, tertiary prevention attempts to reduce the damage caused by symptomatic disease by focusing on mental, physical, and social rehabilitation. Unlike secondary prevention, which aims to prevent disability, the objective of tertiary prevention is to maximize the remaining capabilities and functions of an already disabled patient.
Goals of tertiary prevention include: preventing pain and damage, halting progression and complications from disease, and restoring the health and functions of the individuals affected by disease.
For syphilitic patients, rehabilitation includes measures to prevent complete disability from the disease, such as implementing work-place adjustments for the blind and paralyzed or providing counseling to restore normal daily functions to the greatest extent possible.
Leading causes of preventable death:
United States:
The leading cause of death in the United States was tobacco. However, poor diet and lack of exercise may soon surpass tobacco as a leading cause of death. These behaviors are modifiable and public health and prevention efforts could make a difference to reduce these deaths.
Leading causes of preventable deaths in the United States in the year 2000:
- Tobacco smoking (caused 435,000 deaths, or18.1% of all deaths.
- Poor diet and physical inactivity (caused 400,000 deaths, or 6.6% of all deaths)
- Alcohol consumption (Caused 85,000 deaths, or 3.5% of all deaths)
- Infectious diseases(Caused 75,000 deaths, or 3.1% of all deaths)
- Toxicants (Caused 55,000 deaths, or 2.3% of all deaths)
- Traffic collisions (Caused 43,000 deaths, or 1.8% of all deaths)
- Firearm incidents (Caused 29,000 deaths, or 1.2% of all deaths)
- Sexually transmitted infections (Caused 20,0000 deaths, or 0.8% of all deaths)
- Drug abuse (Caused 17,000 deaths, or 0.7% of all deaths)
Worldwide:
The leading causes of preventable death worldwide share similar trends to the United States. There are a few differences between the two, such as malnutrition, pollution, and unsafe sanitation, that reflect health disparities between the developing and developed world.
Leading causes of preventable death worldwide as of the year 2001:
Deaths caused (in millions per year):
- Hypertension (7.8 million per year)
- Smoking (5.0 million per year)
- High cholesterol (3.9 million per year)
- Malnutrition (3.8 million per year)
- Sexually transmitted infections (3.0 million per year)
- Poor diet (2.8 million per year)
- Overweight and obesity (2.5 million per year)
- Physical inactivity (2.0 million per year)
- Alcohol (1.9 million per year)
- Indoor air pollution from solid fuels (1.8 million per year)
- Unsafe water and poor sanitation (1.6 million per year)
Click on any of the following blue hyperlinks for more about Preventive Healthcare:
- Child mortality
- Preventive methods
- Health disparities and barriers to accessing care
- Economics of lifestyle-based prevention
- Effectiveness
- See also:
- American Board of Preventive Medicine
- American Journal of Preventive Medicine
- American Osteopathic Board of Preventive Medicine
- Mental illness prevention
- Public health
- Pre-exposure prophylaxis
- Preventive Medicine (journal)
- Primary Health Care
- Treatment as prevention
- United States Preventive Services Task Force (USPSTF)
- Canadian Task Force on Preventive Health Care (CTFPHC)
- European Centre for Disease Prevention and Control (ECDC)
Healthcare in the United States
- YouTube Video: The real reason American health care is so expensive
- YouTube Video: Swedish Healthcare vs. US Healthcare!!
- YouTube Video: Health Care in the United States vs. the World
Healthcare in the United States is far outspent than any other nation, measured both in per capita spending and as a percentage of GDP. Despite this, the country has significantly worse healthcare outcomes when compared to peer nations. The US is the only developed nation without a system of universal healthcare, with a large proportion of its population not carrying health insurance, a substantial factor in the country's excess mortality.
Healthcare is provided by many distinct organizations, made up of insurance companies, healthcare providers, hospital systems, and independent providers. Healthcare facilities are largely owned and operated by private sector businesses. 58% of community hospitals in the US are nonprofit, 21% are government-owned, and 21% are for-profit.
According to the World Health Organization (WHO), the US spent $9,403 (equivalent to $10,738 in 2021) on healthcare per capita, and 17.9% on healthcare as percentage of its GDP in 2014.
Healthcare coverage is provided through a combination of private health insurance and public health coverage (e.g., Medicare, Medicaid). In 2013, 64% of health spending was paid for by the government, and funded via programs such as Medicare, Medicaid, the Children's Health Insurance Program, Tricare, and the Veterans Health Administration.
People aged under 65 acquire insurance via their or a family member's employer, by purchasing health insurance on their own, getting government and/or other assistance based on income or another condition, or are uninsured. Health insurance for public sector employees is primarily provided by the government in its role as employer.
Managed care, where payers use various techniques intended to improve quality and limit cost, has become ubiquitous. The US life expectancy is 78.6 years at birth, up from 75.2 years in 1990; this ranks 42nd among 224 nations, and 22nd out of the 35 industrialized OECD countries, down from 20th in 1990.
In 2016 and 2017, life expectancy in the US dropped for the first time since 1993. Of 17 high-income countries studied by the National Institutes of Health, the US in 2013 had the highest or near-highest prevalence of obesity, car accidents, infant mortality, heart and lung disease, sexually transmitted infections, adolescent pregnancies, injuries, and homicides.
A 2017 survey of the healthcare systems of 11 developed countries found the US healthcare system to be the most expensive and worst-performing in terms of health access, efficiency, and equity. In a 2018 study, the US ranked 29th in healthcare access and quality.
The rate of adults uninsured for healthcare peaked at 18.0% in 2013 prior to the Affordable Care Act (ACA) mandate, fell to 10.9% in the third quarter of 2016, and stood at 13.7% in the fourth quarter of 2018, based on surveys by the Gallup organization beginning in 2008.
At over 27 million, the number of people without health insurance coverage in the US is one of the primary concerns raised by advocates of healthcare reform. A 2009 study done at Harvard Medical School with Cambridge Health Alliance by cofounders of Physicians for a National Health Program, a pro-single payer lobbying group, showed that nearly 45,000 annual deaths are associated with a lack of patient health insurance.
The study also found that uninsured, working Americans have an approximately 40% higher mortality risk compared to privately insured working Americans. In 2010, the ACA (formally known as the "Patient Protection and Affordable Care Act" and commonly known as "Obamacare") became law, enacting major changes in health insurance.
The Supreme Court of the US upheld the constitutionality of most of the law in June 2012 and affirmed insurance exchange subsidies in all states in June 2015.
The Human Rights Measurement Initiative finds that the US is achieving 81.3% of what should be possible at their income level for fulfilling the right to health.
At the same time, the United States is the leader in medical innovation, measured either in terms of revenue or the number of new drugs and devices introduced.
History:
Main articles:
In the US, dissimilar to the European nationalized health insurance plans, the market created a private employment-based system. Following the Stabilization Act of 1942, employers, unable to provide higher salaries to attract or retain employees, began to offer insurance plans, including healthcare packages, as a fringe benefit, thereby beginning the practice of employer-sponsored health insurance.
Statistics:
Hospitalizations:
According to a statistical brief by the Healthcare Cost and Utilization Project (HCUP), there were 35.7 million hospitalizations in 2016, a significant decrease from the 38.6 million in 2011.
For every 1,000 in the population, there was an average of 104.2 stays and each stay averaged $11,700 (equivalent to $13,210 in 2021, an increase from the $10,400 (equivalent to $12,275 in 2021) cost per stay in 2012. 7.6% of the population had overnight stays in 2017, each stay lasting an average of 4.6 days.
A study by the National Institutes of Health reported that the lifetime per capita expenditure at birth, using the year 2000 dollars, showed a large difference between the healthcare costs of females ($361,192, equivalent to $568,345 in 2021) and males ($268,679, equivalent to $422,774 in 2021).
A large portion of this cost difference is in the shorter lifespan of men, but, even after adjustment for age (assuming men live as long as women), there still is a 20% difference in lifetime healthcare expenditures.
Health insurance and accessibility:
Main articles:
Unlike most developed nations, the US health system does not provide healthcare to the country's entire population. Instead, most citizens are covered by a combination of private insurance and various federal and state programs.
As of 2017, health insurance was most commonly acquired through a group plan tied to an employer, covering 150 million people. Other major sources include Medicaid, covering 70 million, Medicare, 50 million, and health insurance marketplaces created by the ACA covering around 17 million.
In 2017, a study found that 73% of plans on ACA marketplaces had narrow networks, limiting access and choice in providers.
Measures of accessibility and affordability tracked by national health surveys include:
In 2004, an OECD report noted that "all OECD countries [except Mexico, Turkey, and the US] had achieved universal or near-universal (at least 98.4% insured) coverage of their populations by 1990". The 2004 IOM report also observed that "lack of health insurance causes roughly 18,000 unnecessary deaths every year in the US".
The Gallup organization tracks the percent of adult Americans who are uninsured for healthcare, beginning in 2008. The rate of uninsured peaked at 18.0% in 2013 prior to the ACA mandate, fell to 10.9% in the third quarter of 2016, and stood at 13.7% in the fourth quarter of 2018. "The 2.8-percentage-point increase since that low represents a net increase of about seven million adults without health insurance."
The US Census Bureau reported that 28.5 million people (8.8%) did not have health insurance in 2017, down from 49.9 million (16.3%) in 2010. Between 2004 and 2013, a trend of high rates of underinsurance and wage stagnation contributed to a healthcare consumption decline for low-income Americans. This trend was reversed after the implementation of the major provisions of the ACA in 2014.
As of 2017, the possibility that the ACA may be repealed or replaced has intensified interest in the questions of whether and how health insurance coverage affects health and mortality. Several studies have indicated that there is an association with expansion of the ACA and factors associated with better health outcomes such as having a regular source of care and the ability to afford care.
A 2016 study concluded that an approximately 60% increased ability to afford care can be attributed to Medicaid expansion provisions enacted by the Patient Protection and Affordable Care Act.
Additionally, an analysis of changes in mortality post Medicaid expansion suggests that Medicaid saves lives at a relatively more cost effective rate of a societal cost of $327,000 to $867,000 (equivalent to $369,213 to $978,921 in 2021) per life saved compared to other public policies which cost an average of $7.6 million (equivalent to $8.58 million in 2021) per life.
A 2009 study in five states found that medical debt contributed to 46.2% of all personal bankruptcies, and 62.1% of bankruptcy filers claimed high medical expenses in 2007. Since then, health costs and the numbers of uninsured and underinsured have increased. A 2013 study found that about 25% of all senior citizens declare bankruptcy due to medical expenses.
In practice, the uninsured are often treated, but the cost is covered through taxes and other fees which shift the cost. Forgone medical care due to extensive cost sharing may ultimately increase costs due to downstream medical issues; this dynamic may play a part in US's international ranking as having the highest healthcare expenditures despite significant patient cost-sharing.
Those who are insured may be underinsured such that they cannot afford adequate medical care. A 2003 study estimated that 16 million US adults were underinsured, disproportionately affecting those with lower incomes—73% of the underinsured in the study population had annual incomes below 200% of the federal poverty level.
Lack of insurance or higher cost sharing (user fees for the patient with insurance) create barriers to accessing healthcare: use of care declines with increasing patient cost-sharing obligation. Before the ACA passed in 2014, 39% of below-average income Americans reported forgoing seeing a doctor for a medical issue (whereas 7% of low-income Canadians and 1% of low-income British citizens reported the same).
Health in the US in global context:
In 2019, the under-five child mortality rate was 6.5 deaths per 1000 live births, placing the US 33rd of 37 OECD countries. In 2010–2012, more than 57,000 infants (52%) and children under 18 years died in the US.
While not as high in 2015 as in 2013 (18.5), maternal deaths related to childbirth have shown recent increases; in 1987, the mortality ratio was 7.2 per 100,000. As of 2015, the US rate is double the maternal mortality rate in Belgium or Canada, and more than triple the rate in the Finland as well as several other Western European countries.
Life expectancy at birth for a child born in the US in 2015 is 81.2 (females) or 76.3 (males) years. According to the WHO, life expectancy in the US is 31st in the world (out of 183 countries) as of 2015. The US's average life expectancy (both sexes) is just over 79. Japan ranks first with an average life expectancy of nearly 84 years. The US ranks lower (36th) when considering health-adjusted life expectancy (HALE) at just over 69 years.
Another source, the Central Intelligence Agency, indicates life expectancy at birth in the US is 79.8, ranking it 42nd in the world. Monaco is first on this list of 224, with an average life expectancy of 89.5.
A 2013 National Research Council study stated that, when considered as one of 17 high-income countries, the US was at or near the top in:
Together, such issues place the US at the bottom of the list for life expectancy in high-income countries. Females born in the US in 2015 have a life expectancy of 81.6 years, and males 76.9 years; more than three years less and as much as over five years less than people born in Switzerland (85.3 F, 81.3 M) or Japan (86.8 F, 80.5 M) in 2015.
Causes of mortality in the US:
See also: List of causes of death by rate
The top three causes of death among both sexes and all ages in the US have consistently remained cardiovascular diseases (ranked 1st), neoplasms (2nd) and neurological disorders (3rd), since the 1990s.
In 2015, the total number of deaths by heart disease was 633,842, by cancer it was 595,930, and from chronic lower respiratory disease it was 155,041.
In 2015, 267.18 deaths per 100,000 people were caused by cardiovascular diseases, 204.63 by neoplasms and 100.66 by neurological disorders.
Diarrhea, lower respiratory, and other common infections were ranked sixth overall, but had the highest rate of infectious disease mortality in the US at 31.65 deaths per 100,000 people.
There is evidence, however, that a large proportion of health outcomes and early mortality can be attributed to factors other than communicable or non-communicable disease. As a 2013 National Research Council study concluded, more than half the men who die before the age of 50 die due to murder (19%), traffic accidents (18%), and other accidents (16%).
For women, the percentages are different: 53% of women who die before the age of 50 die due to disease, whereas 38% die due to accidents, homicide, and suicide.
Diseases of despair (drug overdoses, alcoholic liver disease, and suicide), which started increasing in the early 1990s, kill roughly 158,000 Americans a year as of 2018.
Since 2020, the Centers for Disease Control and Prevention (CDC) reports that the life expectancy for the US population was 77.0 years, a decrease of 1.8 years from 2019.
Life expectancy fell again in 2021 to 76.4 years, which has been attributed to COVID-19 and rising death rates from suicide, drug overdoses and liver disease.
Providers:
Healthcare providers in the US encompass individual healthcare personnel, healthcare facilities, and medical products.
Facilities:
Main pages:
In the US, ownership of the healthcare system is mainly in private hands, though federal, state, county, and city governments also own certain facilities.
As of 2018, there were 5,534 registered hospitals in the US. There were 4,840 community hospitals, which are defined as nonfederal, short-term general, or specialty hospitals.
The nonprofit hospitals share of total hospital capacity has remained relatively stable (about 70%) for decades. There are also privately owned for-profit hospitals as well as government hospitals in some locations, mainly owned by county and city governments.
The Hill–Burton Act was passed in 1946, which provided federal funding for hospitals in exchange for treating poor patients.
The largest hospital system in 2016 by revenue was HCA Healthcare in 2019, Dignity Health and Catholic Health Initiatives merged into CommonSpirit Health to create the largest by revenue, spanning 21 states.
Integrated delivery systems, where the provider and the insurer share the risk in an attempt to provide value-based healthcare, have grown in popularity. Regional areas have separate healthcare markets, and in some markets competition is limited as the demand from the local population cannot support multiple hospitals.
About two-thirds of doctors practice in small offices with less than seven physicians, with over 80% owned by physicians; these sometimes join groups such as independent practice associations to increase bargaining power.
There is no nationwide system of government-owned medical facilities open to the general public but there are local government-owned medical facilities open to the general public.
The US Department of Defense operates field hospitals as well as permanent hospitals via the Military Health System to provide military-funded care to active military personnel.
The federal Veterans Health Administration operates VA hospitals open only to veterans, though veterans who seek medical care for conditions they did not receive while serving in the military are charged for services.
The Indian Health Service (IHS) operates facilities open only to Native Americans from recognized tribes. These facilities, plus tribal facilities and privately contracted services funded by IHS to increase system capacity and capabilities, provide medical care to tribespeople beyond what can be paid for by any private insurance or other government programs.
Hospitals provide some outpatient care in their emergency rooms and specialty clinics, but primarily exist to provide inpatient care. Hospital emergency departments and urgent care centers are sources of sporadic problem-focused care. Surgicenters are examples of specialty clinics. Hospice services for the terminally ill who are expected to live six months or less are most commonly subsidized by charities and government.
Prenatal, family planning, and dysplasia clinics are government-funded obstetric and gynecologic specialty clinics respectively, and are usually staffed by nurse practitioners. Services, particularly urgent-care services, may also be delivered remotely via telemedicine by providers such as Teladoc.
Besides government and private healthcare facilities, there are also 355 registered free clinics in the US that provide limited medical services. They are considered to be part of the social safety net for those who lack health insurance. Their services may range from more acute care (i.e., STDs, injuries, respiratory diseases) to long term care (i.e. dentistry, counseling). Another component of the healthcare safety net would be federally funded community health centers.
Other healthcare facilities include long-term housing facilities which, as of 2019, there were 15,600 nursing homes across the US, with a large portion of that number being for-profit (69.3%)
In 2022, 19 hospitals filed for bankruptcy, closed, or announced plans to close.
Physicians (M.D. and D.O.):
Main article: Physicians in the United States
Physicians in the US include those trained by the US medical education system, and those that are international medical graduates who have progressed through the necessary steps to acquire a medical license to practice in a state.
This includes going through the three steps of the US Medical Licensing Examination (USMLE).
The American College of Physicians, uses the term "physician" to describe all medical practitioners holding a professional medical degree. In the US, the vast majority of physicians have a Doctor of Medicine (M.D.) degree. Those with Doctor of Osteopathic Medicine (D.O.) degrees get similar training and go through the same MLE steps as MD's and so are also allowed to use the title "physician".
Medical products, research, and development:
As in most other countries, the manufacture and production of pharmaceuticals and medical devices is carried out by private companies. The research and development of medical devices and pharmaceuticals is supported by both public and private sources of funding.
In 2003, research and development expenditures were approximately $95 billion (equivalent to $136 billion in 2021) with $40 billion (equivalent to $57.3 billion in 2021) coming from public sources and $55 billion (equivalent to $78.8 billion in 2021) coming from private sources.
These investments into medical research have made the US the leader in medical innovation, measured either in terms of revenue or the number of new drugs and devices introduced.
In 2016, the research and development spending by pharmaceutical companies in the US was estimated to be around $59 billion (equivalent to $66 billion in 2021). In 2006, the US accounted for three quarters of the world's biotechnology revenues and 82% of world R&D spending in biotechnology.
According to multiple international pharmaceutical trade groups, the high cost of patented drugs in the US has encouraged substantial reinvestment in such research and development.
However, the ACA will force industry to sell medicine at a cheaper price. Due to this, it is possible budget cuts will be made on research and development of human health and medicine in the US.
Healthcare provider employment in the US:
A major impending demographic shift in the US will require the healthcare system to provide more care, as the older population is predicted to increase medical expenses by 5% or more in North America due to the "baby boomers" reaching retirement age.
The overall spending on healthcare has increased since the late 1990s, and not just due to general price raises as the rate of spending is growing faster than the rate of inflation.
Moreover, the expenditure on health services for people over 45 years old is 8.3 times the maximum of that of those under 45 years old.
Alternative medicine:
Other methods of medical treatment are being practiced more frequently than before. This field is labeled Complementary and Alternative Medicine (CAM) and are defined as therapies generally not taught in medical school nor available in hospitals. They include:
Providers of these CAM treatments are sometimes legally considered healthcare providers in the US. Common reasons for seeking these alternative approaches included improving their well-being, engaging in a transformational experience, gaining more control over their own health, or finding a better way to relieve symptoms caused by chronic disease. They aim to treat not just physical illness but fix its underlying nutritional, social, emotional, and spiritual causes.
In a 2008 survey, it was found that 37% of hospitals in the US offer at least one form of CAM treatment, the main reason being patient demand (84% of hospitals). Costs for CAM treatments average $33.9 (equivalent to $44.30 in 2021) with two-thirds being out-of-pocket, according to a 2007 statistical analysis. Moreover, CAM treatments covered 11.2% of total out-of-pocket payments on healthcare.
During 2002 to 2008, spending on CAM was on the rise, but usage has since plateaued to about 40% of adults in the US.
Spending:
Main articles:
The US spends more as a percentage of GDP than similar countries, and this can be explained either through higher prices for services themselves, higher costs to administer the system, or more utilization of these services, or to a combination of these elements.
Healthcare costs rising far faster than inflation have been a major driver for healthcare reform in the US. As of 2016, the US spent $3.3 trillion (equivalent to $3.69 trillion in 2021; 17.9% of GDP), or $10,438 (equivalent to $11,785 in 2021) per person; major categories included 32% on hospital care, 20% on physician and clinical services, and 10% on prescription drugs. In comparison, the United Kingdom spent $3,749 (equivalent to $4,233 in 2021) per person.
In 2018, an analysis concluded that prices and administrative costs were largely the cause of the high costs, including prices for labor, pharmaceuticals, and diagnostics. The combination of high prices and high volume can cause particular expense; in the US, high-margin high-volume procedures include angioplasties, C-sections, knee replacements, and CT and MRI scans; CT and MRI scans also showed higher utilization in the US.
Aggregate US hospital costs were $387.3 billion in 2011—a 63% increase since 1997 (inflation adjusted). Costs per stay increased 47% since 1997, averaging $10,000 in 2011 (equivalent to $12,046 in 2021). As of 2008, public spending accounts for between 45% and 56% of US healthcare spending. Surgical, injury, and maternal and neonatal health hospital visit costs increased by more than 2% each year from 2003–2011.
Further, while average hospital discharges remained stable, hospital costs rose from $9,100 in 2003 (equivalent to $13,405 in 2021) to $10,600 in 2011 (equivalent to $12,769 in 2021) and were projected to be $11,000 by 2013 (equivalent to $12,796 in 2021).
According to the WHO, total healthcare spending in the US was 18% of its GDP in 2011, the highest in the world. The Health and Human Services Department expects that the health share of GDP will continue its historical upward trend, reaching 19% of GDP by 2017.
Of each dollar spent on healthcare in the US:
In 2017, a study estimated that nearly half of hospital-associated care resulted from emergency department visits.
As of 2017, data from 2009–2011 showed that end-of-life care in the last year of life accounted for about 8.5%, and the last three years of life about 16.7%.
As of 2013, administration of healthcare constituted 30% of US healthcare costs. Free-market advocates claim that the healthcare system is "dysfunctional" because the system of third-party payments from insurers removes the patient as a major participant in the financial and medical choices that affect costs.
The Cato Institute claims that because government intervention has expanded insurance availability through programs such as Medicare and Medicaid, this has exacerbated the problem.
According to a study paid for by America's Health Insurance Plans (a Washington lobbyist for the health insurance industry) and carried out by PriceWaterhouseCoopers, increased utilization is the primary driver of rising healthcare costs in the US.
The study cites numerous causes of increased utilization, including:
The study also mentions cost-shifting from government programs to private payers. Low reimbursement rates for Medicare and Medicaid have increased cost-shifting pressures on hospitals and doctors, who charge higher rates for the same services to private payers, which eventually affects health insurance rates.
In March 2010, Massachusetts released a report on the cost drivers which it called "unique in the nation". The report noted that providers and insurers negotiate privately, and therefore the prices can vary between providers and insurers for the same services, and it found that the variation in prices did not vary based on quality of care but rather on market leverage; the report also found that price increases rather than increased utilization explained the spending increases in the past several years.
Economists Eric Helland and Alex Tabarrok speculate that the increase in costs of healthcare in the US are largely a result of the Baumol effect. Since healthcare is relatively labor intensive, and productivity in the service sector has lagged that in the goods-producing sector, the costs of those services will rise relative to goods.
Regulation and oversight:
Further information:
Involved organizations and institutions:
Healthcare is subject to extensive regulation at both the federal and the state level, much of which "arose haphazardly". Under this system, the federal government cedes primary responsibility to the states under the McCarran–Ferguson Act.
Essential regulation includes the licensure of healthcare providers at the state level and the testing and approval of pharmaceuticals and medical devices by the Food and Drug Administration (FDA), and laboratory testing. These regulations are designed to protect consumers from ineffective or fraudulent healthcare.
Additionally, states regulate the health insurance market and they often have laws which require that health insurance companies cover certain procedures, although state mandates generally do not apply to the self-funded healthcare plans offered by large employers, which exempt from state laws under preemption clause of the Employee Retirement Income Security Act.
In 2010, the ACA was signed by President Barack Obama and includes various new regulations, with one of the most notable being a health insurance mandate which requires all citizens to purchase health insurance. While not regulation per se, the federal government also has a major influence on the healthcare market through its payments to providers under Medicare and Medicaid, which in some cases are used as a reference point in the negotiations between medical providers and insurance companies.
At the federal level, US Department of Health and Human Services (HHS) oversees the various federal agencies involved in healthcare. The health agencies are a part of the US Public Health Service, and include the:
State governments maintain state health departments, and local governments
(counties and municipalities) often have their own health departments, usually branches of the state health department. Regulations of a state board may have executive and police strength to enforce state health laws. In some states, all members of state boards must be healthcare professionals.
Members of state boards may be assigned by the governor or elected by the state committee. Members of local boards may be elected by the mayor council. The McCarran–Ferguson Act, which cedes regulation to the states, does not itself regulate insurance, nor does it mandate that states regulate insurance.
"Acts of Congress" that do not expressly purport to regulate the "business of insurance" will not preempt state laws or regulations that regulate the "business of insurance". The act also provides that federal anti-trust laws will not apply to the "business of insurance" as long as the state regulates in that area, but federal anti-trust laws will apply in cases of boycott, coercion, and intimidation.
By contrast, most other federal laws will not apply to insurance, whether the states regulate in that area or not.
Self-policing of providers by providers is a major part of oversight. Many healthcare organizations also voluntarily submit to inspection and certification by the Joint Commission on Accreditation of Hospital Organizations (JCAHO).
Providers also undergo testing to obtain board certification attesting to their skills. A report issued by Public Citizen in April 2008 found that, for the third year in a row, the number of serious disciplinary actions against physicians by state medical boards declined from 2006 to 2007, and called for more oversight of the boards.
The federal Centers for Medicare and Medicaid Services (CMS) publishes an online searchable database of performance data on nursing homes.
In 2004, libertarian think tank Cato Institute published a study which concluded that regulation provides benefits in the amount of $170 billion but costs the public up to $340 billion. The study concluded that the majority of the cost differential arises from medical malpractice, FDA regulations, and facilities regulations.
"Certificates of need" for hospitals:
In 1978, the federal government required that all states implement Certificate of Need (CON) programs for cardiac care, meaning that hospitals had to apply and receive certificates prior to implementing the program; the intent was to reduce cost by reducing duplicate investments in facilities.
It has been observed that these certificates could be used to increase costs through weakened competition. Many states removed the CON programs after the federal requirement expired in 1986, but some states still have these programs. Empirical research looking at the costs in areas where these programs have been discontinued have not found a clear effect on costs, and the CON programs could decrease costs because of reduced facility construction or increase costs due to reduced competition.
Licensing of providers:
The American Medical Association (AMA) has lobbied the government to highly limit physician education since 1910, currently at 100,000 doctors per year, which has led to a shortage of doctors.
An even bigger problem may be that the doctors are paid for procedures instead of results.
The AMA has also aggressively lobbied for many restrictions that require doctors to carry out operations that might be carried out by cheaper workforce. For example, in 1995, 36 states banned or restricted midwifery even though it delivers equally safe care to that by doctors.
The regulation lobbied by the AMA has decreased the amount and quality of healthcare, according to the consensus of economists: the restrictions do not add to quality, they decrease the supply of care. Moreover, psychologists, nurses and pharmacists are not allowed to prescribe medicines. Previously nurses were not even allowed to vaccinate the patients without direct supervision by doctors.
36 states require that healthcare workers undergo criminal background checks.
Emergency Medical Treatment and Active Labor Act (EMTALA):
Main article: Emergency Medical Treatment and Active Labor Act
EMTALA, enacted by the federal government in 1986, requires that hospital emergency departments treat emergency conditions of all patients regardless of their ability to pay and is considered a critical element in the "safety net" for the uninsured, but established no direct payment mechanism for such care.
Indirect payments and reimbursements through federal and state government programs have never fully compensated public and private hospitals for the full cost of care mandated by EMTALA. More than half of all emergency care in the US now goes uncompensated.
According to some analyses, EMTALA is an unfunded mandate that has contributed to financial pressures on hospitals in the last 20 years, causing them to consolidate and close facilities, and contributing to emergency room overcrowding.
According to the Institute of Medicine, between 1993 and 2003, emergency room visits in the US grew by 26%, while in the same period, the number of emergency departments declined by 425.
Mentally ill patients present a unique challenge for emergency departments and hospitals. In accordance with EMTALA, mentally ill patients who enter emergency rooms are evaluated for emergency medical conditions. Once mentally ill patients are medically stable, regional mental health agencies are contacted to evaluate them.
Patients are evaluated as to whether they are a danger to themselves or others. Those meeting this criterion are admitted to a mental health facility to be further evaluated by a psychiatrist. Typically, mentally ill patients can be held for up to 72 hours, after which a court order is required.
Quality assurance:
See also: Hospital Quality Incentive Demonstration
Healthcare quality assurance consists of the "activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps."
Private companies such as Grand Rounds also release quality information and offer services to employers and plans to map quality within their networks.
One innovation in encouraging quality of healthcare is the public reporting of the performance of hospitals, health professionals or providers, and healthcare organizations.
However, there is "no consistent evidence that the public release of performance data changes consumer behaviour or improves care".
Overall system effectiveness:
Measures of effectiveness:
The US healthcare delivery system unevenly provides medical care of varying quality to its population. In a highly effective healthcare system, individuals would receive reliable care that meets their needs and is based on the best scientific knowledge available.
In order to monitor and evaluate system effectiveness, researchers and policy makers track system measures and trends over time. The HHS populates a publicly available dashboard called the Health System Measurement Project (healthmeasures.aspe.hhs.gov), to ensure a robust monitoring system.
The dashboard captures the access, quality and cost of care; overall population health; and health system dynamics (e.g., workforce, innovation, health information technology).
Included measures align with other system performance measuring activities, include the following:
Waiting times:
Waiting times in US healthcare are usually short, but are not usually 0 for non-urgent care at least. Also, a minority of US patients wait longer than is perceived. In a 2010 Commonwealth Fund survey, most Americans self-reported waiting less than four weeks for their most recent specialist appointment and less than one month for elective surgery.
However, about 30% of patients reported waiting longer than one month for elective surgery, and about 20% longer than four weeks for their most recent specialist appointment.
These percentages were smaller than in France, the UK, New Zealand, and Canada, but not better than Germany and Switzerland (although waits shorter than four weeks/one month may not be equally long across these three countries).
The number of respondents may not be enough to be fully representative. In a study in 1994 comparing Ontario to three regions of the US, self-reported mean wait times to see an orthopedic surgeon were two weeks in those parts of the US, and four weeks in Canada.
Mean waits for the knee or hip surgery were self-reported as three weeks in those parts of the US and eight weeks in Ontario.
However, current waits in both countries' regions may have changed since then (certainly in Canada waiting times went up later).
More recently, at one Michigan hospital, the waiting time for the elective surgical operation open carpel tunnel release was an average of 27 days, most ranging from 17 to 37 days (an average of almost four weeks, ranging from about 2.4 weeks to 5.3 weeks). This appears to be short compared with Canada's waiting time but may compare less favorably to countries like Germany, the Netherlands (where the goal was five weeks), and Switzerland.
It is unclear how many of the patients waiting longer have to. Some may be by choice, because they wish to go to a well-known specialist or clinic that many people wish to attend, and are willing to wait to do so. Waiting times may also vary by region.
One experiment reported that uninsured patients experienced longer waits; patients with poor insurance coverage probably face a disproportionate number of long waits.
US healthcare tends to rely on rationing by exclusion (uninsured and underinsured), out-of-pocket costs for the insured, fixed payments per case to hospitals (resulting in very short stays), and contracts that manage demand instead.
Population health: quality, prevention, vulnerable populations:
The health of the population is also viewed as a measure of the overall effectiveness of the healthcare system. The extent to which the population lives longer healthier lives signals an effective system.
Innovation: workforce, healthcare IT, R&D:
Finally, the US tracks investment in the healthcare system in terms of a skilled healthcare workforce, meaningful use of healthcare IT, and R&D output. This aspect of the healthcare system performance dashboard is important to consider when evaluating cost of care in the US. That is because in much of the policy debate around the high cost of US healthcare, proponents of highly specialized and cutting-edge technologies point to innovation as a marker of an effective healthcare system.
Compared to other countries:
Further information: Comparison of the healthcare systems in Canada and the United States
A 2014 study by the private US foundation Commonwealth Fund found that although the US healthcare system is the most expensive in the world, it ranks last on most dimensions of performance when compared with:
The study found that the US failed to achieve better outcomes than other countries, and is last or near last in terms of access, efficiency, and equity. Study data came from international surveys of patients and primary care physicians, as well as information on healthcare outcomes from Commonwealth Fund, the WHO, and the OECD.
As of 2017, the US stands 43rd in the world with a life expectancy of 80.00 years. The CIA World Factbook ranked the US 170th worst (out of 225)—meaning 55th best—in the world for infant mortality rate (5.80/1,000 live births). Americans also undergo cancer screenings at significantly higher rates than people in other developed countries, and access MRI and CT scans at the highest rate of any OECD nation.
A study found that between 1997 and 2003, preventable deaths declined more slowly in the US than in 18 other industrialized nations. A 2008 study found that 101,000 people a year die in the US that would not if the healthcare system were as effective as that of France, Japan, or Australia.
A 2020 study by the economists Anne Case and Angus Deaton argues that the US "spends huge sums of money for some of the worst health outcomes in the Western world".
The OECD found that the US ranked poorly in terms of years of potential life lost (YPLL), a statistical measure of years of life lost under the age of 70 that were amenable to being saved by healthcare. Among OECD nations for which data are available, the US ranked third last for the healthcare of women (after Mexico and Hungary) and fifth last for men (Slovakia and Poland also ranked worse).
Recent studies find growing gaps in life expectancy based on income and geography. In 2008, a government-sponsored study found that life expectancy declined from 1983 to 1999 for women in 180 counties, and for men in 11 counties, with most of the life expectancy declines occurring in the Deep South, Appalachia, along the Mississippi River, in the Southern Plains, and in Texas.
The difference is as high as three years for men, six years for women. The gap is growing between rich and poor and by educational level, but narrowing between men and women and by race.
Another study found that the mortality gap between the well-educated and the poorly educated widened significantly between 1993 and 2001 for adults ages 25 through 64; the authors speculated that risk factors such as smoking, obesity and high blood pressure may lie behind these disparities.
In 2011 the US National Research Council forecasted that deaths attributed to smoking, on the decline in the US, will drop dramatically, improving life expectancy; it also suggested that one-fifth to one-third of the life expectancy difference can be attributed to obesity which is the worst in the world and has been increasing.
In an analysis of breast cancer, colorectal cancer, and prostate cancer diagnosed during 1990–1994 in 31 countries, the US had the highest five-year relative survival rate for breast cancer and prostate cancer, although survival was systematically and substantially lower in Black US men and women.
The debate about US healthcare concerns questions of access, efficiency, and quality purchased by the high sums spent. The WHO in 2000 ranked the US healthcare system first in responsiveness, but 37th in overall performance and 72nd by overall level of health (among 191 member nations included in the study). The WHO study has been criticized by the free market advocate David Gratzer because "fairness in financial contribution" was used as an assessment factor, marking down countries with high per-capita private or fee-paying health treatment.
The WHO study has been criticized, in an article published in Health Affairs, for its failure to include the satisfaction ratings of the general public. The study found that there was little correlation between the WHO rankings for health systems and the stated satisfaction of citizens using those systems.
Countries such as Italy and Spain, which were given the highest ratings by WHO were ranked poorly by their citizens while other countries, such as Denmark and Finland, were given low scores by WHO but had the highest percentages of citizens reporting satisfaction with their healthcare systems.
WHO staff, however, say that the WHO analysis does reflect system "responsiveness" and argue that this is a superior measure to consumer satisfaction, which is influenced by expectations. Furthermore, the relationship between patient satisfaction and healthcare utilization, expenditures, clinically meaningful measures, and the evaluation of outcomes is complex, not well defined, and only beginning to be explored.
A report released in April 2008 by the Foundation for Child Development, which studied the period from 1994 through 2006, found mixed results for the health of children in the US Mortality rates for children ages 1 through 4 dropped by a third, and the percentage of children with elevated blood lead levels dropped by 84%.
The percentage of mothers who smoked during pregnancy also declined. On the other hand, both obesity and the percentage of low-birth weight babies increased. The authors note that the increase in babies born with low birth weights can be attributed to women delaying childbearing and the increased use of fertility drugs.
In a sample of 13 developed countries, the US was third in its population weighted usage of medication in 14 classes in both 2009 and 2013. The drugs studied were selected on the basis that the conditions treated had high incidence, prevalence and/or mortality, caused significant long-term morbidity and incurred high levels of expenditure and significant developments in prevention or treatment had been made in the last 10 years. The study noted considerable difficulties in cross border comparison of medication use.
A critic of the US healthcare system, British philanthropist Stan Brock, whose charity Remote Area Medical has served over half a million uninsured Americans, stated, "You could be blindfolded and stick a pin on a map of America and you will find people in need."
The charity has over 700 clinics and 80,000 volunteer doctors and nurses around the US Simon Usborne of The Independent writes that in the UK "General practitioners are amazed to hear that poor Americans should need to rely on a charity that was originally conceived to treat people in the developing world."
System efficiency and equity:
Variations in the efficiency of healthcare delivery can cause variations in outcomes. The Dartmouth Atlas Project, for instance, reported that, for over 20 years, marked variations in how medical resources are distributed and used in the US were accompanied by marked variations in outcomes.
The willingness of physicians to work in an area varies with the income of the area and the amenities it offers, a situation aggravated by a general shortage of doctors in the US, particularly those who offer primary care. The ACA is anticipated to produce an additional demand for services which the existing stable of primary care doctors will be unable to fill, particularly in economically depressed areas. Training additional physicians would require some years.
Lean manufacturing techniques such as value stream mapping can help identify and subsequently mitigate waste associated with costs of healthcare. Other product engineering tools such as FMEA and Fish Bone Diagrams have been used to improve efficiencies in healthcare delivery.
Since 2004 the Commonwealth Fund has produced reports comparing healthcare systems in high income countries using survey and administrative data from the OECD and WHO which is analyzed under five themes:
The US has been assessed as worst healthcare system overall among 11 high-income countries in every report, even though it spends the highest proportion of its gross domestic product on healthcare.
In 2021 Norway, the Netherlands and Australia were the top-performing countries. The US spent 16.8% of GDP on healthcare in 2019; the next highest country on the list was Switzerland, at 11.3% of GDP. The lowest was New Zealand, which spent roughly 9% of its GDP on healthcare in 2019. It "consistently demonstrated the largest disparities between income groups" across indicators, apart from those related to preventive services and the safety of care.
Efficiency:
Preventable deaths:
In 2010, coronary artery disease, lung cancer, stroke, chronic obstructive pulmonary diseases, and traffic accidents caused the most years of life lost in the US. Low back pain, depression, musculoskeletal disorders, neck pain, and anxiety caused the most years lost to disability. The most deleterious risk factors were:
Alzheimer's disease, drug abuse, kidney disease and cancer, and falls caused the most additional years of life lost over their age-adjusted 1990 per-capita rates.
Between 1990 and 2010, among the 34 countries in the OECD, the US dropped from 18th to 27th in age-standardized death rate. The US dropped from 23rd to 28th for age-standardized years of life lost. It dropped from 20th to 27th in life expectancy at birth. It dropped from 14th to 26th for healthy life expectancy.
According to a 2009 study conducted at Harvard Medical School by cofounders of Physicians for a National Health Program, a pro-single payer lobbying group, and published by the American Journal of Public Health, lack of health coverage is associated with nearly 45,000 excess preventable deaths annually.
Since then, as the number of uninsured has risen from about 46 million in 2009 to 49 million in 2012, the number of preventable deaths due to lack of insurance has grown to about 48,000 per year.
The group's methodology has been criticized by economist John C. Goodman for not looking at cause of death or tracking insurance status changes over time, including the time of death.
A 2009 study by former Clinton policy adviser Richard Kronick published in the journal Health Services Research found no increased mortality from being uninsured after certain risk factors were controlled for.
Value for money:
A study of international healthcare spending levels published in the health policy journal Health Affairs in the year 2000 found that the US spends substantially more on healthcare than any other country in the OECD (OECD), and that the use of healthcare services in the US is below the OECD median by most measures.
The authors of the study conclude that the prices paid for healthcare services are much higher in the US than elsewhere. While the 19 next most wealthy countries by GDP all pay less than half what the US does for healthcare, they have all gained about six years of life expectancy more than the US since 1970.
Delays in seeking care and increased use of emergency care:
Uninsured Americans are less likely to have regular healthcare and use preventive services. They are more likely to delay seeking care, resulting in more medical crises, which are more expensive than ongoing treatment for such conditions as diabetes and high blood pressure.
A 2007 study published in JAMA concluded that uninsured people were less likely than the insured to receive any medical care after an accidental injury or the onset of a new chronic condition.
The uninsured with an injury were also twice as likely as those with insurance to have received none of the recommended follow-up care, and a similar pattern held for those with a new chronic condition. Uninsured patients are twice as likely to visit hospital emergency rooms as those with insurance; burdening a system meant for true emergencies with less-urgent care needs.
In 2008 researchers with the American Cancer Society found that individuals who lacked private insurance (including those covered by Medicaid) were more likely to be diagnosed with late-stage cancer than those who had such insurance.
Variations in provider practices:
The treatment given to a patient can vary significantly depending on which healthcare providers they use. Research suggests that some cost-effective treatments are not used as often as they should be, while overutilization occurs with other healthcare services.
Unnecessary treatments increase costs and can cause patients unnecessary anxiety. The use of prescription drugs varies significantly by geographic region. The overuse of medical benefits is known as moral hazard—individuals who are insured are then more inclined to consume healthcare.
The way the healthcare system tries to eliminate this problem is through cost-sharing tactics like copays and deductibles. If patients face more of the economic burden they will then only consume healthcare when they perceive it to be necessary. According to the RAND health insurance experiment, individuals with higher coinsurance rates consumed less healthcare than those with lower rates.
The experiment concluded that with less consumption of care there was generally no loss in societal welfare but, for the poorer and sicker groups of people there were definitely negative effects. These patients were forced to forgo necessary preventative care measures in order to save money leading to late diagnosis of easily treated diseases and more expensive procedures later.
With less preventative care, the patient is hurt financially with an increase in expensive visits to the ER. The healthcare costs in the US will also rise with these procedures as well. More expensive procedures lead to greater costs.
One study has found significant geographic variations in Medicare spending for patients in the last two years of life. These spending levels are associated with the amount of hospital capacity available in each area. Higher spending did not result in patients living longer.
Care coordination:
Primary care doctors are often the point of entry for most patients needing care, but in the fragmented healthcare system of the US, many patients and their providers experience problems with care coordination.
For example, a Harris Interactive survey of California physicians found that:
According to an article in The New York Times, the relationship between doctors and patients is deteriorating. A study from Johns Hopkins University found that roughly one in four patients believe their doctors have exposed them to unnecessary risks, and anecdotal evidence such as self-help books and web postings suggest increasing patient frustration.
Possible factors behind the deteriorating doctor/patient relationship include the current system for training physicians and differences in how doctors and patients view the practice of medicine. Doctors may focus on diagnosis and treatment, while patients may be more interested in wellness and being listened to by their doctors.
Many primary care physicians no longer see their patients while they are in the hospital; instead, hospitalists are used. The use of hospitalists is sometimes mandated by health insurance companies as a cost-saving measure which is resented by some primary care physicians.
Administrative costs:
As of 2017, there were 907 health insurance companies in the US, although the top 10 account for about 53% of revenue and the top 100 account for 95% of revenue. The number of insurers contributes to administrative overhead in excess of that in nationalized, single-payer systems, such as that in Canada, where administrative overhead was estimated to be about half of the US.
Insurance industry group America's Health Insurance Plans estimates that administrative costs have averaged approximately 12% of premiums over the last 40 years, with costs shifting away from adjudicating claims and towards medical management, nurse help lines, and negotiating discounted fees with healthcare providers.
A 2003 study published by the Blue Cross and Blue Shield Association (BCBSA) also found that health insurer administrative costs were approximately 11% to 12% of premiums, with Blue Cross and Blue Shield plans reporting slightly lower administrative costs, on average, than commercial insurers.
For the period 1998 through 2003, average insurer administrative costs declined from 13% to 12% of premiums. The largest increases in administrative costs were in customer service and information technology, and the largest decreases were in provider services and contracting and in general administration.
The McKinsey Global Institute estimated that excess spending on "health administration and insurance" accounted for as much as 21% of the estimated total excess spending ($477 billion in 2003).
According to a report published by the CBO in 2008, administrative costs for private insurance represent approximately 12% of premiums. Variations in administrative costs between private plans are largely attributable to economies of scale. Coverage for large employers has the lowest administrative costs. The percentage of premium attributable to administration increases for smaller firms, and is highest for individually purchased coverage.
A 2009 study published by BCBSA found that the average administrative expense cost for all commercial health insurance products was represented 9.2% of premiums in 2008. Administrative costs were 11.1% of premiums for small group products and 16.4% in the individual market.
One study of the billing and insurance-related (BIR) costs borne not only by insurers but also by physicians and hospitals found that BIR among insurers, physicians, and hospitals in California represented 20–22% of privately insured spending in California acute care settings.
Long-term living facilities:
As of 2014, according to a report published the higher the skill of the RN the lower the cost of a financial burden on the facilities. With a growing elderly population, the number of patients in these long term facilities needing more care creates a jump in financial costs.
Based on research done in 2010, annual out of pocket costs jumped 7.5% while the cost for Medicare grew 6.7% annually due to the increases. While Medicare pays for some of the care that the elderly populations receive, 40% of the patients staying in these facilities pay out of pocket.
Third-party payment problem and consumer-driven insurance:
Most Americans pay for medical services largely through insurance, and this can distort the incentives of consumers since the consumer pays only a portion of the ultimate cost directly. The lack of price information on medical services can also distort incentives.
The insurance which pays on behalf of insureds negotiate with medical providers, sometimes using government-established prices such as Medicaid billing rates as a reference point.This reasoning has led for calls to reform the insurance system to create a consumer-driven healthcare system whereby consumers pay more out-of-pocket.
In 2003, the Medicare Prescription Drug, Improvement, and Modernization Act was passed, which encourages consumers to have a high-deductible health plan and a health savings account.
In October 2019, the state of Colorado proposed running public healthcare option through private insurers, which are to bear the brunt of the costs. Premiums under the public option are touted to be 9% to 18% cheaper by 2022.
Equity:
Mental health:
See also: Mental health § United States, and Mentally ill prisoners in the United States
In 2020, 52.9 million adults were affected by mental illness, nearly one in five adults in the country. 44.7 million adults were affected in 2016.
In 2006, mental disorders were ranked one of the top five most costly medical conditions, with expenditures of $57.5 billion (equivalent to $75.5 billion in 2021). A lack of mental health coverage for Americans bears significant ramifications to the US economy and social system.
A report by the US Surgeon General found that mental illnesses are the second leading cause of disability in the nation and affect 20% of all Americans.
It is estimated that less than half of all people with mental illnesses receive treatment (or specifically, an ongoing, much needed, and managed care; where medication alone, cannot easily remove mental conditions) due to factors such as stigma and lack of access to care, including a shortage of mental health professionals.
Treatment rates are understood to vary between different conditions; as an example, only 16% of adults with schizophrenia and 25% with bipolar disorder were estimated to be untreated with appropriate medication in 2007.
The Paul Wellstone Mental Health and Addiction Equity Act of 2008 mandates that group health plans provide mental health and substance-related disorder benefits that are at least equivalent to benefits offered for medical and surgical procedures.
The legislation renews and expands provisions of the Mental Health Parity Act of 1996. The law requires financial equity for annual and lifetime mental health benefits, and compels parity in treatment limits and expands all equity provisions to addiction services.
Insurance companies and third-party disability administrators (most notably, Sedgwick CMS) used loopholes and, though providing financial equity, they often worked around the law by applying unequal copayments or setting limits on the number of days spent in inpatient or outpatient treatment facilities.
Oral health:
In the US, dental care is largely not recognized as healthcare, even though individuals visit a dentist more often than a general practitioner, and thus the field and its practices developed independently. In modern policy and practice, oral health is thus considered distinct from primary health, and dental insurance is separate from health insurance.
Disparities in oral healthcare accessibility mean that many populations, including those without insurance, the low-income, uninsured, racial minorities, immigrants, and rural populations, have a higher probability of poor oral health at every age. While changes have been made to address these disparities for children, the oral health disparity in adults of all previously listed populations has remained consistent or worsened.
The magnitude of this health issue is surprising even in New York state, where the Medicaid program includes dental coverage and is one of the most impressive insurance programs in the nation. Seven out of ten older adults (aged ≥ 65) have periodontal disease, and one in four adults (aged > 65) has no teeth.
This raises concern about the New York State Department of Health's rule, which prevents Medicaid coverage for the replacement of dentures within eight years of initial placement and a ban on coverage of dental implants. In addition, older adults are more likely than those in younger age groups to have medical conditions, such as diabetes and cardiovascular disease, that worsen their oral health.
Medical underwriting and the uninsurable:
Prior to the ACA, medical underwriting was common, but, after the law came into effect in 2014, it became effectively prohibited.
Demographic differences:
Main articles:
Health disparities are well documented in the US in ethnic minorities such as African Americans, Native Americans, and Hispanics.
When compared to whites, these minority groups have higher incidence of chronic diseases, higher mortality, poorer health outcomes and poorer rates of diagnosis and treatment.
Among the disease-specific examples of racial and ethnic disparities in the US is the cancer incidence rate among African Americans, which is 25% higher than among whites. In addition, adult African Americans and Hispanics have approximately twice the risk as whites of developing diabetes and have higher overall obesity rates.
Minorities also have higher rates of cardiovascular disease and HIV/AIDS than whites. In the US, Asian Americans live the longest (87.1 years), followed by Latinos (83.3 years), whites (78.9 years), Native Americans (76.9 years), and African Americans (75.4 years). A 2001 study found large racial differences exist in healthy life expectancy at lower levels of education.
Public spending is highly correlated with age; average per capita public spending for seniors was more than five times that for children ($6,921 versus $1,225, equivalent to $10,427 versus $1,846 in 2021).
Average public spending for non-Hispanic blacks ($2,973, equivalent to $4,479 in 2021) was slightly higher than that for whites ($2,675, equivalent to $4,030 in 2021),
Spending for Hispanics ($1,967, equivalent to $2,963 in 2021) was significantly lower than the population average ($2,612, equivalent to $3,935 in 2021).
Total public spending is also strongly correlated with self-reported health status ($13,770 (equivalent to $20,745 in 2021) for those reporting "poor" health versus $1,279 (equivalent to $1,927 in 2021) for those reporting "excellent" health.
Seniors comprise 13% of the population but take one-third of all prescription drugs. The average senior fills 38 prescriptions annually. A new study has also found that older men and women in the South are more often prescribed antibiotics than older Americans elsewhere, even though there is no evidence that the South has higher rates of diseases requiring antibiotics.
There is considerable research into inequalities in healthcare. In some cases, these inequalities are caused by income disparities that result in lack of health insurance and other barriers to receiving services.
According to the 2009 National Healthcare Disparities Report, uninsured Americans are less likely to receive preventive services in healthcare. For example, minorities are not regularly screened for colon cancer and the death rate for colon cancer has increased among African Americans and Hispanic people.
In other cases, inequalities in healthcare reflect a systemic bias in the way medical procedures and treatments are prescribed for different ethnic groups. Raj Bhopal writes that the history of racism in science and medicine shows that people and institutions behave according to the ethos of their times.
Nancy Krieger wrote that racism underlies unexplained inequities in healthcare, including treatment for heart disease, renal failure, bladder cancer, and pneumonia. Raj Bhopal writes that these inequalities have been documented in numerous studies.
The consistent and repeated findings were that Black Americans received less healthcare than white Americans—particularly when the care involved expensive new technology. One recent study has found that when minority and white patients use the same hospital, they are given the same standard of care.
Prescription drug issues:
Drug efficiency and safety:
See also: Regulation of therapeutic goods in the United States
The FDA is the primary institution tasked with the safety and effectiveness of human and veterinary drugs. It also is responsible for making sure drug information is accurately and informatively presented to the public. The FDA reviews and approves products and establishes drug labeling, drug standards, and medical device manufacturing standards. It sets performance standards for radiation and ultrasonic equipment.
One of the more contentious issues related to drug safety is immunity from prosecution. In 2004, the FDA reversed a federal policy, arguing that FDA premarket approval overrides most claims for damages under state law for medical devices. In 2008, this was confirmed by the Supreme Court in Riegel v. Medtronic, Inc.
On June 30, 2006, an FDA ruling went into effect extending protection from lawsuits to pharmaceutical manufacturers, even if it was found that they submitted fraudulent clinical trial data to the FDA in their quest for approval. This left consumers who experience serious health consequences from drug use with little recourse.
In 2007, the House of Representatives expressed opposition to the FDA ruling, but the Senate took no action. On March 4, 2009, an important US Supreme Court decision was handed down. In Wyeth v. Levine, the court asserted that state-level rights of action could not be pre-empted by federal immunity and could provide "appropriate relief for injured consumers".
In June 2009, under the Public Readiness and Emergency Preparedness Act, Secretary of Health and Human Services Kathleen Sebelius signed an order extending protection to vaccine makers and federal officials from prosecution during a declared health emergency related to the administration of the swine flu vaccine.
Prescription drug prices:
Main article: Prescription drug prices in the United States
During the 1990s, the price of prescription drugs became a major issue in US politics as the prices of many new drugs increased exponentially, and many citizens discovered that neither the government nor their insurer would cover the cost of such drugs.
Per capita, the US spends more on pharmaceuticals than any other country, although expenditures on pharmaceuticals accounts for a smaller share (13%) of total healthcare costs compared to an OECD average of 18% (2003 figures).
Some 25% of out-of-pocket spending by individuals is for prescription drugs. Another study finds that between 1990 and 2016, prescription drug prices in the US increased by 277% while prescription drug prices increased by only 57% in the UK, 13% in Canada, and decreased in France and Japan.
The US government has taken the position (through the Office of the US Trade Representative) that US drug prices are rising because US consumers are effectively subsidizing costs which drug companies cannot recover from consumers in other countries (because many other countries use their bulk-purchasing power to aggressively negotiate drug prices).
The US position (consistent with the primary lobbying position of the Pharmaceutical Research and Manufacturers of America) is that the governments of such countries are free riding on the backs of US consumers.
Such governments should either deregulate their markets, or raise their domestic taxes in order to fairly compensate US consumers by directly remitting the difference (between what the companies would earn in an open market versus what they are earning now) to drug companies or to the US government.
In turn, pharmaceutical companies would be able to continue to produce innovative pharmaceuticals while lowering prices for US consumers. Currently, the US, as a purchaser of pharmaceuticals, negotiates some drug prices but is forbidden by law from negotiating drug prices for the Medicare program due to the Medicare Prescription Drug, Improvement, and Modernization Act passed in 2003.
Democrats have charged that the purpose of this provision is merely to allow the pharmaceutical industry to profiteer off of the Medicare program.
Impact of drug companies:
The US, along with New Zealand, make up the only countries in the world that allows direct-to-consumer advertising of prescription drugs. In 2015, the American Medical Association called for the banning of direct-to-consumer advertising because it is linked with increased drug prices.
Still, other evidence cites that there are some benefits to direct-to-consumer advertising, such as encouraging patients to see the doctor, diagnosis of rare diseases, and the removal of stigma associated with the disease.
When healthcare legislation was being written in 2009, the drug companies were asked to support the legislation in return for not allowing importation of drugs from foreign countries.
Healthcare reform debate:
Further information: Healthcare reform in the United States and Service Excellence – Health Care
In 2008, prior to the major healthcare reform in 2010, Americans were divided in their views of the US health system; 45% said that the US system was best and 39% said that other countries' systems are better.
Much of the historical debate around healthcare reform centered around single-payer healthcare, and particularly pointing to the hidden costs of treating the uninsured while free-market advocates point to freedom of choice in purchasing health insurance and unintended consequences of government intervention, citing the Health Maintenance Organization Act of 1973.
According to a 2020 study published in The Lancet, a single-payer universal healthcare system could save 68,000 lives and $450 billion in national healthcare expenditure annually, while another 2022 study published in the PNAS, estimated that a universal healthcare system could have saved more than 338,000 lives during the COVID-19 pandemic in the US from its start until March 2022.
Ultimately, a single-payer healthcare, sometimes called "socialized medicine", was not adopted in the final ACA.
Patient Protection and Affordable Care Act (2010):
The ACA (Public Law 111–148) is a healthcare reform bill that was signed into law in the US by President Barack Obama on March 23, 2010. The law includes a large number of health-related provisions, most of which took effect in 2014, including expanding Medicaid eligibility for people making up to 133% of FPL, subsidizing insurance premiums for individuals and families making up to 400% of FPL and capping expenses from 2% to 9.8% of annual income.
For the first time, all health policies sold in the US must cap an individual's (or family's) medical expenses out of pocket annually. Other provisions include providing incentives for businesses to provide healthcare benefits, prohibiting denial of coverage and denial of claims based on pre-existing conditions, establishing health insurance exchanges, prohibiting insurers from establishing annual spending caps and support for medical research.
The costs of these provisions are offset by a variety of taxes, fees, and cost-saving measures, such as new Medicare taxes for high-income brackets, taxes on indoor tanning, cuts to the Medicare Advantage program in favor of traditional Medicare, and fees on medical devices and pharmaceutical companies; there is also a tax penalty for citizens who do not obtain health insurance (unless they are exempt due to low income or other reasons).
The Congressional Budget Office estimates that the net effect (including the reconciliation act) will be a reduction in the federal deficit by $143 billion over the first decade.
However, two months later, the office subsequently acknowledged that there was an additional $115 billion in funds needed that were not originally included in the estimate.
Additionally, the CBO estimated that although projected premiums in 2016 would be lower by $100 per person for small and large business health insurance plans with the ACA than without, individual plans would be higher by $1,900 with the bill.
The first open enrollment period of the ACA began in October 2013. Prior to this period, access to healthcare and insurance coverage trends were worsening on a national level. A large, national survey of US adults found that after the act's first two enrollment periods, self-reported coverage, health, and access to care improved significantly.
Furthermore, insurance coverage for low-income adults were significantly greater in states that expanded Medicaid in comparison with states that did not expand Medicaid. However, discrepancies do exist between those covered by Medicaid versus those covered by private insurance. Those insured by Medicaid tend to report fair or poor health, as opposed to excellent or very good health.
On December 22, 2017, the Tax Cuts and Jobs Act of 2017 was signed into law by President Donald Trump. Inside the final version of the bill was a repeal of the individual mandate in the ACA, which required individuals and companies to get healthcare for themselves and their employees. It was this mandate which kept healthcare costs down under the PPACA by promoting cost sharing over a larger pool.
Economists believe the repeal of the individual mandate will lead to higher premiums and lower enrollment in the current market though they do not agree with how much. In 2017, the new Republican healthcare bill known as the American Health Care Act was passed by the House of Representatives under President Donald Trump. Although the ACA and the American Health Care Act both propose tax cuts in order to make insurance more affordable for Americans, each of these bills affected Americans in different ways.
The people most affected by President Trump's plan are young people, individuals of a higher socioeconomic status, and people who live in urban areas. Young people because individuals between the age of 20 and 30 will see drops in the premiums they pay within their plans.
Individuals with higher socioeconomic status because whereas under Obamacare individuals could only make up to $50,000 annually and still receive tax breaks, now under Trump's plan that number has been increased so that individuals who make up to $115,000 annually can receive tax breaks.
In addition, those in urban areas can also benefit from the plan because under Obamacare tax credits were designated also by the cost of local healthcare, but the American Health Care Act does not take this into consideration although rural healthcare is generally more expensive due to the lack of hospitals and available services.
Health insurance coverage for immigrants:
Main article: Immigrant health care in the United States
Of the 26.2 million foreign immigrants living in the US in 1998, 62.9% were non-US citizens. In 1997, 34.3% of non-US citizens living in the US did not have health insurance coverage opposed to the 14.2% of native-born Americans who do not have health insurance coverage.
Among those immigrants who became citizens, 18.5% were uninsured, as opposed to non-citizens, who are 43.6% uninsured. In each age and income group, immigrants are less likely to have health insurance.
With the recent healthcare changes, many legal immigrants with various immigration statuses now are able qualify for affordable health insurance.
Undocumented immigrants within the US do not have access to government funded health insurance. Although the ACA allows immigrants to receive insurance at a discounted rate, the same does not go for those without US citizenship.
While policies like the Patient Protection Act and Affordable Care Act have aimed at expanding health insurance coverage to also improve refugee health in the US, different states have implemented their health insurance programs differently leading to healthcare access disparities between states.
Undocumented immigrants in the US can seek medical help from community centers, or what is termed Safety Net Providers, and participate in fee for service medical assistance, but can only buy health insurance from private health insurers.
Healthcare is provided by many distinct organizations, made up of insurance companies, healthcare providers, hospital systems, and independent providers. Healthcare facilities are largely owned and operated by private sector businesses. 58% of community hospitals in the US are nonprofit, 21% are government-owned, and 21% are for-profit.
According to the World Health Organization (WHO), the US spent $9,403 (equivalent to $10,738 in 2021) on healthcare per capita, and 17.9% on healthcare as percentage of its GDP in 2014.
Healthcare coverage is provided through a combination of private health insurance and public health coverage (e.g., Medicare, Medicaid). In 2013, 64% of health spending was paid for by the government, and funded via programs such as Medicare, Medicaid, the Children's Health Insurance Program, Tricare, and the Veterans Health Administration.
People aged under 65 acquire insurance via their or a family member's employer, by purchasing health insurance on their own, getting government and/or other assistance based on income or another condition, or are uninsured. Health insurance for public sector employees is primarily provided by the government in its role as employer.
Managed care, where payers use various techniques intended to improve quality and limit cost, has become ubiquitous. The US life expectancy is 78.6 years at birth, up from 75.2 years in 1990; this ranks 42nd among 224 nations, and 22nd out of the 35 industrialized OECD countries, down from 20th in 1990.
In 2016 and 2017, life expectancy in the US dropped for the first time since 1993. Of 17 high-income countries studied by the National Institutes of Health, the US in 2013 had the highest or near-highest prevalence of obesity, car accidents, infant mortality, heart and lung disease, sexually transmitted infections, adolescent pregnancies, injuries, and homicides.
A 2017 survey of the healthcare systems of 11 developed countries found the US healthcare system to be the most expensive and worst-performing in terms of health access, efficiency, and equity. In a 2018 study, the US ranked 29th in healthcare access and quality.
The rate of adults uninsured for healthcare peaked at 18.0% in 2013 prior to the Affordable Care Act (ACA) mandate, fell to 10.9% in the third quarter of 2016, and stood at 13.7% in the fourth quarter of 2018, based on surveys by the Gallup organization beginning in 2008.
At over 27 million, the number of people without health insurance coverage in the US is one of the primary concerns raised by advocates of healthcare reform. A 2009 study done at Harvard Medical School with Cambridge Health Alliance by cofounders of Physicians for a National Health Program, a pro-single payer lobbying group, showed that nearly 45,000 annual deaths are associated with a lack of patient health insurance.
The study also found that uninsured, working Americans have an approximately 40% higher mortality risk compared to privately insured working Americans. In 2010, the ACA (formally known as the "Patient Protection and Affordable Care Act" and commonly known as "Obamacare") became law, enacting major changes in health insurance.
The Supreme Court of the US upheld the constitutionality of most of the law in June 2012 and affirmed insurance exchange subsidies in all states in June 2015.
The Human Rights Measurement Initiative finds that the US is achieving 81.3% of what should be possible at their income level for fulfilling the right to health.
At the same time, the United States is the leader in medical innovation, measured either in terms of revenue or the number of new drugs and devices introduced.
History:
Main articles:
- History of medicine in the United States,
- Medicare (United States) § History,
- Medicaid § History,
- and Managed care § History
In the US, dissimilar to the European nationalized health insurance plans, the market created a private employment-based system. Following the Stabilization Act of 1942, employers, unable to provide higher salaries to attract or retain employees, began to offer insurance plans, including healthcare packages, as a fringe benefit, thereby beginning the practice of employer-sponsored health insurance.
Statistics:
Hospitalizations:
According to a statistical brief by the Healthcare Cost and Utilization Project (HCUP), there were 35.7 million hospitalizations in 2016, a significant decrease from the 38.6 million in 2011.
For every 1,000 in the population, there was an average of 104.2 stays and each stay averaged $11,700 (equivalent to $13,210 in 2021, an increase from the $10,400 (equivalent to $12,275 in 2021) cost per stay in 2012. 7.6% of the population had overnight stays in 2017, each stay lasting an average of 4.6 days.
A study by the National Institutes of Health reported that the lifetime per capita expenditure at birth, using the year 2000 dollars, showed a large difference between the healthcare costs of females ($361,192, equivalent to $568,345 in 2021) and males ($268,679, equivalent to $422,774 in 2021).
A large portion of this cost difference is in the shorter lifespan of men, but, even after adjustment for age (assuming men live as long as women), there still is a 20% difference in lifetime healthcare expenditures.
Health insurance and accessibility:
Main articles:
Unlike most developed nations, the US health system does not provide healthcare to the country's entire population. Instead, most citizens are covered by a combination of private insurance and various federal and state programs.
As of 2017, health insurance was most commonly acquired through a group plan tied to an employer, covering 150 million people. Other major sources include Medicaid, covering 70 million, Medicare, 50 million, and health insurance marketplaces created by the ACA covering around 17 million.
In 2017, a study found that 73% of plans on ACA marketplaces had narrow networks, limiting access and choice in providers.
Measures of accessibility and affordability tracked by national health surveys include:
- percent of population with insurance,
- having a usual source of medical care,
- visiting the dentist yearly,
- rates of preventable hospitalizations,
- reported difficulty seeing a specialist,
- delaying care due to cost,
- and rates of health insurance coverage.
In 2004, an OECD report noted that "all OECD countries [except Mexico, Turkey, and the US] had achieved universal or near-universal (at least 98.4% insured) coverage of their populations by 1990". The 2004 IOM report also observed that "lack of health insurance causes roughly 18,000 unnecessary deaths every year in the US".
The Gallup organization tracks the percent of adult Americans who are uninsured for healthcare, beginning in 2008. The rate of uninsured peaked at 18.0% in 2013 prior to the ACA mandate, fell to 10.9% in the third quarter of 2016, and stood at 13.7% in the fourth quarter of 2018. "The 2.8-percentage-point increase since that low represents a net increase of about seven million adults without health insurance."
The US Census Bureau reported that 28.5 million people (8.8%) did not have health insurance in 2017, down from 49.9 million (16.3%) in 2010. Between 2004 and 2013, a trend of high rates of underinsurance and wage stagnation contributed to a healthcare consumption decline for low-income Americans. This trend was reversed after the implementation of the major provisions of the ACA in 2014.
As of 2017, the possibility that the ACA may be repealed or replaced has intensified interest in the questions of whether and how health insurance coverage affects health and mortality. Several studies have indicated that there is an association with expansion of the ACA and factors associated with better health outcomes such as having a regular source of care and the ability to afford care.
A 2016 study concluded that an approximately 60% increased ability to afford care can be attributed to Medicaid expansion provisions enacted by the Patient Protection and Affordable Care Act.
Additionally, an analysis of changes in mortality post Medicaid expansion suggests that Medicaid saves lives at a relatively more cost effective rate of a societal cost of $327,000 to $867,000 (equivalent to $369,213 to $978,921 in 2021) per life saved compared to other public policies which cost an average of $7.6 million (equivalent to $8.58 million in 2021) per life.
A 2009 study in five states found that medical debt contributed to 46.2% of all personal bankruptcies, and 62.1% of bankruptcy filers claimed high medical expenses in 2007. Since then, health costs and the numbers of uninsured and underinsured have increased. A 2013 study found that about 25% of all senior citizens declare bankruptcy due to medical expenses.
In practice, the uninsured are often treated, but the cost is covered through taxes and other fees which shift the cost. Forgone medical care due to extensive cost sharing may ultimately increase costs due to downstream medical issues; this dynamic may play a part in US's international ranking as having the highest healthcare expenditures despite significant patient cost-sharing.
Those who are insured may be underinsured such that they cannot afford adequate medical care. A 2003 study estimated that 16 million US adults were underinsured, disproportionately affecting those with lower incomes—73% of the underinsured in the study population had annual incomes below 200% of the federal poverty level.
Lack of insurance or higher cost sharing (user fees for the patient with insurance) create barriers to accessing healthcare: use of care declines with increasing patient cost-sharing obligation. Before the ACA passed in 2014, 39% of below-average income Americans reported forgoing seeing a doctor for a medical issue (whereas 7% of low-income Canadians and 1% of low-income British citizens reported the same).
Health in the US in global context:
In 2019, the under-five child mortality rate was 6.5 deaths per 1000 live births, placing the US 33rd of 37 OECD countries. In 2010–2012, more than 57,000 infants (52%) and children under 18 years died in the US.
While not as high in 2015 as in 2013 (18.5), maternal deaths related to childbirth have shown recent increases; in 1987, the mortality ratio was 7.2 per 100,000. As of 2015, the US rate is double the maternal mortality rate in Belgium or Canada, and more than triple the rate in the Finland as well as several other Western European countries.
Life expectancy at birth for a child born in the US in 2015 is 81.2 (females) or 76.3 (males) years. According to the WHO, life expectancy in the US is 31st in the world (out of 183 countries) as of 2015. The US's average life expectancy (both sexes) is just over 79. Japan ranks first with an average life expectancy of nearly 84 years. The US ranks lower (36th) when considering health-adjusted life expectancy (HALE) at just over 69 years.
Another source, the Central Intelligence Agency, indicates life expectancy at birth in the US is 79.8, ranking it 42nd in the world. Monaco is first on this list of 224, with an average life expectancy of 89.5.
A 2013 National Research Council study stated that, when considered as one of 17 high-income countries, the US was at or near the top in:
- infant mortality,
- heart and lung disease,
- sexually transmitted infections,
- adolescent pregnancies,
- injuries,
- homicides,
- and rates of disability.
Together, such issues place the US at the bottom of the list for life expectancy in high-income countries. Females born in the US in 2015 have a life expectancy of 81.6 years, and males 76.9 years; more than three years less and as much as over five years less than people born in Switzerland (85.3 F, 81.3 M) or Japan (86.8 F, 80.5 M) in 2015.
Causes of mortality in the US:
See also: List of causes of death by rate
The top three causes of death among both sexes and all ages in the US have consistently remained cardiovascular diseases (ranked 1st), neoplasms (2nd) and neurological disorders (3rd), since the 1990s.
In 2015, the total number of deaths by heart disease was 633,842, by cancer it was 595,930, and from chronic lower respiratory disease it was 155,041.
In 2015, 267.18 deaths per 100,000 people were caused by cardiovascular diseases, 204.63 by neoplasms and 100.66 by neurological disorders.
Diarrhea, lower respiratory, and other common infections were ranked sixth overall, but had the highest rate of infectious disease mortality in the US at 31.65 deaths per 100,000 people.
There is evidence, however, that a large proportion of health outcomes and early mortality can be attributed to factors other than communicable or non-communicable disease. As a 2013 National Research Council study concluded, more than half the men who die before the age of 50 die due to murder (19%), traffic accidents (18%), and other accidents (16%).
For women, the percentages are different: 53% of women who die before the age of 50 die due to disease, whereas 38% die due to accidents, homicide, and suicide.
Diseases of despair (drug overdoses, alcoholic liver disease, and suicide), which started increasing in the early 1990s, kill roughly 158,000 Americans a year as of 2018.
Since 2020, the Centers for Disease Control and Prevention (CDC) reports that the life expectancy for the US population was 77.0 years, a decrease of 1.8 years from 2019.
Life expectancy fell again in 2021 to 76.4 years, which has been attributed to COVID-19 and rising death rates from suicide, drug overdoses and liver disease.
Providers:
Healthcare providers in the US encompass individual healthcare personnel, healthcare facilities, and medical products.
Facilities:
Main pages:
In the US, ownership of the healthcare system is mainly in private hands, though federal, state, county, and city governments also own certain facilities.
As of 2018, there were 5,534 registered hospitals in the US. There were 4,840 community hospitals, which are defined as nonfederal, short-term general, or specialty hospitals.
The nonprofit hospitals share of total hospital capacity has remained relatively stable (about 70%) for decades. There are also privately owned for-profit hospitals as well as government hospitals in some locations, mainly owned by county and city governments.
The Hill–Burton Act was passed in 1946, which provided federal funding for hospitals in exchange for treating poor patients.
The largest hospital system in 2016 by revenue was HCA Healthcare in 2019, Dignity Health and Catholic Health Initiatives merged into CommonSpirit Health to create the largest by revenue, spanning 21 states.
Integrated delivery systems, where the provider and the insurer share the risk in an attempt to provide value-based healthcare, have grown in popularity. Regional areas have separate healthcare markets, and in some markets competition is limited as the demand from the local population cannot support multiple hospitals.
About two-thirds of doctors practice in small offices with less than seven physicians, with over 80% owned by physicians; these sometimes join groups such as independent practice associations to increase bargaining power.
There is no nationwide system of government-owned medical facilities open to the general public but there are local government-owned medical facilities open to the general public.
The US Department of Defense operates field hospitals as well as permanent hospitals via the Military Health System to provide military-funded care to active military personnel.
The federal Veterans Health Administration operates VA hospitals open only to veterans, though veterans who seek medical care for conditions they did not receive while serving in the military are charged for services.
The Indian Health Service (IHS) operates facilities open only to Native Americans from recognized tribes. These facilities, plus tribal facilities and privately contracted services funded by IHS to increase system capacity and capabilities, provide medical care to tribespeople beyond what can be paid for by any private insurance or other government programs.
Hospitals provide some outpatient care in their emergency rooms and specialty clinics, but primarily exist to provide inpatient care. Hospital emergency departments and urgent care centers are sources of sporadic problem-focused care. Surgicenters are examples of specialty clinics. Hospice services for the terminally ill who are expected to live six months or less are most commonly subsidized by charities and government.
Prenatal, family planning, and dysplasia clinics are government-funded obstetric and gynecologic specialty clinics respectively, and are usually staffed by nurse practitioners. Services, particularly urgent-care services, may also be delivered remotely via telemedicine by providers such as Teladoc.
Besides government and private healthcare facilities, there are also 355 registered free clinics in the US that provide limited medical services. They are considered to be part of the social safety net for those who lack health insurance. Their services may range from more acute care (i.e., STDs, injuries, respiratory diseases) to long term care (i.e. dentistry, counseling). Another component of the healthcare safety net would be federally funded community health centers.
Other healthcare facilities include long-term housing facilities which, as of 2019, there were 15,600 nursing homes across the US, with a large portion of that number being for-profit (69.3%)
In 2022, 19 hospitals filed for bankruptcy, closed, or announced plans to close.
Physicians (M.D. and D.O.):
Main article: Physicians in the United States
Physicians in the US include those trained by the US medical education system, and those that are international medical graduates who have progressed through the necessary steps to acquire a medical license to practice in a state.
This includes going through the three steps of the US Medical Licensing Examination (USMLE).
- The first step of the USMLE tests whether medical students both understand and are capable of applying the basic scientific foundations to medicine after the second year of medical school.
- The topics include:
- anatomy,
- biochemistry,
- microbiology,
- pathology,
- pharmacology,
- physiology,
- behavioral sciences,
- nutrition,
- genetics, and aging.
- The second step is designed to test whether medical students can apply their medical skills and knowledge to actual clinical practice during students' fourth year of medical school.
- The third step is done after the first year of residency. It tests whether students can apply medical knowledge to the unsupervised practice of medicine.
The American College of Physicians, uses the term "physician" to describe all medical practitioners holding a professional medical degree. In the US, the vast majority of physicians have a Doctor of Medicine (M.D.) degree. Those with Doctor of Osteopathic Medicine (D.O.) degrees get similar training and go through the same MLE steps as MD's and so are also allowed to use the title "physician".
Medical products, research, and development:
As in most other countries, the manufacture and production of pharmaceuticals and medical devices is carried out by private companies. The research and development of medical devices and pharmaceuticals is supported by both public and private sources of funding.
In 2003, research and development expenditures were approximately $95 billion (equivalent to $136 billion in 2021) with $40 billion (equivalent to $57.3 billion in 2021) coming from public sources and $55 billion (equivalent to $78.8 billion in 2021) coming from private sources.
These investments into medical research have made the US the leader in medical innovation, measured either in terms of revenue or the number of new drugs and devices introduced.
In 2016, the research and development spending by pharmaceutical companies in the US was estimated to be around $59 billion (equivalent to $66 billion in 2021). In 2006, the US accounted for three quarters of the world's biotechnology revenues and 82% of world R&D spending in biotechnology.
According to multiple international pharmaceutical trade groups, the high cost of patented drugs in the US has encouraged substantial reinvestment in such research and development.
However, the ACA will force industry to sell medicine at a cheaper price. Due to this, it is possible budget cuts will be made on research and development of human health and medicine in the US.
Healthcare provider employment in the US:
A major impending demographic shift in the US will require the healthcare system to provide more care, as the older population is predicted to increase medical expenses by 5% or more in North America due to the "baby boomers" reaching retirement age.
The overall spending on healthcare has increased since the late 1990s, and not just due to general price raises as the rate of spending is growing faster than the rate of inflation.
Moreover, the expenditure on health services for people over 45 years old is 8.3 times the maximum of that of those under 45 years old.
Alternative medicine:
Other methods of medical treatment are being practiced more frequently than before. This field is labeled Complementary and Alternative Medicine (CAM) and are defined as therapies generally not taught in medical school nor available in hospitals. They include:
- herbs,
- massages,
- energy healing,
- homeopathy,
- faith healing,
- and, more recently popularized:
- cryotherapy,
- cupping,
- and Transcranial Magnetic Stimulation or TMS.
Providers of these CAM treatments are sometimes legally considered healthcare providers in the US. Common reasons for seeking these alternative approaches included improving their well-being, engaging in a transformational experience, gaining more control over their own health, or finding a better way to relieve symptoms caused by chronic disease. They aim to treat not just physical illness but fix its underlying nutritional, social, emotional, and spiritual causes.
In a 2008 survey, it was found that 37% of hospitals in the US offer at least one form of CAM treatment, the main reason being patient demand (84% of hospitals). Costs for CAM treatments average $33.9 (equivalent to $44.30 in 2021) with two-thirds being out-of-pocket, according to a 2007 statistical analysis. Moreover, CAM treatments covered 11.2% of total out-of-pocket payments on healthcare.
During 2002 to 2008, spending on CAM was on the rise, but usage has since plateaued to about 40% of adults in the US.
Spending:
Main articles:
The US spends more as a percentage of GDP than similar countries, and this can be explained either through higher prices for services themselves, higher costs to administer the system, or more utilization of these services, or to a combination of these elements.
Healthcare costs rising far faster than inflation have been a major driver for healthcare reform in the US. As of 2016, the US spent $3.3 trillion (equivalent to $3.69 trillion in 2021; 17.9% of GDP), or $10,438 (equivalent to $11,785 in 2021) per person; major categories included 32% on hospital care, 20% on physician and clinical services, and 10% on prescription drugs. In comparison, the United Kingdom spent $3,749 (equivalent to $4,233 in 2021) per person.
In 2018, an analysis concluded that prices and administrative costs were largely the cause of the high costs, including prices for labor, pharmaceuticals, and diagnostics. The combination of high prices and high volume can cause particular expense; in the US, high-margin high-volume procedures include angioplasties, C-sections, knee replacements, and CT and MRI scans; CT and MRI scans also showed higher utilization in the US.
Aggregate US hospital costs were $387.3 billion in 2011—a 63% increase since 1997 (inflation adjusted). Costs per stay increased 47% since 1997, averaging $10,000 in 2011 (equivalent to $12,046 in 2021). As of 2008, public spending accounts for between 45% and 56% of US healthcare spending. Surgical, injury, and maternal and neonatal health hospital visit costs increased by more than 2% each year from 2003–2011.
Further, while average hospital discharges remained stable, hospital costs rose from $9,100 in 2003 (equivalent to $13,405 in 2021) to $10,600 in 2011 (equivalent to $12,769 in 2021) and were projected to be $11,000 by 2013 (equivalent to $12,796 in 2021).
According to the WHO, total healthcare spending in the US was 18% of its GDP in 2011, the highest in the world. The Health and Human Services Department expects that the health share of GDP will continue its historical upward trend, reaching 19% of GDP by 2017.
Of each dollar spent on healthcare in the US:
- 31% goes to hospital care,
- 21% goes to physician/clinical services,
- 10% to pharmaceuticals,
- 4% to dental,
- 6% to nursing homes and 3% to home healthcare,
- 3% for other retail products,
- 3% for government public health activities,
- 7% to administrative costs,
- 7% to investment,
- and 6% to other professional services (physical therapists, optometrists, etc.).
In 2017, a study estimated that nearly half of hospital-associated care resulted from emergency department visits.
As of 2017, data from 2009–2011 showed that end-of-life care in the last year of life accounted for about 8.5%, and the last three years of life about 16.7%.
As of 2013, administration of healthcare constituted 30% of US healthcare costs. Free-market advocates claim that the healthcare system is "dysfunctional" because the system of third-party payments from insurers removes the patient as a major participant in the financial and medical choices that affect costs.
The Cato Institute claims that because government intervention has expanded insurance availability through programs such as Medicare and Medicaid, this has exacerbated the problem.
According to a study paid for by America's Health Insurance Plans (a Washington lobbyist for the health insurance industry) and carried out by PriceWaterhouseCoopers, increased utilization is the primary driver of rising healthcare costs in the US.
The study cites numerous causes of increased utilization, including:
- rising consumer demand,
- new treatments,
- more intensive diagnostic testing,
- lifestyle factors,
- the movement to broader-access plans,
- and higher-priced technologies.
The study also mentions cost-shifting from government programs to private payers. Low reimbursement rates for Medicare and Medicaid have increased cost-shifting pressures on hospitals and doctors, who charge higher rates for the same services to private payers, which eventually affects health insurance rates.
In March 2010, Massachusetts released a report on the cost drivers which it called "unique in the nation". The report noted that providers and insurers negotiate privately, and therefore the prices can vary between providers and insurers for the same services, and it found that the variation in prices did not vary based on quality of care but rather on market leverage; the report also found that price increases rather than increased utilization explained the spending increases in the past several years.
Economists Eric Helland and Alex Tabarrok speculate that the increase in costs of healthcare in the US are largely a result of the Baumol effect. Since healthcare is relatively labor intensive, and productivity in the service sector has lagged that in the goods-producing sector, the costs of those services will rise relative to goods.
Regulation and oversight:
Further information:
- American Board of Medical Specialties,
- United States Medical Licensing Examination,
- National Association of Insurance Commissioners
Involved organizations and institutions:
Healthcare is subject to extensive regulation at both the federal and the state level, much of which "arose haphazardly". Under this system, the federal government cedes primary responsibility to the states under the McCarran–Ferguson Act.
Essential regulation includes the licensure of healthcare providers at the state level and the testing and approval of pharmaceuticals and medical devices by the Food and Drug Administration (FDA), and laboratory testing. These regulations are designed to protect consumers from ineffective or fraudulent healthcare.
Additionally, states regulate the health insurance market and they often have laws which require that health insurance companies cover certain procedures, although state mandates generally do not apply to the self-funded healthcare plans offered by large employers, which exempt from state laws under preemption clause of the Employee Retirement Income Security Act.
In 2010, the ACA was signed by President Barack Obama and includes various new regulations, with one of the most notable being a health insurance mandate which requires all citizens to purchase health insurance. While not regulation per se, the federal government also has a major influence on the healthcare market through its payments to providers under Medicare and Medicaid, which in some cases are used as a reference point in the negotiations between medical providers and insurance companies.
At the federal level, US Department of Health and Human Services (HHS) oversees the various federal agencies involved in healthcare. The health agencies are a part of the US Public Health Service, and include the:
- FDA, which certifies the safety of food, effectiveness of drugs and medical products,
- the CDC, which prevents disease, premature death, and disability,
- the Agency of Health Care Research and Quality,
- the Agency Toxic Substances and Disease Registry, which regulates hazardous spills of toxic substances,
- and the National Institutes of Health, which conducts medical research.
State governments maintain state health departments, and local governments
(counties and municipalities) often have their own health departments, usually branches of the state health department. Regulations of a state board may have executive and police strength to enforce state health laws. In some states, all members of state boards must be healthcare professionals.
Members of state boards may be assigned by the governor or elected by the state committee. Members of local boards may be elected by the mayor council. The McCarran–Ferguson Act, which cedes regulation to the states, does not itself regulate insurance, nor does it mandate that states regulate insurance.
"Acts of Congress" that do not expressly purport to regulate the "business of insurance" will not preempt state laws or regulations that regulate the "business of insurance". The act also provides that federal anti-trust laws will not apply to the "business of insurance" as long as the state regulates in that area, but federal anti-trust laws will apply in cases of boycott, coercion, and intimidation.
By contrast, most other federal laws will not apply to insurance, whether the states regulate in that area or not.
Self-policing of providers by providers is a major part of oversight. Many healthcare organizations also voluntarily submit to inspection and certification by the Joint Commission on Accreditation of Hospital Organizations (JCAHO).
Providers also undergo testing to obtain board certification attesting to their skills. A report issued by Public Citizen in April 2008 found that, for the third year in a row, the number of serious disciplinary actions against physicians by state medical boards declined from 2006 to 2007, and called for more oversight of the boards.
The federal Centers for Medicare and Medicaid Services (CMS) publishes an online searchable database of performance data on nursing homes.
In 2004, libertarian think tank Cato Institute published a study which concluded that regulation provides benefits in the amount of $170 billion but costs the public up to $340 billion. The study concluded that the majority of the cost differential arises from medical malpractice, FDA regulations, and facilities regulations.
"Certificates of need" for hospitals:
In 1978, the federal government required that all states implement Certificate of Need (CON) programs for cardiac care, meaning that hospitals had to apply and receive certificates prior to implementing the program; the intent was to reduce cost by reducing duplicate investments in facilities.
It has been observed that these certificates could be used to increase costs through weakened competition. Many states removed the CON programs after the federal requirement expired in 1986, but some states still have these programs. Empirical research looking at the costs in areas where these programs have been discontinued have not found a clear effect on costs, and the CON programs could decrease costs because of reduced facility construction or increase costs due to reduced competition.
Licensing of providers:
The American Medical Association (AMA) has lobbied the government to highly limit physician education since 1910, currently at 100,000 doctors per year, which has led to a shortage of doctors.
An even bigger problem may be that the doctors are paid for procedures instead of results.
The AMA has also aggressively lobbied for many restrictions that require doctors to carry out operations that might be carried out by cheaper workforce. For example, in 1995, 36 states banned or restricted midwifery even though it delivers equally safe care to that by doctors.
The regulation lobbied by the AMA has decreased the amount and quality of healthcare, according to the consensus of economists: the restrictions do not add to quality, they decrease the supply of care. Moreover, psychologists, nurses and pharmacists are not allowed to prescribe medicines. Previously nurses were not even allowed to vaccinate the patients without direct supervision by doctors.
36 states require that healthcare workers undergo criminal background checks.
Emergency Medical Treatment and Active Labor Act (EMTALA):
Main article: Emergency Medical Treatment and Active Labor Act
EMTALA, enacted by the federal government in 1986, requires that hospital emergency departments treat emergency conditions of all patients regardless of their ability to pay and is considered a critical element in the "safety net" for the uninsured, but established no direct payment mechanism for such care.
Indirect payments and reimbursements through federal and state government programs have never fully compensated public and private hospitals for the full cost of care mandated by EMTALA. More than half of all emergency care in the US now goes uncompensated.
According to some analyses, EMTALA is an unfunded mandate that has contributed to financial pressures on hospitals in the last 20 years, causing them to consolidate and close facilities, and contributing to emergency room overcrowding.
According to the Institute of Medicine, between 1993 and 2003, emergency room visits in the US grew by 26%, while in the same period, the number of emergency departments declined by 425.
Mentally ill patients present a unique challenge for emergency departments and hospitals. In accordance with EMTALA, mentally ill patients who enter emergency rooms are evaluated for emergency medical conditions. Once mentally ill patients are medically stable, regional mental health agencies are contacted to evaluate them.
Patients are evaluated as to whether they are a danger to themselves or others. Those meeting this criterion are admitted to a mental health facility to be further evaluated by a psychiatrist. Typically, mentally ill patients can be held for up to 72 hours, after which a court order is required.
Quality assurance:
See also: Hospital Quality Incentive Demonstration
Healthcare quality assurance consists of the "activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps."
Private companies such as Grand Rounds also release quality information and offer services to employers and plans to map quality within their networks.
One innovation in encouraging quality of healthcare is the public reporting of the performance of hospitals, health professionals or providers, and healthcare organizations.
However, there is "no consistent evidence that the public release of performance data changes consumer behaviour or improves care".
Overall system effectiveness:
Measures of effectiveness:
The US healthcare delivery system unevenly provides medical care of varying quality to its population. In a highly effective healthcare system, individuals would receive reliable care that meets their needs and is based on the best scientific knowledge available.
In order to monitor and evaluate system effectiveness, researchers and policy makers track system measures and trends over time. The HHS populates a publicly available dashboard called the Health System Measurement Project (healthmeasures.aspe.hhs.gov), to ensure a robust monitoring system.
The dashboard captures the access, quality and cost of care; overall population health; and health system dynamics (e.g., workforce, innovation, health information technology).
Included measures align with other system performance measuring activities, include the following:
- the HHS Strategic Plan,
- the Government Performance and Results Act,
- Healthy People 2020,
- and the National Strategies for Quality and Prevention.
Waiting times:
Waiting times in US healthcare are usually short, but are not usually 0 for non-urgent care at least. Also, a minority of US patients wait longer than is perceived. In a 2010 Commonwealth Fund survey, most Americans self-reported waiting less than four weeks for their most recent specialist appointment and less than one month for elective surgery.
However, about 30% of patients reported waiting longer than one month for elective surgery, and about 20% longer than four weeks for their most recent specialist appointment.
These percentages were smaller than in France, the UK, New Zealand, and Canada, but not better than Germany and Switzerland (although waits shorter than four weeks/one month may not be equally long across these three countries).
The number of respondents may not be enough to be fully representative. In a study in 1994 comparing Ontario to three regions of the US, self-reported mean wait times to see an orthopedic surgeon were two weeks in those parts of the US, and four weeks in Canada.
Mean waits for the knee or hip surgery were self-reported as three weeks in those parts of the US and eight weeks in Ontario.
However, current waits in both countries' regions may have changed since then (certainly in Canada waiting times went up later).
More recently, at one Michigan hospital, the waiting time for the elective surgical operation open carpel tunnel release was an average of 27 days, most ranging from 17 to 37 days (an average of almost four weeks, ranging from about 2.4 weeks to 5.3 weeks). This appears to be short compared with Canada's waiting time but may compare less favorably to countries like Germany, the Netherlands (where the goal was five weeks), and Switzerland.
It is unclear how many of the patients waiting longer have to. Some may be by choice, because they wish to go to a well-known specialist or clinic that many people wish to attend, and are willing to wait to do so. Waiting times may also vary by region.
One experiment reported that uninsured patients experienced longer waits; patients with poor insurance coverage probably face a disproportionate number of long waits.
US healthcare tends to rely on rationing by exclusion (uninsured and underinsured), out-of-pocket costs for the insured, fixed payments per case to hospitals (resulting in very short stays), and contracts that manage demand instead.
Population health: quality, prevention, vulnerable populations:
The health of the population is also viewed as a measure of the overall effectiveness of the healthcare system. The extent to which the population lives longer healthier lives signals an effective system.
- While life expectancy is one measure, the HHS uses a composite health measure that estimates not only the average length of life but also the part of life expectancy that is expected to be "in good or better health, as well as free of activity limitations". Between 1997 and 2010, the number of expected high quality life years increased from 61.1 to 63.2 years for newborns.
- The underutilization of preventative measures, rates of preventable illness and prevalence of chronic disease suggest that the US healthcare system does not sufficiently promote wellness. Over the past decade rates of teen pregnancy and low birth rates have come down significantly, but not disappeared. Rates of obesity, heart disease (high blood pressure, controlled high cholesterol), and type 2 diabetes are areas of major concern. While chronic disease and multiple comorbidities became increasingly common among a population of elderly Americans who were living longer, the public health system has also found itself fending off a rise of chronically ill younger generation. According to the US Surgeon General "The prevalence of obesity in the US more than doubled (from 15% to 34%) among adults and more than tripled (from 5% to 17%) among children and adolescents from 1980 to 2008."
- A concern for the health system is that the health gains do not accrue equally to the entire population. In the US, disparities in healthcare and health outcomes are widespread. Minorities are more likely to develop serious illnesses (e.g., type 2 diabetes, heart disease and colon cancer) and less likely to have access to quality healthcare, including preventative services. Efforts are underway to close the gap and to provide a more equitable system of care.
Innovation: workforce, healthcare IT, R&D:
Finally, the US tracks investment in the healthcare system in terms of a skilled healthcare workforce, meaningful use of healthcare IT, and R&D output. This aspect of the healthcare system performance dashboard is important to consider when evaluating cost of care in the US. That is because in much of the policy debate around the high cost of US healthcare, proponents of highly specialized and cutting-edge technologies point to innovation as a marker of an effective healthcare system.
Compared to other countries:
Further information: Comparison of the healthcare systems in Canada and the United States
A 2014 study by the private US foundation Commonwealth Fund found that although the US healthcare system is the most expensive in the world, it ranks last on most dimensions of performance when compared with:
- Australia,
- Canada,
- France,
- Germany,
- the Netherlands,
- New Zealand,
- Norway,
- Sweden,
- Switzerland,
- and the UK.
The study found that the US failed to achieve better outcomes than other countries, and is last or near last in terms of access, efficiency, and equity. Study data came from international surveys of patients and primary care physicians, as well as information on healthcare outcomes from Commonwealth Fund, the WHO, and the OECD.
As of 2017, the US stands 43rd in the world with a life expectancy of 80.00 years. The CIA World Factbook ranked the US 170th worst (out of 225)—meaning 55th best—in the world for infant mortality rate (5.80/1,000 live births). Americans also undergo cancer screenings at significantly higher rates than people in other developed countries, and access MRI and CT scans at the highest rate of any OECD nation.
A study found that between 1997 and 2003, preventable deaths declined more slowly in the US than in 18 other industrialized nations. A 2008 study found that 101,000 people a year die in the US that would not if the healthcare system were as effective as that of France, Japan, or Australia.
A 2020 study by the economists Anne Case and Angus Deaton argues that the US "spends huge sums of money for some of the worst health outcomes in the Western world".
The OECD found that the US ranked poorly in terms of years of potential life lost (YPLL), a statistical measure of years of life lost under the age of 70 that were amenable to being saved by healthcare. Among OECD nations for which data are available, the US ranked third last for the healthcare of women (after Mexico and Hungary) and fifth last for men (Slovakia and Poland also ranked worse).
Recent studies find growing gaps in life expectancy based on income and geography. In 2008, a government-sponsored study found that life expectancy declined from 1983 to 1999 for women in 180 counties, and for men in 11 counties, with most of the life expectancy declines occurring in the Deep South, Appalachia, along the Mississippi River, in the Southern Plains, and in Texas.
The difference is as high as three years for men, six years for women. The gap is growing between rich and poor and by educational level, but narrowing between men and women and by race.
Another study found that the mortality gap between the well-educated and the poorly educated widened significantly between 1993 and 2001 for adults ages 25 through 64; the authors speculated that risk factors such as smoking, obesity and high blood pressure may lie behind these disparities.
In 2011 the US National Research Council forecasted that deaths attributed to smoking, on the decline in the US, will drop dramatically, improving life expectancy; it also suggested that one-fifth to one-third of the life expectancy difference can be attributed to obesity which is the worst in the world and has been increasing.
In an analysis of breast cancer, colorectal cancer, and prostate cancer diagnosed during 1990–1994 in 31 countries, the US had the highest five-year relative survival rate for breast cancer and prostate cancer, although survival was systematically and substantially lower in Black US men and women.
The debate about US healthcare concerns questions of access, efficiency, and quality purchased by the high sums spent. The WHO in 2000 ranked the US healthcare system first in responsiveness, but 37th in overall performance and 72nd by overall level of health (among 191 member nations included in the study). The WHO study has been criticized by the free market advocate David Gratzer because "fairness in financial contribution" was used as an assessment factor, marking down countries with high per-capita private or fee-paying health treatment.
The WHO study has been criticized, in an article published in Health Affairs, for its failure to include the satisfaction ratings of the general public. The study found that there was little correlation between the WHO rankings for health systems and the stated satisfaction of citizens using those systems.
Countries such as Italy and Spain, which were given the highest ratings by WHO were ranked poorly by their citizens while other countries, such as Denmark and Finland, were given low scores by WHO but had the highest percentages of citizens reporting satisfaction with their healthcare systems.
WHO staff, however, say that the WHO analysis does reflect system "responsiveness" and argue that this is a superior measure to consumer satisfaction, which is influenced by expectations. Furthermore, the relationship between patient satisfaction and healthcare utilization, expenditures, clinically meaningful measures, and the evaluation of outcomes is complex, not well defined, and only beginning to be explored.
A report released in April 2008 by the Foundation for Child Development, which studied the period from 1994 through 2006, found mixed results for the health of children in the US Mortality rates for children ages 1 through 4 dropped by a third, and the percentage of children with elevated blood lead levels dropped by 84%.
The percentage of mothers who smoked during pregnancy also declined. On the other hand, both obesity and the percentage of low-birth weight babies increased. The authors note that the increase in babies born with low birth weights can be attributed to women delaying childbearing and the increased use of fertility drugs.
In a sample of 13 developed countries, the US was third in its population weighted usage of medication in 14 classes in both 2009 and 2013. The drugs studied were selected on the basis that the conditions treated had high incidence, prevalence and/or mortality, caused significant long-term morbidity and incurred high levels of expenditure and significant developments in prevention or treatment had been made in the last 10 years. The study noted considerable difficulties in cross border comparison of medication use.
A critic of the US healthcare system, British philanthropist Stan Brock, whose charity Remote Area Medical has served over half a million uninsured Americans, stated, "You could be blindfolded and stick a pin on a map of America and you will find people in need."
The charity has over 700 clinics and 80,000 volunteer doctors and nurses around the US Simon Usborne of The Independent writes that in the UK "General practitioners are amazed to hear that poor Americans should need to rely on a charity that was originally conceived to treat people in the developing world."
System efficiency and equity:
Variations in the efficiency of healthcare delivery can cause variations in outcomes. The Dartmouth Atlas Project, for instance, reported that, for over 20 years, marked variations in how medical resources are distributed and used in the US were accompanied by marked variations in outcomes.
The willingness of physicians to work in an area varies with the income of the area and the amenities it offers, a situation aggravated by a general shortage of doctors in the US, particularly those who offer primary care. The ACA is anticipated to produce an additional demand for services which the existing stable of primary care doctors will be unable to fill, particularly in economically depressed areas. Training additional physicians would require some years.
Lean manufacturing techniques such as value stream mapping can help identify and subsequently mitigate waste associated with costs of healthcare. Other product engineering tools such as FMEA and Fish Bone Diagrams have been used to improve efficiencies in healthcare delivery.
Since 2004 the Commonwealth Fund has produced reports comparing healthcare systems in high income countries using survey and administrative data from the OECD and WHO which is analyzed under five themes:
- access to care,
- the care process,
- administrative efficiency,
- equity
- and healthcare outcomes.
The US has been assessed as worst healthcare system overall among 11 high-income countries in every report, even though it spends the highest proportion of its gross domestic product on healthcare.
In 2021 Norway, the Netherlands and Australia were the top-performing countries. The US spent 16.8% of GDP on healthcare in 2019; the next highest country on the list was Switzerland, at 11.3% of GDP. The lowest was New Zealand, which spent roughly 9% of its GDP on healthcare in 2019. It "consistently demonstrated the largest disparities between income groups" across indicators, apart from those related to preventive services and the safety of care.
Efficiency:
Preventable deaths:
In 2010, coronary artery disease, lung cancer, stroke, chronic obstructive pulmonary diseases, and traffic accidents caused the most years of life lost in the US. Low back pain, depression, musculoskeletal disorders, neck pain, and anxiety caused the most years lost to disability. The most deleterious risk factors were:
- poor diet,
- tobacco smoking,
- obesity,
- high blood pressure,
- high blood sugar,
- physical inactivity,
- and alcohol use.
Alzheimer's disease, drug abuse, kidney disease and cancer, and falls caused the most additional years of life lost over their age-adjusted 1990 per-capita rates.
Between 1990 and 2010, among the 34 countries in the OECD, the US dropped from 18th to 27th in age-standardized death rate. The US dropped from 23rd to 28th for age-standardized years of life lost. It dropped from 20th to 27th in life expectancy at birth. It dropped from 14th to 26th for healthy life expectancy.
According to a 2009 study conducted at Harvard Medical School by cofounders of Physicians for a National Health Program, a pro-single payer lobbying group, and published by the American Journal of Public Health, lack of health coverage is associated with nearly 45,000 excess preventable deaths annually.
Since then, as the number of uninsured has risen from about 46 million in 2009 to 49 million in 2012, the number of preventable deaths due to lack of insurance has grown to about 48,000 per year.
The group's methodology has been criticized by economist John C. Goodman for not looking at cause of death or tracking insurance status changes over time, including the time of death.
A 2009 study by former Clinton policy adviser Richard Kronick published in the journal Health Services Research found no increased mortality from being uninsured after certain risk factors were controlled for.
Value for money:
A study of international healthcare spending levels published in the health policy journal Health Affairs in the year 2000 found that the US spends substantially more on healthcare than any other country in the OECD (OECD), and that the use of healthcare services in the US is below the OECD median by most measures.
The authors of the study conclude that the prices paid for healthcare services are much higher in the US than elsewhere. While the 19 next most wealthy countries by GDP all pay less than half what the US does for healthcare, they have all gained about six years of life expectancy more than the US since 1970.
Delays in seeking care and increased use of emergency care:
Uninsured Americans are less likely to have regular healthcare and use preventive services. They are more likely to delay seeking care, resulting in more medical crises, which are more expensive than ongoing treatment for such conditions as diabetes and high blood pressure.
A 2007 study published in JAMA concluded that uninsured people were less likely than the insured to receive any medical care after an accidental injury or the onset of a new chronic condition.
The uninsured with an injury were also twice as likely as those with insurance to have received none of the recommended follow-up care, and a similar pattern held for those with a new chronic condition. Uninsured patients are twice as likely to visit hospital emergency rooms as those with insurance; burdening a system meant for true emergencies with less-urgent care needs.
In 2008 researchers with the American Cancer Society found that individuals who lacked private insurance (including those covered by Medicaid) were more likely to be diagnosed with late-stage cancer than those who had such insurance.
Variations in provider practices:
The treatment given to a patient can vary significantly depending on which healthcare providers they use. Research suggests that some cost-effective treatments are not used as often as they should be, while overutilization occurs with other healthcare services.
Unnecessary treatments increase costs and can cause patients unnecessary anxiety. The use of prescription drugs varies significantly by geographic region. The overuse of medical benefits is known as moral hazard—individuals who are insured are then more inclined to consume healthcare.
The way the healthcare system tries to eliminate this problem is through cost-sharing tactics like copays and deductibles. If patients face more of the economic burden they will then only consume healthcare when they perceive it to be necessary. According to the RAND health insurance experiment, individuals with higher coinsurance rates consumed less healthcare than those with lower rates.
The experiment concluded that with less consumption of care there was generally no loss in societal welfare but, for the poorer and sicker groups of people there were definitely negative effects. These patients were forced to forgo necessary preventative care measures in order to save money leading to late diagnosis of easily treated diseases and more expensive procedures later.
With less preventative care, the patient is hurt financially with an increase in expensive visits to the ER. The healthcare costs in the US will also rise with these procedures as well. More expensive procedures lead to greater costs.
One study has found significant geographic variations in Medicare spending for patients in the last two years of life. These spending levels are associated with the amount of hospital capacity available in each area. Higher spending did not result in patients living longer.
Care coordination:
Primary care doctors are often the point of entry for most patients needing care, but in the fragmented healthcare system of the US, many patients and their providers experience problems with care coordination.
For example, a Harris Interactive survey of California physicians found that:
- Four of every ten physicians report that their patients have had problems with coordination of their care in the last 12 months.
- More than 60% of doctors report that their patients "sometimes" or "often" experience long wait times for diagnostic tests.
- Some 20% of doctors report having their patients repeat tests because of an inability to locate the results during a scheduled visit.
According to an article in The New York Times, the relationship between doctors and patients is deteriorating. A study from Johns Hopkins University found that roughly one in four patients believe their doctors have exposed them to unnecessary risks, and anecdotal evidence such as self-help books and web postings suggest increasing patient frustration.
Possible factors behind the deteriorating doctor/patient relationship include the current system for training physicians and differences in how doctors and patients view the practice of medicine. Doctors may focus on diagnosis and treatment, while patients may be more interested in wellness and being listened to by their doctors.
Many primary care physicians no longer see their patients while they are in the hospital; instead, hospitalists are used. The use of hospitalists is sometimes mandated by health insurance companies as a cost-saving measure which is resented by some primary care physicians.
Administrative costs:
As of 2017, there were 907 health insurance companies in the US, although the top 10 account for about 53% of revenue and the top 100 account for 95% of revenue. The number of insurers contributes to administrative overhead in excess of that in nationalized, single-payer systems, such as that in Canada, where administrative overhead was estimated to be about half of the US.
Insurance industry group America's Health Insurance Plans estimates that administrative costs have averaged approximately 12% of premiums over the last 40 years, with costs shifting away from adjudicating claims and towards medical management, nurse help lines, and negotiating discounted fees with healthcare providers.
A 2003 study published by the Blue Cross and Blue Shield Association (BCBSA) also found that health insurer administrative costs were approximately 11% to 12% of premiums, with Blue Cross and Blue Shield plans reporting slightly lower administrative costs, on average, than commercial insurers.
For the period 1998 through 2003, average insurer administrative costs declined from 13% to 12% of premiums. The largest increases in administrative costs were in customer service and information technology, and the largest decreases were in provider services and contracting and in general administration.
The McKinsey Global Institute estimated that excess spending on "health administration and insurance" accounted for as much as 21% of the estimated total excess spending ($477 billion in 2003).
According to a report published by the CBO in 2008, administrative costs for private insurance represent approximately 12% of premiums. Variations in administrative costs between private plans are largely attributable to economies of scale. Coverage for large employers has the lowest administrative costs. The percentage of premium attributable to administration increases for smaller firms, and is highest for individually purchased coverage.
A 2009 study published by BCBSA found that the average administrative expense cost for all commercial health insurance products was represented 9.2% of premiums in 2008. Administrative costs were 11.1% of premiums for small group products and 16.4% in the individual market.
One study of the billing and insurance-related (BIR) costs borne not only by insurers but also by physicians and hospitals found that BIR among insurers, physicians, and hospitals in California represented 20–22% of privately insured spending in California acute care settings.
Long-term living facilities:
As of 2014, according to a report published the higher the skill of the RN the lower the cost of a financial burden on the facilities. With a growing elderly population, the number of patients in these long term facilities needing more care creates a jump in financial costs.
Based on research done in 2010, annual out of pocket costs jumped 7.5% while the cost for Medicare grew 6.7% annually due to the increases. While Medicare pays for some of the care that the elderly populations receive, 40% of the patients staying in these facilities pay out of pocket.
Third-party payment problem and consumer-driven insurance:
Most Americans pay for medical services largely through insurance, and this can distort the incentives of consumers since the consumer pays only a portion of the ultimate cost directly. The lack of price information on medical services can also distort incentives.
The insurance which pays on behalf of insureds negotiate with medical providers, sometimes using government-established prices such as Medicaid billing rates as a reference point.This reasoning has led for calls to reform the insurance system to create a consumer-driven healthcare system whereby consumers pay more out-of-pocket.
In 2003, the Medicare Prescription Drug, Improvement, and Modernization Act was passed, which encourages consumers to have a high-deductible health plan and a health savings account.
In October 2019, the state of Colorado proposed running public healthcare option through private insurers, which are to bear the brunt of the costs. Premiums under the public option are touted to be 9% to 18% cheaper by 2022.
Equity:
Mental health:
See also: Mental health § United States, and Mentally ill prisoners in the United States
In 2020, 52.9 million adults were affected by mental illness, nearly one in five adults in the country. 44.7 million adults were affected in 2016.
In 2006, mental disorders were ranked one of the top five most costly medical conditions, with expenditures of $57.5 billion (equivalent to $75.5 billion in 2021). A lack of mental health coverage for Americans bears significant ramifications to the US economy and social system.
A report by the US Surgeon General found that mental illnesses are the second leading cause of disability in the nation and affect 20% of all Americans.
It is estimated that less than half of all people with mental illnesses receive treatment (or specifically, an ongoing, much needed, and managed care; where medication alone, cannot easily remove mental conditions) due to factors such as stigma and lack of access to care, including a shortage of mental health professionals.
Treatment rates are understood to vary between different conditions; as an example, only 16% of adults with schizophrenia and 25% with bipolar disorder were estimated to be untreated with appropriate medication in 2007.
The Paul Wellstone Mental Health and Addiction Equity Act of 2008 mandates that group health plans provide mental health and substance-related disorder benefits that are at least equivalent to benefits offered for medical and surgical procedures.
The legislation renews and expands provisions of the Mental Health Parity Act of 1996. The law requires financial equity for annual and lifetime mental health benefits, and compels parity in treatment limits and expands all equity provisions to addiction services.
Insurance companies and third-party disability administrators (most notably, Sedgwick CMS) used loopholes and, though providing financial equity, they often worked around the law by applying unequal copayments or setting limits on the number of days spent in inpatient or outpatient treatment facilities.
Oral health:
In the US, dental care is largely not recognized as healthcare, even though individuals visit a dentist more often than a general practitioner, and thus the field and its practices developed independently. In modern policy and practice, oral health is thus considered distinct from primary health, and dental insurance is separate from health insurance.
Disparities in oral healthcare accessibility mean that many populations, including those without insurance, the low-income, uninsured, racial minorities, immigrants, and rural populations, have a higher probability of poor oral health at every age. While changes have been made to address these disparities for children, the oral health disparity in adults of all previously listed populations has remained consistent or worsened.
The magnitude of this health issue is surprising even in New York state, where the Medicaid program includes dental coverage and is one of the most impressive insurance programs in the nation. Seven out of ten older adults (aged ≥ 65) have periodontal disease, and one in four adults (aged > 65) has no teeth.
This raises concern about the New York State Department of Health's rule, which prevents Medicaid coverage for the replacement of dentures within eight years of initial placement and a ban on coverage of dental implants. In addition, older adults are more likely than those in younger age groups to have medical conditions, such as diabetes and cardiovascular disease, that worsen their oral health.
Medical underwriting and the uninsurable:
Prior to the ACA, medical underwriting was common, but, after the law came into effect in 2014, it became effectively prohibited.
Demographic differences:
Main articles:
Health disparities are well documented in the US in ethnic minorities such as African Americans, Native Americans, and Hispanics.
When compared to whites, these minority groups have higher incidence of chronic diseases, higher mortality, poorer health outcomes and poorer rates of diagnosis and treatment.
Among the disease-specific examples of racial and ethnic disparities in the US is the cancer incidence rate among African Americans, which is 25% higher than among whites. In addition, adult African Americans and Hispanics have approximately twice the risk as whites of developing diabetes and have higher overall obesity rates.
Minorities also have higher rates of cardiovascular disease and HIV/AIDS than whites. In the US, Asian Americans live the longest (87.1 years), followed by Latinos (83.3 years), whites (78.9 years), Native Americans (76.9 years), and African Americans (75.4 years). A 2001 study found large racial differences exist in healthy life expectancy at lower levels of education.
Public spending is highly correlated with age; average per capita public spending for seniors was more than five times that for children ($6,921 versus $1,225, equivalent to $10,427 versus $1,846 in 2021).
Average public spending for non-Hispanic blacks ($2,973, equivalent to $4,479 in 2021) was slightly higher than that for whites ($2,675, equivalent to $4,030 in 2021),
Spending for Hispanics ($1,967, equivalent to $2,963 in 2021) was significantly lower than the population average ($2,612, equivalent to $3,935 in 2021).
Total public spending is also strongly correlated with self-reported health status ($13,770 (equivalent to $20,745 in 2021) for those reporting "poor" health versus $1,279 (equivalent to $1,927 in 2021) for those reporting "excellent" health.
Seniors comprise 13% of the population but take one-third of all prescription drugs. The average senior fills 38 prescriptions annually. A new study has also found that older men and women in the South are more often prescribed antibiotics than older Americans elsewhere, even though there is no evidence that the South has higher rates of diseases requiring antibiotics.
There is considerable research into inequalities in healthcare. In some cases, these inequalities are caused by income disparities that result in lack of health insurance and other barriers to receiving services.
According to the 2009 National Healthcare Disparities Report, uninsured Americans are less likely to receive preventive services in healthcare. For example, minorities are not regularly screened for colon cancer and the death rate for colon cancer has increased among African Americans and Hispanic people.
In other cases, inequalities in healthcare reflect a systemic bias in the way medical procedures and treatments are prescribed for different ethnic groups. Raj Bhopal writes that the history of racism in science and medicine shows that people and institutions behave according to the ethos of their times.
Nancy Krieger wrote that racism underlies unexplained inequities in healthcare, including treatment for heart disease, renal failure, bladder cancer, and pneumonia. Raj Bhopal writes that these inequalities have been documented in numerous studies.
The consistent and repeated findings were that Black Americans received less healthcare than white Americans—particularly when the care involved expensive new technology. One recent study has found that when minority and white patients use the same hospital, they are given the same standard of care.
Prescription drug issues:
Drug efficiency and safety:
See also: Regulation of therapeutic goods in the United States
The FDA is the primary institution tasked with the safety and effectiveness of human and veterinary drugs. It also is responsible for making sure drug information is accurately and informatively presented to the public. The FDA reviews and approves products and establishes drug labeling, drug standards, and medical device manufacturing standards. It sets performance standards for radiation and ultrasonic equipment.
One of the more contentious issues related to drug safety is immunity from prosecution. In 2004, the FDA reversed a federal policy, arguing that FDA premarket approval overrides most claims for damages under state law for medical devices. In 2008, this was confirmed by the Supreme Court in Riegel v. Medtronic, Inc.
On June 30, 2006, an FDA ruling went into effect extending protection from lawsuits to pharmaceutical manufacturers, even if it was found that they submitted fraudulent clinical trial data to the FDA in their quest for approval. This left consumers who experience serious health consequences from drug use with little recourse.
In 2007, the House of Representatives expressed opposition to the FDA ruling, but the Senate took no action. On March 4, 2009, an important US Supreme Court decision was handed down. In Wyeth v. Levine, the court asserted that state-level rights of action could not be pre-empted by federal immunity and could provide "appropriate relief for injured consumers".
In June 2009, under the Public Readiness and Emergency Preparedness Act, Secretary of Health and Human Services Kathleen Sebelius signed an order extending protection to vaccine makers and federal officials from prosecution during a declared health emergency related to the administration of the swine flu vaccine.
Prescription drug prices:
Main article: Prescription drug prices in the United States
During the 1990s, the price of prescription drugs became a major issue in US politics as the prices of many new drugs increased exponentially, and many citizens discovered that neither the government nor their insurer would cover the cost of such drugs.
Per capita, the US spends more on pharmaceuticals than any other country, although expenditures on pharmaceuticals accounts for a smaller share (13%) of total healthcare costs compared to an OECD average of 18% (2003 figures).
Some 25% of out-of-pocket spending by individuals is for prescription drugs. Another study finds that between 1990 and 2016, prescription drug prices in the US increased by 277% while prescription drug prices increased by only 57% in the UK, 13% in Canada, and decreased in France and Japan.
The US government has taken the position (through the Office of the US Trade Representative) that US drug prices are rising because US consumers are effectively subsidizing costs which drug companies cannot recover from consumers in other countries (because many other countries use their bulk-purchasing power to aggressively negotiate drug prices).
The US position (consistent with the primary lobbying position of the Pharmaceutical Research and Manufacturers of America) is that the governments of such countries are free riding on the backs of US consumers.
Such governments should either deregulate their markets, or raise their domestic taxes in order to fairly compensate US consumers by directly remitting the difference (between what the companies would earn in an open market versus what they are earning now) to drug companies or to the US government.
In turn, pharmaceutical companies would be able to continue to produce innovative pharmaceuticals while lowering prices for US consumers. Currently, the US, as a purchaser of pharmaceuticals, negotiates some drug prices but is forbidden by law from negotiating drug prices for the Medicare program due to the Medicare Prescription Drug, Improvement, and Modernization Act passed in 2003.
Democrats have charged that the purpose of this provision is merely to allow the pharmaceutical industry to profiteer off of the Medicare program.
Impact of drug companies:
The US, along with New Zealand, make up the only countries in the world that allows direct-to-consumer advertising of prescription drugs. In 2015, the American Medical Association called for the banning of direct-to-consumer advertising because it is linked with increased drug prices.
Still, other evidence cites that there are some benefits to direct-to-consumer advertising, such as encouraging patients to see the doctor, diagnosis of rare diseases, and the removal of stigma associated with the disease.
When healthcare legislation was being written in 2009, the drug companies were asked to support the legislation in return for not allowing importation of drugs from foreign countries.
Healthcare reform debate:
Further information: Healthcare reform in the United States and Service Excellence – Health Care
In 2008, prior to the major healthcare reform in 2010, Americans were divided in their views of the US health system; 45% said that the US system was best and 39% said that other countries' systems are better.
Much of the historical debate around healthcare reform centered around single-payer healthcare, and particularly pointing to the hidden costs of treating the uninsured while free-market advocates point to freedom of choice in purchasing health insurance and unintended consequences of government intervention, citing the Health Maintenance Organization Act of 1973.
According to a 2020 study published in The Lancet, a single-payer universal healthcare system could save 68,000 lives and $450 billion in national healthcare expenditure annually, while another 2022 study published in the PNAS, estimated that a universal healthcare system could have saved more than 338,000 lives during the COVID-19 pandemic in the US from its start until March 2022.
Ultimately, a single-payer healthcare, sometimes called "socialized medicine", was not adopted in the final ACA.
Patient Protection and Affordable Care Act (2010):
The ACA (Public Law 111–148) is a healthcare reform bill that was signed into law in the US by President Barack Obama on March 23, 2010. The law includes a large number of health-related provisions, most of which took effect in 2014, including expanding Medicaid eligibility for people making up to 133% of FPL, subsidizing insurance premiums for individuals and families making up to 400% of FPL and capping expenses from 2% to 9.8% of annual income.
For the first time, all health policies sold in the US must cap an individual's (or family's) medical expenses out of pocket annually. Other provisions include providing incentives for businesses to provide healthcare benefits, prohibiting denial of coverage and denial of claims based on pre-existing conditions, establishing health insurance exchanges, prohibiting insurers from establishing annual spending caps and support for medical research.
The costs of these provisions are offset by a variety of taxes, fees, and cost-saving measures, such as new Medicare taxes for high-income brackets, taxes on indoor tanning, cuts to the Medicare Advantage program in favor of traditional Medicare, and fees on medical devices and pharmaceutical companies; there is also a tax penalty for citizens who do not obtain health insurance (unless they are exempt due to low income or other reasons).
The Congressional Budget Office estimates that the net effect (including the reconciliation act) will be a reduction in the federal deficit by $143 billion over the first decade.
However, two months later, the office subsequently acknowledged that there was an additional $115 billion in funds needed that were not originally included in the estimate.
Additionally, the CBO estimated that although projected premiums in 2016 would be lower by $100 per person for small and large business health insurance plans with the ACA than without, individual plans would be higher by $1,900 with the bill.
The first open enrollment period of the ACA began in October 2013. Prior to this period, access to healthcare and insurance coverage trends were worsening on a national level. A large, national survey of US adults found that after the act's first two enrollment periods, self-reported coverage, health, and access to care improved significantly.
Furthermore, insurance coverage for low-income adults were significantly greater in states that expanded Medicaid in comparison with states that did not expand Medicaid. However, discrepancies do exist between those covered by Medicaid versus those covered by private insurance. Those insured by Medicaid tend to report fair or poor health, as opposed to excellent or very good health.
On December 22, 2017, the Tax Cuts and Jobs Act of 2017 was signed into law by President Donald Trump. Inside the final version of the bill was a repeal of the individual mandate in the ACA, which required individuals and companies to get healthcare for themselves and their employees. It was this mandate which kept healthcare costs down under the PPACA by promoting cost sharing over a larger pool.
Economists believe the repeal of the individual mandate will lead to higher premiums and lower enrollment in the current market though they do not agree with how much. In 2017, the new Republican healthcare bill known as the American Health Care Act was passed by the House of Representatives under President Donald Trump. Although the ACA and the American Health Care Act both propose tax cuts in order to make insurance more affordable for Americans, each of these bills affected Americans in different ways.
The people most affected by President Trump's plan are young people, individuals of a higher socioeconomic status, and people who live in urban areas. Young people because individuals between the age of 20 and 30 will see drops in the premiums they pay within their plans.
Individuals with higher socioeconomic status because whereas under Obamacare individuals could only make up to $50,000 annually and still receive tax breaks, now under Trump's plan that number has been increased so that individuals who make up to $115,000 annually can receive tax breaks.
In addition, those in urban areas can also benefit from the plan because under Obamacare tax credits were designated also by the cost of local healthcare, but the American Health Care Act does not take this into consideration although rural healthcare is generally more expensive due to the lack of hospitals and available services.
Health insurance coverage for immigrants:
Main article: Immigrant health care in the United States
Of the 26.2 million foreign immigrants living in the US in 1998, 62.9% were non-US citizens. In 1997, 34.3% of non-US citizens living in the US did not have health insurance coverage opposed to the 14.2% of native-born Americans who do not have health insurance coverage.
Among those immigrants who became citizens, 18.5% were uninsured, as opposed to non-citizens, who are 43.6% uninsured. In each age and income group, immigrants are less likely to have health insurance.
With the recent healthcare changes, many legal immigrants with various immigration statuses now are able qualify for affordable health insurance.
Undocumented immigrants within the US do not have access to government funded health insurance. Although the ACA allows immigrants to receive insurance at a discounted rate, the same does not go for those without US citizenship.
While policies like the Patient Protection Act and Affordable Care Act have aimed at expanding health insurance coverage to also improve refugee health in the US, different states have implemented their health insurance programs differently leading to healthcare access disparities between states.
Undocumented immigrants in the US can seek medical help from community centers, or what is termed Safety Net Providers, and participate in fee for service medical assistance, but can only buy health insurance from private health insurers.
- See also:
- Biomedical research in the United States
- Canadian and American health care systems compared
- Centers for Disease Control and Prevention timeline
- Health Care and Education Reconciliation Act of 2010
- Health care compared – tabular comparisons of the US, Canada, and other countries not shown above.
- Health care industry
- Health care politics
- Health care systems (including comparisons)
- Health insurance cooperative
- Healthy People program
- List of countries by health care expenditures
- List of healthcare accreditation organizations in the United States
- Medical centers in the United States
- Medical debt
- Medical education in the United States
- Medicare for All Act
- Medicare Rights Center
- Medicare Sustainable Growth Rate
- Military Health System
- Osteopathic medicine in the United States
- School health services
- Universal Health Care Foundation of Connecticut
- Visitor health insurance
- National Center for Health Statistics from the CDC
- National Health Expenditure Data (US) from the HHS
- US profile from the WHO
- And Pharma Market Research Report
- Health Care in the United States at Curlie
Therapeutic Lifestyle Changes (TLC)
- YouTube Video: What is the TLC Diet and how does it benefit your heart health?
- YouTube Video: Therapeutic Lifestyle Changes for Prediabetes and Type 2 Diabetes
- YouTube Video: Patient Counseling: Therapeutic Lifestyle Changes (TLC) Diet
* -- All about the Therapeutic Lifestyle Changes (TLC) diet & why it’s heart healthy
Have you heard about the Therapeutic Lifestyle Changes diet? Basically, it was created by the National Cholesterol Education program to help lower a person’s cholesterol. It isn’t a fad diet and it’s based on science.
According to the Centers for Disease Control and Prevention, “TLC is an effective lifestyle therapy targeting low density lipoprotein cholesterol (LDL), a risk factor for coronary heart disease.”
But the benefits don’t stop there. In addition to helping lower LDL, the bad cholesterol, TLC also “improves risk factors associated with the metabolic syndrome and diabetes, including blood pressure, high-density lipoprotein cholesterol (HDL), serum triglycerides, blood glucose, and weight status.”
When you break it down, the TLC diet is more of a lifestyle modification plan than a diet because it’s not just about what you eat. It’s also not something that you do for a couple of weeks to drop 10 pounds.
TLC’s more of a commitment to your long-term health. The goal of this “diet” isn’t to fit into your skinny jeans, although that might happen. The goal is to eat well, manage weight, and exercise so you can be healthy and prevent coronary heart disease. Sounds good, right? Let’s break it down further so you can decide if it’s something that would be beneficial to you.
What is the Therapeutic Lifestyle diet?
The Therapeutic Lifestyle Changes diet was created by the National Institutes of Health’s National Cholesterol Education Program. The main goal of the diet, which is really more than a diet because it incorporates lifestyle changes, is to help cut cholesterol and lower the risk of cardiovascular disease.
The TLC diet can be broken down into three main parts.
The components are: diet, exercise, and weight management.
If you follow the TLC diet, you could see some weight loss, your LDL (bad cholesterol) levels can decrease, your HDL (good cholesterol) levels can increase, and your triglycerides (a fat type in your blood) can decrease. That’s all good stuff and good for your long-term health.
How does it improve heart health?
We’re not doctors here, but basically, the TLC diet recommends healthy lifestyle changes that do your heart good. Changes like keeping your dietary cholesterol below 200 milligrams a day and reducing your saturated fat intake to less that 7% of your total calories.
What are some of the specific dietary recommendations to lower LDL?
To reduce your intake of saturated fat and thereby reduce your LDL, the TLC diet recommends that you choose lean meats and low-fat dairy products. It also recommends no more than three whole egges with yolks a week.
Other dietary changes might require you to add certain foods to your diet.
It’s recommended that you increase your consumption of whole grains to 50% of the grains you eat to help lower LDL. Eating fish two to three times a week is also suggested because it helps lower triglycerides and increases HDL. Eating foods that contain plant sterols or stanols is also encouraged because those substances help lower LDL.
What specific foods are recommended?
Recommended foods include whole grains, fruits, veggies, fish, beans, lentils, oatmeal, whole-grain rice, and foods rich in mono and polyunsaturated fats. Basically, you have a lot of options to choose from.
What kind of foods rich in monosaturated fats are recommended?
You can have avocados, nut butters with no added trans fat, nuts, and seeds. In terms of oils, you can use canola, olive, and peanut oils. Again, you have a lot of options to choose from.
What kinds of polyunsaturated fats can you eat on this diet?
Recommended polyunsaturated fat sources include salmon, tuna, halibut, mackerel, pine nuts, walnuts, flaxseeds, pumpkin and sunflower seeds, as well as sesame seeds. Oils you can use include grape seed oil, safflower oil, and sunflower oil.
You will want to decrease your intake of saturated fats.
It is recommended that you limit your intake of saturated fats to no more than twice a week. Saturated fats can be found in bacon, butter, coconut, coconut milk, cream, cream cheese, sour cream, shortening, and lard. Oils you want to avoid include coconut, palm, and palm kernel.
Can the TLC diet help you lose weight?
If you want to lose weight on this diet the National Heart, Lung, and Blood Institute recommends decreasing your calorie intake by 500 to 1,000 calories a day, which should result in a loss of 1 to 2 pounds per week.
How much exercise is recommended?
To reduce the risk of chronic disease, it’s recommended that adults “engage in at least 30 minutes of moderate-intensity physical activity, above usual activity, at work or home on most days of the week.” That’s the bare minimum recommended.
What other lifestyle modifications need to be made?
It’s recommended that you learn the difference between physical fullness and satiety. Physical fullness happens when you pretty much feel stuffed after eating and that most likely means you ate too much. Satiety happens when your body sends a message to your brain saying that it’s had enough to eat before getting to the point of feeling like your belly is distended.
Is it expensive to follow the TLC diet?
No, it doesn’t have to be. You don’t have to buy any specialized foods or products. You’re just spending money on recommended foods. As for exercise, you don’t have to join a gym or anything. How you get your exercise is up to you.
Is it an easy diet to follow?
If you are looking for a quick fix, this isn’t it. The TLC diet requires that you make changes not just in what you eat, but also how you exercise. These changes aren’t meant to be temporary either.
How do I get started on the TLC diet?
Start by talking to your doctor about the diet. You can both decide if it’s a good option for you and your doctor can provide you with more information and may even recommend you work with a nutritionist.
___________________________________________________________________________
Therapeutic Lifestyle Changes (TLC) (Wikipedia)
Therapeutic Lifestyle Changes, also known as the TLC Diet, is a dietary pattern recommended by the National Cholesterol Education Program, part of the National Institutes of Health, to control hypercholesterolemia. This pattern focuses on saturated fats and cholesterol, dietary options to enhance LDL cholesterol lowering, weight control, and physical activity.
Background/History:
High cholesterol is one of the major controllable risk factors for coronary heart disease, heart attack and stroke. The National Institutes of Health created the National Cholesterol Education Program in 1985 to reduce cardiovascular disease rates in the United States by addressing high cholesterol.
They created the TLC diet to be used alone or in conjunction with medication management to control elevated cholesterol. The diet was incorporated into the Adult Treatment Panel III (ATP III) for high cholesterol in adults which was released in 2002. Updated guidelines for cholesterol management were established in 2013 by the American Heart Association (AHA) and American College of Cardiology (ACC).
Diet Components:
Essential Components of Therapeutic Lifestyle Changes:
The main Therapeutic Lifestyle Changes components include:
After six weeks, The National Cholesterol Education Program recommends checking the LDL cholesterol response to the changes; if the LDL cholesterol goal has not been achieved, other therapeutic options for LDL lowering can be implemented. These include: 2 grams per day of plant stanols or sterols and 10–25 grams per day of soluble fiber.
Macronutrient Distribution of the TLC Diet:
The Therapeutic Lifestyle Changes macronutrient profile includes:
Research Findings:
The recommendations for cholesterol management through lifestyle changes from the National Cholesterol Education Program have evolved over time based on data from epidemiological observations, animal studies, and clinical trials. Animal models have demonstrated a direct relationship between LDL cholesterol and atherosclerosis.
Animals consuming diets high in saturated fat and cholesterol develop LDL cholesterol elevation and atherosclerosis. Epidemiologic evidence in humans supports this direct relationship between LDL cholesterol and coronary heart disease risk.
One randomized crossover study completed at Tufts University and New England Medical Center looked at the Therapeutic Lifestyle Change diet relative to a typical Western diet.
Thirty-six participants with moderately elevated cholesterol levels participated in two 32-day phases where the subjects consumed their normal dietary patterns or the experimental diet consistent with the NCEP recommendations. This diet provided 30% calories from fat, 7% calories from saturated fat, and 75 mg cholesterol per 1,000 calories. Relative to the Western diet, the TLC diet resulted in 11% lower LDL cholesterol.
Additional studies have looked at the benefits of plant stanols and sterols on lowering LDL cholesterol. One randomized, placebo-controlled, crossover trial assessed the lipid-altering efficacy of a softgel capsule providing esterified plan stanols/sterols in 28 subjects with primary hypercholesterolemia.
Participants followed the TLC diet for 5 weeks followed by 6 weeks of either the sterol/stanol capsule or a placebo before crossing over to the other product for 6 weeks while continuing the TLC diet.
Results indicated that incorporating sterols/stanols into the TLC diet produced positive changes in LDL cholesterol by 9.2%, total cholesterol by 7.4%, and triglycerides by 9.1%. A following study replicated this original study design, supporting the efficacy of 1.8 grams/day of esterified plant sterols/stanols in adjunct with the TLC diet to reduce lipid levels in participants with hypercholesterolemia.
Have you heard about the Therapeutic Lifestyle Changes diet? Basically, it was created by the National Cholesterol Education program to help lower a person’s cholesterol. It isn’t a fad diet and it’s based on science.
According to the Centers for Disease Control and Prevention, “TLC is an effective lifestyle therapy targeting low density lipoprotein cholesterol (LDL), a risk factor for coronary heart disease.”
But the benefits don’t stop there. In addition to helping lower LDL, the bad cholesterol, TLC also “improves risk factors associated with the metabolic syndrome and diabetes, including blood pressure, high-density lipoprotein cholesterol (HDL), serum triglycerides, blood glucose, and weight status.”
When you break it down, the TLC diet is more of a lifestyle modification plan than a diet because it’s not just about what you eat. It’s also not something that you do for a couple of weeks to drop 10 pounds.
TLC’s more of a commitment to your long-term health. The goal of this “diet” isn’t to fit into your skinny jeans, although that might happen. The goal is to eat well, manage weight, and exercise so you can be healthy and prevent coronary heart disease. Sounds good, right? Let’s break it down further so you can decide if it’s something that would be beneficial to you.
What is the Therapeutic Lifestyle diet?
The Therapeutic Lifestyle Changes diet was created by the National Institutes of Health’s National Cholesterol Education Program. The main goal of the diet, which is really more than a diet because it incorporates lifestyle changes, is to help cut cholesterol and lower the risk of cardiovascular disease.
The TLC diet can be broken down into three main parts.
The components are: diet, exercise, and weight management.
If you follow the TLC diet, you could see some weight loss, your LDL (bad cholesterol) levels can decrease, your HDL (good cholesterol) levels can increase, and your triglycerides (a fat type in your blood) can decrease. That’s all good stuff and good for your long-term health.
How does it improve heart health?
We’re not doctors here, but basically, the TLC diet recommends healthy lifestyle changes that do your heart good. Changes like keeping your dietary cholesterol below 200 milligrams a day and reducing your saturated fat intake to less that 7% of your total calories.
What are some of the specific dietary recommendations to lower LDL?
To reduce your intake of saturated fat and thereby reduce your LDL, the TLC diet recommends that you choose lean meats and low-fat dairy products. It also recommends no more than three whole egges with yolks a week.
Other dietary changes might require you to add certain foods to your diet.
It’s recommended that you increase your consumption of whole grains to 50% of the grains you eat to help lower LDL. Eating fish two to three times a week is also suggested because it helps lower triglycerides and increases HDL. Eating foods that contain plant sterols or stanols is also encouraged because those substances help lower LDL.
What specific foods are recommended?
Recommended foods include whole grains, fruits, veggies, fish, beans, lentils, oatmeal, whole-grain rice, and foods rich in mono and polyunsaturated fats. Basically, you have a lot of options to choose from.
What kind of foods rich in monosaturated fats are recommended?
You can have avocados, nut butters with no added trans fat, nuts, and seeds. In terms of oils, you can use canola, olive, and peanut oils. Again, you have a lot of options to choose from.
What kinds of polyunsaturated fats can you eat on this diet?
Recommended polyunsaturated fat sources include salmon, tuna, halibut, mackerel, pine nuts, walnuts, flaxseeds, pumpkin and sunflower seeds, as well as sesame seeds. Oils you can use include grape seed oil, safflower oil, and sunflower oil.
You will want to decrease your intake of saturated fats.
It is recommended that you limit your intake of saturated fats to no more than twice a week. Saturated fats can be found in bacon, butter, coconut, coconut milk, cream, cream cheese, sour cream, shortening, and lard. Oils you want to avoid include coconut, palm, and palm kernel.
Can the TLC diet help you lose weight?
If you want to lose weight on this diet the National Heart, Lung, and Blood Institute recommends decreasing your calorie intake by 500 to 1,000 calories a day, which should result in a loss of 1 to 2 pounds per week.
How much exercise is recommended?
To reduce the risk of chronic disease, it’s recommended that adults “engage in at least 30 minutes of moderate-intensity physical activity, above usual activity, at work or home on most days of the week.” That’s the bare minimum recommended.
What other lifestyle modifications need to be made?
It’s recommended that you learn the difference between physical fullness and satiety. Physical fullness happens when you pretty much feel stuffed after eating and that most likely means you ate too much. Satiety happens when your body sends a message to your brain saying that it’s had enough to eat before getting to the point of feeling like your belly is distended.
Is it expensive to follow the TLC diet?
No, it doesn’t have to be. You don’t have to buy any specialized foods or products. You’re just spending money on recommended foods. As for exercise, you don’t have to join a gym or anything. How you get your exercise is up to you.
Is it an easy diet to follow?
If you are looking for a quick fix, this isn’t it. The TLC diet requires that you make changes not just in what you eat, but also how you exercise. These changes aren’t meant to be temporary either.
How do I get started on the TLC diet?
Start by talking to your doctor about the diet. You can both decide if it’s a good option for you and your doctor can provide you with more information and may even recommend you work with a nutritionist.
___________________________________________________________________________
Therapeutic Lifestyle Changes (TLC) (Wikipedia)
Therapeutic Lifestyle Changes, also known as the TLC Diet, is a dietary pattern recommended by the National Cholesterol Education Program, part of the National Institutes of Health, to control hypercholesterolemia. This pattern focuses on saturated fats and cholesterol, dietary options to enhance LDL cholesterol lowering, weight control, and physical activity.
Background/History:
High cholesterol is one of the major controllable risk factors for coronary heart disease, heart attack and stroke. The National Institutes of Health created the National Cholesterol Education Program in 1985 to reduce cardiovascular disease rates in the United States by addressing high cholesterol.
They created the TLC diet to be used alone or in conjunction with medication management to control elevated cholesterol. The diet was incorporated into the Adult Treatment Panel III (ATP III) for high cholesterol in adults which was released in 2002. Updated guidelines for cholesterol management were established in 2013 by the American Heart Association (AHA) and American College of Cardiology (ACC).
Diet Components:
Essential Components of Therapeutic Lifestyle Changes:
The main Therapeutic Lifestyle Changes components include:
- Less than 7 percent of your daily calories from saturated fat
- Less than 200 mg a day of cholesterol
- 25–35 percent of daily calories from total fat
- Weight reduction if overweight with only enough calories to reach or maintain a healthy weight
- At least 30 minutes of a moderate intensity physical activity, such as brisk walking, on most, and preferably all, days of the week.
After six weeks, The National Cholesterol Education Program recommends checking the LDL cholesterol response to the changes; if the LDL cholesterol goal has not been achieved, other therapeutic options for LDL lowering can be implemented. These include: 2 grams per day of plant stanols or sterols and 10–25 grams per day of soluble fiber.
Macronutrient Distribution of the TLC Diet:
The Therapeutic Lifestyle Changes macronutrient profile includes:
- Total fat: 25–35% of total calories
- Saturated fat: Less than 7% of total calories
- Polyunsaturated fat: Up to 10% of total calories
- Monounsaturated fat: Up to 20% of total calories
- Carbohydrate: 50–60% of total calories
- Dietary fiber: 20–30 grams per day
- Protein: Approximately 15% of total calories
- Cholesterol: Less than 200 mg/day
Research Findings:
The recommendations for cholesterol management through lifestyle changes from the National Cholesterol Education Program have evolved over time based on data from epidemiological observations, animal studies, and clinical trials. Animal models have demonstrated a direct relationship between LDL cholesterol and atherosclerosis.
Animals consuming diets high in saturated fat and cholesterol develop LDL cholesterol elevation and atherosclerosis. Epidemiologic evidence in humans supports this direct relationship between LDL cholesterol and coronary heart disease risk.
One randomized crossover study completed at Tufts University and New England Medical Center looked at the Therapeutic Lifestyle Change diet relative to a typical Western diet.
Thirty-six participants with moderately elevated cholesterol levels participated in two 32-day phases where the subjects consumed their normal dietary patterns or the experimental diet consistent with the NCEP recommendations. This diet provided 30% calories from fat, 7% calories from saturated fat, and 75 mg cholesterol per 1,000 calories. Relative to the Western diet, the TLC diet resulted in 11% lower LDL cholesterol.
Additional studies have looked at the benefits of plant stanols and sterols on lowering LDL cholesterol. One randomized, placebo-controlled, crossover trial assessed the lipid-altering efficacy of a softgel capsule providing esterified plan stanols/sterols in 28 subjects with primary hypercholesterolemia.
Participants followed the TLC diet for 5 weeks followed by 6 weeks of either the sterol/stanol capsule or a placebo before crossing over to the other product for 6 weeks while continuing the TLC diet.
Results indicated that incorporating sterols/stanols into the TLC diet produced positive changes in LDL cholesterol by 9.2%, total cholesterol by 7.4%, and triglycerides by 9.1%. A following study replicated this original study design, supporting the efficacy of 1.8 grams/day of esterified plant sterols/stanols in adjunct with the TLC diet to reduce lipid levels in participants with hypercholesterolemia.
Use of Semaglutide for Weight Loss
- YouTube Video: What to know about semaglutide for weight loss
- YouTube Video: Everything You MUST Know Before Using Ozempic (Semaglutide) for Weight Loss
- YouTube Video: Pros and Cons of Semaglutide Drugs for Weight Loss
Semaglutide, sold under the brand names Ozempic, Wegovy and Rybelsus, is an antidiabetic medication used for the treatment of type 2 diabetes and an anti-obesity medication used for long-term weight management, developed by Novo Nordisk in 2012.
Semaglutide is a GLP-1 receptor agonist, meaning that it mimics the action of the human incretin glucagon-like peptide-1 (GLP-1), thereby increasing insulin secretion and increasing blood sugar disposal and improving glycemic control. Side effects include nausea, vomiting, diarrhea, abdominal pain, and constipation.
In 2020, semaglutide was the 129th most commonly prescribed medication in the United States, with more than 4 million prescriptions.
Medical uses:
Semaglutide is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes.
The higher-dose formulation of semaglutide is indicated as an adjunct to diet and exercise for long-term weight management in adults with obesity (initial body mass index (BMI) ≥ 30 kg/m2) or who are overweight (initial BMI ≥ 27 kg/m2) and have at least one weight-related comorbidity.
A review of anti-obesity treatments found that semaglutide as well as tirzepatide (which has an overlapping mechanism of action) were more promising than previous anti-obesity drugs, although less effective than bariatric surgery.
Adverse effects:
Possible side effects include the following:
Contraindications:
Data from rodent studies of GLP-1-mediated thyroid C-cell hyperplasia indicates that use is contraindicated in people with a personal or family history of medullary thyroid carcinoma and in patients with multiple endocrine neoplasia type 2
Mechanism of action:
Semaglutide is a glucagon-like peptide-1 receptor agonist. By mimicking the action of the incretin glucagon-like peptide-1 (GLP-1), it increases the production of insulin, the hormone which lowers the blood sugar level. It also appears to enhance growth of pancreatic beta cells, which are responsible for insulin production and release.
Additionally, it inhibits the production of glucagon, the hormone that increases glycogenolysis (release of stored carbohydrate from the liver) and gluconeogenesis (synthesis of new glucose). It reduces food intake by lowering appetite and slowing down digestion in the stomach, helping to reduce body fat. It reduces hunger, food craving and body fat.
Pharmacology:
Semaglutide is chemically similar to human GLP-1, with 94% similarity.
The only differences are two amino acid substitutions at positions 8 and 34, where alanine and lysine are replaced by 2-aminoisobutyric acid and arginine, respectively.
Amino-acid substitution at position 8 prevents chemical breakdown by dipeptidyl peptidase-4. In addition, the lysine at position 26 is in its derivative form (acylated with stearic diacid). Acylation with a spacer and C-18 fatty diacid chain increases the drug's binding to blood protein (albumin), which enables longer presence in the blood circulation.
Semaglutide's half-life in the blood is about seven days (165–184 hours). It can be administered by subcutaneous injection once weekly or once-daily by mouth. Based on its half-life and dosing frequency, it can be expected to accumulate more after each injection of the same dose or increasing dose. For this reason, patients may experience an increase in adverse effects throughout each 4-week phase of the same dose, and a possible increase in the satiety-inducing activity over the 4-week period.
For a given dose of semaglutide subcutaneous injection, the drug will accumulate in the blood more after each injection until steady-state is reached. Steady-state is expected to occur between 28 and 35 days of repeat weekly dosing of the same dose. This is directly related to the absorption and elimination rate constants, which are reported to be 0.0286 and 0.00413 (fraction/hour), respectively.
The peak and trough plasma concentrations are expected to vary by 30% during steady state (a 30% reduction from peak to trough). Note: the steady-state concentration will vary based on patient-specific factors. No significant difference in the decrease from baseline body weight was observed between groups taking it orally (20 mg and 40-mg) or subcutaneously.
History:
In June 2008, a phase II clinical trial began studying Semaglutide.
In 2012, a team of researchers at Novo Nordisk developed semaglutide for a once-weekly diabetes therapy as a longer-acting alternative to liraglutide. It was given the brand name Ozempic. Clinical trials were started in January 2016, and completed in May 2017.
In March 2021, a phase III randomized, double-blind, trial of 1961 adults with a Body mass index of 30 or greater were assigned in a 2:1 ratio, to a treatment with once-weekly subcutaneous semaglutide or placebo, plus lifestyle intervention. The trials occurred at 129 sites in 16 countries in Asia, Europe, North America, and South America.
The mean percentage change in body weight at week 68 was −14.9% in the semaglutide group vs −2.4% with placebo for an estimated treatment difference of −12.4 (95% CI, −13.4 to −11.5).
Society and culture:
Legal status:
In December 2016, the US FDA New Drug Application (NDA) was filed, and in October 2017, the FDA Advisory Committee approved it unanimously.
In December 2017, the injectable version with the brand name Ozempic was approved for use by people with diabetes in the United States, and in January 2018, in Canada.
In February 2018, authorization was granted in the European Union, in March 2018 in Japan, and in August 2019 in Australia.
In September 2019, a version which can be taken by mouth (Rybelsus) was approved for medical use in the United States, and in the European Union in April 2020.
In June 2021, a higher-dose injection version sold under the brand name Wegovy was approved by the US Food and Drug Administration as anti-obesity medication for long-term weight management in adults.
In November 2021, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) recommended to grant a marketing authorization to Wegovy. to Novo Nordisk A/S.
In January 2022, Wegovy was approved for medical use in the European Union.
In January 2023, the label for Rybelsus was updated to reflect that it can be used as a first-line treatment for adults with type 2 diabetes.
Cost to patients:
In the US, Wegovy has a list price of $1,349.02 per month per The New York Times, suggesting that because of the high costs many people "who could most benefit from weight loss may be unable to afford such expensive drugs".
In the UK semaglutide is available on NHS prescription for diabetes and obesity, at nominal or no cost to patients.
Research:
In 2022, a clinical trial conducted among adolescents with obesity was found that once-weekly treatment with a 2.4-mg dose of semaglutide, when added to lifestyle intervention, led to a greater reduction in BMI as compared to lifestyle intervention alone.
In 2021, semaglutide was found to be inferior to tirzepatide when used once weekly as add-on therapy to metformin in people with type 2 diabetes (SURPASS-2), in both endpoints of reduction in A1C and body weight, with a roughly similar safety profile.
A 2014 meta-analysis including a small number of patients found that semaglutide may be effective in lowering liver enzymes (transaminitis) and improving certain radiologically observed features of metabolic-dysfunction–associated fatty-liver disease (MAFLD).
See also:
Semaglutide is a GLP-1 receptor agonist, meaning that it mimics the action of the human incretin glucagon-like peptide-1 (GLP-1), thereby increasing insulin secretion and increasing blood sugar disposal and improving glycemic control. Side effects include nausea, vomiting, diarrhea, abdominal pain, and constipation.
In 2020, semaglutide was the 129th most commonly prescribed medication in the United States, with more than 4 million prescriptions.
Medical uses:
Semaglutide is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes.
The higher-dose formulation of semaglutide is indicated as an adjunct to diet and exercise for long-term weight management in adults with obesity (initial body mass index (BMI) ≥ 30 kg/m2) or who are overweight (initial BMI ≥ 27 kg/m2) and have at least one weight-related comorbidity.
A review of anti-obesity treatments found that semaglutide as well as tirzepatide (which has an overlapping mechanism of action) were more promising than previous anti-obesity drugs, although less effective than bariatric surgery.
Adverse effects:
Possible side effects include the following:
- nausea,
- diarrhea,
- vomiting,
- constipation,
- abdominal pain,
- headache,
- fatigue,
- indigestion/heartburn,
- dizziness, bloating (abdominal distension),
- belching,
- low blood sugar (hypoglycemia) in patients with type 2 diabetes,
- gas (flatulence),
- gastroenteritis,
- and gastroesophageal reflux disease (GERD).
Contraindications:
Data from rodent studies of GLP-1-mediated thyroid C-cell hyperplasia indicates that use is contraindicated in people with a personal or family history of medullary thyroid carcinoma and in patients with multiple endocrine neoplasia type 2
Mechanism of action:
Semaglutide is a glucagon-like peptide-1 receptor agonist. By mimicking the action of the incretin glucagon-like peptide-1 (GLP-1), it increases the production of insulin, the hormone which lowers the blood sugar level. It also appears to enhance growth of pancreatic beta cells, which are responsible for insulin production and release.
Additionally, it inhibits the production of glucagon, the hormone that increases glycogenolysis (release of stored carbohydrate from the liver) and gluconeogenesis (synthesis of new glucose). It reduces food intake by lowering appetite and slowing down digestion in the stomach, helping to reduce body fat. It reduces hunger, food craving and body fat.
Pharmacology:
Semaglutide is chemically similar to human GLP-1, with 94% similarity.
The only differences are two amino acid substitutions at positions 8 and 34, where alanine and lysine are replaced by 2-aminoisobutyric acid and arginine, respectively.
Amino-acid substitution at position 8 prevents chemical breakdown by dipeptidyl peptidase-4. In addition, the lysine at position 26 is in its derivative form (acylated with stearic diacid). Acylation with a spacer and C-18 fatty diacid chain increases the drug's binding to blood protein (albumin), which enables longer presence in the blood circulation.
Semaglutide's half-life in the blood is about seven days (165–184 hours). It can be administered by subcutaneous injection once weekly or once-daily by mouth. Based on its half-life and dosing frequency, it can be expected to accumulate more after each injection of the same dose or increasing dose. For this reason, patients may experience an increase in adverse effects throughout each 4-week phase of the same dose, and a possible increase in the satiety-inducing activity over the 4-week period.
For a given dose of semaglutide subcutaneous injection, the drug will accumulate in the blood more after each injection until steady-state is reached. Steady-state is expected to occur between 28 and 35 days of repeat weekly dosing of the same dose. This is directly related to the absorption and elimination rate constants, which are reported to be 0.0286 and 0.00413 (fraction/hour), respectively.
The peak and trough plasma concentrations are expected to vary by 30% during steady state (a 30% reduction from peak to trough). Note: the steady-state concentration will vary based on patient-specific factors. No significant difference in the decrease from baseline body weight was observed between groups taking it orally (20 mg and 40-mg) or subcutaneously.
History:
In June 2008, a phase II clinical trial began studying Semaglutide.
In 2012, a team of researchers at Novo Nordisk developed semaglutide for a once-weekly diabetes therapy as a longer-acting alternative to liraglutide. It was given the brand name Ozempic. Clinical trials were started in January 2016, and completed in May 2017.
In March 2021, a phase III randomized, double-blind, trial of 1961 adults with a Body mass index of 30 or greater were assigned in a 2:1 ratio, to a treatment with once-weekly subcutaneous semaglutide or placebo, plus lifestyle intervention. The trials occurred at 129 sites in 16 countries in Asia, Europe, North America, and South America.
The mean percentage change in body weight at week 68 was −14.9% in the semaglutide group vs −2.4% with placebo for an estimated treatment difference of −12.4 (95% CI, −13.4 to −11.5).
Society and culture:
Legal status:
In December 2016, the US FDA New Drug Application (NDA) was filed, and in October 2017, the FDA Advisory Committee approved it unanimously.
In December 2017, the injectable version with the brand name Ozempic was approved for use by people with diabetes in the United States, and in January 2018, in Canada.
In February 2018, authorization was granted in the European Union, in March 2018 in Japan, and in August 2019 in Australia.
In September 2019, a version which can be taken by mouth (Rybelsus) was approved for medical use in the United States, and in the European Union in April 2020.
In June 2021, a higher-dose injection version sold under the brand name Wegovy was approved by the US Food and Drug Administration as anti-obesity medication for long-term weight management in adults.
In November 2021, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) recommended to grant a marketing authorization to Wegovy. to Novo Nordisk A/S.
In January 2022, Wegovy was approved for medical use in the European Union.
In January 2023, the label for Rybelsus was updated to reflect that it can be used as a first-line treatment for adults with type 2 diabetes.
Cost to patients:
In the US, Wegovy has a list price of $1,349.02 per month per The New York Times, suggesting that because of the high costs many people "who could most benefit from weight loss may be unable to afford such expensive drugs".
In the UK semaglutide is available on NHS prescription for diabetes and obesity, at nominal or no cost to patients.
Research:
In 2022, a clinical trial conducted among adolescents with obesity was found that once-weekly treatment with a 2.4-mg dose of semaglutide, when added to lifestyle intervention, led to a greater reduction in BMI as compared to lifestyle intervention alone.
In 2021, semaglutide was found to be inferior to tirzepatide when used once weekly as add-on therapy to metformin in people with type 2 diabetes (SURPASS-2), in both endpoints of reduction in A1C and body weight, with a roughly similar safety profile.
A 2014 meta-analysis including a small number of patients found that semaglutide may be effective in lowering liver enzymes (transaminitis) and improving certain radiologically observed features of metabolic-dysfunction–associated fatty-liver disease (MAFLD).
See also:
- "Semaglutide". Drug Information Portal. U.S. National Library of Medicine.
- "Semaglutide". MedlinePlus.