Copyright © 2015 Bert N. Langford (Images may be subject to copyright. Please send feedback)
Welcome to Our Generation USA!
Senior Living
provides activities and programs for those who are retired, including pension plans and other retirement savings and income (including Social Security), health and exercise (through Medicare), senior housing, age-related diseases and other topics.
American Association for Retired Persons (AARP.Org):
YouTube Video: What are the Benefits of being an AARP Member?
Pictured: AARP Magazine, February/March, 2016 Issue.
American Association of Retired Persons (AARP) The AARP was founded in 1958 by a retired teacher, Ethel Percy Andrus, with the goal of helping older Americans remain physically and intellectually active by serving others.
AARP is a nonprofit, nonpartisan, social welfare organization with a membership of nearly 38 million that helps people turn their goals and dreams into real possibilities, strengthens communities and fights for the issues that matter most to families — such as health care, employment and income security, and protection from financial abuse.
Click on the following for Member Benefits
AARP is a nonprofit, nonpartisan, social welfare organization with a membership of nearly 38 million that helps people turn their goals and dreams into real possibilities, strengthens communities and fights for the issues that matter most to families — such as health care, employment and income security, and protection from financial abuse.
Click on the following for Member Benefits
AARP: Best Places to Retire, even Retire to a Good Life for Less
YouTube Video: Best Places to Retire: Deltona/Daytona | AARP
Pictured: The Daytona Boardwalk Amusement Area and Pier offers games and indoor and outdoor rides. — David A. Land.
Whether you're looking for a retirement destination or just seeking new surroundings, our Best Places lists will give you some great ideas. Who knows? You just might find the perfect new place to call home.
Want to retire on $30,000 a year? Or just want to know you could if you had to? We found the 10 most livable, low-cost cities in the U.S. — places where you can retire in comfort no matter how big (or small) your savings account.
Want to retire on $30,000 a year? Or just want to know you could if you had to? We found the 10 most livable, low-cost cities in the U.S. — places where you can retire in comfort no matter how big (or small) your savings account.
U.S. News & World Report: The 10 Best Places to Retire on Social Security Alone
U.S.News and World Report October 14, 2014: "If you don't have a traditional pension through your job and haven't been saving a significant amount in a 401(k) or individual retirement account, Social Security is likely to be your largest source of retirement income. Almost all retirees (86 percent) receive Social Security payments, and for over a third (36 percent) of retirees, Social Security accounts for 90 percent or more of their retirement income. The type of lifestyle Social Security alone will provide largely depends on how much you have earned in Social Security benefits and where you live.
The average Social Security benefit for retired workers was $1,294 per month at the end of 2013. A couple who each brought in this amount would have $31,056 in annual Social Security benefits, which will also be adjusted for inflation each year. U.S. News analyzed Census Bureau and Bureau of Labor Statistics data to determine where a retired couple age 65 or older could cover their basic expenses, including typical costs for housing, food, utilities, transportation and health care, on this amount.
It’s important to note that in most places, Social Security alone barely covered these basic expenses. After paying for those five major costs, retirees living on Social Security alone likely won’t have much cash left over for recreation, hobbies, clothing, consumer goods or travel. “If they are highly dependent on Social Security, it is not an easy life,” says John Palmer, a Syracuse University professor and former public trustee for the Medicare and Social Security programs. “If they own their own home and don’t have high medical expenses, they can probably get by....”
[See: 10 Places to Retire on Social Security Alone.]
For full Article click here.
The average Social Security benefit for retired workers was $1,294 per month at the end of 2013. A couple who each brought in this amount would have $31,056 in annual Social Security benefits, which will also be adjusted for inflation each year. U.S. News analyzed Census Bureau and Bureau of Labor Statistics data to determine where a retired couple age 65 or older could cover their basic expenses, including typical costs for housing, food, utilities, transportation and health care, on this amount.
It’s important to note that in most places, Social Security alone barely covered these basic expenses. After paying for those five major costs, retirees living on Social Security alone likely won’t have much cash left over for recreation, hobbies, clothing, consumer goods or travel. “If they are highly dependent on Social Security, it is not an easy life,” says John Palmer, a Syracuse University professor and former public trustee for the Medicare and Social Security programs. “If they own their own home and don’t have high medical expenses, they can probably get by....”
[See: 10 Places to Retire on Social Security Alone.]
For full Article click here.
Federal Assistance for Old Age including the Social Security Administration.
YouTube Video about the SSA

About the Social Security Administration:
The United States Social Security Administration (SSA) is an independent agency of the United States federal government that administers Social Security, a social insurance program consisting of retirement, disability, and survivors' benefits. To qualify for most of these benefits, most workers pay Social Security taxes on their earnings; the claimant's benefits are based on the wage earner's contributions. Otherwise benefits such as Supplemental Security Income (SSI) are given based on need.
The Social Security Administration was established by a law codified at 42 U.S.C. § 901.
SSA is headquartered in Woodlawn, Maryland, just to the west of Baltimore, at what is known as Central Office. The agency includes 10 regional offices, 8 processing centers, approximately 1300 field offices, and 37 Teleservice Centers. As of 2007, about 62,000 people were employed by SSA.
Headquarters non-supervisory employees of SSA are represented by American Federation of Government Employees Local 1923. Social Security is the largest social welfare program in the United States. For the year 2014, the net cost of social security was 906.4 billion dollars which accounted for 21% of government expenditure. It has been named the 6th best place to work in the federal government.
The OASDI program—which for most Americans means Social Security—is the largest income-maintenance program in the United States. Based on social insurance principles, the program provides monthly benefits designed to replace, in part, the loss of income due to retirement, disability, or death.
Coverage is nearly universal: About 96% of the jobs in the United States are covered. Workers finance the program through a payroll tax that is levied under the Federal Insurance and Self-Employment Contribution Acts (FICA and SECA). The revenues are deposited in two trust funds (the Federal Old-Age and Survivors Insurance Trust Fund and the Federal Disability Insurance Trust Fund), which pay benefits and the operating expenses of the program.
(Click Here to read total PDF article from the Social Security Administration)
SilverSneakers Fitness Benefits For Retirees
YouTube Video of Planet Fitness (gym) (Your Webhost's SilverSneakers Provider)
HealthWays SilverSneaker Fitness (see link above) is but one Medicare Insurance Provider offering free access to Gyms across the country for eligible seniors. Link provides access to database of gyms offering this Program in your area.
Available for some retirees depending on their Medicare Insurance Provider.
You can choose from more than 13,000 locations.
You can use as many facilities as you like! Work out with cardio and weight equipment, access pools or take group exercise classes taught by instructors trained specifically in senior fitness.
Available for some retirees depending on their Medicare Insurance Provider.
You can choose from more than 13,000 locations.
You can use as many facilities as you like! Work out with cardio and weight equipment, access pools or take group exercise classes taught by instructors trained specifically in senior fitness.
Health and Exercise to Live a Longer Life
YouTube Video: Dance Along Workout for Seniors and Elderly - Low Impact Dance Exercise on Chairs
Pictured: Two forms of exercise for Seniors
Do you want to add years to your life? Or life to your years?
Feeling your best boosts your zeal for life!
The American Heart Association recommends at least 150-minutes of moderate activity each week. An easy way to remember this is 30 minutes at least 5 days a week, but three 10-minute periods of activity are as beneficial to your overall fitness as one 30-minute session. This is achievable! Physical activity may also help encourage you to spend some time outdoors.
Here are some reasons why physical activity is proven to improve both mental and physical health.
Physical activity boosts mental wellness. Regular physical activity can relieve tension, anxiety, depression and anger. You may notice a "feel good sensation" immediately following your physical activity, and most people also note an improvement in general well-being over time as physical activity becomes a part of their routine.
Physical activity improves physical wellness.
Reduced Risk Factors
Too much sitting and other sedentary activities can increase your risk of cardiovascular disease. One study showed that adults who watch more than 4 hours of television a day had a 46% increased risk of death from any cause and an 80% increased risk of death from cardiovascular disease.
Becoming more active can help lower your blood pressure and also boost your levels of good cholesterol.
Physical activity prolongs your optimal health.Without regular physical activity, the body slowly loses its strength, stamina and ability to function well. People who are physically active and at a healthy weight live about 7 years longer than those who are not active and are obese.
(Click Here to See Rest of Article)
Feeling your best boosts your zeal for life!
The American Heart Association recommends at least 150-minutes of moderate activity each week. An easy way to remember this is 30 minutes at least 5 days a week, but three 10-minute periods of activity are as beneficial to your overall fitness as one 30-minute session. This is achievable! Physical activity may also help encourage you to spend some time outdoors.
Here are some reasons why physical activity is proven to improve both mental and physical health.
Physical activity boosts mental wellness. Regular physical activity can relieve tension, anxiety, depression and anger. You may notice a "feel good sensation" immediately following your physical activity, and most people also note an improvement in general well-being over time as physical activity becomes a part of their routine.
Physical activity improves physical wellness.
Reduced Risk Factors
Too much sitting and other sedentary activities can increase your risk of cardiovascular disease. One study showed that adults who watch more than 4 hours of television a day had a 46% increased risk of death from any cause and an 80% increased risk of death from cardiovascular disease.
Becoming more active can help lower your blood pressure and also boost your levels of good cholesterol.
Physical activity prolongs your optimal health.Without regular physical activity, the body slowly loses its strength, stamina and ability to function well. People who are physically active and at a healthy weight live about 7 years longer than those who are not active and are obese.
(Click Here to See Rest of Article)
Public employee pension plans in the United States
YouTube Video: Basics of Pension Funds & other Investing Strategies & Investing Options.
In the United States, public sector pensions are offered by federal, state and local levels of government. They are available to most, but not all, public sector employees.
These employer contributions to these plans typically vest after some period of time. These plans may be defined-benefit or defined-contribution pension plans, but the former have been most widely used by public agencies in the U.S. throughout the late twentieth century. Some local governments do not offer defined-benefit pensions but may offer a defined contribution plan. In many states, public employee pension plans are known as Public Employee Retirement Systems (PERS).
Unlike the private sector, in the public sector once an employee is hired their pension benefit terms cannot be changed. Retirement age in the public sector is usually lower than in the private sector. Public pension plan managers in the United States take higher risks investing the funds than ones outside the United States or those in the private sector.
Federal Employees Retirement System - covers approximately 2.44 million full-time civilian employees (as of Dec 2005
Each of the 50 US states has at least one retirement system for its employees. There are 3.68 million full-time and 1.39 million part-time state-level-government civilian employees as of 2002.
At the local level, Many U.S. cities are allowed to participate in the pension plans of their states; some of the largest have their own pension plans. The total number of local government employees in the United States as of 2002 is 13.2 million. There are 10.15 million full-time and 3.13 million part-time local-government civilian employees as of 2002.
These employer contributions to these plans typically vest after some period of time. These plans may be defined-benefit or defined-contribution pension plans, but the former have been most widely used by public agencies in the U.S. throughout the late twentieth century. Some local governments do not offer defined-benefit pensions but may offer a defined contribution plan. In many states, public employee pension plans are known as Public Employee Retirement Systems (PERS).
Unlike the private sector, in the public sector once an employee is hired their pension benefit terms cannot be changed. Retirement age in the public sector is usually lower than in the private sector. Public pension plan managers in the United States take higher risks investing the funds than ones outside the United States or those in the private sector.
Federal Employees Retirement System - covers approximately 2.44 million full-time civilian employees (as of Dec 2005
Each of the 50 US states has at least one retirement system for its employees. There are 3.68 million full-time and 1.39 million part-time state-level-government civilian employees as of 2002.
At the local level, Many U.S. cities are allowed to participate in the pension plans of their states; some of the largest have their own pension plans. The total number of local government employees in the United States as of 2002 is 13.2 million. There are 10.15 million full-time and 3.13 million part-time local-government civilian employees as of 2002.
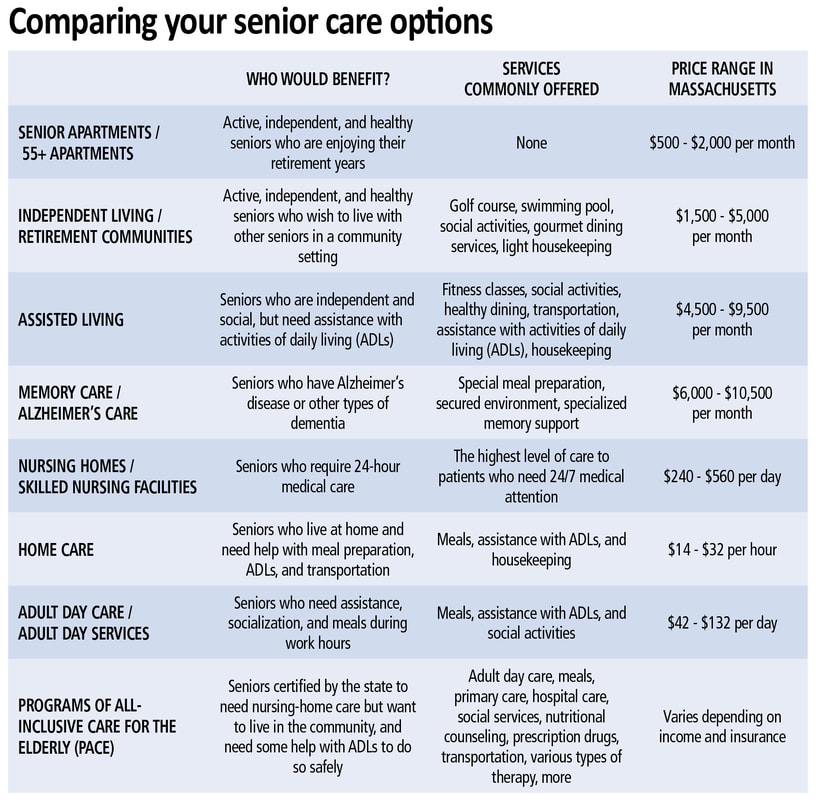
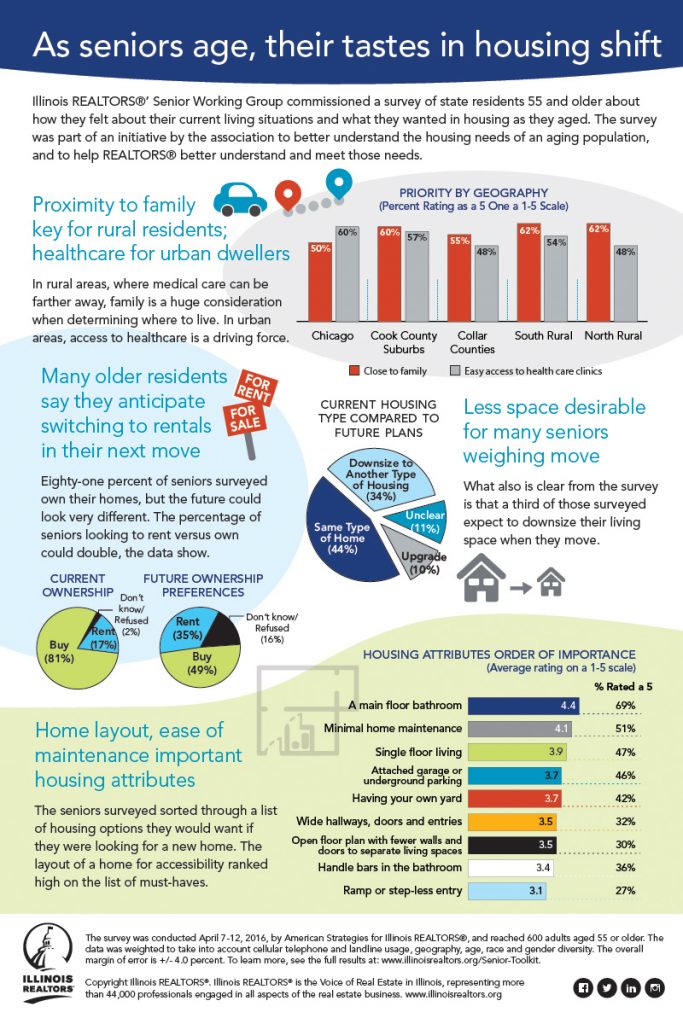
Retirement Communities including Continuing Care Retirement Communities in the United States
YouTube Video of Florida Retirement communities - LAKE ASHTON ACTIVITIES
Pictured: Courtesy of The Hermitage at Cedarfield, a retirement community designed for active older adults aged 62 or better. Located in western Henrico County, a suburban area of Richmond, Virginia.
A retirement community is a housing complex designed for older adults who are generally able to care for themselves; however, assistance from home care agencies is allowed in some communities, and activities and socialization opportunities are often provided.
Some of the characteristics typically are: the community must be age-restricted or age-qualified, residents must be partially or fully retired, and the community offers shared services or amenities.
Additionally, there are different types of retirement communities older adults can choose from including:
New types of retirement communities are being developed as the population ages including elder co-housing, which is defined later in this article. Retirement communities are often built in warm climates, and are common in Arizona, California, Florida and Texas but are increasingly being built in and around major cities throughout the United States.
Youngtown, Arizona, established in 1954, was the first age-restricted community. Del Webb opened Sun City, Arizona, with the active adult concept, in 1960.
In 2011, The Villages, Florida is the largest of these communities.
While new retirement communities have developed in various areas of the United States, they are largely marketed to older adults who are financially secure. Lower income retirement communities are rare except for government subsidized housing, which neglects a large proportion of older adults who have fewer financial resources.
Some of the characteristics typically are: the community must be age-restricted or age-qualified, residents must be partially or fully retired, and the community offers shared services or amenities.
Additionally, there are different types of retirement communities older adults can choose from including:
- Independent living communities, which offer no personal care services.
- Congregate housing, which includes at least one shared meal per day with other residents.
- Mobile homes or RV's for active adults.
- Subsidized housing for lower income older adults.
- Leisure or lifestyle oriented communities or LORCs, which include various amenities.
- Assisted Living Communities: Assisted Living and Memory Care assisted living provide all the daily services seniors need in an apartment or condo style environment. Everything from housekeeping, nursing, dining, wellness,activities, and usually in a locked and secured building.
- Continuing Care Retirement Communities, which are further defined below.
New types of retirement communities are being developed as the population ages including elder co-housing, which is defined later in this article. Retirement communities are often built in warm climates, and are common in Arizona, California, Florida and Texas but are increasingly being built in and around major cities throughout the United States.
Youngtown, Arizona, established in 1954, was the first age-restricted community. Del Webb opened Sun City, Arizona, with the active adult concept, in 1960.
In 2011, The Villages, Florida is the largest of these communities.
While new retirement communities have developed in various areas of the United States, they are largely marketed to older adults who are financially secure. Lower income retirement communities are rare except for government subsidized housing, which neglects a large proportion of older adults who have fewer financial resources.
Retirement Plans in the United States
YouTube Video: How to Plan for Retirement (USA.gov)

A retirement plan is a financial arrangement designed to replace employment income upon retirement. These plans may be set up by employers, insurance companies, trade unions, the government, or other institutions.
Congress has expressed a desire to encourage responsible retirement planning by granting favorable tax treatment to a wide variety of plans. Federal tax aspects of retirement plans in the United States are based on provisions of the Internal Revenue Code and the plans are regulated by the Department of Labor under the provisions of the Employee Retirement Income Security Act (ERISA).
Retirement plans are classified as either defined benefit plans or defined contribution plans, depending on how benefits are determined.In a defined benefit (or pension) plan, benefits are calculated using a fixed formula that typically factors in final pay and service with an employer, and payments are made from a trust fund specifically dedicated to the plan. Separate accounts for each participant do not exist.
By contrast, in a defined contribution plan, each participant has an account, and the benefit for the participant is dependent upon both the amount of money contributed into the account and the performance of the investments purchased with the funds contributed to the account.
Some types of retirement plans, such as cash balance plans, combine features of both defined benefit and defined contribution schemes.
Click on any of the following blue hyperlinks for further amplification:
- Types of retirement plans
- Contrasting types of retirement plans
- Portability and valuation
- Tax advantages
- History of pensions in the United States
- See also:
- Retirement plan
- Individual retirement account (IRA)
- Public employee pension plans in the United States
- 401(k)
- 403(b) - Similar to the 401(k), but for educational, religious, public healthcare, or non-profit workers
- 401(a) and 457 plans - For employees of state and local governments and certain tax-exempt entities
- Roth IRA - Similar to the IRA, but funded with after-tax dollars, with distributions being tax-free
- Roth 401(k) - Introduced in 2006; a 401(k) plan with the tax features of a Roth IRA
Senior Citizen Retirement Benefits for Veterans
Available from the U.S. Department of Veterans Affairs (VA)
YouTube Video Provided by the VA about VA Programs
From the Above Web Site: Services and other Programs Extended to Senior Veterans
Geriatrics and Extended Care Services (GEC): is committed to optimizing the health and well-being of Veterans with multiple chronic conditions, life-limiting illness, frailty or disability associated with chronic disease, aging or injury.
The Guide is a complete resource for Veterans and their caregivers. We encourage you to try the shared decision making approach – where Veterans involve their caregivers, social workers and health care providers to make decisions and choices about their current and future health needs.
Geriatrics and Extended Care Services (GEC): is committed to optimizing the health and well-being of Veterans with multiple chronic conditions, life-limiting illness, frailty or disability associated with chronic disease, aging or injury.
The Guide is a complete resource for Veterans and their caregivers. We encourage you to try the shared decision making approach – where Veterans involve their caregivers, social workers and health care providers to make decisions and choices about their current and future health needs.
Senior Citizen Housing (Federal Housing of Urban Development -- HUD)
YouTube Video: HUD Offers Housing Assistance Grant for Seniors, Disabled
Looking for Information for Senior Citizens looking for housing options for yourself, an aging parent, relative, or friend?
Do some research first to determine what kind of assistance or living arrangement you need; what your health insurance might cover; and what you can afford. Then check here for financial assistance resources and guides for making the right choice. Talk to a HUD-approved housing counselor if you have questions about your situation.
Stay in Your Home
Find an Apartment
- Units for the Elderly and Persons with Disabilities
- Find affordable rents
- Public housing
- Housing Choice Vouchers (Section 8)
- Rural rental help
Protect Yourself
HUD's mission is to create strong, sustainable, inclusive communities and quality affordable homes for all. HUD is working to strengthen the housing market to bolster the economy and protect consumers; meet the need for quality affordable rental homes; utilize housing as a platform for improving quality of life; build inclusive and sustainable communities free from discrimination, and transform the way HUD does business.
Sporting Activities for Seniors
From HelpGuide.org: "A trusted non-profit guide to mental health and well-being"
YouTube Video: 15 Min Senior Workout - HASfit Exercise for Elderly - Seniors Exercises for Elderly - Seniors
Exercise and Fitness as You Age: Exercise Tips to Get Fit and Stay Fit as You Grow Older
From The Website: "As you grow older, an active lifestyle is more important than ever. Regular exercise can help boost energy, maintain your independence, and manage symptoms of illness or pain. Exercise can even reverse some of the symptoms of aging. And not only is exercise good for your body, it’s also good for your mind, mood, and memory. Whether you are generally healthy or are managing an illness, there are plenty of ways to get more active, improve confidence, and boost your fitness.
Exercise is the key to healthy aging
Starting or maintaining a regular exercise routine can be a challenge as you get older. You may feel discouraged by illness, ongoing health problems, or concerns about injuries or falls. Or, if you've never exercised before, you may not know where to begin. Or perhaps you think you're too old or frail, or that exercise is boring or simply not for you.
While these may seem like good reasons to slow down and take it easy as you age, they're actually even better reasons to get moving. Exercise can energize your mood, relieve stress, help you manage symptoms of illness and pain, and improve your overall sense of well-being. In fact, exercise is the key to staying strong, energetic, and healthy as you get older. And it can even be fun, too, especially if you find like-minded people to exercise with.
No matter your age or your current physical condition, you can benefit from exercise. Reaping the rewards of exercise doesn’t have to involve strenuous workouts or trips to the gym. It’s about adding more movement and activity to your life, even in small ways. Whether you are generally healthy or are managing an illness—even if you’re housebound—there are many easy ways to get your body moving and improve your health and outlook..."
(For Rest of Article, Click Here)
From The Website: "As you grow older, an active lifestyle is more important than ever. Regular exercise can help boost energy, maintain your independence, and manage symptoms of illness or pain. Exercise can even reverse some of the symptoms of aging. And not only is exercise good for your body, it’s also good for your mind, mood, and memory. Whether you are generally healthy or are managing an illness, there are plenty of ways to get more active, improve confidence, and boost your fitness.
Exercise is the key to healthy aging
Starting or maintaining a regular exercise routine can be a challenge as you get older. You may feel discouraged by illness, ongoing health problems, or concerns about injuries or falls. Or, if you've never exercised before, you may not know where to begin. Or perhaps you think you're too old or frail, or that exercise is boring or simply not for you.
While these may seem like good reasons to slow down and take it easy as you age, they're actually even better reasons to get moving. Exercise can energize your mood, relieve stress, help you manage symptoms of illness and pain, and improve your overall sense of well-being. In fact, exercise is the key to staying strong, energetic, and healthy as you get older. And it can even be fun, too, especially if you find like-minded people to exercise with.
No matter your age or your current physical condition, you can benefit from exercise. Reaping the rewards of exercise doesn’t have to involve strenuous workouts or trips to the gym. It’s about adding more movement and activity to your life, even in small ways. Whether you are generally healthy or are managing an illness—even if you’re housebound—there are many easy ways to get your body moving and improve your health and outlook..."
(For Rest of Article, Click Here)
Maximize Your Social Security Benefits
YouTube Video: Social Security Benefits Calculator
Expert answers to your most common Social Security questions by Jane Bryant Quinn, AARP Bulletin, July/August 2015
"Are you wringing all the money you can out of Social Security? Based on my reader mail, I worry that some of you are losing out. Here are quick answers to the questions I get the most.
What can you apply for?
Retirement benefits, based on your own lifetime earnings. Spousal benefits, based on a living spouse's lifetime earnings. Survivor's benefits, payable after a spouse's death.
You can effectively collect only one of these benefits at a time. Social Security automatically gives you the largest check you're entitled to. Children might get benefits, too.
What's the best age to claim?
This varies a lot. In general, your check is always reduced for life if you file for any benefit before what Social Security calls your "normal retirement age." That's 66 for people born from 1943 to 1954 and rises gradually for every birth year through 1959.
For those born in 1960 or later, normal retirement age is 67. There's a fat bonus for collecting your benefits late: Social Security pays you an extra 8 percent for every year past "normal" that you delay your claim, up to age 70.
Can you claim a benefit as a spouse and later switch to benefits based on your own earnings record?
Yes, provided you wait to file for spousal benefits until you reach "normal" (or "full") retirement age. You might collect a spousal benefit check from, say, age 66 to 70, then put in for your personal retirement benefit, which will have grown.
This strategy does not work, however, if you file before you reach your normal retirement age. Early filers receive a benefit amount equal to the spousal benefit or their own retirement benefit, whichever is higher. Never both.
Does it ever pay to collect benefits early?
For many married couples, yes. A wife, for example, might retire early on a reduced benefit.
When her husband reaches normal retirement age, he can file for spousal benefits on her account. When he reaches 70, he can switch to his own, larger retirement account. How well this strategy works will depend on your ages and which of you is the higher earner.
What if you're divorced?
You can claim spousal and survivor's benefits on your ex's earnings record if you were married for at least 10 years and are not currently married. (Exception: You can keep the survivor's benefits if you remarry after you pass 60.) Your ex has to be eligible for Social Security, even if he or she has not yet retired.
What if your spouse dies?
If you've been collecting a spousal benefit, you can step up to the larger survivor's benefit. To get the maximum amount, consider putting off your claim until you reach normal retirement age.
You might make a different choice, however, if you have a substantial Social Security earnings record of your own. You might take the survivor's benefit early, then switch to your own, larger benefit at a later age. Play with the numbers until you get it right.
Helpful resources
Jane Bryant Quinn is a personal finance expert and author of Making the Most of Your Money NOW. She writes regularly for the Bulletin.
"Are you wringing all the money you can out of Social Security? Based on my reader mail, I worry that some of you are losing out. Here are quick answers to the questions I get the most.
What can you apply for?
Retirement benefits, based on your own lifetime earnings. Spousal benefits, based on a living spouse's lifetime earnings. Survivor's benefits, payable after a spouse's death.
You can effectively collect only one of these benefits at a time. Social Security automatically gives you the largest check you're entitled to. Children might get benefits, too.
What's the best age to claim?
This varies a lot. In general, your check is always reduced for life if you file for any benefit before what Social Security calls your "normal retirement age." That's 66 for people born from 1943 to 1954 and rises gradually for every birth year through 1959.
For those born in 1960 or later, normal retirement age is 67. There's a fat bonus for collecting your benefits late: Social Security pays you an extra 8 percent for every year past "normal" that you delay your claim, up to age 70.
Can you claim a benefit as a spouse and later switch to benefits based on your own earnings record?
Yes, provided you wait to file for spousal benefits until you reach "normal" (or "full") retirement age. You might collect a spousal benefit check from, say, age 66 to 70, then put in for your personal retirement benefit, which will have grown.
This strategy does not work, however, if you file before you reach your normal retirement age. Early filers receive a benefit amount equal to the spousal benefit or their own retirement benefit, whichever is higher. Never both.
Does it ever pay to collect benefits early?
For many married couples, yes. A wife, for example, might retire early on a reduced benefit.
When her husband reaches normal retirement age, he can file for spousal benefits on her account. When he reaches 70, he can switch to his own, larger retirement account. How well this strategy works will depend on your ages and which of you is the higher earner.
What if you're divorced?
You can claim spousal and survivor's benefits on your ex's earnings record if you were married for at least 10 years and are not currently married. (Exception: You can keep the survivor's benefits if you remarry after you pass 60.) Your ex has to be eligible for Social Security, even if he or she has not yet retired.
What if your spouse dies?
If you've been collecting a spousal benefit, you can step up to the larger survivor's benefit. To get the maximum amount, consider putting off your claim until you reach normal retirement age.
You might make a different choice, however, if you have a substantial Social Security earnings record of your own. You might take the survivor's benefit early, then switch to your own, larger benefit at a later age. Play with the numbers until you get it right.
Helpful resources
- AARP: Social Security Calculator
- Government: Social Security Administration, ssa.gov, 800-772-1213, or any Social Security office
- Commercial services: SocialSecurityChoices.com, SocialSecuritySolutions.com, and Maximize My Social Security's website.
- New books: Get What's Yours: The Secrets to Maxing Out Your Social Security, by Laurence J. Kotlikoff, Philip Moeller and Paul Solman; Personal Finance for Seniors for Dummies, by Eric Tyson and Bob Carlson; Social Security for Dummies (Second Edition), by Jonathan Peterson
Jane Bryant Quinn is a personal finance expert and author of Making the Most of Your Money NOW. She writes regularly for the Bulletin.
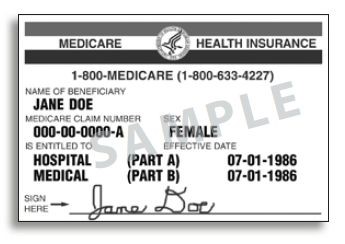
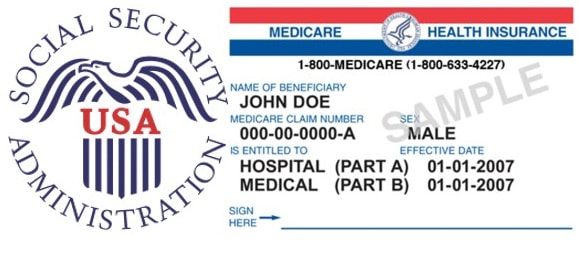
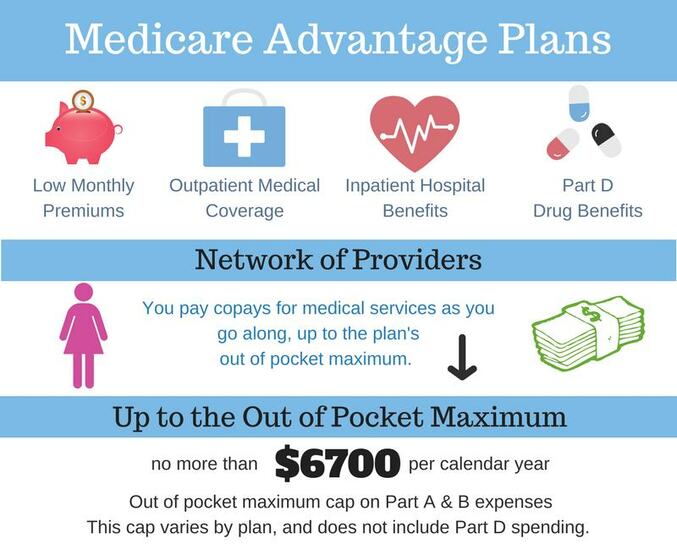
Medicare in the United States including MedigapPictured: A sample Medicare card. There are separate lines for basic Part A and Part B's supplementary medical coverage, each with its own date. There are no lines for Part C or D, which are additional supplemental policies for which a separate card is issued.
In the United States, Medicare is a national social insurance program, administered by the U.S. federal government since 1966, currently using about 30 private insurance companies across the United States.
Medicare provides health insurance for Americans aged 65 and older who have worked and paid into the system. It also provides health insurance to younger people with disabilities, end stage renal disease and amyotrophic lateral sclerosis.
In 2010, Medicare provided health insurance to 48 million Americans—40 million people age 65 and older and eight million younger people with disabilities. It was the primary payer for an estimated 15.3 million inpatient stays in 2011, representing 47.2 percent ($182.7 billion) of total aggregate inpatient hospital costs in the United States.
Medicare serves a large population of elderly and disabled individuals. On average, Medicare covers about half (48 percent) of the health care charges for those enrolled. The enrollees must then cover the remaining approved charges either with supplemental insurance or with another form of out-of-pocket coverage.
Out-of-pocket costs can vary depending on the amount of health care a Medicare enrollee needs. They might include uncovered services—such as long-term, dental, hearing, and vision care—and the supplemental insurance.
The Specialty Society Relative Value Scale Update Committee (or Relative Value Update Committee; RUC), composed of physicians associated with the American Medical Association, advises the government about pay standards for Medicare patient procedures, according to news reports.
Click on any of the following hyperlinks for amplification:
Medigap (also Medicare supplement insurance or Medicare supplemental insurance) refers to various private health insurance plans sold to supplement Medicare in the United States.
Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges.
Medigap's name is derived from the notion that it exists to cover the difference or "gap" between the expenses reimbursed to providers by Medicare Parts A and B for the preceding named services and the total amount allowed to be charged for those services by the United States Centers for Medicare and Medicaid Services (CMS).
As of 2006, 18% of Medicare beneficiaries were covered by a Medigap policy. Public-option Part C Medicare Advantage health plans and private employee retiree insurance provides a similar supplemental role for almost all other Medicare beneficiaries not dual eligible for Medicaid.
Medicare eligibility starts for most Americans when they turn 65 years old. Those who have been on Social Security eligibility for 24 months can also qualify for Medicare Part A and Part B. A person must be enrolled in part A and B of Medicare before they can enroll in a Medigap plan.
When a person turns 65—or if they are older and new to Medicare Part B—they become eligible for Medigap open enrollment. This period starts on the first day of the month you turn 65 and lasts for 6 months. During this period, a person can buy any Medigap plan regardless of their health.
This is different than if someone is losing group coverage or retiring. When this occurs, the person is eligible to exercise his or her "Guarantee Issue" right. With a Medigap guarantee issue right, a person can buy a Medigap Plan A, B, C, F, K, or L that's sold by any insurance company in their state.
In addition, the insurance company cannot deny or raise the premium due to past or current health conditions. Also, the insurance company must cover any pre-existing conditions.
Instead of exercising the guarantee issue right, a person can opt to go through the underwriting process in order to buy a plan G or N. Once a person is outside their open enrollment period and or guarantee issue, they can change their Medigap plan, but they will be subject to health underwriting by the insurance company they are applying with.
It is also important to know that monthly premiums apply, and plans may not be cancelled by the insurer for any reason other than non-payment of premiums/membership dues.
Furthermore, a single Medigap plan may cover only one person. Finally, Medigap insurance is not compatible with a Medicare Advantage plan. You cannot have both a Medicare supplement and a Medicare Advantage plan at the same time. You can only have a Medigap plan if you are still on Medicare Part A and Part B and have not replaced your coverage with a Medicare Advantage Part C coverage.
Medicare recipients under age 65:
Recipients of Social Security Disability Insurance (SSDI) benefits or patients with end-stage renal disease (ESRD) are entitled to Medicare coverage regardless of age, but are not automatically entitled to purchase Medigap policies unless they are at least 65.
Under federal law, insurers are not required to sell Medigap policies to people under 65, and even if they do, they may use medical screening. However, a slight majority of states require insurers to offer at least one kind of Medigap policy to at least some Medicare recipients in that age group.
Of these states, 25 require that Medigap policies be offered to all Medicare recipients. In California, Massachusetts, and Vermont, Medigap policies are not available to end-stage ESRD patients. Part D deductible will go up for about 20% of Americans to over $150.00 a year. That's close to a 50% increase in 2016.
Products Available:
Medigap offerings have been standardized by the Centers for Medicare and Medicaid Services (CMS) into ten different plans, labeled A through N, sold and administered by private companies.
Each Medigap plan offers a different combination of benefits. The coverage provided is roughly proportional to the premium paid. However, many older Medigap plans (these 'older' plans are no longer marketed) offering minimal benefits will cost more than current plans offering full benefits. The reason behind this is that older plans have an older average age per person enrolled in the plan, causing more claims within the group and raising the premium for all members within the group.
Since Medigap is private insurance and not government sponsored, the rules governing the sale and offerings of a Medigap insurance policy can vary from state to state. Some states such as Massachusetts, Minnesota, and Wisconsin require Medigap insurance to provide additional coverage than what is defined in the standardized Medigap plans.
Some employers may provide Medigap coverage as a benefit to their retirees. While Medigap offerings have been standardized since 1992, some seniors who had Medigap plans prior to 1992 are still on non-standard plans. Those plans are no longer eligible for new policies.
Over the years, new laws have brought many changes to Medigap Policies. For example, marketing for plans E, H, I, and J has been stopped as of May 31, 2010. But, if you were already covered by plan E, H, I, or J before June 1, 2010, you can keep that plan. Medigap plans M and N took effect on June 1, 2010, bringing the number of offered plans down to ten from twelve.
Congress passed the bill H.R. 2 on April 14, 2015, which will eliminate plans that cover the part B deductible for new Medicare beneficiaries starting Jan. 1st, 2020. Those who enroll in to Medicare after Jan. 1st, 2020 will not be able to purchase plans F or C; however, those people who enrolled onto Medicare prior to Jan. 1st, 2020 will still be able to purchase plans F or C. Congress believes eliminating first dollar coverage plans will save Medicare money.
Drug Coverage:
Some Medigap policies sold before January 1, 2006 may include prescription drug coverage, but after that date, no new Medigap policies could be sold with drug coverage. This time frame coincides with the introduction of the Medicare Part D benefit.
Medicare beneficiaries who enroll in a Standalone Part D plan may not retain the drug coverage portion of their Medigap policy. People with Medigap policies that include drug coverage who enrolled in Medicare Part D by May 15, 2006 had a guaranteed right to switch to another Medigap policy that has no prescription drug coverage.
Beneficiaries choosing to retain a Medigap policy with drug coverage after that date have no such right; in that case, the opportunity to switch to a Medigap policy without drug coverage is solely at the discretion of the private insurance company issuing the replacement policy, but the beneficiary may choose to remove drug coverage from their current Medigap policy and retain all other benefits.
The vast majority of Medicare beneficiaries who hold a Medigap policy with drug coverage and then enroll in a Part D Plan after May 15, 2006 will have to pay a late enrollment penalty. The only exception is for the few beneficiaries holding a Medigap policy with a drug benefit that is considered "creditable coverage" (i.e. that it meets four criteria defined by the Centers for Medicare and Medicaid Services); a Medigap policy with prescription drug coverage bought before mid-1992 may pay out as much as or more than a Medicare Part D plan.
Medigap policies sold in Massachusetts, Minnesota, and Wisconsin with prescription coverage may also pay out as much as or more than Part D.
Thus, individuals who qualify for the Qualified Medicare Beneficiary (QMB) program generally also do not need, and should not pay for, Medicare Supplement Insurance. Some employers offer health insurance coverage to their retirees. Retirees who are covered by such group plans may not need to purchase an individual policy.
While a retiree may choose to switch to an individual plan, this may not be a good choice because group retiree plans usually do not cost anything to the individual and the group coverage is often as good or better than most individual Medigap policies. Thus, the individual should compare his company's policy costs and coverage with the ten Medigap policies.
The retiree should also consider the stability of his company. If it is conceivable that the company will falter, that his costs will rise, or that coverage will diminish, the individual may wish to purchase an independent policy. Remember, however, that if a new policy is purchased, the old policy must be dropped. More information at:
Enrollment Patterns:
In 2006, 18% of Medicare beneficiaries were covered by Original Medicare (Part A and B) supplemented with a standardized Medigap Plan, while another 65% had other coverage through employer-based policies, Medicare Advantage policies, or Medicaid or other public insurance.
Almost a third of Medigap policyholders (31%) live in rural areas; in comparison, roughly a fourth of all Medicare beneficiaries live in rural areas. Two-thirds of rural Medigap policyholders (66%) report incomes below $30,000.
See Also:
Medicare provides health insurance for Americans aged 65 and older who have worked and paid into the system. It also provides health insurance to younger people with disabilities, end stage renal disease and amyotrophic lateral sclerosis.
In 2010, Medicare provided health insurance to 48 million Americans—40 million people age 65 and older and eight million younger people with disabilities. It was the primary payer for an estimated 15.3 million inpatient stays in 2011, representing 47.2 percent ($182.7 billion) of total aggregate inpatient hospital costs in the United States.
Medicare serves a large population of elderly and disabled individuals. On average, Medicare covers about half (48 percent) of the health care charges for those enrolled. The enrollees must then cover the remaining approved charges either with supplemental insurance or with another form of out-of-pocket coverage.
Out-of-pocket costs can vary depending on the amount of health care a Medicare enrollee needs. They might include uncovered services—such as long-term, dental, hearing, and vision care—and the supplemental insurance.
The Specialty Society Relative Value Scale Update Committee (or Relative Value Update Committee; RUC), composed of physicians associated with the American Medical Association, advises the government about pay standards for Medicare patient procedures, according to news reports.
Click on any of the following hyperlinks for amplification:
- Program history
- Administration
- Financing
- Eligibility
- Benefits
- Out-of-pocket costs
- Payment for services
- Comparison with private insurance
- Costs and funding challenges
- Criticism
- Legislation and reform
- Legislative oversight
- See also:
- Administration on Aging
- Federal Insurance Contributions Act
- Health care in the United States
- Health care politics
- Health care reform in the United States
- Health insurance in the United States
- Medicaid
- Medicare Rights Center
- Patient Protection and Affordable Care Act (Obamacare)
- Philosophy of healthcare
- Quality improvement organizations
- Single-payer health care
- Stark Law
- United States National Health Care Act (Expanded and Improved Medicare for All Act)
- External links
Medigap (also Medicare supplement insurance or Medicare supplemental insurance) refers to various private health insurance plans sold to supplement Medicare in the United States.
Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges.
Medigap's name is derived from the notion that it exists to cover the difference or "gap" between the expenses reimbursed to providers by Medicare Parts A and B for the preceding named services and the total amount allowed to be charged for those services by the United States Centers for Medicare and Medicaid Services (CMS).
As of 2006, 18% of Medicare beneficiaries were covered by a Medigap policy. Public-option Part C Medicare Advantage health plans and private employee retiree insurance provides a similar supplemental role for almost all other Medicare beneficiaries not dual eligible for Medicaid.
Medicare eligibility starts for most Americans when they turn 65 years old. Those who have been on Social Security eligibility for 24 months can also qualify for Medicare Part A and Part B. A person must be enrolled in part A and B of Medicare before they can enroll in a Medigap plan.
When a person turns 65—or if they are older and new to Medicare Part B—they become eligible for Medigap open enrollment. This period starts on the first day of the month you turn 65 and lasts for 6 months. During this period, a person can buy any Medigap plan regardless of their health.
This is different than if someone is losing group coverage or retiring. When this occurs, the person is eligible to exercise his or her "Guarantee Issue" right. With a Medigap guarantee issue right, a person can buy a Medigap Plan A, B, C, F, K, or L that's sold by any insurance company in their state.
In addition, the insurance company cannot deny or raise the premium due to past or current health conditions. Also, the insurance company must cover any pre-existing conditions.
Instead of exercising the guarantee issue right, a person can opt to go through the underwriting process in order to buy a plan G or N. Once a person is outside their open enrollment period and or guarantee issue, they can change their Medigap plan, but they will be subject to health underwriting by the insurance company they are applying with.
It is also important to know that monthly premiums apply, and plans may not be cancelled by the insurer for any reason other than non-payment of premiums/membership dues.
Furthermore, a single Medigap plan may cover only one person. Finally, Medigap insurance is not compatible with a Medicare Advantage plan. You cannot have both a Medicare supplement and a Medicare Advantage plan at the same time. You can only have a Medigap plan if you are still on Medicare Part A and Part B and have not replaced your coverage with a Medicare Advantage Part C coverage.
Medicare recipients under age 65:
Recipients of Social Security Disability Insurance (SSDI) benefits or patients with end-stage renal disease (ESRD) are entitled to Medicare coverage regardless of age, but are not automatically entitled to purchase Medigap policies unless they are at least 65.
Under federal law, insurers are not required to sell Medigap policies to people under 65, and even if they do, they may use medical screening. However, a slight majority of states require insurers to offer at least one kind of Medigap policy to at least some Medicare recipients in that age group.
Of these states, 25 require that Medigap policies be offered to all Medicare recipients. In California, Massachusetts, and Vermont, Medigap policies are not available to end-stage ESRD patients. Part D deductible will go up for about 20% of Americans to over $150.00 a year. That's close to a 50% increase in 2016.
Products Available:
Medigap offerings have been standardized by the Centers for Medicare and Medicaid Services (CMS) into ten different plans, labeled A through N, sold and administered by private companies.
Each Medigap plan offers a different combination of benefits. The coverage provided is roughly proportional to the premium paid. However, many older Medigap plans (these 'older' plans are no longer marketed) offering minimal benefits will cost more than current plans offering full benefits. The reason behind this is that older plans have an older average age per person enrolled in the plan, causing more claims within the group and raising the premium for all members within the group.
Since Medigap is private insurance and not government sponsored, the rules governing the sale and offerings of a Medigap insurance policy can vary from state to state. Some states such as Massachusetts, Minnesota, and Wisconsin require Medigap insurance to provide additional coverage than what is defined in the standardized Medigap plans.
Some employers may provide Medigap coverage as a benefit to their retirees. While Medigap offerings have been standardized since 1992, some seniors who had Medigap plans prior to 1992 are still on non-standard plans. Those plans are no longer eligible for new policies.
Over the years, new laws have brought many changes to Medigap Policies. For example, marketing for plans E, H, I, and J has been stopped as of May 31, 2010. But, if you were already covered by plan E, H, I, or J before June 1, 2010, you can keep that plan. Medigap plans M and N took effect on June 1, 2010, bringing the number of offered plans down to ten from twelve.
Congress passed the bill H.R. 2 on April 14, 2015, which will eliminate plans that cover the part B deductible for new Medicare beneficiaries starting Jan. 1st, 2020. Those who enroll in to Medicare after Jan. 1st, 2020 will not be able to purchase plans F or C; however, those people who enrolled onto Medicare prior to Jan. 1st, 2020 will still be able to purchase plans F or C. Congress believes eliminating first dollar coverage plans will save Medicare money.
Drug Coverage:
Some Medigap policies sold before January 1, 2006 may include prescription drug coverage, but after that date, no new Medigap policies could be sold with drug coverage. This time frame coincides with the introduction of the Medicare Part D benefit.
Medicare beneficiaries who enroll in a Standalone Part D plan may not retain the drug coverage portion of their Medigap policy. People with Medigap policies that include drug coverage who enrolled in Medicare Part D by May 15, 2006 had a guaranteed right to switch to another Medigap policy that has no prescription drug coverage.
Beneficiaries choosing to retain a Medigap policy with drug coverage after that date have no such right; in that case, the opportunity to switch to a Medigap policy without drug coverage is solely at the discretion of the private insurance company issuing the replacement policy, but the beneficiary may choose to remove drug coverage from their current Medigap policy and retain all other benefits.
The vast majority of Medicare beneficiaries who hold a Medigap policy with drug coverage and then enroll in a Part D Plan after May 15, 2006 will have to pay a late enrollment penalty. The only exception is for the few beneficiaries holding a Medigap policy with a drug benefit that is considered "creditable coverage" (i.e. that it meets four criteria defined by the Centers for Medicare and Medicaid Services); a Medigap policy with prescription drug coverage bought before mid-1992 may pay out as much as or more than a Medicare Part D plan.
Medigap policies sold in Massachusetts, Minnesota, and Wisconsin with prescription coverage may also pay out as much as or more than Part D.
Thus, individuals who qualify for the Qualified Medicare Beneficiary (QMB) program generally also do not need, and should not pay for, Medicare Supplement Insurance. Some employers offer health insurance coverage to their retirees. Retirees who are covered by such group plans may not need to purchase an individual policy.
While a retiree may choose to switch to an individual plan, this may not be a good choice because group retiree plans usually do not cost anything to the individual and the group coverage is often as good or better than most individual Medigap policies. Thus, the individual should compare his company's policy costs and coverage with the ten Medigap policies.
The retiree should also consider the stability of his company. If it is conceivable that the company will falter, that his costs will rise, or that coverage will diminish, the individual may wish to purchase an independent policy. Remember, however, that if a new policy is purchased, the old policy must be dropped. More information at:
Enrollment Patterns:
In 2006, 18% of Medicare beneficiaries were covered by Original Medicare (Part A and B) supplemented with a standardized Medigap Plan, while another 65% had other coverage through employer-based policies, Medicare Advantage policies, or Medicaid or other public insurance.
Almost a third of Medigap policyholders (31%) live in rural areas; in comparison, roughly a fourth of all Medicare beneficiaries live in rural areas. Two-thirds of rural Medigap policyholders (66%) report incomes below $30,000.
See Also:
- Health insurance in the United States
- Medicare Supplement Overview at Medicare.gov
- Benefits Grid for the different Medigap plans at Medicare.gov
Retirees as Snowbirds
YouTube Video: Crazy Horse Campground and RV Park in Tucson, Arizona
Pictured: Retirees as Snowbirds migrating to Florida for the Winter as LEFT: “Snowbird” License Plate; RIGHT: Snowbird’s beachfront trailer courtesy Beachfront RV Park
A snowbird is a term often associated with people who move from the higher latitudes and colder climates of the northern United States and Canada and migrate southward in winter to warmer locales such as Florida, California, Hawaii, Arizona, Texas, or elsewhere along the Sun Belt of the southern and southwestern United States, Mexico, and areas of the Caribbean.
Snowbirds are typically retirees who wish to avoid the snow and cold temperatures of northern winter, but maintain ties with family and friends by staying there the rest of the year.
Some snowbirds bring their homes with them, as campers (mounted on bus or truck frames) or as boats following the East Coast Intracoastal waterway.
A significant portion of the snowbird community is made up of recreational vehicle users (RVers). Many own a motorhome for the sole purpose of traveling south in the winter. Often they go to the same location every year and consider the other RVers that do the same a "second family".
Many RV parks label themselves "snowbird friendly" and get the majority of their income from the influx of RVing snowbirds. There are places like Quartzsite, Arizona, that have been labeled "white cities" because from a bird's-eye view all the motorhomes cover the landscape in white and then in the summer are gone.
While historically Florida has been the number one RV snowbird location, other southern U.S. states are experiencing a boom from snowbirds enjoying the southern climate for example.
In the United States, the right to vote for local office is governed by local and state law, so it may be possible to vote for local offices in both places if the locality permits nonresident voting based on property ownership.
However, representation in the United States Congress is for residents as enumerated by the decennial census and voting in U.S. federal elections in more than one jurisdiction is deemed to be electoral fraud.
See also:
Snowbirds are typically retirees who wish to avoid the snow and cold temperatures of northern winter, but maintain ties with family and friends by staying there the rest of the year.
Some snowbirds bring their homes with them, as campers (mounted on bus or truck frames) or as boats following the East Coast Intracoastal waterway.
A significant portion of the snowbird community is made up of recreational vehicle users (RVers). Many own a motorhome for the sole purpose of traveling south in the winter. Often they go to the same location every year and consider the other RVers that do the same a "second family".
Many RV parks label themselves "snowbird friendly" and get the majority of their income from the influx of RVing snowbirds. There are places like Quartzsite, Arizona, that have been labeled "white cities" because from a bird's-eye view all the motorhomes cover the landscape in white and then in the summer are gone.
While historically Florida has been the number one RV snowbird location, other southern U.S. states are experiencing a boom from snowbirds enjoying the southern climate for example.
In the United States, the right to vote for local office is governed by local and state law, so it may be possible to vote for local offices in both places if the locality permits nonresident voting based on property ownership.
However, representation in the United States Congress is for residents as enumerated by the decennial census and voting in U.S. federal elections in more than one jurisdiction is deemed to be electoral fraud.
See also:
- Canadian Snowbird Association
- Canadians of convenience
- Coachella Valley – a major destination in the desert of California for snowbirds and part-time residents from Canada and the Pacific Northwest
- RV lifestyle
- Seasonal human migration
What to Expect in Your 70s and Beyond by AARP Magazine October 10, 2012.
YouTube Video: Age Strongly: Exercises for Ages 70+
Pictured below: (L) Studies show strength training can build muscle, which can take force off the joints.; (R) 44 percent of women 68 through 80 report being very satisfied with their sex lives, compared with just 30 percent of women 55 to 68 years old.
Staying mentally and physically active can help keep you, well, young. What can you expect of the years ahead?
Everyone ages differently, and lifestyle plays a major role, but you'll experience both hard-to-notice and impossible-to-miss changes in your physical and mental health.
Read on for the good, the bad and the what's-up-with-that? transformations you'll encounter — plus the latest advice on feeling happy, sexy and pain-free.
Save Your Skin
The Good News: Your skin is drier, which can be welcome relief for the third of women who were plagued by oily skin and breakouts throughout their adulthood.
The Not-So-Good News: Wrinkles and lines are more plentiful, but so are the options for keeping skin looking bright. Gentle exfoliation and moisturizing are especially important.
Pick skin products with antioxidants and glycolic acid, which promote skin thickening and increase collagen production. And apply a broad-spectrum sunscreen with a sun protection factor (SPF) of at least 30 every day.
Laser treatments can help with dilated superficial blood vessels (called telangiectasias), which tend to appear without warning on the cheeks, nose, chin and legs. (The laser destroys the blood vessels underneath the skin - with no scarring.) And those extra skin tags? Your doctor can remove them through freezing, snipping or cauterizing.
What's Up With That? Non-articular cartilage, the type that gives ears and noses their shape, continues to grow with age, making these appendages larger. But look on the bright side: Such cartilage growth may have evolved to enable people to track and funnel sounds and smells as they age, suggests James Stankiewicz, M.D., chair of the Department of Otolaryngology — Head and Neck Surgery at Loyola University Chicago Stritch School of Medicine.
What's Ahead: As you age, the skin around your jawline tends to sag. If you're bothered by it, ask your doctor about skin-tightening radio-frequency treatments, which can tighten skin without damaging the epidermis.
Bone Up for Good Health:
The Good News: You can maintain muscle strength through activity.
The Not-So-Good News: About one in three women ages 75 through 85 has osteoporosis, a bone-thinning disease, which greatly increases the risk of fractures of the hip and spine. Studies show strength training can build muscle, which can take force off the joints. Plus, weight-bearing activities stimulate the bones to grow stronger and denser.
What's Up With That? Although worn joints may benefit from anti-inflammatory drugs and activity, surgery may become necessary as cartilage loss begins to accelerate. Regenerative techniques such as platelet-rich plasma and autologous (self) stem cell injections may also help, according to Nathan Wei, M.D., a rheumatologist in Frederick, Md.
What's Ahead: Joint-replacement surgeries are common; one study showed that patients 75-plus recover just as quickly as those 65 to 74.
Preserve Your Senses:
The Good News: Lifestyle plays a major role in helping to maintain your senses as you age. So stay away from loud noises, eat a well-balanced diet (which can help ward off such age-related eye disorders as macular degeneration) and see a doctor immediately if you notice that your senses of smell or taste diminish significantly. (This may indicate a sinus infection or be a reaction to medication.)
The Not-So-Good News: You may have trouble seeing when first entering a very dark or bright area. That's because as you age, your eye muscles slow down, causing your eyes' pupils to react more slowly to changes in light. After age 70, the ability to see fine details diminishes as well, because there are fewer nerve cells to transmit visual signals to the brain.
If you're plagued by dry eye, medications like Restasis can help create more tears.
Finally, some 68 percent of 70-somethings experience some degree of hearing loss. What to do? Swallow your pride and get tested for hearing aids, which have been associated with less cognitive decline and dementia. Wearing the devices could pay off in the long run, experts say, by helping you stay engaged with others and your environment.
What's Up With That? Have you noticed that blues seem gray and reds appear more intense? Not to worry. It's just changes in the lenses in your eyes, which have started to yellow with age. If it gets too bad, you may need cataract surgery. About half of people ages 65 through 74 have cataracts; the number rises to more than 70 percent among those 75 or older.
What's Ahead: Your senses of smell and taste have likely declined, reducing the ability to enjoy subtle flavors. Taste buds decrease in number and sensitivity, and nerve endings in the nose may not work as well. The fix? Turn up the dial on seasonings. Ethnic cuisines like Indian and Thai contain spices and herbs that amplify the aromas and tastes of foods.
Improve Your Sex Life:
The Good News: Sex in your 70s and beyond? You bet! A recent survey found that 70-year-old men and women were much more likely to be sexually active, to report being in a happy relationship and to have a positive attitude toward sex than people that age who were polled in the 1970s and 1990s. Some 44 percent of women 68 through 80 report being very satisfied with their sex lives, compared with just 30 percent of women 55 to 68 years old.
The Not-So-Good News: Sex-related hormones — estrogen and progesterone in women, testosterone in men — decline, and vaginal dryness may become more noticeable. But lubricants are effective, as are prescription creams and tablets.
What's Up With That? Rates of erectile dysfunction (ED) increase with age; by 70, between 40 and 60 percent of men will experience symptoms. Research shows that not smoking and eating a diet rich in antioxidants can help.
What's Ahead: A University of Chicago study finds almost 40 percent of men 75 to 85 are sexually active.
Motivate Your Metabolism:
The Good News: While metabolism typically slows up to 5 percent per decade, that doesn't mean you have to gain weight in your 70s. Just stay active and cut calories if needed, says Alice Lichtenstein, D.Sc., director of the Cardiovascular Nutrition Laboratory at the USDA Human Nutrition Research Center on Aging.
The Not-So-Good News: In your 70s you may secrete less hydrochloric acid, which decreases the availability of vitamin B12, says Lichtenstein. Ask your doctor if you need a B12 supplement (optimal dose: 2.4 mcg daily).
What's Up With That? As you age, your ability to produce vitamin D in response to sunlight gradually decreases. Your doctor may recommend a vitamin D supplement — after age 70, you need 800 IU of vitamin D every day, as well as 1,200 mg daily of calcium.
What's Ahead: The sensations of hunger and thirst can decrease with age, often leading to dehydration and malnutrition. Plan to eat several small meals throughout the day, and consume at least 6 cups of liquid.
Ramp Up Your Immunity:
The Good News: Allergies, which result from an overreactive immune system, are likely a thing of the past, because your immune system isn't as sensitive.
The Not-So-Good News: That less-aggressive immune response means you're more susceptible to getting sick. Chronic inflammation, which is linked to heart disease, diabetes and arthritis, makes it even harder for the body to mount an effective immune response. So it's important to shed excess pounds, eat a good diet and exercise.
What's Up With That? Your response to vaccines decreases with age, leaving you even more vulnerable to illnesses like flu and pneumonia. After 65 you're eligible to get a higher-dose flu vaccine. A new study also suggests you can boost the effectiveness of your vaccines by getting at least seven hours of sleep a night.
What's Ahead: Rates of cancer rise with age but then level off around 85, so if you've gotten that far cancer-free, you may reach a very old age.
Keep Your Heart Strong:
The Good News: Older hearts pump about the same volume of blood with each beat as younger hearts.
The Not-So-Good News: Your heart's walls are getting thicker and its valves are stiffer. One way to improve your heart health? Keep moving. Research recently showed that women and men age 70-plus who spent as little as a half hour a day on activities like walking and dancing had a 20 to 40 percent lower risk of dying from heart disease than those who reported no activity.
What's Up With That? A skipped beat or a racing heart could be atrial fibrillation, a type of heart arrhythmia that becomes more common with age. Since it can increase the risk of stroke, mention it to your doctor. You should also say if you're experiencing unusual fatigue, weakness when exercising or dizziness.
What's Ahead: Heart disease incidence rises; it's the leading cause of death for people 75 through 84.
Take Fewer Nighttime Trips:
The Good News: If you're generally healthy, your urological system likely functions pretty well. And an array of therapies can help when problems crop up.
The Not-So-Good News: Bladder tissue contracts and expands less efficiently as you get older, often leading to overactive bladder, incontinence and infection. About 60 percent of women in their 70s will experience some type of urinary incontinence. Ask your doctor about bladder training, medications and pelvic floor exercises ("Kegels"), which can strengthen the muscles around the bladder. More than half of men in their 70s experience symptoms of an enlarged prostate gland, called benign prostatic hyperplasia (BPH). Symptoms include a weak urine flow or difficulty urinating, but medications like tamsulosin and finasteride can help.
What's Up With That? Gotta go during the night? Not to worry; that's normal. "In their 60s, 80 percent of people need to get up at least once a night," says Ryan P. Terlecki, M.D., assistant professor of urology at Wake Forest University School of Medicine in Winston-Salem, North Carolina. And 25 to 35 percent of those in their 70s get up at least twice. Try decreasing fluids after 6 p.m. and avoiding caffeine in the afternoon. If you're on diuretics for high blood pressure, speak to your doctor about taking your pill in the morning.
What's Ahead: Urinary tract infections are common as you age. The counterintuitive advice? If you're not experiencing symptoms, sometimes it's better to do nothing. Antibiotics can clear up the infection, but they often disrupt other bacterial balances.
Be Happy:
The Good News: We're pretty happy. A recent AARP survey showed that of all the decades surveyed, the 70s tend to be some of the happiest years of your life. One explanation for the trend: years of experience. "As you get older, you know that bad times are going to pass," says Laura Carstensen, Ph.D., director of the Stanford Center on Longevity. "You also know that good times will pass, which makes those good times even more precious."
The Not-So-Good News: You might stay away from stressful situations, thereby missing out on new opportunities. Just make sure all of your social interactions stay strong. They may be key to facing future challenges with resilience.
What's Up With That? Does your spouse seem mellower than he or she once did? "The ability to regulate one's emotions improves as you get older," says Bob Knight, Ph.D., professor of gerontology and psychology at the USC Davis School of Gerontology in Los Angeles.
What's Ahead: As long as your health remains good, you can expect to be happy. Studies also suggest that negative emotions like anger and sadness become less frequent with age, perhaps because older adults get better at tuning out negativity.
Stay Sharp:
The Good News: Research shows that the steep loss of brain function once thought intrinsic to aging is often avoidable. "You can improve your brain health by getting regular mental stimulation, social interaction and physical activity," says Gary J. Kennedy, M.D., professor of psychiatry and behavioral science in the Division of Geriatric Psychiatry at Montefiore Medical Center in the Bronx, New York. And your gut instincts remain sharp as you age, too. In one study, older adults fared as well as those under 30 on intuitive decisions.
The Not-So-Good News: Part of your brain circuitry starts to burn out with age, but most of us compensate by relying on other parts of our brain, and our past experiences, to make decisions. "That's the 'wisdom' that accrues with older age," says Kennedy.
What's Up With That? Feeling increasingly forgetful? This happens because the transmission of nerve impulses between cells slows down as you age.
What's Ahead: Real cognitive decline becomes more prevalent by your 80s; nearly half of Americans 85 or older have Alzheimer's. Your best prevention plan, as Kennedy advises: intellectual stimulation, time with family and friends, and exercise.
[End of Article]
Everyone ages differently, and lifestyle plays a major role, but you'll experience both hard-to-notice and impossible-to-miss changes in your physical and mental health.
Read on for the good, the bad and the what's-up-with-that? transformations you'll encounter — plus the latest advice on feeling happy, sexy and pain-free.
Save Your Skin
The Good News: Your skin is drier, which can be welcome relief for the third of women who were plagued by oily skin and breakouts throughout their adulthood.
The Not-So-Good News: Wrinkles and lines are more plentiful, but so are the options for keeping skin looking bright. Gentle exfoliation and moisturizing are especially important.
Pick skin products with antioxidants and glycolic acid, which promote skin thickening and increase collagen production. And apply a broad-spectrum sunscreen with a sun protection factor (SPF) of at least 30 every day.
Laser treatments can help with dilated superficial blood vessels (called telangiectasias), which tend to appear without warning on the cheeks, nose, chin and legs. (The laser destroys the blood vessels underneath the skin - with no scarring.) And those extra skin tags? Your doctor can remove them through freezing, snipping or cauterizing.
What's Up With That? Non-articular cartilage, the type that gives ears and noses their shape, continues to grow with age, making these appendages larger. But look on the bright side: Such cartilage growth may have evolved to enable people to track and funnel sounds and smells as they age, suggests James Stankiewicz, M.D., chair of the Department of Otolaryngology — Head and Neck Surgery at Loyola University Chicago Stritch School of Medicine.
What's Ahead: As you age, the skin around your jawline tends to sag. If you're bothered by it, ask your doctor about skin-tightening radio-frequency treatments, which can tighten skin without damaging the epidermis.
Bone Up for Good Health:
The Good News: You can maintain muscle strength through activity.
The Not-So-Good News: About one in three women ages 75 through 85 has osteoporosis, a bone-thinning disease, which greatly increases the risk of fractures of the hip and spine. Studies show strength training can build muscle, which can take force off the joints. Plus, weight-bearing activities stimulate the bones to grow stronger and denser.
What's Up With That? Although worn joints may benefit from anti-inflammatory drugs and activity, surgery may become necessary as cartilage loss begins to accelerate. Regenerative techniques such as platelet-rich plasma and autologous (self) stem cell injections may also help, according to Nathan Wei, M.D., a rheumatologist in Frederick, Md.
What's Ahead: Joint-replacement surgeries are common; one study showed that patients 75-plus recover just as quickly as those 65 to 74.
Preserve Your Senses:
The Good News: Lifestyle plays a major role in helping to maintain your senses as you age. So stay away from loud noises, eat a well-balanced diet (which can help ward off such age-related eye disorders as macular degeneration) and see a doctor immediately if you notice that your senses of smell or taste diminish significantly. (This may indicate a sinus infection or be a reaction to medication.)
The Not-So-Good News: You may have trouble seeing when first entering a very dark or bright area. That's because as you age, your eye muscles slow down, causing your eyes' pupils to react more slowly to changes in light. After age 70, the ability to see fine details diminishes as well, because there are fewer nerve cells to transmit visual signals to the brain.
If you're plagued by dry eye, medications like Restasis can help create more tears.
Finally, some 68 percent of 70-somethings experience some degree of hearing loss. What to do? Swallow your pride and get tested for hearing aids, which have been associated with less cognitive decline and dementia. Wearing the devices could pay off in the long run, experts say, by helping you stay engaged with others and your environment.
What's Up With That? Have you noticed that blues seem gray and reds appear more intense? Not to worry. It's just changes in the lenses in your eyes, which have started to yellow with age. If it gets too bad, you may need cataract surgery. About half of people ages 65 through 74 have cataracts; the number rises to more than 70 percent among those 75 or older.
What's Ahead: Your senses of smell and taste have likely declined, reducing the ability to enjoy subtle flavors. Taste buds decrease in number and sensitivity, and nerve endings in the nose may not work as well. The fix? Turn up the dial on seasonings. Ethnic cuisines like Indian and Thai contain spices and herbs that amplify the aromas and tastes of foods.
Improve Your Sex Life:
The Good News: Sex in your 70s and beyond? You bet! A recent survey found that 70-year-old men and women were much more likely to be sexually active, to report being in a happy relationship and to have a positive attitude toward sex than people that age who were polled in the 1970s and 1990s. Some 44 percent of women 68 through 80 report being very satisfied with their sex lives, compared with just 30 percent of women 55 to 68 years old.
The Not-So-Good News: Sex-related hormones — estrogen and progesterone in women, testosterone in men — decline, and vaginal dryness may become more noticeable. But lubricants are effective, as are prescription creams and tablets.
What's Up With That? Rates of erectile dysfunction (ED) increase with age; by 70, between 40 and 60 percent of men will experience symptoms. Research shows that not smoking and eating a diet rich in antioxidants can help.
What's Ahead: A University of Chicago study finds almost 40 percent of men 75 to 85 are sexually active.
Motivate Your Metabolism:
The Good News: While metabolism typically slows up to 5 percent per decade, that doesn't mean you have to gain weight in your 70s. Just stay active and cut calories if needed, says Alice Lichtenstein, D.Sc., director of the Cardiovascular Nutrition Laboratory at the USDA Human Nutrition Research Center on Aging.
The Not-So-Good News: In your 70s you may secrete less hydrochloric acid, which decreases the availability of vitamin B12, says Lichtenstein. Ask your doctor if you need a B12 supplement (optimal dose: 2.4 mcg daily).
What's Up With That? As you age, your ability to produce vitamin D in response to sunlight gradually decreases. Your doctor may recommend a vitamin D supplement — after age 70, you need 800 IU of vitamin D every day, as well as 1,200 mg daily of calcium.
What's Ahead: The sensations of hunger and thirst can decrease with age, often leading to dehydration and malnutrition. Plan to eat several small meals throughout the day, and consume at least 6 cups of liquid.
Ramp Up Your Immunity:
The Good News: Allergies, which result from an overreactive immune system, are likely a thing of the past, because your immune system isn't as sensitive.
The Not-So-Good News: That less-aggressive immune response means you're more susceptible to getting sick. Chronic inflammation, which is linked to heart disease, diabetes and arthritis, makes it even harder for the body to mount an effective immune response. So it's important to shed excess pounds, eat a good diet and exercise.
What's Up With That? Your response to vaccines decreases with age, leaving you even more vulnerable to illnesses like flu and pneumonia. After 65 you're eligible to get a higher-dose flu vaccine. A new study also suggests you can boost the effectiveness of your vaccines by getting at least seven hours of sleep a night.
What's Ahead: Rates of cancer rise with age but then level off around 85, so if you've gotten that far cancer-free, you may reach a very old age.
Keep Your Heart Strong:
The Good News: Older hearts pump about the same volume of blood with each beat as younger hearts.
The Not-So-Good News: Your heart's walls are getting thicker and its valves are stiffer. One way to improve your heart health? Keep moving. Research recently showed that women and men age 70-plus who spent as little as a half hour a day on activities like walking and dancing had a 20 to 40 percent lower risk of dying from heart disease than those who reported no activity.
What's Up With That? A skipped beat or a racing heart could be atrial fibrillation, a type of heart arrhythmia that becomes more common with age. Since it can increase the risk of stroke, mention it to your doctor. You should also say if you're experiencing unusual fatigue, weakness when exercising or dizziness.
What's Ahead: Heart disease incidence rises; it's the leading cause of death for people 75 through 84.
Take Fewer Nighttime Trips:
The Good News: If you're generally healthy, your urological system likely functions pretty well. And an array of therapies can help when problems crop up.
The Not-So-Good News: Bladder tissue contracts and expands less efficiently as you get older, often leading to overactive bladder, incontinence and infection. About 60 percent of women in their 70s will experience some type of urinary incontinence. Ask your doctor about bladder training, medications and pelvic floor exercises ("Kegels"), which can strengthen the muscles around the bladder. More than half of men in their 70s experience symptoms of an enlarged prostate gland, called benign prostatic hyperplasia (BPH). Symptoms include a weak urine flow or difficulty urinating, but medications like tamsulosin and finasteride can help.
What's Up With That? Gotta go during the night? Not to worry; that's normal. "In their 60s, 80 percent of people need to get up at least once a night," says Ryan P. Terlecki, M.D., assistant professor of urology at Wake Forest University School of Medicine in Winston-Salem, North Carolina. And 25 to 35 percent of those in their 70s get up at least twice. Try decreasing fluids after 6 p.m. and avoiding caffeine in the afternoon. If you're on diuretics for high blood pressure, speak to your doctor about taking your pill in the morning.
What's Ahead: Urinary tract infections are common as you age. The counterintuitive advice? If you're not experiencing symptoms, sometimes it's better to do nothing. Antibiotics can clear up the infection, but they often disrupt other bacterial balances.
Be Happy:
The Good News: We're pretty happy. A recent AARP survey showed that of all the decades surveyed, the 70s tend to be some of the happiest years of your life. One explanation for the trend: years of experience. "As you get older, you know that bad times are going to pass," says Laura Carstensen, Ph.D., director of the Stanford Center on Longevity. "You also know that good times will pass, which makes those good times even more precious."
The Not-So-Good News: You might stay away from stressful situations, thereby missing out on new opportunities. Just make sure all of your social interactions stay strong. They may be key to facing future challenges with resilience.
What's Up With That? Does your spouse seem mellower than he or she once did? "The ability to regulate one's emotions improves as you get older," says Bob Knight, Ph.D., professor of gerontology and psychology at the USC Davis School of Gerontology in Los Angeles.
What's Ahead: As long as your health remains good, you can expect to be happy. Studies also suggest that negative emotions like anger and sadness become less frequent with age, perhaps because older adults get better at tuning out negativity.
Stay Sharp:
The Good News: Research shows that the steep loss of brain function once thought intrinsic to aging is often avoidable. "You can improve your brain health by getting regular mental stimulation, social interaction and physical activity," says Gary J. Kennedy, M.D., professor of psychiatry and behavioral science in the Division of Geriatric Psychiatry at Montefiore Medical Center in the Bronx, New York. And your gut instincts remain sharp as you age, too. In one study, older adults fared as well as those under 30 on intuitive decisions.
The Not-So-Good News: Part of your brain circuitry starts to burn out with age, but most of us compensate by relying on other parts of our brain, and our past experiences, to make decisions. "That's the 'wisdom' that accrues with older age," says Kennedy.
What's Up With That? Feeling increasingly forgetful? This happens because the transmission of nerve impulses between cells slows down as you age.
What's Ahead: Real cognitive decline becomes more prevalent by your 80s; nearly half of Americans 85 or older have Alzheimer's. Your best prevention plan, as Kennedy advises: intellectual stimulation, time with family and friends, and exercise.
[End of Article]
Social programs in the United States
YouTube Video: How to Maximize Your Social Security Benefits*
*- by Kiplinger (Leader in personal finance news and business forecasting. Get trusted advice on investing, retirement, taxes, saving, real estate, cars, college, insurance.)
YouTube Video: Medicare & You: Understanding Your Medicare Choices
Pictured: (L) Social Security Administration Logo: (R) Medicare Card
Social programs in the United States are welfare subsidies designed to aid the needs of the American population.
Federal and state welfare programs include cash assistance, healthcare and medical provisions, food assistance, housing subsidies, energy and utilities subsidies, education and childcare assistance, and subsidies and assistance for other basic services. Private provisions from employers, either mandated by policy or voluntary, also provide similar social welfare benefits.
The programs vary in eligibility requirements and are provided by various organizations on a federal, state, local and private level. They help to provide food, shelter, education, healthcare and money to U.S. citizens through:
The Social Security system is sometimes considered to be a social aid program and has some characteristics of such programs, but unlike these programs, social security was designed as a self-funded security blanket - so that as the payee pays in (during working years), they are pre-paying for the payments they'll receive back out of the system when they are no longer working.
Medicare is another prominent program, among other healthcare provisions such as Medicaid and the State Children's Health Insurance Program.
Click on any of the following blue hyperlinks for more about Social Programs in the Untied States:
Federal and state welfare programs include cash assistance, healthcare and medical provisions, food assistance, housing subsidies, energy and utilities subsidies, education and childcare assistance, and subsidies and assistance for other basic services. Private provisions from employers, either mandated by policy or voluntary, also provide similar social welfare benefits.
The programs vary in eligibility requirements and are provided by various organizations on a federal, state, local and private level. They help to provide food, shelter, education, healthcare and money to U.S. citizens through:
- primary and secondary education,
- subsidies of college education,
- unemployment disability insurance,
- subsidies for eligible low-wage workers,
- subsidies for housing,
- Supplemental Nutrition Assistance Program benefits,
- pensions for eligible persons,
- and health insurance programs that cover public employees.
The Social Security system is sometimes considered to be a social aid program and has some characteristics of such programs, but unlike these programs, social security was designed as a self-funded security blanket - so that as the payee pays in (during working years), they are pre-paying for the payments they'll receive back out of the system when they are no longer working.
Medicare is another prominent program, among other healthcare provisions such as Medicaid and the State Children's Health Insurance Program.
Click on any of the following blue hyperlinks for more about Social Programs in the Untied States:
Social Security Administration (SSA.Gov)
YouTube Video: How Social Security Works
YouTube Video: Big Changes Coming to Social Security!
Pictured: Social Security Administration (L) Logo (R) Card
The United States Social Security Administration (SSA) is an independent agency of the U.S. federal government that administers Social Security, a social insurance program consisting of retirement, disability, and survivors' benefits.
To qualify for most of these benefits, most workers pay Social Security taxes on their earnings; the claimant's benefits are based on the wage earner's contributions. Otherwise benefits such as Supplemental Security Income (SSI) are given based on need.
The Social Security Administration was established by a law codified at 42 U.S.C. § 901. Its current commissioner, Nancy Berryhill (Acting), was appointed January 19, 2017, and will serve until the true Presidential appointment takes office.
SSA is headquartered in Woodlawn, Maryland, just to the west of Baltimore, at what is known as Central Office. The agency includes 10 regional offices, 8 processing centers, approximately 1300 field offices, and 37 Teleservice Centers.
As of 2007, about 62,000 people were employed by SSA. Headquarters non-supervisory employees of SSA are represented by American Federation of Government Employees Local 1923. Social Security is the largest social welfare program in the United States.
For the year 2014, the net cost of social security was 906.4 billion dollars which accounted for 21% of government expenditure.
It has been named the 9th best place to work in the federal government.
Click on any of the following blue hyperlinks for more about the Social Security Administration:
To qualify for most of these benefits, most workers pay Social Security taxes on their earnings; the claimant's benefits are based on the wage earner's contributions. Otherwise benefits such as Supplemental Security Income (SSI) are given based on need.
The Social Security Administration was established by a law codified at 42 U.S.C. § 901. Its current commissioner, Nancy Berryhill (Acting), was appointed January 19, 2017, and will serve until the true Presidential appointment takes office.
SSA is headquartered in Woodlawn, Maryland, just to the west of Baltimore, at what is known as Central Office. The agency includes 10 regional offices, 8 processing centers, approximately 1300 field offices, and 37 Teleservice Centers.
As of 2007, about 62,000 people were employed by SSA. Headquarters non-supervisory employees of SSA are represented by American Federation of Government Employees Local 1923. Social Security is the largest social welfare program in the United States.
For the year 2014, the net cost of social security was 906.4 billion dollars which accounted for 21% of government expenditure.
It has been named the 9th best place to work in the federal government.
Click on any of the following blue hyperlinks for more about the Social Security Administration:
- History
- Headquarters
- Coverage
- Operations
- Criticism and controversy
- Baby name popularity report
- See also:
- Title 20 of the Code of Federal Regulations
- American welfare state
- Social Security (United States)
- Social Security disability insurance
- Social Security number
- Government operations
- Social Security Death Index
- NOSSCR National Organization of Social Security Claimants' Representatives
- Ticket to Work SSA's Ticket to Work Program
- Richardson v. Perales
Medicare Advantage and Choosing a Medigap Policy
- YouTube Video: What is Medigap and What Do Medigap Plans Cover?
- YouTube Video: Medicare Advantage Plans Pros and Cons
- YouTube Video: Medicare Supplement Plans 2019 - The Top 3 Best Plans
Medicare Advantage is a type of health insurance plan that provides coverage within Part C of Medicare in the United States.
Medicare Advantage health plans pay for managed health care based on a monthly fee per enrollee (capitation), rather than on the basis of billing a fee for each medical service provided (fee-for-service (FFS)), which is the way Original Medicare Parts A and B work.
Most such plans are health maintenance organizations (HMOs) or preferred provider organizations (PPOs).
Medicare Advantage plans finance at a minimum the same medical services as "Original" Parts A and B Medicare finance via FFS. Public Part C plans, including Medicare Advantage plans, also typically finance additional services, including additional health services, and most importantly include an annual out of pocket (OOP) spend limit not included in Parts A and B. A public Part C Medicare Advantage beneficiary must first sign up for both Part A and Part B of Medicare in order to choose Part C.
All four Parts of Medicare—A, B and C, and D—are administered by private companies under contract to the Centers for Medicare and Medicaid Services (CMS). Almost all these companies are insurance companies, except for those that administer most Medicare Advantage and other Part C plans.
Most Medicare Advantage and other Part C plans are administered (CMS uses the term "sponsored") by non-profit integrated health delivery systems and their spin offs. Other sponsors include non-profit charities under their respective states' laws, and/or are under union or religious management.
Public Part C health plans, including Medicare Advantage plans, not only cover the same medical services as Parts A and B but also typically include an annual physical exam and vision and/or dental coverage of some sort not covered under Original Medicare Parts A and B. (Medicare Part A provides FFS payments for admitted in-patient hospital care, hospice, and skilled nursing services if a person is first admitted inpatient for three days.
Part B provides payments for most physician and surgical services, even some that take place in hospitals and skilled nursing facilities after admittance, as well as for medically necessary outpatient hospital services such as ER, surgical center, laboratory, X-rays and diagnostic tests, certain preventative medical services, and certain durable medical equipment and supplies.) Less often, hearing and wellness benefits not found in Original Medicare are included in a Medicare Advantage plan.
The most important difference between a Part C health plan and FFS Original Medicare is that all Part C plans, including Part C Medicare Advantage plans, include a limit on how much a beneficiary will have to spend annually OOP; that amount is unlimited in Original Medicare Parts A and B.
Most but not all Medicare Advantage plans (and many of the other public managed-care health plans within Medicare Part C) include integrated self-administered drug coverage similar to the standalone Part D prescription drug benefit plan. The federal government makes separate capitated-fee payments to Medicare Advantage plan sponsors for providing these Part-D-like benefits if applicable just as it does for the sponsor of a plan that anyone on Original Medicare using Part D might have.
Nearly all Medicare beneficiaries (99%) had access to at least one Medicare Advantage plan in 2015; the average beneficiary had access to 18 plans in 2015. This number varies yearly as new sponsors apply to CMS and/or old ones drop out.
Click on any of the following blue hyperlinks for more about Medicare Advantage:
Medicare Advantage health plans pay for managed health care based on a monthly fee per enrollee (capitation), rather than on the basis of billing a fee for each medical service provided (fee-for-service (FFS)), which is the way Original Medicare Parts A and B work.
Most such plans are health maintenance organizations (HMOs) or preferred provider organizations (PPOs).
Medicare Advantage plans finance at a minimum the same medical services as "Original" Parts A and B Medicare finance via FFS. Public Part C plans, including Medicare Advantage plans, also typically finance additional services, including additional health services, and most importantly include an annual out of pocket (OOP) spend limit not included in Parts A and B. A public Part C Medicare Advantage beneficiary must first sign up for both Part A and Part B of Medicare in order to choose Part C.
All four Parts of Medicare—A, B and C, and D—are administered by private companies under contract to the Centers for Medicare and Medicaid Services (CMS). Almost all these companies are insurance companies, except for those that administer most Medicare Advantage and other Part C plans.
Most Medicare Advantage and other Part C plans are administered (CMS uses the term "sponsored") by non-profit integrated health delivery systems and their spin offs. Other sponsors include non-profit charities under their respective states' laws, and/or are under union or religious management.
Public Part C health plans, including Medicare Advantage plans, not only cover the same medical services as Parts A and B but also typically include an annual physical exam and vision and/or dental coverage of some sort not covered under Original Medicare Parts A and B. (Medicare Part A provides FFS payments for admitted in-patient hospital care, hospice, and skilled nursing services if a person is first admitted inpatient for three days.
Part B provides payments for most physician and surgical services, even some that take place in hospitals and skilled nursing facilities after admittance, as well as for medically necessary outpatient hospital services such as ER, surgical center, laboratory, X-rays and diagnostic tests, certain preventative medical services, and certain durable medical equipment and supplies.) Less often, hearing and wellness benefits not found in Original Medicare are included in a Medicare Advantage plan.
The most important difference between a Part C health plan and FFS Original Medicare is that all Part C plans, including Part C Medicare Advantage plans, include a limit on how much a beneficiary will have to spend annually OOP; that amount is unlimited in Original Medicare Parts A and B.
Most but not all Medicare Advantage plans (and many of the other public managed-care health plans within Medicare Part C) include integrated self-administered drug coverage similar to the standalone Part D prescription drug benefit plan. The federal government makes separate capitated-fee payments to Medicare Advantage plan sponsors for providing these Part-D-like benefits if applicable just as it does for the sponsor of a plan that anyone on Original Medicare using Part D might have.
Nearly all Medicare beneficiaries (99%) had access to at least one Medicare Advantage plan in 2015; the average beneficiary had access to 18 plans in 2015. This number varies yearly as new sponsors apply to CMS and/or old ones drop out.
Click on any of the following blue hyperlinks for more about Medicare Advantage:
- History
- Program structure
- Usage
- See also:
- Government links - current:
- CMS official web site at cms.hhs.gov
- Legal Issues Relating to the Secretary’s Authority to Set Payment Rates Under the Medicare Advantage Program Congressional Research Service
- Medicare.gov — the official website for people with Medicare
- Private links:
- Medicare & Medicaid Resources — Medicare information site
- Kaiser Family Foundation — Wide range of free information about the Medicare program and other U.S. health issues including state-level data on health care spending and utilization, including Medicare.
- Medicare - Alliance for Health Reform The nonpartisan, nonprofit Alliance for Health Reform offers information about health reform, in a number of formats, to elected officials and their staffs, journalists, policy analysts and advocates.
- Social Security and Disability News Resource Center
- How Stuff Works - Medicare
- Government links - current:
Aging-Associated Diseases
- YouTube Video: What is AGING ASSOCIATED DISEASE? What does AGING ASSOCIATED DISEASE mean?
- YouTube Video: Can we defeat the diseases of aging? | James Peyer | TEDxStuttgart
- YouTube Video: Bruce Ames - Vitamin and Mineral Inadequacy Accelerates Aging-Associated Diseases
* -- Decline of NAD+* during Aging, Age-Related Diseases, and Cancer (see image above): See also The Plasma NAD+ Metabolome Is Dysregulated in "Normal" Aging.
Aging-associated diseases:
An aging-associated disease is a disease that is most often seen with increasing frequency with increasing senescence. Essentially, aging-associated diseases are complications arising from senescence. Age-associated diseases are to be distinguished from the aging process itself because all adult animals age, save for a few rare exceptions, but not all adult animals experience all age-associated diseases.
Aging-associated diseases do not refer to age-specific diseases, such as the childhood diseases chicken pox and measles. "Aging-associated disease" is used here to mean "diseases of the elderly". Nor should aging-associated diseases be confused with accelerated aging diseases, all of which are genetic disorders.
Examples of aging-associated diseases are:
The incidence of all of these diseases increases exponentially with age.
Of the roughly 150,000 people who die each day across the globe, about two thirds—100,000 per day—die of age-related causes. In industrialized nations, the proportion is higher, reaching 90%.
Patterns of differences:
By age 3 about 30% of rats have had cancer, whereas by age 85 about 30% of humans have had cancer. Humans, dogs and rabbits get Alzheimer's disease, but rodents do not. Elderly rodents typically die of cancer or kidney disease, but not of cardiovascular disease.
In humans, the relative incidence of cancer increases exponentially with age for most cancers, but levels off or may even decline by age 60–75 (although colon/rectal cancer continues to increase).
People with the so-called segmental progerias are vulnerable to different sets of diseases.
Those with Werner's syndrome suffer from osteoporosis, cataracts, and cardiovascular disease, but not neurodegeneration or Alzheimer's disease; those with Down syndrome suffer type 2 diabetes and Alzheimer's disease, but not high blood pressure, osteoporosis or cataracts.
In Bloom syndrome, those afflicted most often die of cancer.
Research:
Aging (senescence) increases vulnerability to age-associated diseases, whereas genetics determines vulnerability or resistance between species and individuals within species.
Some age-related changes (like graying hair) are said to be unrelated to an increase in mortality. But some biogerontologists believe that the same underlying changes that cause graying hair also increase mortality in other organ systems and that understanding the incidence of age-associated disease will advance knowledge of the biology of senescence just as knowledge of childhood diseases advanced knowledge of human development.
Strategies for Engineered Negligible Senescence (SENS) is a research strategy which aims to repair a few "root causes" for age-related illness and degeneration, as well as develop medical procedures to periodically repair all such damage in the human body, thereby maintaining a youth-like state indefinitely.
So far, the SENS programme has identified seven types of aging-related damage, and feasible solutions have been outlined for each. However, critics argue that the SENS agenda is optimistic at best, and that the aging process is too complex and little-understood for SENS to be scientific or implementable in the foreseeable future.
Recently it has been proposed that age-related diseases are mediated by vicious cycles [10]
Diseases:
Age-Related Macular Degeneration (AMD):
Age-Related Macular Degeneration (AMD) is a disease that affects the eyes and can lead to vision loss through break down of the central part of the retina called the macula.
Degeneration can occur in one eye or both and can be classified as either wet (neovascular) or dry (atrophic). Wet AMD commonly is caused by blood vessels near the retina that lead to swelling of the macula. The cause of dry AMD is less clear, but it is thought to be partly caused by breakdown of light-sensitive cells and tissue surrounding the macula. A major risk factor for AMD is age over the age of 60.
Alzheimer's disease:
Alzheimer's disease is classified as a "protein misfolding" disease. Aging causes mutations in protein folding, and as a result causes deposits of abnormal modified proteins accumulate in specific areas of the brain.
In Alzheimer's, deposits of Beta-amyloid and hyperphosphorylated tau protein form extracellular plaques and extracellular tangles. These deposits are shown to be neurotoxic and cause cognitive impairment due to their initiation of destructive biochemical pathways.
Atherosclerosis:
Atherosclerosis is categorized as an aging disease and is brought about by vascular remodeling, the accumulation of plaque, and the loss of arterial elasticity. Over time, these processes can stiffen the vasculature. For these reasons, older age is listed as a major risk factor for atherosclerosis. Specifically, the risk of atherosclerosis increases for men above 45 years of age and women above 55 years of age.
Benign Prostatic Hyperplasia (BPH):
Benign prostatic hyperplasia (BPH) is a noncancerous enlargement of the prostate gland due to increased growth.
An enlarged prostate can result in incomplete or complete blockage of the bladder and interferes with a man's ability to urinate properly. Symptoms include overactive bladder, decreased stream of urine, hesitancy urinating, and incomplete emptying of the bladder.
By age 40, 10% of men will have signs of BPH and by age 60, this percentage increases by 5 fold. Men over the age of 80 have over a 90% chance of developing BPH and almost 80% of men will develop BPH in their lifetime.
See also:
Aging-associated diseases:
An aging-associated disease is a disease that is most often seen with increasing frequency with increasing senescence. Essentially, aging-associated diseases are complications arising from senescence. Age-associated diseases are to be distinguished from the aging process itself because all adult animals age, save for a few rare exceptions, but not all adult animals experience all age-associated diseases.
Aging-associated diseases do not refer to age-specific diseases, such as the childhood diseases chicken pox and measles. "Aging-associated disease" is used here to mean "diseases of the elderly". Nor should aging-associated diseases be confused with accelerated aging diseases, all of which are genetic disorders.
Examples of aging-associated diseases are:
- atherosclerosis and cardiovascular disease,
- cancer,
- arthritis,
- cataracts,
- osteoporosis,
- type 2 diabetes,
- hypertension
- and Alzheimer's disease.
The incidence of all of these diseases increases exponentially with age.
Of the roughly 150,000 people who die each day across the globe, about two thirds—100,000 per day—die of age-related causes. In industrialized nations, the proportion is higher, reaching 90%.
Patterns of differences:
By age 3 about 30% of rats have had cancer, whereas by age 85 about 30% of humans have had cancer. Humans, dogs and rabbits get Alzheimer's disease, but rodents do not. Elderly rodents typically die of cancer or kidney disease, but not of cardiovascular disease.
In humans, the relative incidence of cancer increases exponentially with age for most cancers, but levels off or may even decline by age 60–75 (although colon/rectal cancer continues to increase).
People with the so-called segmental progerias are vulnerable to different sets of diseases.
Those with Werner's syndrome suffer from osteoporosis, cataracts, and cardiovascular disease, but not neurodegeneration or Alzheimer's disease; those with Down syndrome suffer type 2 diabetes and Alzheimer's disease, but not high blood pressure, osteoporosis or cataracts.
In Bloom syndrome, those afflicted most often die of cancer.
Research:
Aging (senescence) increases vulnerability to age-associated diseases, whereas genetics determines vulnerability or resistance between species and individuals within species.
Some age-related changes (like graying hair) are said to be unrelated to an increase in mortality. But some biogerontologists believe that the same underlying changes that cause graying hair also increase mortality in other organ systems and that understanding the incidence of age-associated disease will advance knowledge of the biology of senescence just as knowledge of childhood diseases advanced knowledge of human development.
Strategies for Engineered Negligible Senescence (SENS) is a research strategy which aims to repair a few "root causes" for age-related illness and degeneration, as well as develop medical procedures to periodically repair all such damage in the human body, thereby maintaining a youth-like state indefinitely.
So far, the SENS programme has identified seven types of aging-related damage, and feasible solutions have been outlined for each. However, critics argue that the SENS agenda is optimistic at best, and that the aging process is too complex and little-understood for SENS to be scientific or implementable in the foreseeable future.
Recently it has been proposed that age-related diseases are mediated by vicious cycles [10]
Diseases:
Age-Related Macular Degeneration (AMD):
Age-Related Macular Degeneration (AMD) is a disease that affects the eyes and can lead to vision loss through break down of the central part of the retina called the macula.
Degeneration can occur in one eye or both and can be classified as either wet (neovascular) or dry (atrophic). Wet AMD commonly is caused by blood vessels near the retina that lead to swelling of the macula. The cause of dry AMD is less clear, but it is thought to be partly caused by breakdown of light-sensitive cells and tissue surrounding the macula. A major risk factor for AMD is age over the age of 60.
Alzheimer's disease:
Alzheimer's disease is classified as a "protein misfolding" disease. Aging causes mutations in protein folding, and as a result causes deposits of abnormal modified proteins accumulate in specific areas of the brain.
In Alzheimer's, deposits of Beta-amyloid and hyperphosphorylated tau protein form extracellular plaques and extracellular tangles. These deposits are shown to be neurotoxic and cause cognitive impairment due to their initiation of destructive biochemical pathways.
Atherosclerosis:
Atherosclerosis is categorized as an aging disease and is brought about by vascular remodeling, the accumulation of plaque, and the loss of arterial elasticity. Over time, these processes can stiffen the vasculature. For these reasons, older age is listed as a major risk factor for atherosclerosis. Specifically, the risk of atherosclerosis increases for men above 45 years of age and women above 55 years of age.
Benign Prostatic Hyperplasia (BPH):
Benign prostatic hyperplasia (BPH) is a noncancerous enlargement of the prostate gland due to increased growth.
An enlarged prostate can result in incomplete or complete blockage of the bladder and interferes with a man's ability to urinate properly. Symptoms include overactive bladder, decreased stream of urine, hesitancy urinating, and incomplete emptying of the bladder.
By age 40, 10% of men will have signs of BPH and by age 60, this percentage increases by 5 fold. Men over the age of 80 have over a 90% chance of developing BPH and almost 80% of men will develop BPH in their lifetime.
See also:
Geriatics vs. Geronotology and the National Institute on Aging
- YouTube Video: How to use the popular selfie app FaceApp
- YouTube Video: How Alzheimer's Changes the Brain
- YouTube Video: What you can do to prevent Alzheimer's | Lisa Genova
Geriatrics, or geriatric medicine, is a specialty that focuses on health care of elderly people. It aims to promote health by preventing and treating diseases and disabilities in older adults.
There is no set age at which patients may be under the care of a geriatrician, or geriatric physician, a physician who specializes in the care of elderly people. Rather, this decision is determined by the individual patient's needs, and the availability of a specialist. It is important to note the difference between geriatrics, the care of aged people, and gerontology (see below following this topic.)
The term geriatrics comes from the Greek γέρων geron meaning "old man", and ιατρός iatros meaning "healer". However, geriatrics is sometimes called medical gerontology.
Click on any of the following blue hyperlinks for more about Geriatics Medicine:
___________________________________________________________________________
Gerontology is the study of the social, cultural, psychological, cognitive, and biological aspects of ageing. The word was coined by Ilya Ilyich Mechnikov in 1903, from the Greek γέρων, geron, "old man" and -λογία, -logia, "study of".
Gerontologists include researchers and practitioners in the fields of biology, nursing, medicine, criminology, dentistry, social work, physical and occupational therapy, psychology, psychiatry, sociology, economics, political science, architecture, geography, pharmacy, public health, housing, and anthropology.
The multidisciplinary nature of gerontology means that there are a number of sub-fields which overlap with gerontology. There are policy issues, for example, involved in government planning and the operation of nursing homes, investigating the effects of an ageing population on society, and the design of residential spaces for older people that facilitate the development of a sense of place or home.
Dr. Lawton, a behavioral psychologist at the Philadelphia Geriatric Center, was among the first to recognize the need for living spaces designed to accommodate the elderly, especially those with Alzheimer's disease. As an academic discipline the field is relatively new. The USC Leonard Davis School created the first PhD, master's and bachelor's degree programs in gerontology in 1975.
Click on any of the following blue hyperlinks for more about Gerontology:
National Institute on Aging
The National Institute on Aging (NIA) is a division of the U.S. National Institutes of Health (NIH), located in Bethesda, Maryland. The NIA itself is headquartered in Baltimore, Maryland.
The NIA leads a broad scientific effort to understand the nature of aging and to extend the healthy, active years of life. In 1974, Congress granted authority to form NIA to provide leadership in aging research, training, health information dissemination, and other programs relevant to aging and older people.
Subsequent amendments to this legislation designated the NIA as the primary Federal agency on Alzheimer's disease research.
Mission:
NIA's mission is to improve the health and well-being of older Americans through research, and specifically to:
Programs:
NIA sponsors research on aging through extramural and intramural programs. The extramural program funds research and training at universities, hospitals, medical centers, and other public and private organizations nationwide. The intramural program conducts basic and clinical research in Baltimore, MD and on the NIH campus in Bethesda, MD.
See also:
There is no set age at which patients may be under the care of a geriatrician, or geriatric physician, a physician who specializes in the care of elderly people. Rather, this decision is determined by the individual patient's needs, and the availability of a specialist. It is important to note the difference between geriatrics, the care of aged people, and gerontology (see below following this topic.)
The term geriatrics comes from the Greek γέρων geron meaning "old man", and ιατρός iatros meaning "healer". However, geriatrics is sometimes called medical gerontology.
Click on any of the following blue hyperlinks for more about Geriatics Medicine:
- Scope
- Subspecialties and related services
- History
- Geriatrician training
- Minimum geriatric competencies
- Research
- Ethical and medico-legal issues
- See also:
- Aging in Place
- Aging-associated diseases
- Alliance for Aging Research
- Commission for Certification in Geriatric Pharmacy
- Elderly care
- Gero-Informatics
- GERRI
- Nosokinetics
- Life extension
- Geriatric medicine in Egypt
- Transgenerational design
- Physical & Occupational Therapy in Geriatrics (journal)
- Gerontological nursing
- Merck Manual of Geriatrics
- Health-EU Portal Care for the elderly in the EU
- American Geriatrics Society
___________________________________________________________________________
Gerontology is the study of the social, cultural, psychological, cognitive, and biological aspects of ageing. The word was coined by Ilya Ilyich Mechnikov in 1903, from the Greek γέρων, geron, "old man" and -λογία, -logia, "study of".
Gerontologists include researchers and practitioners in the fields of biology, nursing, medicine, criminology, dentistry, social work, physical and occupational therapy, psychology, psychiatry, sociology, economics, political science, architecture, geography, pharmacy, public health, housing, and anthropology.
The multidisciplinary nature of gerontology means that there are a number of sub-fields which overlap with gerontology. There are policy issues, for example, involved in government planning and the operation of nursing homes, investigating the effects of an ageing population on society, and the design of residential spaces for older people that facilitate the development of a sense of place or home.
Dr. Lawton, a behavioral psychologist at the Philadelphia Geriatric Center, was among the first to recognize the need for living spaces designed to accommodate the elderly, especially those with Alzheimer's disease. As an academic discipline the field is relatively new. The USC Leonard Davis School created the first PhD, master's and bachelor's degree programs in gerontology in 1975.
Click on any of the following blue hyperlinks for more about Gerontology:
- History
- Aging demographics
- Biogerontology
- Social gerontology
- Environmental gerontology
- Jurisprudential gerontology
- See also:
National Institute on Aging
The National Institute on Aging (NIA) is a division of the U.S. National Institutes of Health (NIH), located in Bethesda, Maryland. The NIA itself is headquartered in Baltimore, Maryland.
The NIA leads a broad scientific effort to understand the nature of aging and to extend the healthy, active years of life. In 1974, Congress granted authority to form NIA to provide leadership in aging research, training, health information dissemination, and other programs relevant to aging and older people.
Subsequent amendments to this legislation designated the NIA as the primary Federal agency on Alzheimer's disease research.
Mission:
NIA's mission is to improve the health and well-being of older Americans through research, and specifically to:
- Support and conduct high-quality research on:
- Aging processes
- Age-related diseases
- Special problems and needs of the aged
- Train and develop highly skilled research scientists from all population groups.
- Develop and maintain state-of-the-art resources to accelerate research progress.
- Disseminate information and communicate with the public and interested groups on health and research advances and on new directions for research.
Programs:
NIA sponsors research on aging through extramural and intramural programs. The extramural program funds research and training at universities, hospitals, medical centers, and other public and private organizations nationwide. The intramural program conducts basic and clinical research in Baltimore, MD and on the NIH campus in Bethesda, MD.
See also:
- NIA homepage
- The University of Southern California Davis School of Gerontology
- American Federation for Aging Research
- Geroscience
- Life extension
"Navigating The New Normal" (AARP July 22, 2020) resulting from the Impact of the COVID-19 pandemic on long-term care facilities
- YouTube Video: How seniors can stay fit during COVID-19 | The A-List
- YouTube Video: COVID-19 and its impact to the elderly`s mental health
- YouTube Video: The COVID-19 Crisis and Seniors in Long-Term Care Facilities
Coronavirus: Navigating the New Normal
AARP: By Craig Davis , July 22, 2020 10:21 AM
How do I maintain a healthy emotional state when I feel isolated?
This week’s live Q&A will focus on the topic of Coronavirus: Navigating the New Normal. During this event experts will provide information, tips and guidance to help 50+ adults navigate the new landscape by focusing on critical questions and life events. Topics and questions include:
Sign up for a free reminder here: https://bit.ly/3ftnZ5G or RSVP to be notified when we go live on Facebook here: https://bit.ly/2BkzyOo
___________________________________________________________________________
Impact of the COVID-19 pandemic on long-term care facilities (Wikipedia)
The COVID-19 pandemic has impacted long-term care facilities and nursing homes around the world. Thousands of residents of these facilities, who are a high-risk group, have died of the disease.
United States:
See also: Nursing home care in the United States
By mid-April 2020, over 7,000 deaths were reported in American nursing homes—about a fifth of the national death toll—and over 36,500 residents and employees had tested positive. (Many facilities were not reporting cases or deaths, implying that the actual toll was higher.) By mid-June, 50,000 deaths—nearly half the national death toll—had been reported in nursing homes.
By April, in addition to steps taken by individual facilities, the federal government had barred visitors, ended group activities, and instituted a mandatory testing regime for workers.
These steps alone do not necessarily prevent infections. Infection control problems were identified at nine locations of Life Care Centers of America during April and early May, as government inspectors identified violations of federal standards.
While some affected facilities are understaffed and have a history of safety violations, others are luxury facilities with excellent records. Regarding testing for coronavirus, the federal government designated long-term care facilities as lower priority than hospitals, leading to longer wait times for test results.
California:
Data analysis by the Los Angeles Times in May found that about half of all coronavirus deaths happened in skilled nursing or assisted living facilities. Governor Gavin Newsom had announced on April 10 that some healthy residents at nursing homes would be transferred to USNS Mercy, a US Navy hospital ship.
The vessel previously was only expected to take patients from southern California hospitals, to free up space there for COVID-19 patients. Six hundred nurses with infectious disease control training were being dispatched to nursing homes and adult care facilities to contain the disease] Some facilities have reorganized residents into discreet buildings for those with and without the virus.
Florida:
As of mid-April 2020, Florida Governor Ron DeSantis was considering a request to grant nursing homes "sovereign immunity" from negligence lawsuits during the pandemic. The request was made by a trade group that represents nearly 700 nursing homes in the state.
Massachusetts:
Life Care Center of Nashoba Valley experienced an outbreak in April 2020. The nurse who reported the outbreak later died of the virus.
One of the most severe outbreaks was at the state-run Holyoke Soldiers' Home for aging veterans. In late March, there were 210 residents; by late May, 74 of them had died with a COVID-19 diagnosis. Dozens of employees also tested positive.
Because the facility is funded by taxpayers and not by Medicare, it is not subject to inspections by Centers for Medicare Services. It is not inspected by the Massachusetts Department of Public Health, either. Following the outbreak, at least four state and federal investigations were opened into the facility.
Maryland:
Sagepoint Senior Living was fined $10,000/day by state regulators. The facility was notified on May 6, 2020 that the fine would be retroactive to March 30 and would continue until Sagepoint complied with state health regulations. At the time of the notification, 34 residents and 1 employee had died from COVID-19 in the 165-bed facility.
Michigan:
Gov. Gretchen Whitmer issued an executive order that nursing homes must readmit residents previously diagnosed with COVID-19.
Minnesota:
The state of Minnesota held a legislative hearing on 7 April into the senior care industry, weeks into a lockdown. The executive director of one facility noted that her residents are showing signs of depression and anxiety from the confinement.
New Jersey:
As of 17 April, two thirds of the state's long-term facilities—a total of 394—had reported cases of the virus, with 1,500 deaths linked to nursing facilities, about 40% of the state's death count.
One facility, Andover Subacute and Rehabilitation Center II, with 543 beds, had a record of safety problems and inadequate staffing. After an anonymous tip, police found seventeen bodies in bags on 13 April. Seventy residents had died of the disease by 19 April. Federal and state investigators have launched an investigation into the facility.
New York:
As of early April, in New York state's 613 licensed facilities, there were nearly 5,000 COVID diagnoses. By mid-April, 72 facilities had five or more confirmed deaths; Cobble Hill Health Center in Brooklyn reported 55 deaths. By early May, it was estimated that 5,000 people had died in nursing homes in New York state.
Washington:
A Life Care Center facility in Kirkland, Washington was the source of a major outbreak of COVID-19 first reported on 19 February 2020, which became the first outbreak in a United States nursing home.
On February 19 there were 120 residents and 180 Center employees at the facility. By 18 March, 101 of the residents had been diagnosed with COVID-19, and thirty-four residents had died, for a case fatality rate of 33.7%. On 2 April 2020 Life Care Center was fined $611,000 for deficiencies in its response to the outbreak, and has until 16 September 2020 to correct the deficiencies, or else face termination of its participation in the Medicare/Medicaid program.
For Other Countries, click here.
AARP: By Craig Davis , July 22, 2020 10:21 AM
How do I maintain a healthy emotional state when I feel isolated?
This week’s live Q&A will focus on the topic of Coronavirus: Navigating the New Normal. During this event experts will provide information, tips and guidance to help 50+ adults navigate the new landscape by focusing on critical questions and life events. Topics and questions include:
- How do you safely proceed with non-critical medical appointments, including elective surgeries, dental procedures, and eye care?
- When will it be okay to shake hands, hug and kiss family, and visit with friends and relatives?
- How do I stay engaged and active and which activities are safest, i.e., church services, swimming, parks, volunteering, dancing, bingo, walking/running/other fitness?
- How do I spot misinformation and scams related to the coronavirus?
- What do I do if I need to provide care for a family member and have no help or lost help during the pandemic? How do I get help?
Sign up for a free reminder here: https://bit.ly/3ftnZ5G or RSVP to be notified when we go live on Facebook here: https://bit.ly/2BkzyOo
___________________________________________________________________________
Impact of the COVID-19 pandemic on long-term care facilities (Wikipedia)
The COVID-19 pandemic has impacted long-term care facilities and nursing homes around the world. Thousands of residents of these facilities, who are a high-risk group, have died of the disease.
United States:
See also: Nursing home care in the United States
By mid-April 2020, over 7,000 deaths were reported in American nursing homes—about a fifth of the national death toll—and over 36,500 residents and employees had tested positive. (Many facilities were not reporting cases or deaths, implying that the actual toll was higher.) By mid-June, 50,000 deaths—nearly half the national death toll—had been reported in nursing homes.
By April, in addition to steps taken by individual facilities, the federal government had barred visitors, ended group activities, and instituted a mandatory testing regime for workers.
These steps alone do not necessarily prevent infections. Infection control problems were identified at nine locations of Life Care Centers of America during April and early May, as government inspectors identified violations of federal standards.
While some affected facilities are understaffed and have a history of safety violations, others are luxury facilities with excellent records. Regarding testing for coronavirus, the federal government designated long-term care facilities as lower priority than hospitals, leading to longer wait times for test results.
California:
Data analysis by the Los Angeles Times in May found that about half of all coronavirus deaths happened in skilled nursing or assisted living facilities. Governor Gavin Newsom had announced on April 10 that some healthy residents at nursing homes would be transferred to USNS Mercy, a US Navy hospital ship.
The vessel previously was only expected to take patients from southern California hospitals, to free up space there for COVID-19 patients. Six hundred nurses with infectious disease control training were being dispatched to nursing homes and adult care facilities to contain the disease] Some facilities have reorganized residents into discreet buildings for those with and without the virus.
Florida:
As of mid-April 2020, Florida Governor Ron DeSantis was considering a request to grant nursing homes "sovereign immunity" from negligence lawsuits during the pandemic. The request was made by a trade group that represents nearly 700 nursing homes in the state.
Massachusetts:
Life Care Center of Nashoba Valley experienced an outbreak in April 2020. The nurse who reported the outbreak later died of the virus.
One of the most severe outbreaks was at the state-run Holyoke Soldiers' Home for aging veterans. In late March, there were 210 residents; by late May, 74 of them had died with a COVID-19 diagnosis. Dozens of employees also tested positive.
Because the facility is funded by taxpayers and not by Medicare, it is not subject to inspections by Centers for Medicare Services. It is not inspected by the Massachusetts Department of Public Health, either. Following the outbreak, at least four state and federal investigations were opened into the facility.
Maryland:
Sagepoint Senior Living was fined $10,000/day by state regulators. The facility was notified on May 6, 2020 that the fine would be retroactive to March 30 and would continue until Sagepoint complied with state health regulations. At the time of the notification, 34 residents and 1 employee had died from COVID-19 in the 165-bed facility.
Michigan:
Gov. Gretchen Whitmer issued an executive order that nursing homes must readmit residents previously diagnosed with COVID-19.
Minnesota:
The state of Minnesota held a legislative hearing on 7 April into the senior care industry, weeks into a lockdown. The executive director of one facility noted that her residents are showing signs of depression and anxiety from the confinement.
New Jersey:
As of 17 April, two thirds of the state's long-term facilities—a total of 394—had reported cases of the virus, with 1,500 deaths linked to nursing facilities, about 40% of the state's death count.
One facility, Andover Subacute and Rehabilitation Center II, with 543 beds, had a record of safety problems and inadequate staffing. After an anonymous tip, police found seventeen bodies in bags on 13 April. Seventy residents had died of the disease by 19 April. Federal and state investigators have launched an investigation into the facility.
New York:
As of early April, in New York state's 613 licensed facilities, there were nearly 5,000 COVID diagnoses. By mid-April, 72 facilities had five or more confirmed deaths; Cobble Hill Health Center in Brooklyn reported 55 deaths. By early May, it was estimated that 5,000 people had died in nursing homes in New York state.
Washington:
A Life Care Center facility in Kirkland, Washington was the source of a major outbreak of COVID-19 first reported on 19 February 2020, which became the first outbreak in a United States nursing home.
On February 19 there were 120 residents and 180 Center employees at the facility. By 18 March, 101 of the residents had been diagnosed with COVID-19, and thirty-four residents had died, for a case fatality rate of 33.7%. On 2 April 2020 Life Care Center was fined $611,000 for deficiencies in its response to the outbreak, and has until 16 September 2020 to correct the deficiencies, or else face termination of its participation in the Medicare/Medicaid program.
For Other Countries, click here.
COVID-19 Safety Tips for Senior Drivers
by Bankrate.com Photo below courtesy of Willowpix/Getty Images
by Bankrate.com Photo below courtesy of Willowpix/Getty Images
COVID-19 Safety Tips for Senior Drivers by Bankrate.com
By Lena Borrelli
Lena Borrelli's Twitter profile
Travel is complicated, even without a global pandemic. For seniors and other high-risk individuals, it can be even more intimidating when you’re dependent on public transportation that presents increased exposure to germs or disease. Planes, buses, taxis and even ride-sharing companies can pose a threat, with COVID-19 potentially floating in the air or living for hours — or even days — on surfaces.
Still, being out and about is sometimes necessary, regardless of your age. There are groceries to be purchased, essential supplies to stock up on and errands or activities to run, such as doctor’s appointments, family visits or religious services. With CDC guidelines urging Americans only to venture out when absolutely mandatory, there has been a marked decline in public transportation use since the beginning of the COVID-19 pandemic, and in particular, seniors are looking for safer ways to travel.
Many seniors have opted to get back behind the wheel, with their personal vehicle serving as a safer means for travel overall. If you are preparing to hit the road during a pandemic, theseare some things to consider for the sake of everyone’s safety.
The impact on seniors:
For seniors, it may have been a while since you were behind the wheel. Family and friends may have enabled or encouraged you to join a community carpool, or perhaps local shuttles gave you a ride to your favorite spots. The arrival and impact of COVID-19 has forced many seniors to consider these alternative forms of transportation — especially if they are unable or unwilling to drive themselves.
Senior transportation:
Shuttles:
Some organizations, like your local medical center or place of worship, may offer you a free ride. When scheduling appointments or making plans, inquire with the venue to see if there are any complimentary or paid shuttles that you can utilize for your visit.
Rideshare for seniors:
Ridesharing is growing in popularity with seniors because it provides an additional outlet for living a more independent life. Instead of dealing with public transit, seniors can use their mobile phone to schedule a private ride through popular companies like Uber and Lyft.
How to book Uber without a smartphone: If you don’t have a cell phone or prefer to use a different device, you can still use Uber. You can use your laptop or desktop computer to book a ride by way of the Uber website.
Family:
If you have family who lives locally and is in good health, consider asking them for a ride. They may need to run many of the same errands you do, creating the perfect opportunity to safely enjoy one another’s company while you check off your to-do list.
Public Transportation:
To help residents get where they need to go, many cities and towns have waived or reduced fees for many forms of public transit. With many people working from home these days, public transportation usage is down, significantly helping to reduce your chances of exposure. Although overall it may not be the least-risky option for getting around, for senior drivers, it’s a viable alternative to driving on their own.
Health safety measures:
Public transit is a great resource for all ages of drivers or those needing a means of transportation. With fewer resources to fight the virus, many locales are stepping up, with government support and expanded public services, to help higher-risk citizens get through these trying times.
What is being done?:
Some local transit organizations are rallying around their community members, offering extended services to help those who have difficulty traveling. This includes critical services like home delivery for all sorts of necessities, such as groceries, meals and prescriptions.
Transit lines and other modes of public transportation have also been undergoing strenuous cleaning and sanitation procedures, with the New York subway even utilizing HVAC systems in each car.
You can also expect enhanced cleaning protocols for ride-sharing services. For example, Uber requires all of its drivers and passengers to wear masks and has instituted a “Leave at door” option for its deliveries as part of its Door-to-Door Safety Standard.
Additionally, the company has pledged 10 million free rides for those in need, including seniors and frontline healthcare workers.
What can I do?
The CDC provides extra guidance for those using public forms of transportation, who want to do what they can for the safety of themselves and others.
Back on the road:
During times like COVID or even flu season, your own car can be the safest place to be when you need to travel. That can be quite a transition for some seniors, who may have grown accustomed to a passenger role instead. However, here are some things you can do to make the transition a little easier.
Consider medical needs:
Don’t forget to plan for any special medical needs when you are leaving your home. Two of the more critical medical considerations to be mindful of are prescriptions and medical alert systems.
Prescription Medications: There are some medications that can impair your judgment and slow your responses, making it incredibly dangerous for you to drive. Some medicines can make you feel sleepy or sick. Others may have a delayed reaction time, with symptoms setting in well after you have taken the medication. Regardless of the specific side effects, it’s important to avoid driving under the influence of certain medications, so be sure to talk to your doctor about safe protocols before you begin driving while medicated.
Medical Alert: A medical alert system is an excellent way for seniors to ensure their safety on the road. GPS tracking ensures that your loved ones and emergency responders can find you in a pinch, with the added benefit of 24/7 support when and where you need it. Built-in features like fall detection, alarm beacons and custom emergency plans can all help you stay safe on the road. There are several models available, from bracelets and pins to dash-mounted options specifically made for your vehicle.
Check vision and hearing:
It’s also important to make sure that your vision and hearing tests are up to date. Your optometrist can help you confirm your eye prescription, so you have the right lenses to see clearly on the road. You may also consider special lenses to help deflect the blinding sunlight of a clear day or anti-reflective lenses to prevent glare from nighttime driving.
It is also recommended that seniors check their hearing to ensure that you have the proper hearing aids needed to make car horns and the other sounds of the road more easily identifiable when driving.
Add roadside assistance:
Much as we try to avoid them, we can’t prevent all natural hazards we might face on the road, so emergency road service is critical in the event of an incident. Roadside assistance typically offers 24/7 support for unexpected events such as a flat tire, requiring a jump-start or needing a tow.
Take a driver safety course:
Regardless of how old you are and how many years of experience you have behind the wheel, there is always room to brush up on your driving skills. A driver safety course is an easy way to hone safe driving habits and refresh your knowledge of the rules of the road. It could also save you significantly, lowering your car insurance rates from some of the nation’s best car insurance companies if you can leverage safe-driving discounts.
Plan for time:
It’s easy to feel rushed when you are running late for an appointment, but remember to slow down and take your time. The biggest mistakes happen when we are in a hurry, so be sure to follow the legal speed limit and drive with caution. It won’t be the end of the world if you are a few minutes late for your appointment, but it could be the end of your world if you sacrifice your safety with reckless or risky driving. If others are in a hurry on the road, that can affect your safety as well. Be sure to give plenty of room and stay in the right lane when possible, so faster drivers can get around you safely.
Car safety:
Car maintenance:
Basic vehicle maintenance is part of the cost of owning a car, which helps to ensure that your vehicle is running in top shape whenever you need to go somewhere. Be sure to keep your windshield clear of debris and make sure washer fluid levels are topped off so your view stays clear.
Other fluids to check include brake fluid, which keeps your brakes in good working order, and power steering fluid, which ensures you are not compromised in your ability to steer with ease. Your mechanic can check and refill these items for you as needed during a regular oil change.
Prepare for weather:
Depending on where you live, you may need to prepare for inclement weather. Snow and ice can present an increased risk of accidents on the road, especially during the holidays, while summer storms like hurricanes and tornadoes can compromise visibility.
If you live in an area with cold weather, be sure to prepare your vehicle with special seasonal accessories. This includes keeping such necessities as tire chains, an ice scraper, de-icing spray, jumper cables, road flares and a first-aid kit in your trunk. A winter maintenance check-up with your local mechanic can ensure that your vehicle is working properly, like your heater, defroster, radiator, belts, hoses, brakes and lights.
Sanitize:
Despite your best efforts, you may come into contact with infected surfaces while outside of the home. The best way to protect yourself is to regularly use hand sanitizer every time you enter your vehicle, using an EPA-approved disinfectant to wipe down your steering wheel, gear shift and control dials. Wearing gloves while pumping gas is an extra protective measure you can use to limit your exposure.
Mobility-friendly features:
There are several additions you can install or use in your vehicle to make it more accessible and comfortable for you when driving, such as special non-slip shoes. Extra handlebars or steps can make getting in and out of the vehicle much easier, while a swivel cushion and assist straps can also help improve mobility.
Wheelchair ramps and docking stations may also be covered by your car insurance for drivers with disabilities, although coverage will depend on your medical needs and insurance policy.
Mirrors and cameras:
Visibility is one of your biggest aids when driving, so windows, mirrors and cameras should always remain clear and unobstructed. Before you turn on your vehicle, check your mirrors to ensure proper placement, and adjust as needed for best visibility. If you experience many blind spots or otherwise have impaired vision in your vehicle, consider installing additional mirrors to eliminate blind spots and ensure that you can see clearly around you at all times.
Resources:
There are many resources available to help senior drivers before, during and after you get back on the road. Here are a few:
Type of Support:
[End of Article]
___________________________________________________________________________
About Bankrate (Wikipedia)
Bankrate is a personal finance company that guides people through pivotal steps of their financial journey. Bankrate's website provides accurate rate information, intuitive calculators and curated editorial content to help visitors reach their goals. The company was founded in 1976 and acquired by Red Ventures in November 2017.
History:
Bankrate was founded in 1976 by Robert K. Heady as a print publisher of the "Bank Rate Monitor."
In 1996, the company began moving its business online.
Today, Bankrate, Inc.'s online network includes Bankrate.com as well as the following:
The online network received over 150 million visits in 2010.
In January 2011, Bankrate completed the acquisition of Trouve Media. In December 2011, Bankrate completed the acquisition of substantially all of the assets of InsWeb Corporation for $65 million in cash.
In March 2012, Bankrate acquired InsuranceAgents.com.
After spending 10 years as a public company traded on the NASDAQ, Bankrate was acquired in 2009 by Apax Partners in a transaction valued at approximately $571 million.
In June 2011, Bankrate raised a total of $300 million in gross proceeds with a successful initial public offering on the New York Stock Exchange. In December 2011, Bankrate priced a secondary offering of 12.5 million shares at $17.50 per share.
In 2012, the company purchased The Points Guy, a site that publishes travel-oriented articles highlighting the credit cards it sells.
In 2014, Bankrate acquired Caring.com for $54 million.
Kenneth S. Esterow was appointed Bankrate's President and Chief Executive Officer in January 2014, having previously served as Senior Vice President – Chief Operating Officer from September 2013 to December 2013.
Bankrate was acquired by Red Ventures for $1.24 billion in November, 2017.
In January 2018, Bankrate expanded into the UK with an office, editorial, and commercial teams in London, along with a localized Bankrate UK website. The site is run by Sebastian Anthony, former editor of Ars Technica.
In September 2018, the former chief financial officer Edward J. DiMaria was found guilty of committing accounting and securities fraud which led to over $25 million in shareholder losses. DiMaria was sentenced to 10 years in prison, and ordered to pay $21,234,214 in restitution.
Former vice president of finance Hyunjin Lerner also pleaded guilty for his role in the conspiracy and was sentenced to 5 years in prison.
Products and Services:
Since the beginning, Bankrate has provided information about interest rates. Beginning in 2004, Bankrate also began offering financial education content, insurance quotes, and credit card offers.
One of Bankrate's reports in 2014 determined the costs of car ownership in each state, taking into account the costs of gas and insurance, among other factors. The data suggested that Wyoming is the most expensive state in the nation to own a car.
Honors:
The National Association of Real Estate Editors in 2014 named Bankrate's Mortgage blog the winner of its Best Blog and Best Column awards.
In October 2012, Advertising Age ranked Bankrate as the fifth fastest-growing media company.
Bankrate's "Financial Regulation, One Year Later" package earned a 2012 "Best in Business" award from the Society of American Business Editors and Writers (SABEW).
Bankrate won two SABEW Awards in 2011: Holden Lewis' mortgage blog and Bankrate's explanatory series on financial reform were honored.
Bankrate writers have won awards from the Society of Professional Journalists several times, most recently in 2007 for their coverage of the Federal Reserve Open Market Committee's rate cut.
In 2008, Forbes named Bankrate #41 in its list of America's 200 Best Small Companies. Forbes previously had honored the website in its "Best of the Web" series five times between 1999 and 2004.
See also:
By Lena Borrelli
Lena Borrelli's Twitter profile
Travel is complicated, even without a global pandemic. For seniors and other high-risk individuals, it can be even more intimidating when you’re dependent on public transportation that presents increased exposure to germs or disease. Planes, buses, taxis and even ride-sharing companies can pose a threat, with COVID-19 potentially floating in the air or living for hours — or even days — on surfaces.
Still, being out and about is sometimes necessary, regardless of your age. There are groceries to be purchased, essential supplies to stock up on and errands or activities to run, such as doctor’s appointments, family visits or religious services. With CDC guidelines urging Americans only to venture out when absolutely mandatory, there has been a marked decline in public transportation use since the beginning of the COVID-19 pandemic, and in particular, seniors are looking for safer ways to travel.
Many seniors have opted to get back behind the wheel, with their personal vehicle serving as a safer means for travel overall. If you are preparing to hit the road during a pandemic, theseare some things to consider for the sake of everyone’s safety.
The impact on seniors:
For seniors, it may have been a while since you were behind the wheel. Family and friends may have enabled or encouraged you to join a community carpool, or perhaps local shuttles gave you a ride to your favorite spots. The arrival and impact of COVID-19 has forced many seniors to consider these alternative forms of transportation — especially if they are unable or unwilling to drive themselves.
Senior transportation:
Shuttles:
Some organizations, like your local medical center or place of worship, may offer you a free ride. When scheduling appointments or making plans, inquire with the venue to see if there are any complimentary or paid shuttles that you can utilize for your visit.
Rideshare for seniors:
Ridesharing is growing in popularity with seniors because it provides an additional outlet for living a more independent life. Instead of dealing with public transit, seniors can use their mobile phone to schedule a private ride through popular companies like Uber and Lyft.
How to book Uber without a smartphone: If you don’t have a cell phone or prefer to use a different device, you can still use Uber. You can use your laptop or desktop computer to book a ride by way of the Uber website.
Family:
If you have family who lives locally and is in good health, consider asking them for a ride. They may need to run many of the same errands you do, creating the perfect opportunity to safely enjoy one another’s company while you check off your to-do list.
Public Transportation:
To help residents get where they need to go, many cities and towns have waived or reduced fees for many forms of public transit. With many people working from home these days, public transportation usage is down, significantly helping to reduce your chances of exposure. Although overall it may not be the least-risky option for getting around, for senior drivers, it’s a viable alternative to driving on their own.
Health safety measures:
Public transit is a great resource for all ages of drivers or those needing a means of transportation. With fewer resources to fight the virus, many locales are stepping up, with government support and expanded public services, to help higher-risk citizens get through these trying times.
What is being done?:
Some local transit organizations are rallying around their community members, offering extended services to help those who have difficulty traveling. This includes critical services like home delivery for all sorts of necessities, such as groceries, meals and prescriptions.
Transit lines and other modes of public transportation have also been undergoing strenuous cleaning and sanitation procedures, with the New York subway even utilizing HVAC systems in each car.
You can also expect enhanced cleaning protocols for ride-sharing services. For example, Uber requires all of its drivers and passengers to wear masks and has instituted a “Leave at door” option for its deliveries as part of its Door-to-Door Safety Standard.
Additionally, the company has pledged 10 million free rides for those in need, including seniors and frontline healthcare workers.
What can I do?
The CDC provides extra guidance for those using public forms of transportation, who want to do what they can for the safety of themselves and others.
- Always use a mask and wear gloves if you expect to touch any surfaces during your outing.
- Avoid unmasked drivers and passengers.
- Use social distancing when in public, always allowing for a distance of six feet between you and others. Allow for as much of a distance as possible between you and the driver, as well as other passengers.
- Refrain from touching surfaces that could spread bacteria or germs, such as door frames, windows, subway poles and pay terminals.
- If you must touch surfaces, use an EPA-approved hand sanitizer or disinfectant afterward, to kill germs that may have transferred to your person.
- Avoid contact through touchless payments, instead using your own phone to schedule rides or adjust orders.
- Improve ventilation wherever possible, either by opening windows or requesting that the driver put the air on a non-recirculation mode.
- If you are not feeling well, stay home. Even if you do not have COVID-19, an immune system weakened by illness of any kind can make you more susceptible to contracting other viruses or infections.
Back on the road:
During times like COVID or even flu season, your own car can be the safest place to be when you need to travel. That can be quite a transition for some seniors, who may have grown accustomed to a passenger role instead. However, here are some things you can do to make the transition a little easier.
Consider medical needs:
Don’t forget to plan for any special medical needs when you are leaving your home. Two of the more critical medical considerations to be mindful of are prescriptions and medical alert systems.
Prescription Medications: There are some medications that can impair your judgment and slow your responses, making it incredibly dangerous for you to drive. Some medicines can make you feel sleepy or sick. Others may have a delayed reaction time, with symptoms setting in well after you have taken the medication. Regardless of the specific side effects, it’s important to avoid driving under the influence of certain medications, so be sure to talk to your doctor about safe protocols before you begin driving while medicated.
Medical Alert: A medical alert system is an excellent way for seniors to ensure their safety on the road. GPS tracking ensures that your loved ones and emergency responders can find you in a pinch, with the added benefit of 24/7 support when and where you need it. Built-in features like fall detection, alarm beacons and custom emergency plans can all help you stay safe on the road. There are several models available, from bracelets and pins to dash-mounted options specifically made for your vehicle.
Check vision and hearing:
It’s also important to make sure that your vision and hearing tests are up to date. Your optometrist can help you confirm your eye prescription, so you have the right lenses to see clearly on the road. You may also consider special lenses to help deflect the blinding sunlight of a clear day or anti-reflective lenses to prevent glare from nighttime driving.
It is also recommended that seniors check their hearing to ensure that you have the proper hearing aids needed to make car horns and the other sounds of the road more easily identifiable when driving.
Add roadside assistance:
Much as we try to avoid them, we can’t prevent all natural hazards we might face on the road, so emergency road service is critical in the event of an incident. Roadside assistance typically offers 24/7 support for unexpected events such as a flat tire, requiring a jump-start or needing a tow.
Take a driver safety course:
Regardless of how old you are and how many years of experience you have behind the wheel, there is always room to brush up on your driving skills. A driver safety course is an easy way to hone safe driving habits and refresh your knowledge of the rules of the road. It could also save you significantly, lowering your car insurance rates from some of the nation’s best car insurance companies if you can leverage safe-driving discounts.
Plan for time:
It’s easy to feel rushed when you are running late for an appointment, but remember to slow down and take your time. The biggest mistakes happen when we are in a hurry, so be sure to follow the legal speed limit and drive with caution. It won’t be the end of the world if you are a few minutes late for your appointment, but it could be the end of your world if you sacrifice your safety with reckless or risky driving. If others are in a hurry on the road, that can affect your safety as well. Be sure to give plenty of room and stay in the right lane when possible, so faster drivers can get around you safely.
Car safety:
Car maintenance:
Basic vehicle maintenance is part of the cost of owning a car, which helps to ensure that your vehicle is running in top shape whenever you need to go somewhere. Be sure to keep your windshield clear of debris and make sure washer fluid levels are topped off so your view stays clear.
Other fluids to check include brake fluid, which keeps your brakes in good working order, and power steering fluid, which ensures you are not compromised in your ability to steer with ease. Your mechanic can check and refill these items for you as needed during a regular oil change.
Prepare for weather:
Depending on where you live, you may need to prepare for inclement weather. Snow and ice can present an increased risk of accidents on the road, especially during the holidays, while summer storms like hurricanes and tornadoes can compromise visibility.
If you live in an area with cold weather, be sure to prepare your vehicle with special seasonal accessories. This includes keeping such necessities as tire chains, an ice scraper, de-icing spray, jumper cables, road flares and a first-aid kit in your trunk. A winter maintenance check-up with your local mechanic can ensure that your vehicle is working properly, like your heater, defroster, radiator, belts, hoses, brakes and lights.
Sanitize:
Despite your best efforts, you may come into contact with infected surfaces while outside of the home. The best way to protect yourself is to regularly use hand sanitizer every time you enter your vehicle, using an EPA-approved disinfectant to wipe down your steering wheel, gear shift and control dials. Wearing gloves while pumping gas is an extra protective measure you can use to limit your exposure.
Mobility-friendly features:
There are several additions you can install or use in your vehicle to make it more accessible and comfortable for you when driving, such as special non-slip shoes. Extra handlebars or steps can make getting in and out of the vehicle much easier, while a swivel cushion and assist straps can also help improve mobility.
Wheelchair ramps and docking stations may also be covered by your car insurance for drivers with disabilities, although coverage will depend on your medical needs and insurance policy.
Mirrors and cameras:
Visibility is one of your biggest aids when driving, so windows, mirrors and cameras should always remain clear and unobstructed. Before you turn on your vehicle, check your mirrors to ensure proper placement, and adjust as needed for best visibility. If you experience many blind spots or otherwise have impaired vision in your vehicle, consider installing additional mirrors to eliminate blind spots and ensure that you can see clearly around you at all times.
Resources:
There are many resources available to help senior drivers before, during and after you get back on the road. Here are a few:
Type of Support:
- Winter driving:
- AAA Winter Driving Tips from America’s leading automotive and driver support service.
- The National Safety Council educates drivers on the best safety tips for driving during winter and other inclement weather.
- Driver safety courses for seniors:
- AAA Senior Driving can help with driver improvement courses for seniors through its Roadwise Driver program.
- The American Association of Retired Persons (AARP) offers valuable information regarding safe driving practices, in addition to classroom and online driver safety courses.
- State driving laws for seniors:
- National Council on Aging (NCOA), a non-profit dedicated to supporting seniors in all aspects of their lives, including time spent on the road.
- The U.S. Administration on Aging offers its Eldercare Locator to help seniors find free or discounted transportation services.
- Car modification/add-ons for seniors:
- The U.S. Department of Transportation’s National Highway Traffic Safety Administration can help you find the right resources and equipment to adapt your vehicle to meet your needs.
- The Association for Driver Rehabilitation Specialists can help pair you with everything you need to modify your vehicle.
- Rideshare services for seniors:
- HopSkipDrive, an organization that helps seniors find rides for errands and receiving Meals on Wheels deliveries.
- GoGoGrandparent works as a concierge service to connect seniors with a ride within minutes, with a network of participating services including Lyft and Uber.
- Apps/assistive accessories for senior driver safety:
- The National Aging and Disability Transportation Center (NADTC) provides active transportation support and resources.
- iTNAmerica is a national network that pairs seniors with door-through-door transportation.
[End of Article]
___________________________________________________________________________
About Bankrate (Wikipedia)
Bankrate is a personal finance company that guides people through pivotal steps of their financial journey. Bankrate's website provides accurate rate information, intuitive calculators and curated editorial content to help visitors reach their goals. The company was founded in 1976 and acquired by Red Ventures in November 2017.
History:
Bankrate was founded in 1976 by Robert K. Heady as a print publisher of the "Bank Rate Monitor."
In 1996, the company began moving its business online.
Today, Bankrate, Inc.'s online network includes Bankrate.com as well as the following:
- CreditCards.com,
- Caring.com,
- Interest.com,
- Bankaholic.com,
- Mortgage-calc.com,
- CreditCardGuide.com,
- ThePointsGuy.com,
- Bankrate.com.cn,
- CreditCards.ca,
- NetQuote.com,
- CD.com,
- Walla.by
- and Quizzle.
The online network received over 150 million visits in 2010.
In January 2011, Bankrate completed the acquisition of Trouve Media. In December 2011, Bankrate completed the acquisition of substantially all of the assets of InsWeb Corporation for $65 million in cash.
In March 2012, Bankrate acquired InsuranceAgents.com.
After spending 10 years as a public company traded on the NASDAQ, Bankrate was acquired in 2009 by Apax Partners in a transaction valued at approximately $571 million.
In June 2011, Bankrate raised a total of $300 million in gross proceeds with a successful initial public offering on the New York Stock Exchange. In December 2011, Bankrate priced a secondary offering of 12.5 million shares at $17.50 per share.
In 2012, the company purchased The Points Guy, a site that publishes travel-oriented articles highlighting the credit cards it sells.
In 2014, Bankrate acquired Caring.com for $54 million.
Kenneth S. Esterow was appointed Bankrate's President and Chief Executive Officer in January 2014, having previously served as Senior Vice President – Chief Operating Officer from September 2013 to December 2013.
Bankrate was acquired by Red Ventures for $1.24 billion in November, 2017.
In January 2018, Bankrate expanded into the UK with an office, editorial, and commercial teams in London, along with a localized Bankrate UK website. The site is run by Sebastian Anthony, former editor of Ars Technica.
In September 2018, the former chief financial officer Edward J. DiMaria was found guilty of committing accounting and securities fraud which led to over $25 million in shareholder losses. DiMaria was sentenced to 10 years in prison, and ordered to pay $21,234,214 in restitution.
Former vice president of finance Hyunjin Lerner also pleaded guilty for his role in the conspiracy and was sentenced to 5 years in prison.
Products and Services:
Since the beginning, Bankrate has provided information about interest rates. Beginning in 2004, Bankrate also began offering financial education content, insurance quotes, and credit card offers.
One of Bankrate's reports in 2014 determined the costs of car ownership in each state, taking into account the costs of gas and insurance, among other factors. The data suggested that Wyoming is the most expensive state in the nation to own a car.
Honors:
The National Association of Real Estate Editors in 2014 named Bankrate's Mortgage blog the winner of its Best Blog and Best Column awards.
In October 2012, Advertising Age ranked Bankrate as the fifth fastest-growing media company.
Bankrate's "Financial Regulation, One Year Later" package earned a 2012 "Best in Business" award from the Society of American Business Editors and Writers (SABEW).
Bankrate won two SABEW Awards in 2011: Holden Lewis' mortgage blog and Bankrate's explanatory series on financial reform were honored.
Bankrate writers have won awards from the Society of Professional Journalists several times, most recently in 2007 for their coverage of the Federal Reserve Open Market Committee's rate cut.
In 2008, Forbes named Bankrate #41 in its list of America's 200 Best Small Companies. Forbes previously had honored the website in its "Best of the Web" series five times between 1999 and 2004.
See also:
Aging in the American Workforce
- YouTube Video: The Future of Employment - The Impact of AI and Automation on Jobs - with Oxford Professor Carl Frey
- YouTube Video: Preparing for Employment: Tips for Beginners
- YouTube Video: How to Survive Change at Work
In recent decades, the fertility rate of the United States has declined, prompting projections of an aging population and workforce, as is already happening elsewhere in the developed world and some developing countries.
Nevertheless, the rate of aging in the United States remains slower than that seen in many other countries, including some developing ones, giving the nation a significant competitive advantage. Still, it remains unclear how population aging would affect the United States.
History
The birth rate in the United States has declined steadily since the beginning of the 19th century, when the average person had as many as seven children.
In a 1905 speech, President Theodore Roosevelt criticized Americans for having fewer children, and described the declining birth rate as a "race suicide" among Americans, quoting eugenicist Edward Alsworth Ross. In the 1930s, the Great Depression caused a substantial decrease in the birth rate, but this trend was reversed in the subsequent Baby Boomer generation.
While U.S. fertility rates were roughly at replacement level during the 1990s and early 2000s, contrary to expectations, they never rebounded after the 2007-2009 Great Recession even though the U.S. economy had recovered.
During the second half of the 2010s, the rate of growth of the U.S. population was in steady decline. More recently, the COVID-19 pandemic caused fertility to decline further, a "bump" in 2021 notwithstanding, while also increasing the death rate in the country.
At the same time, many women are choosing delay childbearing or are choosing a childless life altogether. Millennials are the most reluctant generation in history when it comes to reproduction. Between 1990 and 2015, the number of married couples aged 18 to 34 with children dropped from 37% to 25%.
The number of American women who do not have children by the age of 30 has grown, breaking previous fertility trends where younger women made up the bulk of births. While only 10% of women were childless in 1976 at the end of their reproductive years, it is projected that 25% of those born in 1992 will reach the same benchmark in 2032.
Longitudinal analysis suggests that American women are not merely postponing having children but are increasingly avoiding it altogether. However, among Millennial women who have given birth, the average fertility rate is about 2.02 children per woman.
Regardless, U.S. birth rates have been on the decline across virtually all age groups, socioeconomic classes, and races since the late 2000s. This trend could cause the general population of the country to age significantly in the future. The oldest Baby Boomers, a large demographic cohort, had started to reach retirement age in the 2010s. By the early 2020s, about one in six Americans are 65 or older.
In 2021, the median age of the United States is 38.8, up from 37.2 in 2010. An increase in median age is seen among all ethnic groups, though European Americans are currently the oldest by that measure, followed by African Americans and Asian Americans (including Amerindians and Native Alaskans).
In the modern world, it has become common for developed countries to fall below the replacement level of births or see population decline. Many of these countries have tried to launch government initiatives to combat this trend, including large cash incentives for having more children, but these programs have been largely ineffective.
Nevertheless, American women tend to have their first children at an earlier age and end up having more children than their counterparts from other developed countries even though the U.S. does not have social welfare programs that are as generous as other rich nations.
Given current (2020) demographic trends, it is projected that the U.S. population would grow slightly by 2100, while other countries, including China and India, will shrink.
Causes
Population aging and falling birth rates in the US is driven by a variety of factors, including increased access to birth control, growing awareness of the realities of parenthood (especially motherhood), and changing societal attitudes toward reproduction, resulting in lower fertility among modern Americans.
The number of unintentional pregnancies has plummeted. Compared to a peak of 96.3 births per 1000 females aged 15 to 19 in 1957, when people married and had children early, the adolescent birth rate fell to 17.3 in 2018. (Black and Hispanic teenagers had the largest decline, though they were still above whites and Asians.)
Twenty-first-century American youths are more likely to have access to effective and long-acting methods of contraception, such as an intrauterine device (IUD), and to be more cautious about sexual intercourse than their predecessors.
While economic troubles and climate anxiety are commonly cited reasons, data suggest they are not the primary factors behind falling fertility in the U.S. Rather, it is due to changing attitudes; today's young people, especially women, tend to prioritize and expect more from their careers and are less interested in having children.
According to the Pew Research Center, the number of non-parents aged 18 to 49 who do not expect to have any children has grown. Among them, a lack of interest in children, medical issues, and financial problems were the top reasons for their predictions.
As parenthood continues to lose its appeal, more and more Americans prefer their own careers, leisure time, savings, and personal freedom to having children and fewer consider children to be a source of happiness or fulfillment.
Among those with children, some have chosen not to have more either because they do not want them, because they would like to spend more time with the ones they already have, or because could not afford more children.
In fact, many admit that their financial circumstances would improve once their children leave the house and that they would be better off not having children. Among those having fewer children than they would like, concerns over the state of the economy and personal financial security are common and many believe the cost of raising a child is too high.
More and more women are realizing that having children is an option they can ignore in favor of economic or educational opportunities; some worry that a woman's career might stall if she chooses to have children.
The number of American women earning university degrees has grown relative to men's since the late 2000s, coinciding with the long-term decline in birth rates. Globally, gender equality is associated with lower fertility.
In the early 2020s, as many as one in five American adults do not want to have children, with some reporting they had made their decision early on. It remains unclear whether they would change their minds.
Data dating back to the 1980s show that this is part of a long-term trend, possibly starting with the Baby Boomers, who were the first cohort to begin questioning social norms on family formation. Furthermore, dedication to work and modern expectations of parents have increased the opportunity cost of having a child.
Because of the aforementioned reasons, the birth rates of women of all age groups (except those in their forties), races, and educational levels have fallen. The number of European Americans has been shrinking since 2016 while the rates of growth of people of other races have fallen as well, except for those of mixed heritage.
Overall, the fall of the European-American and youth populations is the biggest factor behind the aging of the United States. But this trend is moderated by the growth of non-white ethnic groups.
Another major cause of population aging in the United States is the fact that the Baby Boomers, a large cohort, are getting older, adding a large group of older Americans to the population and causing the median age to move up. In addition, employment rates among older workers are increasing. The rate of people who continue working after they are 65 is relatively high in the US, when compared to other developed countries.
For example, in 2011, 16.7% among people aged 65 and over and 29.9% among 65–69 were employed in the US.
Impacts:
By 2030, 20% of Americans are projected to be 65 and older. Both the overall population of the country and the average age are projected to increase over coming years. Given that older people tend to need more health services, some demographers have theorized a significant impact on the country resulting from these trends. Population aging could create an increasing need for services such as nursing homes and care-giving.
Economy:
A shortage of workers is expected in the U.S. workforce due to a declining labor participation rate. Projections show that the demand for labor needed now is not being fulfilled, and the gap between labor needed and labor available will continue to expand over the future.
Owing to the relatively large size population size of those born between the end of WWII and the mid-1960s (referred to by some as the "Baby Boomers"), the number of people generally considered to be of working age is declining.
Additionally, young people are spending more time in education and training and are entering the workforce at a later age, and therefore, there are fewer entering the workforce in their early twenties.
A loss in skilled and capable workers has made it harder for employers to recruit new staff. The retirement of members of the aging workforce could possibly result in the shortage of skilled labor in the future. A majority of experienced utility workers and hospital caregivers, for example, will be eligible for retirement.
By the late 2010s, the United States found itself facing a shortage of tradespeople, a problem that persisted in the early 2020s despite the COVID-19 pandemic-induced recession and prospective employers offering higher salaries and paid training. Having an aging population accelerates industrial automation.
Experts expect the labor crunch of the early 2020s will continue for years to come, due to not just the Great Resignation, but also the aging of the U.S. population, the decline of the labor participation rate, and falling rates of legal immigration.
From a demographic point of view, the labor shortage in the United States during the 2020s is inevitable due to the sheer size of the baby boomers. As the oldest economically active cohort, the baby boomers comprised about a quarter of the U.S. workforce in 2018.
Though they were projected by economists to begin retiring in the 2010s, 29% of older (65–72 years of age) baby boomers in the United States remained active in the labor force in 2018, a large portion compared to older cohorts at the same age. In fact, the official age of retirement in the United States had already been raised, and Baby boomers were incentivized to postpone retirement in part because it allowed them to claim more Social Security benefits once they finally retired.
Furthermore, large numbers would like semi-retirement arrangements or flexible work schedules. The COVID-19 pandemic may have sped up the retirement of some baby boomers. The Pew Research Center reported that the number of baby boomers in retirement had increased by 3.2 million in 2020, the largest annual increase in the previous decade.
But even before the pandemic, the United States had a gap between the number of job openings and the number of unemployed people. Like most other members of the Organization for Economic Cooperation and Development (OECD), the U.S. has seen its productivity growth falter and its debt as a share of GDP grow due to demographic trends.
A shrinking birth rate could exacerbate economic inequality by increasing the importance of family inheritance, while an overall decrease in the population could shrink the economy by reducing the demand for basic goods like groceries and real estate. On the other hand, having fewer or no children has enabled women to pursue more opportunities outside the home.
In fact, places with the highest job growths in the 2010s saw the biggest drops in fertility. For women in such places, the opportunity cost of having a child was higher.. Moreover, people without children do not need to save money to pass on to their children and as such can afford to work fewer hours per week and retire early.
Nevertheless, unlike their counterparts in many other countries East and West, American Baby Boomers had many children of their own, the Millennials, who are a large cohort relative to the nation's population and are themselves having a relatively high birth rate, as of the 2010s.
Millennials and Generation Z have been responsible for a surge in labor participation in the U.S. as the same time as the contraction of the workforce of major economies. Indeed, the U.S. workforce is projected to grow by 10% by 2040.
Having a relatively young, diligent, and productive workforce means that the United States will continue to have a significant number of consumers, investors and taxpayers in the upcoming decades. This gives the nation an economic edge over others.
However, an aging population means that the U.S. economy will be less dynamic, innovative, and productive than it was in the past. Moreover, depending on the household, many women could be forced to give up working in order to take care of their family members, exacerbating the labor shortage.
Education:
See also: Higher education bubble in the United States
By the early 2020s, enrollment in K-12 public schools has fallen, partly due to the switch to private schools and home schooling, but also due to a smaller number of school-aged children (5-17).
In the 1970s, American colleges and universities saw a dramatic increase in enrollments due to the post-war baby boom and the growth of women in higher education and the work force.
By the 1980s and 1990s, although the baby boom had long ended, institutions continued to enjoy good fortune due to growing demand. But this all changed in the aftermath of the Great Recession, which saw significant cuts in funding for education and falling birth rates.
Due to declining birth rates, the number of American high-school graduates is expected to drop after 2025, putting more pressure on institutions of higher learning at a time when many have already been permanently shut down.
Many private colleges will not make it while public ones will struggle to convince state and local governments to keep funding them. Demand for education from the nation's top 100 colleges and universities, however, is likely to remain high, in part because of rising numbers of Indian and Chinese Americans, for whom higher education is of utmost importance.
To survive, non-elite institutions will have to cut back or eliminate courses in the liberal arts and humanities, like gender studies, and expand those in emerging fields, such as artificial intelligence, and professional programs, such as law enforcement.
In addition, Americans who work in higher education are older on average than the average American worker. In the future, this sector of the economy will need to find ways to retain staff or to encourage retirees to come back (part-time).
There is some research supporting the idea that in well-educated countries, it might actually benefit the population to have a birth rate below replacement levels because people at different ages do not make the same level of economic contributions on average.
Environment:
Some demographers have suggested that a declining birth rate may have net positive effects on the country. Many environmentalists see this trend more optimistically because it could help combat the perceived problem of overpopulation.
The world population is expected to reach almost 10 billion by the year 2050, which could pose a burden to Earth's natural resources. Having fewer children has been shown to be an effective way to reduce environmental impact through reduced carbon footprint and higher populations could increase the effects of climate change in the future.
Having an expanding population of people who live longer and are wealthier may not be sustainable. Though the details remain debated, in the 2020s, growing numbers of couples have cited climate change as a reason for having fewer or not having children at all.
Geopolitics:
See also: Cold War II and Pax Americana
Many of America's allies—Canada, the United Kingdom, the European Union, Japan, South Korea, Australia, and New Zealand—are themselves aging. For that reason, they would struggle to finance their own defense and would become even more dependent on the United States at a time when U.S. demographic advantage is fading.
Indeed, while the U.S. maintained a fertility advantage over other developed nations during the 1990s and 2000s, this edge faded away during the 2010s. To combat this problem, the U.S. needs to improve ties with emerging economies, such as the Philippines, Indonesia, and India, though some of these countries are already in the process of transitioning towards an aging society. Furthermore, an aging population will reduce the ability of the United States to participate in global affairs the way it once did.
Nevertheless, because the United States is aging more slowly than any one of its main rivals, it will have an advantage in any future geopolitical contests. Given current demographic trends, it is unlikely that the United States will lose its dominant position to China and Russia.
China has a low fertility rate compared to the United States. China's number of people over 65 as a share of the population is predicted to exceed that of the United States by around 2035. Furthermore, the United States has an advantage that China lacks—immigration.
While the U.S. remains an attractive place for immigrants, very few would like to move to China. In fact, projections of China's economic growth from the early 2020s taking into account China's population aging, among other problems facing the nation, tend to delay the date at which China's economy will surpass America's.
Even if China were to overtake the United States, the latter would soon reclaim its position. On one hand, China's demographic decline relative to the U.S. could prompt it to undertake more risky actions, for example with regards to the issue of Taiwanese independence.
On the other hand, continued U.S. superiority might deter adversaries from taking military actions against either the U.S. or its allies. A "geriatric peace" might be at hand, as the graying powers have an incentive to cooperate in order to maintain the global order before their demographic realities prevent them from doing so.
Occupational safety:
Because of the many older adults opting to remain in the U.S. workforce, many studies have been done to investigate whether the older workers are at greater risk of occupational injury than their younger counterparts. Due to the physical declines associated with aging, older adults tend to exhibit losses in eyesight, hearing and physical strength.
Data shows that older adults have low overall injury rates compared to all age groups, but are more likely to suffer from fatal and more severe occupational injuries. Of all fatal occupational injuries in 2005, older workers accounted for 26.4%, despite only comprising 16.4% of the workforce at the time.
Age increases in fatality rates in occupational injury are more pronounced for workers over the age of 65. The return to work for older workers is also extended; older workers experience a greater median number of lost work days and longer recovery times than younger workers.
Some common occupational injuries and illnesses for older workers include arthritis and fractures. Among older workers, hip fractures are a large concern, given the severity of these injuries.
Social welfare and healthcare:
The U.S. federal social security system functions through collecting payroll taxes to support older citizens. It is possible that a smaller workforce, coupled with increased numbers of longer-living elderly, may have a negative impact on the social security system.
The Social Security Administration (SSA) estimates that the dependency ratio (people ages 65+ divided by people ages 20–64) in 2080 will be over 40%, compared to the 20% in 2005.
SSA data shows one out of every four 65-year-olds today will live past the age of 90, while one out of 10 will live past 95. Indeed, 60% of baby boomers are more worried about outliving their savings than dying. Rising life expectancy may result in reductions in social security benefits, devaluing private and public pension programs.
Were there to be a reduction or elimination of programs such as social security and Medicare, many may need delay retirement and to continue working. In 2018, 29% of Americans aged 65–72 remained active in the labor force, according to the Pew Research Center, as Americans generally expect to continue to work after turning 65.
The baby boomers who chose to remain in the work force after the age of 65 tended to be university graduates, whites, and urban residents. That the boomers maintained a relatively high labor participation rate made economic sense because the longer they postpone retirement, the more Social Security benefits they could claim, once they finally retire.
By 2030, 20% of Americans are predicted to be past the age of retirement, which could pose a burden to the healthcare system. Older and retired people tend to need more health services, which must be provided by their younger counterparts, so some demographers have theorized that this could have a negative impact on the country.
Arthritis, cancer, diabetes, obesity, and cognitive issues are among the most common issues faced by Americans over the age of 65. Older adults who have worked in the construction industry have shown high rates of chronic diseases. Experts suggest that the number of geriatricians will have to triple to meet the demands of the rising elderly.
Demand for other healthcare professionals, such as nurses, occupational therapists, physical therapists and dentists is also projected to rise, as well as for common geriatric healthcare needs, such as medications, joint replacements and cardiovascular operations. Between 1966 and 2023, the number of people qualified for Medicare tripled to nearly 65 million, with 10 million seniors and disabled people being added to the system from 2013 to 2023.
In the early 2020s, among Americans aged 65 or older, 14% of all expenditures goes to healthcare, compared to 8% for the general population. While some enjoy living by themselves, others suffer from physical or mental health issues being socially isolated.
Between the late 2010s and early 2020s, Millennials and Generation Z join the workforce in large numbers, allowing the U.S. to maintain a relatively large tax base, alleviating concerns over the financial sustainability of various social welfare programs.
Nevertheless, in 2023, both Medicare and Social Security as they stand are projected to run out of funds by the late 2020s and mid-2030s, respectively. With the Inflation Reduction Act of 2022, the Joe Biden administration sought to curb the cost of medical care by allowing Medicare to negotiate lower costs for certain drugs and treatments, such as insulin.
Society:
Population aging can potentially change American society as a whole. Many companies use a system, in which older, tenured workers get raises and benefits over time, eventually hitting retirement.
With larger numbers of older workers in the workforce, this model might be unsustainable. In addition, perceptions of older adults in society will change, as the elderly are living longer lives and more active than before.
Changing from a youth-focused culture to having a more positive attitude towards aging and being more respectful of seniors like Japan can help elderly Americans extend their life span and live out their sunset years in dignity. American society will have to confront the negative stereotypes of aging and ageism.
Proposed solutions:
A number of solutions have been proposed to address the problems caused by an aging population. Investing in technological and human-capital development in order to enhance productivity might help the United States offset some of the economic effects of population aging.
Raising the retirement age, further automation, and encouraging higher labor participation rates among women could help alleviate the labor shortage, with the latter successfully done in Japan in the 2010s. Cities could render themselves friendlier towards the elderly, for example by improving public transit.
To deal with the increased demand that could be placed on the healthcare system, telehealth and virtual health monitoring has arisen as a way to help support a larger population of older adults.
The Congressional Budget Office (CBO) has proposed 60 different policy options on how to save billions of dollars on Medicare, such as raising monthly premiums. As of 2023, members of Congress are considering various options to salvage Medicare and Social Security, such as addressing fraud in the Medicare Advantage program and raising the ages of legibility for Medicare and Social Security.
Alternatively, some people have advocated for offering more paid parental leave and child care, thereby encouraging people to have more children. These policies have already been employed in other areas of the world, but with limited results at best.
In some countries such as Germany and Czech Republic they successfully raised the birth rate, but not enough to reach replacement level and at a significant cost.
On the other hand, such policies failed in Finland, Singapore, Taiwan, Japan, and South Korea. It is unlikely that similarly pro-natalist policies would work in the U.S., which maintains a relative high fertility rate despite not having social welfare programs that are as generous as some other developed countries.
Some have argued that reduced immigration will have a larger impact on population growth than the declining birth rate. Immigration has historically been a source of growth for the US, and some have suggested that it could slow or reverse the trend of population aging or decline.
However, studies have shown that immigrants from countries with high-fertility rates often have fewer children when they immigrate to a country where small families are the norm, and this patterns also holds in the U.S. It has also been shown that low-birth rates and sudden increases in immigration often lead to increased levels of populism and xenophobia.
Arguments in favor of increasing immigration to combat declining population levels have sparked outcry from some right-wing political factions in the United States and some European countries.
In the United States, past episodes of domestic turmoil have led to moratoriums on immigration. Furthermore, critics argue that the United States today struggles to integrate the various different ethnic groups already living in the country alongside new immigrants.
Political scientist Robert Putnam argues that ethnic and cultural diversity has its downsides in the form of declining cultural capital, falling civic participation, lower general social trust, and greater social fragmentation.
Since 1996, there have been numerous failed attempts to introduce comprehensive immigration reforms, and while many continue to view immigration as a net benefit to the nation, the American people remain mixed on whether or not they support more immigration in general.
Mass migration is politically problematic. Still, high-skilled immigration, the type of immigration that tends to expand the tax base the most, as has been done in Canada, can help.
See also:
Nevertheless, the rate of aging in the United States remains slower than that seen in many other countries, including some developing ones, giving the nation a significant competitive advantage. Still, it remains unclear how population aging would affect the United States.
History
The birth rate in the United States has declined steadily since the beginning of the 19th century, when the average person had as many as seven children.
In a 1905 speech, President Theodore Roosevelt criticized Americans for having fewer children, and described the declining birth rate as a "race suicide" among Americans, quoting eugenicist Edward Alsworth Ross. In the 1930s, the Great Depression caused a substantial decrease in the birth rate, but this trend was reversed in the subsequent Baby Boomer generation.
While U.S. fertility rates were roughly at replacement level during the 1990s and early 2000s, contrary to expectations, they never rebounded after the 2007-2009 Great Recession even though the U.S. economy had recovered.
During the second half of the 2010s, the rate of growth of the U.S. population was in steady decline. More recently, the COVID-19 pandemic caused fertility to decline further, a "bump" in 2021 notwithstanding, while also increasing the death rate in the country.
At the same time, many women are choosing delay childbearing or are choosing a childless life altogether. Millennials are the most reluctant generation in history when it comes to reproduction. Between 1990 and 2015, the number of married couples aged 18 to 34 with children dropped from 37% to 25%.
The number of American women who do not have children by the age of 30 has grown, breaking previous fertility trends where younger women made up the bulk of births. While only 10% of women were childless in 1976 at the end of their reproductive years, it is projected that 25% of those born in 1992 will reach the same benchmark in 2032.
Longitudinal analysis suggests that American women are not merely postponing having children but are increasingly avoiding it altogether. However, among Millennial women who have given birth, the average fertility rate is about 2.02 children per woman.
Regardless, U.S. birth rates have been on the decline across virtually all age groups, socioeconomic classes, and races since the late 2000s. This trend could cause the general population of the country to age significantly in the future. The oldest Baby Boomers, a large demographic cohort, had started to reach retirement age in the 2010s. By the early 2020s, about one in six Americans are 65 or older.
In 2021, the median age of the United States is 38.8, up from 37.2 in 2010. An increase in median age is seen among all ethnic groups, though European Americans are currently the oldest by that measure, followed by African Americans and Asian Americans (including Amerindians and Native Alaskans).
In the modern world, it has become common for developed countries to fall below the replacement level of births or see population decline. Many of these countries have tried to launch government initiatives to combat this trend, including large cash incentives for having more children, but these programs have been largely ineffective.
Nevertheless, American women tend to have their first children at an earlier age and end up having more children than their counterparts from other developed countries even though the U.S. does not have social welfare programs that are as generous as other rich nations.
Given current (2020) demographic trends, it is projected that the U.S. population would grow slightly by 2100, while other countries, including China and India, will shrink.
Causes
Population aging and falling birth rates in the US is driven by a variety of factors, including increased access to birth control, growing awareness of the realities of parenthood (especially motherhood), and changing societal attitudes toward reproduction, resulting in lower fertility among modern Americans.
The number of unintentional pregnancies has plummeted. Compared to a peak of 96.3 births per 1000 females aged 15 to 19 in 1957, when people married and had children early, the adolescent birth rate fell to 17.3 in 2018. (Black and Hispanic teenagers had the largest decline, though they were still above whites and Asians.)
Twenty-first-century American youths are more likely to have access to effective and long-acting methods of contraception, such as an intrauterine device (IUD), and to be more cautious about sexual intercourse than their predecessors.
While economic troubles and climate anxiety are commonly cited reasons, data suggest they are not the primary factors behind falling fertility in the U.S. Rather, it is due to changing attitudes; today's young people, especially women, tend to prioritize and expect more from their careers and are less interested in having children.
According to the Pew Research Center, the number of non-parents aged 18 to 49 who do not expect to have any children has grown. Among them, a lack of interest in children, medical issues, and financial problems were the top reasons for their predictions.
As parenthood continues to lose its appeal, more and more Americans prefer their own careers, leisure time, savings, and personal freedom to having children and fewer consider children to be a source of happiness or fulfillment.
Among those with children, some have chosen not to have more either because they do not want them, because they would like to spend more time with the ones they already have, or because could not afford more children.
In fact, many admit that their financial circumstances would improve once their children leave the house and that they would be better off not having children. Among those having fewer children than they would like, concerns over the state of the economy and personal financial security are common and many believe the cost of raising a child is too high.
More and more women are realizing that having children is an option they can ignore in favor of economic or educational opportunities; some worry that a woman's career might stall if she chooses to have children.
The number of American women earning university degrees has grown relative to men's since the late 2000s, coinciding with the long-term decline in birth rates. Globally, gender equality is associated with lower fertility.
In the early 2020s, as many as one in five American adults do not want to have children, with some reporting they had made their decision early on. It remains unclear whether they would change their minds.
Data dating back to the 1980s show that this is part of a long-term trend, possibly starting with the Baby Boomers, who were the first cohort to begin questioning social norms on family formation. Furthermore, dedication to work and modern expectations of parents have increased the opportunity cost of having a child.
Because of the aforementioned reasons, the birth rates of women of all age groups (except those in their forties), races, and educational levels have fallen. The number of European Americans has been shrinking since 2016 while the rates of growth of people of other races have fallen as well, except for those of mixed heritage.
Overall, the fall of the European-American and youth populations is the biggest factor behind the aging of the United States. But this trend is moderated by the growth of non-white ethnic groups.
Another major cause of population aging in the United States is the fact that the Baby Boomers, a large cohort, are getting older, adding a large group of older Americans to the population and causing the median age to move up. In addition, employment rates among older workers are increasing. The rate of people who continue working after they are 65 is relatively high in the US, when compared to other developed countries.
For example, in 2011, 16.7% among people aged 65 and over and 29.9% among 65–69 were employed in the US.
Impacts:
By 2030, 20% of Americans are projected to be 65 and older. Both the overall population of the country and the average age are projected to increase over coming years. Given that older people tend to need more health services, some demographers have theorized a significant impact on the country resulting from these trends. Population aging could create an increasing need for services such as nursing homes and care-giving.
Economy:
A shortage of workers is expected in the U.S. workforce due to a declining labor participation rate. Projections show that the demand for labor needed now is not being fulfilled, and the gap between labor needed and labor available will continue to expand over the future.
Owing to the relatively large size population size of those born between the end of WWII and the mid-1960s (referred to by some as the "Baby Boomers"), the number of people generally considered to be of working age is declining.
Additionally, young people are spending more time in education and training and are entering the workforce at a later age, and therefore, there are fewer entering the workforce in their early twenties.
A loss in skilled and capable workers has made it harder for employers to recruit new staff. The retirement of members of the aging workforce could possibly result in the shortage of skilled labor in the future. A majority of experienced utility workers and hospital caregivers, for example, will be eligible for retirement.
By the late 2010s, the United States found itself facing a shortage of tradespeople, a problem that persisted in the early 2020s despite the COVID-19 pandemic-induced recession and prospective employers offering higher salaries and paid training. Having an aging population accelerates industrial automation.
Experts expect the labor crunch of the early 2020s will continue for years to come, due to not just the Great Resignation, but also the aging of the U.S. population, the decline of the labor participation rate, and falling rates of legal immigration.
From a demographic point of view, the labor shortage in the United States during the 2020s is inevitable due to the sheer size of the baby boomers. As the oldest economically active cohort, the baby boomers comprised about a quarter of the U.S. workforce in 2018.
Though they were projected by economists to begin retiring in the 2010s, 29% of older (65–72 years of age) baby boomers in the United States remained active in the labor force in 2018, a large portion compared to older cohorts at the same age. In fact, the official age of retirement in the United States had already been raised, and Baby boomers were incentivized to postpone retirement in part because it allowed them to claim more Social Security benefits once they finally retired.
Furthermore, large numbers would like semi-retirement arrangements or flexible work schedules. The COVID-19 pandemic may have sped up the retirement of some baby boomers. The Pew Research Center reported that the number of baby boomers in retirement had increased by 3.2 million in 2020, the largest annual increase in the previous decade.
But even before the pandemic, the United States had a gap between the number of job openings and the number of unemployed people. Like most other members of the Organization for Economic Cooperation and Development (OECD), the U.S. has seen its productivity growth falter and its debt as a share of GDP grow due to demographic trends.
A shrinking birth rate could exacerbate economic inequality by increasing the importance of family inheritance, while an overall decrease in the population could shrink the economy by reducing the demand for basic goods like groceries and real estate. On the other hand, having fewer or no children has enabled women to pursue more opportunities outside the home.
In fact, places with the highest job growths in the 2010s saw the biggest drops in fertility. For women in such places, the opportunity cost of having a child was higher.. Moreover, people without children do not need to save money to pass on to their children and as such can afford to work fewer hours per week and retire early.
Nevertheless, unlike their counterparts in many other countries East and West, American Baby Boomers had many children of their own, the Millennials, who are a large cohort relative to the nation's population and are themselves having a relatively high birth rate, as of the 2010s.
Millennials and Generation Z have been responsible for a surge in labor participation in the U.S. as the same time as the contraction of the workforce of major economies. Indeed, the U.S. workforce is projected to grow by 10% by 2040.
Having a relatively young, diligent, and productive workforce means that the United States will continue to have a significant number of consumers, investors and taxpayers in the upcoming decades. This gives the nation an economic edge over others.
However, an aging population means that the U.S. economy will be less dynamic, innovative, and productive than it was in the past. Moreover, depending on the household, many women could be forced to give up working in order to take care of their family members, exacerbating the labor shortage.
Education:
See also: Higher education bubble in the United States
By the early 2020s, enrollment in K-12 public schools has fallen, partly due to the switch to private schools and home schooling, but also due to a smaller number of school-aged children (5-17).
In the 1970s, American colleges and universities saw a dramatic increase in enrollments due to the post-war baby boom and the growth of women in higher education and the work force.
By the 1980s and 1990s, although the baby boom had long ended, institutions continued to enjoy good fortune due to growing demand. But this all changed in the aftermath of the Great Recession, which saw significant cuts in funding for education and falling birth rates.
Due to declining birth rates, the number of American high-school graduates is expected to drop after 2025, putting more pressure on institutions of higher learning at a time when many have already been permanently shut down.
Many private colleges will not make it while public ones will struggle to convince state and local governments to keep funding them. Demand for education from the nation's top 100 colleges and universities, however, is likely to remain high, in part because of rising numbers of Indian and Chinese Americans, for whom higher education is of utmost importance.
To survive, non-elite institutions will have to cut back or eliminate courses in the liberal arts and humanities, like gender studies, and expand those in emerging fields, such as artificial intelligence, and professional programs, such as law enforcement.
In addition, Americans who work in higher education are older on average than the average American worker. In the future, this sector of the economy will need to find ways to retain staff or to encourage retirees to come back (part-time).
There is some research supporting the idea that in well-educated countries, it might actually benefit the population to have a birth rate below replacement levels because people at different ages do not make the same level of economic contributions on average.
Environment:
Some demographers have suggested that a declining birth rate may have net positive effects on the country. Many environmentalists see this trend more optimistically because it could help combat the perceived problem of overpopulation.
The world population is expected to reach almost 10 billion by the year 2050, which could pose a burden to Earth's natural resources. Having fewer children has been shown to be an effective way to reduce environmental impact through reduced carbon footprint and higher populations could increase the effects of climate change in the future.
Having an expanding population of people who live longer and are wealthier may not be sustainable. Though the details remain debated, in the 2020s, growing numbers of couples have cited climate change as a reason for having fewer or not having children at all.
Geopolitics:
See also: Cold War II and Pax Americana
Many of America's allies—Canada, the United Kingdom, the European Union, Japan, South Korea, Australia, and New Zealand—are themselves aging. For that reason, they would struggle to finance their own defense and would become even more dependent on the United States at a time when U.S. demographic advantage is fading.
Indeed, while the U.S. maintained a fertility advantage over other developed nations during the 1990s and 2000s, this edge faded away during the 2010s. To combat this problem, the U.S. needs to improve ties with emerging economies, such as the Philippines, Indonesia, and India, though some of these countries are already in the process of transitioning towards an aging society. Furthermore, an aging population will reduce the ability of the United States to participate in global affairs the way it once did.
Nevertheless, because the United States is aging more slowly than any one of its main rivals, it will have an advantage in any future geopolitical contests. Given current demographic trends, it is unlikely that the United States will lose its dominant position to China and Russia.
China has a low fertility rate compared to the United States. China's number of people over 65 as a share of the population is predicted to exceed that of the United States by around 2035. Furthermore, the United States has an advantage that China lacks—immigration.
While the U.S. remains an attractive place for immigrants, very few would like to move to China. In fact, projections of China's economic growth from the early 2020s taking into account China's population aging, among other problems facing the nation, tend to delay the date at which China's economy will surpass America's.
Even if China were to overtake the United States, the latter would soon reclaim its position. On one hand, China's demographic decline relative to the U.S. could prompt it to undertake more risky actions, for example with regards to the issue of Taiwanese independence.
On the other hand, continued U.S. superiority might deter adversaries from taking military actions against either the U.S. or its allies. A "geriatric peace" might be at hand, as the graying powers have an incentive to cooperate in order to maintain the global order before their demographic realities prevent them from doing so.
Occupational safety:
Because of the many older adults opting to remain in the U.S. workforce, many studies have been done to investigate whether the older workers are at greater risk of occupational injury than their younger counterparts. Due to the physical declines associated with aging, older adults tend to exhibit losses in eyesight, hearing and physical strength.
Data shows that older adults have low overall injury rates compared to all age groups, but are more likely to suffer from fatal and more severe occupational injuries. Of all fatal occupational injuries in 2005, older workers accounted for 26.4%, despite only comprising 16.4% of the workforce at the time.
Age increases in fatality rates in occupational injury are more pronounced for workers over the age of 65. The return to work for older workers is also extended; older workers experience a greater median number of lost work days and longer recovery times than younger workers.
Some common occupational injuries and illnesses for older workers include arthritis and fractures. Among older workers, hip fractures are a large concern, given the severity of these injuries.
Social welfare and healthcare:
The U.S. federal social security system functions through collecting payroll taxes to support older citizens. It is possible that a smaller workforce, coupled with increased numbers of longer-living elderly, may have a negative impact on the social security system.
The Social Security Administration (SSA) estimates that the dependency ratio (people ages 65+ divided by people ages 20–64) in 2080 will be over 40%, compared to the 20% in 2005.
SSA data shows one out of every four 65-year-olds today will live past the age of 90, while one out of 10 will live past 95. Indeed, 60% of baby boomers are more worried about outliving their savings than dying. Rising life expectancy may result in reductions in social security benefits, devaluing private and public pension programs.
Were there to be a reduction or elimination of programs such as social security and Medicare, many may need delay retirement and to continue working. In 2018, 29% of Americans aged 65–72 remained active in the labor force, according to the Pew Research Center, as Americans generally expect to continue to work after turning 65.
The baby boomers who chose to remain in the work force after the age of 65 tended to be university graduates, whites, and urban residents. That the boomers maintained a relatively high labor participation rate made economic sense because the longer they postpone retirement, the more Social Security benefits they could claim, once they finally retire.
By 2030, 20% of Americans are predicted to be past the age of retirement, which could pose a burden to the healthcare system. Older and retired people tend to need more health services, which must be provided by their younger counterparts, so some demographers have theorized that this could have a negative impact on the country.
Arthritis, cancer, diabetes, obesity, and cognitive issues are among the most common issues faced by Americans over the age of 65. Older adults who have worked in the construction industry have shown high rates of chronic diseases. Experts suggest that the number of geriatricians will have to triple to meet the demands of the rising elderly.
Demand for other healthcare professionals, such as nurses, occupational therapists, physical therapists and dentists is also projected to rise, as well as for common geriatric healthcare needs, such as medications, joint replacements and cardiovascular operations. Between 1966 and 2023, the number of people qualified for Medicare tripled to nearly 65 million, with 10 million seniors and disabled people being added to the system from 2013 to 2023.
In the early 2020s, among Americans aged 65 or older, 14% of all expenditures goes to healthcare, compared to 8% for the general population. While some enjoy living by themselves, others suffer from physical or mental health issues being socially isolated.
Between the late 2010s and early 2020s, Millennials and Generation Z join the workforce in large numbers, allowing the U.S. to maintain a relatively large tax base, alleviating concerns over the financial sustainability of various social welfare programs.
Nevertheless, in 2023, both Medicare and Social Security as they stand are projected to run out of funds by the late 2020s and mid-2030s, respectively. With the Inflation Reduction Act of 2022, the Joe Biden administration sought to curb the cost of medical care by allowing Medicare to negotiate lower costs for certain drugs and treatments, such as insulin.
Society:
Population aging can potentially change American society as a whole. Many companies use a system, in which older, tenured workers get raises and benefits over time, eventually hitting retirement.
With larger numbers of older workers in the workforce, this model might be unsustainable. In addition, perceptions of older adults in society will change, as the elderly are living longer lives and more active than before.
Changing from a youth-focused culture to having a more positive attitude towards aging and being more respectful of seniors like Japan can help elderly Americans extend their life span and live out their sunset years in dignity. American society will have to confront the negative stereotypes of aging and ageism.
Proposed solutions:
A number of solutions have been proposed to address the problems caused by an aging population. Investing in technological and human-capital development in order to enhance productivity might help the United States offset some of the economic effects of population aging.
Raising the retirement age, further automation, and encouraging higher labor participation rates among women could help alleviate the labor shortage, with the latter successfully done in Japan in the 2010s. Cities could render themselves friendlier towards the elderly, for example by improving public transit.
To deal with the increased demand that could be placed on the healthcare system, telehealth and virtual health monitoring has arisen as a way to help support a larger population of older adults.
The Congressional Budget Office (CBO) has proposed 60 different policy options on how to save billions of dollars on Medicare, such as raising monthly premiums. As of 2023, members of Congress are considering various options to salvage Medicare and Social Security, such as addressing fraud in the Medicare Advantage program and raising the ages of legibility for Medicare and Social Security.
Alternatively, some people have advocated for offering more paid parental leave and child care, thereby encouraging people to have more children. These policies have already been employed in other areas of the world, but with limited results at best.
In some countries such as Germany and Czech Republic they successfully raised the birth rate, but not enough to reach replacement level and at a significant cost.
On the other hand, such policies failed in Finland, Singapore, Taiwan, Japan, and South Korea. It is unlikely that similarly pro-natalist policies would work in the U.S., which maintains a relative high fertility rate despite not having social welfare programs that are as generous as some other developed countries.
Some have argued that reduced immigration will have a larger impact on population growth than the declining birth rate. Immigration has historically been a source of growth for the US, and some have suggested that it could slow or reverse the trend of population aging or decline.
However, studies have shown that immigrants from countries with high-fertility rates often have fewer children when they immigrate to a country where small families are the norm, and this patterns also holds in the U.S. It has also been shown that low-birth rates and sudden increases in immigration often lead to increased levels of populism and xenophobia.
Arguments in favor of increasing immigration to combat declining population levels have sparked outcry from some right-wing political factions in the United States and some European countries.
In the United States, past episodes of domestic turmoil have led to moratoriums on immigration. Furthermore, critics argue that the United States today struggles to integrate the various different ethnic groups already living in the country alongside new immigrants.
Political scientist Robert Putnam argues that ethnic and cultural diversity has its downsides in the form of declining cultural capital, falling civic participation, lower general social trust, and greater social fragmentation.
Since 1996, there have been numerous failed attempts to introduce comprehensive immigration reforms, and while many continue to view immigration as a net benefit to the nation, the American people remain mixed on whether or not they support more immigration in general.
Mass migration is politically problematic. Still, high-skilled immigration, the type of immigration that tends to expand the tax base the most, as has been done in Canada, can help.
See also:
Aging and Society
- YouTube Video: Senior Living for those with No Money
- YouTube Video: How to Pay for Assisted Living | Senior Care Options | Seniorly
- YouTube Video: Independent Living vs Assisted Living: Understand the Difference | Seniorly
Aging has a significant impact on society. People of different ages and gender tend to differ in many aspects, such as legal and social responsibilities, outlooks on life, and self-perceptions.
Young people tend to have fewer legal privileges (if they are below the age of majority), they are more likely to push for political and social change, to develop and adopt new technologies, and to need education.
Older people have different requirements from society and government, and frequently have differing values as well, such as for property and pension rights. Older people are also more likely to vote, and in many countries the young are forbidden from voting. Thus, the aged have comparatively more, or at least different, political influence.
In different societies, age may be viewed or treated differently. For example, age may be measured starting from conception or from birth, and starting at either age zero or age one.
Transitions such as reaching puberty, age of majority, or retirement are often socially significant. The concepts of successful aging and healthy aging refer to both social and physical aspects of the aging process.
Cultural variations:
Arbitrary divisions set to mark periods of life may include:
More casual terms may include "teenagers", "tweens", "twentysomething", "thirtysomething", etc. as well as "vicenarian", "tricenarian", "quadragenarian", etc.
The age of an adult human is commonly measured in whole years since the day of birth. Fractional years, months or even weeks may be used to describe the age of children and infants for finer resolution. The time of day the birth occurred is not commonly considered.
In some cultures, there are other ways to express age. For example, some cultures measure age by counting years including the current year, while others count years without including it. It could be said for the same person that he is twenty years old or that he is in the twenty-first year of his life.
In Russian the former expression is generally used, the latter one has restricted usage: it is used for age of a deceased person in obituaries and for the age of an adult when it is desired to show him/her older than he/she is. (Psychologically, a woman in her 20th year seems older than one who is 19 years old.)
Other cultures that express age differently may not use years elapsed since birth at all. Inuit culture is an example in which birthdays are not celebrated because maturity is not signified in terms of years.
The Navajo culture is another in which age is not counted through years elapsed from birth. In this case, age is measured through certain milestones in a person's life, such as the first time they laugh.
In cultures where age is not measured by years since birth, most individuals do not know how old they are in years. People in these cultures may find more importance in other aspects of their birth, such as the season, agricultural practices, or spiritual connections taking place when they were born.
A culture may also choose to place a greater emphasis on family lineage than age, as is done in Mayan society. A Mayan adult would not determine a child's responsibility and status in terms of age by years, but instead by relative seniority to others in the family or community.
The main purpose of counting age in terms of years from birth is for the convenience of grouping individuals by age, as is needed in industrialized society. The medical practices and compulsory schooling that resulted from industrialization factored largely into the need for counting age in terms of years since birth.
Even in Westernized societies such as the United States, age in terms of years since birth did not begin until the mid-1800s.
Depending on cultural and personal philosophy, ageing can be seen as an undesirable phenomenon, reducing beauty and bringing one closer to death; or as an accumulation of wisdom, mark of survival and a status worthy of respect.
In some cases numerical age is important (whether good or bad), whereas others find the stage in life that one has reached (adulthood, independence, marriage, retirement, career success) to be more important.
East Asian age reckoning is different from that found in Western culture. Traditional Chinese culture uses a different ageing method, called Xusui (虛歲) with respect to common ageing which is called Zhousui (周歲).
According to Luo Zhufeng (1991), the Xusui method, people are born at age 1, not age 0, possibly because conception is already considered to be the start of the life span and possibly because the number '0' was not historically present in Ancient China, and another difference is the ageing day: Xusui grows up at the Spring Festival (aka. Chinese New Year's Day), while Zhousui grows up at one's birthday. In parts of Tibet, age is counted from conception i.e. one is usually 9 months old when one is born.
Age in prenatal development is normally measured in gestational age, taking the last menstruation of the mother as a point of beginning. Alternatively, fertilisation age, beginning from fertilisation can be taken.
Legal;
Most legal systems define a specific age for when an individual is allowed or obliged to do particular activities. These age specifications include:
Admission to a movie for instance, may depend on age according to a motion picture rating system. A bus fare might be discounted for the young or old. Each nation, government and non-government organisation has different ways of classifying age.
Similarly, in many countries in jurisprudence, the defence of infancy is a form of defence by which a defendant argues that, at the time a law was broken, they were not liable for their actions and thus should not be held liable for a crime. Many courts recognise that defendants who are considered to be juveniles may avoid criminal prosecution on account of their age and in borderline cases the age of the offender is often held to be a mitigating circumstance.
Political:
Older people have different requirements from society and government, and frequently have differing values as well, such as for property and pension rights. Older people are also more likely to vote, and in many countries the young are forbidden from voting. Thus, the aged have comparatively more, or at least different, political influence.
Education tends to lose political significance for people as they age.
Coping and well-being:
Psychologists have examined coping skills in the elderly. Various factors, such as social support, religion and spirituality, active engagement with life and having an internal locus of control have been proposed as being beneficial in helping people to cope with stressful life events in later life.
Social support and personal control are possibly the two most important factors that predict well-being, morbidity and mortality in adults. Other factors that may link to well-being and quality of life in the elderly include social relationships (possibly relationships with pets as well as humans), and health.
Retirement, a common transition faced by the elderly, may have both positive and negative consequences. Individuals in different wings in the same retirement home have demonstrated a lower risk of mortality and higher alertness and self-rated health in the wing where residents had greater control over their environment, though personal control may have less impact on specific measures of health.
Social control, perceptions of how much influence one has over one's social relationships, shows support as a moderator variable for the relationship between social support and perceived health in the elderly and may positively influence coping in the elderly.
Religion:
Religion is an important factor used by the elderly in coping with the demands of later life and appears more often than other forms of coping later in life. Religiosity is a multidimensional variable; while participation in religious activities in the sense of participation in formal and organised rituals may decline, it may become a more informal, but still important aspect of life such as through personal or private prayer.
Self-rated health:
Positive self-perception of health has been correlated with higher well-being and reduced mortality in the elderly.
Various reasons have been proposed for this association; people who are objectively healthy may naturally rate their health better than that of their ill counterparts, though this link has been observed even in studies which have controlled for socioeconomic status, psychological functioning and health status.
This finding is generally stronger for men than women, though the pattern between genders is not universal across all studies and some results suggest sex-based differences only appear in certain age groups, for certain causes of mortality and within a specific sub-set of self-ratings of health.
Paradox of ageing:
Seniors' subjective health remains relatively stable while objective health worsens with age.
Furthermore, it seems that the perceived health improves with age when objective health is controlled in the equation. This phenomenon is known as the paradox of ageing. People's expectations concerning health co-evolve with the health norms surrounding one's age.
Elderly people often associate their functional and physical decline with the normal ageing process. The elderly may actually enhance their perception of their own health through social comparison; for instance, the older people get, the more they may consider themselves in better health than their same-aged peers.
Hence, the older a person becomes and the more their actual health declines, the greater the potential role is for social comparison processes to create a gap between a person's objective and subjective health.
Healthcare:
Many societies in Western Europe and Japan have ageing populations. While the effects on society are complex, there is a concern about the impact on health care demand. The large number of suggestions in the literature for specific interventions to cope with the expected increase in demand for long-term care in ageing societies can be organised under four headings:
However, the annual growth in national health spending is not mainly due to increasing demand from ageing populations, but rather has been driven by rising incomes, costly new medical technology, a shortage of health care workers and informational asymmetries between providers and patients.
A number of health problems become more prevalent as people get older. These include mental health problems as well as physical health problems, especially dementia.
Even so, it has been estimated that population ageing only explains 0.2 percentage points of the annual growth rate in medical spending of 4.3 percent since 1970. In addition, certain reforms to the Medicare system in the United States decreased elderly spending on home health care by 12.5 percent per year between 1996 and 2000. This would suggest that the impact of ageing populations on health care costs is not inevitable.
In United States prisons, medical costs for an ageing inmate could be above $100 per day as of July 2007, while typical inmates cost $33 per day. Most State DOCs report spending more than 10 percent of the annual budget on elderly care. That is expected to rise over the next 10–20 years. Some states have talked about releasing ageing inmates early.
Housing:
As Taiwan heads into an ageing society, a study in the city of Kaoshiung suggests that compared to their parents, the current generation of adults have shown a greater interest in age-friendly housing of high-quality building materials and community environment.
The poor living conditions for the elderly was exposed after a fire in the city tore through multiple stories of a dilapidated apartment block.
Successful ageing:
Main article: Successful ageing
The concept of successful ageing can be traced back to the 1950s and was popularised in the 1980s. Previous research into ageing exaggerated the extent to which health disabilities, such as diabetes or osteoporosis, could be attributed exclusively to age and research in gerontology exaggerated the homogeneity of samples of elderly people.
Other research shows that even late in life, potential exists for physical, mental, and social growth and development.
Successful ageing consists of three components:
A greater number of people self-report successful ageing than those that strictly meet these criteria.
Successful ageing may be viewed an interdisciplinary concept, spanning both psychology and sociology, where it is seen as the transaction between society and individuals across the life span with specific focus on the later years of life.
The terms "healthy ageing" and "optimal ageing" have been proposed as alternatives to successful ageing, partly because the term "successful ageing" has been criticised for making healthy ageing sound too competitive.
Six suggested dimensions of successful ageing include:
Numerous worldwide health, ageing and retirement surveys contain questions pertaining to pensions. The Meta Data Repository – created by the non-profit RAND Corporation and sponsored by the National Institute on Aging at the National Institutes of Health – provides access to meta data for these questions as well as links to obtain respondent data from the originating surveys.
Recent studies utilizing artificial intelligence showed that in order to stay biologically younger and lower the chances of most age-related diseases, people should not be unhappy and lonely.
Ageing and communication:
Healthy ageing implies optimal well-being in spite of barriers resulting from age. The global population is ageing and will continue to have communication inabilities unless barriers of communication with the elderly are more highly promoted.
Sensory impairments include hearing and vision deficits, which can cause communication barriers. Changes in cognition, hearing, and vision are easily associated with healthy ageing and can cause problems when diagnosing dementia and aphasia due to the similarities.
Hearing loss:
Hearing loss is a common condition among ageing adults. Common conditions that can increase the risk of hearing loss in elderly people are high blood pressure, diabetes or the use of certain medications harmful to the ear.
Hearing aids are commonly referred to as personal amplifying systems, which can generally improve hearing by about 50%.
Hearing loss among the aged community lessens elders' ability to compensate for other age related social and/or physical problems. Communication problems of elderly adults can be greatly impacted by mechanical problems such as: the translation of ideas into linguistic representation or expression, the perception of linguistic stimuli or the derivation of an idea from a given unit of disclosure.
Changes in these mechanical problems are more important than changes in linguistic knowledge. The main goal of hearing aids is to improve communication and quality of life, not just to restore hearing.
Presbycusis is an example of a hearing deficit that cannot be corrected by hearing aids. Presbycusis, the alteration of hearing sensitivity associated with normal hearing loss, is caused by the decreased amount of hair cells of the inner ear. This is normally caused by long periods of distressing noise that diminish the hair cells which with increasing age will not grow back.
Presbycusis and other such hearing-related problems promote social withdrawal, as individuals begin to lose touch with the world around them. Hearing loss among the aged community lessens elders' ability to compensate for other age-related social and/or physical problems.
This impairment can cause elders to lose touch of social skills because they may have trouble keeping up with fast-paced or hearing different pitched voices in conversation.
Visual impairment:
The interpretation of facial expressions and mouthing can be difficult to understand when an individual has a visual impairment. Such problems hinder the ability of people to understand stimuli and translate information pertaining to perception with their brain for analysis.
Non-verbal communication is important in effective communication and elders with vision loss are more likely to misinterpret or read the other person's actions in a wrong way. Visual impairments also cause a loss in positive perceptions of the environment around them. This can lead to isolation and possible depression in elderly people.
Macular degeneration is a common cause of vision loss in elderly people. It diminishes the macula of the eye, which is responsible for clear vision. It causes progressive loss of central vision and possible loss of colour vision.
This degeneration is caused by systemic changes in the circulation of waste products and growth of abnormal vessels around the retina causing the photoreceptors not to receive proper images. Though ageing almost always causes this, other possible effects and risk factors include smoking, obesity, family history and excessive sunlight exposure.
Digital world:
In a world increasingly relying on digital technologies, older adults face higher risks of social exclusion and prejudices (see digital ageism). Generational segregation naturalizes youth as digitally adept and the old as digitally inept. Older adults' experiences are often excluded from research agendas on digital media.
Political struggle against ageing:
Though many scientists state that radical life extension, delaying and stopping ageing are achievable, there are still no international or national programs focused on stopping ageing or on radical life extension.
There are political forces staying for and against life extension. In 2012 the Longevity political parties started in Russia, then in the US, Israel and the Netherlands. These parties aim to provide political support to anti-ageing and radical life extension research and technologies and want to ensure the fastest possible and at the same time the softest societal transition to the next step: radical life extension and life without ageing, that will make it possible to provide the access to such technologies to the most of the currently living people.
Social science of ageing:
Other definitions:
As cyborgs currently are on the rise some theorists argue there is a need to develop new definitions of aging and for instance a bio-techno-social definition of aging has been suggested.
Young people tend to have fewer legal privileges (if they are below the age of majority), they are more likely to push for political and social change, to develop and adopt new technologies, and to need education.
Older people have different requirements from society and government, and frequently have differing values as well, such as for property and pension rights. Older people are also more likely to vote, and in many countries the young are forbidden from voting. Thus, the aged have comparatively more, or at least different, political influence.
In different societies, age may be viewed or treated differently. For example, age may be measured starting from conception or from birth, and starting at either age zero or age one.
Transitions such as reaching puberty, age of majority, or retirement are often socially significant. The concepts of successful aging and healthy aging refer to both social and physical aspects of the aging process.
Cultural variations:
Arbitrary divisions set to mark periods of life may include:
- juvenile
- (via infancy,
- childhood,
- preadolescence,
- adolescence),
- early adulthood,
- middle adulthood,
- and late adulthood.
More casual terms may include "teenagers", "tweens", "twentysomething", "thirtysomething", etc. as well as "vicenarian", "tricenarian", "quadragenarian", etc.
The age of an adult human is commonly measured in whole years since the day of birth. Fractional years, months or even weeks may be used to describe the age of children and infants for finer resolution. The time of day the birth occurred is not commonly considered.
In some cultures, there are other ways to express age. For example, some cultures measure age by counting years including the current year, while others count years without including it. It could be said for the same person that he is twenty years old or that he is in the twenty-first year of his life.
In Russian the former expression is generally used, the latter one has restricted usage: it is used for age of a deceased person in obituaries and for the age of an adult when it is desired to show him/her older than he/she is. (Psychologically, a woman in her 20th year seems older than one who is 19 years old.)
Other cultures that express age differently may not use years elapsed since birth at all. Inuit culture is an example in which birthdays are not celebrated because maturity is not signified in terms of years.
The Navajo culture is another in which age is not counted through years elapsed from birth. In this case, age is measured through certain milestones in a person's life, such as the first time they laugh.
In cultures where age is not measured by years since birth, most individuals do not know how old they are in years. People in these cultures may find more importance in other aspects of their birth, such as the season, agricultural practices, or spiritual connections taking place when they were born.
A culture may also choose to place a greater emphasis on family lineage than age, as is done in Mayan society. A Mayan adult would not determine a child's responsibility and status in terms of age by years, but instead by relative seniority to others in the family or community.
The main purpose of counting age in terms of years from birth is for the convenience of grouping individuals by age, as is needed in industrialized society. The medical practices and compulsory schooling that resulted from industrialization factored largely into the need for counting age in terms of years since birth.
Even in Westernized societies such as the United States, age in terms of years since birth did not begin until the mid-1800s.
Depending on cultural and personal philosophy, ageing can be seen as an undesirable phenomenon, reducing beauty and bringing one closer to death; or as an accumulation of wisdom, mark of survival and a status worthy of respect.
In some cases numerical age is important (whether good or bad), whereas others find the stage in life that one has reached (adulthood, independence, marriage, retirement, career success) to be more important.
East Asian age reckoning is different from that found in Western culture. Traditional Chinese culture uses a different ageing method, called Xusui (虛歲) with respect to common ageing which is called Zhousui (周歲).
According to Luo Zhufeng (1991), the Xusui method, people are born at age 1, not age 0, possibly because conception is already considered to be the start of the life span and possibly because the number '0' was not historically present in Ancient China, and another difference is the ageing day: Xusui grows up at the Spring Festival (aka. Chinese New Year's Day), while Zhousui grows up at one's birthday. In parts of Tibet, age is counted from conception i.e. one is usually 9 months old when one is born.
Age in prenatal development is normally measured in gestational age, taking the last menstruation of the mother as a point of beginning. Alternatively, fertilisation age, beginning from fertilisation can be taken.
Legal;
Most legal systems define a specific age for when an individual is allowed or obliged to do particular activities. These age specifications include:
- voting age,
- drinking age,
- age of consent,
- age of majority,
- age of criminal responsibility,
- marriageable age,
- age of candidacy,
- and mandatory retirement age.
Admission to a movie for instance, may depend on age according to a motion picture rating system. A bus fare might be discounted for the young or old. Each nation, government and non-government organisation has different ways of classifying age.
Similarly, in many countries in jurisprudence, the defence of infancy is a form of defence by which a defendant argues that, at the time a law was broken, they were not liable for their actions and thus should not be held liable for a crime. Many courts recognise that defendants who are considered to be juveniles may avoid criminal prosecution on account of their age and in borderline cases the age of the offender is often held to be a mitigating circumstance.
Political:
Older people have different requirements from society and government, and frequently have differing values as well, such as for property and pension rights. Older people are also more likely to vote, and in many countries the young are forbidden from voting. Thus, the aged have comparatively more, or at least different, political influence.
Education tends to lose political significance for people as they age.
Coping and well-being:
Psychologists have examined coping skills in the elderly. Various factors, such as social support, religion and spirituality, active engagement with life and having an internal locus of control have been proposed as being beneficial in helping people to cope with stressful life events in later life.
Social support and personal control are possibly the two most important factors that predict well-being, morbidity and mortality in adults. Other factors that may link to well-being and quality of life in the elderly include social relationships (possibly relationships with pets as well as humans), and health.
Retirement, a common transition faced by the elderly, may have both positive and negative consequences. Individuals in different wings in the same retirement home have demonstrated a lower risk of mortality and higher alertness and self-rated health in the wing where residents had greater control over their environment, though personal control may have less impact on specific measures of health.
Social control, perceptions of how much influence one has over one's social relationships, shows support as a moderator variable for the relationship between social support and perceived health in the elderly and may positively influence coping in the elderly.
Religion:
Religion is an important factor used by the elderly in coping with the demands of later life and appears more often than other forms of coping later in life. Religiosity is a multidimensional variable; while participation in religious activities in the sense of participation in formal and organised rituals may decline, it may become a more informal, but still important aspect of life such as through personal or private prayer.
Self-rated health:
Positive self-perception of health has been correlated with higher well-being and reduced mortality in the elderly.
Various reasons have been proposed for this association; people who are objectively healthy may naturally rate their health better than that of their ill counterparts, though this link has been observed even in studies which have controlled for socioeconomic status, psychological functioning and health status.
This finding is generally stronger for men than women, though the pattern between genders is not universal across all studies and some results suggest sex-based differences only appear in certain age groups, for certain causes of mortality and within a specific sub-set of self-ratings of health.
Paradox of ageing:
Seniors' subjective health remains relatively stable while objective health worsens with age.
Furthermore, it seems that the perceived health improves with age when objective health is controlled in the equation. This phenomenon is known as the paradox of ageing. People's expectations concerning health co-evolve with the health norms surrounding one's age.
Elderly people often associate their functional and physical decline with the normal ageing process. The elderly may actually enhance their perception of their own health through social comparison; for instance, the older people get, the more they may consider themselves in better health than their same-aged peers.
Hence, the older a person becomes and the more their actual health declines, the greater the potential role is for social comparison processes to create a gap between a person's objective and subjective health.
Healthcare:
Many societies in Western Europe and Japan have ageing populations. While the effects on society are complex, there is a concern about the impact on health care demand. The large number of suggestions in the literature for specific interventions to cope with the expected increase in demand for long-term care in ageing societies can be organised under four headings:
- improve system performance;
- redesign service delivery;
- support informal caregivers;
- and shift demographic parameters.
However, the annual growth in national health spending is not mainly due to increasing demand from ageing populations, but rather has been driven by rising incomes, costly new medical technology, a shortage of health care workers and informational asymmetries between providers and patients.
A number of health problems become more prevalent as people get older. These include mental health problems as well as physical health problems, especially dementia.
Even so, it has been estimated that population ageing only explains 0.2 percentage points of the annual growth rate in medical spending of 4.3 percent since 1970. In addition, certain reforms to the Medicare system in the United States decreased elderly spending on home health care by 12.5 percent per year between 1996 and 2000. This would suggest that the impact of ageing populations on health care costs is not inevitable.
In United States prisons, medical costs for an ageing inmate could be above $100 per day as of July 2007, while typical inmates cost $33 per day. Most State DOCs report spending more than 10 percent of the annual budget on elderly care. That is expected to rise over the next 10–20 years. Some states have talked about releasing ageing inmates early.
Housing:
As Taiwan heads into an ageing society, a study in the city of Kaoshiung suggests that compared to their parents, the current generation of adults have shown a greater interest in age-friendly housing of high-quality building materials and community environment.
The poor living conditions for the elderly was exposed after a fire in the city tore through multiple stories of a dilapidated apartment block.
Successful ageing:
Main article: Successful ageing
The concept of successful ageing can be traced back to the 1950s and was popularised in the 1980s. Previous research into ageing exaggerated the extent to which health disabilities, such as diabetes or osteoporosis, could be attributed exclusively to age and research in gerontology exaggerated the homogeneity of samples of elderly people.
Other research shows that even late in life, potential exists for physical, mental, and social growth and development.
Successful ageing consists of three components:
- The avoidance of illness and disease
- High cognitive and physical function
- Social and productive engagement
A greater number of people self-report successful ageing than those that strictly meet these criteria.
Successful ageing may be viewed an interdisciplinary concept, spanning both psychology and sociology, where it is seen as the transaction between society and individuals across the life span with specific focus on the later years of life.
The terms "healthy ageing" and "optimal ageing" have been proposed as alternatives to successful ageing, partly because the term "successful ageing" has been criticised for making healthy ageing sound too competitive.
Six suggested dimensions of successful ageing include:
- No physical disability over the age of 75 as rated by a physician;
- Good subjective health assessment (i.e. good self-ratings of one's health);
- Length of undisabled life;
- Good mental health;
- Objective social support;
- Self-rated life satisfaction in eight domains, namely marriage, income-related work, children, friendship and social contacts, hobbies, community service activities, religion and recreation/sports.
Numerous worldwide health, ageing and retirement surveys contain questions pertaining to pensions. The Meta Data Repository – created by the non-profit RAND Corporation and sponsored by the National Institute on Aging at the National Institutes of Health – provides access to meta data for these questions as well as links to obtain respondent data from the originating surveys.
Recent studies utilizing artificial intelligence showed that in order to stay biologically younger and lower the chances of most age-related diseases, people should not be unhappy and lonely.
Ageing and communication:
Healthy ageing implies optimal well-being in spite of barriers resulting from age. The global population is ageing and will continue to have communication inabilities unless barriers of communication with the elderly are more highly promoted.
Sensory impairments include hearing and vision deficits, which can cause communication barriers. Changes in cognition, hearing, and vision are easily associated with healthy ageing and can cause problems when diagnosing dementia and aphasia due to the similarities.
Hearing loss:
Hearing loss is a common condition among ageing adults. Common conditions that can increase the risk of hearing loss in elderly people are high blood pressure, diabetes or the use of certain medications harmful to the ear.
Hearing aids are commonly referred to as personal amplifying systems, which can generally improve hearing by about 50%.
Hearing loss among the aged community lessens elders' ability to compensate for other age related social and/or physical problems. Communication problems of elderly adults can be greatly impacted by mechanical problems such as: the translation of ideas into linguistic representation or expression, the perception of linguistic stimuli or the derivation of an idea from a given unit of disclosure.
Changes in these mechanical problems are more important than changes in linguistic knowledge. The main goal of hearing aids is to improve communication and quality of life, not just to restore hearing.
Presbycusis is an example of a hearing deficit that cannot be corrected by hearing aids. Presbycusis, the alteration of hearing sensitivity associated with normal hearing loss, is caused by the decreased amount of hair cells of the inner ear. This is normally caused by long periods of distressing noise that diminish the hair cells which with increasing age will not grow back.
Presbycusis and other such hearing-related problems promote social withdrawal, as individuals begin to lose touch with the world around them. Hearing loss among the aged community lessens elders' ability to compensate for other age-related social and/or physical problems.
This impairment can cause elders to lose touch of social skills because they may have trouble keeping up with fast-paced or hearing different pitched voices in conversation.
Visual impairment:
The interpretation of facial expressions and mouthing can be difficult to understand when an individual has a visual impairment. Such problems hinder the ability of people to understand stimuli and translate information pertaining to perception with their brain for analysis.
Non-verbal communication is important in effective communication and elders with vision loss are more likely to misinterpret or read the other person's actions in a wrong way. Visual impairments also cause a loss in positive perceptions of the environment around them. This can lead to isolation and possible depression in elderly people.
Macular degeneration is a common cause of vision loss in elderly people. It diminishes the macula of the eye, which is responsible for clear vision. It causes progressive loss of central vision and possible loss of colour vision.
This degeneration is caused by systemic changes in the circulation of waste products and growth of abnormal vessels around the retina causing the photoreceptors not to receive proper images. Though ageing almost always causes this, other possible effects and risk factors include smoking, obesity, family history and excessive sunlight exposure.
Digital world:
In a world increasingly relying on digital technologies, older adults face higher risks of social exclusion and prejudices (see digital ageism). Generational segregation naturalizes youth as digitally adept and the old as digitally inept. Older adults' experiences are often excluded from research agendas on digital media.
Political struggle against ageing:
Though many scientists state that radical life extension, delaying and stopping ageing are achievable, there are still no international or national programs focused on stopping ageing or on radical life extension.
There are political forces staying for and against life extension. In 2012 the Longevity political parties started in Russia, then in the US, Israel and the Netherlands. These parties aim to provide political support to anti-ageing and radical life extension research and technologies and want to ensure the fastest possible and at the same time the softest societal transition to the next step: radical life extension and life without ageing, that will make it possible to provide the access to such technologies to the most of the currently living people.
Social science of ageing:
- Disengagement theory is the idea that separation of older people from active roles in society is normal and appropriate, and benefits both society and older individuals. Disengagement theory, first proposed by Cumming and Henry, has received considerable attention in gerontology, but has been much criticised. The original data on which Cumming and Henry based the theory were from a rather small sample of older adults in Kansas City and from this select sample Cumming and Henry then took disengagement to be a universal theory. There are research data suggesting that the elderly who do become detached from society are those who were initially reclusive individuals and such disengagement is not purely a response to ageing.
- Activity theory, in contrast to disengagement theory, implies that the more active elderly people are, the more likely they are to be satisfied with life. The view that elderly adults should maintain well-being by keeping active has had a considerable history and since 1972, this has come to be known as activity theory. However, this theory may be just as inappropriate as disengagement for some people as the current paradigm on the psychology of ageing is that both disengagement theory and activity theory may be optimal for certain people in old age, depending on both circumstances and personality traits of the individual concerned. There are also data which query whether, as activity theory implies, greater social activity is linked with well-being in adulthood.
- Selectivity theory mediates between the activity and disengagement theories, and suggests that it may benefit older people to become more active in some aspects of their lives, more disengaged in others.
- Continuity theory is the view that in ageing people are inclined to maintain, as much as they can, the same habits, personalities and styles of life that they have developed in earlier years. Continuity theory is Atchley's theory that individuals, in later life, make adaptations to enable them to gain a sense of continuity between the past and the present and the theory implies that this sense of continuity helps to contribute to well-being in later life. Disengagement theory, activity theory and continuity theory are social theories about ageing, though all may be products of their era rather than a valid, universal theory.
Other definitions:
As cyborgs currently are on the rise some theorists argue there is a need to develop new definitions of aging and for instance a bio-techno-social definition of aging has been suggested.
Elderly Care
- YouTube Video: How to Turn Single-Family Homes Into a Residential Assisted-Living Facility
- YouTube Video: Elderly Housing - Retirement and Independent Living Communities
- YouTube Video: Section 202 Low Income Housing, Subsidized Senior Housing & Assisted living
Elder Abuse Can Happen to Anyone. Take These Steps to Keep Your Loved Ones Safe (Continued from above):
Senior citizen abuse can happen to anyone and impacts more than 5 million older adults annually in the United States.:
It breaks our hearts to hear stories on the news of vulnerable seniors who’ve experienced mistreatment and abuse, and maybe it seems as though it’s something that will happen to “somebody else” – definitely not to our own senior loved ones.
However, approximately 5 million seniors in the United States are put through some type of elder abuse annually – and many of these incidents frequently go unreported, according to The Elder Justice Roadmap report released by the U.S. Department of Justice together with Department of Health and Human Services.
The report also clearly shows that, tragically, senior citizen abuse most often happens at the hands of a member of family or close friend – a person the senior knows and trusts. Whether the motivation is financial gain, stress, or another cause, it is important for all of us to recognize the warning signs of elder abuse and to take steps to prevent it.
Elder Abuse Warning Signs
The National Center on Elder Abuse has put together a fact sheet to shed light on the signs of abuse or neglect in older adults. Abuse may be financial, emotional or physical. Watch out for any of the following in your older loved ones, and document any suspected abuse without delay to your local Adult Protective Services agency. Contact information is listed by state on the National Adult Protective Services Association website.
Elder Abuse Prevention:
The easiest way to help older adults stay safe from any kind of abuse is by continuing to be aware, alert, and attentive. Check in with elderly loved ones regularly, and have a network of support set up to make certain seniors have ample opportunities for socialization and interesting activities in order to avoid isolation – one of the key factors that increases an older adult’s risk for abuse or neglect.
You can also proactively tackle the inherent causes of elder abuse. For example, acknowledge if a family caregiver is enduring undue stress, and come up with an alternative care plan for your senior loved one; and make sure there’s no economic motivation in a family member’s desire to act as caregiver.
And, provide the older person with the knowledge and insight required to spot possible abuse, and encourage her or him to tell you right away about any cause for worry.
One of the recommended methods to make certain elder loved ones remain safe from senior citizen abuse is by partnering with At-Home Care Company. Each of our caregivers is put through rigorous criminal background checks and is provided with the supervision that guarantees senior loved ones are safe from abuse.
To learn more about the most experienced elderly care in Des Moines, IA and the surrounding areas, give us a call today at (515) 292-2650.
___________________________________________________________________________
Elderly care (Wikipedia)
Elderly care, or simply eldercare (also known in parts of the English-speaking world as aged care), serves the needs of old adults. It encompasses assisted living, adult daycare, long-term care, nursing homes (often called residential care), hospice care, and home care.
Elderly care emphasizes the social and personal requirements of senior citizens who wish to age with dignity while needing assistance with daily activities and with healthcare. Much elderly care is unpaid.
Elderly care includes a broad range of practices and institutions, as there is a wide variety of elderly care needs and cultural perspectives on the elderly throughout the world.
Cultural and geographic differences:
The form of care provided for older adults varies greatly by country and even region, and is changing rapidly. Older people worldwide consume the most health spending of any age group. There is also an increasingly large proportion of older people worldwide, especially in developing nations with continued pressure to limit fertility and shrink families.
Traditionally, care for older adults has been the responsibility of family members and was provided within the extended family home. Increasingly in modern societies, care is now provided by state or charitable institutions. The reasons for this change include shrinking families, longer life expectancy and geographical dispersion of families. Although these changes have affected European and North American countries first, they are now increasingly affecting Asian countries.
In most western countries, care facilities for older adults are residential family care homes, freestanding assisted living facilities, nursing homes, and continuing care retirement communities (CCRCs). A family care home is a residential home with support and supervisory personnel by an agency, organization, or individual that provides room and board, personal care and habilitation services in a family environment for at least two and no more than six persons.
Due to the wide variety of elderly care needs and cultural perspectives on the elderly, there is a broad range of practices and institutions across different parts of the world.
For example, in many Asian countries whereby younger generations often care for the elderly due to societal norms, government-run elderly care is seldom used in developing countries throughout Asia due to a lack of sufficient taxation necessary to provide an adequate standard of care, whilst privately-run elderly care in developing countries throughout Asia is relatively uncommon due to the stigma of exhibiting insufficient filial piety, having a relatively relaxed work–life interface and insufficient funding from family to pay for privately-run elderly care.
However, institutional elderly care is increasingly adopted across various Asian societies, as the work–life interface becomes more constrained and people with increasing incomes being able to afford the cost of elderly care.
Gender discrepancies in caregivers:
According to Family Caregiver Alliance, the majority of family caregivers are women:
"Many studies have looked at the role of women as family caregivers. Although not all have addressed gender issues and caregiving specifically, the results are still generalizable [sic] to:
In developed nations:
Australia:
Aged care in Australia is designed to make sure that every Australian can contribute as much as possible towards their cost of care, depending on their individual income and assets.
That means that residents pay only what they can afford, and the Commonwealth government pays what the residents cannot pay. An Australian statutory authority, the Productivity Commission, conducted a review of aged care commencing in 2010 and reporting in 2011.
The review concluded that approximately 80% of care for older Australians is informal care provided by family, friends and neighbours. Around a million people received government-subsidised aged care services, most of these received low-level community care support, with 160,000 people in permanent residential care. Expenditure on aged care by all governments in 2009-10 was approximately $11 billion.
The need to increase the level of care, and known weaknesses in the care system (such as skilled workforce shortages and rationing of available care places), led several reviews in the 2000s to conclude that Australia's aged care system needs reform. This culminated in the 2011 Productivity Commission report and subsequent reform proposals.
In accordance with the Living Longer, Living Better amendments of 2013, assistance is provided in accordance with assessed care needs, with additional supplements available for people experiencing homelessness, dementia and veterans.
Australian Aged Care is often considered complicated due to various state and federal funding. Furthermore, there are many acronyms that customers need to be aware of, including ACAT, ACAR, NRCP, HACC, CACP, EACH, EACH-D and CDC (Consumer Directed Care) to name a few.
Canada:
Private for-profit and not-for-profit facilities exist in Canada, but due to cost factors, some provinces operate or subsidize public facilities run by the provincial Ministry of Health. In public care homes, elderly Canadians may pay for their care on a sliding scale, based on annual income.
The scale that they are charged on depends on whether they are considered for "Long Term Care" or "Assisted Living." For example, in January 2010, seniors living in British Columbia's government-subsidized "Long Term Care" (also called "Residential Care") started paying 80% of their after-tax income unless their after-tax income is less than $16,500.
The "Assisted Living" tariff is calculated more simply as 70% of the after-tax income. As seen in Ontario, there are waiting lists for many long-term care homes, so families may need to resort to hiring home healthcare or paying to stay in a private retirement home.
United Kingdom:
Care for the elderly in the UK has traditionally been funded by the state, but it is increasingly rationed, according to a joint report by the King's Fund and Nuffield Trust, as the cost of care to the nation rises. People who have minimal savings or other assets are provided with care either in their own home (from visiting carers) or by moving to a residential care home or nursing home.
Larger numbers of old people need help because of an aging population and medical advances increasing life expectancy, but less is being paid out by the government to help them. A million people who need care get neither formal nor informal help.
A growing number of retirement communities, retirement villages or sheltered housing in the UK also offer an alternative to care homes but only for those with simple care needs. Extra Care housing provision can be suitable for older people with more complex needs. These models allow older people to live independently in a residential community or housing complex with other older people, helping to combat problems common amongst older people such as isolation.
In these communities, residents may access shared services, amenities, and access care services if required.
In general, retirement communities are privately owned and operated, representing a shift from a ‘care as service’ to ‘care as business’ model. Some commercially operated villages have come under scrutiny for a lack of transparency over exit fees or ‘event fees’. It has been noted, however, that paying less now and more later may suit ‘an equity-rich, yet cash-poor, generation of British pensioners.’
Although most retirement village operators are run for profit, there are some charitable organisations in the space: for example, the ExtraCare Charitable Trust, which operates 14 retirement villages mostly in the Midlands, is a registered charity. Charities may derive additional funding from sources such as statutory agencies, charity appeals, legacies, and income from charity shops.
Surplus funds are used to support residents' housing, health and well-being programmes, and for the development of new villages to meet growing national demand.
Extra Care housing usually involves provision of:
United States:
According to the United States Department of Health and Human Services, the older population—persons 65 years or older—numbered 39.6 million in 2009. They represented 12.9% of the U.S. population, about one in every eight Americans.
By 2030, there will be about 72.1 million older persons, more than twice their number in 2000.
People aged over 65 years represented 12.4% of the population in the year 2000, but that is expected to grow to be 19% of the population by 2030. This means there will be more demand for elderly care facilities in the coming years.
There were more than 36,000 assisted living facilities in the United States in 2009, according to the Assisted Living Federation of America. More than 1 million senior citizens are served by these assisted living facilities.
Last-year-of-life expenses represent 22% of all medical spending in the United States, 26% of all Medicare spending, 18% of all non-Medicare spending, and 25% of all Medicaid spending for the poor.
A November 2020 study by the West Health Policy Center stated that more than 1.1 million senior citizens in the U.S. Medicare program are expected to die prematurely over the next decade because they will be unable to afford their prescription medications, requiring an additional $17.7 billion to be spent annually on avoidable medical costs due to health complications.
In the United States, most of the large multi-facility providers are publicly owned and managed as for-profit businesses. However, there are exceptions; the largest operator in the US is the Evangelical Lutheran Good Samaritan Society, a not-for-profit organization that manages 6,531 beds in 22 states, according to a study by the American Health Care Association in 1995.
Given the choice, most older adults would prefer to continue to live in their homes (aging in place). Many elderly people gradually lose functioning ability and require either additional assistance in the home or a move to an elder-care facility.
Their adult children often find it challenging to help their elderly parents make the right choices. Assisted living is one option for the elderly who need assistance with everyday tasks. It costs less than nursing home care but is still considered expensive for most people. Home care services may allow seniors to live in their own home for a longer period of time.
One relatively new service in the United States that can help keep older people in their homes longer is respite care. This type of care allows caregivers the opportunity to go on a vacation or a business trip and to know that their family member has good quality temporary care.
Also, without this help the elder might have to move permanently to an outside facility. Another unique type of care cropping in U.S. hospitals is called acute care of elder units, or ACE units, which provide "a homelike setting" within a medical center specifically for older adults.
Information about long-term care options in the United States can be found by contacting the local Area Agency on Aging, searching through ZIP code, or elder referral agencies such as Silver Living or A Place for Mom. Furthermore, the U.S. government recommends evaluation of health care facilities through websites using data collected from sources such as Medicare records.
In developing nations:
China:
Population ageing is a challenge across the world, and China is no exception. Due to the one-child policy, rural/urban migration and other social changes, the traditional long-term care (LTC) for the elderly which was through direct family care in the past will no longer suffice.
Barely existent now, both institutional and community-based services are expanding to meet the growing need. China is still at an earlier stage in economic development and will be challenged to build these services and train staff.
India:
India's cultural view of elderly care is similar to that of Nepal. Parents are typically cared for by their children into old age, most commonly by their sons. In these countries, elderly citizens, especially men, are viewed in very high regard. Traditional values demand honor and respect for older, wiser people.
Using data on health and living conditions from India's 60th National Sample Survey, a study found that almost a fourth of the elderly reported poor health. Reports of poor health were clustered among the poor, single, lower-educated, and economically inactive groups.
Under its eleventh Five-Year plan, the Indian government has made many strides similar to that of Nepal. Article 41 of the Indian Constitution states that elderly citizens will be guaranteed Social Security support for health care and welfare.
A section of the 1973 Criminal Procedure Code, alluding to its traditional background, mandates that children support their parents if they no longer can themselves.
Nepal:
Due to health and economic benefits, the life expectancy in Nepal jumped from 27 years in 1951 to 65 in 2008. Most elderly Nepali citizens, roughly 85%, live in rural areas.
Because of this, there is a significant lack of government sponsored programs or homes for the elderly. Traditionally, parents live with their children, and today, it is estimated that 90% of the elderly do live in the homes of their family.
This number is changing as more children leave home for work or school, leading to loneliness and mental problems in Nepali elderly.
The Ninth Five-Year Plan included policies in an attempt to care for the elderly left without children as caretakers. A Senior Health Facilities Fund has been established in each district.
The Senior Citizens Health Facilities Program Implementation Guideline, 2061BS provides medical facilities to the elderly, and free medicines as well as health care to people who are poverty stricken in all districts.
In its yearly budget, the government has planned to fund free health care to all heart and kidney patients older than 75. Unfortunately, many of these plans are overly ambitious, which has been recognized by the Nepali government.
Nepal is a developing nation and may not be able to fund all of these programs after the development of an Old Age Allowance (OAA). OAA provides a monthly stipend to all citizens over 70 years old and widows over 60 years old.
There are a handful of private day care facilities for elderly, but they are limited to the capital city. These day care services are very expensive and beyond the reach of general public.
Thailand:
Thailand has observed global patterns of an enlarging elderly class: as fertility control is encouraged and medical advances are being made, the birth rate has diminished and people live longer. The Thai government is noticing and concerned about this trend but tends to let families care for their elderly members rather than create extraneous policies for them.
As of 2011, there are only 25 state-sponsored homes for the elderly, with no more than a few thousand members of each home. Such programs are largely run by volunteers and the services tend to be limited, considering there is not always a guarantee that care will be available.
Private care is tough to follow, often based on assumptions. Because children are less likely to care for their parents, private caretakers are in demand. Volunteer NGOs are available but in very limited quantities.
While there are certainly programs available for use by the elderly in Thailand, questions of equity have risen since their introduction. The rich elderly in Thailand are much more likely to have access to care resources, while the poor elderly are more likely to actually use their acquired health care, as observed in a study by Bhumisuk Khananurak.
However, over 96% of the nation has health insurance with varying degrees of care available.
Medical (skilled care) versus non-medical (social care):
A distinction is generally made between medical and non-medical care, the latter not being provided by medical professionals and much less likely to be covered by insurance or public funds.
In the US, 67% of the one million or so residents in assisted living facilities pay for care out of their own funds. The rest get help from family and friends and from state agencies.
Medicare does not pay unless skilled-nursing care is needed and given in certified skilled nursing facilities or by a skilled nursing agency in the home. Assisted living facilities usually do not meet Medicare's requirements. However, Medicare pays for some skilled care if the elderly person meets the requirements for the Medicare home health benefit.
Thirty-two U.S. states pay for care in assisted living facilities through their Medicaid waiver programs. Similarly, in the United Kingdom the National Health Service provides medical care for the elderly, as for all, free at the point of use, but social care is paid for by the state only in Scotland. England, Wales and Northern Ireland have failed to introduce any legislation on the matter and so social care is not funded by public authorities unless a person has exhausted their private resources, such as by selling the home.
Money provided for supporting elderly people in the UK has fallen by 20% per person during the ten years from 2005 to 2015 and in real terms, the fall is even greater. L Experts claim that vulnerable UK people do not get what they need.
However, elderly care is focused on satisfying the expectations of two tiers of customers: the resident customer and the purchasing customer, who are often not identical, since relatives or public authorities, rather than the resident, may be providing the cost of care. If residents are confused or have communication difficulties, it may be very difficult for relatives or other concerned parties to be sure of the standard of care being given, and the possibility of elder abuse is a continuing source of concern.
The Adult Protective Services Agency, a component of the human service agency in most states, is typically responsible for investigating reports of domestic elder abuse and providing families with help and guidance. Other professionals who may be able to help include doctors or nurses, police officers, lawyers, and social workers.
Shared-decision making:
During primary care:
There is currently limited evidence to form a robust conclusion that involving older patients with multiple health conditions in decision-making during primary care consultations has benefits.
Examples of patient involvement in decision-making about their health care include patient workshops and coaching, individual patient coaching. Further research in this developing area is needed.
Promoting independence:
See also: Dignity of risk
Older adults are scared of losing their independence more than they fear death.
Promoting independence in self-care can provide older adults with the capability to maintain independence longer and can leave them with a sense of achievement when they complete a task unaided. Older adults that require assistance with activities of daily living are at a greater risk of losing their independence with self-care tasks as dependent personal behaviours are often met with reinforcement from caregivers.
It is important for caregivers to ensure that measures are put into place to preserve and promote function rather than contribute to a decline in status of an older adult that has physical limitations.
Caregivers need to be conscious of actions and behaviors that cause older adults to become dependent on them and need to allow older patients to maintain as much independence as possible. Providing information to the older patient on why it is important to perform self-care may allow them to see the benefit in performing self-care independently.
If the older adult is able to complete self-care activities on their own, or even if they need supervision, encourage them in their efforts as maintaining independence can provide them with a sense of accomplishment and the ability to maintain independence longer.
A study done by Langer and Rodin in 1976, investigated what the impacts could be if nursing home residents are given more responsibility in different daily activities, and more choices, compared if those responsibilities given to the nursing home staff.
Residents in the nursing home were split into two different groups. One group of elderly residents was given more responsibility in their choices, and their day-to-day activities than the other group. This involved differences such as having the hospital administrator talked separately to the two groups. The group that was more responsibility induced was given a talk emphasizing their responsibility for themselves, while the talk given to the second group emphasized the responsibility of the nursing staff in taking care of the elderly residents.
Another difference between the two groups is that both groups were given a plant. The group that was more responsibility induced was told they there were responsible for watering the plant each day while, the second group was told that the nursing staff was responsible for watering the plant.
Results from this study indicated that the group that was more responsibility induced became more active, reported being happier, and increased alertness and they showed increased behavioral involvement in activities such as socializing, participation, and attendance in the nursing home activities such the nursing home's movie nights.
They also showed higher health and mood which also declined more slowly than the previous group over time. It is also noted that these long-term benefits were most likely obtained because the treatment was not directed toward one single behavior or stimulus condition.
Elderly-friendly interior design plays a vital role in promoting independence among the elderly. The integration of Internet of Things (IoT) in smart homes provides a remote monitoring system to keep track of the daily activities of the elderly.
Thus adults can live on their own confidently knowing that a feedback alarm will be sent to their caregivers immediately in case of an emergency. This not only allows the aging population to maintain their independence and confidenc, but also brings peace of mind to their friends and family.
Improving physical mobility:
See also: Age-related mobility disability
Impaired mobility is a major health concern for older adults, affecting 50% of people over 85 and at least a fourth of those over 75 years old. As adults lose the ability to walk, climb stairs, or rise from a chair, they become completely disabled. The problem cannot be ignored because people over 65 years old constitute the fastest growing segment of the population.
Therapy designed to improve mobility in elderly patients is usually built around diagnosing and treating specific impairments, such as reduced strength or poor balance. It is appropriate to compare older adults seeking to improve their mobility because athletes seeking to improve their split times.
People in both groups perform best when they measure their progress and work toward specific goals related to strength, aerobic capacity, and other physical qualities. Someone attempting to improve an older adult's mobility must decide what impairments to focus on, and in many cases, there is little scientific evidence to justify any of the options.
Today, many caregivers choose to focus on leg strength and balance. New research suggests that limb velocity and core strength may also be important factors in mobility. Assistive technology and advancements in the health care field are further giving elders greater freedom and mobility.
Several platforms now use artificial intelligence to suggest assistive devices to the elder for a better match. Well planned exercise programs can reduce the rate of falls in older people if they involve multiple categories such as balance, functional and resistance exercise.
Family members are one of the most important caregivers to the elderly, often comprising the majority and most commonly being a daughter or a granddaughter. Family and friends can provide a home (i.e. host elderly relatives), help with money and meet social needs by visiting, taking them out on trips, etc.
One of the major causes of elderly falls is hyponatremia, an electrolyte disturbance when the level of sodium in a person's serum drops below 135 mEq/L. Hyponatremia is the most common electrolyte disorder encountered in the elderly patient population.
Studies have shown that older patients are more prone to hyponatremia as a result of multiple factors including physiologic changes associated with aging such as decreases in glomerular filtration rate, a tendency for defective sodium conservation, and increased vasopressin activity.
Mild hyponatremia ups the risk of fracture in elderly patients because hyponatremia has been shown to cause subtle neurologic impairment that affects gait and attention, similar to that of moderate alcohol intake.
Improving personal mobility:
There are relatively few studies focusing on interventions to improve personal mobility of older adults living at home.
An elderly-friendly interior space can reduce mobility issues as well as other old-age issues.
Staircase, lights, flooring etc can help elders combat mobility issues. Interior design can positively influence the physical and psychological wellness of the elderly, and if each area in house is designed for accommodation, it can let older adults live safely, comfortably and happily.
While navigating floors, climbing stairs is one of the greatest challenges due to high risk of collapsing. A poorly designed staircase can negatively impact elders' psychology as they develop loss of confidence and fear of accidents. However, a staircase designed with the ergonomics and usage patterns of the elderly in mind, can make it easier for everyone.
A stairlift can be a huge step to combat mobility issues.
Appropriate lighting in the interior space makes it easier for elders to move around in the house. An average 60-year-old person requires three times more illuminance than an average 20-year-old boy. Windows, skylight and door openings can incorporate daylight into interior spaces.
However, unplanned opening designs can lead to glare and increase the risk of falls and hinder their ability to perform daily tasks as the elderly are more sensitive to glare than young adults. Dual-layer curtains, drapes, window blinds, light shelves, low visual transmittance glazing or other shading systems can reduce glare.
Illuminance can be increased by combining natural light with various kinds of artificial lights.
When a person slips due to mobility issues, the flooring material plays a major role in the level of impact the person experiences after falling. Choosing the right flooring material in homes depending on whether an individual uses a walker, a wheelchair, or a cane, can also resolve many of the mobility issues faced by adults due to decline in physical strength, loss of balance.
For elders, tile flooring is the least preferred option. Carpet, cork, sheet vinyl flooring are some of the flooring options which can be used for bedrooms, kitchen and bathrooms used by elders. Tiles can be extremely slippery when they are wet which increases the risk of accidents. Also, they are very hard and cold on feet which makes it difficult to walk barefoot during winters.
Legal issues about incapacity:
Legal incapacity is an invasive and sometimes, difficult legal procedure. It requires that a person file a petition with the local courts, stating that the elderly person lacks the capacity to carry out activities that include making medical decisions, voting, making gifts, seeking public benefits, marrying, managing property and financial affairs, choosing where to live and who they socialize with.
Most states' laws require two doctors or other health professionals to provide reports as evidence of such incompetence and the person to be represented by an attorney. Only then can the individual's legal rights be removed, and legal supervision by a guardian or conservator be initiated.
The legal guardian or conservator is the person to whom the court delegates the responsibility of acting on the incapacitated person's behalf and must report regularly his or her activities to the court.
A less restrictive alternative to legal incapacity is the use of "advance directives," powers of attorney, trusts, living wills and healthcare directives. The person who has such documents in place should have prepared them with their attorney when that person had capacity.
Then, if the time comes that the person lacks capacity to carry out the tasks laid out in the documents, the person they named (their agent) can step in to make decisions on their behalf.
The agent has a duty to act as that person would have done so and to act in their best interest.
See also:
Senior citizen abuse can happen to anyone and impacts more than 5 million older adults annually in the United States.:
It breaks our hearts to hear stories on the news of vulnerable seniors who’ve experienced mistreatment and abuse, and maybe it seems as though it’s something that will happen to “somebody else” – definitely not to our own senior loved ones.
However, approximately 5 million seniors in the United States are put through some type of elder abuse annually – and many of these incidents frequently go unreported, according to The Elder Justice Roadmap report released by the U.S. Department of Justice together with Department of Health and Human Services.
The report also clearly shows that, tragically, senior citizen abuse most often happens at the hands of a member of family or close friend – a person the senior knows and trusts. Whether the motivation is financial gain, stress, or another cause, it is important for all of us to recognize the warning signs of elder abuse and to take steps to prevent it.
Elder Abuse Warning Signs
The National Center on Elder Abuse has put together a fact sheet to shed light on the signs of abuse or neglect in older adults. Abuse may be financial, emotional or physical. Watch out for any of the following in your older loved ones, and document any suspected abuse without delay to your local Adult Protective Services agency. Contact information is listed by state on the National Adult Protective Services Association website.
- Unmet hygiene, nutrition, or hydration needs
- Untreated medical conditions
- Hazardous or unhealthy living conditions
- Unusual changes in behavior
- Isolation and/or lack of supervision by primary caregiver
- Bruises, fractures, cuts, burns, etc. without a satisfactory explanation
- Hostile, demeaning, or controlling behavior displayed by primary caregiver
Elder Abuse Prevention:
The easiest way to help older adults stay safe from any kind of abuse is by continuing to be aware, alert, and attentive. Check in with elderly loved ones regularly, and have a network of support set up to make certain seniors have ample opportunities for socialization and interesting activities in order to avoid isolation – one of the key factors that increases an older adult’s risk for abuse or neglect.
You can also proactively tackle the inherent causes of elder abuse. For example, acknowledge if a family caregiver is enduring undue stress, and come up with an alternative care plan for your senior loved one; and make sure there’s no economic motivation in a family member’s desire to act as caregiver.
And, provide the older person with the knowledge and insight required to spot possible abuse, and encourage her or him to tell you right away about any cause for worry.
One of the recommended methods to make certain elder loved ones remain safe from senior citizen abuse is by partnering with At-Home Care Company. Each of our caregivers is put through rigorous criminal background checks and is provided with the supervision that guarantees senior loved ones are safe from abuse.
To learn more about the most experienced elderly care in Des Moines, IA and the surrounding areas, give us a call today at (515) 292-2650.
___________________________________________________________________________
Elderly care (Wikipedia)
Elderly care, or simply eldercare (also known in parts of the English-speaking world as aged care), serves the needs of old adults. It encompasses assisted living, adult daycare, long-term care, nursing homes (often called residential care), hospice care, and home care.
Elderly care emphasizes the social and personal requirements of senior citizens who wish to age with dignity while needing assistance with daily activities and with healthcare. Much elderly care is unpaid.
Elderly care includes a broad range of practices and institutions, as there is a wide variety of elderly care needs and cultural perspectives on the elderly throughout the world.
Cultural and geographic differences:
The form of care provided for older adults varies greatly by country and even region, and is changing rapidly. Older people worldwide consume the most health spending of any age group. There is also an increasingly large proportion of older people worldwide, especially in developing nations with continued pressure to limit fertility and shrink families.
Traditionally, care for older adults has been the responsibility of family members and was provided within the extended family home. Increasingly in modern societies, care is now provided by state or charitable institutions. The reasons for this change include shrinking families, longer life expectancy and geographical dispersion of families. Although these changes have affected European and North American countries first, they are now increasingly affecting Asian countries.
In most western countries, care facilities for older adults are residential family care homes, freestanding assisted living facilities, nursing homes, and continuing care retirement communities (CCRCs). A family care home is a residential home with support and supervisory personnel by an agency, organization, or individual that provides room and board, personal care and habilitation services in a family environment for at least two and no more than six persons.
Due to the wide variety of elderly care needs and cultural perspectives on the elderly, there is a broad range of practices and institutions across different parts of the world.
For example, in many Asian countries whereby younger generations often care for the elderly due to societal norms, government-run elderly care is seldom used in developing countries throughout Asia due to a lack of sufficient taxation necessary to provide an adequate standard of care, whilst privately-run elderly care in developing countries throughout Asia is relatively uncommon due to the stigma of exhibiting insufficient filial piety, having a relatively relaxed work–life interface and insufficient funding from family to pay for privately-run elderly care.
However, institutional elderly care is increasingly adopted across various Asian societies, as the work–life interface becomes more constrained and people with increasing incomes being able to afford the cost of elderly care.
Gender discrepancies in caregivers:
According to Family Caregiver Alliance, the majority of family caregivers are women:
"Many studies have looked at the role of women as family caregivers. Although not all have addressed gender issues and caregiving specifically, the results are still generalizable [sic] to:
- Estimates of the age of family or informal caregivers who are women range from 59% to 75%.
- The average caregiver is age 46, female, married and worked outside the home earning an annual income of $35,000.
- Although men also provide assistance, female caregivers may spend as much as 50% more time providing care than male caregivers."
In developed nations:
Australia:
Aged care in Australia is designed to make sure that every Australian can contribute as much as possible towards their cost of care, depending on their individual income and assets.
That means that residents pay only what they can afford, and the Commonwealth government pays what the residents cannot pay. An Australian statutory authority, the Productivity Commission, conducted a review of aged care commencing in 2010 and reporting in 2011.
The review concluded that approximately 80% of care for older Australians is informal care provided by family, friends and neighbours. Around a million people received government-subsidised aged care services, most of these received low-level community care support, with 160,000 people in permanent residential care. Expenditure on aged care by all governments in 2009-10 was approximately $11 billion.
The need to increase the level of care, and known weaknesses in the care system (such as skilled workforce shortages and rationing of available care places), led several reviews in the 2000s to conclude that Australia's aged care system needs reform. This culminated in the 2011 Productivity Commission report and subsequent reform proposals.
In accordance with the Living Longer, Living Better amendments of 2013, assistance is provided in accordance with assessed care needs, with additional supplements available for people experiencing homelessness, dementia and veterans.
Australian Aged Care is often considered complicated due to various state and federal funding. Furthermore, there are many acronyms that customers need to be aware of, including ACAT, ACAR, NRCP, HACC, CACP, EACH, EACH-D and CDC (Consumer Directed Care) to name a few.
Canada:
Private for-profit and not-for-profit facilities exist in Canada, but due to cost factors, some provinces operate or subsidize public facilities run by the provincial Ministry of Health. In public care homes, elderly Canadians may pay for their care on a sliding scale, based on annual income.
The scale that they are charged on depends on whether they are considered for "Long Term Care" or "Assisted Living." For example, in January 2010, seniors living in British Columbia's government-subsidized "Long Term Care" (also called "Residential Care") started paying 80% of their after-tax income unless their after-tax income is less than $16,500.
The "Assisted Living" tariff is calculated more simply as 70% of the after-tax income. As seen in Ontario, there are waiting lists for many long-term care homes, so families may need to resort to hiring home healthcare or paying to stay in a private retirement home.
United Kingdom:
Care for the elderly in the UK has traditionally been funded by the state, but it is increasingly rationed, according to a joint report by the King's Fund and Nuffield Trust, as the cost of care to the nation rises. People who have minimal savings or other assets are provided with care either in their own home (from visiting carers) or by moving to a residential care home or nursing home.
Larger numbers of old people need help because of an aging population and medical advances increasing life expectancy, but less is being paid out by the government to help them. A million people who need care get neither formal nor informal help.
A growing number of retirement communities, retirement villages or sheltered housing in the UK also offer an alternative to care homes but only for those with simple care needs. Extra Care housing provision can be suitable for older people with more complex needs. These models allow older people to live independently in a residential community or housing complex with other older people, helping to combat problems common amongst older people such as isolation.
In these communities, residents may access shared services, amenities, and access care services if required.
In general, retirement communities are privately owned and operated, representing a shift from a ‘care as service’ to ‘care as business’ model. Some commercially operated villages have come under scrutiny for a lack of transparency over exit fees or ‘event fees’. It has been noted, however, that paying less now and more later may suit ‘an equity-rich, yet cash-poor, generation of British pensioners.’
Although most retirement village operators are run for profit, there are some charitable organisations in the space: for example, the ExtraCare Charitable Trust, which operates 14 retirement villages mostly in the Midlands, is a registered charity. Charities may derive additional funding from sources such as statutory agencies, charity appeals, legacies, and income from charity shops.
Surplus funds are used to support residents' housing, health and well-being programmes, and for the development of new villages to meet growing national demand.
Extra Care housing usually involves provision of:
- Purpose-built, accessible housing design
- Safety and security e.g. controlled entry to the building
- Fully self-contained properties, where occupants have their own front doors, and legal status as tenants with security of tenure
- Tenants have the right to control who enters their home
- Office space for use by staff serving the scheme (and sometimes the wider community)
- Some communal spaces and facilities
- Access to care and support services 24 hours per day
- Community alarms and other assistive technologies.
United States:
According to the United States Department of Health and Human Services, the older population—persons 65 years or older—numbered 39.6 million in 2009. They represented 12.9% of the U.S. population, about one in every eight Americans.
By 2030, there will be about 72.1 million older persons, more than twice their number in 2000.
People aged over 65 years represented 12.4% of the population in the year 2000, but that is expected to grow to be 19% of the population by 2030. This means there will be more demand for elderly care facilities in the coming years.
There were more than 36,000 assisted living facilities in the United States in 2009, according to the Assisted Living Federation of America. More than 1 million senior citizens are served by these assisted living facilities.
Last-year-of-life expenses represent 22% of all medical spending in the United States, 26% of all Medicare spending, 18% of all non-Medicare spending, and 25% of all Medicaid spending for the poor.
A November 2020 study by the West Health Policy Center stated that more than 1.1 million senior citizens in the U.S. Medicare program are expected to die prematurely over the next decade because they will be unable to afford their prescription medications, requiring an additional $17.7 billion to be spent annually on avoidable medical costs due to health complications.
In the United States, most of the large multi-facility providers are publicly owned and managed as for-profit businesses. However, there are exceptions; the largest operator in the US is the Evangelical Lutheran Good Samaritan Society, a not-for-profit organization that manages 6,531 beds in 22 states, according to a study by the American Health Care Association in 1995.
Given the choice, most older adults would prefer to continue to live in their homes (aging in place). Many elderly people gradually lose functioning ability and require either additional assistance in the home or a move to an elder-care facility.
Their adult children often find it challenging to help their elderly parents make the right choices. Assisted living is one option for the elderly who need assistance with everyday tasks. It costs less than nursing home care but is still considered expensive for most people. Home care services may allow seniors to live in their own home for a longer period of time.
One relatively new service in the United States that can help keep older people in their homes longer is respite care. This type of care allows caregivers the opportunity to go on a vacation or a business trip and to know that their family member has good quality temporary care.
Also, without this help the elder might have to move permanently to an outside facility. Another unique type of care cropping in U.S. hospitals is called acute care of elder units, or ACE units, which provide "a homelike setting" within a medical center specifically for older adults.
Information about long-term care options in the United States can be found by contacting the local Area Agency on Aging, searching through ZIP code, or elder referral agencies such as Silver Living or A Place for Mom. Furthermore, the U.S. government recommends evaluation of health care facilities through websites using data collected from sources such as Medicare records.
In developing nations:
China:
Population ageing is a challenge across the world, and China is no exception. Due to the one-child policy, rural/urban migration and other social changes, the traditional long-term care (LTC) for the elderly which was through direct family care in the past will no longer suffice.
Barely existent now, both institutional and community-based services are expanding to meet the growing need. China is still at an earlier stage in economic development and will be challenged to build these services and train staff.
India:
India's cultural view of elderly care is similar to that of Nepal. Parents are typically cared for by their children into old age, most commonly by their sons. In these countries, elderly citizens, especially men, are viewed in very high regard. Traditional values demand honor and respect for older, wiser people.
Using data on health and living conditions from India's 60th National Sample Survey, a study found that almost a fourth of the elderly reported poor health. Reports of poor health were clustered among the poor, single, lower-educated, and economically inactive groups.
Under its eleventh Five-Year plan, the Indian government has made many strides similar to that of Nepal. Article 41 of the Indian Constitution states that elderly citizens will be guaranteed Social Security support for health care and welfare.
A section of the 1973 Criminal Procedure Code, alluding to its traditional background, mandates that children support their parents if they no longer can themselves.
Nepal:
Due to health and economic benefits, the life expectancy in Nepal jumped from 27 years in 1951 to 65 in 2008. Most elderly Nepali citizens, roughly 85%, live in rural areas.
Because of this, there is a significant lack of government sponsored programs or homes for the elderly. Traditionally, parents live with their children, and today, it is estimated that 90% of the elderly do live in the homes of their family.
This number is changing as more children leave home for work or school, leading to loneliness and mental problems in Nepali elderly.
The Ninth Five-Year Plan included policies in an attempt to care for the elderly left without children as caretakers. A Senior Health Facilities Fund has been established in each district.
The Senior Citizens Health Facilities Program Implementation Guideline, 2061BS provides medical facilities to the elderly, and free medicines as well as health care to people who are poverty stricken in all districts.
In its yearly budget, the government has planned to fund free health care to all heart and kidney patients older than 75. Unfortunately, many of these plans are overly ambitious, which has been recognized by the Nepali government.
Nepal is a developing nation and may not be able to fund all of these programs after the development of an Old Age Allowance (OAA). OAA provides a monthly stipend to all citizens over 70 years old and widows over 60 years old.
There are a handful of private day care facilities for elderly, but they are limited to the capital city. These day care services are very expensive and beyond the reach of general public.
Thailand:
Thailand has observed global patterns of an enlarging elderly class: as fertility control is encouraged and medical advances are being made, the birth rate has diminished and people live longer. The Thai government is noticing and concerned about this trend but tends to let families care for their elderly members rather than create extraneous policies for them.
As of 2011, there are only 25 state-sponsored homes for the elderly, with no more than a few thousand members of each home. Such programs are largely run by volunteers and the services tend to be limited, considering there is not always a guarantee that care will be available.
Private care is tough to follow, often based on assumptions. Because children are less likely to care for their parents, private caretakers are in demand. Volunteer NGOs are available but in very limited quantities.
While there are certainly programs available for use by the elderly in Thailand, questions of equity have risen since their introduction. The rich elderly in Thailand are much more likely to have access to care resources, while the poor elderly are more likely to actually use their acquired health care, as observed in a study by Bhumisuk Khananurak.
However, over 96% of the nation has health insurance with varying degrees of care available.
Medical (skilled care) versus non-medical (social care):
A distinction is generally made between medical and non-medical care, the latter not being provided by medical professionals and much less likely to be covered by insurance or public funds.
In the US, 67% of the one million or so residents in assisted living facilities pay for care out of their own funds. The rest get help from family and friends and from state agencies.
Medicare does not pay unless skilled-nursing care is needed and given in certified skilled nursing facilities or by a skilled nursing agency in the home. Assisted living facilities usually do not meet Medicare's requirements. However, Medicare pays for some skilled care if the elderly person meets the requirements for the Medicare home health benefit.
Thirty-two U.S. states pay for care in assisted living facilities through their Medicaid waiver programs. Similarly, in the United Kingdom the National Health Service provides medical care for the elderly, as for all, free at the point of use, but social care is paid for by the state only in Scotland. England, Wales and Northern Ireland have failed to introduce any legislation on the matter and so social care is not funded by public authorities unless a person has exhausted their private resources, such as by selling the home.
Money provided for supporting elderly people in the UK has fallen by 20% per person during the ten years from 2005 to 2015 and in real terms, the fall is even greater. L Experts claim that vulnerable UK people do not get what they need.
However, elderly care is focused on satisfying the expectations of two tiers of customers: the resident customer and the purchasing customer, who are often not identical, since relatives or public authorities, rather than the resident, may be providing the cost of care. If residents are confused or have communication difficulties, it may be very difficult for relatives or other concerned parties to be sure of the standard of care being given, and the possibility of elder abuse is a continuing source of concern.
The Adult Protective Services Agency, a component of the human service agency in most states, is typically responsible for investigating reports of domestic elder abuse and providing families with help and guidance. Other professionals who may be able to help include doctors or nurses, police officers, lawyers, and social workers.
Shared-decision making:
During primary care:
There is currently limited evidence to form a robust conclusion that involving older patients with multiple health conditions in decision-making during primary care consultations has benefits.
Examples of patient involvement in decision-making about their health care include patient workshops and coaching, individual patient coaching. Further research in this developing area is needed.
Promoting independence:
See also: Dignity of risk
Older adults are scared of losing their independence more than they fear death.
Promoting independence in self-care can provide older adults with the capability to maintain independence longer and can leave them with a sense of achievement when they complete a task unaided. Older adults that require assistance with activities of daily living are at a greater risk of losing their independence with self-care tasks as dependent personal behaviours are often met with reinforcement from caregivers.
It is important for caregivers to ensure that measures are put into place to preserve and promote function rather than contribute to a decline in status of an older adult that has physical limitations.
Caregivers need to be conscious of actions and behaviors that cause older adults to become dependent on them and need to allow older patients to maintain as much independence as possible. Providing information to the older patient on why it is important to perform self-care may allow them to see the benefit in performing self-care independently.
If the older adult is able to complete self-care activities on their own, or even if they need supervision, encourage them in their efforts as maintaining independence can provide them with a sense of accomplishment and the ability to maintain independence longer.
A study done by Langer and Rodin in 1976, investigated what the impacts could be if nursing home residents are given more responsibility in different daily activities, and more choices, compared if those responsibilities given to the nursing home staff.
Residents in the nursing home were split into two different groups. One group of elderly residents was given more responsibility in their choices, and their day-to-day activities than the other group. This involved differences such as having the hospital administrator talked separately to the two groups. The group that was more responsibility induced was given a talk emphasizing their responsibility for themselves, while the talk given to the second group emphasized the responsibility of the nursing staff in taking care of the elderly residents.
Another difference between the two groups is that both groups were given a plant. The group that was more responsibility induced was told they there were responsible for watering the plant each day while, the second group was told that the nursing staff was responsible for watering the plant.
Results from this study indicated that the group that was more responsibility induced became more active, reported being happier, and increased alertness and they showed increased behavioral involvement in activities such as socializing, participation, and attendance in the nursing home activities such the nursing home's movie nights.
They also showed higher health and mood which also declined more slowly than the previous group over time. It is also noted that these long-term benefits were most likely obtained because the treatment was not directed toward one single behavior or stimulus condition.
Elderly-friendly interior design plays a vital role in promoting independence among the elderly. The integration of Internet of Things (IoT) in smart homes provides a remote monitoring system to keep track of the daily activities of the elderly.
Thus adults can live on their own confidently knowing that a feedback alarm will be sent to their caregivers immediately in case of an emergency. This not only allows the aging population to maintain their independence and confidenc, but also brings peace of mind to their friends and family.
Improving physical mobility:
See also: Age-related mobility disability
Impaired mobility is a major health concern for older adults, affecting 50% of people over 85 and at least a fourth of those over 75 years old. As adults lose the ability to walk, climb stairs, or rise from a chair, they become completely disabled. The problem cannot be ignored because people over 65 years old constitute the fastest growing segment of the population.
Therapy designed to improve mobility in elderly patients is usually built around diagnosing and treating specific impairments, such as reduced strength or poor balance. It is appropriate to compare older adults seeking to improve their mobility because athletes seeking to improve their split times.
People in both groups perform best when they measure their progress and work toward specific goals related to strength, aerobic capacity, and other physical qualities. Someone attempting to improve an older adult's mobility must decide what impairments to focus on, and in many cases, there is little scientific evidence to justify any of the options.
Today, many caregivers choose to focus on leg strength and balance. New research suggests that limb velocity and core strength may also be important factors in mobility. Assistive technology and advancements in the health care field are further giving elders greater freedom and mobility.
Several platforms now use artificial intelligence to suggest assistive devices to the elder for a better match. Well planned exercise programs can reduce the rate of falls in older people if they involve multiple categories such as balance, functional and resistance exercise.
Family members are one of the most important caregivers to the elderly, often comprising the majority and most commonly being a daughter or a granddaughter. Family and friends can provide a home (i.e. host elderly relatives), help with money and meet social needs by visiting, taking them out on trips, etc.
One of the major causes of elderly falls is hyponatremia, an electrolyte disturbance when the level of sodium in a person's serum drops below 135 mEq/L. Hyponatremia is the most common electrolyte disorder encountered in the elderly patient population.
Studies have shown that older patients are more prone to hyponatremia as a result of multiple factors including physiologic changes associated with aging such as decreases in glomerular filtration rate, a tendency for defective sodium conservation, and increased vasopressin activity.
Mild hyponatremia ups the risk of fracture in elderly patients because hyponatremia has been shown to cause subtle neurologic impairment that affects gait and attention, similar to that of moderate alcohol intake.
Improving personal mobility:
There are relatively few studies focusing on interventions to improve personal mobility of older adults living at home.
An elderly-friendly interior space can reduce mobility issues as well as other old-age issues.
Staircase, lights, flooring etc can help elders combat mobility issues. Interior design can positively influence the physical and psychological wellness of the elderly, and if each area in house is designed for accommodation, it can let older adults live safely, comfortably and happily.
While navigating floors, climbing stairs is one of the greatest challenges due to high risk of collapsing. A poorly designed staircase can negatively impact elders' psychology as they develop loss of confidence and fear of accidents. However, a staircase designed with the ergonomics and usage patterns of the elderly in mind, can make it easier for everyone.
A stairlift can be a huge step to combat mobility issues.
Appropriate lighting in the interior space makes it easier for elders to move around in the house. An average 60-year-old person requires three times more illuminance than an average 20-year-old boy. Windows, skylight and door openings can incorporate daylight into interior spaces.
However, unplanned opening designs can lead to glare and increase the risk of falls and hinder their ability to perform daily tasks as the elderly are more sensitive to glare than young adults. Dual-layer curtains, drapes, window blinds, light shelves, low visual transmittance glazing or other shading systems can reduce glare.
Illuminance can be increased by combining natural light with various kinds of artificial lights.
When a person slips due to mobility issues, the flooring material plays a major role in the level of impact the person experiences after falling. Choosing the right flooring material in homes depending on whether an individual uses a walker, a wheelchair, or a cane, can also resolve many of the mobility issues faced by adults due to decline in physical strength, loss of balance.
For elders, tile flooring is the least preferred option. Carpet, cork, sheet vinyl flooring are some of the flooring options which can be used for bedrooms, kitchen and bathrooms used by elders. Tiles can be extremely slippery when they are wet which increases the risk of accidents. Also, they are very hard and cold on feet which makes it difficult to walk barefoot during winters.
Legal issues about incapacity:
Legal incapacity is an invasive and sometimes, difficult legal procedure. It requires that a person file a petition with the local courts, stating that the elderly person lacks the capacity to carry out activities that include making medical decisions, voting, making gifts, seeking public benefits, marrying, managing property and financial affairs, choosing where to live and who they socialize with.
Most states' laws require two doctors or other health professionals to provide reports as evidence of such incompetence and the person to be represented by an attorney. Only then can the individual's legal rights be removed, and legal supervision by a guardian or conservator be initiated.
The legal guardian or conservator is the person to whom the court delegates the responsibility of acting on the incapacitated person's behalf and must report regularly his or her activities to the court.
A less restrictive alternative to legal incapacity is the use of "advance directives," powers of attorney, trusts, living wills and healthcare directives. The person who has such documents in place should have prepared them with their attorney when that person had capacity.
Then, if the time comes that the person lacks capacity to carry out the tasks laid out in the documents, the person they named (their agent) can step in to make decisions on their behalf.
The agent has a duty to act as that person would have done so and to act in their best interest.
See also:
- Food preferences in older adults and seniors
- Friendly caller program
- Gerontology
- Home automation for the elderly and disabled
- Social impact of the COVID-19 pandemic#Elderly care
- Transgenerational design
Senior Living as either Assisted Living (including Nursing Homes); vs. Independent Living
- YouTube Video: Senior Living Options | What Senior Care Option is Right for You?
- YouTube Video: Costs of Care: In Home Care Versus Assisted Living
- YouTube Video: Difference between Skilled Nursing and Assisted Living? Does Medicaid pay for Assisted Living?
[Your Webhost: for this topic you will find several choices including options for senior care to give you all the considerations and options when looking for health care options for yourself or your aging family members.]
Senior living
Senior living is a concept that encompasses a range of housing and lifestyle options for ageing persons adapted to the challenges of health issues associated with ageing, such as limited mobility and susceptibility to illness.
Common forms:
Based on the health and financial means of the individual, these may include living in a retirement community or an age-restricted community, independent senior living, or living in a nursing home or retirement home.
A retirement community is a residential community or housing complex designed for older adults who are generally able to care for themselves; however, assistance from home care agencies is allowed in some communities, and activities and socialization opportunities are often provided. Some of the characteristics typically are: the community must be age-restricted or age-qualified, residents must be partially or fully retired, and the community offers shared services or amenities.
An age-restricted community is a residential community, often gated, that typically limits 80% of the residency to individuals who are over a set age. The minimum age is frequently set at 55 years old, but it can vary. These communities are set up to accommodate older individuals who would like to live in an area without the perceived problems of having children around. In most cases a younger spouse or significant other is permitted to live in the community as long as one member meets the minimum age requirement.
Age-qualified communities, also known as 55+ communities, active adult communities, lifestyle communities, or retirement communities, are often planned communities that offer homes and community features that are attractive to 55+ adults. These might include a clubhouse or lifestyle center with a good many activities, sometimes with indoor and outdoor swimming pools, exercise facilities, craft rooms, demonstration kitchens, and decks and patios for gathering.
Independent senior living communities commonly provide apartments, but some also offer cottages, condominiums, and single-family homes. Residents include seniors who do not require assistance with daily activities or 24/7 skilled nursing, but may benefit from convenient services, senior-friendly surroundings, and increased social opportunities that independent senior living communities offer.
Independent senior living properties do not provide health care or assistance with activities of daily living (ADLs) such as medication, bathing, eating, dressing, toileting and more.
Independent senior living differs from continuing care communities, which offer independent living along with multiple other levels of care, such as assisted living and skilled nursing, in one single residence.
A retirement home is a multi-residence housing facility intended for the elderly. The concept is sometimes called an old people's home, old folks' home, or old age home, although old people's home can also refer to a nursing home. Typically, each person or couple in the home has an apartment-style room or suite of rooms.
Additional facilities are provided within the building. This can include facilities for meals, gatherings, recreation activities, and some form of health or hospice care. A place in a retirement home can be paid for on a rental basis, like an apartment, or can be bought in perpetuity on the same basis as a condominium.
___________________________________________________________________________
Assisted living
An assisted living residence or assisted living facility (ALF) is a housing facility for people with disabilities or for adults who cannot or who choose not to live independently. The term is popular in the United States, but the setting is similar to a retirement home, in the sense that facilities provide a group living environment and typically cater to an older adult population. There is also Caribbean assisted living, which offers a similar service in a resort-like environment (somewhat like assisted vacationing).
The expansion of assisted living has been the shift from "care as service" to "care as business" in the broader health care system predicted in 1982. A consumer-driven industry, assisted living offers a wide range of options, levels of care, and diversity of services (Lockhart, 2009) and is subject to state rather than federal regulatory oversight.
What "Assisted living" means depends on both the state and provider in question: variations in state regulatory definitions are significant and provider variables include everything from philosophy, geographic location and auspice, to organizational size and structure.
Assisted living evolved from small "board and care" or "personal care" homes and offers a "social model" of care (compared to the medical model of a skilled nursing facility). The assisted living industry is a segment of the senior housing industry and assisted living services can be delivered in stand-alone facilities or as part of multi-level senior living community.
The industry is fragmented and dominated by for-profit providers. In 2010, six of the seventy largest providers were non-profit and none of the top twenty was non-profit (Martin, 2010). Information in this edit is from an article published in 2012 that reviewed the industry and reports results of a research study of assisted living facilities.
In 2012 the U.S. Government estimated that there were 22,200 assisted living facilities in the U.S. (compared to 15,700 nursing homes) and that 713,300 people were residents of these facilities. The number of assisted living facilities in the U.S. has increased dramatically since the early 2000s.
In the U.S., ALFs can be owned by for-profit companies (publicly traded companies or limited liability companies [LLCs]), non-profit organizations, or governments. These facilities typically provide supervision or assistance with activities of daily living (ADLs); coordination of services by outside health care providers; and monitoring of resident activities to help to ensure their health, safety, and well-being. Assistance often includes the administration or supervision of medication, or personal care services.
There has been controversy generated by reports of neglect, abuse and mistreatment of residents at assisted living facilities in the U.S.
Within the United States assisted living spectrum, there is no nationally recognized definition of assisted living. Assisted living facilities are regulated and licensed at the US state level. These regulations include staffing, training, and quality and safety standards.
This is differentiated from nursing homes, which are regulated on a federal level and are generally held to more stringent standards. More than two-thirds of the states use the licensure term "assisted living." Other licensure terms used for this philosophy of care include residential care home, assisted care living facilities, and personal care homes. Each state licensing agency has its own definition of the term it uses to describe assisted living.
Because the term assisted living has not been defined in some states it is often a marketing term used by a variety of senior living communities, licensed or unlicensed. Assisted living facilities in the United States had a national median monthly rate of $3,500.00 in 2014, a 1.45% increase over 2013 and a 4.29% increase over a five-year period from 2009 to 2014.
Types:
As widely varied as the state licensing and definitions are, so are the types of physical layouts of buildings in which assisted living services are provided.
The average assisted living facility is in a commercial building, yet some assisted living services use large residential buildings, known as Residential Assisted Living homes, or "RAL".
Residential Assisted Living homes can vary in price and amenities, and can even be grouped into a separate term known as a Luxury Residential Assisted Living Home, or "LRAL".
Assisted living facilities can range in size from a small residential house for one resident up to very large facilities providing services to hundreds of residents. Assisted living falls somewhere between an independent living community and a skilled nursing facility in terms of the level of care provided. Continuing care retirement facilities combine independent living, assisted living, and nursing care in one facility.
People who live in newer assisted living facilities usually have their own private apartment. There is usually no special medical monitoring equipment that one would find in a nursing home, and their nursing staff may not be available at all hours. However, trained staff are usually on-site around the clock to provide other needed services. Household chores are performed: sheets are changed, laundry is done, and food is cooked and served as part of the base rent and included services.
Depending on their disclosure of services, assisted living services may include medication management, bathing assistance, dressing, escorts to meals and activities, toileting, transferring, and insulin injections by an RN.
Some assisted living providers also offer amenities like exercise rooms or a beauty parlor on site. Grocery service is often available too. Where provided, private apartments generally are self-contained; i.e., they have their own bedroom and bathroom, and may have a separate living area or small kitchen.
Registered nurses and licensed practical nurses are available by phone or e-mail 24 hours a day, to ensure proper teaching and/or education of staff is available.
Alternatively, individual living spaces may resemble a dormitory or hotel room consisting of a private or semi-private sleeping area and a shared bathroom. There are usually common areas for socializing, as well as a central kitchen and dining room for preparing and eating meals.
Typical resident:
An assisted living resident is defined as a resident who needs assistance with at least one of the activities of daily living.
A typical assisted living facility resident would usually be an older adult who does not need the level of care offered by a nursing home but prefers more companionship and needs some assistance in day-to-day living. Age groups will vary with every facility.
There is currently a transformation occurring in long-term care. Assisted living communities are accepting higher and higher levels of care and nursing homes are becoming a place for those who are undergoing rehabilitation after a hospital stay or who need extensive assistance. Many assisted living communities now accept individuals who need assistance with all activities of daily living.
The "Overview of Assisted Living Report" from 2010 stated that:
Special needs:
The residence may assist in arranging the appropriate medical, health, and dental care services for each resident. The resident generally chooses his or her medical doctor and dental services.
Residents who have periods of temporary incapacity due to illness, injury, or recuperation from surgery often choose assisted living as a supportive option to help them recover quickly so they can return home. In the case of these short-term respite stays, assisted living residences act as the bridge between hospital and home.
Short-term respite stays in assisted living are also an option for families when the primary caregiver goes out of town or is otherwise unable to provide the needed care.
More recently built facilities are designed with an emphasis on ease of use for disabled people. Bathrooms and kitchens are designed with wheelchairs and walkers in mind.
Hallways and doors are extra-wide to accommodate wheelchairs. These facilities are by necessity fully compliant with the Americans with Disabilities Act of 1990 (ADA) or similar legislation elsewhere.
The socialization aspects of ALFs are very beneficial to the occupants. Normally the facility has many activities scheduled for the occupants, keeping in mind different disabilities and needs.
Locked units:
Many ALFs also serve the needs of people with some form of dementia including Alzheimer's disease and others with mental disabilities, as long as they do not present an imminent danger to themselves or others.
The sections of the building where these residents live are often referred to as memory care.
In the United States, legislation enacted by each state defines not only the level of care, but often what conditions are prohibited from being cared for in such a home.
In California, these units are not "locked" they are secured by alarms, delays, keypads needing a code, etc. However, they are not locked units like a psychiatric ward.
Many ALFs will work to accommodate a person with severe forms of Alzheimer's by having separate private units. These specialized care areas are part of the main building but are secured so residents with Alzheimer's cannot leave and possibly do harm to themselves.
These care areas usually house fewer people and more attention from the caregivers is provided.
The units, usually called locked units, focus on applying cognitive and mental activities to try to help keep the mind fresh. Since there is no cure for the disease, the goal is to work at prolonging or delaying the disease. If one is not engaged in activity, his or her memory will deteriorate more rapidly.
Controversy:
2011 Miami Herald investigation:
A 2011 investigation by the Miami Herald into assisted living facilities in Florida won the Pulitzer Prize, and found that:
The investigation found dozens of incidents of gross mismanagement and criminal behavior at assisted living facilities across Florida, a state of 20 million people which is popular with American retirees. The newspaper requested the release of state documents related to the deaths of over 300 people in assisted living facilities between 2003 and 2011 but were denied these documents.
Still, the newspaper's investigation found no less than 70 people who had died due to the "actions of their caregivers." The deaths were found to have resulted from the mismanagement of assisted living facilities and by the practices of their staff and managers who drugged residents, deprived them of basic necessities such as food and water, abused residents verbally, psychologically and physically, and neglecting their needs.
2013 Frontline investigation:
On July 30, 2013 Frontline ran an hour long program with help from ProPublica detailing some tragedies that happened in assisted living.
At the time the documentary was broadcast and published, Frontline stated that, "Today, nearly 750,000 people live in assisted living facilities across the country. National for-profit chains, concerned both about caring for their residents and pleasing their shareholders, have come to dominate the industry.
Standards for care and training—and even definitions for the term 'assisted living'—vary from state to state. Assisted living facilities, unlike nursing homes, are not regulated by the federal government." An accompanying written brief cites deaths of residents, facilities that are understaffed, employees that are inadequately trained, and that an overall "push to fill facilities and maximize revenues has left staff overwhelmed and the care of residents endangered."
A related article by ProPublica (Thomson and Jones, July 29, 2013) states that a facility operated by Emeritus Senior Living "...had been found wanting in almost every important regard. And, in truth, those 'specially trained' staffers hadn't actually been trained to care for people with Alzheimer's and other forms of dementia, a violation of California law."
It goes on to say, "The facility relied on a single nurse to track the health of its scores of residents, and the few licensed medical professionals who worked there tended not to last long," but also that "During some stretches, the facility went months without a full-time nurse on the payroll." ProPublica's article claimed the problem was not specific to one facility and that "State inspectors for years had cited Emeritus facilities across California."
Emeritus replied to that claim, describing "any shortcomings as isolated," as well as that "any problems that arise are promptly addressed." The company cited their "growing popularity as evidence of consumer satisfaction."
Comparison between assisted living and personal care:
In Pennsylvania, personal care and assisted living are terms that are defined separately.
Personal care and assisted living in PA are regulated by the Pennsylvania Bureau of Human Services Licensing (a division of the Department of Human Services).
Up until January 2011, the terms "assisted living" and "personal care" were considered interchangeable. At that time, Pennsylvania began licensing assisted living facilities separately from personal care facilities.
Chapter 2800 of the 55 Pennsylvania Code defines assisted living as "a significant long-term care alternative to allow individuals to age in place," where residents "will receive the assistance they need to age in place and develop and maintain maximum independence, exercise decision-making and personal choice."
Likewise, Chapter 2600 of the 55 Pa. Code defines personal care as "A premise in which food, shelter and personal assistance or supervision are provided for a period exceeding 24 hours, for four or more adults who are not relatives of the operator, who do not require the services in or of a licensed long-term care facility, but who do require assistance or supervision in activities of daily living or instrumental activities of daily living."
The differences between the two levels of care is broken down into three categories:
See also:
Nursing homes
A nursing home is a facility for the residential care of older people, senior citizens, or disabled people. Nursing homes may also be referred to as care homes, skilled nursing facilities (SNF) or long-term care facilities.
Often, these terms have slightly different meanings to indicate whether the institutions are public or private, and whether they provide mostly assisted living, or nursing care and emergency medical care.
Nursing homes are used by people who do not need to be in a hospital, but cannot be cared for at home. The nursing home facility nurses have the responsibilities of caring for the patients' medical needs and also the responsibility of being in charge of other employees, depending on their ranks. Most nursing homes have nursing aides and skilled nurses on hand 24 hours a day.
In the United States, while nearly 1 in 10 residents aged 75 to 84 stays in a nursing home for five or more years, nearly 3 in 10 residents in that age group stay less than 100 days, the maximum duration covered by Medicare, according to the American Association for Long-Term Care Insurance.
Some nursing homes also provide short-term rehabilitative stays following surgery, illness, or injury.
Services may include physical therapy, occupational therapy, or speech-language therapy. Nursing homes also offer other services, such as planned activities and daily housekeeping. Nursing homes may offer memory care services, often called dementia care.
Considerations:
Below are a few reasons to consider a nursing home:
When looking into nursing homes, consider what activities and/or medical needs patients one would need from the nursing home. Also consider finances, such as medical insurance and personal funds.
Ensure the nursing home is properly licensed and has qualified staff. If time allows, visit the nursing home in person to receive a walk through of the facility and if given the opportunity to speak with a guest or family member of guest, ask about their experience thus far.
Staff:
Nursing home employees are all required to be licensed or uphold a certificate in the state of which they work. In most facilities, nursing homes are required to provide enough staff to adequately care for residents.
In the U.S., for instance, nursing homes must have at least one registered nurse (RN) available for at least 8 straight hours a day throughout the week, and at least one licensed practical nurse (LPN) on duty 24 hours a day. Direct care nursing home employees usually include registered nurses, licensed practical nurses, social workers, certified nursing assistants, and physical therapists, amongst others.
Medical staff:
Nurses:
Main article: Nursing
Nursing homes require assessment and monitoring of residents by a registered nurse (RN) who is typically required to have between two and six years of education. The RN's job duties include:
RNs are not required to choose a specialization. To gain recognition as a specialized nurse professional, RNs typically need education in their specialized field, and further experience through clinical practices. LPNs are typically required to have a year of training before working with any patients.
The LPN monitors residents' well-being and administers treatments and medications, such as dressing wounds and dispensing prescribed drugs. LPNs are responsible for patients' direct bed care and carry out a daily routine.
Nursing assistants:
A nursing assistant provides basic care to patients while working directly under a LPN or RN. These basic care activities, also referred to as activities of daily living, can include assisting with bathing and dressing residents, helping residents with meals, either serving them or with feeding, transferring to and from the bed or wheelchair, making and cleaning beds, assisting with toileting, and answering call lights.
Nursing assistants' official titles can vary between jurisdictions and facilities. They can include Certified Nursing Assistants (CNAs), nursing aides, caregivers, patient care associates, patient care technicians, personal care attendants (PCAs), and care assistants.
Physicians:
At skilled nursing facilities, in addition to required 24 hour skilled nursing, a licensed physician supervises individual patients. At nursing homes other than skilled nursing facilities, patients receive care from physicians not affiliated with the nursing home.
These physicians are typically employed by a private agency that sends physicians to nursing homes per the request of the patient, nursing home, or patient's family. The majority of these physicians are family medicine doctors or internists; however, some specialists such as cardiologist or nephrologist may also make independent visits to supplement their care.
Non-medical staff:
Administration:
Depending on the size of the nursing home, a nursing home may have either a nursing home administrator or an executive director. Some nursing homes may have both, but their job duties are similar and can include overseeing staff, supplying medical supplies, and financial matters.
Some nursing homes also have human resources personnel, who are in charge of all aspects of hiring new employees. Human resources job duties vary but can also include coordinating payroll, organizing orientation programs for new employees, interviewing, disciplinary actions, and ensuring compliance with federal and state laws.
Nursing homes are usually licensed and heavily regulated under governing legislation. Compliance with the federal and state legislatures are reviewed regularly for adherence to strict standards of building codes, care plans, behavior and altercations between residents, nutrition and dietary services, medical services, nursing and personal care, religious and spiritual practices, pets, and recreational programs.
Housekeeping:
Housekeepers perform everyday cleaning and upkeep in nursing homes. They play a huge part in ensuring that nursing homes are kept clean and free of disease causing agents.
Housekeepers have a long list of duties which include cleaning floors, changing linens, disinfecting bathrooms, changing towels, washing clothes, emptying trashcans, sanitizing rooms, replenishing supplies, dusting, vacuuming, and keeping windows and woodwork clean.
These duties can vary from facility to facility but it will overall include basic cleaning. Housekeeping does not require any licensure or schooling, but some jobs may prefer experienced housekeepers.
Recreational staff:
Recreational staff usually include an activity director and possibly activity assistants depending on the size of the nursing home. Activities aim to meet each resident's emotional, intellectual, physical, social, spiritual, and vocational needs.
The transition from being independent to having to depend on others and be away from home is oftentimes very difficult, which is why activities are important to combat depression and anxiety.
Some of the different activities that may be offered include hosting birthday parties, celebrating holidays, book clubs, musical events, outdoor activities, discussion and social groups, exercise, arts and crafts, pet therapy, religious services and community outings.
Volunteer involvement is also an important part of nursing home activities given that volunteers can act as a link between the nursing home and the outside community.
Therapy:
Occupational therapy:
One of the many services offered in a nursing home is occupational therapy. Occupational therapy may be necessary following an injury or illness in order to regain skills and to receive support during any physical or cognitive changes.
Occupational therapy will focus on activities of daily living such as bathing, dressing, grooming. Occupational therapy also assists with instrumental activities of daily living which include home and financial management, rest and sleep, education, work, play, leisure, and social participation.
Occupational therapists work to allow the person to safely and comfortably reintegrate into society by practicing public dining, transferring to different surfaces (chairs, beds, couches etc.), and will assess the need for any home modifications or safety equipment to ensure a proper and safe transition.
When a cognitive and/or perceptual deficit is presented, therapists will work with the person by teaching strategies to maximize memory, sequencing and attention span length.
Physical therapy:
Another important service found in a nursing home is physical therapy. Physical therapy may be necessary following an injury, illness or surgery. Physical therapy works with the person to help them regain strength, endurance, flexibility, balance and range of motion.
Physical therapy is also used as a way of preventing injuries and accidents by focusing on restoring mobility, increasing fitness levels, reducing pain and overall reaching a certain point of independence.
There are many conditions that can benefit from receiving physical therapy in a nursing home, these conditions include:
Speech language therapy:
Speech-language pathology is another service found in a nursing home. Speech language pathologists specialize in working with those who have a difficult time with language and/or speech, usually following an injury or an underlying diagnoses. The SLP will evaluate the person's speech.
If the person is having trouble with speech, this points to an issue with coordinating the movements and muscles used to produce speech. Trouble with language points to the person having difficulty with understanding what they are hearing and seeing. The SLP will also look at difficulty with swallowing food and will evaluate the person in order to figure out which part of the swallowing process is not working.
Some of the many speech disorders worked with by the SLP are:
Elder abuse:
Main article: Elder abuse
Elder abuse is more prevalent in hospitalized settings including nursing homes than in the general community. There are three major types of abuses reported in nursing homes: physical, emotional, and sexual abuse.
Nursing home neglect is similar to elder abuse. It is when employees begin to repeatedly ignore and leave a patient alone, neglect the patient's personal hygiene like bathing and brushing of teeth, provide the patient with an inadequate amount of food and water, or neglect to provide the patient with the correct amount of medication they require.
One factor unique to elder abuse in nursing homes is that many nursing home contracts require residents to sign delegation clauses, giving up their right to trial by jury and instead using an arbitrator to settle disputes.
United States:
Main article: Nursing home care in the United States
In the United States, there are three main types of nursing facilities (NFs).
An intermediate care facility (ICF) is a health care facility for individuals who are disabled, elderly, or non-acutely ill, usually providing less intensive care than that offered at a hospital or skilled nursing facility.
Typically an ICF is privately paid by the individual or by the individual's family. An individual's private health insurance and/or a third party service like a hospice company may cover the cost.
Board and Care Homes are special facilities designed to provide those who require assisted living services both living quarters and proper care. Often referred to as residential care homes, these facilities can either be located in a small residential home or a large modern facility. In fact, a large majority of board and care homes are designed to accommodate fewer than 6 people.
Board and care homes are typically staffed by licensed professionals, including nurses, doctors and other medical professionals. These facilities are highly regulated in order to ensure that the best possible care is being provided for the residents. Board and care homes offer residents 24-hour assistance, making them a highly popular choice for those in need of regular assistance.
Assisted living residences or assisted living facilities (ALFs) are housing facilities for people with disabilities. These facilities provide supervision or assistance with activities of daily living (ADL); ALFs are an elder-care alternative on the continuum of care for people, for whom independent living is not appropriate but who do not need the 24-hour medical care provided by a nursing home and are too young to live in a retirement home. Assisted living is a philosophy of care and services promoting independence and dignity.
A skilled nursing facility (SNF) is a nursing home certified to participate in, and be reimbursed by Medicare. Medicare is the federal program primarily for the aged (65+) who contributed to Social Security and Medicare while they were employed.
Medicaid is the federal program implemented with each state to provide health care and related services to those who are below the poverty line. Each state defines poverty and therefore Medicaid eligibility. Those eligible for Medicaid may be low-income parents, children (including those in State Children's Health Insurance Programs (SCHIPs) and maternal-child wellness and food programs), seniors, and people with disabilities.
The Centers for Medicare and Medicaid Services is the component of the U.S. Department of Health and Human Services (DHHS) that oversees Medicare and Medicaid. A large portion of Medicare and Medicaid dollars is used each year to cover nursing home care and services for the elderly and disabled.
State governments oversee the licensing of nursing homes. In addition, states have a contract with CMS to monitor those nursing homes that want to be eligible to provide care to Medicare and Medicaid beneficiaries. Congress established minimum requirements for nursing homes that want to provide services under Medicare and Medicaid.
These requirements are broadly outlined in the Social Security Act, which also entrusts the Secretary of Health and Human Services with the responsibility of monitoring and enforcing these requirements. CMS is also charged with the responsibility of working out the details of the law and how it will be implemented, which it does by writing regulations and manuals.
See also:
Independent Senior Living
Senior living
Senior living is a concept that encompasses a range of housing and lifestyle options for ageing persons adapted to the challenges of health issues associated with ageing, such as limited mobility and susceptibility to illness.
Common forms:
Based on the health and financial means of the individual, these may include living in a retirement community or an age-restricted community, independent senior living, or living in a nursing home or retirement home.
A retirement community is a residential community or housing complex designed for older adults who are generally able to care for themselves; however, assistance from home care agencies is allowed in some communities, and activities and socialization opportunities are often provided. Some of the characteristics typically are: the community must be age-restricted or age-qualified, residents must be partially or fully retired, and the community offers shared services or amenities.
An age-restricted community is a residential community, often gated, that typically limits 80% of the residency to individuals who are over a set age. The minimum age is frequently set at 55 years old, but it can vary. These communities are set up to accommodate older individuals who would like to live in an area without the perceived problems of having children around. In most cases a younger spouse or significant other is permitted to live in the community as long as one member meets the minimum age requirement.
Age-qualified communities, also known as 55+ communities, active adult communities, lifestyle communities, or retirement communities, are often planned communities that offer homes and community features that are attractive to 55+ adults. These might include a clubhouse or lifestyle center with a good many activities, sometimes with indoor and outdoor swimming pools, exercise facilities, craft rooms, demonstration kitchens, and decks and patios for gathering.
Independent senior living communities commonly provide apartments, but some also offer cottages, condominiums, and single-family homes. Residents include seniors who do not require assistance with daily activities or 24/7 skilled nursing, but may benefit from convenient services, senior-friendly surroundings, and increased social opportunities that independent senior living communities offer.
Independent senior living properties do not provide health care or assistance with activities of daily living (ADLs) such as medication, bathing, eating, dressing, toileting and more.
Independent senior living differs from continuing care communities, which offer independent living along with multiple other levels of care, such as assisted living and skilled nursing, in one single residence.
A retirement home is a multi-residence housing facility intended for the elderly. The concept is sometimes called an old people's home, old folks' home, or old age home, although old people's home can also refer to a nursing home. Typically, each person or couple in the home has an apartment-style room or suite of rooms.
Additional facilities are provided within the building. This can include facilities for meals, gatherings, recreation activities, and some form of health or hospice care. A place in a retirement home can be paid for on a rental basis, like an apartment, or can be bought in perpetuity on the same basis as a condominium.
___________________________________________________________________________
Assisted living
An assisted living residence or assisted living facility (ALF) is a housing facility for people with disabilities or for adults who cannot or who choose not to live independently. The term is popular in the United States, but the setting is similar to a retirement home, in the sense that facilities provide a group living environment and typically cater to an older adult population. There is also Caribbean assisted living, which offers a similar service in a resort-like environment (somewhat like assisted vacationing).
The expansion of assisted living has been the shift from "care as service" to "care as business" in the broader health care system predicted in 1982. A consumer-driven industry, assisted living offers a wide range of options, levels of care, and diversity of services (Lockhart, 2009) and is subject to state rather than federal regulatory oversight.
What "Assisted living" means depends on both the state and provider in question: variations in state regulatory definitions are significant and provider variables include everything from philosophy, geographic location and auspice, to organizational size and structure.
Assisted living evolved from small "board and care" or "personal care" homes and offers a "social model" of care (compared to the medical model of a skilled nursing facility). The assisted living industry is a segment of the senior housing industry and assisted living services can be delivered in stand-alone facilities or as part of multi-level senior living community.
The industry is fragmented and dominated by for-profit providers. In 2010, six of the seventy largest providers were non-profit and none of the top twenty was non-profit (Martin, 2010). Information in this edit is from an article published in 2012 that reviewed the industry and reports results of a research study of assisted living facilities.
In 2012 the U.S. Government estimated that there were 22,200 assisted living facilities in the U.S. (compared to 15,700 nursing homes) and that 713,300 people were residents of these facilities. The number of assisted living facilities in the U.S. has increased dramatically since the early 2000s.
In the U.S., ALFs can be owned by for-profit companies (publicly traded companies or limited liability companies [LLCs]), non-profit organizations, or governments. These facilities typically provide supervision or assistance with activities of daily living (ADLs); coordination of services by outside health care providers; and monitoring of resident activities to help to ensure their health, safety, and well-being. Assistance often includes the administration or supervision of medication, or personal care services.
There has been controversy generated by reports of neglect, abuse and mistreatment of residents at assisted living facilities in the U.S.
Within the United States assisted living spectrum, there is no nationally recognized definition of assisted living. Assisted living facilities are regulated and licensed at the US state level. These regulations include staffing, training, and quality and safety standards.
This is differentiated from nursing homes, which are regulated on a federal level and are generally held to more stringent standards. More than two-thirds of the states use the licensure term "assisted living." Other licensure terms used for this philosophy of care include residential care home, assisted care living facilities, and personal care homes. Each state licensing agency has its own definition of the term it uses to describe assisted living.
Because the term assisted living has not been defined in some states it is often a marketing term used by a variety of senior living communities, licensed or unlicensed. Assisted living facilities in the United States had a national median monthly rate of $3,500.00 in 2014, a 1.45% increase over 2013 and a 4.29% increase over a five-year period from 2009 to 2014.
Types:
As widely varied as the state licensing and definitions are, so are the types of physical layouts of buildings in which assisted living services are provided.
The average assisted living facility is in a commercial building, yet some assisted living services use large residential buildings, known as Residential Assisted Living homes, or "RAL".
Residential Assisted Living homes can vary in price and amenities, and can even be grouped into a separate term known as a Luxury Residential Assisted Living Home, or "LRAL".
Assisted living facilities can range in size from a small residential house for one resident up to very large facilities providing services to hundreds of residents. Assisted living falls somewhere between an independent living community and a skilled nursing facility in terms of the level of care provided. Continuing care retirement facilities combine independent living, assisted living, and nursing care in one facility.
People who live in newer assisted living facilities usually have their own private apartment. There is usually no special medical monitoring equipment that one would find in a nursing home, and their nursing staff may not be available at all hours. However, trained staff are usually on-site around the clock to provide other needed services. Household chores are performed: sheets are changed, laundry is done, and food is cooked and served as part of the base rent and included services.
Depending on their disclosure of services, assisted living services may include medication management, bathing assistance, dressing, escorts to meals and activities, toileting, transferring, and insulin injections by an RN.
Some assisted living providers also offer amenities like exercise rooms or a beauty parlor on site. Grocery service is often available too. Where provided, private apartments generally are self-contained; i.e., they have their own bedroom and bathroom, and may have a separate living area or small kitchen.
Registered nurses and licensed practical nurses are available by phone or e-mail 24 hours a day, to ensure proper teaching and/or education of staff is available.
Alternatively, individual living spaces may resemble a dormitory or hotel room consisting of a private or semi-private sleeping area and a shared bathroom. There are usually common areas for socializing, as well as a central kitchen and dining room for preparing and eating meals.
Typical resident:
An assisted living resident is defined as a resident who needs assistance with at least one of the activities of daily living.
A typical assisted living facility resident would usually be an older adult who does not need the level of care offered by a nursing home but prefers more companionship and needs some assistance in day-to-day living. Age groups will vary with every facility.
There is currently a transformation occurring in long-term care. Assisted living communities are accepting higher and higher levels of care and nursing homes are becoming a place for those who are undergoing rehabilitation after a hospital stay or who need extensive assistance. Many assisted living communities now accept individuals who need assistance with all activities of daily living.
The "Overview of Assisted Living Report" from 2010 stated that:
- 54 percent of assisted living residents are 85 years or older;
- 27 percent are 75–84 years old;
- 9 percent of residents are between 65 and 74 years;
- and 11 percent are younger than 65 years old.
- 74% of assisted living residents are female;
- 26 percent are male.
Special needs:
The residence may assist in arranging the appropriate medical, health, and dental care services for each resident. The resident generally chooses his or her medical doctor and dental services.
Residents who have periods of temporary incapacity due to illness, injury, or recuperation from surgery often choose assisted living as a supportive option to help them recover quickly so they can return home. In the case of these short-term respite stays, assisted living residences act as the bridge between hospital and home.
Short-term respite stays in assisted living are also an option for families when the primary caregiver goes out of town or is otherwise unable to provide the needed care.
More recently built facilities are designed with an emphasis on ease of use for disabled people. Bathrooms and kitchens are designed with wheelchairs and walkers in mind.
Hallways and doors are extra-wide to accommodate wheelchairs. These facilities are by necessity fully compliant with the Americans with Disabilities Act of 1990 (ADA) or similar legislation elsewhere.
The socialization aspects of ALFs are very beneficial to the occupants. Normally the facility has many activities scheduled for the occupants, keeping in mind different disabilities and needs.
Locked units:
Many ALFs also serve the needs of people with some form of dementia including Alzheimer's disease and others with mental disabilities, as long as they do not present an imminent danger to themselves or others.
The sections of the building where these residents live are often referred to as memory care.
In the United States, legislation enacted by each state defines not only the level of care, but often what conditions are prohibited from being cared for in such a home.
In California, these units are not "locked" they are secured by alarms, delays, keypads needing a code, etc. However, they are not locked units like a psychiatric ward.
Many ALFs will work to accommodate a person with severe forms of Alzheimer's by having separate private units. These specialized care areas are part of the main building but are secured so residents with Alzheimer's cannot leave and possibly do harm to themselves.
These care areas usually house fewer people and more attention from the caregivers is provided.
The units, usually called locked units, focus on applying cognitive and mental activities to try to help keep the mind fresh. Since there is no cure for the disease, the goal is to work at prolonging or delaying the disease. If one is not engaged in activity, his or her memory will deteriorate more rapidly.
Controversy:
2011 Miami Herald investigation:
A 2011 investigation by the Miami Herald into assisted living facilities in Florida won the Pulitzer Prize, and found that:
- "the safeguards once hailed as the most progressive in the nation have been ignored in a string of tragedies never before revealed to the public,"
- "that the Agency for Health Care Administration, which oversees the state's 2,850 assisted-living facilities, has failed to monitor shoddy operators, investigate dangerous practices or shut down the worst offenders," and
- "as the ranks of assisted-living facilities grew to make room for Florida's booming elderly population, the state failed to protect the people it was meant to serve."
The investigation found dozens of incidents of gross mismanagement and criminal behavior at assisted living facilities across Florida, a state of 20 million people which is popular with American retirees. The newspaper requested the release of state documents related to the deaths of over 300 people in assisted living facilities between 2003 and 2011 but were denied these documents.
Still, the newspaper's investigation found no less than 70 people who had died due to the "actions of their caregivers." The deaths were found to have resulted from the mismanagement of assisted living facilities and by the practices of their staff and managers who drugged residents, deprived them of basic necessities such as food and water, abused residents verbally, psychologically and physically, and neglecting their needs.
2013 Frontline investigation:
On July 30, 2013 Frontline ran an hour long program with help from ProPublica detailing some tragedies that happened in assisted living.
At the time the documentary was broadcast and published, Frontline stated that, "Today, nearly 750,000 people live in assisted living facilities across the country. National for-profit chains, concerned both about caring for their residents and pleasing their shareholders, have come to dominate the industry.
Standards for care and training—and even definitions for the term 'assisted living'—vary from state to state. Assisted living facilities, unlike nursing homes, are not regulated by the federal government." An accompanying written brief cites deaths of residents, facilities that are understaffed, employees that are inadequately trained, and that an overall "push to fill facilities and maximize revenues has left staff overwhelmed and the care of residents endangered."
A related article by ProPublica (Thomson and Jones, July 29, 2013) states that a facility operated by Emeritus Senior Living "...had been found wanting in almost every important regard. And, in truth, those 'specially trained' staffers hadn't actually been trained to care for people with Alzheimer's and other forms of dementia, a violation of California law."
It goes on to say, "The facility relied on a single nurse to track the health of its scores of residents, and the few licensed medical professionals who worked there tended not to last long," but also that "During some stretches, the facility went months without a full-time nurse on the payroll." ProPublica's article claimed the problem was not specific to one facility and that "State inspectors for years had cited Emeritus facilities across California."
Emeritus replied to that claim, describing "any shortcomings as isolated," as well as that "any problems that arise are promptly addressed." The company cited their "growing popularity as evidence of consumer satisfaction."
Comparison between assisted living and personal care:
In Pennsylvania, personal care and assisted living are terms that are defined separately.
Personal care and assisted living in PA are regulated by the Pennsylvania Bureau of Human Services Licensing (a division of the Department of Human Services).
Up until January 2011, the terms "assisted living" and "personal care" were considered interchangeable. At that time, Pennsylvania began licensing assisted living facilities separately from personal care facilities.
Chapter 2800 of the 55 Pennsylvania Code defines assisted living as "a significant long-term care alternative to allow individuals to age in place," where residents "will receive the assistance they need to age in place and develop and maintain maximum independence, exercise decision-making and personal choice."
Likewise, Chapter 2600 of the 55 Pa. Code defines personal care as "A premise in which food, shelter and personal assistance or supervision are provided for a period exceeding 24 hours, for four or more adults who are not relatives of the operator, who do not require the services in or of a licensed long-term care facility, but who do require assistance or supervision in activities of daily living or instrumental activities of daily living."
The differences between the two levels of care is broken down into three categories:
- Concept – Assisted living residences permit residents to age in place, meaning that even as their health care needs increase, they will not have to relocate to another senior living home to receive that care, such as skilled nursing.
- Construction – Assisted living residences must provide residents a private room with a lockable door, a private bathroom and small kitchen. Personal care homes are not required to offer these amenities.
- Level of Care – Assisted living residences must ensure that residents receive skilled nursing care if their needs surpass standard assisted living services.
See also:
- Aging in place
- Eldercare
- Food preferences in older adults and seniors
- Retirement home
- Group home
- Retirement community
- Transgenerational design
- Assistive technology
Nursing homes
- Click here for a List of companies operating nursing homes
- Click here for a List of Nursing home residents' rights
A nursing home is a facility for the residential care of older people, senior citizens, or disabled people. Nursing homes may also be referred to as care homes, skilled nursing facilities (SNF) or long-term care facilities.
Often, these terms have slightly different meanings to indicate whether the institutions are public or private, and whether they provide mostly assisted living, or nursing care and emergency medical care.
Nursing homes are used by people who do not need to be in a hospital, but cannot be cared for at home. The nursing home facility nurses have the responsibilities of caring for the patients' medical needs and also the responsibility of being in charge of other employees, depending on their ranks. Most nursing homes have nursing aides and skilled nurses on hand 24 hours a day.
In the United States, while nearly 1 in 10 residents aged 75 to 84 stays in a nursing home for five or more years, nearly 3 in 10 residents in that age group stay less than 100 days, the maximum duration covered by Medicare, according to the American Association for Long-Term Care Insurance.
Some nursing homes also provide short-term rehabilitative stays following surgery, illness, or injury.
Services may include physical therapy, occupational therapy, or speech-language therapy. Nursing homes also offer other services, such as planned activities and daily housekeeping. Nursing homes may offer memory care services, often called dementia care.
Considerations:
Below are a few reasons to consider a nursing home:
- managing a worsening and progressive disease such as Alzheimers
- after a recent hospital admission and not ready to transition to independently caring for oneself at home
- when medical needs at home become unmanageable by the primary caregiver at home.
When looking into nursing homes, consider what activities and/or medical needs patients one would need from the nursing home. Also consider finances, such as medical insurance and personal funds.
Ensure the nursing home is properly licensed and has qualified staff. If time allows, visit the nursing home in person to receive a walk through of the facility and if given the opportunity to speak with a guest or family member of guest, ask about their experience thus far.
Staff:
Nursing home employees are all required to be licensed or uphold a certificate in the state of which they work. In most facilities, nursing homes are required to provide enough staff to adequately care for residents.
In the U.S., for instance, nursing homes must have at least one registered nurse (RN) available for at least 8 straight hours a day throughout the week, and at least one licensed practical nurse (LPN) on duty 24 hours a day. Direct care nursing home employees usually include registered nurses, licensed practical nurses, social workers, certified nursing assistants, and physical therapists, amongst others.
Medical staff:
Nurses:
Main article: Nursing
Nursing homes require assessment and monitoring of residents by a registered nurse (RN) who is typically required to have between two and six years of education. The RN's job duties include:
- implementing care plans,
- administering medications,
- recording and maintaining accurate reports for each resident,
- monitoring and recording medical changes,
- and providing direction to the nursing assistants and licensed practical nurses (LPN).
RNs are not required to choose a specialization. To gain recognition as a specialized nurse professional, RNs typically need education in their specialized field, and further experience through clinical practices. LPNs are typically required to have a year of training before working with any patients.
The LPN monitors residents' well-being and administers treatments and medications, such as dressing wounds and dispensing prescribed drugs. LPNs are responsible for patients' direct bed care and carry out a daily routine.
Nursing assistants:
A nursing assistant provides basic care to patients while working directly under a LPN or RN. These basic care activities, also referred to as activities of daily living, can include assisting with bathing and dressing residents, helping residents with meals, either serving them or with feeding, transferring to and from the bed or wheelchair, making and cleaning beds, assisting with toileting, and answering call lights.
Nursing assistants' official titles can vary between jurisdictions and facilities. They can include Certified Nursing Assistants (CNAs), nursing aides, caregivers, patient care associates, patient care technicians, personal care attendants (PCAs), and care assistants.
Physicians:
At skilled nursing facilities, in addition to required 24 hour skilled nursing, a licensed physician supervises individual patients. At nursing homes other than skilled nursing facilities, patients receive care from physicians not affiliated with the nursing home.
These physicians are typically employed by a private agency that sends physicians to nursing homes per the request of the patient, nursing home, or patient's family. The majority of these physicians are family medicine doctors or internists; however, some specialists such as cardiologist or nephrologist may also make independent visits to supplement their care.
Non-medical staff:
Administration:
Depending on the size of the nursing home, a nursing home may have either a nursing home administrator or an executive director. Some nursing homes may have both, but their job duties are similar and can include overseeing staff, supplying medical supplies, and financial matters.
Some nursing homes also have human resources personnel, who are in charge of all aspects of hiring new employees. Human resources job duties vary but can also include coordinating payroll, organizing orientation programs for new employees, interviewing, disciplinary actions, and ensuring compliance with federal and state laws.
Nursing homes are usually licensed and heavily regulated under governing legislation. Compliance with the federal and state legislatures are reviewed regularly for adherence to strict standards of building codes, care plans, behavior and altercations between residents, nutrition and dietary services, medical services, nursing and personal care, religious and spiritual practices, pets, and recreational programs.
Housekeeping:
Housekeepers perform everyday cleaning and upkeep in nursing homes. They play a huge part in ensuring that nursing homes are kept clean and free of disease causing agents.
Housekeepers have a long list of duties which include cleaning floors, changing linens, disinfecting bathrooms, changing towels, washing clothes, emptying trashcans, sanitizing rooms, replenishing supplies, dusting, vacuuming, and keeping windows and woodwork clean.
These duties can vary from facility to facility but it will overall include basic cleaning. Housekeeping does not require any licensure or schooling, but some jobs may prefer experienced housekeepers.
Recreational staff:
Recreational staff usually include an activity director and possibly activity assistants depending on the size of the nursing home. Activities aim to meet each resident's emotional, intellectual, physical, social, spiritual, and vocational needs.
The transition from being independent to having to depend on others and be away from home is oftentimes very difficult, which is why activities are important to combat depression and anxiety.
Some of the different activities that may be offered include hosting birthday parties, celebrating holidays, book clubs, musical events, outdoor activities, discussion and social groups, exercise, arts and crafts, pet therapy, religious services and community outings.
Volunteer involvement is also an important part of nursing home activities given that volunteers can act as a link between the nursing home and the outside community.
Therapy:
Occupational therapy:
One of the many services offered in a nursing home is occupational therapy. Occupational therapy may be necessary following an injury or illness in order to regain skills and to receive support during any physical or cognitive changes.
Occupational therapy will focus on activities of daily living such as bathing, dressing, grooming. Occupational therapy also assists with instrumental activities of daily living which include home and financial management, rest and sleep, education, work, play, leisure, and social participation.
Occupational therapists work to allow the person to safely and comfortably reintegrate into society by practicing public dining, transferring to different surfaces (chairs, beds, couches etc.), and will assess the need for any home modifications or safety equipment to ensure a proper and safe transition.
When a cognitive and/or perceptual deficit is presented, therapists will work with the person by teaching strategies to maximize memory, sequencing and attention span length.
Physical therapy:
Another important service found in a nursing home is physical therapy. Physical therapy may be necessary following an injury, illness or surgery. Physical therapy works with the person to help them regain strength, endurance, flexibility, balance and range of motion.
Physical therapy is also used as a way of preventing injuries and accidents by focusing on restoring mobility, increasing fitness levels, reducing pain and overall reaching a certain point of independence.
There are many conditions that can benefit from receiving physical therapy in a nursing home, these conditions include:
- arthritis,
- pain associated with cancer,
- dementia,
- Alzheimer's,
- stroke
- and incontinence.
Speech language therapy:
Speech-language pathology is another service found in a nursing home. Speech language pathologists specialize in working with those who have a difficult time with language and/or speech, usually following an injury or an underlying diagnoses. The SLP will evaluate the person's speech.
If the person is having trouble with speech, this points to an issue with coordinating the movements and muscles used to produce speech. Trouble with language points to the person having difficulty with understanding what they are hearing and seeing. The SLP will also look at difficulty with swallowing food and will evaluate the person in order to figure out which part of the swallowing process is not working.
Some of the many speech disorders worked with by the SLP are:
- phonology meaning the speech patterns used,
- apraxia meaning difficulty with coordinating the movements needed to make sounds,
- receptive language meaning difficulty understanding language,
- fluency meaning stuttering,
- expressive language meaning difficulty using language, and many other disorders.
Elder abuse:
Main article: Elder abuse
Elder abuse is more prevalent in hospitalized settings including nursing homes than in the general community. There are three major types of abuses reported in nursing homes: physical, emotional, and sexual abuse.
- Physical abuse is the intention or action to hurt an elderly person resulting in scars and bruising.
- Emotional abuse occurs when an employee makes verbal threats and continuously degrades the patient, resulting in the patient experiencing mood swings, anxiety, and depression.
- Sexual abuse is when an elderly patient is being forced into unwanted sexual activity by an employee, resident or visitor, usually attempted and reported when the patient is sleeping, sick, or weak.
Nursing home neglect is similar to elder abuse. It is when employees begin to repeatedly ignore and leave a patient alone, neglect the patient's personal hygiene like bathing and brushing of teeth, provide the patient with an inadequate amount of food and water, or neglect to provide the patient with the correct amount of medication they require.
One factor unique to elder abuse in nursing homes is that many nursing home contracts require residents to sign delegation clauses, giving up their right to trial by jury and instead using an arbitrator to settle disputes.
United States:
Main article: Nursing home care in the United States
In the United States, there are three main types of nursing facilities (NFs).
An intermediate care facility (ICF) is a health care facility for individuals who are disabled, elderly, or non-acutely ill, usually providing less intensive care than that offered at a hospital or skilled nursing facility.
Typically an ICF is privately paid by the individual or by the individual's family. An individual's private health insurance and/or a third party service like a hospice company may cover the cost.
Board and Care Homes are special facilities designed to provide those who require assisted living services both living quarters and proper care. Often referred to as residential care homes, these facilities can either be located in a small residential home or a large modern facility. In fact, a large majority of board and care homes are designed to accommodate fewer than 6 people.
Board and care homes are typically staffed by licensed professionals, including nurses, doctors and other medical professionals. These facilities are highly regulated in order to ensure that the best possible care is being provided for the residents. Board and care homes offer residents 24-hour assistance, making them a highly popular choice for those in need of regular assistance.
Assisted living residences or assisted living facilities (ALFs) are housing facilities for people with disabilities. These facilities provide supervision or assistance with activities of daily living (ADL); ALFs are an elder-care alternative on the continuum of care for people, for whom independent living is not appropriate but who do not need the 24-hour medical care provided by a nursing home and are too young to live in a retirement home. Assisted living is a philosophy of care and services promoting independence and dignity.
A skilled nursing facility (SNF) is a nursing home certified to participate in, and be reimbursed by Medicare. Medicare is the federal program primarily for the aged (65+) who contributed to Social Security and Medicare while they were employed.
Medicaid is the federal program implemented with each state to provide health care and related services to those who are below the poverty line. Each state defines poverty and therefore Medicaid eligibility. Those eligible for Medicaid may be low-income parents, children (including those in State Children's Health Insurance Programs (SCHIPs) and maternal-child wellness and food programs), seniors, and people with disabilities.
The Centers for Medicare and Medicaid Services is the component of the U.S. Department of Health and Human Services (DHHS) that oversees Medicare and Medicaid. A large portion of Medicare and Medicaid dollars is used each year to cover nursing home care and services for the elderly and disabled.
State governments oversee the licensing of nursing homes. In addition, states have a contract with CMS to monitor those nursing homes that want to be eligible to provide care to Medicare and Medicaid beneficiaries. Congress established minimum requirements for nursing homes that want to provide services under Medicare and Medicaid.
These requirements are broadly outlined in the Social Security Act, which also entrusts the Secretary of Health and Human Services with the responsibility of monitoring and enforcing these requirements. CMS is also charged with the responsibility of working out the details of the law and how it will be implemented, which it does by writing regulations and manuals.
See also:
- American Medical Directors Association
- Care Quality Commission
- Child care
- Elderly care
- Home care
- Retirement community
- Caring for people with dementia
Independent Senior Living
- YouTube Video: How to Find Affordable Senior Housing
- YouTube Video: Downsizing to an Independent Senior Living Community
- YouTube Video: Downsizing? Tips for moving when you're older
Independent senior living communities (also known as retirement communities, senior living communities or independent retirement communities) are housing designed for seniors 55 and older.
Independent senior living communities commonly provide apartments, but some also offer cottages, condominiums, and single-family homes. Residents include seniors who do not require assistance with daily activities or 24/7 skilled nursing, but may benefit from convenient services, senior-friendly surroundings, and increased social opportunities that independent senior living communities offer.
Independent senior living communities are also popular among snowbird seniors who wish to downsize or travel freely without the burden of managing a home.
Many retirement communities offer dining services, basic housekeeping and laundry services, transportation to appointments and errands, activities, social programs, and access to exercise equipment.
Some also offer emergency alert systems, live-in managers, and amenities like pools, spas, clubhouses, and on-site beauty and barber salons.
Independent senior living properties do not provide health care or assistance with activities of daily living (ADLs) such as medication, bathing, eating, dressing, toileting and more.
Independent senior living differs from continuing care communities, which offer independent living along with multiple other levels of care, such as assisted living and skilled nursing, in one single residence.
Independent senior living residents are permitted to use third-party home health care services to meet additional needs.
The total operational resident capacity for independent senior living communities in the United States is 245,000. Holiday Retirement is the largest single provider of independent living with a resident capacity of 40,440 at 315 retirement communities throughout the U.S. and Canada.
Types:
Typical residents:
A typical independent senior living community resident is a person 55 and older who is mentally and physically capable of living alone without skilled nursing or assistance with day-to-day activities. Some residents may need assistance with a few activities of daily living and can obtain third-party home health care services.
Seniors who may benefit from less home upkeep and increased access to nutritious meals, social interaction, physical and mental stimulation, and transportation make ideal independent senior living community residents.
Vs. assisted living:
The most significant difference between assisted living and independent senior living is the care provided. Residents of assisted living facilities require assistance with daily activities like medication, eating, bathing, dressing, and toileting.
Residents of a purpose-built independent senior living complex have taken an active decision to improve their quality of life by living in a secure, low maintenance home. Elderly people who have chosen to live in assisted retirement complex will often require more care and support to improve their quality of life.
There are around 50,000 private senior living developments in the UK alone, which is insufficient to meet the demand from an increasing number of retirees. It has been predicted that by 2020, 19.3% of the UK population will be aged 65 and a minimum of 35,000 new senior living development properties will need to be created to meet housing demands.
Independent senior living residents are able to live on their own with limited assistance (provided by third-party home health care providers if needed) and without around-the-clock supervision. Neither assisted living nor senior independent living communities offer 24/7 skilled nursing that is provided at nursing homes.
Cost:
Independent senior living communities are the least expensive of the three primary senior living options. Monthly costs vary significantly by community type, size of apartment, location and services offered. The average total cost for a U.S. one bedroom independent senior living apartment is $2,750 per month.
In 2011, the average rate for a private bedroom at a U.S. nursing home was $239 per day, or nearly $7,270 per month. Average rate for a private bedroom at an assisted living community was $3,477 per month. Continuing care communities require an entrance fee that ranges from $20,000 to $500,000, in addition to monthly fees that range from $500 to $3,000 or more depending on services.
See also:
Independent senior living communities commonly provide apartments, but some also offer cottages, condominiums, and single-family homes. Residents include seniors who do not require assistance with daily activities or 24/7 skilled nursing, but may benefit from convenient services, senior-friendly surroundings, and increased social opportunities that independent senior living communities offer.
Independent senior living communities are also popular among snowbird seniors who wish to downsize or travel freely without the burden of managing a home.
Many retirement communities offer dining services, basic housekeeping and laundry services, transportation to appointments and errands, activities, social programs, and access to exercise equipment.
Some also offer emergency alert systems, live-in managers, and amenities like pools, spas, clubhouses, and on-site beauty and barber salons.
Independent senior living properties do not provide health care or assistance with activities of daily living (ADLs) such as medication, bathing, eating, dressing, toileting and more.
Independent senior living differs from continuing care communities, which offer independent living along with multiple other levels of care, such as assisted living and skilled nursing, in one single residence.
Independent senior living residents are permitted to use third-party home health care services to meet additional needs.
The total operational resident capacity for independent senior living communities in the United States is 245,000. Holiday Retirement is the largest single provider of independent living with a resident capacity of 40,440 at 315 retirement communities throughout the U.S. and Canada.
Types:
- Senior Apartments: Most common type of independent senior living. Services usually include recreational programs, transportation, and meals service.
- Housing Units: Senior communities that offer single-family homes, duplexes, mobile homes, townhouses, cottages, or condominiums. Some communities are tied to an adjoining, apartment-style independent senior living community. Residents may have the option to rent or buy.
- Continuing Care: Communities that provide access to independent living communities, as well as assisted living and skilled nursing. Residents can transfer among levels of care as needs change. Some CCRCs also provide memory care facilities.
- Subsidized Housing: The Department of Housing and Urban Development (HUD) provides communities for low-income seniors. Subsidized communities usually adhere to strict criteria and may have lengthy waiting lists.
- Naturally Occurring Retirement Community (NORC): A community that has a large population of senior residents but was not originally designed for seniors. These evolve naturally as people age-in-place over time or migrate into the same area. They are not created to meet the needs of seniors.
- Co-Care: Residents live with three other older adults in a four-bedroom, two-bathroom unit. Each unit has a small kitchen and space for laundry, living and dining, reducing costs for middle income seniors.
Typical residents:
A typical independent senior living community resident is a person 55 and older who is mentally and physically capable of living alone without skilled nursing or assistance with day-to-day activities. Some residents may need assistance with a few activities of daily living and can obtain third-party home health care services.
Seniors who may benefit from less home upkeep and increased access to nutritious meals, social interaction, physical and mental stimulation, and transportation make ideal independent senior living community residents.
Vs. assisted living:
The most significant difference between assisted living and independent senior living is the care provided. Residents of assisted living facilities require assistance with daily activities like medication, eating, bathing, dressing, and toileting.
Residents of a purpose-built independent senior living complex have taken an active decision to improve their quality of life by living in a secure, low maintenance home. Elderly people who have chosen to live in assisted retirement complex will often require more care and support to improve their quality of life.
There are around 50,000 private senior living developments in the UK alone, which is insufficient to meet the demand from an increasing number of retirees. It has been predicted that by 2020, 19.3% of the UK population will be aged 65 and a minimum of 35,000 new senior living development properties will need to be created to meet housing demands.
Independent senior living residents are able to live on their own with limited assistance (provided by third-party home health care providers if needed) and without around-the-clock supervision. Neither assisted living nor senior independent living communities offer 24/7 skilled nursing that is provided at nursing homes.
Cost:
Independent senior living communities are the least expensive of the three primary senior living options. Monthly costs vary significantly by community type, size of apartment, location and services offered. The average total cost for a U.S. one bedroom independent senior living apartment is $2,750 per month.
In 2011, the average rate for a private bedroom at a U.S. nursing home was $239 per day, or nearly $7,270 per month. Average rate for a private bedroom at an assisted living community was $3,477 per month. Continuing care communities require an entrance fee that ranges from $20,000 to $500,000, in addition to monthly fees that range from $500 to $3,000 or more depending on services.
See also:
- Key Differences Between Independent Living and Assisted Living
- Active and Healthy Ageing and Independent Living
- Quality of Life in Assisted Living Homes: A Multidimensional Analysis
- Personality and Adjustment to Assisted Living
- Assisted Living Expansion and the Market for Nursing Home Care
- Why Senior Housing Prices Are Impossible To Find
Old Age Discrimination in the United States
- YouTube Video: How to Recognize Old Age Discrimination in the Workplace
- YouTube Video: An Overview of the Age Discrimination in Employment Act (ADEA)
- YouTube Video: Ageism in the workplace: What older workers can do to stay employed
Age discrimination in the United States:
In the United States, all states have passed laws that restrict age discrimination, and age discrimination is restricted under federal laws such as the Age Discrimination in Employment Act of 1967 (ADEA). However, it is worthy of note that age discrimination is still an issue in employment as of 2019.
Credit transactions:
The Equal Credit Opportunity Act (ECOA) is a United States law (codified at 15 U.S.C. § 1691 et seq.), enacted 28 October 1974, that makes it unlawful for any creditor to discriminate against any applicant, with respect to any aspect of a credit transaction, on the basis of (among other things) age, provided the applicant has the capacity to contract.
Elected office:
Some U.S. political offices have qualifications that discriminate on the basis of age. For example, pursuant to the Constitution of the United States the President of the United States must be at least 35 years old; a United States senator must be at least 30; and a member of the United States House of Representatives must be at least age 25.
Employment:
The Age Discrimination in Employment Act of 1967 (ADEA) (29 U.S.C. § 621 to 29 U.S.C. § 634) is a federal law that provides certain employment protections to workers who are over the age of forty, who work for an employer who has twenty or more employees.
For protected workers, the ADEA prohibits discrimination at all levels of employment, from recruitment and hiring, through the employment relationship, and through decisions for layoffs or termination of the employment relationship.
An age limit may only be legally specified for protected workers in the circumstance where age has been shown to be a "bona fide occupational qualification [BFOQ] reasonably necessary to the normal operation of the particular business".
In practice, BFOQs for age are limited to the obvious (hiring a young actor to play a young character in a movie), when a job is physically demanding (police, firefighters, military service), or when public safety is a concern (for example, in the case of age limits for pilots, truck drivers, and bus drivers).
Some states like New York and New Jersey including District of Columbia have laws that protect younger workers from reverse age discrimination, a practice not prohibited under the ADEA. In these jurisdictions, employers are legally prohibited from discriminating against workers 18 and older for their age unless a bona fide occupational qualification exists (i.e., employers may require bartenders to be at least 21 to comply with the legal drinking age).
In 1968, the EEOC declared age restrictions on flight attendants' employment to be illegal sex discrimination under Title VII of the Civil Rights Act of 1964.
Mandatory retirement:
Mandatory retirement due to age is generally unlawful in the United States, except in certain industries and occupations that are regulated by law, and are often part of the government (such as military service and federal police agencies, such as the Federal Bureau of Investigation).
Minnesota has statutorily established mandatory retirement for all judges at age 70 (more precisely, at the end of the month a judge reaches that age). The Minnesota Legislature has had the constitutional right to set judicial retirement ages since 1956, but did not do so until 1973, setting the age at 70.
The Federal Age Discrimination in Employment Act, which became law in 1986, ended mandatory age-related retirement at age 70 for many jobs, not including the Minnesota judiciary; another exception was all postsecondary institutions (colleges, etc.) This exception ended on December 31, 1993.
The Fair Treatment for Experienced Pilots Act (Public Law 110-135) went into effect on December 13, 2007, raising the mandatory retirement age for pilots to 65 from the previous 60.
Minimum wage:
In 1986, the Fair Labor Standards Act was amended to allow the United States Secretary of Labor to provide special certificates to allow an employer to pay less than the minimum wage to individuals whose earning or productive capacity is impaired by age, physical or mental deficiency, or injury.
These employees must still be paid wages that are related to the individual's productivity and commensurate with those paid to similarly located and employed nonhandicapped workers.
Federal minimum wage laws allow for employers to pay lower wages to young workers. Many state and local minimum wage laws mirror such an age-based, tiered minimum wage.
Employment of minors:
In the United States, a person must generally be at least 14 years old to seek a job, and workers face additional restrictions on their work activities until they reach age 16.
Additional age restrictions for workers vary by state. For example, many states require workers under 18 years of age to have work permits and not fulfill occupations deemed hazardous.
Notable case law:
In Western Air Lines, Inc v Criswell 472 US 400 (1985) the United States Supreme Court held it was lawful to require airline pilots to retire at 60, because the Federal Aviation Authority forbid using pilots over 60 in aviation.
But the Court held that refusing to employ flight engineers over that age was unjustified as there were no such FAA requirements. (Note that The Fair Treatment for Experienced Pilots Act (Public Law 110-135) went into effect on December 13, 2007, raising the mandatory retirement age for pilots to 65 from the previous 60.)
DeMarco v. Holy Cross High School 4 F.3d 166 (2nd Cir. 1993) was an employment discrimination case brought under the ADEA (Age Discrimination in Employment Act of 1967). The appellant, Guy DeMarco, was released from employment prior to his eligibility for tenure at the age of forty-nine.
Holy Cross High School argued that it was not subject to ADEA laws, and if it were that this case against it was in violation of the Free Exercise Clause and the Establishment Clause of the First Amendment. The defendant also argued that the plaintiff failed to utilize the administrative remedies available.
The court noted that other anti-discrimination statutes were held to be applicable to religious organizations, with the exception of statutes that prohibited discrimination based on religious belief.
Since statutes prohibiting discrimination by race, gender and national origin were already found applicable to religious organizations, it was logical (and a reasonable interpretation of the legislative history) to extend the prohibition against age discrimination to religious organizations as well. The decision of the district court was reversed and the case remanded for further proceedings.
Hazen Paper Co. v. Biggins 507 U.S. 604 (1993) was a United States Supreme Court case in which the court held that a disparate treatment claim cannot succeed unless the employee's protected trait had a determinative influence on the employer's decision-making. This case concerned how Hazen Paper fired Biggins, 62, a few weeks before his service would have reached the required number of years for his pension to vest.
Biggins sued Hazen Paper alleging a violation of the Age Discrimination in Employment Act of 1967.
In Kimel v. Florida Bd. of Regents, 528 U.S. 62 (2000), the United States Supreme Court held that state employees cannot sue states for monetary damages under the Age Discrimination in Employment Act of 1967 in federal court.
The EEOC may still enforce the ADEA against states, and state employees may still sue state officials for declaratory and injunctive relief.
In Gomez-Perez v. Potter (2008), the United States Supreme Court allowed federal workers who experience retaliation as a result of reporting age discrimination under the law to sue for damages.
The United States Supreme Court, in Meacham v. Knolls Atomic Power Lab, 554 U.S. 84 (2008), held that the employer, not the employee, bears the burden of proving that a layoff or other action that hurts older workers more than others was based not on age but on some other “reasonable factor.”
In 2009, the United States Supreme Court issued its opinion on Gross v. FBL Financial Services, Inc.. In a 5–4 opinion, the Court ruled that private-sector plaintiffs must prove that age was the "but for" cause of the adverse employment action they are suing over. That is, the plaintiff must prove that age discrimination was the determining reason for the adverse employment action (e.g. the action would not have been taken 'but for' the plaintiff's age).
However, the Supreme Court's opinion did not explicitly mention public-sector workers. A later opinion, University of Texas Southwestern Medical Center v. Nassar (2013) applied the same 'but for' standard to retaliation claims.
In September 2016, California passed state bill AB-1687, an anti-ageism law taking effect on 1 January 2017, requiring "commercial online entertainment employment" services that allow paid subscribers to submit information and resumes (such as IMDbPro), to honor requests to have their ages and birthdays removed.
The bill was supported by SAG-AFTRA's former and current presidents Ken Howard and Gabrielle Carteris, who felt that the law would help to reduce ageism in the entertainment industry.
On 23 February 2017, U.S. District Judge Vince Girdhari Chhabria issued a stay on the bill pending a further trial, claiming that it was "difficult to imagine how AB 1687 could not violate the First Amendment" because it inhibited the public consumption of factual information.
In February 2018, Girdhari ruled that the law was unconstitutional, arguing that the state of California "[had] not shown that partially eliminating one source of age-related information will appreciably diminish the amount of age discrimination occurring in the entertainment industry."
The ruling was criticized by SAG-AFTRA, alleging that the court "incorrectly concluded there were no material disputed factual issues, while precluding the parties from acquiring additional evidence or permitting the case to go to trial". The ruling was eventually appealed, but the Ninth Circuit Court of Appeals upheld it in 2020.
Babb v. Wilkie, No. 18-882, , 589 U.S. ___ (2020), is a case of the United States Supreme Court in which the justices considered the scope of protections for federal employees in the Age Discrimination in Employment Act of 1967. Specifically, the Court ruled that plaintiffs only need to prove that age was a motivating factor in the decision in order to sue.
However, establishing but for causation is still necessary in determining the appropriate remedy. If a plaintiff can establish that the age was the determining factor in the employment outcome, they may be entitled to compensatory damages or other relief relating to the end result of the employment decision.
Our Lady of Guadalupe School v. Morrissey-Berru, 591 U.S. ___ (2020), is a United States Supreme Court case involving the ministerial exception of federal employment discrimination laws. The case extends from the Supreme Court's prior decision in Hosanna-Tabor Evangelical Lutheran Church & School v. Equal Employment Opportunity Commission (2012) which created the ministerial exception based on the Establishment and Free Exercise Clauses of the United States Constitution, asserting that federal discrimination laws cannot be applied to leaders of religious organizations.
The Supreme Court case Our Lady of Guadalupe School v. Morrissey-Berru, along with the consolidated St. James School v. Biel (Docket 19-348), both arose from rulings in the United States Court of Appeals for the Ninth Circuit that found that federal discrimination laws do apply to others within a religious organization that serve an important religious function but lack the title or training to be considered a religious leader under Hosanna-Tabor.
One of those rulings in the United States Court of Appeals for the Ninth Circuit was the ruling in Morrissey-Berru v. Our Lady of Guadalupe School, in 2019, in which the United States Court of Appeals for the Ninth Circuit allowed a Catholic elementary school teacher's age discrimination suit to move forward.
The religious organization challenged that ruling on the basis of Hosanna-Tabor. The Supreme Court ruled in a 7–2 decision called Our Lady of Guadalupe School v. Morrissey-Berru on July 8, 2020 that reversed the Ninth Circuit's ruling, affirming that the principles of Hosanna-Tabor, that a person can be serving an important religious function even if not holding the title or training of a religious leader, satisfied the ministerial exception in employment discrimination.
Federally funded programs:
The Older Americans Amendments of 1975 (Pub. L. 94–135) is an Act of the 94th U.S. Congress amending the Older Americans Act of 1965. It prohibits discrimination based on age in programs or activities that receive federal financial assistance, for instance, financial assistance to schools and colleges, provided by the U.S. Department of Education.
Hate crimes:
The District of Columbia and the following twelve states define age as a specific motivation for hate crimes:
Voting:
The Twenty-sixth Amendment to the United States Constitution reads:
That amendment was ratified in 1971.
Prior to that:
In 1943 and 1955 respectively, the Georgia and Kentucky legislatures approved measures to lower the voting age to 18.
On June 22, 1970, President Richard Nixon signed an extension of the Voting Rights Act of 1965 that required the voting age to be 18 in all federal, state, and local elections. In his statement on signing the extension, Nixon said: "Despite my misgivings about the constitutionality of this one provision, I have signed the bill. I have directed the Attorney General to cooperate fully in expediting a swift court test of the constitutionality of the 18-year-old provision."
Subsequently, Oregon and Texas challenged the law in court, and the case came before the Supreme Court in 1970 as Oregon v. Mitchell. By this time, four states had a minimum voting age below 21: Georgia, Kentucky, Alaska and Hawaii.
In Oregon v. Mitchell (1970), the Supreme Court considered whether the voting-age provisions Congress added to the Voting Rights Act in 1970 were constitutional. The Court struck down the provisions that established 18 as the voting age in state and local elections.
However, the Court upheld the provision establishing the voting age as 18 in federal elections. The Court was deeply divided in this case, and a majority of justices did not agree on a rationale for the holding.
The decision resulted in states being able to maintain 21 as the voting age in state and local elections, but being required to establish separate voter rolls so that voters between 18 and 21 years old could vote in federal elections.
Activism:
The Newsboys Strike of 1899 fought ageist employment practices targeted against youth by large newspaper syndicates in the Northeast. The strikers demonstrated across the city for several days, effectively stopping circulation of the two papers, along with the news distribution for many New England cities.
The strike lasted two weeks, causing Pulitzer's New York World to decrease its circulation from 360,000 papers sold per day to 125,000. Although the price of papers was not lowered, the strike was successful in forcing the World and Journal to offer full buybacks to their sellers, thus increasing the amount of money that newsies received for their work.
The American Youth Congress, or AYC, was formed in 1935 to advocate for youth rights in U.S. politics. It ended in 1940.
The AARP was founded in 1958 by Ethel Percy Andrus (a retired educator from California) and Leonard Davis (later the founder of the Colonial Penn Group of insurance companies). Its stated mission is "to empower people to choose how they live as they age". It is an influential lobbying group in the United States focusing largely on issues affecting the elderly.
The Gray Panthers was formed in 1970 by Maggie Kuhn, with a goal of eliminating mandatory retirement; they now work on many social justice issues including eliminating ageism.
Youth Liberation of Ann Arbor started in 1970 to promote youth and fight ageism.
Three O'Clock Lobby formed in 1976 to promote youth participation throughout traditionally ageist government structures in Michigan.
Senior Action in a Gay Environment (SAGE) was incorporated in 1978 by lesbian and gay activists and aging service professionals; it is now called Services & Advocacy for GLBT Elders. It works with LGBT older adults and aging service providers to address and overcome the challenges of discrimination in older adult service settings.
OWL - The Voice of Women 40+ was founded as the Older Women's League by Tish Sommers and Laurie Shields, following the White House Mini-Conference on Older Women in Des Moines, Iowa in October 1980. It advocated for women in the U.S. who were age 40 and over. In March 2017, it was reported that the national organization had decided to disband, but local chapters may continue to function under the OWL name or possibly another name.
Old Lesbians Organizing for Change was founded in 1987; the mission of the organization is to "eliminate the oppression of ageism and to stand in solidarity against all oppressions" through “[the] cooperative community of Old Lesbian feminist activists from many backgrounds working for justice and the well-being of all old lesbians.”
Their initial meeting was inspired by the publication of the book Look Me in the Eye: Old Women, Aging and Ageism by Barbara Macdonald and Cynthia Rich in 1983.
Americans for a Society Free from Age Restrictions: was formed in 1996 to advance the civil and human rights of young people through eliminating ageist laws targeted against young people, and to help youth counter ageism in America.
The National Youth Rights Association started in 1998 to promote awareness of the legal and human rights of young people in the United States.
The Freechild Project was formed in 2001 to identify, unify and promote diverse opportunities for youth engagement in social change by fighting ageism. In 2002 the Freechild Project created an information and training initiative to provide resources to youth organizations and schools focused on youth rights.
See also:
In the United States, all states have passed laws that restrict age discrimination, and age discrimination is restricted under federal laws such as the Age Discrimination in Employment Act of 1967 (ADEA). However, it is worthy of note that age discrimination is still an issue in employment as of 2019.
Credit transactions:
The Equal Credit Opportunity Act (ECOA) is a United States law (codified at 15 U.S.C. § 1691 et seq.), enacted 28 October 1974, that makes it unlawful for any creditor to discriminate against any applicant, with respect to any aspect of a credit transaction, on the basis of (among other things) age, provided the applicant has the capacity to contract.
Elected office:
Some U.S. political offices have qualifications that discriminate on the basis of age. For example, pursuant to the Constitution of the United States the President of the United States must be at least 35 years old; a United States senator must be at least 30; and a member of the United States House of Representatives must be at least age 25.
Employment:
The Age Discrimination in Employment Act of 1967 (ADEA) (29 U.S.C. § 621 to 29 U.S.C. § 634) is a federal law that provides certain employment protections to workers who are over the age of forty, who work for an employer who has twenty or more employees.
For protected workers, the ADEA prohibits discrimination at all levels of employment, from recruitment and hiring, through the employment relationship, and through decisions for layoffs or termination of the employment relationship.
An age limit may only be legally specified for protected workers in the circumstance where age has been shown to be a "bona fide occupational qualification [BFOQ] reasonably necessary to the normal operation of the particular business".
In practice, BFOQs for age are limited to the obvious (hiring a young actor to play a young character in a movie), when a job is physically demanding (police, firefighters, military service), or when public safety is a concern (for example, in the case of age limits for pilots, truck drivers, and bus drivers).
Some states like New York and New Jersey including District of Columbia have laws that protect younger workers from reverse age discrimination, a practice not prohibited under the ADEA. In these jurisdictions, employers are legally prohibited from discriminating against workers 18 and older for their age unless a bona fide occupational qualification exists (i.e., employers may require bartenders to be at least 21 to comply with the legal drinking age).
In 1968, the EEOC declared age restrictions on flight attendants' employment to be illegal sex discrimination under Title VII of the Civil Rights Act of 1964.
Mandatory retirement:
Mandatory retirement due to age is generally unlawful in the United States, except in certain industries and occupations that are regulated by law, and are often part of the government (such as military service and federal police agencies, such as the Federal Bureau of Investigation).
Minnesota has statutorily established mandatory retirement for all judges at age 70 (more precisely, at the end of the month a judge reaches that age). The Minnesota Legislature has had the constitutional right to set judicial retirement ages since 1956, but did not do so until 1973, setting the age at 70.
The Federal Age Discrimination in Employment Act, which became law in 1986, ended mandatory age-related retirement at age 70 for many jobs, not including the Minnesota judiciary; another exception was all postsecondary institutions (colleges, etc.) This exception ended on December 31, 1993.
The Fair Treatment for Experienced Pilots Act (Public Law 110-135) went into effect on December 13, 2007, raising the mandatory retirement age for pilots to 65 from the previous 60.
Minimum wage:
In 1986, the Fair Labor Standards Act was amended to allow the United States Secretary of Labor to provide special certificates to allow an employer to pay less than the minimum wage to individuals whose earning or productive capacity is impaired by age, physical or mental deficiency, or injury.
These employees must still be paid wages that are related to the individual's productivity and commensurate with those paid to similarly located and employed nonhandicapped workers.
Federal minimum wage laws allow for employers to pay lower wages to young workers. Many state and local minimum wage laws mirror such an age-based, tiered minimum wage.
Employment of minors:
In the United States, a person must generally be at least 14 years old to seek a job, and workers face additional restrictions on their work activities until they reach age 16.
Additional age restrictions for workers vary by state. For example, many states require workers under 18 years of age to have work permits and not fulfill occupations deemed hazardous.
Notable case law:
In Western Air Lines, Inc v Criswell 472 US 400 (1985) the United States Supreme Court held it was lawful to require airline pilots to retire at 60, because the Federal Aviation Authority forbid using pilots over 60 in aviation.
But the Court held that refusing to employ flight engineers over that age was unjustified as there were no such FAA requirements. (Note that The Fair Treatment for Experienced Pilots Act (Public Law 110-135) went into effect on December 13, 2007, raising the mandatory retirement age for pilots to 65 from the previous 60.)
DeMarco v. Holy Cross High School 4 F.3d 166 (2nd Cir. 1993) was an employment discrimination case brought under the ADEA (Age Discrimination in Employment Act of 1967). The appellant, Guy DeMarco, was released from employment prior to his eligibility for tenure at the age of forty-nine.
Holy Cross High School argued that it was not subject to ADEA laws, and if it were that this case against it was in violation of the Free Exercise Clause and the Establishment Clause of the First Amendment. The defendant also argued that the plaintiff failed to utilize the administrative remedies available.
The court noted that other anti-discrimination statutes were held to be applicable to religious organizations, with the exception of statutes that prohibited discrimination based on religious belief.
Since statutes prohibiting discrimination by race, gender and national origin were already found applicable to religious organizations, it was logical (and a reasonable interpretation of the legislative history) to extend the prohibition against age discrimination to religious organizations as well. The decision of the district court was reversed and the case remanded for further proceedings.
Hazen Paper Co. v. Biggins 507 U.S. 604 (1993) was a United States Supreme Court case in which the court held that a disparate treatment claim cannot succeed unless the employee's protected trait had a determinative influence on the employer's decision-making. This case concerned how Hazen Paper fired Biggins, 62, a few weeks before his service would have reached the required number of years for his pension to vest.
Biggins sued Hazen Paper alleging a violation of the Age Discrimination in Employment Act of 1967.
In Kimel v. Florida Bd. of Regents, 528 U.S. 62 (2000), the United States Supreme Court held that state employees cannot sue states for monetary damages under the Age Discrimination in Employment Act of 1967 in federal court.
The EEOC may still enforce the ADEA against states, and state employees may still sue state officials for declaratory and injunctive relief.
In Gomez-Perez v. Potter (2008), the United States Supreme Court allowed federal workers who experience retaliation as a result of reporting age discrimination under the law to sue for damages.
The United States Supreme Court, in Meacham v. Knolls Atomic Power Lab, 554 U.S. 84 (2008), held that the employer, not the employee, bears the burden of proving that a layoff or other action that hurts older workers more than others was based not on age but on some other “reasonable factor.”
In 2009, the United States Supreme Court issued its opinion on Gross v. FBL Financial Services, Inc.. In a 5–4 opinion, the Court ruled that private-sector plaintiffs must prove that age was the "but for" cause of the adverse employment action they are suing over. That is, the plaintiff must prove that age discrimination was the determining reason for the adverse employment action (e.g. the action would not have been taken 'but for' the plaintiff's age).
However, the Supreme Court's opinion did not explicitly mention public-sector workers. A later opinion, University of Texas Southwestern Medical Center v. Nassar (2013) applied the same 'but for' standard to retaliation claims.
In September 2016, California passed state bill AB-1687, an anti-ageism law taking effect on 1 January 2017, requiring "commercial online entertainment employment" services that allow paid subscribers to submit information and resumes (such as IMDbPro), to honor requests to have their ages and birthdays removed.
The bill was supported by SAG-AFTRA's former and current presidents Ken Howard and Gabrielle Carteris, who felt that the law would help to reduce ageism in the entertainment industry.
On 23 February 2017, U.S. District Judge Vince Girdhari Chhabria issued a stay on the bill pending a further trial, claiming that it was "difficult to imagine how AB 1687 could not violate the First Amendment" because it inhibited the public consumption of factual information.
In February 2018, Girdhari ruled that the law was unconstitutional, arguing that the state of California "[had] not shown that partially eliminating one source of age-related information will appreciably diminish the amount of age discrimination occurring in the entertainment industry."
The ruling was criticized by SAG-AFTRA, alleging that the court "incorrectly concluded there were no material disputed factual issues, while precluding the parties from acquiring additional evidence or permitting the case to go to trial". The ruling was eventually appealed, but the Ninth Circuit Court of Appeals upheld it in 2020.
Babb v. Wilkie, No. 18-882, , 589 U.S. ___ (2020), is a case of the United States Supreme Court in which the justices considered the scope of protections for federal employees in the Age Discrimination in Employment Act of 1967. Specifically, the Court ruled that plaintiffs only need to prove that age was a motivating factor in the decision in order to sue.
However, establishing but for causation is still necessary in determining the appropriate remedy. If a plaintiff can establish that the age was the determining factor in the employment outcome, they may be entitled to compensatory damages or other relief relating to the end result of the employment decision.
Our Lady of Guadalupe School v. Morrissey-Berru, 591 U.S. ___ (2020), is a United States Supreme Court case involving the ministerial exception of federal employment discrimination laws. The case extends from the Supreme Court's prior decision in Hosanna-Tabor Evangelical Lutheran Church & School v. Equal Employment Opportunity Commission (2012) which created the ministerial exception based on the Establishment and Free Exercise Clauses of the United States Constitution, asserting that federal discrimination laws cannot be applied to leaders of religious organizations.
The Supreme Court case Our Lady of Guadalupe School v. Morrissey-Berru, along with the consolidated St. James School v. Biel (Docket 19-348), both arose from rulings in the United States Court of Appeals for the Ninth Circuit that found that federal discrimination laws do apply to others within a religious organization that serve an important religious function but lack the title or training to be considered a religious leader under Hosanna-Tabor.
One of those rulings in the United States Court of Appeals for the Ninth Circuit was the ruling in Morrissey-Berru v. Our Lady of Guadalupe School, in 2019, in which the United States Court of Appeals for the Ninth Circuit allowed a Catholic elementary school teacher's age discrimination suit to move forward.
The religious organization challenged that ruling on the basis of Hosanna-Tabor. The Supreme Court ruled in a 7–2 decision called Our Lady of Guadalupe School v. Morrissey-Berru on July 8, 2020 that reversed the Ninth Circuit's ruling, affirming that the principles of Hosanna-Tabor, that a person can be serving an important religious function even if not holding the title or training of a religious leader, satisfied the ministerial exception in employment discrimination.
Federally funded programs:
The Older Americans Amendments of 1975 (Pub. L. 94–135) is an Act of the 94th U.S. Congress amending the Older Americans Act of 1965. It prohibits discrimination based on age in programs or activities that receive federal financial assistance, for instance, financial assistance to schools and colleges, provided by the U.S. Department of Education.
Hate crimes:
The District of Columbia and the following twelve states define age as a specific motivation for hate crimes:
- California,
- Florida,
- Iowa,
- Hawaii,
- Kansas,
- Louisiana,
- Maine,
- Minnesota,
- Nebraska,
- New Mexico,
- New York,
- and Vermont
Voting:
The Twenty-sixth Amendment to the United States Constitution reads:
- Section 1. The right of citizens of the United States, who are eighteen years of age or older, to vote shall not be denied or abridged by the United States or by any State on account of age.
- Section 2. The Congress shall have power to enforce this article by appropriate legislation.
That amendment was ratified in 1971.
Prior to that:
In 1943 and 1955 respectively, the Georgia and Kentucky legislatures approved measures to lower the voting age to 18.
On June 22, 1970, President Richard Nixon signed an extension of the Voting Rights Act of 1965 that required the voting age to be 18 in all federal, state, and local elections. In his statement on signing the extension, Nixon said: "Despite my misgivings about the constitutionality of this one provision, I have signed the bill. I have directed the Attorney General to cooperate fully in expediting a swift court test of the constitutionality of the 18-year-old provision."
Subsequently, Oregon and Texas challenged the law in court, and the case came before the Supreme Court in 1970 as Oregon v. Mitchell. By this time, four states had a minimum voting age below 21: Georgia, Kentucky, Alaska and Hawaii.
In Oregon v. Mitchell (1970), the Supreme Court considered whether the voting-age provisions Congress added to the Voting Rights Act in 1970 were constitutional. The Court struck down the provisions that established 18 as the voting age in state and local elections.
However, the Court upheld the provision establishing the voting age as 18 in federal elections. The Court was deeply divided in this case, and a majority of justices did not agree on a rationale for the holding.
The decision resulted in states being able to maintain 21 as the voting age in state and local elections, but being required to establish separate voter rolls so that voters between 18 and 21 years old could vote in federal elections.
Activism:
The Newsboys Strike of 1899 fought ageist employment practices targeted against youth by large newspaper syndicates in the Northeast. The strikers demonstrated across the city for several days, effectively stopping circulation of the two papers, along with the news distribution for many New England cities.
The strike lasted two weeks, causing Pulitzer's New York World to decrease its circulation from 360,000 papers sold per day to 125,000. Although the price of papers was not lowered, the strike was successful in forcing the World and Journal to offer full buybacks to their sellers, thus increasing the amount of money that newsies received for their work.
The American Youth Congress, or AYC, was formed in 1935 to advocate for youth rights in U.S. politics. It ended in 1940.
The AARP was founded in 1958 by Ethel Percy Andrus (a retired educator from California) and Leonard Davis (later the founder of the Colonial Penn Group of insurance companies). Its stated mission is "to empower people to choose how they live as they age". It is an influential lobbying group in the United States focusing largely on issues affecting the elderly.
The Gray Panthers was formed in 1970 by Maggie Kuhn, with a goal of eliminating mandatory retirement; they now work on many social justice issues including eliminating ageism.
Youth Liberation of Ann Arbor started in 1970 to promote youth and fight ageism.
Three O'Clock Lobby formed in 1976 to promote youth participation throughout traditionally ageist government structures in Michigan.
Senior Action in a Gay Environment (SAGE) was incorporated in 1978 by lesbian and gay activists and aging service professionals; it is now called Services & Advocacy for GLBT Elders. It works with LGBT older adults and aging service providers to address and overcome the challenges of discrimination in older adult service settings.
OWL - The Voice of Women 40+ was founded as the Older Women's League by Tish Sommers and Laurie Shields, following the White House Mini-Conference on Older Women in Des Moines, Iowa in October 1980. It advocated for women in the U.S. who were age 40 and over. In March 2017, it was reported that the national organization had decided to disband, but local chapters may continue to function under the OWL name or possibly another name.
Old Lesbians Organizing for Change was founded in 1987; the mission of the organization is to "eliminate the oppression of ageism and to stand in solidarity against all oppressions" through “[the] cooperative community of Old Lesbian feminist activists from many backgrounds working for justice and the well-being of all old lesbians.”
Their initial meeting was inspired by the publication of the book Look Me in the Eye: Old Women, Aging and Ageism by Barbara Macdonald and Cynthia Rich in 1983.
Americans for a Society Free from Age Restrictions: was formed in 1996 to advance the civil and human rights of young people through eliminating ageist laws targeted against young people, and to help youth counter ageism in America.
The National Youth Rights Association started in 1998 to promote awareness of the legal and human rights of young people in the United States.
The Freechild Project was formed in 2001 to identify, unify and promote diverse opportunities for youth engagement in social change by fighting ageism. In 2002 the Freechild Project created an information and training initiative to provide resources to youth organizations and schools focused on youth rights.
See also:
- Aging in the American workforce
- History of youth rights in the United States
- Nursing home residents' rights
- Youth rights
Elder Law in the United States
- YouTube Video: Understanding What Elder Law Attorneys Do
- YouTube Video: The DIFFERENCE Between Estate Planning and Elder Law
- YouTube Video: Elder Law Session about Medicaid Basics and Upcoming Changes
Elder law is an area of legal practice that specializes on issues that affect the senior population. The purpose of elder law planning is to prepare the elderly person for financial freedom and autonomy through proper financial planning and long-term care options.
Categories:
The three major categories that make up elder law are:
Other issues found under the umbrella of elder law include such areas as:
History:
Elder law developed as a specialty because as lifespans increased there was an increased need for medical care, care giving, and financial management.
The Older Americans Act (OAA), originally signed into law by President Lyndon B. Johnson on July 14, 1965 (the same year Medicare was created), created the Administration on Aging (AOA), a division within the Department of Health and Human Services.
The OAA also authorized grants to States for community planning and services programs, funding for research, and demonstration and training projects in the field of aging.
In 1972 Amendments to the OAA added the national nutrition program for the elderly. The OAA of 2000 was amended on November 13, 2000, to include the National Family Caregiver Support Program, which was intended to help hundreds of thousands of family members who are struggling to care for their older loved ones who are ill or who have disabilities.
This program provides grant funding for combined services between state and local agencies for such things as counseling, support groups, respite and other community-based services.
These services are focused on the care of the frail and aging members of society. The program also provides services geared towards the family units of grandparents and other older relatives now in the stages of care-taking for related children eighteen years of age and under.
Elder law is an expansion of the traditional trust and estates practice.
Careers in or associated with elder law:
Careers that are developing around the area of Elder Law include:
Essentially, any career field can create a benefit to the aging of modern society.
See also:
Categories:
The three major categories that make up elder law are:
- Estate planning and administration, including tax questions
- Medicaid, disability and other long-term care issues
- Guardianship, conservatorship and commitment matters, including fiduciary administration
Other issues found under the umbrella of elder law include such areas as:
- estate planning
- wills
- trusts
- guardianships
- protection against elder abuse, neglect, and fraud
- end-of-life planning
- all levels of disability and medical care
- retirement planning
- Social Security benefits
- Medicare and Medicaid coverage
- Medicaid planning (United States)
- consumer protection
- nursing homes and in-home care
- powers of attorney
- physicians' or medical care directives, declarations and powers of attorney
- landlord/tenant needs
- real estate and mortgage assistance
- various levels of advice, counseling and advocacy of rights
- tax issues
- discrimination
History:
Elder law developed as a specialty because as lifespans increased there was an increased need for medical care, care giving, and financial management.
The Older Americans Act (OAA), originally signed into law by President Lyndon B. Johnson on July 14, 1965 (the same year Medicare was created), created the Administration on Aging (AOA), a division within the Department of Health and Human Services.
The OAA also authorized grants to States for community planning and services programs, funding for research, and demonstration and training projects in the field of aging.
In 1972 Amendments to the OAA added the national nutrition program for the elderly. The OAA of 2000 was amended on November 13, 2000, to include the National Family Caregiver Support Program, which was intended to help hundreds of thousands of family members who are struggling to care for their older loved ones who are ill or who have disabilities.
This program provides grant funding for combined services between state and local agencies for such things as counseling, support groups, respite and other community-based services.
These services are focused on the care of the frail and aging members of society. The program also provides services geared towards the family units of grandparents and other older relatives now in the stages of care-taking for related children eighteen years of age and under.
Elder law is an expansion of the traditional trust and estates practice.
Careers in or associated with elder law:
Careers that are developing around the area of Elder Law include:
- social workers
- lawyers
- paralegals
- legal assistants
- legal secretaries
- guardians ad litem (GAL)
- various types of psychologists
- care givers
- financial planners
- policy makers and legal advocates
- benefit specialists
- Better Business Bureau
- Attorney General's Office
- Consumer Protection Agency
- political watch-dog groups
- health care providers
- researchers
- funeral planners
- grief counselors
- case workers
- abuse & fraud investigators
- educators
- product developers
- transportation providers
- entertainment and tour guides
- real estate agents
- mortgage brokers
- insurance providers
- elder companions
Essentially, any career field can create a benefit to the aging of modern society.
See also:
- National Academy of Elder Law Attorneys
- National Elder Law Foundation
- Administration on Aging
- https://web.archive.org/web/20051119010913/http://www.neln.org/sitemap.html
Old Age, and How to Extend One's Life
- YouTube Video: How to Extend Your Lifespan with David Sinclair
- YouTube Video: Oldest Person in the World - Guinness World Records
- YouTube Video: When Living 200 Year Becomes Normal - the End of Ageing(?)
* -- From Above Photo: National Institute of Health:
Can You Lengthen Your Life? Researchers Explore How To Stay Healthy Longer
Want the secret to living a longer and healthier life? Scientists have found ways to prolong the healthy lifespans of worms, mice, and even monkeys. Their work has revealed exciting new clues about the biology of aging.
But solid evidence still shows that the best way to boost the chance of living a long and active life is to follow the advice you likely heard from your parents: eat well, exercise regularly, get plenty of sleep, and stay away from bad habits.
People born in the U.S. today can expect to live to an average age of about 79. A century ago, life expectancy was closer to 54. “We’ve had a significant increase in lifespan over the last century,” says Dr. Marie Bernard, deputy director of NIH’s National Institute on Aging. “Now if you make it to age 65, the likelihood that you’ll make it to 85 is very high. And if you make it to 85, the likelihood that you’ll make it to 92 is very high. So people are living longer, and it’s happening across the globe.”
Older people tend to be healthier nowadays, too. Research has shown that healthful behaviors can help you stay active and healthy into your 60s, 70s, and beyond. In fact, a long-term study of Seventh-day Adventists—a religious group with a generally healthy lifestyle—shows that they tend to remain healthier into old age. Their life expectancy is nearly 10 years longer on average than most Americans. The Adventists’ age-enhancing behaviors include regular exercise, a vegetarian diet, avoiding tobacco and alcohol, and maintaining a healthy weight.
“If I had to rank behaviors in terms of priority, I’d say that exercise is the most important thing associated with living longer and healthier,” says Dr. Luigi Ferrucci, an NIH geriatrician who oversees research on aging and health. “Exercise is especially important for lengthening active life expectancy, which is life without disease and without physical and mental/thinking disability.”
Natural changes to the body as we age can lead to a gradual loss of muscle, reduced energy, and achy joints. These changes may make it tempting to move less and sit more. But doing that can raise your risk for disease, disability, and even death. It’s important to work with a doctor to find the types of physical activity that can help you maintain your health and mobility.
Even frail older adults can benefit from regular physical activity. One NIH-funded study included over 600 adults, ages 70 to 89, who were at risk for disability. They were randomly placed in either a moderate exercise program or a comparison group without structured exercise. The exercise group gradually worked up to 150 minutes of weekly activity. This included brisk walking, strength and balance training, and flexibility exercises.
“After more than 2 years, the physical activity group had less disability, and if they became disabled, they were disabled for a shorter time than those in the comparison group,” Bernard explains. “The combination of different types of exercise—aerobic, strength and balance training, and flexibility—is important to healthy aging.” NIH’s Go4Life website has tips to help older adults get and stay active.
Another sure way to improve your chances for a longer, healthier life is to shed excess weight. “Being obese—with a body mass index (BMI) higher than 30—is a risk factor for early death, and it shortens your active life expectancy,” Ferrucci says. BMI is an estimate of your body fat based on your weight and height. Use NIH’s BMI calculator to determine your BMI. Talk with a doctor about reaching a healthy weight.
Studies in animals have found that certain types of dietary changes—such as extremely low-calorie diets—can lead to longer, healthier lives. These studies offer clues to the biological processes that affect healthy aging. But to date, calorie-restricted diets and other dietary changes have had mixed results in extending the healthy lives of people.
“We have indirect evidence that nutritional adjustments can improve active longevity in people, but this is still an area of intense research,” Ferrucci says. “So far, we don’t really have solid evidence about caloric restriction and whether it may have a positive effect on human aging.” Researchers are now studying potential drugs or other approaches that might mimic calorie restriction’s benefits.
Not smoking is another pathway to a longer, healthier life. “There’s no question that smoking is a hard habit to break. But data suggest that from the moment you stop smoking, there are health benefits. So it’s worthwhile making that effort,” Bernard says.
You might think you need good genes to live longer. But genes are only part of the equation for most of us, says Dr. Thomas Perls, an aging expert and director of the New England Centenarian Study at the Boston University School of Medicine. “Research shows that genes account for less than one-third of your chances of surviving to age 85. The vast majority of variation in how old we live to be is due to our health behaviors,” Perls says. “Our genes could get most of us close to the remarkable age of 90 if we lead a healthy lifestyle.”
The influence of genes is stronger, though, for people who live to older ages, such as beyond 95. Perls has been studying people who live to age 100 and up (centenarians) and their families to learn more about the biological, psychological, and social factors that promote healthy aging.
“It seems there’s not a single gene that imparts a strong effect on the ability to get to these older ages,” Perls says. “Instead, it’s the combined effects of probably hundreds of genes, each with weak effects individually, but having the right combination can lead to a very strong effect, especially for living to the oldest ages we study.”
It’s a good idea to be skeptical of claims for a quick fix to aging-related problems. Perls cautions against marketed “anti-aging” measures such as “hormone replacement therapy,” which has little proven benefit for healthy aging and can have severe side effects. “People used to say, ‘the older you get the sicker you get.’ But with common sense, healthy habits such as regular exercise, a healthy weight, avoiding red meat, not smoking, and managing stress, it can be ‘the older you get, the healthier you’ve been,” Perls says.
The key to healthy aging is to engage fully in life—mentally, physically, and socially. “Transitioning to older years isn’t about sitting in a rocking chair and letting the days slip by,” Bernard says. “Older adults have unique experiences, intellectual capital, and emotional involvement that can be shared with younger generations. This engagement is really key to helping our society move forward.”
___________________________________________________________________________
Old Age: Wikipedia
Old age is the range of ages nearing and surpassing the life expectancy of human beings; it is the end of the human life cycle. People of old age are also referred to as: old people, elderly, seniors, senior citizens, elders, or older adults.
Old age is not a definite biological stage: the chronological age denoted as "old age" varies culturally and historically. Some disciplines and domains focus on the aging and the aged, such as the organic processes of aging (senescence), medical studies of the aging process (gerontology), diseases that afflict older adults (geriatrics), technology to support the aging society (gerontechnology), and leisure and sport activities adapted to older people (such as senior sport).
Old people often have limited regenerative abilities and are more susceptible to illness and injury than younger adults. They face social problems related to retirement, loneliness, and ageism.
In 2011, the United Nations proposed a human-rights convention to protect old people.
Definitions:
Definitions of old age include official definitions, sub-group definitions, and four dimensions as follows.
Official definitions:
Most developed Western countries set the retirement age between 62 and 67; this is also generally considered to mark the transition from middle to old age. Having one's age within this range is commonly a requirement to become eligible for senior social programs. In non-Western nations, old age can begin as early as the mid-40s or as late as the 70s.
Old age cannot be universally defined because it is context-sensitive. The United Nations, for example, considers old age to be 60 years or older.
In contrast, a 2001 joint report by the U.S. National Institute on Aging and the World Health Organization [WHO] Regional Office for Africa set the beginning of old age in Sub-Saharan Africa at 50. This lower threshold stems primarily from a different way of thinking about old age in developing nations.
Unlike in the developed world, where chronological age determines retirement, societies in developing countries determine old age according to a person's ability to make active contributions to society. This number is also significantly affected by lower life expectancy rates throughout the developing world.
Sub-group definitions:
Gerontologists have recognized that people experience very different conditions as they approach old age. In developed countries, many people in their 60s and 70s are still fit, active, and able to care for themselves. However, after 80, they generally become increasingly frail, a condition marked by serious mental and physical debilitation.
Therefore, rather than lumping together all people who have been defined as old, some gerontologists have recognized the diversity of old age by defining sub-groups. One study distinguishes the young-old (60 to 69), the middle-old (70 to 79), and the very old (80+).
Another study's sub-grouping is young-old (65 to 74), middle-old (75 to 84), and oldest-old (85+). A third sub-grouping is young-old (65 to 74), old (74 to 84), and old-old (85+).
Describing sub-groups in the 65+ population enables a more accurate portrayal of significant life changes.
Two British scholars, Paul Higgs and Chris Gilleard, have added a "fourth age" sub-group. In British English, the "third age" is "the period in life of active retirement, following middle age". Higgs and Gilleard describe the fourth age as "an arena of inactive, unhealthy, unproductive, and ultimately unsuccessful ageing".
Dimensions:
Key Concepts in Social Gerontology lists four dimensions: chronological, biological, psychological, and social. Wattis and Curran add a fifth dimension: developmental. Chronological age may differ considerably from a person's functional age.
The distinguishing marks of old age normally occur in all five senses at different times and at different rates for different people. In addition to chronological age, people can be considered old because of the other dimensions of old age.
For example, people may be considered old when they become grandparents or when they begin to do less or different work in retirement.
Senior citizen:
Senior citizen is a common euphemism for an old person used in American English, and sometimes in British English. It implies that the person being referred to is retired.
This in turn usually implies that the person is over the retirement age, which varies according to country. Synonyms include old age pensioner or pensioner in British English, and retiree and senior in American English.
Some dictionaries describe widespread use of "senior citizen" for people over the age of 65.
When defined in a legal context, senior citizen is often used for legal or policy-related reasons in determining who is eligible for certain benefits available to the age group.
It is used in general usage instead of traditional terms such as "old person", "old-age pensioner", or "elderly" as a courtesy and to signify continuing relevance of and respect for this population group as "citizens" of society, of senior "rank".
The term was apparently coined in 1938 during a political campaign. Famed caricaturist Al Hirschfeld claimed on several occasions that his father Isaac Hirschfeld invented the term "senior citizen". It has come into widespread use in recent decades in legislation, commerce, and common speech. Especially in less formal contexts, it is often abbreviated as "senior(s)", which is also used as an adjective.
Age qualifications:
The age which qualifies for senior citizen status varies widely. In governmental contexts, it is usually associated with an age at which pensions or medical benefits for the elderly become available. In commercial contexts, where it may serve as a marketing device to attract customers, the age is often significantly lower.
In commerce, some businesses offer customers of a certain age a "senior discount". The age at which these discounts are available varies from 55, 60, 62 or 65 upwards, and other criteria may also apply. Sometimes a special "senior discount card" or other proof of age needs to be produced to show entitlement.
In the United States, the standard retirement age is currently 66 (gradually increasing to 67).
In Canada, the OAS (Old Age Security) pension is available at 65 (the Conservative government of Stephen Harper had planned to gradually increase the age of eligibility to 67, starting in the years 2023–2029, although the Liberal government of Justin Trudeau is considering leaving it at 65), and the CPP (Canada Pension Plan) as early as age 60.
The AARP allows couples in which one spouse has reached the age of 50 to join, regardless of the age of the other spouse.
Signs:
See also: Aging § Signs
The distinguishing characteristics of old age are both physical and mental. The marks of old age are so unlike the marks of middle age that legal scholar Richard Posner suggests that, as an individual transitions into old age, that person can be thought of as different people "time-sharing" the same identity.
These marks do not occur at the same chronological age for everyone. Also, they occur at different rates and order for different people. Marks of old age can easily vary between people of the same chronological age.
A basic mark of old age that affects both body and mind is "slowness of behavior". The term describes a correlation between advancing age and slowness of reaction and physical and mental task performance. However, studies from Buffalo University and Northwestern University have shown that the elderly are a happier age group than their younger counterparts.
Physical:
Physical marks of old age include the following:
Mental:
Mental marks of old age include the following:
Perspectives:
Middle age:
Many books written by authors in middle adulthood depict a few common perceptions on old age. One writer notices the change in his parents: They move slowly, they have less strength, they repeat stories, their minds wander, and they fret. Another writer sees her aged parents and is bewildered: They refuse to follow her advice, they are obsessed with the past, they avoid risk, and they live at a "glacial pace".
In her The Denial of Aging, Dr. Muriel R. Gillick, a baby boomer, accuses her contemporaries of believing that by proper exercise and diet they can avoid the scourges of old age and proceed from middle age to death.
Studies find that many people in the 55–75 range can postpone morbidity by practicing healthy lifestyles. However, at about age 80, most people experience similar morbidity. Even with healthy lifestyles, most 85+ people will undergo extended "frailty and disability".
Old age:
Early old age can be a pleasant time; children are grown, work is over, and there is time to pursue other interests. Many old people are also willing to get involved in community and activist organizations to promote their well-being. In contrast, perceptions of old age by writers 80+ years old tend to be negative.
Georges Minois [Wikidata] writes that the first man known to talk about his old age was an Egyptian scribe who lived 4,500 years ago. The scribe addressed God with a prayer of lament:
Minois comments that the scribe's "cry shows that nothing has changed in the drama of decrepitude between the age of the Pharaoh and the atomic age" and "expresses all the anguish of old people in the past and the present".
Lillian Rubin, active in her 80s as an author, sociologist, and psychotherapist, opens her book 60 on Up: The Truth about Aging in America with "getting old sucks. It always has, it always will." Dr. Rubin contrasts the "real old age" with the "rosy pictures" painted by middle-age writers.
Writing at the age of 87, Mary C. Morrison describes the "heroism" required by old age: to live through the disintegration of one's own body or that of someone you love. Morrison concludes, "old age is not for the fainthearted".
In the book Life Beyond 85 Years, the 150 interviewees had to cope with physical and mental debilitation and with losses of loved ones. One interviewee described living in old age as "pure hell".
Research has shown that in high-income countries, on average, one in four people over 60 and one in three over 75 feels lonely.
Misconceptions:
Johnson and Barer did a pioneering study of Life Beyond 85 Years by interviews over a six-year period. In talking with 85-year-olds and older, they found some popular conceptions about old age to be erroneous. Such erroneous conceptions include:
In their interviews, Johnson and Barer found that 24% of the 85+ had no face-to-face family relationships; many have outlived their families. Second, that contrary to popular notions, the interviews revealed that the reduced activity and socializing of the over-85s does not harm their well-being; they "welcome increased detachment".
Third, rather than a continuity of self-concept, as the interviewees faced new situations they changed their "cognitive and emotional processes" and reconstituted their "self–representation".
Societal and historical:
Based on his survey of old age in history, Georges Minois concludes that "it is clear that always and everywhere youth has been preferred to old age". In Western thought, "old age is an evil, an infirmity and a dreary time of preparation for death". Furthermore, death is often preferred over "decrepitude, because death means deliverance".
"The problem of the ambiguity of old age has . . . been with us since the stage of primitive society; it was both the source of wisdom and of infirmity, experience and decrepitude, of prestige and suffering."
In the Classical period of Greek and Roman cultures, old age was denigrated as a time of "decline and decrepitude". "Beauty and strength" were esteemed and old age was viewed as defiling and ugly. Old age was reckoned as one of the unanswerable "great mysteries" along with evil, pain, and suffering. "Decrepitude, which shrivels heroes, seemed worse than death."
Historical periods reveal a mixed picture of the "position and status" of old people, but there has never been a "golden age of aging". Studies have challenged the popular belief that in the past old people were venerated by society and cared for by their families.
Veneration for and antagonism toward the aged have coexisted in complex relationships throughout history. "Old people were respected or despised, honoured or put to death according to circumstance."
In ancient times, although some strong and healthy people lived until they were over 70, most died before they were 50. The general understanding is that those who lived into their 40s were treated with respect and awe. In contrast, those who were frail were seen as a burden and ignored or, in extreme cases, killed.
People were defined as "old" because of their inability to perform useful tasks rather than their years.
Although he was skeptical of the gods, Aristotle concurred in the dislike of old people. In his Ethics, he wrote that "old people are miserly; they do not acknowledge disinterested friendship; only seeking for what can satisfy their selfish needs".
The Medieval and Renaissance periods depicted old age as "cruel or weak".
The 16th-century Utopians Thomas More and Antonio de Guevara allowed no decrepit old people in their fictional lands.
For Thomas More, on the island of Utopia, when people are so old as to have "out-lived themselves" and are terminally ill, in pain, and a burden to everyone, the priests exhort them about choosing to die. The priests assure them that "they shall be happy after death". If they choose to die, they end their lives by starvation or by taking opium.
Antonio de Guevara's utopian nation "had a custom, not to live longer than sixty five years". At that age, they practiced self-immolation. Rather than condemn the practice, Bishop Guevara called it a "golden world" in which people "have overcome the natural appetite to desire to live".
Contemporary Perspectives:
In the Modern period, the "cultural status" of old people has declined in many cultures. Joan Erikson observed that "aged individuals are often ostracized, neglected, and overlooked; elders are seen no longer as bearers of wisdom but as embodiments of shame".
Attitudes toward old age well being vary somewhat between cultures. For example, in the United States being healthy, physically, and socially active are signs of a good old age. On the other hand, Africans focus more on food and material security and a helpful family when describing old age well being. Additionally, Koreans are more anxious about aging, and more scared of old people than Americans are.
Research on age-related attitudes consistently finds that negative attitudes exceed positive attitudes toward old people because of their looks and behavior. In his study Aging and Old Age, Posner discovers "resentment and disdain of older people" in American society.
Harvard University's implicit-association test measures implicit "attitudes and beliefs" about "Young vis a vis Old".
Blind Spot: Hidden Biases of Good People, a book about the test, reports that 80% of Americans have an "automatic preference for the young over old" and that attitude is true worldwide. The young are "consistent in their negative attitude" toward the old.
Ageism documents that Americans generally have "little tolerance for older persons and very few reservations about harboring negative attitudes" about them.
Despite its prevalence, ageism is seldom the subject of public discourse.
Simulated:
Simone de Beauvoir wrote that "there is one form of experience that belongs only to those that are old – that of old age itself". Nevertheless, simulations of old age attempt to help younger people gain some understanding.
Texas A&M University offers a plan for an "Aging Simulation" workshop. The workshop is adapted from Sensitizing People to the Processes of Aging. Some of the simulations include:
The Macklin Intergenerational Institute conducts Xtreme Aging workshops, as depicted in The New York Times. A condensed version was presented on NBC's Today Show and is available online.
One exercise was to lay out 3 sets of 5 slips of paper. On set #1, write your 5 most enjoyed activities; on set #2, write your 5 most valued possessions; on set #3, write your 5 most loved people. Then "lose" them one by one, trying to feel each loss, until you have lost them all, as happens in old age.
Frailty:
Most people in the age range of 60–80 (the years of retirement and early old age), enjoy rich possibilities for a full life, but the condition of frailty distinguished by "bodily failure" and greater dependence becomes increasingly common after that. In the United States, hospital discharge data from 2003 to 2011 shows that injury was the most common reason for hospitalization among patients aged 65+.
Gerontologists note the lack of research regarding and the difficulty in defining frailty. However, they add that physicians recognize frailty when they see it.
A group of geriatricians proposed a general definition of frailty as "a physical state of increased vulnerability to stressors that results from decreased reserves and dis-regulation in multiple physiological systems".
Frailty is a common condition in later old age but different definitions of frailty produce diverse assessments of prevalence.
One study placed the incidence of frailty for ages 65+ at 10.7%. Another study placed the incidence of frailty in age 65+ population at 22% for women and 15% for men. A Canadian study illustrated how frailty increases with age and calculated the prevalence for 65+ as 22.4% and for 85+ as 43.7%.
A worldwide study of "patterns of frailty" based on data from 20 nations found (a) a consistent correlation between frailty and age, (b) a higher frequency among women, and (c) more frailty in wealthier nations where greater support and medical care increases longevity.
In Norway, a 20-year longitudinal study of 400 people found that bodily failure and greater dependence became prevalent in the 80+ years. The study calls these years the "fourth age" or "old age in the real meaning of the term".
Similarly, the "Berlin Aging Study" rated over-all functionality on four levels: good, medium, poor, and very poor. People in their 70s were mostly rated good. In the 80–90 year range, the four levels of functionality were divided equally.
By the 90–100 year range, 60% would be considered frail because of very poor functionality and only 5% still possessed good functionality.
Markers:
Three unique markers of frailty have been proposed: (a) loss of any notion of invincibility, (b) loss of ability to do things essential to one's care, and (c) loss of possibility for a subsequent life stage.
Old age survivors on-average deteriorate from agility in their 65–80s to a period of frailty preceding death. This deterioration is gradual for some and precipitous for others. Frailty is marked by an array of chronic physical and mental problems which means that frailty is not treatable as a specific disease.
These problems coupled with increased dependency in the basic activities of daily living (ADLs) required for personal care add emotional problems: depression and anxiety. In sum, frailty has been depicted as a group of "complex issues", distinct but "causally interconnected", that often include "comorbid diseases", progressive weakness, stress, exhaustion, and depression.
Care and costs:
Frail people require a high level of care. Medical advances have made it possible to "postpone death" for years. This added time costs many frail people "prolonged sickness, dependence, pain, and suffering".
According to a study by the Agency for Healthcare Research and Quality (AHRQ), the rate of emergency department visits was consistently highest among patients ages 85 years and older in 2006–2011 in the United States.
Additionally, patients aged 65+ had the highest percentage of hospital stays for adults with multiple chronic conditions but the second highest percentage of hospital costs in 2003–2014.
These final years are also costly in economic terms. One out of every four Medicare dollars is spent on the frail in their last year of life . . . in attempts to postpone death.
Medical treatments in the final days are not only economically costly, they are often unnecessary, even harmful. Nortin Hadler, M.D. warns against the tendency to medicalize and overtreat the frail.
In his Choosing Medical Care in Old Age, Michael R. Gillick M.D. argues that appropriate medical treatment for the frail is not the same as for the robust. The frail are vulnerable to "being tipped over" by any physical stress put on the system such as medical interventions.
In addition to everyday care, frail elderly people and others with disabilities are particularly vulnerable during natural disasters. They may be unable or unwilling to evacuate to avoid a hurricane or wildfire.
Death:
Old age, death, and frailty are linked because approximately half the deaths in old age are preceded by months or years of frailty.
Older Adults' Views on Death is based on interviews with 109 people in the 70–90 age range, with a mean age of 80.7. Almost 20% of the people wanted to use whatever treatment that might postpone death. About the same number said that, given a terminal illness, they would choose assisted suicide.
Roughly half chose doing nothing except live day by day until death comes naturally without medical or other intervention designed to prolong life. This choice was coupled with a desire to receive palliative care if needed.
About half of older adults have multimorbidity, that is, they have three or more chronic conditions. Medical advances have made it possible to "postpone death", but in many cases this postponement adds "prolonged sickness, dependence, pain, and suffering", a time that is costly in social, psychological, and economic terms.
The longitudinal interviews of 150 age 85+ people summarized in Life Beyond 85 Years found "progressive terminal decline" in the year prior to death: constant fatigue, much sleep, detachment from people, things, and activities, simplified lives.
Most of the interviewees did not fear death; some would welcome it. One person said, "Living this long is pure hell." However, nearly everyone feared a long process of dying. Some wanted to die in their sleep; others wanted to die "on their feet".
The study of Older Adults' Views on Death found that the more frail people were, the more "pain, suffering, and struggles" they were enduring, the more likely they were to "accept and welcome" death as a release from their misery.
Their fear about the process of dying was that it would prolong their distress. Besides being a release from misery, some saw death as a way to reunion with departed loved ones. Others saw death as a way to free their caretakers from the burden of their care.
Religiosity:
Generally speaking, old people have always been more religious than young people. At the same time, wide cultural variations exist.
In the United States, 90% of old age Hispanics view themselves as very, quite, or somewhat religious. The Pew Research Center's study of black and white old people found that 62% of those in ages 65–74 and 70% in ages 75+ asserted that religion was "very important" to them.
For all 65+ people, more women (76%) than men (53%) and more blacks (87%) than whites (63%) consider religion "very important" to them. This compares to 54% in the 30–49 age range.
In a British 20-year longitudinal study, less than half of the old people surveyed said that religion was "very important" to them, and a quarter said they had become less religious in old age.
The late-life rise in religiosity is stronger in Japan than in the United States, but in the Netherlands it is minimal.
In the practice of religion, a study of 60+ people found that 25% read the Bible every day and over 40% look at religious TV. Pew Research found that in the age 65+ range, 75% of whites and 87% of blacks pray daily.
When comparing religiosity, the individual practice may be a more accurate measure than participation in organized religion. With organized religion, participation may often be hindered due to transportation or health problems.
Demographic changes:
In the industrialized countries, life expectancy and, thus, the old age population have increased consistently over the last decades.
In the United States the proportion of people aged 65 or older increased from 4% in 1900 to about 12% in 2000.
In 1900, only about 3 million of the nation's citizens were 65 or older (out of 76 million total American citizens).
By 2000, the number of senior citizens had increased to about 35 million (of 280 million US citizens). Population experts estimate that more than 50 million Americans—about 17 percent of the population—will be 65 or older in 2020. By 2050, it is projected that at least 400,000 Americans will be 100 or older.
The number of old people is growing around the world chiefly because of the post–World War II baby boom and increases in the provision and standards of health care. By 2050, 33% of the developed world's population and almost 20% of the less developed world's population will be over 60 years old.
The growing number of people living to their 80s and 90s in the developed world has strained public welfare systems and has also resulted in increased incidence of diseases like cancer and dementia that were rarely seen in premodern times.
When the United States Social Security program was created, people older than 65 numbered only around 5% of the population and the average life expectancy of a 65-year-old in 1936 was approximately 5 years, while in 2011 it could often range from 10 to 20 years.
Other issues that can arise from an increasing population are growing demands for health care and an increase in demand for different types of services.
Of the roughly 150,000 people who die each day across the globe, about two thirds—100,000 per day—die of age-related causes. In industrialized nations, the proportion is much higher, reaching 90%.
Psychosocial aspects:
According to Erik Erikson's "Stages of Psychosocial Development", the human personality is developed in a series of eight stages that take place from the time of birth and continue on throughout an individual's complete life. He characterises old age as a period of "Integrity vs. Despair", during which a person focuses on reflecting back on his life.
Those who are unsuccessful during this phase will feel that their life has been wasted and will experience many regrets. The individual will be left with feelings of bitterness and despair. Those who feel proud of their accomplishments will feel a sense of integrity.
Successfully completing this phase means looking back with few regrets and a general feeling of satisfaction. These individuals will attain wisdom, even when confronting death. Coping is a very important skill needed in the aging process to move forward with life and not be 'stuck' in the past. The way a person adapts and copes, reflects his aging process on a psycho-social level.
For people in their 80s and 90s, Joan Erikson added a ninth stage in The Life Cycle Completed: Extended Version. As she wrote, she added the ninth stage because the Integrity of the eighth stage imposes "a serious demand on the senses of elders" and the Wisdom of the eighth stage requires capacities that ninth stage elders "do not usually have".
Newman & Newman also proposed a ninth stage of life, Elderhood. Elderhood refers to those individuals who live past the life expectancy of their birth cohorts. They described two different types of people in this stage of life. The "young old" are the healthy individuals who can function on their own without assistance and can complete their daily tasks independently, while the "old old" are those who depend on specific services due to declining health or diseases.
Theories:
Social theories, or concepts, propose explanations for the distinctive relationships between old people and their societies.
One theory, proposed in 1961, is the disengagement theory, which proposes that, in old age, a mutual disengagement between people and their society occurs in anticipation of death. By becoming disengaged from work and family responsibilities, according to this concept, people are enabled to enjoy their old age without stress.
This theory has been subjected to the criticism that old age disengagement is neither natural, inevitable, nor beneficial. Furthermore, disengaging from social ties in old age is not across the board: unsatisfactory ties are dropped and satisfying ones kept.
In opposition to the disengagement theory, the activity theory of old age argues that disengagement in old age occurs not by desire, but by the barriers to social engagement imposed by society.
This theory has been faulted for not factoring in psychological changes that occur in old age as shown by reduced activity, even when available. It has also been found that happiness in old age is not proportional to activity.
According to the continuity theory, in spite of the inevitable differences imposed by their old age, most people try to maintain continuity in personhood, activities, and relationships with their younger days.
Socioemotional selectivity theory also depicts how people maintain continuity in old age. The focus of this theory is continuity sustained by social networks, albeit networks narrowed by choice and by circumstances. The choice is for more harmonious relationships. The circumstances are loss of relationships by death and distance.
Life expectancy:
Life expectancy by nation at birth in the year 2011 ranged from 48 years to 82. Low values indicate high death rates for infants and children.
In most parts of the world women live, on average, longer than men; even so, the disparities vary between 12 years in Russia to no difference or higher life expectancy for men in countries such as Zimbabwe and Uganda.
The number of elderly people worldwide began to surge in the second half of the 20th century. In developed countries before then, five or less percent of the population was over 65. Few lived longer than their 70s and people who attained advanced age (i.e. their 80s) were rare enough to be a novelty and were revered as wise sages.
The worldwide over-65 population in 1960 was one-third of the under-5 population. By 2013, the over-65 population had grown to equal the under-5 population and is projected to double the under-5 population by 2050.
Before the surge in the over-65 population, accidents and disease claimed many people before they could attain old age, and health problems in those over 65 meant a quick death in most cases. If a person lived to an advanced age, it was due to genetic factors and/or a relatively easy lifestyle, since diseases of old age could not be treated before the 20th century.
In October 2016, a group of scientists identified the maximum human lifespan at an average age of 115, with an absolute upper limit of 125 years. However, the concept of a maximum lifespan of humans is still widely debated among the scientific community.
Benefits:
German chancellor Otto von Bismarck created the world's first comprehensive government social safety net in the 1880s, providing for old age pensions.
In the United States of America, and the United Kingdom, 65 (UK 60 for women) was traditionally the age of retirement with full old age benefits.
In 2003, the age at which a United States citizen became eligible for full Social Security benefits began to increase gradually, and will continue to do so until it reaches 67 in 2027.
Full retirement age for Social Security benefits for people retiring in 2012 is age 66. In the United Kingdom, the state pension age for men and women will rise to 66 in 2020 with further increases scheduled after that.
Originally, the purpose of old age pensions was to prevent elderly people from being reduced to beggary, which is still common in some underdeveloped countries, but growing life expectancies and older populations have brought into question the model under which pension systems were designed.
By 1990, the United States was spending 30 per cent of its budget on the elderly, compared with 2 per cent on education. The dominant perception of the American old age population changed from "needy" and "worthy" to "powerful" and "greedy", old people getting more than their share of the nation's resources.
However, in 2011, using a Supplemental Poverty Measure (SPM), the old age American poverty rate was measured as 15.9%.
Assistance: devices and personal
In the United States in 2008, 11 million people aged 65+ lived alone: 5 million or 22% of ages 65–74, 4 million or 34% of ages 75–84, and 2 million or 41% of ages 85+. The 2007 gender breakdown for all people 65+ was men 19% and women 39%.
Many new assistive devices made especially for the home have enabled more old people to care for their own activities of daily living (ADL).
Some examples of devices are:
A Swedish study found that at age 76, 46% of the subjects used assistive devices. When they reached age 86, 69% used them. The subjects were ambivalent regarding the use of the assistive devices: as "enablers" or as "disablers".
People who view assistive devices as enabling greater independence accept and use them, whereas those who see them as symbols of disability reject them.
However, organizations like Love for the Elderly aim to combat such age-related prejudice by educating the public about the importance of appreciating growing older, while also providing services of kindness to elders in senior homes.
Even with assistive devices as of 2006, 8.5 million Americans needed personal assistance because of impaired basic activities of daily living required for personal care or impaired instrumental activities of daily living (IADL) required for independent living.
Projections place this number at 21 million by 2030 when 40% of Americans over 70 will need assistance. There are many options for such long-term care to those who require it.
There is home care in which a family member, volunteer, or trained professional will aid the person in need and help with daily activities. Another option is community services which can provide the person with transportation, meal plans, or activities in senior centers.
A third option is assisted living where 24-hour round-the-clock supervision is given with aid in eating, bathing, dressing, etc. A final option is a nursing home which provides professional nursing care.
Culture:
In 2014, a documentary film called The Age of Love used humor and the poignant adventures of 30 seniors who attend a speed dating event for 70 to 90-year-olds and discover how the search for romance changes—or does not change—from childhood to old age.
Artistic depiction:
Scholarly literature has emerged, especially in Britain, showing historical trends in the visual depiction of old age.
See also:
Life extension
Life extension is the concept of extending the human lifespan, either modestly through improvements in medicine or dramatically by increasing the maximum lifespan beyond its generally-settled limit of 125 years.
Several researchers in the area, along with "life extensionists", "immortalists" or "longevists" (those who wish to achieve longer lives themselves), postulate that future breakthroughs in:
The above will eventually enable humans to have indefinite lifespans (agerasia) through complete rejuvenation to a healthy youthful condition. The ethical ramifications, if life extension becomes a possibility, are debated by bioethicists.
The sale of purported anti-aging products such as supplements and hormone replacement is a lucrative global industry. For example, the industry that promotes the use of hormones as a treatment for consumers to slow or reverse the aging process in the US market generated about $50 billion of revenue a year in 2009.
The use of such hormone products has not been proven to be effective or safe.
Average life expectancy and lifespan:
Main article: Senescence
During the process of aging, an organism accumulates damage to its macromolecules, cells, tissues, and organs.
Specifically, aging is characterized as and thought to be caused by:
Oxidation damage to cellular contents caused by free radicals is believed to contribute to aging as well.
The longest documented human lifespan is 122 years 164 days, the case of Jeanne Calment who according to records was born in 1875 and died in 1997, whereas the maximum lifespan of a wildtype mouse, commonly used as a model in research on aging, is about three years.
Genetic differences between humans and mice that may account for these different aging rates include differences in efficiency of DNA repair, antioxidant defenses, energy metabolism, proteostasis maintenance, and recycling mechanisms such as autophagy.
The average life expectancy in a population is lowered by infant and child mortality, which are frequently linked to infectious diseases or nutrition problems.
Later in life, vulnerability to accidents and age-related chronic disease such as cancer or cardiovascular disease play an increasing role in mortality. Extension of life expectancy and lifespan can often be achieved by access to improved medical care, vaccinations, good diet, exercise, and avoidance of hazards such as smoking.
Maximum lifespan is determined by the rate of aging for a species inherent in its genes and by environmental factors. Widely recognized methods of extending maximum lifespan in model organisms such as nematodes, fruit flies, and mice include caloric restriction, gene manipulation, and administration of pharmaceuticals.
Another technique uses evolutionary pressures such as breeding from only older members or altering levels of extrinsic mortality. Some animals such as hydra, planarian flatworms, and certain sponges, corals, and jellyfish do not die of old age and exhibit potential immortality.
Strategies:
See also: Ageing § Prevention and delay, and Brain aging
Senolytics and prolongevity drugs:
See also: Geroprotector and MTOR inhibitors § Rapamycin and rapalogs
This section is an excerpt from Senolytic.
A senolytic (from the words senescence and -lytic, "destroying") is among a class of small molecules under basic research to determine if they can selectively induce death of senescent cells and improve health in humans. A goal of this research is to discover or develop agents to delay, prevent, alleviate, or reverse age-related diseases.
A related concept is "senostatic", which means to suppress senescence.Senolytics eliminate senescent cells whereas senomorphics – with candidates such as Apigenin, Everolimus and Rapamycin – modulate properties of senescent cells without eliminating them, suppressing phenotypes of senescence, including the SASP.
Senomorphic effects may be one major effect mechanism of a range of prolongevity drug candidates. Such candidates are, however, typically not studied for just one mechanism, but multiple.
There are biological databases of prolongevity drug candidates under research as well as of potential gene/protein targets. These are enhanced by the following:
Recently, artificial intelligence has been used to discover new senolytics, resulting in the identification of structurally distinct senolytic compounds with more favorable medicinal chemistry properties than previous senolytic candidates.
Such strategies as well as testing with model organisms and xenografts may attempt to or help address difficulties of trials with humans which have relatively long lifespans (compared to other animals) as well as the (larger) need to protect human health from early-trial-stage interventions (in clinical trials).
Besides rapamycin and senolytics, the drug-repurposing candidates studied most extensively include:
Many prolongevity drugs are synthetic alternatives or potential complements to existing nutraceuticals, such as various sirtuin-activating compounds under investigation like SRT2104.
In some cases pharmaceutical administration is combined with that of neutraceuticals – such as in the case of glycine combined with NAC. Often studies are structured based on or thematize specific prolongevity targets, listing both nutraceuticals and pharmaceuticals (together or separately) such as FOXO3-activators.
Researchers are also exploring ways to mitigate side-effects from such substances (possibly most notably rapamycin and its derivatives) such as via protocols of intermittent administration and have called for research that helps determine optimal treatment schedules (including timing) in general.
Diets and supplements:
Vitamins and antioxidants:
See also: Inflammaging and DNA damage theory of aging
The free-radical theory of aging suggests that antioxidant supplements might extend human life. Reviews, however, have found that use of vitamin A (as β-carotene) and vitamin E supplements possibly can increase mortality. Other reviews have found no relationship between vitamin E and other vitamins with mortality.
Vitamin D supplementation of various dosages is investigated in trials and there also is research into GlyNAC (see above).
Complications:
Complications of antioxidant supplementation (especially continuous high dosages far above the RDA) include that reactive oxygen species (ROS), which are mitigated by antioxidants, "have been found to be physiologically vital for signal transduction, gene regulation, and redox regulation, among others, implying that their complete elimination would be harmful".
In particular, one way of multiple they can be detrimental is by inhibiting adaptation to exercise such as muscle hypertrophy (e.g. during dedicated periods of caloric surplus).
There is also research into stimulating/activating/fueling endogenous antioxidant generation, in particular e.g. of neutraceutical glycine and pharmaceutical NAC. Antioxidants can change the oxidation status of different e.g. tissues, targets or sites each with potentially different implications, especially for different concentrations.
A review suggests mitochondria have a hormetic response to ROS, whereby low oxidative damage can be beneficial.
Dietary restriction:
Main article: Diet and longevity
See also: Caloric restriction mimetic
As of 2021, there is no clinical evidence that any dietary practice contributes to human longevity.
Healthy diet:
Research suggests that increasing adherence to Mediterranean diet patterns is associated with a reduction in total and cause-specific mortality, extending health- and lifespan.
Research is identifying the key beneficial components of the Mediterranean diet. It shares various characteristics with the similarly beneficial Okinawa diet. Potential anti-aging mechanisms of various nutrients are not yet understood.
Shares of macronutrients and level of caloric intake may also be of significance, including in periods when no dietary restriction occurs – such as not having a fat-intake that is too low and not having a prolonged caloric surplus or caloric deficit that is too large.
Studies suggest dietary changes are a major cause of national relative rises in life-span.
Microbiome:
Mechanistically, research suggests that the gut microbiome, which varies per person and changes throughout lifespan, is also involved in the beneficial effects, due to which various diet supplementations with prebiotics, various diverse (multi-strain) probiotics and synbiotics, and fecal microbiota transplantation are being investigated for life extension, mainly for prolonging healthspan, with many important questions being unresolved.
Optimal diet:
See also: Sustainable consumption § Sustainable food consumption
Approaches to develop optimal diets for health- and lifespan (or "longevity diets") include:
Nutraceuticals:
See also: Anti-aging supplements
Beyond, research into senolytics and (synthetic) prolongevity-drugs, vitamins and antioxidants, prebiotics and probiotics, there are neutraceuticals – dietary supplements and bioactive plant compounds (phytochemicals) but not pharmaceuticals – that are being investigated in life sciences, nutrition science and gerontology for potential health- and lifespan extension in healthy humans.
Sometimes, their use is researched or recommended as a way to correct nutritional deficiencies from switching to otherwise healthy foods – in particular from replacing meat consumption with a higher intake of plant-based foods.
Especially, but not only, in such cases the supplementation of minerals and various specific micronutrients is investigated. Correcting magnesium deficiency for instance could prolong life. Many supplements are researched primarily for potential improvements in health and healthspan rather than for extending lifespan.
Some studies hypothesize that relative health and longevity benefits of various foods and diets can be largely or to a large part attributed to the nutraceuticals they contain.
Some studies suggest increasing the intake of specific foods (see above) based on such results, while some investigate supplementation, including of dosages that are impractical to achieve with whole foods.
Researched substances include various polyphenols such as pterostilbene or flavonoids, notably epicatechin. Some herbal-extracts like rhodiola rosea are also being investigated due to results of tests with model organisms. Some of these are AMPK activators and hence caloric restriction mimetics (some possibly exercise mimetics as well). AMPK activators include resveratrol and berberine.
Many such nutraceuticals are also potent antioxidants. Like prolongevity-drugs and bioactive compounds in general, they can have multiple potential effect mechanisms, the polyphenol resveratrol for instance also activates possibly pro-longevity sirtuin activity.
A common issue with many already-existing natural nutraceuticals like resveratrol is their low bioavailability. Their side-effects are often low compared to several major longevity drug candidates. On the other hand, they are considered to often have "intrinsic natural bio-compatibility and safety". Some of the compounds can have a "biphasic dose response" (a trait/effect of hormesis) whereby they (can) have beneficial effects at low or moderate doses and toxic effects at high doses.
Other approaches:
Further advanced biosciences-based approaches include:
Within the field:
See also: Biogerontology
There is a need and research into the development of aging biomarkers such as the epigenetic clock "to assess the ageing process and the efficacy of interventions to bypass the need for large-scale longitudinal studies".
Such biomarkers may also include in vivo brain imaging.
Reviews sometimes include structured tables that provide systematic overviews of intervention/drug candidates with a review calling for integrating "current knowledge with multi-omics, health records, and drug safety data to predict drugs that can improve health in late life" and listing major outstanding questions.
Biological databases of prolongevity drug candidates under research as well as of potential gene/protein targets include GenAge, DrugAge and Geroprotectors.
A review has pointed out that the approach of "'epidemiological' comparison of how a low versus a high consumption of an isolated macronutrient and its association with health and mortality may not only fail to identify protective or detrimental nutrition patterns but may lead to misleading interpretations".
It proposes a multi-pillar approach, and summarizes findings towards constructing – multi-system-considering and at least age-personalized dynamic – refined longevity diets.
Epidemiological-type observational studies included in meta-analyses should according to the study at least be complemented by "(1) basic research focused on lifespan and healthspan, (2) carefully controlled clinical trials, and (3) studies of individuals and populations with record longevity"
Hormone treatment:
The anti-aging industry offers several hormone therapies. Some of these have been criticized for possible dangers and a lack of proven effect. For example, the American Medical Association has been critical of some anti-aging hormone therapies.
While growth hormone (GH) decreases with age, the evidence for use of growth hormone as an anti-aging therapy is mixed and based mostly on animal studies. There are mixed reports that GH or IGF-1 modulates the aging process in humans and about whether the direction of its effect is positive or negative.
Klotho and exerkines (see above) like irisin are being investigated for potential pro-longevity therapies.
Lifestyle factors:
See also: Lifestyle disease
The following are investigated as potential (modulatable) factors of life extension:
Healthy lifestyle practices and healthy diet have been suggested as "first-line function-preserving strategies, with pharmacological agents, including existing and new pharmaceuticals and novel 'nutraceutical' compounds, serving as potential complementary approaches".
Societal strategies
See also:
Collectively, addressing common causes of death could extend lifespans of populations and humanity overall. For instance, a 2020 study indicates that the global mean loss of life expectancy (LLE) from air pollution in 2015 was 2.9 years, substantially more than, for example, 0.3 years from all forms of direct violence, albeit a significant fraction of the LLE (a measure similar to years of potential life lost) is considered to be unavoidable.
Regular screening and doctor visits has been suggested as a lifestyle-societal intervention. (See also: medical test and biomarker)
Health policy and changes to standard healthcare could support the adoption of the field's conclusions – a review suggests that the longevity diet would be a "valuable complement to standard healthcare and that, taken as a preventative measure, it could aid in avoiding morbidity, sustaining health into advanced age" as a form of preventive healthcare.
It has been suggested that in terms of healthy diets, Mediterranean-style diets could be promoted by countries for ensuring healthy-by-default choices ("to ensure the healthiest choice is the easiest choice") and with highly effective measures including dietary education, food checklists and recipes that are "simple, palatable, and affordable".
A review suggests that "targeting the aging process per se may be a far more effective approach to prevent or delay aging-associated pathologies than treatments specifically targeted to particular clinical conditions".
Low ambient temperature:
Low ambient temperature as a physical factor affecting free radical levels was identified as a treatment producing exceptional lifespan increase in Drosophila melanogaster and other living beings.
History:
Further information: Timeline of senescence research
The extension of life has been a desire of humanity and a mainstay motif in the history of scientific pursuits and ideas throughout history, from the Sumerian Epic of Gilgamesh and the Egyptian Smith medical papyrus, all the way through:
However, the beginning of the modern period in this endeavor can be traced to the end of the 19th – beginning of the 20th century, to the so-called "fin-de-siècle" (end of the century) period, denoted as an "end of an epoch" and characterized by the rise of scientific optimism and therapeutic activism, entailing the pursuit of life extension (or life-extensionism).
Among the foremost researchers of life extension at this period were the Nobel Prize winning biologist Elie Metchnikoff (1845-1916) -- the author of the cell theory of immunity and vice director of Institut Pasteur in Paris, and Charles-Édouard Brown-Séquard (1817-1894) -- the president of the French Biological Society and one of the founders of modern endocrinology.
Sociologist James Hughes claims that science has been tied to a cultural narrative of conquering death since the Age of Enlightenment. He cites Francis Bacon (1561–1626) as an advocate of using science and reason to extend human life, noting Bacon's novel New Atlantis, wherein scientists worked toward delaying aging and prolonging life.
Robert Boyle (1627–1691), founding member of the Royal Society, also hoped that science would make substantial progress with life extension, according to Hughes, and proposed such experiments as "to replace the blood of the old with the blood of the young".
Biologist Alexis Carrel (1873–1944) was inspired by a belief in indefinite human lifespan that he developed after experimenting with cells, says Hughes.
Regulatory and legal struggles between the Food and Drug Administration (FDA) and the Life Extension organization included seizure of merchandise and court action. In 1991, Saul Kent and Bill Faloon, the principals of the organization, were jailed for four hours and were released on $850,000 bond each. After 11 years of legal battles, Kent and Faloon convinced the US Attorney's Office to dismiss all criminal indictments brought against them by the FDA.
In 2003, Doubleday published "The Immortal Cell: One Scientist's Quest to Solve the Mystery of Human Aging," by Michael D. West. West emphasised the potential role of embryonic stem cells in life extension.
Other modern life extensionists include:
Scientific research:
See also: Timeline of senescence research
In 1991, the American Academy of Anti-Aging Medicine (A4M) was formed. The American Board of Medical Specialties recognizes neither anti-aging medicine nor the A4M's professional standing.
In 2003, Aubrey de Grey and David Gobel formed the Methuselah Foundation, which gives financial grants to anti-aging research projects. In 2009, de Grey and several others founded the SENS Research Foundation, a California-based scientific research organization which conducts research into aging and funds other anti-aging research projects at various universities.
In 2013, Google announced Calico, a new company based in San Francisco that will harness new technologies to increase scientific understanding of the biology of aging. It is led by Arthur D. Levinson, and its research team includes scientists such as Hal V. Barron, David Botstein, and Cynthia Kenyon.
In 2014, biologist Craig Venter founded Human Longevity Inc., a company dedicated to scientific research to end aging through genomics and cell therapy. They received funding with the goal of compiling a comprehensive human genotype, microbiome, and phenotype database.
Aside from private initiatives, aging research is being conducted in university laboratories, and includes universities such as Harvard and UCLA. University researchers have made a number of breakthroughs in extending the lives of mice and insects by reversing certain aspects of aging.
Ethics and politics:
Scientific controversy:
Some critics dispute the portrayal of aging as a disease. For example, Leonard Hayflick, who determined that fibroblasts are limited to around 50 cell divisions, reasons that aging is an unavoidable consequence of entropy. Hayflick and fellow biogerontologists Jay Olshansky and Bruce Carnes have strongly criticized the anti-aging industry in response to what they see as unscrupulous profiteering from the sale of unproven anti-aging supplements.
Consumer motivations:
Research by Sobh and Martin (2011) suggests that people buy anti-aging products to obtain a hoped-for self (e.g., keeping a youthful skin) or to avoid a feared-self (e.g., looking old). The research shows that when consumers pursue a hoped-for self, it is expectations of success that most strongly drive their motivation to use the product.
The research also shows why doing badly when trying to avoid a feared self is more motivating than doing well. When product use is seen to fail it is more motivating than success when consumers seek to avoid a feared-self.
Political parties:
Though many scientists state that life extension and radical life extension are possible, there are still no international or national programs focused on radical life extension. There are political forces staying for and against life extension.
By 2012, in Russia, the United States, Israel, and the Netherlands, the Longevity political parties started. They aimed to provide political support to radical life extension research and technologies, and ensure the fastest possible and at the same time soft transition of society to the next step – life without aging and with radical life extension, and to provide access to such technologies to most currently living people.
Silicon Valley:
Some tech innovators and Silicon Valley entrepreneurs have invested heavily into anti-aging research. These include:
Commentators:
Leon Kass (chairman of the US President's Council on Bioethics from 2001 to 2005) has questioned whether potential exacerbation of overpopulation problems would make life extension unethical. He states his opposition to life extension with the words:
"simply to covet a prolonged life span for ourselves is both a sign and a cause of our failure to open ourselves to procreation and to any higher purpose ... [The] desire to prolong youthfulness is not only a childish desire to eat one's life and keep it; it is also an expression of a childish and narcissistic wish incompatible with devotion to posterity."
John Harris, former editor-in-chief of the Journal of Medical Ethics, argues that as long as life is worth living, according to the person himself, we have a powerful moral imperative to save the life and thus to develop and offer life extension therapies to those who want them.
Transhumanist philosopher Nick Bostrom has argued that any technological advances in life extension must be equitably distributed and not restricted to a privileged few. In an extended metaphor entitled "The Fable of the Dragon-Tyrant", Bostrom envisions death as a monstrous dragon who demands human sacrifices. In the fable, after a lengthy debate between those who believe the dragon is a fact of life and those who believe the dragon can and should be destroyed, the dragon is finally killed. Bostrom argues that political inaction allowed many preventable human deaths to occur.
Overpopulation concerns:
Controversy about life extension is due to fear of overpopulation and possible effects on society. Biogerontologist Aubrey De Grey counters the overpopulation critique by pointing out that the therapy could postpone or eliminate menopause, allowing women to space out their pregnancies over more years and thus decreasing the yearly population growth rate.
Moreover, the philosopher and futurist Max More argues that, given the fact the worldwide population growth rate is slowing down and is projected to eventually stabilize and begin falling, superlongevity would be unlikely to contribute to overpopulation.
Opinion polls:
A Spring 2013 Pew Research poll in the United States found that 38% of Americans would want life extension treatments, and 56% would reject it. However, it also found that 68% believed most people would want it and that only 4% consider an "ideal lifespan" to be more than 120 years.
The median "ideal lifespan" was 91 years of age and the majority of the public (63%) viewed medical advances aimed at prolonging life as generally good. 41% of Americans believed that radical life extension (RLE) would be good for society, while 51% said they believed it would be bad for society.
One possibility for why 56% of Americans claim they would reject life extension treatments may be due to the cultural perception that living longer would result in a longer period of decrepitude, and that the elderly in our current society are unhealthy.
Religious people are no more likely to oppose life extension than the unaffiliated though some variation exists between religious denominations.
Aging as a disease:
Mainstream medical organizations and practitioners do not consider aging to be a disease. Biologist David Sinclair says: "I don't see aging as a disease, but as a collection of quite predictable diseases caused by the deterioration of the body."
The two main arguments used are that aging is both inevitable and universal while diseases are not. However, not everyone agrees. Harry R. Moody, director of academic affairs for AARP, notes that what is normal and what is disease strongly depend on a historical context.
David Gems, assistant director of the Institute of Healthy Ageing, argues that aging should be viewed as a disease. In response to the universality of aging, David Gems notes that it is as misleading as arguing that Basenji are not dogs because they do not bark.
Because of the universality of aging he calls it a "special sort of disease". Robert M. Perlman, coined the terms "aging syndrome" and "disease complex" in 1954 to describe aging.
The discussion whether aging should be viewed as a disease or not has important implications. One view is, this would stimulate pharmaceutical companies to develop life extension therapies and in the United States of America, it would also increase the regulation of the anti-aging market by the Food and Drug Administration (FDA).
Anti-aging now falls under the regulations for cosmetic medicine which are less tight than those for drugs.
Research:
Theoretically, extension of maximum lifespan in humans could be achieved by reducing the rate of aging damage by periodic replacement of damaged tissues, molecular repair or rejuvenation of deteriorated cells and tissues, reversal of harmful epigenetic changes, or the enhancement of enzyme telomerase activity.
Research geared towards life extension strategies in various organisms is currently under way at a number of academic and private institutions. Since 2009, investigators have found ways to increase the lifespan of nematode worms and yeast by 10-fold; the record in nematodes was achieved through genetic engineering and the extension in yeast by a combination of genetic engineering and caloric restriction.
A 2009 review of longevity research noted: "Extrapolation from worms to mammals is risky at best, and it cannot be assumed that interventions will result in comparable life extension factors. Longevity gains from dietary restriction, or from mutations studied previously, yield smaller benefits to Drosophila than to nematodes, and smaller still to mammals.
This is not unexpected, since mammals have evolved to live many times the worm's lifespan, and humans live nearly twice as long as the next longest-lived primate. From an evolutionary perspective, mammals and their ancestors have already undergone several hundred million years of natural selection favoring traits that could directly or indirectly favor increased longevity, and may thus have already settled on gene sequences that promote lifespan.
Moreover, the very notion of a "life-extension factor" that could apply across taxa presumes a linear response rarely seen in biology."
Anti-aging drugs:
There are a number of chemicals intended to slow the aging process currently being studied in animal models. One type of research is related to the observed effects of a calorie restriction (CR) diet, which has been shown to extend lifespan in some animals.
Based on that research, there have been attempts to develop drugs that will have the same effect on the aging process as a caloric restriction diet, which are known as caloric restriction mimetic drugs.
Some drugs that are already approved for other uses have been studied for possible longevity effects on laboratory animals because of a possible CR-mimic effect; they include rapamycin for mTOR inhibition and metformin for AMPK activation.
Sirtuin activating polyphenols, such as resveratrol and pterostilbene, and flavonoids, such as quercetin and fisetin, as well as oleic acid are dietary supplements that have also been studied in this context. Other popular supplements with less clear biological pathways to target aging include, lipoic acid, senolytics such as curcumin, and Coenzyme Q10.
Daily low doses of ethanol as a potential supplement in spite of its highly negative hormesis response at higher doses has also been studied.
Other attempts to create anti-aging drugs have taken different research paths. One notable direction of research explores the possibility of lengthening chromosomal telomeres (protective caps at the end of chromosomes) by reactivating telomerase, the enzyme responsible for telomere length maintenance.
However, telomerase is virtually unexpressed in normal, healthy somatic cells and there are potential dangers in this approach as research has shown a strong link between telomerase expression and cancer and tumors in somatic (non-germ line) cells.
Nanotechnology:
Future advances in nanomedicine could give rise to life extension through the repair of many processes thought to be responsible for aging. K. Eric Drexler, one of the founders of nanotechnology, postulated cell repair machines, including ones operating within cells and utilizing as yet hypothetical molecular computers, in his 1986 book Engines of Creation.
Raymond Kurzweil, a futurist and transhumanist, stated in his book The Singularity Is Near that he believes that advanced medical nanorobotics could completely remedy the effects of aging by 2030.
According to Richard Feynman, it was his former graduate student and collaborator Albert Hibbs who originally suggested to him (circa 1959) the idea of a medical use for Feynman's theoretical nanomachines (see biological machine). Hibbs suggested that certain repair machines might one day be reduced in size to the point that it would, in theory, be possible to (as Feynman put it) "swallow the doctor".
The idea was incorporated into Feynman's 1959 essay There's Plenty of Room at the Bottom.
Cloning and body part replacement:
Some life extensionists suggest that therapeutic cloning and stem cell research could one day provide a way to generate cells, body parts, or even entire bodies (generally referred to as reproductive cloning) that would be genetically identical to a prospective patient.
Recently, the US Department of Defense initiated a program to research the possibility of growing human body parts on mice. Complex biological structures, such as mammalian joints and limbs, have not yet been replicated.
Dog and primate brain transplantation experiments were conducted in the mid-20th century but failed due to rejection and the inability to restore nerve connections. As of 2006, the implantation of bio-engineered bladders grown from patients' own cells has proven to be a viable treatment for bladder disease.
Proponents of body part replacement and cloning contend that the required biotechnologies are likely to appear earlier than other life-extension technologies.
The use of human stem cells, particularly embryonic stem cells, is controversial. Opponents' objections generally are based on interpretations of religious teachings or ethical considerations. Proponents of stem cell research point out that cells are routinely formed and destroyed in a variety of contexts. Use of stem cells taken from the umbilical cord or parts of the adult body may not provoke controversy.
The controversies over cloning are similar, except general public opinion in most countries stands in opposition to reproductive cloning. Some proponents of therapeutic cloning predict the production of whole bodies, lacking consciousness, for eventual brain transplantation.
Cyborgs:
Main article: Cyborg
Replacement of biological (susceptible to diseases) organs with mechanical ones could extend life. This is the goal of the 2045 Initiative.
Cryonics:
Main article: Cryonics
Cryonics is the low-temperature freezing (usually at −196 °C or −320.8 °F or 77.1 K) of a human corpse, with the hope that resuscitation may be possible in the future. It is regarded with skepticism within the mainstream scientific community and has been characterized as quackery.
Strategies for engineered negligible senescence:
Main articles:
Another proposed life extension technology aims to combine existing and predicted future biochemical and genetic techniques. SENS proposes that rejuvenation may be obtained by removing aging damage via the use of:
While some biogerontologists find these ideas "worthy of discussion", others contend that the alleged benefits are too speculative given the current state of technology, referring to it as "fantasy rather than science".
Genetic editing:
Main articles: Genetics of aging and Genome editing
Genome editing, in which nucleic acid polymers are delivered as a drug and are either expressed as proteins, interfere with the expression of proteins, or correct genetic mutations, has been proposed as a future strategy to prevent aging.
A large array of genetic modifications have been found to increase lifespan in model organisms such as yeast, nematode worms, fruit flies, and mice. As of 2013, the longest extension of life caused by a single gene manipulation was roughly 50% in mice and 10-fold in nematode worms.
"Healthspan, parental lifespan, and longevity are highly genetically correlated."
In July 2020 scientists, using public biological data on 1.75 m people with known lifespans overall, identify 10 genomic loci which appear to intrinsically influence healthspan, lifespan, and longevity – of which half have not been reported previously at genome-wide significance and most being associated with cardiovascular disease – and identify haem metabolism as a promising candidate for further research within the field. Their study suggests that high levels of iron in the blood likely reduce, and genes involved in metabolising iron likely increase healthy years of life in humans.
The same month other scientists report that yeast cells of the same genetic material and within the same environment age in two distinct ways, describe a biomolecular mechanism that can determine which process dominates during aging and genetically engineer a novel aging route with substantially extended lifespan.
Fooling genes:
In The Selfish Gene, Richard Dawkins describes an approach to life-extension that involves "fooling genes" into thinking the body is young. Dawkins attributes inspiration for this idea to Peter Medawar. The basic idea is that our bodies are composed of genes that activate throughout our lifetimes, some when we are young and others when we are older.
Presumably, these genes are activated by environmental factors, and the changes caused by these genes activating can be lethal. It is a statistical certainty that we possess more lethal genes that activate in later life than in early life.
Therefore, to extend life, we should be able to prevent these genes from switching on, and we should be able to do so by "identifying changes in the internal chemical environment of a body that take place during aging... and by simulating the superficial chemical properties of a young body".
Mind uploading:
Main article: Mind uploading
One hypothetical future strategy that "eliminates" the complications related to a physical body, involves the copying or transferring (e.g. by progressively replacing neurons with transistors) of a conscious mind from a biological brain to a non-biological computer system or computational device.
The basic idea is to scan the structure of a particular brain in detail, and then construct a software model of it that is so faithful to the original that, when run on appropriate hardware, it will behave in essentially the same way as the original brain. Whether or not an exact copy of one's mind constitutes actual life extension is matter of debate.
However, critics argue that the uploaded mind would simply be a clone and not a true continuation of a person's consciousness.
Some scientists believe that the dead may one day be "resurrected" through simulation technology.
Young blood injection:
Further information: Young blood transfusion
Some clinics currently offer injection of blood products from young donors. The alleged benefits of the treatment, none of which have been demonstrated in a proper study, include:
The approach is based on parabiosis studies such as those Irina Conboy has done on mice, but Conboy says young blood does not reverse aging (even in mice) and that those who offer those treatments have misunderstood her research.
Neuroscientist Tony Wyss-Coray, who also studied blood exchanges on mice as recently as 2014, said people offering those treatments are "basically abusing people's trust" and that young blood treatments are "the scientific equivalent of fake news". The treatment appeared in HBO's Silicon Valley fiction series.
Two clinics in California, run by Jesse Karmazin and David C. Wright, offer $8,000 injections of plasma extracted from the blood of young people. However, Karmazin has not published in any peer-reviewed journal and his current study does not use a control group.
Microbiome alterations:
Fecal microbiota transplantation and probiotics are being investigated as means for life and healthspan extension.
See also:
Main articles: List of life extension topics and Index of life extension-related articles
Can You Lengthen Your Life? Researchers Explore How To Stay Healthy Longer
Want the secret to living a longer and healthier life? Scientists have found ways to prolong the healthy lifespans of worms, mice, and even monkeys. Their work has revealed exciting new clues about the biology of aging.
But solid evidence still shows that the best way to boost the chance of living a long and active life is to follow the advice you likely heard from your parents: eat well, exercise regularly, get plenty of sleep, and stay away from bad habits.
People born in the U.S. today can expect to live to an average age of about 79. A century ago, life expectancy was closer to 54. “We’ve had a significant increase in lifespan over the last century,” says Dr. Marie Bernard, deputy director of NIH’s National Institute on Aging. “Now if you make it to age 65, the likelihood that you’ll make it to 85 is very high. And if you make it to 85, the likelihood that you’ll make it to 92 is very high. So people are living longer, and it’s happening across the globe.”
Older people tend to be healthier nowadays, too. Research has shown that healthful behaviors can help you stay active and healthy into your 60s, 70s, and beyond. In fact, a long-term study of Seventh-day Adventists—a religious group with a generally healthy lifestyle—shows that they tend to remain healthier into old age. Their life expectancy is nearly 10 years longer on average than most Americans. The Adventists’ age-enhancing behaviors include regular exercise, a vegetarian diet, avoiding tobacco and alcohol, and maintaining a healthy weight.
“If I had to rank behaviors in terms of priority, I’d say that exercise is the most important thing associated with living longer and healthier,” says Dr. Luigi Ferrucci, an NIH geriatrician who oversees research on aging and health. “Exercise is especially important for lengthening active life expectancy, which is life without disease and without physical and mental/thinking disability.”
Natural changes to the body as we age can lead to a gradual loss of muscle, reduced energy, and achy joints. These changes may make it tempting to move less and sit more. But doing that can raise your risk for disease, disability, and even death. It’s important to work with a doctor to find the types of physical activity that can help you maintain your health and mobility.
Even frail older adults can benefit from regular physical activity. One NIH-funded study included over 600 adults, ages 70 to 89, who were at risk for disability. They were randomly placed in either a moderate exercise program or a comparison group without structured exercise. The exercise group gradually worked up to 150 minutes of weekly activity. This included brisk walking, strength and balance training, and flexibility exercises.
“After more than 2 years, the physical activity group had less disability, and if they became disabled, they were disabled for a shorter time than those in the comparison group,” Bernard explains. “The combination of different types of exercise—aerobic, strength and balance training, and flexibility—is important to healthy aging.” NIH’s Go4Life website has tips to help older adults get and stay active.
Another sure way to improve your chances for a longer, healthier life is to shed excess weight. “Being obese—with a body mass index (BMI) higher than 30—is a risk factor for early death, and it shortens your active life expectancy,” Ferrucci says. BMI is an estimate of your body fat based on your weight and height. Use NIH’s BMI calculator to determine your BMI. Talk with a doctor about reaching a healthy weight.
Studies in animals have found that certain types of dietary changes—such as extremely low-calorie diets—can lead to longer, healthier lives. These studies offer clues to the biological processes that affect healthy aging. But to date, calorie-restricted diets and other dietary changes have had mixed results in extending the healthy lives of people.
“We have indirect evidence that nutritional adjustments can improve active longevity in people, but this is still an area of intense research,” Ferrucci says. “So far, we don’t really have solid evidence about caloric restriction and whether it may have a positive effect on human aging.” Researchers are now studying potential drugs or other approaches that might mimic calorie restriction’s benefits.
Not smoking is another pathway to a longer, healthier life. “There’s no question that smoking is a hard habit to break. But data suggest that from the moment you stop smoking, there are health benefits. So it’s worthwhile making that effort,” Bernard says.
You might think you need good genes to live longer. But genes are only part of the equation for most of us, says Dr. Thomas Perls, an aging expert and director of the New England Centenarian Study at the Boston University School of Medicine. “Research shows that genes account for less than one-third of your chances of surviving to age 85. The vast majority of variation in how old we live to be is due to our health behaviors,” Perls says. “Our genes could get most of us close to the remarkable age of 90 if we lead a healthy lifestyle.”
The influence of genes is stronger, though, for people who live to older ages, such as beyond 95. Perls has been studying people who live to age 100 and up (centenarians) and their families to learn more about the biological, psychological, and social factors that promote healthy aging.
“It seems there’s not a single gene that imparts a strong effect on the ability to get to these older ages,” Perls says. “Instead, it’s the combined effects of probably hundreds of genes, each with weak effects individually, but having the right combination can lead to a very strong effect, especially for living to the oldest ages we study.”
It’s a good idea to be skeptical of claims for a quick fix to aging-related problems. Perls cautions against marketed “anti-aging” measures such as “hormone replacement therapy,” which has little proven benefit for healthy aging and can have severe side effects. “People used to say, ‘the older you get the sicker you get.’ But with common sense, healthy habits such as regular exercise, a healthy weight, avoiding red meat, not smoking, and managing stress, it can be ‘the older you get, the healthier you’ve been,” Perls says.
The key to healthy aging is to engage fully in life—mentally, physically, and socially. “Transitioning to older years isn’t about sitting in a rocking chair and letting the days slip by,” Bernard says. “Older adults have unique experiences, intellectual capital, and emotional involvement that can be shared with younger generations. This engagement is really key to helping our society move forward.”
___________________________________________________________________________
Old Age: Wikipedia
Old age is the range of ages nearing and surpassing the life expectancy of human beings; it is the end of the human life cycle. People of old age are also referred to as: old people, elderly, seniors, senior citizens, elders, or older adults.
Old age is not a definite biological stage: the chronological age denoted as "old age" varies culturally and historically. Some disciplines and domains focus on the aging and the aged, such as the organic processes of aging (senescence), medical studies of the aging process (gerontology), diseases that afflict older adults (geriatrics), technology to support the aging society (gerontechnology), and leisure and sport activities adapted to older people (such as senior sport).
Old people often have limited regenerative abilities and are more susceptible to illness and injury than younger adults. They face social problems related to retirement, loneliness, and ageism.
In 2011, the United Nations proposed a human-rights convention to protect old people.
Definitions:
Definitions of old age include official definitions, sub-group definitions, and four dimensions as follows.
Official definitions:
Most developed Western countries set the retirement age between 62 and 67; this is also generally considered to mark the transition from middle to old age. Having one's age within this range is commonly a requirement to become eligible for senior social programs. In non-Western nations, old age can begin as early as the mid-40s or as late as the 70s.
Old age cannot be universally defined because it is context-sensitive. The United Nations, for example, considers old age to be 60 years or older.
In contrast, a 2001 joint report by the U.S. National Institute on Aging and the World Health Organization [WHO] Regional Office for Africa set the beginning of old age in Sub-Saharan Africa at 50. This lower threshold stems primarily from a different way of thinking about old age in developing nations.
Unlike in the developed world, where chronological age determines retirement, societies in developing countries determine old age according to a person's ability to make active contributions to society. This number is also significantly affected by lower life expectancy rates throughout the developing world.
Sub-group definitions:
Gerontologists have recognized that people experience very different conditions as they approach old age. In developed countries, many people in their 60s and 70s are still fit, active, and able to care for themselves. However, after 80, they generally become increasingly frail, a condition marked by serious mental and physical debilitation.
Therefore, rather than lumping together all people who have been defined as old, some gerontologists have recognized the diversity of old age by defining sub-groups. One study distinguishes the young-old (60 to 69), the middle-old (70 to 79), and the very old (80+).
Another study's sub-grouping is young-old (65 to 74), middle-old (75 to 84), and oldest-old (85+). A third sub-grouping is young-old (65 to 74), old (74 to 84), and old-old (85+).
Describing sub-groups in the 65+ population enables a more accurate portrayal of significant life changes.
Two British scholars, Paul Higgs and Chris Gilleard, have added a "fourth age" sub-group. In British English, the "third age" is "the period in life of active retirement, following middle age". Higgs and Gilleard describe the fourth age as "an arena of inactive, unhealthy, unproductive, and ultimately unsuccessful ageing".
Dimensions:
Key Concepts in Social Gerontology lists four dimensions: chronological, biological, psychological, and social. Wattis and Curran add a fifth dimension: developmental. Chronological age may differ considerably from a person's functional age.
The distinguishing marks of old age normally occur in all five senses at different times and at different rates for different people. In addition to chronological age, people can be considered old because of the other dimensions of old age.
For example, people may be considered old when they become grandparents or when they begin to do less or different work in retirement.
Senior citizen:
Senior citizen is a common euphemism for an old person used in American English, and sometimes in British English. It implies that the person being referred to is retired.
This in turn usually implies that the person is over the retirement age, which varies according to country. Synonyms include old age pensioner or pensioner in British English, and retiree and senior in American English.
Some dictionaries describe widespread use of "senior citizen" for people over the age of 65.
When defined in a legal context, senior citizen is often used for legal or policy-related reasons in determining who is eligible for certain benefits available to the age group.
It is used in general usage instead of traditional terms such as "old person", "old-age pensioner", or "elderly" as a courtesy and to signify continuing relevance of and respect for this population group as "citizens" of society, of senior "rank".
The term was apparently coined in 1938 during a political campaign. Famed caricaturist Al Hirschfeld claimed on several occasions that his father Isaac Hirschfeld invented the term "senior citizen". It has come into widespread use in recent decades in legislation, commerce, and common speech. Especially in less formal contexts, it is often abbreviated as "senior(s)", which is also used as an adjective.
Age qualifications:
The age which qualifies for senior citizen status varies widely. In governmental contexts, it is usually associated with an age at which pensions or medical benefits for the elderly become available. In commercial contexts, where it may serve as a marketing device to attract customers, the age is often significantly lower.
In commerce, some businesses offer customers of a certain age a "senior discount". The age at which these discounts are available varies from 55, 60, 62 or 65 upwards, and other criteria may also apply. Sometimes a special "senior discount card" or other proof of age needs to be produced to show entitlement.
In the United States, the standard retirement age is currently 66 (gradually increasing to 67).
In Canada, the OAS (Old Age Security) pension is available at 65 (the Conservative government of Stephen Harper had planned to gradually increase the age of eligibility to 67, starting in the years 2023–2029, although the Liberal government of Justin Trudeau is considering leaving it at 65), and the CPP (Canada Pension Plan) as early as age 60.
The AARP allows couples in which one spouse has reached the age of 50 to join, regardless of the age of the other spouse.
Signs:
See also: Aging § Signs
The distinguishing characteristics of old age are both physical and mental. The marks of old age are so unlike the marks of middle age that legal scholar Richard Posner suggests that, as an individual transitions into old age, that person can be thought of as different people "time-sharing" the same identity.
These marks do not occur at the same chronological age for everyone. Also, they occur at different rates and order for different people. Marks of old age can easily vary between people of the same chronological age.
A basic mark of old age that affects both body and mind is "slowness of behavior". The term describes a correlation between advancing age and slowness of reaction and physical and mental task performance. However, studies from Buffalo University and Northwestern University have shown that the elderly are a happier age group than their younger counterparts.
Physical:
Physical marks of old age include the following:
- Bone and joint problems: Old bones are marked by "thinning and shrinkage". This might result in a loss of height (about two inches (5 cm) by age 80), a stooping posture in many people, and a greater susceptibility to bone and joint diseases such as osteoarthritis and osteoporosis.
- Chronic diseases: Some older people have at least one chronic condition and many have multiple conditions. In 2007–2009, the most frequently occurring conditions among older people in the United States were uncontrolled hypertension (34%), arthritis (50%), and heart disease (32%).
- Chronic mucus hypersecretion (CMH), defined as "coughing and bringing up sputum", is a common respiratory symptom in elderly people.
- Dental problems: Older people may have less saliva and reduced ability to maintain oral hygiene, consequently increasing the chance of tooth decay and infection.
- Digestive system issues: About 40% of the time, old age is marked by digestive disorders such as difficulty in swallowing, inability to eat enough and to absorb nutrition, constipation and bleeding.
- Essential tremor (ET): An uncontrollable shaking in a part of the upper body. It is more common in the elderly and symptoms worsen with age.
- Eyesight deterioration: Presbyopia can occur by age 50 and it hinders reading, especially of small print in low lighting. The speed with which an individual reads and the ability to locate objects may also be impaired. By age 80, more than half of all Americans either have a cataract or have had cataract surgery.
- Falls: Old age increases the risk of injury from falls. Every year, about a third of those 65 years old and more than half of those 80 years old fall. Falls are the leading cause of injury and death for old people.
- Gait change: Some aspects of gait normally change with old age. Speed slows after age 70. Time with both feet on the ground ("double stance") increases. Old people sometimes move as if they were walking carefully on ice.
- Hair usually turns gray and may become thinner. About age 50, about 50% of Europeans have 50% grey hair. Many men are affected by balding.
- Women enter menopause.
- Hearing loss: By age 75, 48% of men and 37% of women have lost at least some significant hearing. Of the 26.7 million people [where?] over age 50 with a hearing impairment, one seventh use hearing aids. In the 70–79 age range, partial hearing loss affecting communication rises to 65%, mostly in low-income men.
- Hearts can become less efficient in old age, lessening stamina. Atherosclerosis can constrict blood flow.
- Immune-function loss (Immunosenescence).
- Lungs may expand less efficiently, providing less oxygen.
- Mobility impairment or loss: "Impairment in mobility affects 14% of those between 65 and 74, [and] half of those over 85." Loss of mobility is common in old people and has serious "social, psychological, and physical consequences".
- Pain: 25% of seniors have chronic pain, increasing with age, up to 80% of those in nursing homes. Most pains are rheumatological or malignant.
- Decreases in sexual drive in both men and women. Increasing research on sexual behavior and desires in later life is challenging the "asexual" image of older adults. People aged 75–102 do experience sensuality and sexual pleasure. Sexual attitudes and identity are established in early adulthood and change little. Sexuality remains important throughout life, and the sexual expression of "typical, healthy older persons is a relatively neglected topic of research". Other known sexual behaviors in older age groups include sexual thoughts, fantasies, and dreams; masturbation; oral sex; and vaginal and anal intercourse.
- Skin loses elasticity and gets drier and more lined and wrinkled.
- Wounds take longer to heal and are likelier to leave permanent scars.
- Trouble sleeping and daytime sleepiness affect more than half of seniors. In a study of 9,000 people with a mean age of 74, only 12% reported no sleep complaints. By age 65, deep sleep drops to about 5% of sleep time.
- Taste buds diminish by up to half by the age of 80. Food becomes less appealing and nutrition can suffer.
- Over the age of 85, thirst perception decreases, so that 41% of the elderly don't drink enough.
- Urinary incontinence is often found in old age.
- Vocal cords weaken and vibrate more slowly. This results in a weakened, breathy voice, "old person's voice".
Mental:
Mental marks of old age include the following:
- Agreeability: Despite the stressfulness of old age, the words "agreeable" and "accepting" are used commonly to describe people of old age. However, in some people, the dependence that comes with old age induces feelings of incompetence and worthlessness from having to rely on others for many different basic living functions.
- Caution follows closely with old age. This antipathy toward "risk-taking" often stems from the fact that old people have less to gain and more to lose than younger people.
- Depressed mood. According to Cox, Abramson, Devine, and Hollon (2012), old age is a risk factor for depression caused by prejudice. When younger people are prejudiced against the elderly and then become old themselves, their anti-elderly prejudice turns inward, causing depression. "People with more negative age stereotypes will likely have higher rates of depression as they get older." Old age depression results in the over-65 population having the highest suicide rate.
- Fear of crime in old age, especially among the frail, sometimes weighs more heavily than concerns about finances or health and restricts what they do. The fear persists in spite of the fact that old people are victims of crime less often than younger people.
- Increasing fear of health problems.
- Mental disorders affect about 15% of people aged 60+ according to estimates by the World Health Organization. Another survey taken in 15 countries reported that mental disorders of adults interfered with their daily activities more than physical problems.
- Reduced mental and cognitive ability: Memory loss is common in old age due to the brain's decreased ability to encode, store, and retrieve information. It takes more time to learn the same amount of new information. The prevalence of dementia increases in old age from about 10% at age 65 to about 50% over age 85. Alzheimer's disease accounts for 50 to 80 percent of dementia cases. Demented behavior can include wandering, physical aggression, verbal outbursts, depression, and psychosis.
- Stubbornness: A study of over 400 seniors found a "preference for the routine". Explanations include old age's toll on "fluid intelligence" and the "more deeply entrenched" ways of the old.
Perspectives:
Middle age:
Many books written by authors in middle adulthood depict a few common perceptions on old age. One writer notices the change in his parents: They move slowly, they have less strength, they repeat stories, their minds wander, and they fret. Another writer sees her aged parents and is bewildered: They refuse to follow her advice, they are obsessed with the past, they avoid risk, and they live at a "glacial pace".
In her The Denial of Aging, Dr. Muriel R. Gillick, a baby boomer, accuses her contemporaries of believing that by proper exercise and diet they can avoid the scourges of old age and proceed from middle age to death.
Studies find that many people in the 55–75 range can postpone morbidity by practicing healthy lifestyles. However, at about age 80, most people experience similar morbidity. Even with healthy lifestyles, most 85+ people will undergo extended "frailty and disability".
Old age:
Early old age can be a pleasant time; children are grown, work is over, and there is time to pursue other interests. Many old people are also willing to get involved in community and activist organizations to promote their well-being. In contrast, perceptions of old age by writers 80+ years old tend to be negative.
Georges Minois [Wikidata] writes that the first man known to talk about his old age was an Egyptian scribe who lived 4,500 years ago. The scribe addressed God with a prayer of lament:
- "O Sovereign my Lord! Oldness has come; old age has descended. Feebleness has arrived; dotage is here anew. The heart sleeps wearily every day.
- The eyes are weak, the ears are deaf, the strength is disappearing because of weariness of the heart and the mouth is silent and cannot speak.
- The heart is forgetful and cannot recall yesterday. The bone suffers old age. Good is become evil. All taste is gone. What old age does to men is evil in every respect.
Minois comments that the scribe's "cry shows that nothing has changed in the drama of decrepitude between the age of the Pharaoh and the atomic age" and "expresses all the anguish of old people in the past and the present".
Lillian Rubin, active in her 80s as an author, sociologist, and psychotherapist, opens her book 60 on Up: The Truth about Aging in America with "getting old sucks. It always has, it always will." Dr. Rubin contrasts the "real old age" with the "rosy pictures" painted by middle-age writers.
Writing at the age of 87, Mary C. Morrison describes the "heroism" required by old age: to live through the disintegration of one's own body or that of someone you love. Morrison concludes, "old age is not for the fainthearted".
In the book Life Beyond 85 Years, the 150 interviewees had to cope with physical and mental debilitation and with losses of loved ones. One interviewee described living in old age as "pure hell".
Research has shown that in high-income countries, on average, one in four people over 60 and one in three over 75 feels lonely.
Misconceptions:
Johnson and Barer did a pioneering study of Life Beyond 85 Years by interviews over a six-year period. In talking with 85-year-olds and older, they found some popular conceptions about old age to be erroneous. Such erroneous conceptions include:
- people in old age have at least one family member for support,
- old age well-being requires social activity,
- "successful adaptation" to age-related changes demands a continuity of self-concept.
In their interviews, Johnson and Barer found that 24% of the 85+ had no face-to-face family relationships; many have outlived their families. Second, that contrary to popular notions, the interviews revealed that the reduced activity and socializing of the over-85s does not harm their well-being; they "welcome increased detachment".
Third, rather than a continuity of self-concept, as the interviewees faced new situations they changed their "cognitive and emotional processes" and reconstituted their "self–representation".
Societal and historical:
Based on his survey of old age in history, Georges Minois concludes that "it is clear that always and everywhere youth has been preferred to old age". In Western thought, "old age is an evil, an infirmity and a dreary time of preparation for death". Furthermore, death is often preferred over "decrepitude, because death means deliverance".
"The problem of the ambiguity of old age has . . . been with us since the stage of primitive society; it was both the source of wisdom and of infirmity, experience and decrepitude, of prestige and suffering."
In the Classical period of Greek and Roman cultures, old age was denigrated as a time of "decline and decrepitude". "Beauty and strength" were esteemed and old age was viewed as defiling and ugly. Old age was reckoned as one of the unanswerable "great mysteries" along with evil, pain, and suffering. "Decrepitude, which shrivels heroes, seemed worse than death."
Historical periods reveal a mixed picture of the "position and status" of old people, but there has never been a "golden age of aging". Studies have challenged the popular belief that in the past old people were venerated by society and cared for by their families.
Veneration for and antagonism toward the aged have coexisted in complex relationships throughout history. "Old people were respected or despised, honoured or put to death according to circumstance."
In ancient times, although some strong and healthy people lived until they were over 70, most died before they were 50. The general understanding is that those who lived into their 40s were treated with respect and awe. In contrast, those who were frail were seen as a burden and ignored or, in extreme cases, killed.
People were defined as "old" because of their inability to perform useful tasks rather than their years.
Although he was skeptical of the gods, Aristotle concurred in the dislike of old people. In his Ethics, he wrote that "old people are miserly; they do not acknowledge disinterested friendship; only seeking for what can satisfy their selfish needs".
The Medieval and Renaissance periods depicted old age as "cruel or weak".
The 16th-century Utopians Thomas More and Antonio de Guevara allowed no decrepit old people in their fictional lands.
For Thomas More, on the island of Utopia, when people are so old as to have "out-lived themselves" and are terminally ill, in pain, and a burden to everyone, the priests exhort them about choosing to die. The priests assure them that "they shall be happy after death". If they choose to die, they end their lives by starvation or by taking opium.
Antonio de Guevara's utopian nation "had a custom, not to live longer than sixty five years". At that age, they practiced self-immolation. Rather than condemn the practice, Bishop Guevara called it a "golden world" in which people "have overcome the natural appetite to desire to live".
Contemporary Perspectives:
In the Modern period, the "cultural status" of old people has declined in many cultures. Joan Erikson observed that "aged individuals are often ostracized, neglected, and overlooked; elders are seen no longer as bearers of wisdom but as embodiments of shame".
Attitudes toward old age well being vary somewhat between cultures. For example, in the United States being healthy, physically, and socially active are signs of a good old age. On the other hand, Africans focus more on food and material security and a helpful family when describing old age well being. Additionally, Koreans are more anxious about aging, and more scared of old people than Americans are.
Research on age-related attitudes consistently finds that negative attitudes exceed positive attitudes toward old people because of their looks and behavior. In his study Aging and Old Age, Posner discovers "resentment and disdain of older people" in American society.
Harvard University's implicit-association test measures implicit "attitudes and beliefs" about "Young vis a vis Old".
Blind Spot: Hidden Biases of Good People, a book about the test, reports that 80% of Americans have an "automatic preference for the young over old" and that attitude is true worldwide. The young are "consistent in their negative attitude" toward the old.
Ageism documents that Americans generally have "little tolerance for older persons and very few reservations about harboring negative attitudes" about them.
Despite its prevalence, ageism is seldom the subject of public discourse.
Simulated:
Simone de Beauvoir wrote that "there is one form of experience that belongs only to those that are old – that of old age itself". Nevertheless, simulations of old age attempt to help younger people gain some understanding.
Texas A&M University offers a plan for an "Aging Simulation" workshop. The workshop is adapted from Sensitizing People to the Processes of Aging. Some of the simulations include:
- Sight: Wearing swimmer's goggles with black paper pasted to lens with only a small hole to simulate tunnel vision
- Hearing: Use ear plugs to dull the sound of people talking
- Touch: Trying to button a shirt or buckle a belt while wearing thick gloves
- Dexterity: Unscrew a jar lid with tape around several fingers
- Mobility and balance: Carry packages in one hand while using a walker
The Macklin Intergenerational Institute conducts Xtreme Aging workshops, as depicted in The New York Times. A condensed version was presented on NBC's Today Show and is available online.
One exercise was to lay out 3 sets of 5 slips of paper. On set #1, write your 5 most enjoyed activities; on set #2, write your 5 most valued possessions; on set #3, write your 5 most loved people. Then "lose" them one by one, trying to feel each loss, until you have lost them all, as happens in old age.
Frailty:
Most people in the age range of 60–80 (the years of retirement and early old age), enjoy rich possibilities for a full life, but the condition of frailty distinguished by "bodily failure" and greater dependence becomes increasingly common after that. In the United States, hospital discharge data from 2003 to 2011 shows that injury was the most common reason for hospitalization among patients aged 65+.
Gerontologists note the lack of research regarding and the difficulty in defining frailty. However, they add that physicians recognize frailty when they see it.
A group of geriatricians proposed a general definition of frailty as "a physical state of increased vulnerability to stressors that results from decreased reserves and dis-regulation in multiple physiological systems".
Frailty is a common condition in later old age but different definitions of frailty produce diverse assessments of prevalence.
One study placed the incidence of frailty for ages 65+ at 10.7%. Another study placed the incidence of frailty in age 65+ population at 22% for women and 15% for men. A Canadian study illustrated how frailty increases with age and calculated the prevalence for 65+ as 22.4% and for 85+ as 43.7%.
A worldwide study of "patterns of frailty" based on data from 20 nations found (a) a consistent correlation between frailty and age, (b) a higher frequency among women, and (c) more frailty in wealthier nations where greater support and medical care increases longevity.
In Norway, a 20-year longitudinal study of 400 people found that bodily failure and greater dependence became prevalent in the 80+ years. The study calls these years the "fourth age" or "old age in the real meaning of the term".
Similarly, the "Berlin Aging Study" rated over-all functionality on four levels: good, medium, poor, and very poor. People in their 70s were mostly rated good. In the 80–90 year range, the four levels of functionality were divided equally.
By the 90–100 year range, 60% would be considered frail because of very poor functionality and only 5% still possessed good functionality.
Markers:
Three unique markers of frailty have been proposed: (a) loss of any notion of invincibility, (b) loss of ability to do things essential to one's care, and (c) loss of possibility for a subsequent life stage.
Old age survivors on-average deteriorate from agility in their 65–80s to a period of frailty preceding death. This deterioration is gradual for some and precipitous for others. Frailty is marked by an array of chronic physical and mental problems which means that frailty is not treatable as a specific disease.
These problems coupled with increased dependency in the basic activities of daily living (ADLs) required for personal care add emotional problems: depression and anxiety. In sum, frailty has been depicted as a group of "complex issues", distinct but "causally interconnected", that often include "comorbid diseases", progressive weakness, stress, exhaustion, and depression.
Care and costs:
Frail people require a high level of care. Medical advances have made it possible to "postpone death" for years. This added time costs many frail people "prolonged sickness, dependence, pain, and suffering".
According to a study by the Agency for Healthcare Research and Quality (AHRQ), the rate of emergency department visits was consistently highest among patients ages 85 years and older in 2006–2011 in the United States.
Additionally, patients aged 65+ had the highest percentage of hospital stays for adults with multiple chronic conditions but the second highest percentage of hospital costs in 2003–2014.
These final years are also costly in economic terms. One out of every four Medicare dollars is spent on the frail in their last year of life . . . in attempts to postpone death.
Medical treatments in the final days are not only economically costly, they are often unnecessary, even harmful. Nortin Hadler, M.D. warns against the tendency to medicalize and overtreat the frail.
In his Choosing Medical Care in Old Age, Michael R. Gillick M.D. argues that appropriate medical treatment for the frail is not the same as for the robust. The frail are vulnerable to "being tipped over" by any physical stress put on the system such as medical interventions.
In addition to everyday care, frail elderly people and others with disabilities are particularly vulnerable during natural disasters. They may be unable or unwilling to evacuate to avoid a hurricane or wildfire.
Death:
Old age, death, and frailty are linked because approximately half the deaths in old age are preceded by months or years of frailty.
Older Adults' Views on Death is based on interviews with 109 people in the 70–90 age range, with a mean age of 80.7. Almost 20% of the people wanted to use whatever treatment that might postpone death. About the same number said that, given a terminal illness, they would choose assisted suicide.
Roughly half chose doing nothing except live day by day until death comes naturally without medical or other intervention designed to prolong life. This choice was coupled with a desire to receive palliative care if needed.
About half of older adults have multimorbidity, that is, they have three or more chronic conditions. Medical advances have made it possible to "postpone death", but in many cases this postponement adds "prolonged sickness, dependence, pain, and suffering", a time that is costly in social, psychological, and economic terms.
The longitudinal interviews of 150 age 85+ people summarized in Life Beyond 85 Years found "progressive terminal decline" in the year prior to death: constant fatigue, much sleep, detachment from people, things, and activities, simplified lives.
Most of the interviewees did not fear death; some would welcome it. One person said, "Living this long is pure hell." However, nearly everyone feared a long process of dying. Some wanted to die in their sleep; others wanted to die "on their feet".
The study of Older Adults' Views on Death found that the more frail people were, the more "pain, suffering, and struggles" they were enduring, the more likely they were to "accept and welcome" death as a release from their misery.
Their fear about the process of dying was that it would prolong their distress. Besides being a release from misery, some saw death as a way to reunion with departed loved ones. Others saw death as a way to free their caretakers from the burden of their care.
Religiosity:
Generally speaking, old people have always been more religious than young people. At the same time, wide cultural variations exist.
In the United States, 90% of old age Hispanics view themselves as very, quite, or somewhat religious. The Pew Research Center's study of black and white old people found that 62% of those in ages 65–74 and 70% in ages 75+ asserted that religion was "very important" to them.
For all 65+ people, more women (76%) than men (53%) and more blacks (87%) than whites (63%) consider religion "very important" to them. This compares to 54% in the 30–49 age range.
In a British 20-year longitudinal study, less than half of the old people surveyed said that religion was "very important" to them, and a quarter said they had become less religious in old age.
The late-life rise in religiosity is stronger in Japan than in the United States, but in the Netherlands it is minimal.
In the practice of religion, a study of 60+ people found that 25% read the Bible every day and over 40% look at religious TV. Pew Research found that in the age 65+ range, 75% of whites and 87% of blacks pray daily.
When comparing religiosity, the individual practice may be a more accurate measure than participation in organized religion. With organized religion, participation may often be hindered due to transportation or health problems.
Demographic changes:
In the industrialized countries, life expectancy and, thus, the old age population have increased consistently over the last decades.
In the United States the proportion of people aged 65 or older increased from 4% in 1900 to about 12% in 2000.
In 1900, only about 3 million of the nation's citizens were 65 or older (out of 76 million total American citizens).
By 2000, the number of senior citizens had increased to about 35 million (of 280 million US citizens). Population experts estimate that more than 50 million Americans—about 17 percent of the population—will be 65 or older in 2020. By 2050, it is projected that at least 400,000 Americans will be 100 or older.
The number of old people is growing around the world chiefly because of the post–World War II baby boom and increases in the provision and standards of health care. By 2050, 33% of the developed world's population and almost 20% of the less developed world's population will be over 60 years old.
The growing number of people living to their 80s and 90s in the developed world has strained public welfare systems and has also resulted in increased incidence of diseases like cancer and dementia that were rarely seen in premodern times.
When the United States Social Security program was created, people older than 65 numbered only around 5% of the population and the average life expectancy of a 65-year-old in 1936 was approximately 5 years, while in 2011 it could often range from 10 to 20 years.
Other issues that can arise from an increasing population are growing demands for health care and an increase in demand for different types of services.
Of the roughly 150,000 people who die each day across the globe, about two thirds—100,000 per day—die of age-related causes. In industrialized nations, the proportion is much higher, reaching 90%.
Psychosocial aspects:
According to Erik Erikson's "Stages of Psychosocial Development", the human personality is developed in a series of eight stages that take place from the time of birth and continue on throughout an individual's complete life. He characterises old age as a period of "Integrity vs. Despair", during which a person focuses on reflecting back on his life.
Those who are unsuccessful during this phase will feel that their life has been wasted and will experience many regrets. The individual will be left with feelings of bitterness and despair. Those who feel proud of their accomplishments will feel a sense of integrity.
Successfully completing this phase means looking back with few regrets and a general feeling of satisfaction. These individuals will attain wisdom, even when confronting death. Coping is a very important skill needed in the aging process to move forward with life and not be 'stuck' in the past. The way a person adapts and copes, reflects his aging process on a psycho-social level.
For people in their 80s and 90s, Joan Erikson added a ninth stage in The Life Cycle Completed: Extended Version. As she wrote, she added the ninth stage because the Integrity of the eighth stage imposes "a serious demand on the senses of elders" and the Wisdom of the eighth stage requires capacities that ninth stage elders "do not usually have".
Newman & Newman also proposed a ninth stage of life, Elderhood. Elderhood refers to those individuals who live past the life expectancy of their birth cohorts. They described two different types of people in this stage of life. The "young old" are the healthy individuals who can function on their own without assistance and can complete their daily tasks independently, while the "old old" are those who depend on specific services due to declining health or diseases.
Theories:
Social theories, or concepts, propose explanations for the distinctive relationships between old people and their societies.
One theory, proposed in 1961, is the disengagement theory, which proposes that, in old age, a mutual disengagement between people and their society occurs in anticipation of death. By becoming disengaged from work and family responsibilities, according to this concept, people are enabled to enjoy their old age without stress.
This theory has been subjected to the criticism that old age disengagement is neither natural, inevitable, nor beneficial. Furthermore, disengaging from social ties in old age is not across the board: unsatisfactory ties are dropped and satisfying ones kept.
In opposition to the disengagement theory, the activity theory of old age argues that disengagement in old age occurs not by desire, but by the barriers to social engagement imposed by society.
This theory has been faulted for not factoring in psychological changes that occur in old age as shown by reduced activity, even when available. It has also been found that happiness in old age is not proportional to activity.
According to the continuity theory, in spite of the inevitable differences imposed by their old age, most people try to maintain continuity in personhood, activities, and relationships with their younger days.
Socioemotional selectivity theory also depicts how people maintain continuity in old age. The focus of this theory is continuity sustained by social networks, albeit networks narrowed by choice and by circumstances. The choice is for more harmonious relationships. The circumstances are loss of relationships by death and distance.
Life expectancy:
Life expectancy by nation at birth in the year 2011 ranged from 48 years to 82. Low values indicate high death rates for infants and children.
In most parts of the world women live, on average, longer than men; even so, the disparities vary between 12 years in Russia to no difference or higher life expectancy for men in countries such as Zimbabwe and Uganda.
The number of elderly people worldwide began to surge in the second half of the 20th century. In developed countries before then, five or less percent of the population was over 65. Few lived longer than their 70s and people who attained advanced age (i.e. their 80s) were rare enough to be a novelty and were revered as wise sages.
The worldwide over-65 population in 1960 was one-third of the under-5 population. By 2013, the over-65 population had grown to equal the under-5 population and is projected to double the under-5 population by 2050.
Before the surge in the over-65 population, accidents and disease claimed many people before they could attain old age, and health problems in those over 65 meant a quick death in most cases. If a person lived to an advanced age, it was due to genetic factors and/or a relatively easy lifestyle, since diseases of old age could not be treated before the 20th century.
In October 2016, a group of scientists identified the maximum human lifespan at an average age of 115, with an absolute upper limit of 125 years. However, the concept of a maximum lifespan of humans is still widely debated among the scientific community.
Benefits:
German chancellor Otto von Bismarck created the world's first comprehensive government social safety net in the 1880s, providing for old age pensions.
In the United States of America, and the United Kingdom, 65 (UK 60 for women) was traditionally the age of retirement with full old age benefits.
In 2003, the age at which a United States citizen became eligible for full Social Security benefits began to increase gradually, and will continue to do so until it reaches 67 in 2027.
Full retirement age for Social Security benefits for people retiring in 2012 is age 66. In the United Kingdom, the state pension age for men and women will rise to 66 in 2020 with further increases scheduled after that.
Originally, the purpose of old age pensions was to prevent elderly people from being reduced to beggary, which is still common in some underdeveloped countries, but growing life expectancies and older populations have brought into question the model under which pension systems were designed.
By 1990, the United States was spending 30 per cent of its budget on the elderly, compared with 2 per cent on education. The dominant perception of the American old age population changed from "needy" and "worthy" to "powerful" and "greedy", old people getting more than their share of the nation's resources.
However, in 2011, using a Supplemental Poverty Measure (SPM), the old age American poverty rate was measured as 15.9%.
Assistance: devices and personal
In the United States in 2008, 11 million people aged 65+ lived alone: 5 million or 22% of ages 65–74, 4 million or 34% of ages 75–84, and 2 million or 41% of ages 85+. The 2007 gender breakdown for all people 65+ was men 19% and women 39%.
Many new assistive devices made especially for the home have enabled more old people to care for their own activities of daily living (ADL).
Some examples of devices are:
- a medical alert and safety system,
- shower seat (making it so the person does not get tired in the shower and fall),
- a bed cane (offering support to those with unsteadiness getting in and out of bed)
- and an ADL cuff (used with eating utensils for people with paralysis or hand weakness).
A Swedish study found that at age 76, 46% of the subjects used assistive devices. When they reached age 86, 69% used them. The subjects were ambivalent regarding the use of the assistive devices: as "enablers" or as "disablers".
People who view assistive devices as enabling greater independence accept and use them, whereas those who see them as symbols of disability reject them.
However, organizations like Love for the Elderly aim to combat such age-related prejudice by educating the public about the importance of appreciating growing older, while also providing services of kindness to elders in senior homes.
Even with assistive devices as of 2006, 8.5 million Americans needed personal assistance because of impaired basic activities of daily living required for personal care or impaired instrumental activities of daily living (IADL) required for independent living.
Projections place this number at 21 million by 2030 when 40% of Americans over 70 will need assistance. There are many options for such long-term care to those who require it.
There is home care in which a family member, volunteer, or trained professional will aid the person in need and help with daily activities. Another option is community services which can provide the person with transportation, meal plans, or activities in senior centers.
A third option is assisted living where 24-hour round-the-clock supervision is given with aid in eating, bathing, dressing, etc. A final option is a nursing home which provides professional nursing care.
Culture:
In 2014, a documentary film called The Age of Love used humor and the poignant adventures of 30 seniors who attend a speed dating event for 70 to 90-year-olds and discover how the search for romance changes—or does not change—from childhood to old age.
Artistic depiction:
Scholarly literature has emerged, especially in Britain, showing historical trends in the visual depiction of old age.
See also:
- Ageing
- Ageism
- Aging in dogs
- Aging in place
- Centenarian
- Elder rights
- Elder village
- Geriatric care management
- Gerontology
- Gerascophobia
- International Day of Older Persons
- List of the verified oldest people
- Oldest people
- Pensioner
- Paternal age effect
- Respect for the Aged Day
- Silver Alert
- Supercentenarian
- Successful ageing
- Activist ageing
Life extension
Life extension is the concept of extending the human lifespan, either modestly through improvements in medicine or dramatically by increasing the maximum lifespan beyond its generally-settled limit of 125 years.
Several researchers in the area, along with "life extensionists", "immortalists" or "longevists" (those who wish to achieve longer lives themselves), postulate that future breakthroughs in:
- issue rejuvenation,
- stem cells,
- regenerative medicine,
- molecular repair,
- gene therapy,
- pharmaceuticals,
- and organ replacement (such as with artificial organs or xenotransplantations)
The above will eventually enable humans to have indefinite lifespans (agerasia) through complete rejuvenation to a healthy youthful condition. The ethical ramifications, if life extension becomes a possibility, are debated by bioethicists.
The sale of purported anti-aging products such as supplements and hormone replacement is a lucrative global industry. For example, the industry that promotes the use of hormones as a treatment for consumers to slow or reverse the aging process in the US market generated about $50 billion of revenue a year in 2009.
The use of such hormone products has not been proven to be effective or safe.
Average life expectancy and lifespan:
Main article: Senescence
During the process of aging, an organism accumulates damage to its macromolecules, cells, tissues, and organs.
Specifically, aging is characterized as and thought to be caused by:
- "genomic instability,
- telomere attrition,
- epigenetic alterations,
- loss of proteostasis,
- deregulated nutrient sensing,
- mitochondrial dysfunction,
- cellular senescence,
- stem cell exhaustion,
- and altered intercellular communication."
Oxidation damage to cellular contents caused by free radicals is believed to contribute to aging as well.
The longest documented human lifespan is 122 years 164 days, the case of Jeanne Calment who according to records was born in 1875 and died in 1997, whereas the maximum lifespan of a wildtype mouse, commonly used as a model in research on aging, is about three years.
Genetic differences between humans and mice that may account for these different aging rates include differences in efficiency of DNA repair, antioxidant defenses, energy metabolism, proteostasis maintenance, and recycling mechanisms such as autophagy.
The average life expectancy in a population is lowered by infant and child mortality, which are frequently linked to infectious diseases or nutrition problems.
Later in life, vulnerability to accidents and age-related chronic disease such as cancer or cardiovascular disease play an increasing role in mortality. Extension of life expectancy and lifespan can often be achieved by access to improved medical care, vaccinations, good diet, exercise, and avoidance of hazards such as smoking.
Maximum lifespan is determined by the rate of aging for a species inherent in its genes and by environmental factors. Widely recognized methods of extending maximum lifespan in model organisms such as nematodes, fruit flies, and mice include caloric restriction, gene manipulation, and administration of pharmaceuticals.
Another technique uses evolutionary pressures such as breeding from only older members or altering levels of extrinsic mortality. Some animals such as hydra, planarian flatworms, and certain sponges, corals, and jellyfish do not die of old age and exhibit potential immortality.
Strategies:
See also: Ageing § Prevention and delay, and Brain aging
Senolytics and prolongevity drugs:
See also: Geroprotector and MTOR inhibitors § Rapamycin and rapalogs
This section is an excerpt from Senolytic.
A senolytic (from the words senescence and -lytic, "destroying") is among a class of small molecules under basic research to determine if they can selectively induce death of senescent cells and improve health in humans. A goal of this research is to discover or develop agents to delay, prevent, alleviate, or reverse age-related diseases.
A related concept is "senostatic", which means to suppress senescence.Senolytics eliminate senescent cells whereas senomorphics – with candidates such as Apigenin, Everolimus and Rapamycin – modulate properties of senescent cells without eliminating them, suppressing phenotypes of senescence, including the SASP.
Senomorphic effects may be one major effect mechanism of a range of prolongevity drug candidates. Such candidates are, however, typically not studied for just one mechanism, but multiple.
There are biological databases of prolongevity drug candidates under research as well as of potential gene/protein targets. These are enhanced by the following:
- longitudinal cohort studies,
- electronic health records,
- computational (drug) screening methods,
- computational biomarker-discovery methods
- and computational biodata-interpretation/personalized medicine methods.
Recently, artificial intelligence has been used to discover new senolytics, resulting in the identification of structurally distinct senolytic compounds with more favorable medicinal chemistry properties than previous senolytic candidates.
Such strategies as well as testing with model organisms and xenografts may attempt to or help address difficulties of trials with humans which have relatively long lifespans (compared to other animals) as well as the (larger) need to protect human health from early-trial-stage interventions (in clinical trials).
Besides rapamycin and senolytics, the drug-repurposing candidates studied most extensively include:
- metformin,
- acarbose,
- spermidine (see below)
- and NAD+ enhancers.
Many prolongevity drugs are synthetic alternatives or potential complements to existing nutraceuticals, such as various sirtuin-activating compounds under investigation like SRT2104.
In some cases pharmaceutical administration is combined with that of neutraceuticals – such as in the case of glycine combined with NAC. Often studies are structured based on or thematize specific prolongevity targets, listing both nutraceuticals and pharmaceuticals (together or separately) such as FOXO3-activators.
Researchers are also exploring ways to mitigate side-effects from such substances (possibly most notably rapamycin and its derivatives) such as via protocols of intermittent administration and have called for research that helps determine optimal treatment schedules (including timing) in general.
Diets and supplements:
Vitamins and antioxidants:
See also: Inflammaging and DNA damage theory of aging
The free-radical theory of aging suggests that antioxidant supplements might extend human life. Reviews, however, have found that use of vitamin A (as β-carotene) and vitamin E supplements possibly can increase mortality. Other reviews have found no relationship between vitamin E and other vitamins with mortality.
Vitamin D supplementation of various dosages is investigated in trials and there also is research into GlyNAC (see above).
Complications:
Complications of antioxidant supplementation (especially continuous high dosages far above the RDA) include that reactive oxygen species (ROS), which are mitigated by antioxidants, "have been found to be physiologically vital for signal transduction, gene regulation, and redox regulation, among others, implying that their complete elimination would be harmful".
In particular, one way of multiple they can be detrimental is by inhibiting adaptation to exercise such as muscle hypertrophy (e.g. during dedicated periods of caloric surplus).
There is also research into stimulating/activating/fueling endogenous antioxidant generation, in particular e.g. of neutraceutical glycine and pharmaceutical NAC. Antioxidants can change the oxidation status of different e.g. tissues, targets or sites each with potentially different implications, especially for different concentrations.
A review suggests mitochondria have a hormetic response to ROS, whereby low oxidative damage can be beneficial.
Dietary restriction:
Main article: Diet and longevity
See also: Caloric restriction mimetic
As of 2021, there is no clinical evidence that any dietary practice contributes to human longevity.
Healthy diet:
Research suggests that increasing adherence to Mediterranean diet patterns is associated with a reduction in total and cause-specific mortality, extending health- and lifespan.
Research is identifying the key beneficial components of the Mediterranean diet. It shares various characteristics with the similarly beneficial Okinawa diet. Potential anti-aging mechanisms of various nutrients are not yet understood.
Shares of macronutrients and level of caloric intake may also be of significance, including in periods when no dietary restriction occurs – such as not having a fat-intake that is too low and not having a prolonged caloric surplus or caloric deficit that is too large.
Studies suggest dietary changes are a major cause of national relative rises in life-span.
Microbiome:
Mechanistically, research suggests that the gut microbiome, which varies per person and changes throughout lifespan, is also involved in the beneficial effects, due to which various diet supplementations with prebiotics, various diverse (multi-strain) probiotics and synbiotics, and fecal microbiota transplantation are being investigated for life extension, mainly for prolonging healthspan, with many important questions being unresolved.
Optimal diet:
See also: Sustainable consumption § Sustainable food consumption
Approaches to develop optimal diets for health- and lifespan (or "longevity diets") include:
- modifying or further particularizing the Mediterranean diet as the baseline via nutrition science. For instance, via:
- (additional) increase in plant-based (but protein-rich) foods alongside additional restriction of meat intake – meat reduction is (or can be) typically healthy,
- regular moderate consumption of green tea or (filtered) coffee while ensuring adequate calcium intake
- (additional) increase in omega-3-containing seafoods (see also: algal oil)
- adding various foods thought to be healthy (e.g. due to results about various mechanistic effects) to the regular dietary consumption patterns (see also: functional food)
- increasing the intake of high-spermidine foods – studies suggest spermidine could extend lifespan, with high amounts that are larger than common supplements being present in fungi (e.g. mushrooms) and green peas
- increasing resistant starch-intake – legumes, especially e.g. green peas contain large amounts of resistant starch, especially if pre-cooked as cooling the cooked peas in a refrigerator substantially increases the resistant starch content due to starch retrogradation. It is a prebiotic (see Microbiome) and may promote healthy aging.
- keeping alcohol consumption of any type at a minimum – conventional Mediterranean diets include alcohol consumption (i.e. of wine), which is under research due to data suggesting negative long-term brain impacts even at low/moderate consumption levels. Anthocyanins which are present in red wine and suggested along with other flavanols to be a candidate for further longevity research are also present in comparable concentrations in bilberry and elderberry
- fully replacing refined grains – some guidelines of Mediterranean diets do not clarify or include the principle of whole-grain consumption instead of refined grains. Whole-grain are a significant source of spermidine and are associated with longevity. They are a main characteristic pillar of Mediterranean diets according to multiple reviews.
- aiming for a sufficient level of food variety and diversity – which some guidelines of Mediterranean diets do not clarify or include. One review suggests that food variety and diversity could be a factor of diet quality, and another review indicates that sufficient food variety may at least in some specific cases "increase intake of important nutrients and positively affect the gut microbiome structure and function". The required level of food variety may or may not be low and vary per person and diet.
- completely eliminating processed foods from the diet – some guidelines of Mediterranean diets may not clarify this principle. Diets associated with longevity are characterized by minimally processed foods.
- adjusting the diet for personal characteristics such as age as effects of e.g. macronutrient intake can vary per age (see below)
- inferring an optimal diet indiscriminately for all levels and forms of physical activities and age and other person-characteristics by integrating the available meta-analyses and data from mostly observational studies.
- This has been done for a tool and visualizations that show populations' relative general life extension potentials of (shifting diets towards) different food groups, suggesting i.a. that a 20-years old male in Europe who switches to the "optimal diet" could gain a mean of ~13.7 years of life and a 60-years old female in the U.S. switching to the "optimal diet" could gain a mean of ~8.0 years of life. It found the largest gains would be made by eating more legumes, whole grains, and nuts, and less red meat and processed meat. The optimal diet contains no consumption of sugar-sweetened beverages (moving from "typical Western diet" of 500 g/day to 0 g/day). The study notes of uncertainty in "the effect of eggs, white meat, and oils, individual variation in protective and risk factors, uncertainties for future development of medical treatments; and changes in lifestyle".
Nutraceuticals:
See also: Anti-aging supplements
Beyond, research into senolytics and (synthetic) prolongevity-drugs, vitamins and antioxidants, prebiotics and probiotics, there are neutraceuticals – dietary supplements and bioactive plant compounds (phytochemicals) but not pharmaceuticals – that are being investigated in life sciences, nutrition science and gerontology for potential health- and lifespan extension in healthy humans.
Sometimes, their use is researched or recommended as a way to correct nutritional deficiencies from switching to otherwise healthy foods – in particular from replacing meat consumption with a higher intake of plant-based foods.
Especially, but not only, in such cases the supplementation of minerals and various specific micronutrients is investigated. Correcting magnesium deficiency for instance could prolong life. Many supplements are researched primarily for potential improvements in health and healthspan rather than for extending lifespan.
Some studies hypothesize that relative health and longevity benefits of various foods and diets can be largely or to a large part attributed to the nutraceuticals they contain.
Some studies suggest increasing the intake of specific foods (see above) based on such results, while some investigate supplementation, including of dosages that are impractical to achieve with whole foods.
Researched substances include various polyphenols such as pterostilbene or flavonoids, notably epicatechin. Some herbal-extracts like rhodiola rosea are also being investigated due to results of tests with model organisms. Some of these are AMPK activators and hence caloric restriction mimetics (some possibly exercise mimetics as well). AMPK activators include resveratrol and berberine.
Many such nutraceuticals are also potent antioxidants. Like prolongevity-drugs and bioactive compounds in general, they can have multiple potential effect mechanisms, the polyphenol resveratrol for instance also activates possibly pro-longevity sirtuin activity.
A common issue with many already-existing natural nutraceuticals like resveratrol is their low bioavailability. Their side-effects are often low compared to several major longevity drug candidates. On the other hand, they are considered to often have "intrinsic natural bio-compatibility and safety". Some of the compounds can have a "biphasic dose response" (a trait/effect of hormesis) whereby they (can) have beneficial effects at low or moderate doses and toxic effects at high doses.
Other approaches:
Further advanced biosciences-based approaches include:
- Genetic and epigenetic alterations: Human genetic enhancement for pro-longevity and protective genes – see genetics of aging
- Cellular reprogramming': in vivo reprogramming to complement or augment human regenerative capacity and rejuvenate or replace cells
- Epigenetic reprogramming: early-stage research about rejuvenating/repairing epigenetic machinery
- Stem-cell interventions: "Increasing the number and quality of stem cells and activate regenerative signals"
- Nanomedicine: early-stage research of in vivo pro-longevity nanotechnology
- Tissue engineering: of tissues and organs (see also: xenotransplantation and artificial organ)
- Endogenous circulating biomolecules: Blood proteins of blood from young animals have shown some pro-longevity potential in animal studies (e.g. via transfer of blood or plasma, and of plasma proteins). Moreover, exerkines – signalling biomolecules released during/after exercise – have also shown promising results. Exerkines include myokines. Extracellular vesicles were shown to be secreted concomitantly with exerkines and are also investigated. (See also: body fluid and cerebrospinal fluid)
- Personalized interventions: future studies may tailor and investigate personalized medicine-type interventions For instance, effects of interventions or e.g. dosages may vary per age and/or genome. A review suggests that the field of precision medicine and geroscience will have to interact closely (see also: combination therapy)
- Peptides: such as MOTS-c released by mitochondria
- Mitochondria modulation: early-stage research indicates mitochondrial interventions such as mitochondrial transplantation may have potential to be efficacious (See also: mitochondrial theory of ageing)
Within the field:
See also: Biogerontology
There is a need and research into the development of aging biomarkers such as the epigenetic clock "to assess the ageing process and the efficacy of interventions to bypass the need for large-scale longitudinal studies".
Such biomarkers may also include in vivo brain imaging.
Reviews sometimes include structured tables that provide systematic overviews of intervention/drug candidates with a review calling for integrating "current knowledge with multi-omics, health records, and drug safety data to predict drugs that can improve health in late life" and listing major outstanding questions.
Biological databases of prolongevity drug candidates under research as well as of potential gene/protein targets include GenAge, DrugAge and Geroprotectors.
A review has pointed out that the approach of "'epidemiological' comparison of how a low versus a high consumption of an isolated macronutrient and its association with health and mortality may not only fail to identify protective or detrimental nutrition patterns but may lead to misleading interpretations".
It proposes a multi-pillar approach, and summarizes findings towards constructing – multi-system-considering and at least age-personalized dynamic – refined longevity diets.
Epidemiological-type observational studies included in meta-analyses should according to the study at least be complemented by "(1) basic research focused on lifespan and healthspan, (2) carefully controlled clinical trials, and (3) studies of individuals and populations with record longevity"
Hormone treatment:
The anti-aging industry offers several hormone therapies. Some of these have been criticized for possible dangers and a lack of proven effect. For example, the American Medical Association has been critical of some anti-aging hormone therapies.
While growth hormone (GH) decreases with age, the evidence for use of growth hormone as an anti-aging therapy is mixed and based mostly on animal studies. There are mixed reports that GH or IGF-1 modulates the aging process in humans and about whether the direction of its effect is positive or negative.
Klotho and exerkines (see above) like irisin are being investigated for potential pro-longevity therapies.
Lifestyle factors:
See also: Lifestyle disease
The following are investigated as potential (modulatable) factors of life extension:
- Loneliness/isolation,
- social life and support,
- exercise/physical activity (partly via neurobiological effects and increased NAD+ levels),
- psychological characteristics/personality (possibly highly indirectly),
- sleep duration,
- circadian rhythms (patterns of sleep, drug-administration and feeding),
- type of leisure activities,
- not smoking,
- altruistic emotions and behaviors,
- subjective well-being,
- mood
- and stress (including via heat shock protein)
Healthy lifestyle practices and healthy diet have been suggested as "first-line function-preserving strategies, with pharmacological agents, including existing and new pharmaceuticals and novel 'nutraceutical' compounds, serving as potential complementary approaches".
Societal strategies
See also:
- § Ethics and politics,
- § Scientific research,
- Clinical trial,
- Metascience,
- Telehealth,
- Health economics,
- Health education,
- and Medical research
Collectively, addressing common causes of death could extend lifespans of populations and humanity overall. For instance, a 2020 study indicates that the global mean loss of life expectancy (LLE) from air pollution in 2015 was 2.9 years, substantially more than, for example, 0.3 years from all forms of direct violence, albeit a significant fraction of the LLE (a measure similar to years of potential life lost) is considered to be unavoidable.
Regular screening and doctor visits has been suggested as a lifestyle-societal intervention. (See also: medical test and biomarker)
Health policy and changes to standard healthcare could support the adoption of the field's conclusions – a review suggests that the longevity diet would be a "valuable complement to standard healthcare and that, taken as a preventative measure, it could aid in avoiding morbidity, sustaining health into advanced age" as a form of preventive healthcare.
It has been suggested that in terms of healthy diets, Mediterranean-style diets could be promoted by countries for ensuring healthy-by-default choices ("to ensure the healthiest choice is the easiest choice") and with highly effective measures including dietary education, food checklists and recipes that are "simple, palatable, and affordable".
A review suggests that "targeting the aging process per se may be a far more effective approach to prevent or delay aging-associated pathologies than treatments specifically targeted to particular clinical conditions".
Low ambient temperature:
Low ambient temperature as a physical factor affecting free radical levels was identified as a treatment producing exceptional lifespan increase in Drosophila melanogaster and other living beings.
History:
Further information: Timeline of senescence research
The extension of life has been a desire of humanity and a mainstay motif in the history of scientific pursuits and ideas throughout history, from the Sumerian Epic of Gilgamesh and the Egyptian Smith medical papyrus, all the way through:
- the Taoists,
- Ayurveda practitioners,
- alchemists,
- hygienists such as Luigi Cornaro, Johann Cohausen and Christoph Wilhelm Hufeland,
- and philosophers such as Francis Bacon, René Descartes, Benjamin Franklin and Nicolas Condorcet.
However, the beginning of the modern period in this endeavor can be traced to the end of the 19th – beginning of the 20th century, to the so-called "fin-de-siècle" (end of the century) period, denoted as an "end of an epoch" and characterized by the rise of scientific optimism and therapeutic activism, entailing the pursuit of life extension (or life-extensionism).
Among the foremost researchers of life extension at this period were the Nobel Prize winning biologist Elie Metchnikoff (1845-1916) -- the author of the cell theory of immunity and vice director of Institut Pasteur in Paris, and Charles-Édouard Brown-Séquard (1817-1894) -- the president of the French Biological Society and one of the founders of modern endocrinology.
Sociologist James Hughes claims that science has been tied to a cultural narrative of conquering death since the Age of Enlightenment. He cites Francis Bacon (1561–1626) as an advocate of using science and reason to extend human life, noting Bacon's novel New Atlantis, wherein scientists worked toward delaying aging and prolonging life.
Robert Boyle (1627–1691), founding member of the Royal Society, also hoped that science would make substantial progress with life extension, according to Hughes, and proposed such experiments as "to replace the blood of the old with the blood of the young".
Biologist Alexis Carrel (1873–1944) was inspired by a belief in indefinite human lifespan that he developed after experimenting with cells, says Hughes.
Regulatory and legal struggles between the Food and Drug Administration (FDA) and the Life Extension organization included seizure of merchandise and court action. In 1991, Saul Kent and Bill Faloon, the principals of the organization, were jailed for four hours and were released on $850,000 bond each. After 11 years of legal battles, Kent and Faloon convinced the US Attorney's Office to dismiss all criminal indictments brought against them by the FDA.
In 2003, Doubleday published "The Immortal Cell: One Scientist's Quest to Solve the Mystery of Human Aging," by Michael D. West. West emphasised the potential role of embryonic stem cells in life extension.
Other modern life extensionists include:
- writer Gennady Stolyarov, who insists that death is "the enemy of us all, to be fought with medicine, science, and technology";
- transhumanist philosopher Zoltan Istvan, who proposes that the "transhumanist must safeguard one's own existence above all else";
- futurist George Dvorsky, who considers aging to be a problem that desperately needs to be solved;
- and recording artist Steve Aoki, who has been called "one of the most prolific campaigners for life extension".
Scientific research:
See also: Timeline of senescence research
In 1991, the American Academy of Anti-Aging Medicine (A4M) was formed. The American Board of Medical Specialties recognizes neither anti-aging medicine nor the A4M's professional standing.
In 2003, Aubrey de Grey and David Gobel formed the Methuselah Foundation, which gives financial grants to anti-aging research projects. In 2009, de Grey and several others founded the SENS Research Foundation, a California-based scientific research organization which conducts research into aging and funds other anti-aging research projects at various universities.
In 2013, Google announced Calico, a new company based in San Francisco that will harness new technologies to increase scientific understanding of the biology of aging. It is led by Arthur D. Levinson, and its research team includes scientists such as Hal V. Barron, David Botstein, and Cynthia Kenyon.
In 2014, biologist Craig Venter founded Human Longevity Inc., a company dedicated to scientific research to end aging through genomics and cell therapy. They received funding with the goal of compiling a comprehensive human genotype, microbiome, and phenotype database.
Aside from private initiatives, aging research is being conducted in university laboratories, and includes universities such as Harvard and UCLA. University researchers have made a number of breakthroughs in extending the lives of mice and insects by reversing certain aspects of aging.
Ethics and politics:
Scientific controversy:
Some critics dispute the portrayal of aging as a disease. For example, Leonard Hayflick, who determined that fibroblasts are limited to around 50 cell divisions, reasons that aging is an unavoidable consequence of entropy. Hayflick and fellow biogerontologists Jay Olshansky and Bruce Carnes have strongly criticized the anti-aging industry in response to what they see as unscrupulous profiteering from the sale of unproven anti-aging supplements.
Consumer motivations:
Research by Sobh and Martin (2011) suggests that people buy anti-aging products to obtain a hoped-for self (e.g., keeping a youthful skin) or to avoid a feared-self (e.g., looking old). The research shows that when consumers pursue a hoped-for self, it is expectations of success that most strongly drive their motivation to use the product.
The research also shows why doing badly when trying to avoid a feared self is more motivating than doing well. When product use is seen to fail it is more motivating than success when consumers seek to avoid a feared-self.
Political parties:
Though many scientists state that life extension and radical life extension are possible, there are still no international or national programs focused on radical life extension. There are political forces staying for and against life extension.
By 2012, in Russia, the United States, Israel, and the Netherlands, the Longevity political parties started. They aimed to provide political support to radical life extension research and technologies, and ensure the fastest possible and at the same time soft transition of society to the next step – life without aging and with radical life extension, and to provide access to such technologies to most currently living people.
Silicon Valley:
Some tech innovators and Silicon Valley entrepreneurs have invested heavily into anti-aging research. These include:
- Jeff Bezos (founder of Amazon),
- Larry Ellison (founder of Oracle),
- Peter Thiel (former PayPal CEO),
- Larry Page (co-founder of Google),
- Peter Diamandis,
- Sam Altman (CEO of OpenAI, invested in Retro Biosciences),
- and Brian Armstrong (founder of Coinbase and NewLimit).
Commentators:
Leon Kass (chairman of the US President's Council on Bioethics from 2001 to 2005) has questioned whether potential exacerbation of overpopulation problems would make life extension unethical. He states his opposition to life extension with the words:
"simply to covet a prolonged life span for ourselves is both a sign and a cause of our failure to open ourselves to procreation and to any higher purpose ... [The] desire to prolong youthfulness is not only a childish desire to eat one's life and keep it; it is also an expression of a childish and narcissistic wish incompatible with devotion to posterity."
John Harris, former editor-in-chief of the Journal of Medical Ethics, argues that as long as life is worth living, according to the person himself, we have a powerful moral imperative to save the life and thus to develop and offer life extension therapies to those who want them.
Transhumanist philosopher Nick Bostrom has argued that any technological advances in life extension must be equitably distributed and not restricted to a privileged few. In an extended metaphor entitled "The Fable of the Dragon-Tyrant", Bostrom envisions death as a monstrous dragon who demands human sacrifices. In the fable, after a lengthy debate between those who believe the dragon is a fact of life and those who believe the dragon can and should be destroyed, the dragon is finally killed. Bostrom argues that political inaction allowed many preventable human deaths to occur.
Overpopulation concerns:
Controversy about life extension is due to fear of overpopulation and possible effects on society. Biogerontologist Aubrey De Grey counters the overpopulation critique by pointing out that the therapy could postpone or eliminate menopause, allowing women to space out their pregnancies over more years and thus decreasing the yearly population growth rate.
Moreover, the philosopher and futurist Max More argues that, given the fact the worldwide population growth rate is slowing down and is projected to eventually stabilize and begin falling, superlongevity would be unlikely to contribute to overpopulation.
Opinion polls:
A Spring 2013 Pew Research poll in the United States found that 38% of Americans would want life extension treatments, and 56% would reject it. However, it also found that 68% believed most people would want it and that only 4% consider an "ideal lifespan" to be more than 120 years.
The median "ideal lifespan" was 91 years of age and the majority of the public (63%) viewed medical advances aimed at prolonging life as generally good. 41% of Americans believed that radical life extension (RLE) would be good for society, while 51% said they believed it would be bad for society.
One possibility for why 56% of Americans claim they would reject life extension treatments may be due to the cultural perception that living longer would result in a longer period of decrepitude, and that the elderly in our current society are unhealthy.
Religious people are no more likely to oppose life extension than the unaffiliated though some variation exists between religious denominations.
Aging as a disease:
Mainstream medical organizations and practitioners do not consider aging to be a disease. Biologist David Sinclair says: "I don't see aging as a disease, but as a collection of quite predictable diseases caused by the deterioration of the body."
The two main arguments used are that aging is both inevitable and universal while diseases are not. However, not everyone agrees. Harry R. Moody, director of academic affairs for AARP, notes that what is normal and what is disease strongly depend on a historical context.
David Gems, assistant director of the Institute of Healthy Ageing, argues that aging should be viewed as a disease. In response to the universality of aging, David Gems notes that it is as misleading as arguing that Basenji are not dogs because they do not bark.
Because of the universality of aging he calls it a "special sort of disease". Robert M. Perlman, coined the terms "aging syndrome" and "disease complex" in 1954 to describe aging.
The discussion whether aging should be viewed as a disease or not has important implications. One view is, this would stimulate pharmaceutical companies to develop life extension therapies and in the United States of America, it would also increase the regulation of the anti-aging market by the Food and Drug Administration (FDA).
Anti-aging now falls under the regulations for cosmetic medicine which are less tight than those for drugs.
Research:
Theoretically, extension of maximum lifespan in humans could be achieved by reducing the rate of aging damage by periodic replacement of damaged tissues, molecular repair or rejuvenation of deteriorated cells and tissues, reversal of harmful epigenetic changes, or the enhancement of enzyme telomerase activity.
Research geared towards life extension strategies in various organisms is currently under way at a number of academic and private institutions. Since 2009, investigators have found ways to increase the lifespan of nematode worms and yeast by 10-fold; the record in nematodes was achieved through genetic engineering and the extension in yeast by a combination of genetic engineering and caloric restriction.
A 2009 review of longevity research noted: "Extrapolation from worms to mammals is risky at best, and it cannot be assumed that interventions will result in comparable life extension factors. Longevity gains from dietary restriction, or from mutations studied previously, yield smaller benefits to Drosophila than to nematodes, and smaller still to mammals.
This is not unexpected, since mammals have evolved to live many times the worm's lifespan, and humans live nearly twice as long as the next longest-lived primate. From an evolutionary perspective, mammals and their ancestors have already undergone several hundred million years of natural selection favoring traits that could directly or indirectly favor increased longevity, and may thus have already settled on gene sequences that promote lifespan.
Moreover, the very notion of a "life-extension factor" that could apply across taxa presumes a linear response rarely seen in biology."
Anti-aging drugs:
There are a number of chemicals intended to slow the aging process currently being studied in animal models. One type of research is related to the observed effects of a calorie restriction (CR) diet, which has been shown to extend lifespan in some animals.
Based on that research, there have been attempts to develop drugs that will have the same effect on the aging process as a caloric restriction diet, which are known as caloric restriction mimetic drugs.
Some drugs that are already approved for other uses have been studied for possible longevity effects on laboratory animals because of a possible CR-mimic effect; they include rapamycin for mTOR inhibition and metformin for AMPK activation.
Sirtuin activating polyphenols, such as resveratrol and pterostilbene, and flavonoids, such as quercetin and fisetin, as well as oleic acid are dietary supplements that have also been studied in this context. Other popular supplements with less clear biological pathways to target aging include, lipoic acid, senolytics such as curcumin, and Coenzyme Q10.
Daily low doses of ethanol as a potential supplement in spite of its highly negative hormesis response at higher doses has also been studied.
Other attempts to create anti-aging drugs have taken different research paths. One notable direction of research explores the possibility of lengthening chromosomal telomeres (protective caps at the end of chromosomes) by reactivating telomerase, the enzyme responsible for telomere length maintenance.
However, telomerase is virtually unexpressed in normal, healthy somatic cells and there are potential dangers in this approach as research has shown a strong link between telomerase expression and cancer and tumors in somatic (non-germ line) cells.
Nanotechnology:
Future advances in nanomedicine could give rise to life extension through the repair of many processes thought to be responsible for aging. K. Eric Drexler, one of the founders of nanotechnology, postulated cell repair machines, including ones operating within cells and utilizing as yet hypothetical molecular computers, in his 1986 book Engines of Creation.
Raymond Kurzweil, a futurist and transhumanist, stated in his book The Singularity Is Near that he believes that advanced medical nanorobotics could completely remedy the effects of aging by 2030.
According to Richard Feynman, it was his former graduate student and collaborator Albert Hibbs who originally suggested to him (circa 1959) the idea of a medical use for Feynman's theoretical nanomachines (see biological machine). Hibbs suggested that certain repair machines might one day be reduced in size to the point that it would, in theory, be possible to (as Feynman put it) "swallow the doctor".
The idea was incorporated into Feynman's 1959 essay There's Plenty of Room at the Bottom.
Cloning and body part replacement:
Some life extensionists suggest that therapeutic cloning and stem cell research could one day provide a way to generate cells, body parts, or even entire bodies (generally referred to as reproductive cloning) that would be genetically identical to a prospective patient.
Recently, the US Department of Defense initiated a program to research the possibility of growing human body parts on mice. Complex biological structures, such as mammalian joints and limbs, have not yet been replicated.
Dog and primate brain transplantation experiments were conducted in the mid-20th century but failed due to rejection and the inability to restore nerve connections. As of 2006, the implantation of bio-engineered bladders grown from patients' own cells has proven to be a viable treatment for bladder disease.
Proponents of body part replacement and cloning contend that the required biotechnologies are likely to appear earlier than other life-extension technologies.
The use of human stem cells, particularly embryonic stem cells, is controversial. Opponents' objections generally are based on interpretations of religious teachings or ethical considerations. Proponents of stem cell research point out that cells are routinely formed and destroyed in a variety of contexts. Use of stem cells taken from the umbilical cord or parts of the adult body may not provoke controversy.
The controversies over cloning are similar, except general public opinion in most countries stands in opposition to reproductive cloning. Some proponents of therapeutic cloning predict the production of whole bodies, lacking consciousness, for eventual brain transplantation.
Cyborgs:
Main article: Cyborg
Replacement of biological (susceptible to diseases) organs with mechanical ones could extend life. This is the goal of the 2045 Initiative.
Cryonics:
Main article: Cryonics
Cryonics is the low-temperature freezing (usually at −196 °C or −320.8 °F or 77.1 K) of a human corpse, with the hope that resuscitation may be possible in the future. It is regarded with skepticism within the mainstream scientific community and has been characterized as quackery.
Strategies for engineered negligible senescence:
Main articles:
Another proposed life extension technology aims to combine existing and predicted future biochemical and genetic techniques. SENS proposes that rejuvenation may be obtained by removing aging damage via the use of:
- stem cells and tissue engineering,
- telomere-lengthening machinery,
- allotopic expression of mitochondrial proteins,
- targeted ablation of cells,
- immunotherapeutic clearance,
- and novel lysosomal hydrolases.
While some biogerontologists find these ideas "worthy of discussion", others contend that the alleged benefits are too speculative given the current state of technology, referring to it as "fantasy rather than science".
Genetic editing:
Main articles: Genetics of aging and Genome editing
Genome editing, in which nucleic acid polymers are delivered as a drug and are either expressed as proteins, interfere with the expression of proteins, or correct genetic mutations, has been proposed as a future strategy to prevent aging.
A large array of genetic modifications have been found to increase lifespan in model organisms such as yeast, nematode worms, fruit flies, and mice. As of 2013, the longest extension of life caused by a single gene manipulation was roughly 50% in mice and 10-fold in nematode worms.
"Healthspan, parental lifespan, and longevity are highly genetically correlated."
In July 2020 scientists, using public biological data on 1.75 m people with known lifespans overall, identify 10 genomic loci which appear to intrinsically influence healthspan, lifespan, and longevity – of which half have not been reported previously at genome-wide significance and most being associated with cardiovascular disease – and identify haem metabolism as a promising candidate for further research within the field. Their study suggests that high levels of iron in the blood likely reduce, and genes involved in metabolising iron likely increase healthy years of life in humans.
The same month other scientists report that yeast cells of the same genetic material and within the same environment age in two distinct ways, describe a biomolecular mechanism that can determine which process dominates during aging and genetically engineer a novel aging route with substantially extended lifespan.
Fooling genes:
In The Selfish Gene, Richard Dawkins describes an approach to life-extension that involves "fooling genes" into thinking the body is young. Dawkins attributes inspiration for this idea to Peter Medawar. The basic idea is that our bodies are composed of genes that activate throughout our lifetimes, some when we are young and others when we are older.
Presumably, these genes are activated by environmental factors, and the changes caused by these genes activating can be lethal. It is a statistical certainty that we possess more lethal genes that activate in later life than in early life.
Therefore, to extend life, we should be able to prevent these genes from switching on, and we should be able to do so by "identifying changes in the internal chemical environment of a body that take place during aging... and by simulating the superficial chemical properties of a young body".
Mind uploading:
Main article: Mind uploading
One hypothetical future strategy that "eliminates" the complications related to a physical body, involves the copying or transferring (e.g. by progressively replacing neurons with transistors) of a conscious mind from a biological brain to a non-biological computer system or computational device.
The basic idea is to scan the structure of a particular brain in detail, and then construct a software model of it that is so faithful to the original that, when run on appropriate hardware, it will behave in essentially the same way as the original brain. Whether or not an exact copy of one's mind constitutes actual life extension is matter of debate.
However, critics argue that the uploaded mind would simply be a clone and not a true continuation of a person's consciousness.
Some scientists believe that the dead may one day be "resurrected" through simulation technology.
Young blood injection:
Further information: Young blood transfusion
Some clinics currently offer injection of blood products from young donors. The alleged benefits of the treatment, none of which have been demonstrated in a proper study, include:
- a longer life,
- darker hair,
- better memory,
- better sleep,
- curing heart diseases, diabetes and Alzheimer's disease.
The approach is based on parabiosis studies such as those Irina Conboy has done on mice, but Conboy says young blood does not reverse aging (even in mice) and that those who offer those treatments have misunderstood her research.
Neuroscientist Tony Wyss-Coray, who also studied blood exchanges on mice as recently as 2014, said people offering those treatments are "basically abusing people's trust" and that young blood treatments are "the scientific equivalent of fake news". The treatment appeared in HBO's Silicon Valley fiction series.
Two clinics in California, run by Jesse Karmazin and David C. Wright, offer $8,000 injections of plasma extracted from the blood of young people. However, Karmazin has not published in any peer-reviewed journal and his current study does not use a control group.
Microbiome alterations:
Fecal microbiota transplantation and probiotics are being investigated as means for life and healthspan extension.
See also:
Main articles: List of life extension topics and Index of life extension-related articles
- Advanced glycation end product
- Aging brain
- Aging movement control
- Alzheimer's disease
- Anti-aging movement
- Biological immortality
- Centenarian
- Clinical Interventions in Aging
- Dementia
- DNA damage theory of aging
- Human enhancement
- Immortal DNA strand hypothesis
- Immortality
- Maximum lifespan
- Particulates
- Rejuvenation Research
- Senescence
- Slow aging
- Supercentenarian
- Timeline of senescence research
- Transgenerational design
- Life extension on Wikiversity