Copyright © 2015 Bert N. Langford (Images may be subject to copyright. Please send feedback)
Welcome to Our Generation USA!
Below, we cover
Modern Medicine
including the Medical Profession as well as ailments and cures, whether physical or mental in cause and treatment.
See also: "Health & Fitness"
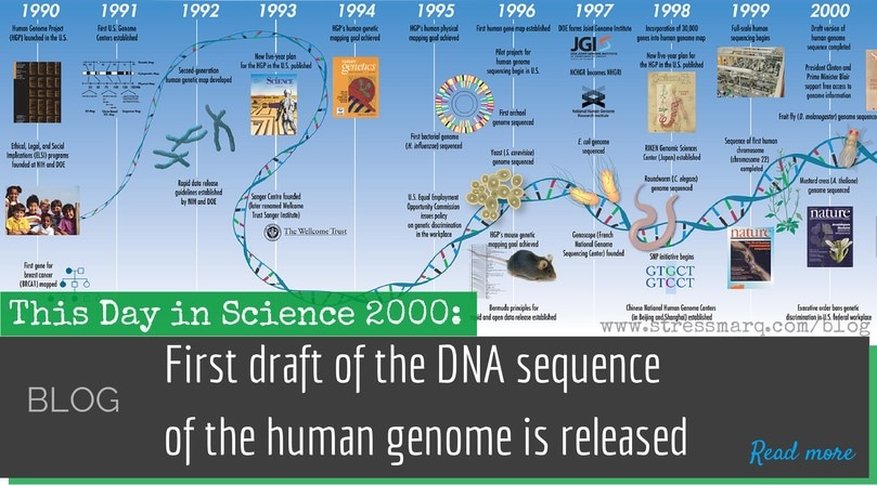
The Human Genome Project
YouTube Video: Cracking the Code Of Life | PBS Nova | 2001
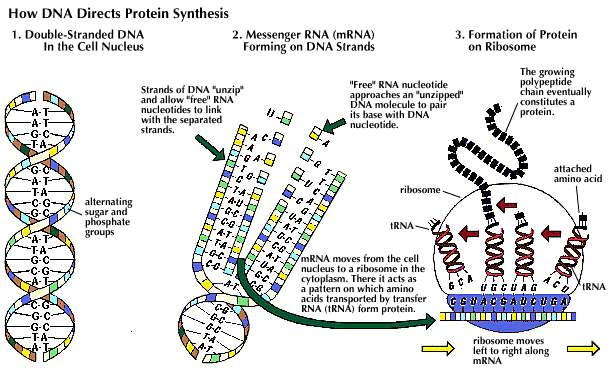
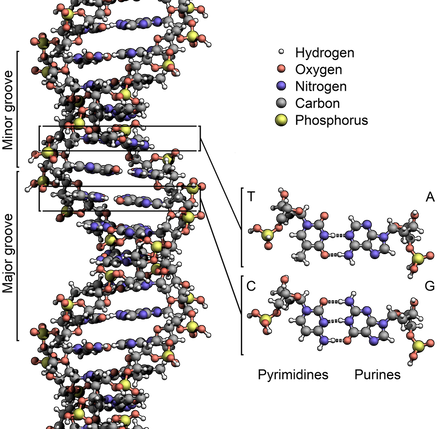
The Human Genome Project (HGP) is an international scientific research project with the goal of determining the sequence of chemical base pairs which make up human DNA, and of identifying and mapping all of the genes of the human genome from both a physical and functional standpoint.
It remains the world's largest collaborative biological project. After the idea was picked up in 1984 by the US government the planning started, with the project formally launched in 1990, and finally declared complete in 2003.
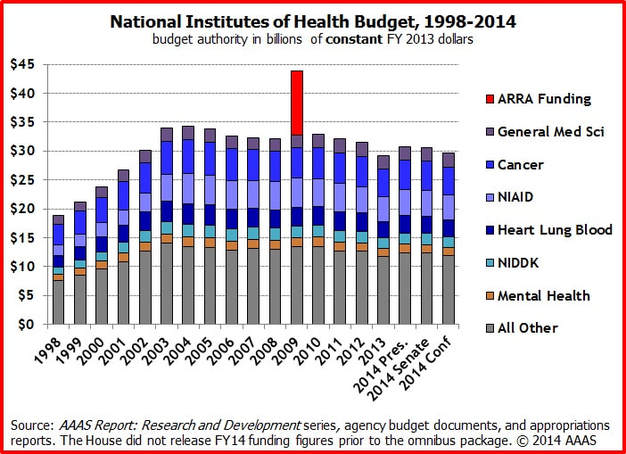
Funding came from the US government through the National Institutes of Health as well as numerous other groups from around the world. A parallel project was conducted outside of government by the Celera Corporation, or Celera Genomics, which was formally launched in 1998. Most of the government-sponsored sequencing was performed in twenty universities and research centers in the United States, the United Kingdom, Japan, France, Germany, and China.
The Human Genome Project originally aimed to map the nucleotides contained in a human haploid reference genome (more than three billion). The "genome" of any given individual is unique; mapping "the human genome" involves sequencing multiple variations of each gene.
It remains the world's largest collaborative biological project. After the idea was picked up in 1984 by the US government the planning started, with the project formally launched in 1990, and finally declared complete in 2003.
Funding came from the US government through the National Institutes of Health as well as numerous other groups from around the world. A parallel project was conducted outside of government by the Celera Corporation, or Celera Genomics, which was formally launched in 1998. Most of the government-sponsored sequencing was performed in twenty universities and research centers in the United States, the United Kingdom, Japan, France, Germany, and China.
The Human Genome Project originally aimed to map the nucleotides contained in a human haploid reference genome (more than three billion). The "genome" of any given individual is unique; mapping "the human genome" involves sequencing multiple variations of each gene.
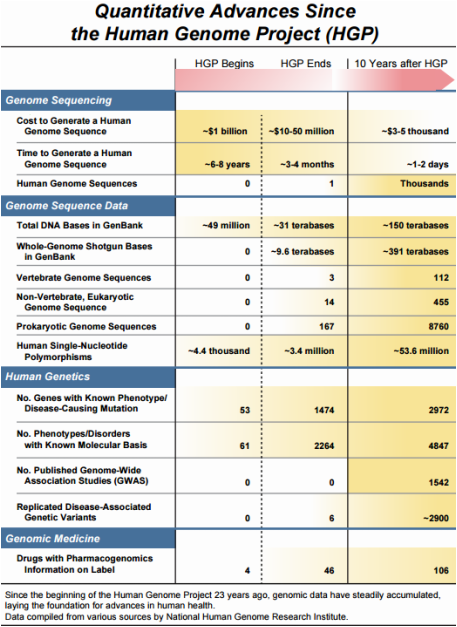
A Decade of Advancements Since the Human Genome Project
YouTube Video: Sequencing of the Human Genome to Treat Cancer - Mayo Clinic
A View by Susan Young Rojahn of MIT Technology Review.
April 12, 2013: "This Sunday, the National Institutes of Health will celebrate the 10th anniversary of the completion of the Human Genome Project.
Since the end of the 13-year and $3-billion effort to determine the sequence of a human genome (a mosaic of genomes from several people in this case), there have been some impressive advances in technology and biological understanding and the dawn of a new branch of medicine: medical genomics.
Today, sequencing a human genome can cost less than $5,000 and take only a day or two. This means genome analysis is now in the cost range of a sophisticated medical test, said Eric Green, director of the National Human Genome Research Institute, in a teleconference on Friday. Doctors can now using DNA analysis to diagnose challenging cases, such as mysterious neurodevelopmental disorders, mitochondrial disease, or other disease or unknown origin in children (see “Making Genome Sequencing Part of Clinical Care”). In such cases, genomic analysis can identify disease-causing mutations 19 percent to 33 percent of the time, according to a recent analysis.
Genomics is possibly making its biggest strides in cancer medicine. Doctors can now sequence a patient’s tumor to identify the best treatments. Specific drug targets may be found in as many as 70 percent of tumors (see “Foundation Medicine: Personalizing Cancer Drugs” and “Cancer Genomics”).
The dropping price of DNA sequencing is also changing prenatal care. A pregnant woman now has the option to eschew amniocenteses or other invasive methods for checking for chromosome aberrations in her fetus. Instead, she can get a simple blood draw (see “A Brave New World of Prenatal DNA Sequencing”).
Before the Human Genome Project, researchers knew the genetic basis of about 60 disorders. Today, they know the basis of nearly 5,000 conditions. Prescriptions are also changing because of genomics. More than 100 different FDA-approved drugs are now packaged with genomic information that tells doctors to test their patients for genetic variants linked to efficacy, dosages or risky side-effects.
But the work for human genome scientists is hardly over. There are still regions of the human genome yet to be sequenced. Most of these still unyielding regions are in parts of chromosomes that are full of complex, repetitive sequence, said Green. The much larger challenge will be to decipher what all the A’s, T’s, G’s and C’s in the human genome mean. Only a small proportion of the genome encodes for proteins and there is ongoing debate as to how much of the remainder is functional or just junk or redundant sequences.
And many scientists agree that the advances in medical genomics are just the tip of the iceberg— much more work lies ahead to fully harness genomic information to improve patient health.
You can see more of the numbers behind the advances in genome science since the Human Genome Project in this chart published by the NHGRI on Friday....: (See Chart above).
(For rest of article, click on title above).
Since the end of the 13-year and $3-billion effort to determine the sequence of a human genome (a mosaic of genomes from several people in this case), there have been some impressive advances in technology and biological understanding and the dawn of a new branch of medicine: medical genomics.
Today, sequencing a human genome can cost less than $5,000 and take only a day or two. This means genome analysis is now in the cost range of a sophisticated medical test, said Eric Green, director of the National Human Genome Research Institute, in a teleconference on Friday. Doctors can now using DNA analysis to diagnose challenging cases, such as mysterious neurodevelopmental disorders, mitochondrial disease, or other disease or unknown origin in children (see “Making Genome Sequencing Part of Clinical Care”). In such cases, genomic analysis can identify disease-causing mutations 19 percent to 33 percent of the time, according to a recent analysis.
Genomics is possibly making its biggest strides in cancer medicine. Doctors can now sequence a patient’s tumor to identify the best treatments. Specific drug targets may be found in as many as 70 percent of tumors (see “Foundation Medicine: Personalizing Cancer Drugs” and “Cancer Genomics”).
The dropping price of DNA sequencing is also changing prenatal care. A pregnant woman now has the option to eschew amniocenteses or other invasive methods for checking for chromosome aberrations in her fetus. Instead, she can get a simple blood draw (see “A Brave New World of Prenatal DNA Sequencing”).
Before the Human Genome Project, researchers knew the genetic basis of about 60 disorders. Today, they know the basis of nearly 5,000 conditions. Prescriptions are also changing because of genomics. More than 100 different FDA-approved drugs are now packaged with genomic information that tells doctors to test their patients for genetic variants linked to efficacy, dosages or risky side-effects.
But the work for human genome scientists is hardly over. There are still regions of the human genome yet to be sequenced. Most of these still unyielding regions are in parts of chromosomes that are full of complex, repetitive sequence, said Green. The much larger challenge will be to decipher what all the A’s, T’s, G’s and C’s in the human genome mean. Only a small proportion of the genome encodes for proteins and there is ongoing debate as to how much of the remainder is functional or just junk or redundant sequences.
And many scientists agree that the advances in medical genomics are just the tip of the iceberg— much more work lies ahead to fully harness genomic information to improve patient health.
You can see more of the numbers behind the advances in genome science since the Human Genome Project in this chart published by the NHGRI on Friday....: (See Chart above).
(For rest of article, click on title above).
10 Top Medical Breakthroughs
Exciting advances to health care are coming next year by Candy Sagon, AARP Bulletin, December 2015
YouTube Video: Top 10 Medical Breakthroughs according to WatchMojo
Pictured: A mind-controlled robotic limb may help those who suffer from paralysis in the future. — Zackary Canepari/ The New York Times/Redux
Game-changing new clot retriever for stroke victims. A way to restore movement by linking the brain to paralyzed limbs. New vaccines for our deadliest cancers. These will be the biggest medical advancements for 2016, according to three nationally known experts: Francis Collins, M.D., director of the National Institutes of Health; Michael Roizen, M.D., director of the Cleveland Clinic's Wellness Institute; and pathologist Michael Misialek, M.D., of Tufts University School of Medicine and Newton-Wellesley Hospital. Here are their top predictions.
1. Personalized treatment
What if you could get medical care tailored just for you, based on genetic information? The Precision Medicine Initiative, set to launch in 2016, would revolutionize how we treat disease, taking it from a one-size-fits-all approach to one fitted to each patient's unique differences. The project, Collins says, hopes to answer such important questions as: Why does a medical treatment work for some people with the same disease but not for others? One million volunteers will be asked to share their genomic and other molecular information with researchers working to understand factors that influence health.
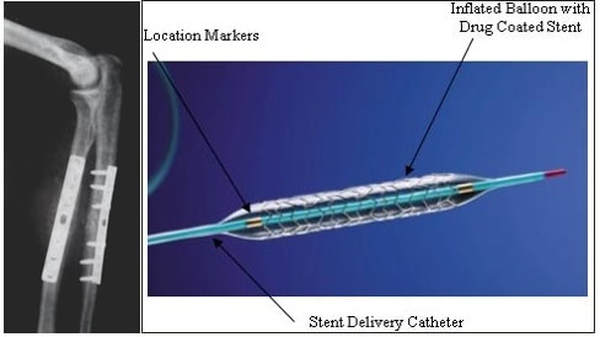
2. Busting brain clots
A tiny new tool to get rid of brain clots will be a "game changer for stroke treatment," Roizen says. Although clot-dissolving drugs are the first line of treatment for the most common type of stroke, when they don't do the trick, physicians can now use a stent retriever to remove the small mass. A wire with a mesh-like tip is guided through the artery into the brain to grab the clot. When the wire is removed, the clot goes with it. The American Heart Association has given the device its strongest recommendation, after studies found it improves the odds that certain patients will survive and function normally again.
3. Brain-limb connection
The goal of linking the brain to a robotic limb to help paralyzed people and amputees move naturally is closer than ever. Previously, brain implants to help move these artificial limbs have had limited success because the person had to think about each individual action (open hand, close hand) in order to move the limb. But now researchers are putting implants in the area of the brain that controls the intention to move, not just the physical movement itself. This allows patients to fluidly guide a robotic limb. "We think this will get FDA approval in the next year and will have a major clinical impact on paralyzed patients," Roizen says.
4. Fine-tuning genes
Next year could see major strides toward the goal of cutting harmful genetic mistakes from a person's DNA. A gene-editing tool is a powerful technology that allows scientists to easily correct or edit DNA. "It basically gives you a scissors to cut out pieces of genes," Roizen explains. The technology was recently used to eradicate leukemia in a British child by giving her gene-edited immune cells to fight off the disease. This could represent a huge step toward treating other diseases, including correcting gene mutations that cause inherited diseases, but ethicists and scientists worry the technology could also be used to alter traits for nonmedical reasons.
5. New cancer vaccines
Your body's immune system fights off germs that cause infections — could it be taught to fight off cancer cells? That's the idea behind new immunotherapy cancer vaccines, which train the immune system to use its antiviral fighting response to destroy cancer cells without harming healthy cells. The Food and Drug Administration (FDA) already has approved such vaccines for the treatment of advanced prostate cancer and melanoma. Current research is focused on pairing new and old vaccines, including the tetanus vaccine with a newer cancer vaccine to treat glioblastoma, a type of brain cancer. Those who received the dual vaccine lived three to seven more years after treatment than those who received an injection without the tetanus portion. Among the most eagerly anticipated vaccines in 2016, Misialek says, is a lung cancer vaccine. Work on such a vaccine, first developed in Cuba, is already underway here.
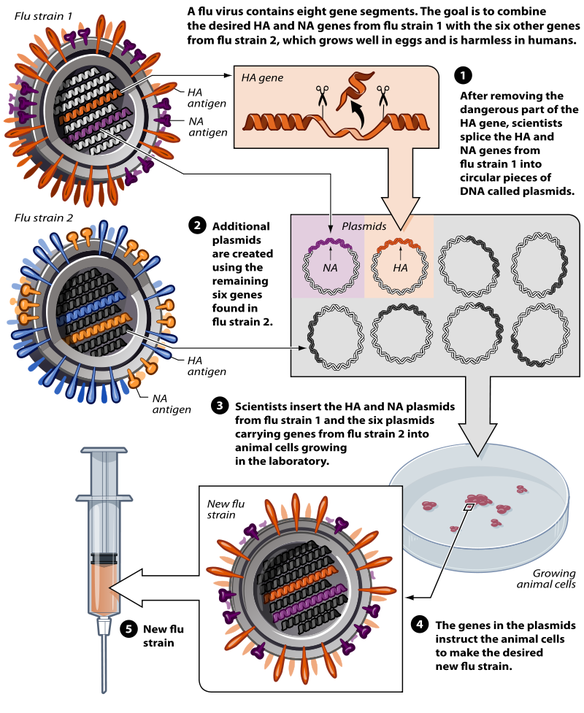
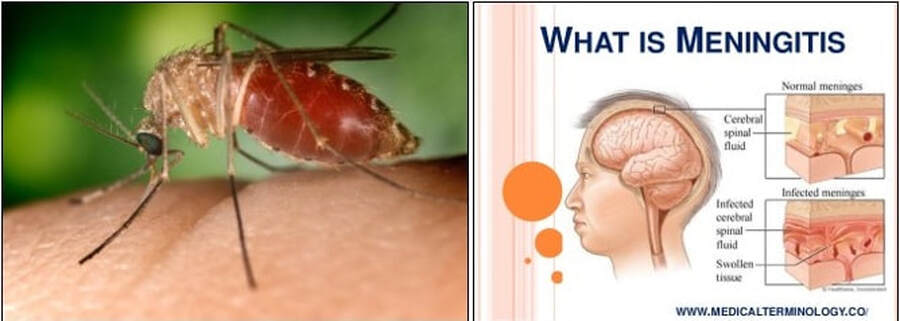
6. Faster public health vaccines
In the wake of the Ebola outbreak last year, the process for producing vaccines to protect the public against a possible epidemic has gone into warp drive — a feat that makes it the Cleveland Clinic's top medical innovation for 2016. The fear that, with international travel, a single person could potentially infect huge numbers of people "has led to a system to be able to immunize a large number of people really fast," Roizen explains. Where previously it took decades to develop a vaccine, the Ebola vaccine was ready in six months. A similarly accelerated process was behind the approval of a meningitis B vaccine following outbreaks at two universities.
7. Targeting cancer
Researchers are closing in on the day when a single drug will treat many different cancers. While traditional clinical trials focus on testing a drug for a particular type of cancer based on its location — breast or lung, for example — new studies are testing therapies that target a specific genetic mutation found in a tumor, regardless of where the cancer originated. "We're throwing all cancers with the same mutation in one basket," pathologist Misialek says, and then testing a drug that targets that mutation. Results of an international basket trial found that a drug focused on a single genetic mutation can be effective across multiple cancer types, including a common form of lung cancer and a rare form of bone cancer.
8. Wearable sensors
Wearable health sensors could soon change the way people with chronic diseases, such as diabetes, heart disease and asthma, control and monitor their condition. Drug companies and researchers are looking into using wearable technology to monitor patients more accurately in clinical trials, and hospitals and outpatient clinics could use it to monitor patients after discharge. Devices, from stick-on sensors to wristbands and special clothing, can already be used to monitor respiratory and heart rates, including EKG readings, as well as body temperature and glucose level. Stress levels and inflammation readings may be next, Roizen says.
9. Fighting superbugs
Decoding the DNA of bacteria is transforming the way we identify infectious diseases in the microbiology lab. That could help prevent the spread of dangerous, drug-resistant infections in hospitals and nursing homes, says Misialek. "Instead of identifying bugs in the traditional way and waiting days or weeks for the results, we can analyze genes and get exact identification sooner," he adds. That could help protect vulnerable patients against the spread of superbugs like MRSA, C. diff and streptococcus pneumoniae that currently resist treatment.
10. Better cancer screening
Some of the deadliest, most difficult-to-find cancers may be detected by analyzing blood for abnormal proteins. Cancer produces these abnormal protein structures. Up to now, blood tests weren't sensitive enough to identify them. A new type of analysis allows researchers to find the proteins earlier, which means cancer treatment can be started at an earlier stage. Cleveland Clinic experts predict this will lead to more effective tests for pancreatic cancer, considered the most deadly type with only about 7 percent surviving five years, as well as for prostate and ovarian cancer. A new test trial using protein analysis identified twice as many cases of ovarian cancer at an earlier stage than current tests.
At the bottom of the above link to the AARP article, you can click on a video about a Parkinson's Breakthrough: This health video will focus on the new breakthrough in the treatment of Parkinson's disease.
1. Personalized treatment
What if you could get medical care tailored just for you, based on genetic information? The Precision Medicine Initiative, set to launch in 2016, would revolutionize how we treat disease, taking it from a one-size-fits-all approach to one fitted to each patient's unique differences. The project, Collins says, hopes to answer such important questions as: Why does a medical treatment work for some people with the same disease but not for others? One million volunteers will be asked to share their genomic and other molecular information with researchers working to understand factors that influence health.
2. Busting brain clots
A tiny new tool to get rid of brain clots will be a "game changer for stroke treatment," Roizen says. Although clot-dissolving drugs are the first line of treatment for the most common type of stroke, when they don't do the trick, physicians can now use a stent retriever to remove the small mass. A wire with a mesh-like tip is guided through the artery into the brain to grab the clot. When the wire is removed, the clot goes with it. The American Heart Association has given the device its strongest recommendation, after studies found it improves the odds that certain patients will survive and function normally again.
3. Brain-limb connection
The goal of linking the brain to a robotic limb to help paralyzed people and amputees move naturally is closer than ever. Previously, brain implants to help move these artificial limbs have had limited success because the person had to think about each individual action (open hand, close hand) in order to move the limb. But now researchers are putting implants in the area of the brain that controls the intention to move, not just the physical movement itself. This allows patients to fluidly guide a robotic limb. "We think this will get FDA approval in the next year and will have a major clinical impact on paralyzed patients," Roizen says.
4. Fine-tuning genes
Next year could see major strides toward the goal of cutting harmful genetic mistakes from a person's DNA. A gene-editing tool is a powerful technology that allows scientists to easily correct or edit DNA. "It basically gives you a scissors to cut out pieces of genes," Roizen explains. The technology was recently used to eradicate leukemia in a British child by giving her gene-edited immune cells to fight off the disease. This could represent a huge step toward treating other diseases, including correcting gene mutations that cause inherited diseases, but ethicists and scientists worry the technology could also be used to alter traits for nonmedical reasons.
5. New cancer vaccines
Your body's immune system fights off germs that cause infections — could it be taught to fight off cancer cells? That's the idea behind new immunotherapy cancer vaccines, which train the immune system to use its antiviral fighting response to destroy cancer cells without harming healthy cells. The Food and Drug Administration (FDA) already has approved such vaccines for the treatment of advanced prostate cancer and melanoma. Current research is focused on pairing new and old vaccines, including the tetanus vaccine with a newer cancer vaccine to treat glioblastoma, a type of brain cancer. Those who received the dual vaccine lived three to seven more years after treatment than those who received an injection without the tetanus portion. Among the most eagerly anticipated vaccines in 2016, Misialek says, is a lung cancer vaccine. Work on such a vaccine, first developed in Cuba, is already underway here.
6. Faster public health vaccines
In the wake of the Ebola outbreak last year, the process for producing vaccines to protect the public against a possible epidemic has gone into warp drive — a feat that makes it the Cleveland Clinic's top medical innovation for 2016. The fear that, with international travel, a single person could potentially infect huge numbers of people "has led to a system to be able to immunize a large number of people really fast," Roizen explains. Where previously it took decades to develop a vaccine, the Ebola vaccine was ready in six months. A similarly accelerated process was behind the approval of a meningitis B vaccine following outbreaks at two universities.
7. Targeting cancer
Researchers are closing in on the day when a single drug will treat many different cancers. While traditional clinical trials focus on testing a drug for a particular type of cancer based on its location — breast or lung, for example — new studies are testing therapies that target a specific genetic mutation found in a tumor, regardless of where the cancer originated. "We're throwing all cancers with the same mutation in one basket," pathologist Misialek says, and then testing a drug that targets that mutation. Results of an international basket trial found that a drug focused on a single genetic mutation can be effective across multiple cancer types, including a common form of lung cancer and a rare form of bone cancer.
8. Wearable sensors
Wearable health sensors could soon change the way people with chronic diseases, such as diabetes, heart disease and asthma, control and monitor their condition. Drug companies and researchers are looking into using wearable technology to monitor patients more accurately in clinical trials, and hospitals and outpatient clinics could use it to monitor patients after discharge. Devices, from stick-on sensors to wristbands and special clothing, can already be used to monitor respiratory and heart rates, including EKG readings, as well as body temperature and glucose level. Stress levels and inflammation readings may be next, Roizen says.
9. Fighting superbugs
Decoding the DNA of bacteria is transforming the way we identify infectious diseases in the microbiology lab. That could help prevent the spread of dangerous, drug-resistant infections in hospitals and nursing homes, says Misialek. "Instead of identifying bugs in the traditional way and waiting days or weeks for the results, we can analyze genes and get exact identification sooner," he adds. That could help protect vulnerable patients against the spread of superbugs like MRSA, C. diff and streptococcus pneumoniae that currently resist treatment.
10. Better cancer screening
Some of the deadliest, most difficult-to-find cancers may be detected by analyzing blood for abnormal proteins. Cancer produces these abnormal protein structures. Up to now, blood tests weren't sensitive enough to identify them. A new type of analysis allows researchers to find the proteins earlier, which means cancer treatment can be started at an earlier stage. Cleveland Clinic experts predict this will lead to more effective tests for pancreatic cancer, considered the most deadly type with only about 7 percent surviving five years, as well as for prostate and ovarian cancer. A new test trial using protein analysis identified twice as many cases of ovarian cancer at an earlier stage than current tests.
At the bottom of the above link to the AARP article, you can click on a video about a Parkinson's Breakthrough: This health video will focus on the new breakthrough in the treatment of Parkinson's disease.
Immunology and Immunotherapy:
The list of cancers being taken down by immunotherapy keeps growing (as reported by the Washington Post on April 19, 2016)
YouTube Video: "Immunotherapy Fights Cancer"
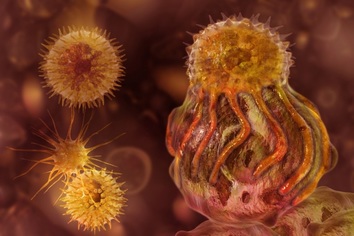
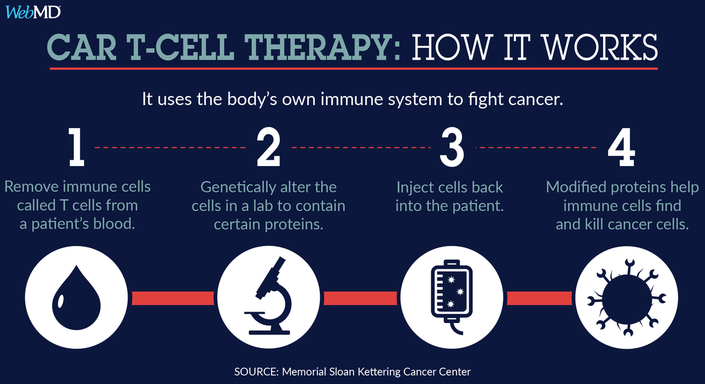
Pictured: From the Article: “In immunotherapy, T-cells from a cancer patient can be genetically engineered to be specific to a tumor. Dendritic cells (lower left) are special cells that help the immune system recognize the cancer cells and initiate a response. Drugs called "checkpoint inhibitors" also can spur the immune system. (Science Source)”
Washington Post Article By Laurie McGinley April 19 at 4:00 PM
"NEW ORLEANS — New immunotherapy drugs are showing significant and extended effectiveness against a broadening range of cancers, including rare and intractable tumors often caused by viruses. Researchers say these advances suggest the treatment approach is poised to become a critical part of the nation’s anti-cancer strategy.
Scientists reported Tuesday on two new studies showing that the medications, which marshal the body’s own immune defenses, are now proving effective against recurrent, difficult-to-treat head and neck cancer and an extremely lethal skin cancer called Merkel cell carcinoma. The diseases can be caused by viruses as well as DNA mutations, and the data show that the drugs help the immune system to recognize and attack cancers resulting from either cause.
The new studies appear to be the first to find that "virus-driven cancers can be amenable to treatment by immunotherapy," said Paul Nghiem, an investigator with the Fred Hutchinson Cancer Research Center in Seattle who led the Merkel cell study. Since viruses and other pathogens are responsible for more than 20 percent of all cancers, “these results have implications that go far beyond" Merkel cell carcinoma, which affects about 2,000 Americans a year, he said.
The new data, plus research released Sunday that showed sharply higher survival rates among advanced-melanoma patients who received immunotherapy, is prompting growing albeit guarded optimism among researchers attending the American Association for Cancer Research annual meeting here. In addition to melanoma, the infusion drugs already have been approved for use against lung and kidney cancers...."
(Click Here for Rest of Washington Post Article)
___________________________________________________________________________
Below, we cover the underlying Medical Sciences of Immunology and Immunotherapy:
Excerpted from Stanford University: "Immunology & Immunotherapy of Cancer Program":
The Program's two major goals are:
These goals will be achieved by fostering collaborative research, advancing the latest technologies to probe immunological mechanisms, and by enhancing the infrastructure for clinical translation.
Research by program members has resulted in exciting new developments in both understanding immune function and developing novel therapies. Advances include the development and application of CyTOF and high-throughput sequencing for evaluating cellular function and responses and the translation of important concepts to the clinic in promising early phase clinical trials.
___________________________________________________________________________
Immunology is a branch of biology that covers the study of immune systems in all organisms. The Russian biologist Ilya Ilyich Mechnikov advanced studies on immunology and received the Nobel Prize for his work in 1908. He pinned small thorns into starfish larvae and noticed unusual cells surrounding the thorns. This was the active response of the body trying to maintain its integrity. It was Mechnikov who first observed the phenomenon of phagocytosis, in which the body defends itself against a foreign body, and coined the term.
Immunology charts, measures, and contextualizes:
Immunology has applications in numerous disciplines of medicine, particularly in the fields of organ transplantation, oncology, virology, bacteriology, parasitology, psychiatry, and dermatology.
Prior to the designation of immunity from the etymological root immunis, which is Latin for "exempt"; early physicians characterized organs that would later be proven as essential components of the immune system.
The important lymphoid organs of the immune system are the thymus and bone marrow, and chief lymphatic tissues such as spleen, tonsils, lymph vessels, lymph nodes, adenoids, and liver.
When health conditions worsen to emergency status, portions of immune system organs including the thymus, spleen, bone marrow, lymph nodes and other lymphatic tissues can be surgically excised for examination while patients are still alive.
Many components of the immune system are typically cellular in nature and not associated with any specific organ; but rather are embedded or circulating in various tissues located throughout the body.
Click on any of the following blue hyperlinks for more about Immunology:
Immunotherapy is the "treatment of disease by inducing, enhancing, or suppressing an immune response".
Immunotherapies designed to elicit or amplify an immune response are classified as activation immunotherapies, while immunotherapies that reduce or suppress are classified as suppression immunotherapies. In recent years, immunotherapy has become of great interest to researchers, clinicians and pharmaceutical companies, particularly in its promise to treat various forms of cancer.
Immunomodulatory regimens often have fewer side effects than existing drugs, including less potential for creating resistance when treating microbial disease.
Cell-based immunotherapies are effective for some cancers. Immune effector cells such as lymphocytes, macrophages, dendritic cells, natural killer cells (NK Cell), cytotoxic T lymphocytes (CTL), etc., work together to defend the body against cancer by targeting abnormal antigens expressed on the surface of tumor cells.
Therapies such as granulocyte colony-stimulating factor (G-CSF), interferons, imiquimod and cellular membrane fractions from bacteria are licensed for medical use. Others including IL-2, IL-7, IL-12, various chemokines, synthetic cytosine phosphate-guanosine (CpG) oligodeoxynucleotides and glucans are involved in clinical and preclinical studies.
Click on any of the following blue hyperlinks for more about Immunotherapy:
"NEW ORLEANS — New immunotherapy drugs are showing significant and extended effectiveness against a broadening range of cancers, including rare and intractable tumors often caused by viruses. Researchers say these advances suggest the treatment approach is poised to become a critical part of the nation’s anti-cancer strategy.
Scientists reported Tuesday on two new studies showing that the medications, which marshal the body’s own immune defenses, are now proving effective against recurrent, difficult-to-treat head and neck cancer and an extremely lethal skin cancer called Merkel cell carcinoma. The diseases can be caused by viruses as well as DNA mutations, and the data show that the drugs help the immune system to recognize and attack cancers resulting from either cause.
The new studies appear to be the first to find that "virus-driven cancers can be amenable to treatment by immunotherapy," said Paul Nghiem, an investigator with the Fred Hutchinson Cancer Research Center in Seattle who led the Merkel cell study. Since viruses and other pathogens are responsible for more than 20 percent of all cancers, “these results have implications that go far beyond" Merkel cell carcinoma, which affects about 2,000 Americans a year, he said.
The new data, plus research released Sunday that showed sharply higher survival rates among advanced-melanoma patients who received immunotherapy, is prompting growing albeit guarded optimism among researchers attending the American Association for Cancer Research annual meeting here. In addition to melanoma, the infusion drugs already have been approved for use against lung and kidney cancers...."
(Click Here for Rest of Washington Post Article)
___________________________________________________________________________
Below, we cover the underlying Medical Sciences of Immunology and Immunotherapy:
Excerpted from Stanford University: "Immunology & Immunotherapy of Cancer Program":
The Program's two major goals are:
- To understand the nature of the immune system and its response to malignancies.
- To explore auto- and allo-immune responses to cancer with the goal of enabling the discovery and development of more effective anti-tumor immunotherapy.
These goals will be achieved by fostering collaborative research, advancing the latest technologies to probe immunological mechanisms, and by enhancing the infrastructure for clinical translation.
Research by program members has resulted in exciting new developments in both understanding immune function and developing novel therapies. Advances include the development and application of CyTOF and high-throughput sequencing for evaluating cellular function and responses and the translation of important concepts to the clinic in promising early phase clinical trials.
___________________________________________________________________________
Immunology is a branch of biology that covers the study of immune systems in all organisms. The Russian biologist Ilya Ilyich Mechnikov advanced studies on immunology and received the Nobel Prize for his work in 1908. He pinned small thorns into starfish larvae and noticed unusual cells surrounding the thorns. This was the active response of the body trying to maintain its integrity. It was Mechnikov who first observed the phenomenon of phagocytosis, in which the body defends itself against a foreign body, and coined the term.
Immunology charts, measures, and contextualizes:
- physiological functioning of the immune system in states of both health and diseases;
- malfunctions of the immune system in immunological disorders (such as autoimmune diseases, hypersensitivities, immune deficiency, and transplant rejection);
- and the physical, chemical and physiological characteristics of the components of the immune system in vitro, in situ, and in vivo.
Immunology has applications in numerous disciplines of medicine, particularly in the fields of organ transplantation, oncology, virology, bacteriology, parasitology, psychiatry, and dermatology.
Prior to the designation of immunity from the etymological root immunis, which is Latin for "exempt"; early physicians characterized organs that would later be proven as essential components of the immune system.
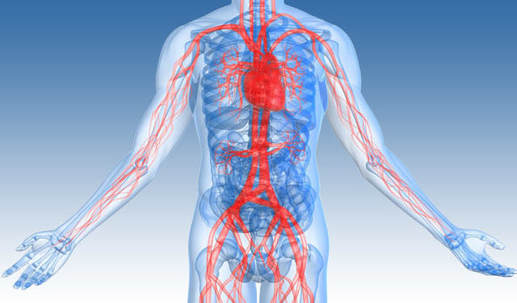
The important lymphoid organs of the immune system are the thymus and bone marrow, and chief lymphatic tissues such as spleen, tonsils, lymph vessels, lymph nodes, adenoids, and liver.
When health conditions worsen to emergency status, portions of immune system organs including the thymus, spleen, bone marrow, lymph nodes and other lymphatic tissues can be surgically excised for examination while patients are still alive.
Many components of the immune system are typically cellular in nature and not associated with any specific organ; but rather are embedded or circulating in various tissues located throughout the body.
Click on any of the following blue hyperlinks for more about Immunology:
- Classical immunology
- Clinical immunology
- Developmental immunology
- Ecoimmunology and behavioural immunity
- Immunotherapy: see next topic
- Diagnostic immunology
- Cancer immunology
- Reproductive immunology
- Theoretical immunology
- Immunologist
- Career in immunology
- See also:
- History of immunology
- Immunomics
- International Reviews of Immunology
- List of immunologists
- Osteoimmunology
- Outline of immunology
- American Association of Immunologists
- British Society for Immunology
- Annual Review of Immunology journal
- BMC: Immunology at BioMed Central, an open-access journal publishing original peer-reviewed research articles.
- Nature reviews: Immunology
- The Immunology Database and Analysis Portal, a NIAID-funded database resource.
- Federation of Clinical Immunology Societies
Immunotherapy is the "treatment of disease by inducing, enhancing, or suppressing an immune response".
Immunotherapies designed to elicit or amplify an immune response are classified as activation immunotherapies, while immunotherapies that reduce or suppress are classified as suppression immunotherapies. In recent years, immunotherapy has become of great interest to researchers, clinicians and pharmaceutical companies, particularly in its promise to treat various forms of cancer.
Immunomodulatory regimens often have fewer side effects than existing drugs, including less potential for creating resistance when treating microbial disease.
Cell-based immunotherapies are effective for some cancers. Immune effector cells such as lymphocytes, macrophages, dendritic cells, natural killer cells (NK Cell), cytotoxic T lymphocytes (CTL), etc., work together to defend the body against cancer by targeting abnormal antigens expressed on the surface of tumor cells.
Therapies such as granulocyte colony-stimulating factor (G-CSF), interferons, imiquimod and cellular membrane fractions from bacteria are licensed for medical use. Others including IL-2, IL-7, IL-12, various chemokines, synthetic cytosine phosphate-guanosine (CpG) oligodeoxynucleotides and glucans are involved in clinical and preclinical studies.
Click on any of the following blue hyperlinks for more about Immunotherapy:
- Immunomodulators
- Activation immunotherapies
- Suppression immunotherapies
- Helminthic therapies
- See also:
- Biological response modifiers
- Interleukin-2 immunotherapy
- Microtransplantation
- Langreth, Robert (12 February 2009). "Cancer Miracles". Forbes.
- International Society for Biological Therapy of Cancer
Medical Ultrasound Technology
YouTube Video Diagnostic Ultrasonography Procedure
Pictured: Portable Ultrasound Machine
Medical ultrasound (also known as diagnostic sonography or ultrasonography) is a diagnostic imaging technique based on the application of ultrasound.
It is used to see internal body structures such as tendons, muscles, joints, vessels and internal organs. Its aim is often to find a source of a disease or to exclude any pathology. The practice of examining pregnant women using ultrasound is called obstetric ultrasound, and is widely used. But, ultrasound is also used for non-invasive examination of body organs like the liver.
Ultrasound is sound waves with frequencies which are higher than those audible to humans (>20,000 Hz). Ultrasonic images also known as sonograms are made by sending pulses of ultrasound into tissue using a probe.
The sound echoes off the tissue; with different tissues reflecting varying degrees of sound. These echoes are recorded and displayed as an image to the operator.
Many different types of images can be formed using sonographic instruments. The most well-known type is a B-mode image, which displays the acoustic impedance of a two-dimensional cross-section of tissue. Other types of image can display blood flow, motion of tissue over time, the location of blood, the presence of specific molecules, the stiffness of tissue, or the anatomy of a three-dimensional region.
Compared to other prominent methods of medical imaging, ultrasound has several advantages. It provides images in real-time, it is portable and can be brought to the bedside, it is substantially lower in cost, and it does not use harmful ionizing radiation.
Drawbacks of ultrasonography include various limits on its field of view including patient cooperation and physique, difficulty imaging structures behind bone and air, and its dependence on a skilled operator.
It is used to see internal body structures such as tendons, muscles, joints, vessels and internal organs. Its aim is often to find a source of a disease or to exclude any pathology. The practice of examining pregnant women using ultrasound is called obstetric ultrasound, and is widely used. But, ultrasound is also used for non-invasive examination of body organs like the liver.
Ultrasound is sound waves with frequencies which are higher than those audible to humans (>20,000 Hz). Ultrasonic images also known as sonograms are made by sending pulses of ultrasound into tissue using a probe.
The sound echoes off the tissue; with different tissues reflecting varying degrees of sound. These echoes are recorded and displayed as an image to the operator.
Many different types of images can be formed using sonographic instruments. The most well-known type is a B-mode image, which displays the acoustic impedance of a two-dimensional cross-section of tissue. Other types of image can display blood flow, motion of tissue over time, the location of blood, the presence of specific molecules, the stiffness of tissue, or the anatomy of a three-dimensional region.
Compared to other prominent methods of medical imaging, ultrasound has several advantages. It provides images in real-time, it is portable and can be brought to the bedside, it is substantially lower in cost, and it does not use harmful ionizing radiation.
Drawbacks of ultrasonography include various limits on its field of view including patient cooperation and physique, difficulty imaging structures behind bone and air, and its dependence on a skilled operator.
Brain-Computer Interface
YouTube Video EEG mind controlled wheelchair - UC Berkeley ME102B/ME135 (demo)
Pictured: LEFT: The groundbreaking mind-controlled BIONIC ARM that plugs into the body and has given wearers back their sense of touch; RIGHT: The First Ever Bionic Leg is powered by man’s brain.
A brain–computer interface (BCI), sometimes called a mind-machine interface (MMI), direct neural interface (DNI), or brain–machine interface (BMI), is a direct communication pathway between an enhanced or wired brain and an external device.
BCIs are often directed at researching, mapping, assisting, augmenting, or repairing human cognitive or sensory-motor functions.
Research on BCIs began in the 1970s at the University of California, Los Angeles (UCLA) under a grant from the National Science Foundation, followed by a contract from DARPA. The papers published after this research also mark the first appearance of the expression brain–computer interface in scientific literature.
The field of BCI research and development has since focused primarily on neuroprosthetics applications that aim at restoring damaged hearing, sight and movement. Thanks to the remarkable cortical plasticity of the brain, signals from implanted prostheses can, after adaptation, be handled by the brain like natural sensor or effector channels.
Following years of animal experimentation, the first neuroprosthetic devices implanted in humans appeared in the mid-1990s.
For further amplification about this topic, click here.
BCIs are often directed at researching, mapping, assisting, augmenting, or repairing human cognitive or sensory-motor functions.
Research on BCIs began in the 1970s at the University of California, Los Angeles (UCLA) under a grant from the National Science Foundation, followed by a contract from DARPA. The papers published after this research also mark the first appearance of the expression brain–computer interface in scientific literature.
The field of BCI research and development has since focused primarily on neuroprosthetics applications that aim at restoring damaged hearing, sight and movement. Thanks to the remarkable cortical plasticity of the brain, signals from implanted prostheses can, after adaptation, be handled by the brain like natural sensor or effector channels.
Following years of animal experimentation, the first neuroprosthetic devices implanted in humans appeared in the mid-1990s.
For further amplification about this topic, click here.
Advancements in Neuro-imaging Technology
YouTube Video: New center advances biomedical and brain imaging
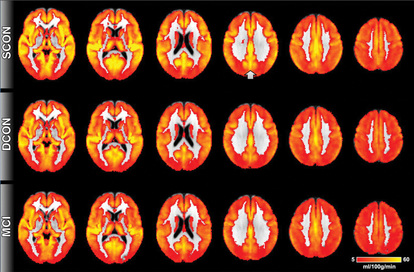
Pictured: Click for an article about the use of neuroimaging: From the National Institute of Mental Health: Neuroimaging and Mental Illness: A Window Into the Brain
Neuroimaging or brain imaging is the use of various techniques to either directly or indirectly image the structure, function/pharmacology of the nervous system.
It is a relatively new discipline within medicine and neuroscience/psychology.
Physicians who specialize in the performance and interpretation of neuroimaging in the clinical setting are neuroradiologists.
Neuroimaging falls into two broad categories:
Functional imaging enables, for example, the processing of information by centers in the brain to be visualized directly. Such processing causes the involved area of the brain to increase metabolism and "light up" on the scan. One of the more controversial uses of neuroimaging has been research into "thought identification" or mind-reading.
For further amplification, click on any of the following:
It is a relatively new discipline within medicine and neuroscience/psychology.
Physicians who specialize in the performance and interpretation of neuroimaging in the clinical setting are neuroradiologists.
Neuroimaging falls into two broad categories:
- Structural imaging, which deals with the structure of the nervous system and the diagnosis of gross (large scale) intracranial disease (such as tumor), and injury, and
- Functional imaging, which is used to diagnose metabolic diseases and lesions on a finer scale (such as Alzheimer's disease) and also for neurological and cognitive psychology research and building brain-computer interfaces.
Functional imaging enables, for example, the processing of information by centers in the brain to be visualized directly. Such processing causes the involved area of the brain to increase metabolism and "light up" on the scan. One of the more controversial uses of neuroimaging has been research into "thought identification" or mind-reading.
For further amplification, click on any of the following:
- 1 History
- 2 Indications
- 3 Brain imaging techniques
- 3.1 Computed axial tomography
- 3.2 Diffuse optical imaging
- 3.3 Event-related optical signal
- 3.4 Magnetic resonance imaging
- 3.5 Functional magnetic resonance imaging
- 3.6 Magnetoencephalography
- 3.7 Positron emission tomography
- 3.8 Single-photon emission computed tomography
- 3.9 Cranial Ultrasound
- 3.10 Comparison of imaging types
- 4 See also
- 5 References
- 6 External links
Advancements in Radiology
YouTube Video MRI Brain Sequences - radiology video tutorial
Pictured: Los Angeles Times May 12, 2016 issue: Radiologists use MRIs to find biomarker for Alzheimer's disease
Radiology is a medical specialty that uses imaging to diagnose and treat diseases seen within the body.
A variety of imaging techniques such as
Interventional radiology is the performance of (usually minimally invasive) medical procedures with the guidance of imaging technologies.
The acquisition of medical imaging is usually carried out by the radiographer, often known as a radiologic technologist.
Depending on location, the diagnostic radiologist, or reporting radiographer, then interprets or "reads" the images and produces a report of their findings and impression or diagnosis. This report is then transmitted to the clinician who requested the imaging, either routinely or emergently.
Imaging exams are stored digitally in the picture archiving and communication system (PACS) where they can be viewed by all members of the healthcare team within the same health system and compared later on with future imaging exams.
Click on any of the following hyperlinks for amplification:
A variety of imaging techniques such as
- X-ray radiography,
- ultrasound,
- computed tomography (CT),
- nuclear medicine including positron emission tomography (PET),
- and magnetic resonance imaging (MRI)
Interventional radiology is the performance of (usually minimally invasive) medical procedures with the guidance of imaging technologies.
The acquisition of medical imaging is usually carried out by the radiographer, often known as a radiologic technologist.
Depending on location, the diagnostic radiologist, or reporting radiographer, then interprets or "reads" the images and produces a report of their findings and impression or diagnosis. This report is then transmitted to the clinician who requested the imaging, either routinely or emergently.
Imaging exams are stored digitally in the picture archiving and communication system (PACS) where they can be viewed by all members of the healthcare team within the same health system and compared later on with future imaging exams.
Click on any of the following hyperlinks for amplification:
- 1 Diagnostic imaging modalities
- 2 Interventional radiology
- 3 Teleradiology
- 4 Professional training
- 5 See also
- 6 References
- 7 External links
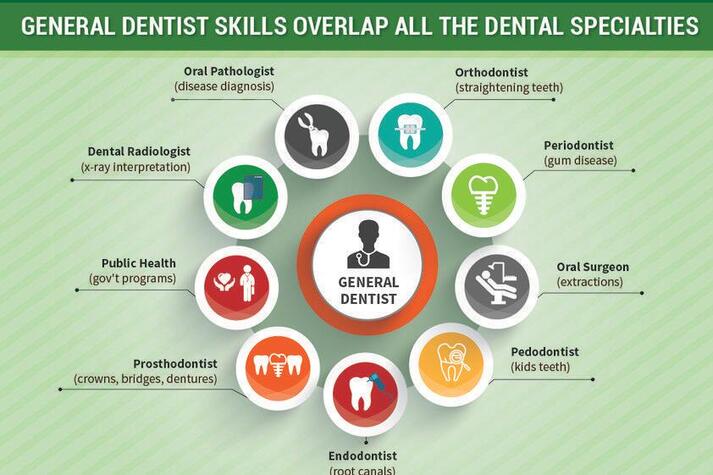
Advancements in Organ Transplants
YouTube Video: Donation and Transplantation: How does it work?
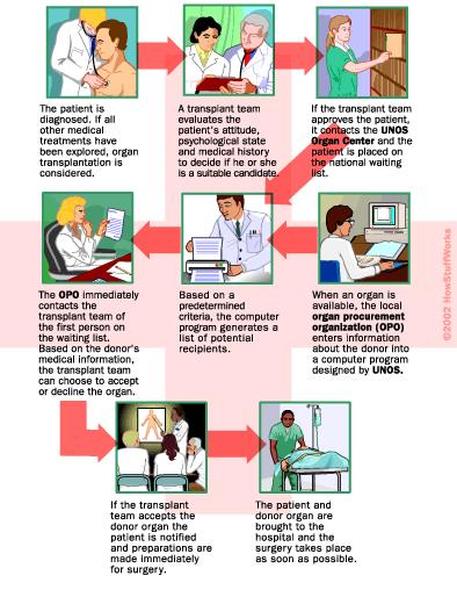
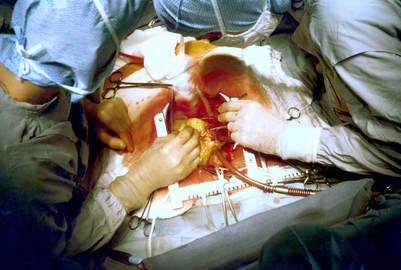
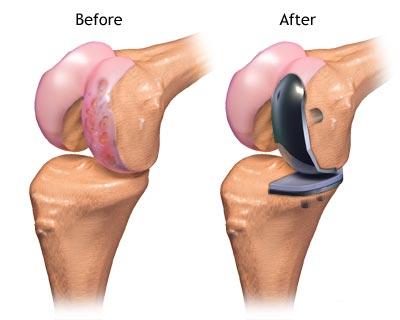
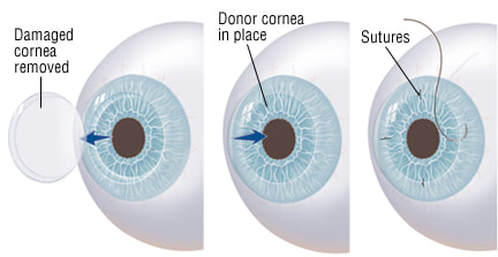
Pictured: How Organ Transplants Work
Organ transplantation is the moving of an organ from one body to another or from a donor site to another location on the person's own body, to replace the recipient's damaged or absent organ.
Organs and/or tissues that are transplanted within the same person's body are called autografts. Transplants that are recently performed between two subjects of the same species are called allografts.
Allografts can either be from a living or cadaveric source.
Organs that can be transplanted are the heart, kidneys, liver, lungs, pancreas, intestine, and thymus. Tissues include bones, tendons (both referred to as musculoskeletal grafts), cornea, skin, heart valves, nerves and veins.
Worldwide, the kidneys are the most commonly transplanted organs, followed by the liver and then the heart. Cornea and musculoskeletal grafts are the most commonly transplanted tissues; these outnumber organ transplants by more than tenfold.
Organ donors may be living, brain dead, or dead via circulatory death. Tissue may be recovered from donors who die of circulatory death, as well as of brain death – up to 24 hours past the cessation of heartbeat.
Unlike organs, most tissues (with the exception of corneas) can be preserved and stored for up to five years, meaning they can be "banked". Transplantation raises a number of bioethical issues, including the definition of death, when and how consent should be given for an organ to be transplanted, and payment for organs for transplantation.
Other ethical issues include transplantation tourism and more broadly the socio-economic context in which organ procurement or transplantation may occur. A particular problem is organ trafficking.
Some organs, such as the brain, cannot be transplanted.
Transplantation medicine is one of the most challenging and complex areas of modern medicine. Some of the key areas for medical management are the problems of transplant rejection, during which the body has an immune response to the transplanted organ, possibly leading to transplant failure and the need to immediately remove the organ from the recipient.
When possible, transplant rejection can be reduced through serotyping to determine the most appropriate donor-recipient match and through the use of immunosuppressant drugs.
For further information, click on any of the following:
Organs and/or tissues that are transplanted within the same person's body are called autografts. Transplants that are recently performed between two subjects of the same species are called allografts.
Allografts can either be from a living or cadaveric source.
Organs that can be transplanted are the heart, kidneys, liver, lungs, pancreas, intestine, and thymus. Tissues include bones, tendons (both referred to as musculoskeletal grafts), cornea, skin, heart valves, nerves and veins.
Worldwide, the kidneys are the most commonly transplanted organs, followed by the liver and then the heart. Cornea and musculoskeletal grafts are the most commonly transplanted tissues; these outnumber organ transplants by more than tenfold.
Organ donors may be living, brain dead, or dead via circulatory death. Tissue may be recovered from donors who die of circulatory death, as well as of brain death – up to 24 hours past the cessation of heartbeat.
Unlike organs, most tissues (with the exception of corneas) can be preserved and stored for up to five years, meaning they can be "banked". Transplantation raises a number of bioethical issues, including the definition of death, when and how consent should be given for an organ to be transplanted, and payment for organs for transplantation.
Other ethical issues include transplantation tourism and more broadly the socio-economic context in which organ procurement or transplantation may occur. A particular problem is organ trafficking.
Some organs, such as the brain, cannot be transplanted.
Transplantation medicine is one of the most challenging and complex areas of modern medicine. Some of the key areas for medical management are the problems of transplant rejection, during which the body has an immune response to the transplanted organ, possibly leading to transplant failure and the need to immediately remove the organ from the recipient.
When possible, transplant rejection can be reduced through serotyping to determine the most appropriate donor-recipient match and through the use of immunosuppressant drugs.
For further information, click on any of the following:
- 1 Types of transplant
- 2 Organs and tissues transplanted
- 3 Types of donor
- 4 Allocation of organs
- 5 Reasons for donation and ethical issues
- 6 Usage
- 7 History
- 8 Society and culture
- 9 Research
- 10 See also
- 11 References
- 12 Further reading
- 13 External links
Advancements in Neurosurgery
YouTube Video A day in the life of a neurosurgeon
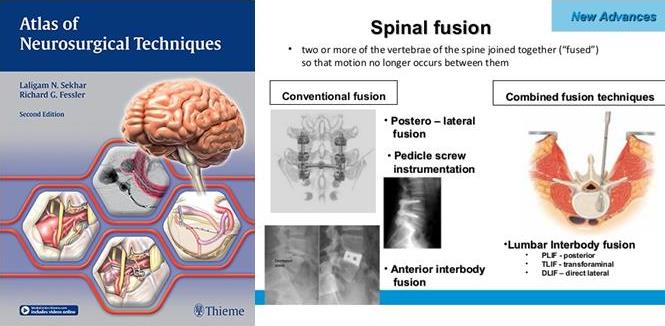
Pictured: LEFT: Atlas of Neurosurgical Techniques; RIGHT: Illustration of Spinal Fusion Surgery
Neurosurgery (or neurological surgery) is the medical specialty concerned with the prevention, diagnosis, treatment, and rehabilitation of disorders which affect any portion of the nervous system including the brain, spinal cord, peripheral nerves, and extra-cranial cerebrovascular system.
In the United States, a neurosurgeon must generally complete four years of undergraduate education, four years of medical school, and seven years of residency
Most, but not all, residency programs have some component of basic science or clinical research. Neurosurgeons may pursue additional training in the form of a fellowship, after residency or in some cases, as a senior resident.
These fellowships include pediatric neurosurgery, trauma/neurocritical care, functional and stereotactic surgery, surgical neuro-oncology, radiosurgery, neurovascular surgery, skull-base surgery, peripheral nerve and spine surgery.
In the U.S., neurosurgery is considered a highly competitive specialty composed of 0.6% of all practicing physicians.
Main divisions of neurosurgery:
General neurosurgery involves most neurosurgical conditions including neuro-trauma and other neuro-emergencies such as intracranial hemorrhage. Most level 1 hospitals have this kind of practice.
Specialized branches have developed to cater to special and difficult conditions. These specialized branches co-exist with general neurosurgery in more sophisticated hospitals. To practice advanced specialization within neurosurgery, additional higher fellowship training of one to two years is expected from the neurosurgeon.
Some of these divisions of neurosurgery are:
Neuroanesthesia is a field of anesthesiology which focuses on neurosurgery. Anesthesia is not used during the middle of an "awake" brain surgery. Awake brain surgery is where the patient is conscious for the middle of the procedure and sedated for the beginning and end. This procedure is used when the tumor does not have clear boundaries and the surgeon wants to know if they are invading on critical regions of the brain which involve functions like talking, cognition, vision, and hearing. It will also be conducted for procedures which the surgeon is trying to combat epileptic seizures.
Neurosurgery methods
Neuroradiology plays a key role not only in diagnosis but also in the operative phase of neurosurgery.
Neuroradiology methods are used in modern neurosurgery diagnosis and treatment. They include:
Some neurosurgery procedures involve the use of intra-operative MRI and functional MRI.
In conventional open surgery the neurosurgeon opens the skull, creating a large opening to access the brain. Techniques involving smaller openings with the aid of microscopes and endoscopes are now being used as well.
Methods that utilize small craniotomies in conjunction with high-clarity microscopic visualization of neural tissue offer excellent results. However, the open methods are still traditionally used in trauma or emergency situations.
Microsurgery is utilized in many aspects of neurological surgery. Microvascular techniques are used in EC-IC bypass surgery and in restoration carotid endarterectomy. The clipping of an aneurysm is performed under microscopic vision. minimally-invasive spine surgery utilizes microscopes or endoscopes. Procedures such as microdiscectomy, laminectomy, and artificial disc replacement rely on microsurgery.
Using stereotaxy neurosurgeons can approach a minute target in the brain through a minimal opening. This is used in functional neurosurgery where electrodes are implanted or gene therapy is instituted with high level of accuracy as in the case of Parkinson's disease or Alzheimer's disease. Using the combination method of open and stereotactic surgery, intraventricular hemorrhages can potentially be evacuated successfully.
Conventional surgery using image guidance technologies is also becoming common and is referred to as surgical navigation, computer assisted surgery, navigated surgery, stereotactic navigation. Similar to a car or mobile Global Positioning System (GPS), image guided surgery systems, like Curve Image Guided Surgery and StealthStation, use cameras or electromagnetic fields to capture and relay the patient’s anatomy and the surgeon’s precise movements in relation to the patient, to computer monitors in the operating room.
These sophisticated computerized systems are used before and during surgery to help orient the surgeon with three-dimensional images of the patient’s anatomy including the tumor.
Minimally invasive endoscopic surgery is commonly utilized by neurosurgeons when appropriate. Techniques such as endoscopic endonasal surgery are used in pituitary tumors, craniopharyngiomas, chordomas, and the repair of cerebrospinal fluid leaks.
Ventricular endoscopy is used in the treatment of intraventricular bleeds, hydrocephalus, colloid cyst and neurocysticercosis. Endonasal endoscopy is at times carried out with neurosurgeons and ENT surgeons working together as a team.
Repair of craniofacial disorders and disturbance of cerebrospinal fluid circulation is done by neurosurgeons who also occasionally team up with maxillofacial and plastic surgeons. Cranioplasty for craniosynostosis is performed by pediatric neurosurgeons with or without plastic surgeons.
Neurosurgeons are involved in stereotactic radiosurgery along with radiation oncologists in tumor and AVM treatment. Radiosurgical methods such as Gamma knife, Cyberknife and Novalis Radiosurgery are used as well.
Endovascular Neurosurgery utilize endovascular image guided procedures for the treatment of aneurysms, AVMs, carotid stenosis, strokes, and spinal malformations, and vasospasms. Techniques such as angioplasty, stenting, clot retrieval, embolization, and diagnostic angiography are endovascular procedures.
A common procedure performed in neurosurgery is the placement of Ventriculo-Peritoneal Shunt (VP Shunt). In pediatric practice this is often implemented in cases of congenital hydrocephalus. The most common indication for this procedure in adults is Normal Pressure Hydrocephalus (NPH).
Neurosurgery of the spine covers the cervical, thoracic and lumbar spine. Some indications for spine surgery include spinal cord compression resulting from trauma, arthritis of the spinal discs, or spondylosis. In cervical cord compression, patients may have difficulty with gait, balance issues, and/or numbness and tingling in the hands or feet.
Spondylosis is the condition of spinal disc degeneration and arthritis that may compress the spinal canal. This condition can often result in bone-spurring and disc herniation. Power drills and special instruments are often used to correct any compression problems of the spinal canal. Disc herniations of spinal vertebral discs are removed with special rongeurs. This procedure is known as a discectomy.
Generally once a disc is removed it is replaced by an implant which will create a bony fusion between vertebral bodies above and below. Instead, a mobile disc could be implanted into the disc space to maintain mobility. This is commonly used in cervical disc surgery. At times instead of disc removal a Laser discectomy could be used to decompress a nerve root. This method is mainly used for lumbar discs. Laminectomy is the removal of the Lamina portion of the vertebrae of the spine in order to make room for the compressed nerve tissue.
Radiology assisted spine surgery uses minimally-invasive procedures. They include the techniques of vertebroplasty and kyphoplasty in which certain types of spinal fractures are managed.
Potentially unstable spines will need spine fusions. At present these procedures include complex instrumentation. Spine fusions could be performed as open surgery or as minimally invasive surgery. Anterior cervical diskectomy and fusion is a common surgery that is performed for disc disease of cervical spine.
However, each method described above may not work in all patients. Therefore, careful selection of patients for each procedure is important. It has to be noted that if there is prior permanent neural tissue damage spinal surgery may not take away the symptoms.
Surgery for chronic pain is a sub branch of functional neurosurgery. Some of the techniques include implantation of deep brain stimulators, spinal cord stimulators, peripheral stimulators and pain pumps.
Surgery of the peripheral nervous system is also possible, and includes the very common procedures of carpal tunnel decompression and peripheral nerve transposition. Numerous other types of nerve entrapment conditions and other problems with the peripheral nervous system are treated as well.
Other conditions treated by neurosurgeons include:
In the United States, a neurosurgeon must generally complete four years of undergraduate education, four years of medical school, and seven years of residency
Most, but not all, residency programs have some component of basic science or clinical research. Neurosurgeons may pursue additional training in the form of a fellowship, after residency or in some cases, as a senior resident.
These fellowships include pediatric neurosurgery, trauma/neurocritical care, functional and stereotactic surgery, surgical neuro-oncology, radiosurgery, neurovascular surgery, skull-base surgery, peripheral nerve and spine surgery.
In the U.S., neurosurgery is considered a highly competitive specialty composed of 0.6% of all practicing physicians.
Main divisions of neurosurgery:
General neurosurgery involves most neurosurgical conditions including neuro-trauma and other neuro-emergencies such as intracranial hemorrhage. Most level 1 hospitals have this kind of practice.
Specialized branches have developed to cater to special and difficult conditions. These specialized branches co-exist with general neurosurgery in more sophisticated hospitals. To practice advanced specialization within neurosurgery, additional higher fellowship training of one to two years is expected from the neurosurgeon.
Some of these divisions of neurosurgery are:
- stereotactic neurosurgery, functional neurosurgery, and epilepsy surgery (the latter includes partial or total corpus callosotomy- severing part or all of the corpus callosum to stop or lessen seizure spread and activity, and the surgical removal of functional- physiological- and/or anatomical pieces or divisions of the brain, called epileptic foci, that are operable and that are causing seizures, and also the more radical and very, very rare partial or total lobectomy, or even hemispherectomy- the removal of part or all of one of the lobes, or one of the cerebral hemispheres of the brain; those two procedures, when possible, are also very, very rarely used in oncological neurosurgery or to treat very severe neurological trauma, such as stab or gunshot wounds to the brain)
- oncological neurosurgery also called neurosurgical oncology; includes pediatric oncological neurosurgery; treatment of benign and malignant central and peripheral nervous system cancers and pre-cancerous lesions in adults and children (including, among others, glioblastoma multiforme and other gliomas, brain stem cancer, astrocytoma, pontine glioma, medulloblastoma, spinal cancer, tumors of the meninges and intracranial spaces, secondary metastases to the brain, spine, and nerves, and peripheral nervous system tumors)
- peripheral nerve surgery
- pediatric neurosurgery (for cancer, seizures, bleeding, stroke, cognitive disorders or congenital neurological disorders)
- neuropsychiatric surgery (neurosurgery for the treatment of adult or pediatric mental illnesses)
- geriatric neurosurgery (for the treatment of neurological disorders and dementias and mental impairments due to age, but not due to a stroke, seizure, tumor, concussion, or neurovascular cause- namely, Parkinsonism, Alzheimer's, multiple sclerosis, and similar disorders)
Neuroanesthesia is a field of anesthesiology which focuses on neurosurgery. Anesthesia is not used during the middle of an "awake" brain surgery. Awake brain surgery is where the patient is conscious for the middle of the procedure and sedated for the beginning and end. This procedure is used when the tumor does not have clear boundaries and the surgeon wants to know if they are invading on critical regions of the brain which involve functions like talking, cognition, vision, and hearing. It will also be conducted for procedures which the surgeon is trying to combat epileptic seizures.
Neurosurgery methods
Neuroradiology plays a key role not only in diagnosis but also in the operative phase of neurosurgery.
Neuroradiology methods are used in modern neurosurgery diagnosis and treatment. They include:
- computer assisted imaging computed tomography (CT),
- magnetic resonance imaging (MRI),
- positron emission tomography (PET),
- magnetoencephalography (MEG),
- and stereotactic radiosurgery.
Some neurosurgery procedures involve the use of intra-operative MRI and functional MRI.
In conventional open surgery the neurosurgeon opens the skull, creating a large opening to access the brain. Techniques involving smaller openings with the aid of microscopes and endoscopes are now being used as well.
Methods that utilize small craniotomies in conjunction with high-clarity microscopic visualization of neural tissue offer excellent results. However, the open methods are still traditionally used in trauma or emergency situations.
Microsurgery is utilized in many aspects of neurological surgery. Microvascular techniques are used in EC-IC bypass surgery and in restoration carotid endarterectomy. The clipping of an aneurysm is performed under microscopic vision. minimally-invasive spine surgery utilizes microscopes or endoscopes. Procedures such as microdiscectomy, laminectomy, and artificial disc replacement rely on microsurgery.
Using stereotaxy neurosurgeons can approach a minute target in the brain through a minimal opening. This is used in functional neurosurgery where electrodes are implanted or gene therapy is instituted with high level of accuracy as in the case of Parkinson's disease or Alzheimer's disease. Using the combination method of open and stereotactic surgery, intraventricular hemorrhages can potentially be evacuated successfully.
Conventional surgery using image guidance technologies is also becoming common and is referred to as surgical navigation, computer assisted surgery, navigated surgery, stereotactic navigation. Similar to a car or mobile Global Positioning System (GPS), image guided surgery systems, like Curve Image Guided Surgery and StealthStation, use cameras or electromagnetic fields to capture and relay the patient’s anatomy and the surgeon’s precise movements in relation to the patient, to computer monitors in the operating room.
These sophisticated computerized systems are used before and during surgery to help orient the surgeon with three-dimensional images of the patient’s anatomy including the tumor.
Minimally invasive endoscopic surgery is commonly utilized by neurosurgeons when appropriate. Techniques such as endoscopic endonasal surgery are used in pituitary tumors, craniopharyngiomas, chordomas, and the repair of cerebrospinal fluid leaks.
Ventricular endoscopy is used in the treatment of intraventricular bleeds, hydrocephalus, colloid cyst and neurocysticercosis. Endonasal endoscopy is at times carried out with neurosurgeons and ENT surgeons working together as a team.
Repair of craniofacial disorders and disturbance of cerebrospinal fluid circulation is done by neurosurgeons who also occasionally team up with maxillofacial and plastic surgeons. Cranioplasty for craniosynostosis is performed by pediatric neurosurgeons with or without plastic surgeons.
Neurosurgeons are involved in stereotactic radiosurgery along with radiation oncologists in tumor and AVM treatment. Radiosurgical methods such as Gamma knife, Cyberknife and Novalis Radiosurgery are used as well.
Endovascular Neurosurgery utilize endovascular image guided procedures for the treatment of aneurysms, AVMs, carotid stenosis, strokes, and spinal malformations, and vasospasms. Techniques such as angioplasty, stenting, clot retrieval, embolization, and diagnostic angiography are endovascular procedures.
A common procedure performed in neurosurgery is the placement of Ventriculo-Peritoneal Shunt (VP Shunt). In pediatric practice this is often implemented in cases of congenital hydrocephalus. The most common indication for this procedure in adults is Normal Pressure Hydrocephalus (NPH).
Neurosurgery of the spine covers the cervical, thoracic and lumbar spine. Some indications for spine surgery include spinal cord compression resulting from trauma, arthritis of the spinal discs, or spondylosis. In cervical cord compression, patients may have difficulty with gait, balance issues, and/or numbness and tingling in the hands or feet.
Spondylosis is the condition of spinal disc degeneration and arthritis that may compress the spinal canal. This condition can often result in bone-spurring and disc herniation. Power drills and special instruments are often used to correct any compression problems of the spinal canal. Disc herniations of spinal vertebral discs are removed with special rongeurs. This procedure is known as a discectomy.
Generally once a disc is removed it is replaced by an implant which will create a bony fusion between vertebral bodies above and below. Instead, a mobile disc could be implanted into the disc space to maintain mobility. This is commonly used in cervical disc surgery. At times instead of disc removal a Laser discectomy could be used to decompress a nerve root. This method is mainly used for lumbar discs. Laminectomy is the removal of the Lamina portion of the vertebrae of the spine in order to make room for the compressed nerve tissue.
Radiology assisted spine surgery uses minimally-invasive procedures. They include the techniques of vertebroplasty and kyphoplasty in which certain types of spinal fractures are managed.
Potentially unstable spines will need spine fusions. At present these procedures include complex instrumentation. Spine fusions could be performed as open surgery or as minimally invasive surgery. Anterior cervical diskectomy and fusion is a common surgery that is performed for disc disease of cervical spine.
However, each method described above may not work in all patients. Therefore, careful selection of patients for each procedure is important. It has to be noted that if there is prior permanent neural tissue damage spinal surgery may not take away the symptoms.
Surgery for chronic pain is a sub branch of functional neurosurgery. Some of the techniques include implantation of deep brain stimulators, spinal cord stimulators, peripheral stimulators and pain pumps.
Surgery of the peripheral nervous system is also possible, and includes the very common procedures of carpal tunnel decompression and peripheral nerve transposition. Numerous other types of nerve entrapment conditions and other problems with the peripheral nervous system are treated as well.
Other conditions treated by neurosurgeons include:
- Meningitis and other central nervous system infections including abscesses
- Spinal disc herniation
- Cervical spinal stenosis and Lumbar spinal stenosis
- Hydrocephalus
- Head trauma (brain hemorrhages, skull fractures, etc.)
- Spinal cord trauma
- Traumatic injuries of peripheral nerves
- Tumors of the spine, spinal cord and peripheral nerves
- Intracerebral hemorrhage, such as subarachnoid hemorrhage, interdepartmental, and intracellular hemorrhages
- Some forms of drug-resistant epilepsy
- Some forms of movement disorders (advanced Parkinson's disease, chorea) – this involves the use of specially developed minimally invasive stereotactic techniques (functional, stereotactic neurosurgery) such as ablative surgery and deep brain stimulation surgery
- Intractable pain of cancer or trauma patients and cranial/peripheral nerve pain
- Some forms of intractable psychiatric disorders
- Vascular malformations (i.e., arteriovenous malformations, venous angiomas, cavernous angiomas, capillary telangectasias) of the brain and spinal cord
- Moyamoya disease.
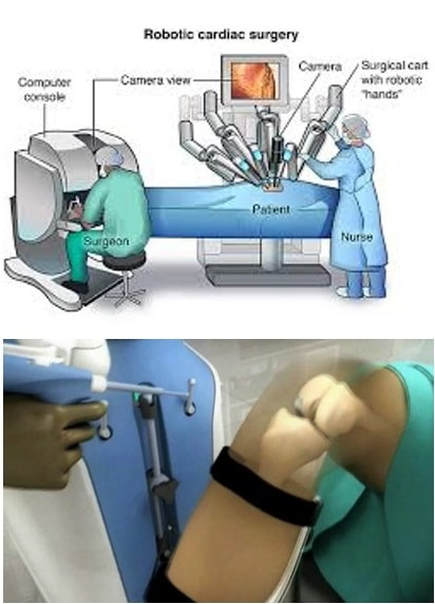
Advancements in Heart and Lung Surgery
YouTube Video by the American College of Surgeons (ACS) Education for a Better Recovery Program, 'Your Lung Operation.'
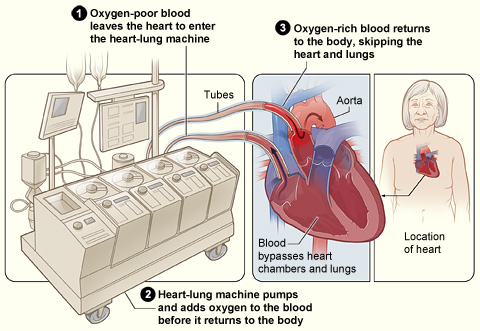
Pictured: The image shows how a heart-lung bypass machine works during surgery (courtesy of the National Heart, Lung and Blood Institute: a department of the U.S. National Institute of Health
Cardiothoracic surgery is the field of medicine involved in surgical treatment of organs inside the thorax (the chest)—generally treatment of conditions of the heart (heart disease) and lungs (lung disease).
A cardiac surgery residency typically comprises anywhere from 9 to 14 years (or longer) of training to become a fully qualified surgeon.
Cardiac surgery training may be combined with thoracic surgery and / or vascular surgery and called cardiovascular (CV) / cardiothoracic (CT) / cardiovascular thoracic (CVT) surgery.
Cardiac surgeons may enter a cardiac surgery residency directly from medical school, or first complete a general surgery residency followed by a fellowship.
Cardiac surgeons may further sub-specialize cardiac surgery by doing a fellowship in a variety of topics including: pediatric cardiac surgery, cardiac transplantation, adult acquired heart disease, weak heart issues, and many more problems in the heart.
Cardiac surgery training in the United States is combined with thoracic surgery and called cardiothoracic surgery. A cardiothoracic surgeon in the U.S. is a physician (D.O. or M.D.) who first completes a general surgery residency (typically 5–7 years), followed by a cardiothoracic surgery fellowship (typically 2–3 years).
The cardiothoracic surgery fellowship typically spans two or three years, but certification is based on the number of surgeries performed as the operating surgeon, not the time spent in the program, in addition to passing rigorous board certification tests. Recently, however, options for an integrated 6-year cardiothoracic residency (in place of the general surgery residency plus cardiothoracic residency) have been established at several programs.
Applicants match into these I-6 programs directly out of medical school, and the application process has been extremely competitive for these positions as there were approximately 160 applicants for 10 spots in the U.S. in 2010. As of May 2013, there are now 20 approved programs, which include the following:
Click Here for List of Approved Programs
Click on any of the following Hyperlinks for amplification:
A cardiac surgery residency typically comprises anywhere from 9 to 14 years (or longer) of training to become a fully qualified surgeon.
Cardiac surgery training may be combined with thoracic surgery and / or vascular surgery and called cardiovascular (CV) / cardiothoracic (CT) / cardiovascular thoracic (CVT) surgery.
Cardiac surgeons may enter a cardiac surgery residency directly from medical school, or first complete a general surgery residency followed by a fellowship.
Cardiac surgeons may further sub-specialize cardiac surgery by doing a fellowship in a variety of topics including: pediatric cardiac surgery, cardiac transplantation, adult acquired heart disease, weak heart issues, and many more problems in the heart.
Cardiac surgery training in the United States is combined with thoracic surgery and called cardiothoracic surgery. A cardiothoracic surgeon in the U.S. is a physician (D.O. or M.D.) who first completes a general surgery residency (typically 5–7 years), followed by a cardiothoracic surgery fellowship (typically 2–3 years).
The cardiothoracic surgery fellowship typically spans two or three years, but certification is based on the number of surgeries performed as the operating surgeon, not the time spent in the program, in addition to passing rigorous board certification tests. Recently, however, options for an integrated 6-year cardiothoracic residency (in place of the general surgery residency plus cardiothoracic residency) have been established at several programs.
Applicants match into these I-6 programs directly out of medical school, and the application process has been extremely competitive for these positions as there were approximately 160 applicants for 10 spots in the U.S. in 2010. As of May 2013, there are now 20 approved programs, which include the following:
Click Here for List of Approved Programs
Click on any of the following Hyperlinks for amplification:
Dental Technology Advancements by Consumer Guide to Dentistry including the Timeline for the History of Dentistry by the American Dental Association (ADA)
YouTube Video: The Newest Technology in Dentistry
To the casual observer, it may appear that not much has changed in dentistry. Yet dental technologies have been evolving continually, helping to transform the field of dentistry. New technologies are developed with a focus on creating products and developing techniques that can be used by your dentist to help prevent, diagnose and/or treat dental conditions and diseases early and effectively.
There are many dental technologies for your dentist to choose from, with benefits that can provide you with more comfort and ease during treatment.
Some of the more popular technologies include:
Air-Abrasion: Serving as an alternative to a traditional dental drill, an air-abrasion system is primarily used to treat small cavities, preserving healthy tooth structure without the use of a local anesthetic. Air-abrasion allows for the precise removal of decay through a blast of pellets consisting of air and aluminum oxide. The air-abrasion technique can also be used to help repair old tooth restorations by accessing difficult areas such as those between the teeth.
Bone Replacement: There are three types of bone replacement used to assist people suffering from bone loss or those requiring extraction:
Platelet-rich growth factors can help induce rapid bone growth and healing. It is used in bone replacement and offers rapid healing properties. Bone replacement performed by clinicians today is more refined than in the past and can be more easily assimilated into the existing bone structure.
CAD/CAM: CAD/CAM (computer assisted design, computer assisted manufacture) technology allows for the fabrication of dental restorations through computerized technology. Your dentist may work with CAD/CAM in the office to complete tooth restorations in one visit that would otherwise require two visits to complete. These procedures can include: inlays, onlays, porcelain veneers, dental crowns and dental bridges.
Caries Detection Solution: Caries detection solution is a liquid red dye that is applied over a tooth to confirm that all tooth decay is removed from an affected area that has been treated. This solution is very similar to plaque disclosing tablets that are used after brushing to highlight any areas you missed or that aren't thoroughly cleaned.
CAT Scans: A 3-D image CAT scan is used to help implantologists (dentists who provide surgical and restorative implant services) view and work on the jawbone or surrounding bone structure to produce more accurate results. CAT scan technology has become increasingly specialized for dentistry as implants, rather than dentures, have become the standard of care for tooth replacement.
Composite Materials: Composite resin materials are now used in some veneers and other restorations, to fill cavities and to bond onto or rebuild a tooth. Composite resins offer a tooth-like resolution and have grown in popularity over the years. They are continually being improved and refined to better replicate tooth colors, to be easier to apply and to hold their shape without slumping off the tooth. The handling of and the speeds associated with curing composite resins, coupled with the translucent qualities of the newer materials, has helped to produce beautiful natural looking results.
Diagnodent: Diagnodent is a tool used for the early detection of cavities. The advanced technology uses sound pulse and laser to detect caries earlier than traditional methods allowed, so that treatment can commence immediately limiting the amount of decay allowed to occur. This helps preserve the maximum amount of natural healthy tooth structure.
Dental Implants: Dental implant technology continues to improve. Mini-implants can now accommodate small tooth replacements. The bio-integration of the titanium tooth root with human bone is completely predictable. The results are very long lasting. The industry has also focused on reducing treatment time and some implants can be placed immediately after tooth extraction as opposed to waiting six months after extraction. In many instances, dental implants are now the standard of care if a tooth needs to be extracted or if there is a question as to whether a root canal procedure should be done.
Desensitizers: Desensitizers can be used by your dentist or hygienist prior to dental treatment if you have sensitive teeth, so that you are comfortable throughout treatment. Desensitizers can be used alone or in conjunction with other pain and anxiety relief modalities such as a local anesthetic or sedation dentistry.
Digital X-rays: Digital radiographs offer a way to capture dental images through a sensor that processes the image onto a computer screen. Digital X-rays can provide greater comfort than traditional X-rays and certainly reduce exposure to radiation. Four digital radiographs are about equal to one "paper" X-ray.
Electric Hand Pieces: Electric hand pieces can assist in hygiene procedures and can be used with rotary cutting instruments. Electric hand pieces offer a smooth delivery of material which puts less stress on the healthy tooth structure. They are often quieter too.
Internet: Today, dental appointments can be made through a practice website. Dentists can send dental technicians emails with your intra-oral photos in real time so that they can discuss the case in real time with you in the chair. The Internet also serves as an informational tool through which you can receive updates as they relate to the field of dentistry.
Intra-Oral Camera: Intra-oral cameras can produce accurate images of your teeth and the supporting structure. This allows you, your dentist and a dental technician that might be involved in your treatment, to see tooth defects. Intra-oral cameras also help you to learn more about dental hygiene practices, including where to focus on brushing your teeth.
Lasers: Lasers offer reduced discomfort and in some cases, a suture free option for the treatment of benign tumors, cold sores, crown lengthening, decay removal, gummy smile changes, dental fillings, tongue tie and speech impediment improvements, nerve regeneration for damaged nerves and blood vessels and scars. Lasers may also be applied in the treatment of select dental conditions such as sleep apnea, certain cases of TMD and tooth sensitivity. This is a very exciting area of development in dental technologies. Lasers use light energy as their method of operation, resulting in a shortened and almost painless healing period.
Optical Scanners: Optical Scanners provide a digital map of the tooth and create a 3-D replica model of the dental structure. This helps in accurate color analysis for cosmetic restorations made in a dental laboratory such as porcelain veneers, crowns and bridges.
Microscope: The use of microscopes in dentistry has been one of the latest trends to perfect acute vision for dentists. Microscopes offer dentists the ability to see micro-cracks, weakened underlying tooth structure and the proximity of the dental nerves with precise accuracy. Microscopes also offer more accuracy in removing affected tooth structure while preserving healthy tooth structure. The microscope is an improved diagnostic tool as well as a treatment-assist dental tool.
NTI Splint: The NTI splint is an anterior splint used for TMD patients. The NTI and other splints, such as the Kois Deprogrammer have the potential application of helping to treat patients affected by migraine headaches.
Periodontal Antibiotics: There are "site specific" antibiotics that are designed to concentrate the treatment in specific locations. Periodontal antibiotics are applied directly to the diseased site, enhancing the effectiveness of treatment for periodontal disease.
VELscope: VELscope is a brand new FDA-approved oral cancer screening system that uses incandescent light so your dentist can see abnormalities that may not be apparent or visible to the naked eye. VELscope is also used by oral surgeons to help identify diseased tissue around a lesion and determine the appropriate margin for surgical excision.
ViziLite: ViziLite is a recently approved oral lesion identification and marking device. It is a painless screening tool for the detection of small changes in your mouth. Vizilite also identifies, evaluates and monitors oral abnormalities in patients who are at increased risk for oral cancer.
Periometer: The Periometer is an instrumented percussion diagnostic system designed for a range of dental applications, including monitoring implant osseointegration and the formation of cracks in natural teeth. Thus far, the results have been correlated with the presence and location of defects as well as the overall dynamic properties of any oral structure. The use of the Periometer for determining optimum dental therapeutics has also been explored. Current research indicates that routine use of the Periometer in a dental practice can be critically important for avoiding catastrophic failure of both implants and teeth.
The Wand: The Wand is a computerized tool that can deliver anesthesia in a slow and methodic manner. The sensation of pain often associated with an injection is caused as a result of the pressure of the liquid being injected. The slow and gentle delivery associated with The Wand often makes injections painless. The delivery holder is small and easy for the dentist to use.
There are an increasing number of dental technologies from which your dentist can choose. The benefits that you can receive by visiting your dentist today may offer you more comfort and ease than in days past.
There are many dental technologies for your dentist to choose from, with benefits that can provide you with more comfort and ease during treatment.
Some of the more popular technologies include:
Air-Abrasion: Serving as an alternative to a traditional dental drill, an air-abrasion system is primarily used to treat small cavities, preserving healthy tooth structure without the use of a local anesthetic. Air-abrasion allows for the precise removal of decay through a blast of pellets consisting of air and aluminum oxide. The air-abrasion technique can also be used to help repair old tooth restorations by accessing difficult areas such as those between the teeth.
Bone Replacement: There are three types of bone replacement used to assist people suffering from bone loss or those requiring extraction:
- Autogenous Man Made Bone Replacement: A freeze dried material that is made in the laboratory.
- Cadaver/Animal Bone Replacement: Bone that is preserved, processed and sterilized from a deceased individual or animal source.
- Grafting Bone Replacement: Bone taken from another area of the body, such as the iliac crest section of the pelvis.
Platelet-rich growth factors can help induce rapid bone growth and healing. It is used in bone replacement and offers rapid healing properties. Bone replacement performed by clinicians today is more refined than in the past and can be more easily assimilated into the existing bone structure.
CAD/CAM: CAD/CAM (computer assisted design, computer assisted manufacture) technology allows for the fabrication of dental restorations through computerized technology. Your dentist may work with CAD/CAM in the office to complete tooth restorations in one visit that would otherwise require two visits to complete. These procedures can include: inlays, onlays, porcelain veneers, dental crowns and dental bridges.
Caries Detection Solution: Caries detection solution is a liquid red dye that is applied over a tooth to confirm that all tooth decay is removed from an affected area that has been treated. This solution is very similar to plaque disclosing tablets that are used after brushing to highlight any areas you missed or that aren't thoroughly cleaned.
CAT Scans: A 3-D image CAT scan is used to help implantologists (dentists who provide surgical and restorative implant services) view and work on the jawbone or surrounding bone structure to produce more accurate results. CAT scan technology has become increasingly specialized for dentistry as implants, rather than dentures, have become the standard of care for tooth replacement.
Composite Materials: Composite resin materials are now used in some veneers and other restorations, to fill cavities and to bond onto or rebuild a tooth. Composite resins offer a tooth-like resolution and have grown in popularity over the years. They are continually being improved and refined to better replicate tooth colors, to be easier to apply and to hold their shape without slumping off the tooth. The handling of and the speeds associated with curing composite resins, coupled with the translucent qualities of the newer materials, has helped to produce beautiful natural looking results.
Diagnodent: Diagnodent is a tool used for the early detection of cavities. The advanced technology uses sound pulse and laser to detect caries earlier than traditional methods allowed, so that treatment can commence immediately limiting the amount of decay allowed to occur. This helps preserve the maximum amount of natural healthy tooth structure.
Dental Implants: Dental implant technology continues to improve. Mini-implants can now accommodate small tooth replacements. The bio-integration of the titanium tooth root with human bone is completely predictable. The results are very long lasting. The industry has also focused on reducing treatment time and some implants can be placed immediately after tooth extraction as opposed to waiting six months after extraction. In many instances, dental implants are now the standard of care if a tooth needs to be extracted or if there is a question as to whether a root canal procedure should be done.
Desensitizers: Desensitizers can be used by your dentist or hygienist prior to dental treatment if you have sensitive teeth, so that you are comfortable throughout treatment. Desensitizers can be used alone or in conjunction with other pain and anxiety relief modalities such as a local anesthetic or sedation dentistry.
Digital X-rays: Digital radiographs offer a way to capture dental images through a sensor that processes the image onto a computer screen. Digital X-rays can provide greater comfort than traditional X-rays and certainly reduce exposure to radiation. Four digital radiographs are about equal to one "paper" X-ray.
Electric Hand Pieces: Electric hand pieces can assist in hygiene procedures and can be used with rotary cutting instruments. Electric hand pieces offer a smooth delivery of material which puts less stress on the healthy tooth structure. They are often quieter too.
Internet: Today, dental appointments can be made through a practice website. Dentists can send dental technicians emails with your intra-oral photos in real time so that they can discuss the case in real time with you in the chair. The Internet also serves as an informational tool through which you can receive updates as they relate to the field of dentistry.
Intra-Oral Camera: Intra-oral cameras can produce accurate images of your teeth and the supporting structure. This allows you, your dentist and a dental technician that might be involved in your treatment, to see tooth defects. Intra-oral cameras also help you to learn more about dental hygiene practices, including where to focus on brushing your teeth.
Lasers: Lasers offer reduced discomfort and in some cases, a suture free option for the treatment of benign tumors, cold sores, crown lengthening, decay removal, gummy smile changes, dental fillings, tongue tie and speech impediment improvements, nerve regeneration for damaged nerves and blood vessels and scars. Lasers may also be applied in the treatment of select dental conditions such as sleep apnea, certain cases of TMD and tooth sensitivity. This is a very exciting area of development in dental technologies. Lasers use light energy as their method of operation, resulting in a shortened and almost painless healing period.
Optical Scanners: Optical Scanners provide a digital map of the tooth and create a 3-D replica model of the dental structure. This helps in accurate color analysis for cosmetic restorations made in a dental laboratory such as porcelain veneers, crowns and bridges.
Microscope: The use of microscopes in dentistry has been one of the latest trends to perfect acute vision for dentists. Microscopes offer dentists the ability to see micro-cracks, weakened underlying tooth structure and the proximity of the dental nerves with precise accuracy. Microscopes also offer more accuracy in removing affected tooth structure while preserving healthy tooth structure. The microscope is an improved diagnostic tool as well as a treatment-assist dental tool.
NTI Splint: The NTI splint is an anterior splint used for TMD patients. The NTI and other splints, such as the Kois Deprogrammer have the potential application of helping to treat patients affected by migraine headaches.
Periodontal Antibiotics: There are "site specific" antibiotics that are designed to concentrate the treatment in specific locations. Periodontal antibiotics are applied directly to the diseased site, enhancing the effectiveness of treatment for periodontal disease.
VELscope: VELscope is a brand new FDA-approved oral cancer screening system that uses incandescent light so your dentist can see abnormalities that may not be apparent or visible to the naked eye. VELscope is also used by oral surgeons to help identify diseased tissue around a lesion and determine the appropriate margin for surgical excision.
ViziLite: ViziLite is a recently approved oral lesion identification and marking device. It is a painless screening tool for the detection of small changes in your mouth. Vizilite also identifies, evaluates and monitors oral abnormalities in patients who are at increased risk for oral cancer.
Periometer: The Periometer is an instrumented percussion diagnostic system designed for a range of dental applications, including monitoring implant osseointegration and the formation of cracks in natural teeth. Thus far, the results have been correlated with the presence and location of defects as well as the overall dynamic properties of any oral structure. The use of the Periometer for determining optimum dental therapeutics has also been explored. Current research indicates that routine use of the Periometer in a dental practice can be critically important for avoiding catastrophic failure of both implants and teeth.
The Wand: The Wand is a computerized tool that can deliver anesthesia in a slow and methodic manner. The sensation of pain often associated with an injection is caused as a result of the pressure of the liquid being injected. The slow and gentle delivery associated with The Wand often makes injections painless. The delivery holder is small and easy for the dentist to use.
There are an increasing number of dental technologies from which your dentist can choose. The benefits that you can receive by visiting your dentist today may offer you more comfort and ease than in days past.
Facial Transplants
YouTube Video: Man Gets Full Facial Transplant*
*--Meet Patrick Hardison, a firefighter who lost his face and received the first successful total face transplant in 2015. You can read more about him here: http://www.nymag.com/face-transplant
Pictured: Man with LEFT: Original face; CENTER: after Injuries; and RIGHT: Today
A face transplant is a medical procedure to replace all or part of a person's face using tissue from a cadaver. The world's first partial face transplant on a living human was carried out in France in 2005. The world's first full face transplant was completed in Spain in 2010. Turkey, France, the United States and Spain (in order of total number of successful face transplants performed) are considered the leading countries in the research into the procedure.
People with faces disfigured by trauma, burns, disease, or birth defects might aesthetically benefit from the procedure. Professor Peter Butler at the Royal Free Hospital first suggested this approach in treating people with facial disfigurement in a Lancet article in 2002. This suggestion caused considerable debate at the time concerning the ethics of this procedure.
An alternative to a face transplant is facial reconstruction, which typically involves moving the patient's own skin from their back, buttocks, thighs, or chest to their face in a series of as many as 50 operations to regain even limited functionality, and a face that is often likened to a mask or a living quilt.
L. Scott Levin, M.D., FACS, Chair, Department of Orthopaedic Surgery at University of Pennsylvania School of Medicine, has described the procedure as "the single most important area of reconstructive research".
Click on any of the following blue hyperlinks for further amplification:
People with faces disfigured by trauma, burns, disease, or birth defects might aesthetically benefit from the procedure. Professor Peter Butler at the Royal Free Hospital first suggested this approach in treating people with facial disfigurement in a Lancet article in 2002. This suggestion caused considerable debate at the time concerning the ethics of this procedure.
An alternative to a face transplant is facial reconstruction, which typically involves moving the patient's own skin from their back, buttocks, thighs, or chest to their face in a series of as many as 50 operations to regain even limited functionality, and a face that is often likened to a mask or a living quilt.
L. Scott Levin, M.D., FACS, Chair, Department of Orthopaedic Surgery at University of Pennsylvania School of Medicine, has described the procedure as "the single most important area of reconstructive research".
Click on any of the following blue hyperlinks for further amplification:
Potential Cure for Cancer through Immunotherapy, including an Article by the Washington Post*
*- By Arthur Allen February 17, 2014
YouTube Video Immunotherapy & Chemo: What's the Difference? Trailer
YouTube & Picture: by Cancer Research Institute
Click here to read full article in the February 17, 2014 issue of the Washington Post.
The article begins:
"In the summer of 2012, a year after his wife had died of lung cancer, Michael Harris scraped open an old mole on his back and it would not stop bleeding. The doctors said he had stage 4 melanoma, with a virtually inoperable tumor, and that patients in his condition typically lived about eight months. By last June, the cancer had spread to his liver and lungs.
At that point Harris joined a clinical trial at Georgetown University, one of scores that have sprung up around the country to test a new class of cancer drugs called immune-checkpoint inhibitors. Two weeks after his first infusion, Harris’s primary tumor was fading, along with the black cancerous beads around it. A month later, his liver and lungs were clean.
“This stuff was like vanishing cream,” says Harris’s daughter, Rhonda Farrell. Today, Harris, a sun-leathered 66-year-old Vietnam veteran from Waldorf, Md., is back at work. And though his doctors won’t declare him cured, he says, “I feel like a normal person.”
Because it can be so inexorable and deadly, cancer tends to inspire hopes of miracle cures. Because of all the failed miracle cures, cancer doctors are a cautious lot. This makes it all the more astounding to hear cautious clinicians and scientists describe the treatments Harris and thousands of others are receiving.
“It’s a breakthrough,” says oncologist Michael Atkins, who recruited Harris to the trial at Georgetown’s Lombardi Cancer Center. “This is real,” adds Louis Weiner, the physician who leads the center. “We’re still in a bit of shock,” says Suzanne Topalian, a cancer immunologist at Johns Hopkins University who has been a key player in bringing the substances into clinical trials."
___________________________________________________________________________
Cancer immunotherapy is the use of the immune system to treat cancer.
Immunotherapies can be categorized as active, passive or hybrid (active and passive). These approaches exploit the fact that cancer cells often have molecules on their surface that can be detected by the immune system, known as tumour-associated antigens (TAAs); they are often proteins or other macromolecules (e.g. carbohydrates).
Active immunotherapy directs the immune system to attack tumor cells by targeting TAAs.
Passive immunotherapies enhance existing anti-tumor responses and include the use of monoclonal antibodies, lymphocytes and cytokines.
Among these, multiple antibody therapies are approved in various jurisdictions to treat a wide range of cancers. Antibodies are proteins produced by the immune system that bind to a target antigen on the cell surface. The immune system normally uses them to fight pathogens.
Each antibody is specific to one or a few proteins. Those that bind to tumor antigens treat cancer. Cell surface receptors are common targets for antibody therapies and include CD20, CD274 and CD279. Once bound to a cancer antigen, antibodies can induce antibody-dependent cell-mediated cytotoxicity, activate the complement system, or prevent a receptor from interacting with its ligand, all of which can lead to cell death.
Approved antibodies include:
Active cellular therapies usually involve the removal of immune cells from the blood or from a tumor. Those specific for the tumor are cultured and returned to the patient where they attack the tumor; alternatively, immune cells can be genetically engineered to express a tumor-specific receptor, cultured and returned to the patient. Cell types that can be used in this way are natural killer cells, lymphokine-activated killer cells, cytotoxic T cells and dendritic cells.
The only US-approved cell-based therapy is Dendreon's Provenge, for the treatment of prostate cancer.
Interleukin-2 and interferon-α are cytokines, proteins that regulate and coordinate the behaviour of the immune system. They have the ability to enhance anti-tumor activity and thus can be used as passive cancer treatments.
Interferon-α is used in the treatment of hairy-cell leukaemia, AIDS-related Kaposi's sarcoma, follicular lymphoma, chronic myeloid leukaemia and malignant melanoma. Interleukin-2 is used in the treatment of malignant melanoma and renal cell carcinoma.
Click on any of the following blue hyperlinks for more about Cancer immunotherapy:
The article begins:
"In the summer of 2012, a year after his wife had died of lung cancer, Michael Harris scraped open an old mole on his back and it would not stop bleeding. The doctors said he had stage 4 melanoma, with a virtually inoperable tumor, and that patients in his condition typically lived about eight months. By last June, the cancer had spread to his liver and lungs.
At that point Harris joined a clinical trial at Georgetown University, one of scores that have sprung up around the country to test a new class of cancer drugs called immune-checkpoint inhibitors. Two weeks after his first infusion, Harris’s primary tumor was fading, along with the black cancerous beads around it. A month later, his liver and lungs were clean.
“This stuff was like vanishing cream,” says Harris’s daughter, Rhonda Farrell. Today, Harris, a sun-leathered 66-year-old Vietnam veteran from Waldorf, Md., is back at work. And though his doctors won’t declare him cured, he says, “I feel like a normal person.”
Because it can be so inexorable and deadly, cancer tends to inspire hopes of miracle cures. Because of all the failed miracle cures, cancer doctors are a cautious lot. This makes it all the more astounding to hear cautious clinicians and scientists describe the treatments Harris and thousands of others are receiving.
“It’s a breakthrough,” says oncologist Michael Atkins, who recruited Harris to the trial at Georgetown’s Lombardi Cancer Center. “This is real,” adds Louis Weiner, the physician who leads the center. “We’re still in a bit of shock,” says Suzanne Topalian, a cancer immunologist at Johns Hopkins University who has been a key player in bringing the substances into clinical trials."
___________________________________________________________________________
Cancer immunotherapy is the use of the immune system to treat cancer.
Immunotherapies can be categorized as active, passive or hybrid (active and passive). These approaches exploit the fact that cancer cells often have molecules on their surface that can be detected by the immune system, known as tumour-associated antigens (TAAs); they are often proteins or other macromolecules (e.g. carbohydrates).
Active immunotherapy directs the immune system to attack tumor cells by targeting TAAs.
Passive immunotherapies enhance existing anti-tumor responses and include the use of monoclonal antibodies, lymphocytes and cytokines.
Among these, multiple antibody therapies are approved in various jurisdictions to treat a wide range of cancers. Antibodies are proteins produced by the immune system that bind to a target antigen on the cell surface. The immune system normally uses them to fight pathogens.
Each antibody is specific to one or a few proteins. Those that bind to tumor antigens treat cancer. Cell surface receptors are common targets for antibody therapies and include CD20, CD274 and CD279. Once bound to a cancer antigen, antibodies can induce antibody-dependent cell-mediated cytotoxicity, activate the complement system, or prevent a receptor from interacting with its ligand, all of which can lead to cell death.
Approved antibodies include:
Active cellular therapies usually involve the removal of immune cells from the blood or from a tumor. Those specific for the tumor are cultured and returned to the patient where they attack the tumor; alternatively, immune cells can be genetically engineered to express a tumor-specific receptor, cultured and returned to the patient. Cell types that can be used in this way are natural killer cells, lymphokine-activated killer cells, cytotoxic T cells and dendritic cells.
The only US-approved cell-based therapy is Dendreon's Provenge, for the treatment of prostate cancer.
Interleukin-2 and interferon-α are cytokines, proteins that regulate and coordinate the behaviour of the immune system. They have the ability to enhance anti-tumor activity and thus can be used as passive cancer treatments.
Interferon-α is used in the treatment of hairy-cell leukaemia, AIDS-related Kaposi's sarcoma, follicular lymphoma, chronic myeloid leukaemia and malignant melanoma. Interleukin-2 is used in the treatment of malignant melanoma and renal cell carcinoma.
Click on any of the following blue hyperlinks for more about Cancer immunotherapy:
Milestones in Medical Technology
(Reported in New York Times October 5, 2012)
YouTube Video: Robotic Surgery Demonstration Using Da Vinci Surgical System
Pictured: Fetal Ultrasound: Dr. Edward Hon of Yale reported using a Doppler monitor on a woman's abdomen to detect fetal heartbeat. Ultrasound's principles had been known for more than a century (a Swedish physicist, Christian Andreas Doppler, gave his name to the phenomenon in 1842), but this was its first use in prenatal care.
From eyeglasses to the stethoscope to imaging the brain at work, a long list of inventions and innovations have changed medicine.
Medical breakthroughs since 1950 are excerpted below:
1950:
Intraocular Lens
Dr. Harold Ridley, a British ophthalmologist, implanted the first permanently placed intraocular lens to correct cataract.
1952:
Mechanical Heart
Henry Opitek, 41, was operated on using an artificial heart, the Dodrill GMR heart machine, manufactured by General Motors and generally considered the first mechanical heart. The surgeon, Dr. Forest Dewey Dodrill, successfully repaired the patient's mitral valve, and Mr. Opitek lived until 1981.
Magnetic Resonance
The Nobel Prize in Physics was awarded to Felix Bloch and Edward Mills Purcell for their work in developing nuclear magnetic resonance, the principle behind M.R.I. machines.
1953:
Heart-Lung Bypass
Dr. John Heysham Gibbon used his new invention, the heart-lung bypass machine, for the first time in open-heart surgery, completely supporting a patient's heart and lung functions for about half the time of the surgery. It was the culmination of his decades of work in developing the machine.
Cochlear Prosthesis
Dr. André Djourno of France developed a cochlear prosthesis, a method of stimulating the cochlear nerve in deaf people. It was the beginning of the long road to the development of effective cochlear implants. In 1957, he performed the first cochlear implantation. He believed that medical devices should remain in the public domain and refused to patent his invention.
1954:
Kidney Transplant
In the first successful kidney transplant, after at least nine failures, a team of surgeons at Peter Bent Brigham Hospital in Boston transplanted a kidney from a 24-year-old man to his twin brother. The recipient lived 11 years more, and in 1990 the lead surgeon, Dr. Joseph E. Murray, won the Nobel Prize in Medicine or Physiology.
1958:
Pacemaker
Dr. Seymour Furman, a cardiologist at Montefiore Hospital in the Bronx, succeeded in extending a patient's life by more than two months using a cardiac pacemaker, a large machine to which the patient was attached by a 50-foot extension cord. By the next year, portable versions of the machine were in use.
Fetal Ultrasound
Dr. Edward Hon of Yale reported using a Doppler monitor on a woman's abdomen to detect fetal heartbeat. Ultrasound's principles had been known for more than a century (a Swedish physicist, Christian Andreas Doppler, gave his name to the phenomenon in 1842), but this was its first use in prenatal care.
1961:
Minimally Invasive Surgery
Dr. Thomas J. Fogarty came up with the idea for the balloon embolectomy catheter for removing blood clots, and used it on a patient six weeks later. It was the first minimally invasive surgery technique.
1963:
Artificial Heart
Paul Winchell, the ventriloquist and inventor, patented the first artificial heart, developed in collaboration with Dr. Henry J. Heimlich, later famous for the Heimlich maneuver.
Liver Transplant
The first human liver transplant was performed by Dr. Thomas E. Starzl. The patient, a 3-year-old child, rapidly bled to death.
1965:
Portable Defibrillator
Dr. Frank Pantridge installed the first portable defibrillator in an ambulance in Belfast, Northern Ireland. It weighed 150 pounds and was powered by car batteries.
Commercial Ultrasound
Walter Erich Krause of the Siemens Corporation filed a patent for the first practical commercial ultrasound machine. According to the patent, his machine could be "used for practical ultra-sonic-optical examination to achieve a lifelike reproduction of the body part under examination."
1967:
Heart Transplant
Dr. Christiaan Barnard, a South African, performed the first human heart transplant. The patient, a 53-year-old man, died 18 days later.
1971:
CT Scanner
The first commercial CT scanner, developed by Dr. Godfrey Hounsfield, was used on a patient in London. Dr. Hounsfield shared the 1979 Nobel Prize in Physiology or Medicine for his invention.
1973:
Insulin Pump
An inventor and entrepreneur, Dean L. Kamen, patented the first insulin pump. He became perhaps even better known for a later invention, the Segway transporter.
1978:
M.R.I.
Dr. Raymond V. Damadian announced that he had patented a technique using nuclear magnetic resonance to distinguish between normal and cancerous tissue. In 2003, two other researchers won a Nobel Prize for further discoveries.
1992:
DNA Sequencing
Dr. Leroy E. Hood patents his invention of the automated DNA sequencing technique. The patent is owned by the California Institute of Technology.
Imaging Thought
A paper in the journal Magnetic Resonance Medicine by a group of researchers at the Medical College of Wisconsin announced the first use of functional magnetic resonance imaging to detect brain blood flow in conjunction with a human mental activity.
2000:
Human Genome
The first draft of the human genome was announced. Three years later, it was declared complete three years later.
2004:
Adaptive Artificial Knee
The Rheo knee, a plastic prosthetic joint that adapts to a user's walking style and changes in terrain, was produced by the Ossur Corporation.
2006:
Artificial Liver
Dr. Colin McGucklin and Dr. Nico Forraz of Newcastle University developed a liver grown from stem cells. The size of a small coin, it was not an organ that could be implanted in a human.
Medical breakthroughs since 1950 are excerpted below:
1950:
Intraocular Lens
Dr. Harold Ridley, a British ophthalmologist, implanted the first permanently placed intraocular lens to correct cataract.
1952:
Mechanical Heart
Henry Opitek, 41, was operated on using an artificial heart, the Dodrill GMR heart machine, manufactured by General Motors and generally considered the first mechanical heart. The surgeon, Dr. Forest Dewey Dodrill, successfully repaired the patient's mitral valve, and Mr. Opitek lived until 1981.
Magnetic Resonance
The Nobel Prize in Physics was awarded to Felix Bloch and Edward Mills Purcell for their work in developing nuclear magnetic resonance, the principle behind M.R.I. machines.
1953:
Heart-Lung Bypass
Dr. John Heysham Gibbon used his new invention, the heart-lung bypass machine, for the first time in open-heart surgery, completely supporting a patient's heart and lung functions for about half the time of the surgery. It was the culmination of his decades of work in developing the machine.
Cochlear Prosthesis
Dr. André Djourno of France developed a cochlear prosthesis, a method of stimulating the cochlear nerve in deaf people. It was the beginning of the long road to the development of effective cochlear implants. In 1957, he performed the first cochlear implantation. He believed that medical devices should remain in the public domain and refused to patent his invention.
1954:
Kidney Transplant
In the first successful kidney transplant, after at least nine failures, a team of surgeons at Peter Bent Brigham Hospital in Boston transplanted a kidney from a 24-year-old man to his twin brother. The recipient lived 11 years more, and in 1990 the lead surgeon, Dr. Joseph E. Murray, won the Nobel Prize in Medicine or Physiology.
1958:
Pacemaker
Dr. Seymour Furman, a cardiologist at Montefiore Hospital in the Bronx, succeeded in extending a patient's life by more than two months using a cardiac pacemaker, a large machine to which the patient was attached by a 50-foot extension cord. By the next year, portable versions of the machine were in use.
Fetal Ultrasound
Dr. Edward Hon of Yale reported using a Doppler monitor on a woman's abdomen to detect fetal heartbeat. Ultrasound's principles had been known for more than a century (a Swedish physicist, Christian Andreas Doppler, gave his name to the phenomenon in 1842), but this was its first use in prenatal care.
1961:
Minimally Invasive Surgery
Dr. Thomas J. Fogarty came up with the idea for the balloon embolectomy catheter for removing blood clots, and used it on a patient six weeks later. It was the first minimally invasive surgery technique.
1963:
Artificial Heart
Paul Winchell, the ventriloquist and inventor, patented the first artificial heart, developed in collaboration with Dr. Henry J. Heimlich, later famous for the Heimlich maneuver.
Liver Transplant
The first human liver transplant was performed by Dr. Thomas E. Starzl. The patient, a 3-year-old child, rapidly bled to death.
1965:
Portable Defibrillator
Dr. Frank Pantridge installed the first portable defibrillator in an ambulance in Belfast, Northern Ireland. It weighed 150 pounds and was powered by car batteries.
Commercial Ultrasound
Walter Erich Krause of the Siemens Corporation filed a patent for the first practical commercial ultrasound machine. According to the patent, his machine could be "used for practical ultra-sonic-optical examination to achieve a lifelike reproduction of the body part under examination."
1967:
Heart Transplant
Dr. Christiaan Barnard, a South African, performed the first human heart transplant. The patient, a 53-year-old man, died 18 days later.
1971:
CT Scanner
The first commercial CT scanner, developed by Dr. Godfrey Hounsfield, was used on a patient in London. Dr. Hounsfield shared the 1979 Nobel Prize in Physiology or Medicine for his invention.
1973:
Insulin Pump
An inventor and entrepreneur, Dean L. Kamen, patented the first insulin pump. He became perhaps even better known for a later invention, the Segway transporter.
1978:
M.R.I.
Dr. Raymond V. Damadian announced that he had patented a technique using nuclear magnetic resonance to distinguish between normal and cancerous tissue. In 2003, two other researchers won a Nobel Prize for further discoveries.
1992:
DNA Sequencing
Dr. Leroy E. Hood patents his invention of the automated DNA sequencing technique. The patent is owned by the California Institute of Technology.
Imaging Thought
A paper in the journal Magnetic Resonance Medicine by a group of researchers at the Medical College of Wisconsin announced the first use of functional magnetic resonance imaging to detect brain blood flow in conjunction with a human mental activity.
2000:
Human Genome
The first draft of the human genome was announced. Three years later, it was declared complete three years later.
2004:
Adaptive Artificial Knee
The Rheo knee, a plastic prosthetic joint that adapts to a user's walking style and changes in terrain, was produced by the Ossur Corporation.
2006:
Artificial Liver
Dr. Colin McGucklin and Dr. Nico Forraz of Newcastle University developed a liver grown from stem cells. The size of a small coin, it was not an organ that could be implanted in a human.
Timeline of medicine and medical technology
YouTube Video of The Electric Eye: A Visual Prosthesis*
* -- Science for the Public, October 26, 2010. Shawn Kelly, Senior Systems Scientist, Institute for Complex Engineered Systems, Carnegie Mellon University: The complexity of the eye makes restoration of vision a formidable challenge. Dr. Shawn Kelly explains how the eye "sees," how blindness affects the retinal cells, and the difficulty of restoring even partial vision. He shows the development and testing of the visual prosthesis developed by the Boston Retinal Implant Project. This project, which involves teams from multiple institutions, is an outstanding example of the great achievements of science and engineering.
Pictured: This Day in Science June 26, 2000 – First DNA sequence released by human genome project
The history of medicine, as practiced by trained professionals, shows how societies have changed in their approach to illness and disease from ancient times to the present.
Early medical traditions include those of Babylon, China, Egypt and India. The Greeks went even further, introducing the concepts of medical diagnosis, prognosis, and advanced medical ethics.
The Hippocratic Oath, still taken (although significantly changed from the original) by doctors up to today, was written in Greece in the 5th century BCE. In the medieval age, surgical practices inherited from the ancient masters were improved and then systematized in Rogerius's The Practice of Surgery. Universities began systematic training of physicians around the years 1220 in Italy. During the Renaissance, understanding of anatomy improved, and the microscope was invented.
The germ theory of disease in the 19th century led to cures for many infectious diseases. Military doctors advanced the methods of trauma treatment and surgery. Public health measures were developed especially in the 19th century as the rapid growth of cities required systematic sanitary measures. Advanced research centers opened in the early 20th century, often connected with major hospitals.
The mid-20th century was characterized by new biological treatments, such as antibiotics. These advancements, along with developments in chemistry, genetics, and lab technology (such as the x-ray) led to modern medicine. Medicine was heavily professionalized in the 20th century, and new careers opened to women as nurses (from the 1870s) and as physicians (especially after 1970). The 21st century is characterized by highly advanced research involving numerous fields of science.
Health technology is defined by the World Health Organization as the "application of organized knowledge and skills in the form of devices, medicines, vaccines, procedures and systems developed to solve a health problem and improve quality of lives." This includes the pharmaceuticals, devices, procedures and organizational systems used in health care.
Click on the following blue hyperlinks for a listing of the timeline for medicine and medical technology:
Early medical traditions include those of Babylon, China, Egypt and India. The Greeks went even further, introducing the concepts of medical diagnosis, prognosis, and advanced medical ethics.
The Hippocratic Oath, still taken (although significantly changed from the original) by doctors up to today, was written in Greece in the 5th century BCE. In the medieval age, surgical practices inherited from the ancient masters were improved and then systematized in Rogerius's The Practice of Surgery. Universities began systematic training of physicians around the years 1220 in Italy. During the Renaissance, understanding of anatomy improved, and the microscope was invented.
The germ theory of disease in the 19th century led to cures for many infectious diseases. Military doctors advanced the methods of trauma treatment and surgery. Public health measures were developed especially in the 19th century as the rapid growth of cities required systematic sanitary measures. Advanced research centers opened in the early 20th century, often connected with major hospitals.
The mid-20th century was characterized by new biological treatments, such as antibiotics. These advancements, along with developments in chemistry, genetics, and lab technology (such as the x-ray) led to modern medicine. Medicine was heavily professionalized in the 20th century, and new careers opened to women as nurses (from the 1870s) and as physicians (especially after 1970). The 21st century is characterized by highly advanced research involving numerous fields of science.
Health technology is defined by the World Health Organization as the "application of organized knowledge and skills in the form of devices, medicines, vaccines, procedures and systems developed to solve a health problem and improve quality of lives." This includes the pharmaceuticals, devices, procedures and organizational systems used in health care.
Click on the following blue hyperlinks for a listing of the timeline for medicine and medical technology:
Stem Cell Therapy
YouTube Video: Another Promising Application for Stem Cells: Crohn’s Complications - Mayo Clinic
YouTube Video: Bone Marrow Transplant-Mayo Clinic
Pictured: Different applications for Stem Cell Therapy
Stem-cell therapy is the use of stem cells to treat or prevent a disease or condition.
Bone marrow transplant is the most widely used stem-cell therapy, but some therapies derived from umbilical cord blood are also in use. Research is underway to develop various sources for stem cells, and to apply stem-cell treatments for neurodegenerative diseases and conditions such as diabetes, heart disease, and other conditions.
Stem-cell therapy has become controversial following developments such as the ability of scientists to isolate and culture embryonic stem cells, to create stem cells using somatic cell nuclear transfer and their use of techniques to create induced pluripotent stem cells. This controversy is often related to abortion politics and to human cloning. Additionally, efforts to market treatments based on transplant of stored umbilical cord blood have been controversial.
Medical Uses:
For over 30 years, bone marrow has been used to treat cancer patients with conditions such as leukaemia and lymphoma; this is the only form of stem-cell therapy that is widely practiced.
During chemotherapy, most growing cells are killed by the cytotoxic agents. These agents, however, cannot discriminate between the leukaemia or neoplastic cells, and the hematopoietic stem cells within the bone marrow. It is this side effect of conventional chemotherapy strategies that the stem-cell transplant attempts to reverse; a donor's healthy bone marrow reintroduces functional stem cells to replace the cells lost in the host's body during treatment.
The transplanted cells also generate an immune response that helps to kill off the cancer cells; this process can go too far, however, leading to graft vs host disease, the most serious side effect of this treatment.
Another stem-cell therapy called Prochymal, was conditionally approved in Canada in 2012 for the management of acute graft-vs-host disease in children who are unresponsive to steroids. It is an allogenic stem therapy based on mesenchymal stem cells (MSCs) derived from the bone marrow of adult donors. MSCs are purified from the marrow, cultured and packaged, with up to 10,000 doses derived from a single donor. The doses are stored frozen until needed.
The FDA has approved five hematopoietic stem-cell products derived from umbilical cord blood, for the treatment of blood and immunological diseases.
In 2014, the European Medicines Agency recommended approval of Holoclar, a treatment involving stem cells, for use in the European Union. Holoclar is used for people with severe limbal stem cell deficiency due to burns in the eye.
Click on any of the following blue hyperlinks for more about Stem Cell Therapy:
Bone marrow transplant is the most widely used stem-cell therapy, but some therapies derived from umbilical cord blood are also in use. Research is underway to develop various sources for stem cells, and to apply stem-cell treatments for neurodegenerative diseases and conditions such as diabetes, heart disease, and other conditions.
Stem-cell therapy has become controversial following developments such as the ability of scientists to isolate and culture embryonic stem cells, to create stem cells using somatic cell nuclear transfer and their use of techniques to create induced pluripotent stem cells. This controversy is often related to abortion politics and to human cloning. Additionally, efforts to market treatments based on transplant of stored umbilical cord blood have been controversial.
Medical Uses:
For over 30 years, bone marrow has been used to treat cancer patients with conditions such as leukaemia and lymphoma; this is the only form of stem-cell therapy that is widely practiced.
During chemotherapy, most growing cells are killed by the cytotoxic agents. These agents, however, cannot discriminate between the leukaemia or neoplastic cells, and the hematopoietic stem cells within the bone marrow. It is this side effect of conventional chemotherapy strategies that the stem-cell transplant attempts to reverse; a donor's healthy bone marrow reintroduces functional stem cells to replace the cells lost in the host's body during treatment.
The transplanted cells also generate an immune response that helps to kill off the cancer cells; this process can go too far, however, leading to graft vs host disease, the most serious side effect of this treatment.
Another stem-cell therapy called Prochymal, was conditionally approved in Canada in 2012 for the management of acute graft-vs-host disease in children who are unresponsive to steroids. It is an allogenic stem therapy based on mesenchymal stem cells (MSCs) derived from the bone marrow of adult donors. MSCs are purified from the marrow, cultured and packaged, with up to 10,000 doses derived from a single donor. The doses are stored frozen until needed.
The FDA has approved five hematopoietic stem-cell products derived from umbilical cord blood, for the treatment of blood and immunological diseases.
In 2014, the European Medicines Agency recommended approval of Holoclar, a treatment involving stem cells, for use in the European Union. Holoclar is used for people with severe limbal stem cell deficiency due to burns in the eye.
Click on any of the following blue hyperlinks for more about Stem Cell Therapy:
Robotic-assisted Surgery, including a List of Categories
YouTube Video: Robot-Assisted Surgery: Autonomous Tumor Localization and Extraction
YouTube Video: da Vinci Robot-Assisted Surgery
Pictured: TOP: Robotic Cardiac Surgery; BOTTOM: Robotic Knee Replacement Surgery
Robotic surgery, computer-assisted surgery, and robotic-assisted surgery are terms for technological developments that use robotic systems to aid in surgical procedures. Robotically-assisted surgery was developed to overcome the limitations of pre-existing minimally-invasive surgical procedures and to enhance the capabilities of surgeons performing open surgery.
In the case of robotically-assisted minimally-invasive surgery, instead of directly moving the instruments, the surgeon uses one of two methods to control the instruments; either a direct telemanipulator or through computer control. A telemanipulator is a remote manipulator that allows the surgeon to perform the normal movements associated with the surgery while the robotic arms carry out those movements using end-effectors and manipulators to perform the actual surgery on the patient.
In computer-controlled systems the surgeon uses a computer to control the robotic arms and its end-effectors, though these systems can also still use telemanipulators for their input. One advantage of using the computerised method is that the surgeon does not have to be present, but can be anywhere in the world, leading to the possibility for remote surgery.
In the case of enhanced open surgery, autonomous instruments (in familiar configurations) replace traditional steel tools, performing certain actions (such as rib spreading) with much smoother, feedback-controlled motions than could be achieved by a human hand.
The main object of such smart instruments is to reduce or eliminate the tissue trauma traditionally associated with open surgery without requiring more than a few minutes' training on the part of surgeons. This approach seeks to improve open surgeries, particularly cardio-thoracic, that have so far not benefited from minimally-invasive techniques.
Robotic surgery has been criticized for its expense, by one estimate costing $1,500 to $2000 more per patient.
Click on any of the following blue hyperlinks for more about Robotic-assisted Surgery:
In the case of robotically-assisted minimally-invasive surgery, instead of directly moving the instruments, the surgeon uses one of two methods to control the instruments; either a direct telemanipulator or through computer control. A telemanipulator is a remote manipulator that allows the surgeon to perform the normal movements associated with the surgery while the robotic arms carry out those movements using end-effectors and manipulators to perform the actual surgery on the patient.
In computer-controlled systems the surgeon uses a computer to control the robotic arms and its end-effectors, though these systems can also still use telemanipulators for their input. One advantage of using the computerised method is that the surgeon does not have to be present, but can be anywhere in the world, leading to the possibility for remote surgery.
In the case of enhanced open surgery, autonomous instruments (in familiar configurations) replace traditional steel tools, performing certain actions (such as rib spreading) with much smoother, feedback-controlled motions than could be achieved by a human hand.
The main object of such smart instruments is to reduce or eliminate the tissue trauma traditionally associated with open surgery without requiring more than a few minutes' training on the part of surgeons. This approach seeks to improve open surgeries, particularly cardio-thoracic, that have so far not benefited from minimally-invasive techniques.
Robotic surgery has been criticized for its expense, by one estimate costing $1,500 to $2000 more per patient.
Click on any of the following blue hyperlinks for more about Robotic-assisted Surgery:
"Scientists Develop Blood Test That Spots Tumor-Derived DNA in People With Early-Stage Cancers"
(By John Hopkins University, (8/16/2017)
YouTube Video: The Future of Personalized Cancer Medicine (John Hopkins University)
The article follows:
In a bid to detect cancers early and in a noninvasive way, scientists at the Johns Hopkins Kimmel Cancer Center report they have developed a test that spots tiny amounts of cancer-specific DNA in blood and have used it to accurately identify more than half of 138 people with relatively early-stage colorectal, breast, lung and ovarian cancers. The test, the scientists say, is novel in that it can distinguish between DNA shed from tumors and other altered DNA that can be mistaken for cancer biomarkers.
A report on the research, performed on blood and tumor tissue samples from 200 people with all stages of cancer in the U.S., Denmark and the Netherlands, appears in the Aug. 16 issue of Science Translational Medicine.
“This study shows that identifying cancer early using DNA changes in the blood is feasible and that our high accuracy sequencing method is a promising approach to achieve this goal,” says Victor Velculescu, M.D., Ph.D., professor of oncology at the Johns Hopkins Kimmel Cancer Center.
Blood tests for cancer are a growing part of clinical oncology, but they remain in the early stages of development. To find small bits of cancer-derived DNA in the blood of cancer patients, scientists have frequently relied on DNA alterations found in patients’ biopsied tumor samples as guideposts for the genetic mistakes they should be looking for among the masses of DNA circulating in those patients’ blood samples.
To develop a cancer screening test that could be used to screen seemingly healthy people, scientists had to find novel ways to spot DNA alterations that could be lurking in a person’s blood but had not been previously identified.
“The challenge was to develop a blood test that could predict the probable presence of cancer without knowing the genetic mutations present in a person’s tumor,” says Velculescu.
The goal, adds Jillian Phallen, a graduate student at the Johns Hopkins Kimmel Cancer Center who was involved in the research, was to develop a screening test that is highly specific for cancer and accurate enough to detect the cancer when present, while reducing the risk of “false positive” results that often lead to unnecessary overtesting and overtreatments.
The task is notably complicated, says Phallen, by the need to sort between true cancer-derived mutations and genetic alterations that occur in blood cells and as part of normal, inherited variations in DNA.
As blood cells divide, for example, Velculescu says there is a chance these cells will acquire mistakes or mutations. In a small fraction of people, these changes will spur a blood cell to multiply faster than its neighboring cells, potentially leading to pre-leukemic conditions.
However, most of the time, the blood-derived mutations are not cancer-initiating.
His team also ruled out so-called “germline” mutations. While germline mutations are indeed alterations in DNA, they occur as a result of normal variations between individuals, and are not usually linked to particular cancers.
To develop the new test, Velculescu, Phallen and their colleagues obtained blood samples from 200 patients with breast, lung, ovarian and colorectal cancer. The scientists’ blood test screened the patients’ blood samples for mutations within 58 genes widely linked to various cancers.
Overall, the scientists were able to detect 86 of 138 (62 percent) stage I and II cancers. More specifically, among 42 people with colorectal cancer, the test correctly predicted cancer in half of the eight patients with stage I disease, eight of nine (89 percent) with stage II disease, nine of 10 (90 percent) with stage III and 14 of 15 (93 percent) with stage IV disease.
Of 71 people with lung cancer, the scientists’ test identified cancer among:
For 42 patients with ovarian cancer,
Among 45 breast cancer patients, the test spotted cancer-derived mutations in two of three (67 percent) patients with stage I disease, 17 of 29 (59 percent) with stage II disease and six of 13 (46 percent) with stage III cancers.
They found none of the cancer-derived mutations among blood samples of 44 healthy individuals.
Despite these initial promising results for early detection, the blood test needs to be validated in studies of much larger numbers of people, say the scientists.
Velculescu and his team also performed independent genomic sequencing on available tumors removed from 100 of the 200 patients with cancer and found that 82 (82 percent) had mutations in their tumors that correlated with the genetic alterations found in the blood.
The Johns Hopkins-developed blood test uses a type of genomic sequencing the researchers call “targeted error correction sequencing.” The sequencing method is based on deep sequencing, which reads each chemical code in DNA 30,000 times. “We’re trying to find the needle in the haystack, so when we do find a DNA alteration, we want to make sure it is what we think it is,” says Velculescu.
Such deep sequencing, covering more than 80,000 base pairs of DNA, has the potential to be very costly, but Velculescu says sequencing technology is becoming cheaper, and his research team may eventually be able to reduce the number of DNA locations they screen while preserving the test’s accuracy.
He says the populations that could benefit most from such a DNA-based blood test include those at high risk for cancer including smokers — for whom standard computed tomography scans for identifying lung cancer often lead to false positives — and women with hereditary mutations for breast and ovarian cancer within BRCA1 and BRCA2 genes.
Scientists who contributed to the research include:
Funding for the study was provided by:
Phallen, Sausen, Diaz and Velculescu are inventors on patent applications related to this research. Velculescu, a founder of Personal Genome Diagnostics and a member of its scientific advisory board and board of directors, owns Personal Genome Diagnostics stock, which is subject to certain restrictions under university policy.
Velculescu is also on the scientific advisory board for Ignyta. The terms of these arrangements are managed by The Johns Hopkins University in accordance with its conflict of interest policies.
Useful Links
Show me more...
In a bid to detect cancers early and in a noninvasive way, scientists at the Johns Hopkins Kimmel Cancer Center report they have developed a test that spots tiny amounts of cancer-specific DNA in blood and have used it to accurately identify more than half of 138 people with relatively early-stage colorectal, breast, lung and ovarian cancers. The test, the scientists say, is novel in that it can distinguish between DNA shed from tumors and other altered DNA that can be mistaken for cancer biomarkers.
A report on the research, performed on blood and tumor tissue samples from 200 people with all stages of cancer in the U.S., Denmark and the Netherlands, appears in the Aug. 16 issue of Science Translational Medicine.
“This study shows that identifying cancer early using DNA changes in the blood is feasible and that our high accuracy sequencing method is a promising approach to achieve this goal,” says Victor Velculescu, M.D., Ph.D., professor of oncology at the Johns Hopkins Kimmel Cancer Center.
Blood tests for cancer are a growing part of clinical oncology, but they remain in the early stages of development. To find small bits of cancer-derived DNA in the blood of cancer patients, scientists have frequently relied on DNA alterations found in patients’ biopsied tumor samples as guideposts for the genetic mistakes they should be looking for among the masses of DNA circulating in those patients’ blood samples.
To develop a cancer screening test that could be used to screen seemingly healthy people, scientists had to find novel ways to spot DNA alterations that could be lurking in a person’s blood but had not been previously identified.
“The challenge was to develop a blood test that could predict the probable presence of cancer without knowing the genetic mutations present in a person’s tumor,” says Velculescu.
The goal, adds Jillian Phallen, a graduate student at the Johns Hopkins Kimmel Cancer Center who was involved in the research, was to develop a screening test that is highly specific for cancer and accurate enough to detect the cancer when present, while reducing the risk of “false positive” results that often lead to unnecessary overtesting and overtreatments.
The task is notably complicated, says Phallen, by the need to sort between true cancer-derived mutations and genetic alterations that occur in blood cells and as part of normal, inherited variations in DNA.
As blood cells divide, for example, Velculescu says there is a chance these cells will acquire mistakes or mutations. In a small fraction of people, these changes will spur a blood cell to multiply faster than its neighboring cells, potentially leading to pre-leukemic conditions.
However, most of the time, the blood-derived mutations are not cancer-initiating.
His team also ruled out so-called “germline” mutations. While germline mutations are indeed alterations in DNA, they occur as a result of normal variations between individuals, and are not usually linked to particular cancers.
To develop the new test, Velculescu, Phallen and their colleagues obtained blood samples from 200 patients with breast, lung, ovarian and colorectal cancer. The scientists’ blood test screened the patients’ blood samples for mutations within 58 genes widely linked to various cancers.
Overall, the scientists were able to detect 86 of 138 (62 percent) stage I and II cancers. More specifically, among 42 people with colorectal cancer, the test correctly predicted cancer in half of the eight patients with stage I disease, eight of nine (89 percent) with stage II disease, nine of 10 (90 percent) with stage III and 14 of 15 (93 percent) with stage IV disease.
Of 71 people with lung cancer, the scientists’ test identified cancer among:
- 13 of 29 (45 percent) with stage I disease,
- 23 of 32 (72 percent) with stage II disease,
- three of four (75 percent) with stage III disease
- and five of six (83 percent) with stage IV cancer.
For 42 patients with ovarian cancer,
- 16 of 24 (67 percent) with stage I disease were correctly identified,
- as well as three of four (75 percent) with stage II disease,
- six of eight (75 percent) with stage III cancer
- and five of six (83 percent) with stage IV disease.
Among 45 breast cancer patients, the test spotted cancer-derived mutations in two of three (67 percent) patients with stage I disease, 17 of 29 (59 percent) with stage II disease and six of 13 (46 percent) with stage III cancers.
They found none of the cancer-derived mutations among blood samples of 44 healthy individuals.
Despite these initial promising results for early detection, the blood test needs to be validated in studies of much larger numbers of people, say the scientists.
Velculescu and his team also performed independent genomic sequencing on available tumors removed from 100 of the 200 patients with cancer and found that 82 (82 percent) had mutations in their tumors that correlated with the genetic alterations found in the blood.
The Johns Hopkins-developed blood test uses a type of genomic sequencing the researchers call “targeted error correction sequencing.” The sequencing method is based on deep sequencing, which reads each chemical code in DNA 30,000 times. “We’re trying to find the needle in the haystack, so when we do find a DNA alteration, we want to make sure it is what we think it is,” says Velculescu.
Such deep sequencing, covering more than 80,000 base pairs of DNA, has the potential to be very costly, but Velculescu says sequencing technology is becoming cheaper, and his research team may eventually be able to reduce the number of DNA locations they screen while preserving the test’s accuracy.
He says the populations that could benefit most from such a DNA-based blood test include those at high risk for cancer including smokers — for whom standard computed tomography scans for identifying lung cancer often lead to false positives — and women with hereditary mutations for breast and ovarian cancer within BRCA1 and BRCA2 genes.
Scientists who contributed to the research include:
- Mark Sausen, Derek Murphy, Sonya Parpart-Li, David Riley, Monica Nesselbush, Naomi Sengamalay, Andrew Georgiadis, Siân Jones and Sam Angiuoli from Personal Genome Diagnostics;
- Vilmos Adleff, Alessandro Leal, Carolyn Hruban, James White, Valsamo Anagnostou, Jacob Fiksel, Stephen Cristiano, Eniko Papp, Savannah Speir Qing Kay Li, Robert B Scharpf and Luis A. Diaz Jr. from Johns Hopkins;
- Thomas Reinert, Mai-Britt Worm Orntoft, Frank Viborg Mortensen, Torben Ørntoft and Claus Lindbjerg Andersen from Aarhus University Hospital, Denmark; Brian D Woodward and Hatim Husain from the University of California, San Diego;
- Mogens Rørbæk Madsen from the Herning Regional Hospital, Denmark;
- Joost Huiskens and Cornelis Punt from the University of Amsterdam, The Netherlands;
- Nicole van Grieken from the VU University Medical Center, The Netherlands;
- Remond Fijneman and Gerrit Meijer from The Netherlands Cancer Institute and Hans Jørgen Nielsen from Hvidovre Hospital, Denmark.
Funding for the study was provided by:
- the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation;
- the Stand Up to Cancer-Dutch Cancer Society International Translational Cancer Research Dream Team Grant;
- the Commonwealth Foundation;
- the Cigarette Restitution Fund Program;
- the Burroughs Wellcome Fund;
- the Maryland-Genetics, Epidemiology and Medicine Training Program;
- the International Association for the Study of Lung Cancer/Prevent Cancer Foundation;
- the National Institutes of Health’s National Cancer Institute (grants CA121113, CA006973 and CA180950); the Danish Council for Independent Research;
- the Danish Council for Strategic Research; the Novo Nordisk Foundation; and the Danish Cancer Society.
Phallen, Sausen, Diaz and Velculescu are inventors on patent applications related to this research. Velculescu, a founder of Personal Genome Diagnostics and a member of its scientific advisory board and board of directors, owns Personal Genome Diagnostics stock, which is subject to certain restrictions under university policy.
Velculescu is also on the scientific advisory board for Ignyta. The terms of these arrangements are managed by The Johns Hopkins University in accordance with its conflict of interest policies.
Useful Links
- Contact JHM Media Team
- Find a Doctor
- Search Contacts by Beat
- Subscribe to RSS Feeds
- Sign-Up for E-Newsletters
Show me more...
"FDA Approves First-of-Its-Kind Cancer Treatment" (by WebMD)
(FDA: Food and Drug Administration)
YouTube Video: How Car T-Cell Therapy Works
By WebMD August 30, 2017 -- The FDA has for the first time approved a treatment that uses a patient’s own genetically modified cells to attack a type of leukemia, opening the door to what the agency calls "a new frontier" in medicine.
The approval Wednesday allows a process known as CAR T-cell therapy to be used in children or young adults fighting an often fatal recurrence of the most common childhood cancer -- B-cell acute lymphoblastic leukemia.
And it clears the way for a new approach to fighting cancer by harnessing the body’s immune system -- a long-sought goal of medical researchers.
“This is a dream come true,” says Henry Fung, MD, director of the Fox Chase Cancer Center-Temple University Hospital Bone Marrow Transplant Program. “It’s now limited to one disease in children only, but that platform potentially can benefit a lot of different types of cancer patients, particularly blood cancer patients.”
'A New Frontier'
FDA Commissioner Scott Gottlieb, MD, called the approval of the therapy -- brand named Kymriah -- a "new frontier in medical innovation."
In a news conference on Wednesday, Gottlieb said the FDA had 76 active investigational new drug applications related to CAR T-cell products, and more than 500 for gene therapy products are being studied for a variety of ailments, ranging from genetic disorders to autoimmune diseases, diabetes, cancer, and HIV.
"New technologies such as gene and cell therapies hold out the potential to transform medicine and create an inflection point in our ability to treat and even cure many intractable illnesses," Gottlieb says.
Fung, who's also vice chairman of hematology/oncology at Fox Chase, says the treatment could help patients beat back an illness that has resisted conventional treatments like chemotherapy and radiation, leaving them facing death. “This is the breakthrough of the century,” he says.
And Hetty Carraway, MD, an acute leukemia doctor at the Cleveland Clinic, says the newly approved therapy represents a first step for a new way of treating cancer. “If it can bring this kind of paradigm to other types of cancers, that’s really where I think the larger implications are,” she says.
Taking the Fight to Cancer:
B-cell acute lymphoblastic leukemia attacks the blood cells that make antibodies, which help your body fight off disease. Most of the time, it’s treated successfully with chemotherapy, radiation, or by transplants of bone marrow, which produces blood cells. But in some cases, treatment fails to beat back the cancer, or it comes back. When that happens, the odds of survival fall to as little as 1 in 10.
The new treatment is a one-time infusion developed by researchers at the University of Pennsylvania and the pharmaceutical company Novartis. Officially known as chimeric antigen receptor T-cell therapy, it starts with doctors extracting disease-fighting white blood cells, known as T cells, from a patient’s blood. The cells are frozen and shipped to a laboratory, where they’re genetically engineered to attack a specific protein on the cancerous B cells.
They’re then put back into the body, where they seek out and destroy cancer cells. And because they’re cells taken from the patient’s own body, there’s no need for anti-rejection drugs, which are needed after transplants.
“This is really combining everything together,” Fung says. “This is truly using patients’ own immune cells to fight cancer.”
Dangerous Side Effects Remain a Concern:
The therapy can have dangerous side effects -- mainly a condition known as cytokine release syndrome (CRS). That happens when T cells release a lot of a chemical messenger into the bloodstream. This affects the vascular system, causing high fevers and sharp drops in blood pressure. More than 60% of patients in clinical trials had side effects due to cytokine release, Novartis reported, but none of those reactions were fatal.
Emily Whitehead, the first pediatric patient to try the therapy in 2011, had such a bad reaction initially that she was in a coma for 14 days. Her doctors told the family to say their good-byes.
“They believed she had less than a 1-in-1,000 chance of surviving to the next morning,” says her father, Tom Whitehead.
As a last hope, doctors gave Emily the arthritis drug Actemra (tocilizumab), which blocks one of the main inflammatory signals driving the CRS. On Wednesday, the FDA also approved Actemra as a treatment for CRS.
In fact, under the conditions of approval, doctor's can't use CAR T therapy unless they also have Actemra on hand to manage side effects.
Within 12 hours, Emily started to recover. She has been cancer free for five years.
Because of the side effects, Kymriah won't be available everywhere. Hopsitals and clinics will have to be specially certified to administer the treatment. Doctors and other staff will also have get additional training before they can prescribe it.
“We know and expect that type of side effect will happen, and we know that we can successfully manage it,” she says. “But it needs to be managed by people who are familiar with this type of side effect and how best to support patients,” Carraway says.
Other side effects included anemia, nausea, diarrhea, and headaches.
In three trials involving about 150 people, the remission rates were 69%, 83%, and 95%. A total of 17 patients died after receiving the treatment; 14 of them from the disease and three from infections, according to documents the company filed with the FDA.
“We believe this treatment can change the world,” says Tom Whitehead, who frequently speaks about his daughter’s experience and testified before the FDA about the treatment. He also helps raise money for children’s cancer research through The Emily Whitehead Foundation. “But we know some children relapse and we know children who didn’t make it.”
Big Possibilities and a Big Price Tag:
Another concern is the price tag associated with the therapy: The process is reported to cost as much as $475,000.
In a press release, the Center for Medicare and Medicaid Services (CMS) announced that it was exploring "innovative payment modes and arrangements" for Kymriah and other potentially life-saving treatments.
In a news release, Novartis, the company that makes Kymriah, said it was collaborating with CMS on an outcomes-based approach to pricing, which would mean that the company would only be reimbursed if a patient responds to the therapy by the end of the first month of treatment.
“Certainly, it’s far and above the expense that we typically see for drugs,” Carraway says. But current treatments can also run into the low six figures, sometimes with little success. The number of patients with relapsed acute lymphoblastic leukemia is small, “and the options for them in their young lives are pretty limited.”
“Our hope is we’ll get better at making these medications, and hopefully, with time, the cost of this will decrease,” she adds.
Novartis spokeswoman Julie Masow says the company will do “everything we can” to help get the treatment to patients who need it.
“We are carefully considering the appropriate price for CTL019, taking into consideration the value that this treatment represents for patients, society, and the health care system, both near-term and long-term, as well as input from external health economic experts,” Masow says.
The therapy was produced “via pioneering technology and a sophisticated manufacturing process,” she says -- however, “We recognize our responsibility in bringing this innovative treatment to patients.”
'He's Started School'
One of the more recent patients to have CAR T-cell therapy is 5-year-old Liam Thistlethwaite. He has been cancer free for 4 months since starting the therapy to treat his acute lymphoblastic leukemia.
First diagnosed shortly before his second birthday, Liam had gotten 32 months of different kinds of chemotherapy drugs to poison the cancer out of his small body. The treatment is harsh but almost always successful. Doctors told Liam’s parents he had a 96% chance of a cure if he could finish it.
But 8 months later, Liam’s cancer came back, with a vengeance. Leukemia cells spread to his spinal fluid. Tumors grew on two glands in his brain.
Liam’s doctor, Ching-Hon Pui, MD, chairman of the Oncology Department at St. Jude, had recently been to a medical conference that discussed the results of the CAR T-cell therapy.
He convinced Children’s Hospital of Philadelphia to put him on its waiting list, which was about 6 months long at the time.
Because Liam was relatively healthy and had a low cancer burden when he was treated, his father thinks he avoided some of the most severe side effects of the therapy. He spiked very high fevers and spent a few days in the hospital but pulled through.
“He’s started school. He’s doing wonderfully,” says Patrick Thistlethwaite.
Despite Optimism, Major Questions Remain:
One of the unanswered questions is how long CAR T cells can last in the body. In some patients, they’ve persisted for as long as 5 years. Others have their cells die in weeks or months. Another big question is whether the cancer will come back if the CAR T cells are gone.
The Thistlethwaites say it was very hard to know whether to try CAR T on a toddler.
“Our physician truly felt that we’d have the same odds, so to speak, as going into a stem cell transplant with heavy radiation. He believed CAR T to have high side effects up front, but no high long-term side effects," Patrick Thistlethwaite says.
They knew radiation to Liam’s brain and spinal cord could cause long-term damage.
“We still have those options,” Patrick says. “We hope we never have to use them.”
“We hope CAR T is the end of it all.”
[End of Article]
The approval Wednesday allows a process known as CAR T-cell therapy to be used in children or young adults fighting an often fatal recurrence of the most common childhood cancer -- B-cell acute lymphoblastic leukemia.
And it clears the way for a new approach to fighting cancer by harnessing the body’s immune system -- a long-sought goal of medical researchers.
“This is a dream come true,” says Henry Fung, MD, director of the Fox Chase Cancer Center-Temple University Hospital Bone Marrow Transplant Program. “It’s now limited to one disease in children only, but that platform potentially can benefit a lot of different types of cancer patients, particularly blood cancer patients.”
'A New Frontier'
FDA Commissioner Scott Gottlieb, MD, called the approval of the therapy -- brand named Kymriah -- a "new frontier in medical innovation."
In a news conference on Wednesday, Gottlieb said the FDA had 76 active investigational new drug applications related to CAR T-cell products, and more than 500 for gene therapy products are being studied for a variety of ailments, ranging from genetic disorders to autoimmune diseases, diabetes, cancer, and HIV.
"New technologies such as gene and cell therapies hold out the potential to transform medicine and create an inflection point in our ability to treat and even cure many intractable illnesses," Gottlieb says.
Fung, who's also vice chairman of hematology/oncology at Fox Chase, says the treatment could help patients beat back an illness that has resisted conventional treatments like chemotherapy and radiation, leaving them facing death. “This is the breakthrough of the century,” he says.
And Hetty Carraway, MD, an acute leukemia doctor at the Cleveland Clinic, says the newly approved therapy represents a first step for a new way of treating cancer. “If it can bring this kind of paradigm to other types of cancers, that’s really where I think the larger implications are,” she says.
Taking the Fight to Cancer:
B-cell acute lymphoblastic leukemia attacks the blood cells that make antibodies, which help your body fight off disease. Most of the time, it’s treated successfully with chemotherapy, radiation, or by transplants of bone marrow, which produces blood cells. But in some cases, treatment fails to beat back the cancer, or it comes back. When that happens, the odds of survival fall to as little as 1 in 10.
The new treatment is a one-time infusion developed by researchers at the University of Pennsylvania and the pharmaceutical company Novartis. Officially known as chimeric antigen receptor T-cell therapy, it starts with doctors extracting disease-fighting white blood cells, known as T cells, from a patient’s blood. The cells are frozen and shipped to a laboratory, where they’re genetically engineered to attack a specific protein on the cancerous B cells.
They’re then put back into the body, where they seek out and destroy cancer cells. And because they’re cells taken from the patient’s own body, there’s no need for anti-rejection drugs, which are needed after transplants.
“This is really combining everything together,” Fung says. “This is truly using patients’ own immune cells to fight cancer.”
Dangerous Side Effects Remain a Concern:
The therapy can have dangerous side effects -- mainly a condition known as cytokine release syndrome (CRS). That happens when T cells release a lot of a chemical messenger into the bloodstream. This affects the vascular system, causing high fevers and sharp drops in blood pressure. More than 60% of patients in clinical trials had side effects due to cytokine release, Novartis reported, but none of those reactions were fatal.
Emily Whitehead, the first pediatric patient to try the therapy in 2011, had such a bad reaction initially that she was in a coma for 14 days. Her doctors told the family to say their good-byes.
“They believed she had less than a 1-in-1,000 chance of surviving to the next morning,” says her father, Tom Whitehead.
As a last hope, doctors gave Emily the arthritis drug Actemra (tocilizumab), which blocks one of the main inflammatory signals driving the CRS. On Wednesday, the FDA also approved Actemra as a treatment for CRS.
In fact, under the conditions of approval, doctor's can't use CAR T therapy unless they also have Actemra on hand to manage side effects.
Within 12 hours, Emily started to recover. She has been cancer free for five years.
Because of the side effects, Kymriah won't be available everywhere. Hopsitals and clinics will have to be specially certified to administer the treatment. Doctors and other staff will also have get additional training before they can prescribe it.
“We know and expect that type of side effect will happen, and we know that we can successfully manage it,” she says. “But it needs to be managed by people who are familiar with this type of side effect and how best to support patients,” Carraway says.
Other side effects included anemia, nausea, diarrhea, and headaches.
In three trials involving about 150 people, the remission rates were 69%, 83%, and 95%. A total of 17 patients died after receiving the treatment; 14 of them from the disease and three from infections, according to documents the company filed with the FDA.
“We believe this treatment can change the world,” says Tom Whitehead, who frequently speaks about his daughter’s experience and testified before the FDA about the treatment. He also helps raise money for children’s cancer research through The Emily Whitehead Foundation. “But we know some children relapse and we know children who didn’t make it.”
Big Possibilities and a Big Price Tag:
Another concern is the price tag associated with the therapy: The process is reported to cost as much as $475,000.
In a press release, the Center for Medicare and Medicaid Services (CMS) announced that it was exploring "innovative payment modes and arrangements" for Kymriah and other potentially life-saving treatments.
In a news release, Novartis, the company that makes Kymriah, said it was collaborating with CMS on an outcomes-based approach to pricing, which would mean that the company would only be reimbursed if a patient responds to the therapy by the end of the first month of treatment.
“Certainly, it’s far and above the expense that we typically see for drugs,” Carraway says. But current treatments can also run into the low six figures, sometimes with little success. The number of patients with relapsed acute lymphoblastic leukemia is small, “and the options for them in their young lives are pretty limited.”
“Our hope is we’ll get better at making these medications, and hopefully, with time, the cost of this will decrease,” she adds.
Novartis spokeswoman Julie Masow says the company will do “everything we can” to help get the treatment to patients who need it.
“We are carefully considering the appropriate price for CTL019, taking into consideration the value that this treatment represents for patients, society, and the health care system, both near-term and long-term, as well as input from external health economic experts,” Masow says.
The therapy was produced “via pioneering technology and a sophisticated manufacturing process,” she says -- however, “We recognize our responsibility in bringing this innovative treatment to patients.”
'He's Started School'
One of the more recent patients to have CAR T-cell therapy is 5-year-old Liam Thistlethwaite. He has been cancer free for 4 months since starting the therapy to treat his acute lymphoblastic leukemia.
First diagnosed shortly before his second birthday, Liam had gotten 32 months of different kinds of chemotherapy drugs to poison the cancer out of his small body. The treatment is harsh but almost always successful. Doctors told Liam’s parents he had a 96% chance of a cure if he could finish it.
But 8 months later, Liam’s cancer came back, with a vengeance. Leukemia cells spread to his spinal fluid. Tumors grew on two glands in his brain.
Liam’s doctor, Ching-Hon Pui, MD, chairman of the Oncology Department at St. Jude, had recently been to a medical conference that discussed the results of the CAR T-cell therapy.
He convinced Children’s Hospital of Philadelphia to put him on its waiting list, which was about 6 months long at the time.
Because Liam was relatively healthy and had a low cancer burden when he was treated, his father thinks he avoided some of the most severe side effects of the therapy. He spiked very high fevers and spent a few days in the hospital but pulled through.
“He’s started school. He’s doing wonderfully,” says Patrick Thistlethwaite.
Despite Optimism, Major Questions Remain:
One of the unanswered questions is how long CAR T cells can last in the body. In some patients, they’ve persisted for as long as 5 years. Others have their cells die in weeks or months. Another big question is whether the cancer will come back if the CAR T cells are gone.
The Thistlethwaites say it was very hard to know whether to try CAR T on a toddler.
“Our physician truly felt that we’d have the same odds, so to speak, as going into a stem cell transplant with heavy radiation. He believed CAR T to have high side effects up front, but no high long-term side effects," Patrick Thistlethwaite says.
They knew radiation to Liam’s brain and spinal cord could cause long-term damage.
“We still have those options,” Patrick says. “We hope we never have to use them.”
“We hope CAR T is the end of it all.”
[End of Article]
[Your Webhost: I actually had a pacemaker implanted into my chest recently. Since I have been able to resume my cardio workout at the gym, thanks to the MedTronic device!]
Artificial Cardiac Pacemakers
YouTube Video: What Is a Pacemaker and How Does It Work?
Pictured: (L) position of pacemaker, (R) pacemaker
A pacemaker (or artificial pacemaker, so as not to be confused with the heart's natural pacemaker) is a medical device which uses electrical impulses, delivered by electrodes contracting the heart muscles, to regulate the beating of the heart.
The primary purpose of a pacemaker is to maintain an adequate heart rate, either because the heart's natural pacemaker is not fast enough, or because there is a block in the heart's electrical conduction system.
Modern pacemakers are externally programmable and allow a cardiologist to select the optimum pacing modes for individual patients. Some combine a pacemaker and defibrillator in a single implantable device. Others have multiple electrodes stimulating differing positions within the heart to improve synchronization of the lower chambers (ventricles) of the heart.
Click on any of the following blue hyperlinks for more about Artificial Cardiac Pacemakers:
The primary purpose of a pacemaker is to maintain an adequate heart rate, either because the heart's natural pacemaker is not fast enough, or because there is a block in the heart's electrical conduction system.
Modern pacemakers are externally programmable and allow a cardiologist to select the optimum pacing modes for individual patients. Some combine a pacemaker and defibrillator in a single implantable device. Others have multiple electrodes stimulating differing positions within the heart to improve synchronization of the lower chambers (ventricles) of the heart.
Click on any of the following blue hyperlinks for more about Artificial Cardiac Pacemakers:
- Methods of pacing
- Basic function
- Biventricular pacing
- Advancements in function
- Considerations
- Other devices
- History
- See also:
- Biological pacemaker
- Button cell
- Electrical conduction system of the heart
- Implantable cardioverter-defibrillator
- Infective endocarditis
- Pacemaker syndrome
- WiTricity
- Qi (inductive power standard)
- Detecting and Distinguishing Cardiac Pacing Artifacts
- Implantable Cardioverter Defibrillator from National Heart, Lung and Blood Institute
(U.S.) National Institutes of Health (NIH), including Medical Advancements to Eliminate Forms of Cancer
YouTube Video: Jim Parsons* on Documentary "First In Human"
* -- Jim Parsons
Pictured: Aerial photograph from the north of the Mark O. Hatfield Clinical Research Center (Building 10) on the National Institutes of Health Bethesda, Maryland campus.
The National Institutes of Health (NIH) is the primary agency of the United States government responsible for biomedical and public health research, founded in the late 1870s. It is part of the United States Department of Health and Human Services with facilities mainly located in Bethesda, Maryland.
The NIH conducts its own scientific research through its Intramural Research Program (IRP) and provides major biomedical research funding to non-NIH research facilities through its Extramural Research Program.
As of 2013, the IRP had 1,200 principal investigators and more than 4,000 postdoctoral fellows in basic, translational, and clinical research, being the largest biomedical research institution in the world, while, as of 2003, the extramural arm provided 28% of biomedical research funding spent annually in the U.S., or about US$26.4 billion.
The NIH comprises 27 separate institutes and centers of different biomedical disciplines and is responsible for many scientific accomplishments, including the discovery of fluoride to prevent tooth decay, the use of lithium to manage bipolar disorder, and the creation of vaccines against hepatitis, Haemophilus influenzae (HIB), and human papillomavirus (HPV).
Click on any of the following blue hyperlinks for more about The National Institutes of Health (NIH):
Medical Advancements to Eliminate Forms of Cancer (Fact Sheet by NIH)
Click on the following blue hyperlinks for more about each topic listed below:
The NIH conducts its own scientific research through its Intramural Research Program (IRP) and provides major biomedical research funding to non-NIH research facilities through its Extramural Research Program.
As of 2013, the IRP had 1,200 principal investigators and more than 4,000 postdoctoral fellows in basic, translational, and clinical research, being the largest biomedical research institution in the world, while, as of 2003, the extramural arm provided 28% of biomedical research funding spent annually in the U.S., or about US$26.4 billion.
The NIH comprises 27 separate institutes and centers of different biomedical disciplines and is responsible for many scientific accomplishments, including the discovery of fluoride to prevent tooth decay, the use of lithium to manage bipolar disorder, and the creation of vaccines against hepatitis, Haemophilus influenzae (HIB), and human papillomavirus (HPV).
Click on any of the following blue hyperlinks for more about The National Institutes of Health (NIH):
- History
- Directors
- Locations and campuses
- Research
- Funding
- Stakeholders
- Commercial partnerships
- Institutes and centers
- See also:
- List of institutes and centers of the National Institutes of Health
- United States Public Health Service
- National Institutes of Health Stroke Scale
- Heads of International Research Organizations
- NIH Toolbox
- Official website
- National Institutes of Health in the Federal Register
- Regional Medical Programs Collection of information on NIH's Regional Medical Programs, from the National Library of Medicine
- Nice health tips for all age people
Medical Advancements to Eliminate Forms of Cancer (Fact Sheet by NIH)
Click on the following blue hyperlinks for more about each topic listed below:
- What is the immune system?
- Are cancer cells recognized by the immune system?
- What are vaccines?
- What are cancer vaccines?
- How do cancer preventive vaccines work?
- What cancer preventive vaccines are approved in the United States?
- How are cancer treatment vaccines designed to work?
- Has the FDA approved any cancer treatment vaccines?
- How are cancer vaccines made?
- Are adjuvants used with cancer vaccines?
- Do cancer vaccines have side effects?
- Can cancer treatment vaccines be combined with other types of cancer therapy?
- What additional research is under way to improve cancer treatment vaccines?
- What types of vaccines are being studied in clinical trials?
Pharmaceutical Industry ("Big Pharma") including List of pharmaceutical companies
TOP: US Pharmaceutical Pricing: An Overview
BOTTOM: Why do Americans spend so much on pharmaceuticals?
- YouTube Video: Top 10 Largest Pharmaceutical Companies
- YouTube Video: The Facts on America's Opioid Epidemic (NY Times)
- YouTube Video: How Does the FDA Approve a Drug?
TOP: US Pharmaceutical Pricing: An Overview
BOTTOM: Why do Americans spend so much on pharmaceuticals?
Click to set custom HTML
Click here for a List of Pharmaceutical Companies that comprise "Big Pharma".
The pharmaceutical industry discovers, develops, produces, and markets drugs or pharmaceutical drugs for use as medications. Pharmaceutical companies may deal in generic or brand medications and medical devices. They are subject to a variety of laws and regulations that govern the patenting, testing, safety, efficacy and marketing of drugs.
Research and development:
Main articles: Drug discovery and Drug development
Drug discovery is the process by which potential drugs are discovered or designed. In the past most drugs have been discovered either by isolating the active ingredient from traditional remedies or by serendipitous discovery. Modern biotechnology often focuses on understanding the metabolic pathways related to a disease state or pathogen, and manipulating these pathways using molecular biology or biochemistry.
A great deal of early-stage drug discovery has traditionally been carried out by universities and research institutions.
Drug development refers to activities undertaken after a compound is identified as a potential drug in order to establish its suitability as a medication. Objectives of drug development are to determine appropriate formulation and dosing, as well as to establish safety. Research in these areas generally includes a combination of in vitro studies, in vivo studies, and clinical trials. The cost of late stage development has meant it is usually done by the larger pharmaceutical companies.
Often, large multinational corporations exhibit vertical integration, participating in a broad range of drug discovery and development, manufacturing and quality control, marketing, sales, and distribution.
Smaller organizations, on the other hand, often focus on a specific aspect such as discovering drug candidates or developing formulations. Often, collaborative agreements between research organizations and large pharmaceutical companies are formed to explore the potential of new drug substances.
More recently, multi-nationals are increasingly relying on contract research organizations to manage drug development.
The cost of innovation:
Drug discovery and development is very expensive; of all compounds investigated for use in humans only a small fraction are eventually approved in most nations by government appointed medical institutions or boards, who have to approve new drugs before they can be marketed in those countries.
In 2010 18 NMEs (New Molecular Entities) were approved and three biologics by the FDA, or 21 in total, which is down from 26 in 2009 and 24 in 2008. On the other hand, there were only 18 approvals in total in 2007 and 22 back in 2006.
Since 2001, the Center for Drug Evaluation and Research has averaged 22.9 approvals a year. This approval comes only after heavy investment in pre-clinical development and clinical trials, as well as a commitment to ongoing safety monitoring.
Drugs which fail part-way through this process often incur large costs, while generating no revenue in return. If the cost of these failed drugs is taken into account, the cost of developing a successful new drug (new chemical entity, or NCE), has been estimated at about US$1.3 billion, not including marketing expenses). Professors Light and Lexchin reported in 2012, however, that the rate of approval for new drugs has been a relatively stable average rate of 15 to 25 for decades.
Industry-wide research and investment reached a record $65.3 billion in 2009.[78] While the cost of research in the U.S. was about $34.2 billion between 1995 and 2010, revenues rose faster (revenues rose by $200.4 billion in that time).
A study by the consulting firm Bain & Company reported that the cost for discovering, developing and launching (which factored in marketing and other business expenses) a new drug (along with the prospective drugs that fail) rose over a five-year period to nearly $1.7 billion in 2003. According to Forbes, by 2010 development costs were between $4 billion to $11 billion per drug.
Some of these estimates also take into account the opportunity cost of investing capital many years before revenues are realized (see Time-value of money). Because of the very long time needed for discovery, development, and approval of pharmaceuticals, these costs can accumulate to nearly half the total expense.
A direct consequence within the pharmaceutical industry value chain is that major pharmaceutical multinationals tend to increasingly outsource risks related to fundamental research, which somewhat reshapes the industry ecosystem with biotechnology companies playing an increasingly important role, and overall strategies being redefined accordingly.
Some approved drugs, such as those based on re-formulation of an existing active ingredient (also referred to as Line-extensions) are much less expensive to develop.
Controversies:
Due to repeated accusations and findings that some clinical trials conducted or funded by pharmaceutical companies may report only positive results for the preferred medication, the industry has been looked at much more closely by independent groups and government agencies.
In response to specific cases in which unfavorable data from pharmaceutical company-sponsored research was not published, the Pharmaceutical Research and Manufacturers of America have published new guidelines urging companies to report all findings and limit the financial involvement in drug companies of researchers.
US congress signed into law a bill which requires phase II and phase III clinical trials to be registered by the sponsor on the clinicaltrials.gov website run by the NIH.
Drug researchers not directly employed by pharmaceutical companies often look to companies for grants, and companies often look to researchers for studies that will make their products look favorable. Sponsored researchers are rewarded by drug companies, for example with support for their conference/symposium costs. Lecture scripts and even journal articles presented by academic researchers may actually be "ghost-written" by pharmaceutical companies.
An investigation by ProPublica found that at least 21 doctors have been paid more than $500,000 for speeches and consulting by drugs manufacturers since 2009, with half of the top earners working in psychiatry, and about $2 billion in total paid to doctors for such services. AstraZeneca, Johnson & Johnson and Eli Lilly have paid billions of dollars in federal settlements over allegations that they paid doctors to promote drugs for unapproved uses. Some prominent medical schools have since tightened rules on faculty acceptance of such payments by drug companies.
In contrast to this viewpoint, an article and associated editorial in the New England Journal of Medicine in May 2015 emphasized the importance of pharmaceutical industry-physician interactions for the development of novel treatments, and argued that moral outrage over industry malfeasance had unjustifiably led many to overemphasize the problems created by financial conflicts of interest.
The article noted that major healthcare organizations such as National Center for Advancing Translational Sciences of the National Institutes of Health, the President's Council of Advisors on Science and Technology, the World Economic Forum, the Gates Foundation, the Wellcome Trust, and the Food and Drug Administration had encouraged greater interactions between physicians and industry in order to bring greater benefits to patients.
Product approval:
In the United States, new pharmaceutical products must be approved by the Food and Drug Administration (FDA) as being both safe and effective. This process generally involves submission of an Investigational New Drug filing with sufficient pre-clinical data to support proceeding with human trials. Following IND approval, three phases of progressively larger human clinical trials may be conducted.
Phase I generally studies toxicity using healthy volunteers. Phase II can include pharmacokinetics and dosing in patients, and Phase III is a very large study of efficacy in the intended patient population.
Following the successful completion of phase III testing, a New Drug Application is submitted to the FDA. The FDA review the data and if the product is seen as having a positive benefit-risk assessment, approval to market the product in the US is granted.
A fourth phase of post-approval surveillance is also often required due to the fact that even the largest clinical trials cannot effectively predict the prevalence of rare side-effects.
Postmarketing surveillance ensures that after marketing the safety of a drug is monitored closely. In certain instances, its indication may need to be limited to particular patient groups, and in others the substance is withdrawn from the market completely. The FDA provides information about approved drugs at the Orange Book site.
In the UK, the Medicines and Healthcare Products Regulatory Agency approves drugs for use, though the evaluation is done by the European Medicines Agency, an agency of the European Union based in London. Normally an approval in the UK and other European countries comes later than one in the USA. Then it is the National Institute for Health and Care Excellence (NICE), for England and Wales, who decides if and how the National Health Service (NHS) will allow (in the sense of paying for) their use. The British National Formulary is the core guide for pharmacists and clinicians.
In many non-US western countries a 'fourth hurdle' of cost effectiveness analysis has developed before new technologies can be provided. This focuses on the efficiency (in terms of the cost per QALY) of the technologies in question rather than their efficacy. In England and Wales NICE decides whether and in what circumstances drugs and technologies will be made available by the NHS, whilst similar arrangements exist with the Scottish Medicines Consortium in Scotland, and the Pharmaceutical Benefits Advisory Committee in Australia. A product must pass the threshold for cost-effectiveness if it is to be approved.
Treatments must represent 'value for money' and a net benefit to society.
Orphan drugs:
Main article: Orphan drug
There are special rules for certain rare diseases ("orphan diseases") in several major drug regulatory territories. For example, diseases involving fewer than 200,000 patients in the United States, or larger populations in certain circumstances are subject to the Orphan Drug Act.
Because medical research and development of drugs to treat such diseases is financially disadvantageous, companies that do so are rewarded with tax reductions, fee waivers, and market exclusivity on that drug for a limited time (seven years), regardless of whether the drug is protected by patents.
Click on any of the following blue hyperlinks for more abou the Pharmaceutical Industry:
The pharmaceutical industry discovers, develops, produces, and markets drugs or pharmaceutical drugs for use as medications. Pharmaceutical companies may deal in generic or brand medications and medical devices. They are subject to a variety of laws and regulations that govern the patenting, testing, safety, efficacy and marketing of drugs.
Research and development:
Main articles: Drug discovery and Drug development
Drug discovery is the process by which potential drugs are discovered or designed. In the past most drugs have been discovered either by isolating the active ingredient from traditional remedies or by serendipitous discovery. Modern biotechnology often focuses on understanding the metabolic pathways related to a disease state or pathogen, and manipulating these pathways using molecular biology or biochemistry.
A great deal of early-stage drug discovery has traditionally been carried out by universities and research institutions.
Drug development refers to activities undertaken after a compound is identified as a potential drug in order to establish its suitability as a medication. Objectives of drug development are to determine appropriate formulation and dosing, as well as to establish safety. Research in these areas generally includes a combination of in vitro studies, in vivo studies, and clinical trials. The cost of late stage development has meant it is usually done by the larger pharmaceutical companies.
Often, large multinational corporations exhibit vertical integration, participating in a broad range of drug discovery and development, manufacturing and quality control, marketing, sales, and distribution.
Smaller organizations, on the other hand, often focus on a specific aspect such as discovering drug candidates or developing formulations. Often, collaborative agreements between research organizations and large pharmaceutical companies are formed to explore the potential of new drug substances.
More recently, multi-nationals are increasingly relying on contract research organizations to manage drug development.
The cost of innovation:
Drug discovery and development is very expensive; of all compounds investigated for use in humans only a small fraction are eventually approved in most nations by government appointed medical institutions or boards, who have to approve new drugs before they can be marketed in those countries.
In 2010 18 NMEs (New Molecular Entities) were approved and three biologics by the FDA, or 21 in total, which is down from 26 in 2009 and 24 in 2008. On the other hand, there were only 18 approvals in total in 2007 and 22 back in 2006.
Since 2001, the Center for Drug Evaluation and Research has averaged 22.9 approvals a year. This approval comes only after heavy investment in pre-clinical development and clinical trials, as well as a commitment to ongoing safety monitoring.
Drugs which fail part-way through this process often incur large costs, while generating no revenue in return. If the cost of these failed drugs is taken into account, the cost of developing a successful new drug (new chemical entity, or NCE), has been estimated at about US$1.3 billion, not including marketing expenses). Professors Light and Lexchin reported in 2012, however, that the rate of approval for new drugs has been a relatively stable average rate of 15 to 25 for decades.
Industry-wide research and investment reached a record $65.3 billion in 2009.[78] While the cost of research in the U.S. was about $34.2 billion between 1995 and 2010, revenues rose faster (revenues rose by $200.4 billion in that time).
A study by the consulting firm Bain & Company reported that the cost for discovering, developing and launching (which factored in marketing and other business expenses) a new drug (along with the prospective drugs that fail) rose over a five-year period to nearly $1.7 billion in 2003. According to Forbes, by 2010 development costs were between $4 billion to $11 billion per drug.
Some of these estimates also take into account the opportunity cost of investing capital many years before revenues are realized (see Time-value of money). Because of the very long time needed for discovery, development, and approval of pharmaceuticals, these costs can accumulate to nearly half the total expense.
A direct consequence within the pharmaceutical industry value chain is that major pharmaceutical multinationals tend to increasingly outsource risks related to fundamental research, which somewhat reshapes the industry ecosystem with biotechnology companies playing an increasingly important role, and overall strategies being redefined accordingly.
Some approved drugs, such as those based on re-formulation of an existing active ingredient (also referred to as Line-extensions) are much less expensive to develop.
Controversies:
Due to repeated accusations and findings that some clinical trials conducted or funded by pharmaceutical companies may report only positive results for the preferred medication, the industry has been looked at much more closely by independent groups and government agencies.
In response to specific cases in which unfavorable data from pharmaceutical company-sponsored research was not published, the Pharmaceutical Research and Manufacturers of America have published new guidelines urging companies to report all findings and limit the financial involvement in drug companies of researchers.
US congress signed into law a bill which requires phase II and phase III clinical trials to be registered by the sponsor on the clinicaltrials.gov website run by the NIH.
Drug researchers not directly employed by pharmaceutical companies often look to companies for grants, and companies often look to researchers for studies that will make their products look favorable. Sponsored researchers are rewarded by drug companies, for example with support for their conference/symposium costs. Lecture scripts and even journal articles presented by academic researchers may actually be "ghost-written" by pharmaceutical companies.
An investigation by ProPublica found that at least 21 doctors have been paid more than $500,000 for speeches and consulting by drugs manufacturers since 2009, with half of the top earners working in psychiatry, and about $2 billion in total paid to doctors for such services. AstraZeneca, Johnson & Johnson and Eli Lilly have paid billions of dollars in federal settlements over allegations that they paid doctors to promote drugs for unapproved uses. Some prominent medical schools have since tightened rules on faculty acceptance of such payments by drug companies.
In contrast to this viewpoint, an article and associated editorial in the New England Journal of Medicine in May 2015 emphasized the importance of pharmaceutical industry-physician interactions for the development of novel treatments, and argued that moral outrage over industry malfeasance had unjustifiably led many to overemphasize the problems created by financial conflicts of interest.
The article noted that major healthcare organizations such as National Center for Advancing Translational Sciences of the National Institutes of Health, the President's Council of Advisors on Science and Technology, the World Economic Forum, the Gates Foundation, the Wellcome Trust, and the Food and Drug Administration had encouraged greater interactions between physicians and industry in order to bring greater benefits to patients.
Product approval:
In the United States, new pharmaceutical products must be approved by the Food and Drug Administration (FDA) as being both safe and effective. This process generally involves submission of an Investigational New Drug filing with sufficient pre-clinical data to support proceeding with human trials. Following IND approval, three phases of progressively larger human clinical trials may be conducted.
Phase I generally studies toxicity using healthy volunteers. Phase II can include pharmacokinetics and dosing in patients, and Phase III is a very large study of efficacy in the intended patient population.
Following the successful completion of phase III testing, a New Drug Application is submitted to the FDA. The FDA review the data and if the product is seen as having a positive benefit-risk assessment, approval to market the product in the US is granted.
A fourth phase of post-approval surveillance is also often required due to the fact that even the largest clinical trials cannot effectively predict the prevalence of rare side-effects.
Postmarketing surveillance ensures that after marketing the safety of a drug is monitored closely. In certain instances, its indication may need to be limited to particular patient groups, and in others the substance is withdrawn from the market completely. The FDA provides information about approved drugs at the Orange Book site.
In the UK, the Medicines and Healthcare Products Regulatory Agency approves drugs for use, though the evaluation is done by the European Medicines Agency, an agency of the European Union based in London. Normally an approval in the UK and other European countries comes later than one in the USA. Then it is the National Institute for Health and Care Excellence (NICE), for England and Wales, who decides if and how the National Health Service (NHS) will allow (in the sense of paying for) their use. The British National Formulary is the core guide for pharmacists and clinicians.
In many non-US western countries a 'fourth hurdle' of cost effectiveness analysis has developed before new technologies can be provided. This focuses on the efficiency (in terms of the cost per QALY) of the technologies in question rather than their efficacy. In England and Wales NICE decides whether and in what circumstances drugs and technologies will be made available by the NHS, whilst similar arrangements exist with the Scottish Medicines Consortium in Scotland, and the Pharmaceutical Benefits Advisory Committee in Australia. A product must pass the threshold for cost-effectiveness if it is to be approved.
Treatments must represent 'value for money' and a net benefit to society.
Orphan drugs:
Main article: Orphan drug
There are special rules for certain rare diseases ("orphan diseases") in several major drug regulatory territories. For example, diseases involving fewer than 200,000 patients in the United States, or larger populations in certain circumstances are subject to the Orphan Drug Act.
Because medical research and development of drugs to treat such diseases is financially disadvantageous, companies that do so are rewarded with tax reductions, fee waivers, and market exclusivity on that drug for a limited time (seven years), regardless of whether the drug is protected by patents.
Click on any of the following blue hyperlinks for more abou the Pharmaceutical Industry:
- History
- Global sales
- Marketing
- Controversy about drug marketing and lobbying
- Developing world
- See also:
Generic Medications and their Manufacturers
YouTube Video: Meet Blue: Generic Medications PSA
Pictured: 2017 Generic Drug Access and Savings in the U.S. Report
Click here for an alphabetical listing of generic drug manufactures.
A generic drug is a pharmaceutical drug that is equivalent to a brand-name product in dosage, strength, route of administration, quality, performance and intended use. The term may also refer to any drug marketed under its chemical name without advertising, or to the chemical makeup of a drug rather than the brand name under which the drug is sold.
Although they may not be associated with a particular company, generic drugs are usually subject to government regulations in the countries where they are dispensed. They are labeled with the name of the manufacturer and a generic nonproprietary name such as the United States Adopted Name or international non-proprietary name of the drug.
A generic drug must contain the same active ingredients as the original brand-name formulation. The U.S. Food and Drug Administration (FDA) requires that generics be identical to, or within an acceptable bioequivalent range of, their brand-name counterparts with respect to pharmacokinetic and pharmacodynamic properties. (The FDA's use of the word "identical" is a legal interpretation, not literal.)
Biopharmaceuticals such as monoclonal antibodies differ biologically from small molecule drugs. Generic versions of these drugs, known as biosimilars, are typically regulated under an extended set of rules.
In most cases, generic products become available after the patent protections afforded to a drug's original developer expire. Once generic drugs enter the market, competition often leads to substantially lower prices for both the original brand-name product and its generic equivalents. In most countries, patents give 20 years of protection.
However, many countries and regions, such as the European Union and the United States,may grant up to five years of additional protection ("patent term restoration") if manufacturers meet specific goals, such as conducting clinical trials for pediatric patients. Manufacturers, wholesalers, insurers, and drugstores can each increase prices at various stages of production and distribution.
In 2014, according to an analysis by the Generic Pharmaceutical Association, generic drugs accounted for 88% of the 4.3 billion prescriptions filled in the United States.
Click on any of the blue hyperlinks for more about Generic Drugs:
A generic drug is a pharmaceutical drug that is equivalent to a brand-name product in dosage, strength, route of administration, quality, performance and intended use. The term may also refer to any drug marketed under its chemical name without advertising, or to the chemical makeup of a drug rather than the brand name under which the drug is sold.
Although they may not be associated with a particular company, generic drugs are usually subject to government regulations in the countries where they are dispensed. They are labeled with the name of the manufacturer and a generic nonproprietary name such as the United States Adopted Name or international non-proprietary name of the drug.
A generic drug must contain the same active ingredients as the original brand-name formulation. The U.S. Food and Drug Administration (FDA) requires that generics be identical to, or within an acceptable bioequivalent range of, their brand-name counterparts with respect to pharmacokinetic and pharmacodynamic properties. (The FDA's use of the word "identical" is a legal interpretation, not literal.)
Biopharmaceuticals such as monoclonal antibodies differ biologically from small molecule drugs. Generic versions of these drugs, known as biosimilars, are typically regulated under an extended set of rules.
In most cases, generic products become available after the patent protections afforded to a drug's original developer expire. Once generic drugs enter the market, competition often leads to substantially lower prices for both the original brand-name product and its generic equivalents. In most countries, patents give 20 years of protection.
However, many countries and regions, such as the European Union and the United States,may grant up to five years of additional protection ("patent term restoration") if manufacturers meet specific goals, such as conducting clinical trials for pediatric patients. Manufacturers, wholesalers, insurers, and drugstores can each increase prices at various stages of production and distribution.
In 2014, according to an analysis by the Generic Pharmaceutical Association, generic drugs accounted for 88% of the 4.3 billion prescriptions filled in the United States.
Click on any of the blue hyperlinks for more about Generic Drugs:
- Nomenclature
- Economics
- Regulation in the United States
- See also:
- Anti-Counterfeiting Trade Agreement#Criminalizing generic medicine (ACTA)
- Bayh–Dole Act
- Biosimilars
- Chemical patents
- Evergreening
- Generic brand
- International Nonproprietary Name
- Inverse benefit law
- Prescription costs
- Research exemption
- SOPA#Protection against counterfeit drugs
- Trans-Pacific Partnership Intellectual Property Provisions
- Transatlantic Trade and Investment Partnership
- United States Adopted Names Program, generic drug naming process, lists of adopted names
- The Medical Letter on Drugs and Therapeutics
- Collection of national and international Guidelines
- GPhA Generic Pharmaceutical Association
Surgery, including a List of Surgical Procedures
YouTube Video: Laparoscopic Cholecystectomy (Gallbladder Removal)
Pictured: (L-R) Surgeons repairing a ruptured Achilles tendon on a man; Stereotactic Surgery
Click Here for a List of Surgical Procedures.
Surgery is a medical specialty that uses operative manual and instrumental techniques on a patient to investigate or treat a pathological condition such as a disease or injury, to help improve bodily function or appearance or to repair unwanted ruptured areas.
An act of performing surgery may be called a "surgical procedure", "operation", or simply "surgery". In this context, the verb "operate" means to perform surgery. The adjective "surgical" means pertaining to surgery; e.g. surgical instruments or surgical nurse. The patient or subject on which the surgery is performed can be a person or an animal.
A surgeon is a person who practices surgery and a surgeon's assistant is a person who practices surgical assistance. A surgical team is made up of surgeon, surgeon's assistant, anesthesia provider, circulating nurse and surgical technologist. Surgery usually spans minutes to hours, but it is typically not an ongoing or periodic type of treatment. The term "surgery" can also refer to the place where surgery is performed, or simply the office of a physician, dentist, or veterinarian.
Click on the following blue hyperlinks for more about Surgery:
Surgery is a medical specialty that uses operative manual and instrumental techniques on a patient to investigate or treat a pathological condition such as a disease or injury, to help improve bodily function or appearance or to repair unwanted ruptured areas.
An act of performing surgery may be called a "surgical procedure", "operation", or simply "surgery". In this context, the verb "operate" means to perform surgery. The adjective "surgical" means pertaining to surgery; e.g. surgical instruments or surgical nurse. The patient or subject on which the surgery is performed can be a person or an animal.
A surgeon is a person who practices surgery and a surgeon's assistant is a person who practices surgical assistance. A surgical team is made up of surgeon, surgeon's assistant, anesthesia provider, circulating nurse and surgical technologist. Surgery usually spans minutes to hours, but it is typically not an ongoing or periodic type of treatment. The term "surgery" can also refer to the place where surgery is performed, or simply the office of a physician, dentist, or veterinarian.
Click on the following blue hyperlinks for more about Surgery:
- Definitions
- Description of surgical procedure
- Epidemiology
- Special populations
- In low- and middle-income countries
- History
- Modern surgery
- Surgical specialties
- National societies
- See also:
- Anesthesia
- ASA physical status classification system
- Biomaterial
- Cardiac surgery
- Current Procedural Terminology (CPT; for outpatient surgical procedures medical coding)
- Surgical drain
- Endoscopy
- Fluorescence image-guided surgery
- Hypnosurgery
- ICD-10-PCS (International Classification of Diseases, 10th edition, Procedural Coding System; inpatient surgical procedures medical coding)
- Jet ventilation
- Minimally invasive procedure
- Operative report
- Perioperative mortality
- Remote surgery
- Robotic surgery
- Surgeon's assistant
- Surgical Outcomes Analysis and Research
- Surgical Sieve
- Trauma surgery
- Reconstructive surgery
- Rheumasurgery
- WHO Surgical Safety Checklist
Cardiac Surgery
YouTube Video: Open Heart Surgery Performed at Christian Hospital in St. Louis, Missouri
Pictured: Two cardiac surgeons performing coronary artery bypass surgery. Note the use of a steel retractor to forcefully maintain the exposure of the heart.
Cardiac surgery, or cardiovascular surgery, is surgery on the heart or great vessels performed by cardiac surgeons. It is often used to treat complications of ischemic heart disease (for example, with coronary artery bypass grafting); to correct congenital heart disease; or to treat valvular heart disease from various causes, including endocarditis, rheumatic heart disease, and atherosclerosis. It also includes heart transplantation.
Types of Cardiac Surgery:
Open heart surgery:
In open heart surgery, the patient's heart is opened and surgery is performed on its internal structures.
Dr. Wilfred G. Bigelow of the University of Toronto found that such procedures could be performed better in a bloodless and motionless environment. Therefore, during open heart surgery, the heart is temporarily stopped, and the patient is placed on cardiopulmonary bypass, meaning a machine pumps their blood and oxygen.
Because the machine cannot function the same way as the heart, surgeons try to minimize the time a patient spends on it.
Cardiopulmonary bypass was developed after surgeons realized the limitations of hypothermia in cardiac surgery: Complex intracardiac repairs take time, and the patient needs blood flow to the body (particularly to the brain), as well as heart and lung function.
In 1953, Dr. John Heysham Gibbon of Jefferson Medical School in Philadelphia reported the first successful use of extracorporeal circulation by means of an oxygenator, but he abandoned the method after subsequent failures.
In 1954, Dr. Lillehei performed a series of successful operations with the controlled cross-circulation technique, in which the patient's mother or father was used as a "heart-lung machine". Dr. John W. Kirklin at the Mayo Clinic was the first to use a Gibbon-type pump-oxygenator.
Nazih Zuhdi performed the first total intentional hemodilution open heart surgery on Terry Gene Nix, age 7, on 25 February 1960 at Mercy Hospital in Oklahoma City. The operation was a success; however, Nix died three years later. In March 1961, Zuhdi, Carey, and Greer performed open heart surgery on a child, age 3 1⁄2, using the total intentional hemodilution machine.
Modern beating-heart surgery:
In the early 1990s, surgeons began to perform off-pump coronary artery bypass, done without cardiopulmonary bypass. In these operations, the heart continues beating during surgery, but is stabilized to provide an almost still work area in which to connect a conduit vessel that bypasses a blockage using a technique known as endoscopic vessel harvesting (EVH).
Heart transplant:
In 1945, the Soviet pathologist Nikolai Sinitsyn successfully transplanted a heart from one frog to another frog and from one dog to another dog.
Norman Shumway is widely regarded as the father of human heart transplantation, although the world's first adult heart transplant was performed by a South African cardiac surgeon, Christiaan Barnard, using techniques developed by Shumway and Richard Lower.
Barnard performed the first transplant on Louis Washkansky on 3 December 1967 at Groote Schuur Hospital in Cape Town. Adrian Kantrowitz performed the first pediatric heart transplant on 6 December 1967 at Maimonides Hospital (now Maimonides Medical Center) in Brooklyn, New York, barely three days later. Shumway performed the first adult heart transplant in the United States on 6 January 1968 at Stanford University Hospital.
Coronary artery bypass grafting:
Coronary artery bypass grafting, also called revascularization, is a common surgical procedure to create an alternative path to deliver blood supply to the heart and body, with the goal of preventing clot formation. This can be done in many ways, and the arteries used can be taken from several areas of the body. Arteries are typically harvested from the chest, arm, or wrist and then attached to a portion of the coronary artery, relieving pressure and limiting clotting factors in that area of the heart.
The procedure is typically performed because of coronary artery disease (CAD), in which a plaque-like substance builds up in the coronary artery, the main pathway carrying oxygen-rich blood to the heart. This can cause a blockage and/or a rupture, which can lead to a heart attack.
Minimally invasive surgery:
As an alternative to open heart surgery, which involves a five- to eight-inch incision in the chest wall, a surgeon may perform an endoscopic procedure by making very small incisions through which a camera and specialized tools are inserted.
In robot-assisted heart surgery, a machine controlled by a cardiac surgeon is used to perform a procedure. The main advantage to this is the size of the incision required: three small holes instead of an incision big enough for the surgeon's hands.
Post-surgical procedures:
As with any surgical procedure, cardiac surgery requires postoperative precautions to avoid complications. Incision care is needed to avoid infection and minimize scarring. Swelling and loss of appetite are common.
Recovery from open heart surgery begins with about 48 hours in an intensive care unit, where heart rate, blood pressure, and oxygen levels are closely monitored. Chest tubes are inserted to drain blood around the heart and lungs. After discharge from the hospital, compression socks may be recommended in order to regulate blood flow.
Risks:
The advancement of cardiac surgery and cardiopulmonary bypass techniques has greatly reduced the mortality rates of these procedures. For instance, repairs of congenital heart defects are currently estimated to have 4–6% mortality rates.
A major concern with cardiac surgery is neurological damage. Stroke occurs in 2–3% of all people undergoing cardiac surgery, and the rate is higher in patients with other risk factors for stroke.
A more subtle complication attributed to cardiopulmonary bypass is postperfusion syndrome, sometimes called "pumphead". The neurocognitive symptoms of postperfusion syndrome were initially thought to be permanent, but turned out to be transient, with no permanent neurological impairment.
In order to assess the performance of surgical units and individual surgeons, a popular risk model has been created called the EuroSCORE. It takes a number of health factors from a patient and, using precalculated logistic regression coefficients, attempts to quantify the probability that they will survive to discharge.
Within the United Kingdom, the EuroSCORE was used to give a breakdown of all cardiothoracic surgery centers and to indicate whether the units and their individuals surgeons performed within an acceptable range. The results are available on the Care Quality Commission website.
Another important source of complications are the neuropsychological and psychopathologic changes following open heart surgery. One example is Skumin syndrome, described by Victor Skumin in 1978, which is a "cardioprosthetic psychopathological syndrome" associated with mechanical heart valve implants and characterized by irrational fear, anxiety, depression, sleep disorder, and weakness.
Risk reduction:
A 2012 Cochrane systematic review found evidence that preoperative physical therapy reduced postoperative pulmonary complications, such as pneumonia and atelectasis, in patients undergoing elective cardiac surgery. In addition, the researchers found that preoperative physical therapy decreased the length of hospital stay by more than three days on average.
A 2013 Cochrane review showed that both pharmacological and non-pharmacological prevention reduce the risk of atrial fibrillation after an operation and reduced the length of hospital stays. No difference in mortality could be shown.
There is evidence that quitting smoking at least four weeks before surgery may reduce the risk of postoperative complications.
Click on any of the following blue hyperlinks for more about Cardiac Surgery:
Types of Cardiac Surgery:
Open heart surgery:
In open heart surgery, the patient's heart is opened and surgery is performed on its internal structures.
Dr. Wilfred G. Bigelow of the University of Toronto found that such procedures could be performed better in a bloodless and motionless environment. Therefore, during open heart surgery, the heart is temporarily stopped, and the patient is placed on cardiopulmonary bypass, meaning a machine pumps their blood and oxygen.
Because the machine cannot function the same way as the heart, surgeons try to minimize the time a patient spends on it.
Cardiopulmonary bypass was developed after surgeons realized the limitations of hypothermia in cardiac surgery: Complex intracardiac repairs take time, and the patient needs blood flow to the body (particularly to the brain), as well as heart and lung function.
In 1953, Dr. John Heysham Gibbon of Jefferson Medical School in Philadelphia reported the first successful use of extracorporeal circulation by means of an oxygenator, but he abandoned the method after subsequent failures.
In 1954, Dr. Lillehei performed a series of successful operations with the controlled cross-circulation technique, in which the patient's mother or father was used as a "heart-lung machine". Dr. John W. Kirklin at the Mayo Clinic was the first to use a Gibbon-type pump-oxygenator.
Nazih Zuhdi performed the first total intentional hemodilution open heart surgery on Terry Gene Nix, age 7, on 25 February 1960 at Mercy Hospital in Oklahoma City. The operation was a success; however, Nix died three years later. In March 1961, Zuhdi, Carey, and Greer performed open heart surgery on a child, age 3 1⁄2, using the total intentional hemodilution machine.
Modern beating-heart surgery:
In the early 1990s, surgeons began to perform off-pump coronary artery bypass, done without cardiopulmonary bypass. In these operations, the heart continues beating during surgery, but is stabilized to provide an almost still work area in which to connect a conduit vessel that bypasses a blockage using a technique known as endoscopic vessel harvesting (EVH).
Heart transplant:
In 1945, the Soviet pathologist Nikolai Sinitsyn successfully transplanted a heart from one frog to another frog and from one dog to another dog.
Norman Shumway is widely regarded as the father of human heart transplantation, although the world's first adult heart transplant was performed by a South African cardiac surgeon, Christiaan Barnard, using techniques developed by Shumway and Richard Lower.
Barnard performed the first transplant on Louis Washkansky on 3 December 1967 at Groote Schuur Hospital in Cape Town. Adrian Kantrowitz performed the first pediatric heart transplant on 6 December 1967 at Maimonides Hospital (now Maimonides Medical Center) in Brooklyn, New York, barely three days later. Shumway performed the first adult heart transplant in the United States on 6 January 1968 at Stanford University Hospital.
Coronary artery bypass grafting:
Coronary artery bypass grafting, also called revascularization, is a common surgical procedure to create an alternative path to deliver blood supply to the heart and body, with the goal of preventing clot formation. This can be done in many ways, and the arteries used can be taken from several areas of the body. Arteries are typically harvested from the chest, arm, or wrist and then attached to a portion of the coronary artery, relieving pressure and limiting clotting factors in that area of the heart.
The procedure is typically performed because of coronary artery disease (CAD), in which a plaque-like substance builds up in the coronary artery, the main pathway carrying oxygen-rich blood to the heart. This can cause a blockage and/or a rupture, which can lead to a heart attack.
Minimally invasive surgery:
As an alternative to open heart surgery, which involves a five- to eight-inch incision in the chest wall, a surgeon may perform an endoscopic procedure by making very small incisions through which a camera and specialized tools are inserted.
In robot-assisted heart surgery, a machine controlled by a cardiac surgeon is used to perform a procedure. The main advantage to this is the size of the incision required: three small holes instead of an incision big enough for the surgeon's hands.
Post-surgical procedures:
As with any surgical procedure, cardiac surgery requires postoperative precautions to avoid complications. Incision care is needed to avoid infection and minimize scarring. Swelling and loss of appetite are common.
Recovery from open heart surgery begins with about 48 hours in an intensive care unit, where heart rate, blood pressure, and oxygen levels are closely monitored. Chest tubes are inserted to drain blood around the heart and lungs. After discharge from the hospital, compression socks may be recommended in order to regulate blood flow.
Risks:
The advancement of cardiac surgery and cardiopulmonary bypass techniques has greatly reduced the mortality rates of these procedures. For instance, repairs of congenital heart defects are currently estimated to have 4–6% mortality rates.
A major concern with cardiac surgery is neurological damage. Stroke occurs in 2–3% of all people undergoing cardiac surgery, and the rate is higher in patients with other risk factors for stroke.
A more subtle complication attributed to cardiopulmonary bypass is postperfusion syndrome, sometimes called "pumphead". The neurocognitive symptoms of postperfusion syndrome were initially thought to be permanent, but turned out to be transient, with no permanent neurological impairment.
In order to assess the performance of surgical units and individual surgeons, a popular risk model has been created called the EuroSCORE. It takes a number of health factors from a patient and, using precalculated logistic regression coefficients, attempts to quantify the probability that they will survive to discharge.
Within the United Kingdom, the EuroSCORE was used to give a breakdown of all cardiothoracic surgery centers and to indicate whether the units and their individuals surgeons performed within an acceptable range. The results are available on the Care Quality Commission website.
Another important source of complications are the neuropsychological and psychopathologic changes following open heart surgery. One example is Skumin syndrome, described by Victor Skumin in 1978, which is a "cardioprosthetic psychopathological syndrome" associated with mechanical heart valve implants and characterized by irrational fear, anxiety, depression, sleep disorder, and weakness.
Risk reduction:
A 2012 Cochrane systematic review found evidence that preoperative physical therapy reduced postoperative pulmonary complications, such as pneumonia and atelectasis, in patients undergoing elective cardiac surgery. In addition, the researchers found that preoperative physical therapy decreased the length of hospital stay by more than three days on average.
A 2013 Cochrane review showed that both pharmacological and non-pharmacological prevention reduce the risk of atrial fibrillation after an operation and reduced the length of hospital stays. No difference in mortality could be shown.
There is evidence that quitting smoking at least four weeks before surgery may reduce the risk of postoperative complications.
Click on any of the following blue hyperlinks for more about Cardiac Surgery:
- History
- See also:
- Cardioplegia
- Eagle score
- Chest tube
- Overview at American Heart Association
- "Congenital Heart Disease Surgical Corrective Procedures", a list of surgical procedures at learningradiology.com
- "Cardiac Surgery in Adult", Specialized doctors at Narayahahealth.org
- What to expect before, during and after heart surgery from Children's Hospital and Regional Medical Center (Seattle)
- MedlinePlus Encyclopedia Minimally invasive heart surgery
Implant Surgery
YouTube Video: Surgeons Implant Heart Stent Into Awake Patient by KETV Omaha
Pictured: L-R: Orthopedic implants to repair fractures to the radius and ulna. Note the visible break in the ulna. (right forearm); An coronary stent — in this case a drug-eluting stent — is another common item implanted in humans.
An implant is a medical device manufactured to replace a missing biological structure, support a damaged biological structure, or enhance an existing biological structure. Medical implants are man-made devices, in contrast to a transplant, which is a transplanted biomedical tissue.
The surface of implants that contact the body might be made of a biomedical material such as titanium, silicone, or apatite depending on what is the most functional. In some cases implants contain electronics e.g. artificial pacemaker and cochlear implants. Some implants are bioactive, such as subcutaneous drug delivery devices in the form of implantable pills or drug-eluting stents.
Applications:
Implants can roughly be categorized into groups by application:
Sensory and Neurological:
Sensory and neurological implants are used for disorders affecting the major senses and the brain, as well as other neurological disorders. They are predominately used in the treatment of conditions such as the following:
Examples include the:
Cardiovascular:
Cardiovascular medical devices are implanted in cases where the heart, its valves, and the rest of the circulatory system is in disorder. They are used to treat conditions such as the following:
Examples include
Orthopaedic:
Orthopaedic implants help alleviate issues with the bones and joints of the body. They're used to treat bone fractures, osteoarthritis, scoliosis, spinal stenosis, and chronic pain. Examples include a wide variety of pins, rods, screws, and plates used to anchor fractured bones while they heal.
Metallic glasses based on magnesium with zinc and calcium addition are tested as the potential metallic biomaterials for biodegradable medical implants.
Contraception:
Contraceptive implants are primarily used to prevent unintended pregnancy and treat conditions such as non-pathological forms of menorrhagia. Examples include copper-and hormone-based intrauterine devices.
Cosmetic:
Cosmetic implants — often prosthetics — attempt to bring some portion of the body back to an acceptable aesthetic norm. They are used as a follow-up to mastectomy due to breast cancer, for correcting some forms of disfigurement, and modifying aspects of the body (as in buttock augmentation and chin augmentation). Examples include the breast implant, nose prosthesis, ocular prosthesis, and injectable filler.
Other organs and systems:
Other types of organ dysfunction can occur in the systems of the body, including the gastrointestinal, respiratory, and urological systems. Implants are used in those and other locations to treat conditions such as the following:
Examples include the following:
Click on any of the following blue hyperlinks for more about Implant Surgery:
The surface of implants that contact the body might be made of a biomedical material such as titanium, silicone, or apatite depending on what is the most functional. In some cases implants contain electronics e.g. artificial pacemaker and cochlear implants. Some implants are bioactive, such as subcutaneous drug delivery devices in the form of implantable pills or drug-eluting stents.
Applications:
Implants can roughly be categorized into groups by application:
Sensory and Neurological:
Sensory and neurological implants are used for disorders affecting the major senses and the brain, as well as other neurological disorders. They are predominately used in the treatment of conditions such as the following:
- cataract,
- glaucoma,
- keratoconus,
- and other visual impairments;
- otosclerosis and other hearing loss issues, as well as middle ear diseases such as otitis media;
- and neurological diseases such as epilepsy, Parkinson's disease, and treatment-resistant depression.
Examples include the:
- intraocular lens,
- intrastromal corneal ring segment,
- cochlear implant,
- tympanostomy tube,
- and neurostimulator.
Cardiovascular:
Cardiovascular medical devices are implanted in cases where the heart, its valves, and the rest of the circulatory system is in disorder. They are used to treat conditions such as the following:
- heart failure,
- cardiac arrhythmia,
- ventricular tachycardia,
- valvular heart disease,
- angina pectoris,
- and atherosclerosis.
Examples include
- the artificial heart,
- artificial heart valve,
- implantable cardioverter-defibrillator,
- cardiac pacemaker,
- and coronary stent.
Orthopaedic:
Orthopaedic implants help alleviate issues with the bones and joints of the body. They're used to treat bone fractures, osteoarthritis, scoliosis, spinal stenosis, and chronic pain. Examples include a wide variety of pins, rods, screws, and plates used to anchor fractured bones while they heal.
Metallic glasses based on magnesium with zinc and calcium addition are tested as the potential metallic biomaterials for biodegradable medical implants.
Contraception:
Contraceptive implants are primarily used to prevent unintended pregnancy and treat conditions such as non-pathological forms of menorrhagia. Examples include copper-and hormone-based intrauterine devices.
Cosmetic:
Cosmetic implants — often prosthetics — attempt to bring some portion of the body back to an acceptable aesthetic norm. They are used as a follow-up to mastectomy due to breast cancer, for correcting some forms of disfigurement, and modifying aspects of the body (as in buttock augmentation and chin augmentation). Examples include the breast implant, nose prosthesis, ocular prosthesis, and injectable filler.
Other organs and systems:
Other types of organ dysfunction can occur in the systems of the body, including the gastrointestinal, respiratory, and urological systems. Implants are used in those and other locations to treat conditions such as the following:
- gastroesophageal reflux disease,
- gastroparesis,
- respiratory failure,
- sleep apnea,
- urinary and fecal incontinence,
- and erectile dysfunction.
Examples include the following:
- LINX,
- implantable gastric stimulator,
- diaphragmatic/phrenic nerve stimulator,
- neurostimulator,
- surgical mesh,
- and penile prosthesis
Click on any of the following blue hyperlinks for more about Implant Surgery:
- Classification
- Complications
- Failures
- See also:
Joint Replacement Surgery
YouTube Video: How Does Joint Replacement Surgery Work?
Replacement arthroplasty (from Greek arthron, joint, limb, articulate, + plassein, to form, mould, forge, feign, make an image of), or joint replacement surgery, is a procedure of orthopedic surgery in which an arthritic or dysfunctional joint surface is replaced with an orthopedic prosthesis.
Joint replacement is considered as a treatment when severe joint pain or dysfunction is not alleviated by less-invasive therapies. During the latter half of the 20th century, rheumasurgery developed as a sub-specialty focused on these and a few other procedures in patients with rheumatic diseases.
Joint replacement surgery is becoming more common with knees and hips replaced most often. About 773,000 Americans had a hip or knee replaced in 2009
Click on any of the following blue hyperlinks for more about Joint Replacement Surgery:
Joint replacement is considered as a treatment when severe joint pain or dysfunction is not alleviated by less-invasive therapies. During the latter half of the 20th century, rheumasurgery developed as a sub-specialty focused on these and a few other procedures in patients with rheumatic diseases.
Joint replacement surgery is becoming more common with knees and hips replaced most often. About 773,000 Americans had a hip or knee replaced in 2009
Click on any of the following blue hyperlinks for more about Joint Replacement Surgery:
- Background
- Procedural timeline
- Materials
- Risks and complications
- Prosthesis replacement
- See also:
- Specific joint replacements
- Related treatments
- Rheumasurgery
- Arthroplasty
- Orthopedic surgery
- Joint replacement registry
- Specific joint replacements:
- Related treatments:
- Patient Information from the American Academy of Orthopedic Surgeons
- P. Benum; A. Aamodt; and K. Haugan Uncementeed Custom Femoral Components In Hip Arthroplasty
- Finkelstein, JA; Anderson, GI; Richards, RR; Waddell, JP (1991). "Polyethylene synovitis following canine total hip arthroplasty. Histomorphometric analysis". The Journal of arthroplasty. 6 Suppl: S91–6. PMID 1774577. doi:10.1016/s0883-5403(08)80062-9
Dental Surgery
YouTube Video of Famous People with Disabilities Slideshow: Cleft Palate
Pictured: Tom Cruise (L) Before and (R) After Dental Surgery
Dental surgery is any of a number of medical procedures that involve artificially modifying dentition; in other words, surgery of the teeth and jaw bones.
Types of Dental Surgery:
Some of the more common types of dental surgery are,
Professional Dental Care:
See also: Oral hygiene
Regular tooth cleaning by a dental professional is recommended to remove tartar (mineralized plaque) that may develop even with careful brushing and flossing, especially in areas of the mouth that are difficult to clean.
Professional cleaning includes tooth scaling and tooth polishing, as well as debridement if too much tartar has accumulated. This involves the use of various instruments and/or devices to loosen and remove tartar from the teeth.
Most dental hygienists recommend having the teeth professionally cleaned at least every six months.
More frequent cleaning and examination may be necessary during the treatment of many different dental/oral disorders or due to recent surgical procedures such as dental implants. Routine examination of the teeth by a dental professional is recommended at least every year. This may include yearly, select dental X-rays. See also dental plaque identification procedure and removal.
Dental instruments and restorative materials:
Main articles: Dental instruments and Dental restorative materials
Dental anesthesia:
Main article: Dental anesthesia
Dentists inject anesthetic to block sensory transmission by the alveolar nerves. The superior alveolar nerves are not usually anesthetized directly because they are difficult to approach with a needle.
For this reason, the maxillary teeth are usually anesthetized locally by inserting the needle beneath the oral mucosa surrounding the teeth. The inferior alveolar nerve is probably anesthetized more often than any other nerve in the body. To anesthetize this nerve, the dentist inserts the needle somewhat posterior to the patient’s last molar.
See also:
Types of Dental Surgery:
Some of the more common types of dental surgery are,
- Endodontic (surgery involving the pulp or root of the tooth)
- Root canal
- Pulpotomy — the opening of the pulp chamber of the tooth to allow an infection to drain; usually a precursor to a root canal
- Pulpectomy — the removal of the pulp from the pulp chamber to temporarily relieve pain; usually a precursor to a root canal
- Apicoectomy — a root-end resection. Occasionally a root canal alone is be enough to relieve pain and the end of the tooth, called the apex, is removed by entering through the gingiva and surgically extracting the diseased material.
- Root canal
- Prosthodontics (dental prosthetics)
- Crown (caps) — artificial covering of a tooth made from a variety of biocompatible materials, including CMC/PMC (ceramic/porcelain metal composite), gold or a tin/aluminum mixture. The underlying tooth must be reshaped to accommodate these fixed restorations
- Veneers — artificial coverings similar to above, except that they only cover the forward (labial or buccal) surface of the tooth. Usually for aesthetic purposes only.
- Bridge — a fixed prothesis in which two or more crowns are connected together, which replace a missing tooth or teeth through a bridge. Typically used after an extraction.
- Implant — a procedure in which a titanium implant is surgically placed in the bone (mandible or maxilla), allowed to heal, and 4–6 months later an artificial tooth is connected to the implant by cement or retained by a screw.
- Dentures (false teeth) — a partial or complete set of dentition which either attach to neighboring teeth by use of metal or plastic grasps or to the gingival or palatal surface by use of adhesive.
- Implant-supported prosthesis — a combination of dentures and implants; bases are placed into the bone, allowed to heal, and metal appliances are fixed to the gingival surface, following which dentures are placed atop and fixed into place.
- Orthodontic treatment
- Implants and implant-supported prosthesis — also an orthodontic treatment as it involves bones
- Apicoectomy — also an orthodontic treatment as part of the underlying bone structure must be removed
- Extraction — a procedure in which a diseased, redundant, or problematic tooth is removed, either by pulling or cutting out. This procedure can be done under local or general anesthesia and is very common — many people have their wisdom teeth removed before they become problematic.
- Fiberotomy — a procedure to sever the fibers around a tooth, preventing it from relapsing
- Periodontics
- Oral and maxillofacial surgery
Professional Dental Care:
See also: Oral hygiene
Regular tooth cleaning by a dental professional is recommended to remove tartar (mineralized plaque) that may develop even with careful brushing and flossing, especially in areas of the mouth that are difficult to clean.
Professional cleaning includes tooth scaling and tooth polishing, as well as debridement if too much tartar has accumulated. This involves the use of various instruments and/or devices to loosen and remove tartar from the teeth.
Most dental hygienists recommend having the teeth professionally cleaned at least every six months.
More frequent cleaning and examination may be necessary during the treatment of many different dental/oral disorders or due to recent surgical procedures such as dental implants. Routine examination of the teeth by a dental professional is recommended at least every year. This may include yearly, select dental X-rays. See also dental plaque identification procedure and removal.
Dental instruments and restorative materials:
Main articles: Dental instruments and Dental restorative materials
Dental anesthesia:
Main article: Dental anesthesia
Dentists inject anesthetic to block sensory transmission by the alveolar nerves. The superior alveolar nerves are not usually anesthetized directly because they are difficult to approach with a needle.
For this reason, the maxillary teeth are usually anesthetized locally by inserting the needle beneath the oral mucosa surrounding the teeth. The inferior alveolar nerve is probably anesthetized more often than any other nerve in the body. To anesthetize this nerve, the dentist inserts the needle somewhat posterior to the patient’s last molar.
See also:
Laparoscopic Surgery
YouTube Video: Laparoscopic Hysterectomy Procedure Animation
Pictured: (L-R) Surgeons perform laparoscopic stomach surgery; Laparoscopic instruments (Courtesy of Wikipedia)
Laparoscopic surgery, also called minimally invasive surgery (MIS), bandaid surgery, or keyhole surgery, is a modern surgical technique in which operations are performed far from their location through small incisions (usually 0.5–1.5 cm) elsewhere in the body.
There are a number of advantages to the patient with laparoscopic surgery versus the more common, open procedure. Pain and hemorrhaging are reduced due to smaller incisions and recovery times are shorter.
The key element in laparoscopic surgery is the use of a laparoscope, a long fiber optic cable system which allows viewing of the affected area by snaking the cable from a more distant, but more easily accessible location.
There are two types of laparoscope: (1) a telescopic rod lens system, that is usually connected to a video camera (single chip or three chip), or (2) a digital laparoscope where the charge-coupled device is placed at the end of the laparoscope.
Also attached is a fiber optic cable system connected to a "cold" light source (halogen or xenon), to illuminate the operative field, which is inserted through a 5 mm or 10 mm cannula or trocar.
The abdomen is usually insufflated with carbon dioxide gas. This elevates the abdominal wall above the internal organs to create a working and viewing space. CO2 is used because it is common to the human body and can be absorbed by tissue and removed by the respiratory system. It is also non-flammable, which is important because electrosurgical devices are commonly used in laparoscopic procedures.
Laparoscopic surgery includes operations within the abdominal or pelvic cavities, whereas keyhole surgery performed on the thoracic or chest cavity is called thoracoscopic surgery. Specific surgical instruments used in a laparoscopic surgery include: forceps, scissors, probes, dissectors, hooks, retractors and more. Laparoscopic and thoracoscopic surgery belong to the broader field of endoscopy.
Procedures:
Laparoscopic cholecystectomy is the most common laparoscopic procedure performed. In this procedure, 5–10 mm diameter instruments (graspers, scissors, clip applier) can be introduced by the surgeon into the abdomen through trocars (hollow tubes with a seal to keep the CO2 from leaking).
Over one million cholecystectomies are performed in the U.S. annually, with over 96% of those being performed laparoscopically.
There are two different formats for laparoscopic surgery. Multiple incisions are required for technology such as the da Vinci Surgical System, which uses a console located away from the patient, with the surgeon controlling a camera, vacuum pump, saline cleansing solution, cutting tools, etc. each located within its own incision site, but oriented toward the surgical objective.
In contrast, requiring only a single small incision, the "Bonati system" (invented by Dr. Alfred Bonati), uses a single 5-function control, so that a saline solution and the vacuum pump operate together when the laser cutter is activated. A camera and light provide feedback to the surgeon, who sees the enlarged surgical elements on a TV monitor. The Bonati system was designed for spinal surgery and has been promoted only for that purpose.
Rather than a minimum 20 cm incision as in traditional (open) cholecystectomy, four incisions of 0.5–1.0 cm, or more recently a single incision of 1.5–2.0 cm, will be sufficient to perform a laparoscopic removal of a gallbladder. Since the gallbladder is similar to a small balloon that stores and releases bile, it can usually be removed from the abdomen by suctioning out the bile and then removing the deflated gallbladder through the 1 cm incision at the patient's navel. The length of postoperative stay in the hospital is minimal, and same-day discharges are possible in cases of early morning procedures.
In certain advanced laparoscopic procedures, where the size of the specimen being removed would be too large to pull out through a trocar site (as would be done with a gallbladder), an incision larger than 10 mm must be made.
The most common of these procedures are removal of all or part of the colon (colectomy), or removal of the kidney (nephrectomy). Some surgeons perform these procedures completely laparoscopically, making the larger incision toward the end of the procedure for specimen removal, or, in the case of a colectomy, to also prepare the remaining healthy bowel to be reconnected (create an anastomosis).
Many other surgeons feel that since they will have to make a larger incision for specimen removal anyway, they might as well use this incision to have their hand in the operative field during the procedure to aid as a retractor, dissector, and to be able to feel differing tissue densities (palpate), as they would in open surgery. This technique is called hand-assist laparoscopy.
Since they will still be working with scopes and other laparoscopic instruments, CO2 will have to be maintained in the patient's abdomen, so a device known as a hand access port (a sleeve with a seal that allows passage of the hand) must be used.
Surgeons who choose this hand-assist technique feel it reduces operative time significantly versus the straight laparoscopic approach. It also gives them more options in dealing with unexpected adverse events (e.g. uncontrolled bleeding) that may otherwise require creating a much larger incision and converting to a fully open surgical procedure.
Conceptually, the laparoscopic approach is intended to minimize post-operative pain and speed up recovery times, while maintaining an enhanced visual field for surgeons.
Due to improved patient outcomes, in the last two decades, laparoscopic surgery has been adopted by various surgical sub-specialties including gastrointestinal surgery (including bariatric procedures for morbid obesity), gynecologic surgery and urology.
Based on numerous prospective randomized controlled trials, the approach has proven to be beneficial in reducing post-operative morbidities such as wound infections and incisional hernias (especially in morbidly obese patients), and is now deemed safe when applied to surgery for cancers such as cancer of colon.
The restricted vision, the difficulty in handling of the instruments (new hand-eye coordination skills are needed), the lack of tactile perception and the limited working area are factors which add to the technical complexity of this surgical approach. For these reasons, minimally invasive surgery has emerged as a highly competitive new sub-specialty within various fields of surgery.
Surgical residents who wish to focus on this area of surgery gain additional laparoscopic surgery training during one or two years of fellowship after completing their basic surgical residency. In OB-GYN residency programs, the average laparoscopy-to-laparotomy quotient (LPQ) is 0.55.
The first transatlantic surgery (Lindbergh operation) ever performed was a laparoscopic gallbladder removal.
Laparoscopic techniques have also been developed in the field of veterinary medicine. Due to the relative high cost of the equipment required, however, it has not become commonplace in most traditional practices today but rather limited to specialty-type practices. Many of the same surgeries performed in humans can be applied to animal cases – everything from an egg-bound tortoise to a German Shepherd can benefit from MIS.
A paper published in JAVMA (Journal of the American Veterinary Medical Association) in 2005 showed that dogs spayed laparoscopically experienced significantly less pain (65%) than those that were spayed with traditional "open" methods.
Arthroscopy, thoracoscopy, cystoscopy are all performed in veterinary medicine today. The University of Georgia School of Veterinary Medicine and Colorado State University's School of Veterinary Medicine are two of the main centers where veterinary laparoscopy got started and have excellent training programs for veterinarians interested in getting started in MIS.
Advantages:
There are a number of advantages to the patient with laparoscopic surgery versus an open procedure. These include:
Although laparoscopy in adult age group is widely accepted, its advantages in pediatric age group is questioned. Benefits of laparoscopy appears to recede with younger age. Efficacy of laparoscopy is inferior to open surgery in certain conditions such as pyloromyotomy for Infantile hypertrophic pyloric stenosis. Although laparoscopic appendectomy has lesser wound problems than open surgery, the former is associated with more intra-abdominal abscesses.
Disadvantages:
While laparoscopic surgery is clearly advantageous in terms of patient outcomes, the procedure is more difficult from the surgeon's perspective when compared to traditional, open surgery:
Risks:
Some of the risks are briefly described below:
The risk of such injuries is increased in patients who have a low body mass index or have a history of prior abdominal surgery. While these injuries are rare, significant complications can occur, and they are primarily related to the umbilical insertion site. Vascular injuries can result in hemorrhage that may be life-threatening. Injuries to the bowel can cause a delayed peritonitis. It is very important that these injuries be recognized as early as possible.
Robotic laparoscopic surgery:
Main article: Robotic surgery
The process of minimally invasive surgery has been augmented by specialized tools for decades. For example, TransEnterix of Durham, North Carolina received U.S. Food and Drug Administration approval in October 2009 for its SPIDER Surgical System using flexible instruments and one incision in the navel area instead of several, allowing quicker healing for patients. Dr. Richard Stac of Duke University developed the process.
In recent years, electronic tools have been developed to aid surgeons. Some of the features include:
There has been a distinct lack of disclosure regarding nano-scale developments in keyhole surgery and remote medicine, a "disparity of disclosure" which does not correlate with the rapid advancements in both the medical and nanotechnology fields over the last two decades.
Robotic surgery has been touted as a solution to underdeveloped nations, whereby a single central hospital can operate several remote machines at distant locations. The potential for robotic surgery has had strong military interest as well, with the intention of providing mobile medical care while keeping trained doctors safe from battle.
Non-robotic hand guided assistance systems:
There are also user-friendly non robotic assistance systems that are single hand guided devices with a high potential to save time and money. These assistance devices are not bound by the restrictions of common medical robotic systems. The systems enhance the manual possibilities of the surgeon and his/her team, regarding the need of replacing static holding force during the intervention.
Some of the features are:
Click on any of the following blue hyperlinks for more about Laparoscopic Surgery:
There are a number of advantages to the patient with laparoscopic surgery versus the more common, open procedure. Pain and hemorrhaging are reduced due to smaller incisions and recovery times are shorter.
The key element in laparoscopic surgery is the use of a laparoscope, a long fiber optic cable system which allows viewing of the affected area by snaking the cable from a more distant, but more easily accessible location.
There are two types of laparoscope: (1) a telescopic rod lens system, that is usually connected to a video camera (single chip or three chip), or (2) a digital laparoscope where the charge-coupled device is placed at the end of the laparoscope.
Also attached is a fiber optic cable system connected to a "cold" light source (halogen or xenon), to illuminate the operative field, which is inserted through a 5 mm or 10 mm cannula or trocar.
The abdomen is usually insufflated with carbon dioxide gas. This elevates the abdominal wall above the internal organs to create a working and viewing space. CO2 is used because it is common to the human body and can be absorbed by tissue and removed by the respiratory system. It is also non-flammable, which is important because electrosurgical devices are commonly used in laparoscopic procedures.
Laparoscopic surgery includes operations within the abdominal or pelvic cavities, whereas keyhole surgery performed on the thoracic or chest cavity is called thoracoscopic surgery. Specific surgical instruments used in a laparoscopic surgery include: forceps, scissors, probes, dissectors, hooks, retractors and more. Laparoscopic and thoracoscopic surgery belong to the broader field of endoscopy.
Procedures:
Laparoscopic cholecystectomy is the most common laparoscopic procedure performed. In this procedure, 5–10 mm diameter instruments (graspers, scissors, clip applier) can be introduced by the surgeon into the abdomen through trocars (hollow tubes with a seal to keep the CO2 from leaking).
Over one million cholecystectomies are performed in the U.S. annually, with over 96% of those being performed laparoscopically.
There are two different formats for laparoscopic surgery. Multiple incisions are required for technology such as the da Vinci Surgical System, which uses a console located away from the patient, with the surgeon controlling a camera, vacuum pump, saline cleansing solution, cutting tools, etc. each located within its own incision site, but oriented toward the surgical objective.
In contrast, requiring only a single small incision, the "Bonati system" (invented by Dr. Alfred Bonati), uses a single 5-function control, so that a saline solution and the vacuum pump operate together when the laser cutter is activated. A camera and light provide feedback to the surgeon, who sees the enlarged surgical elements on a TV monitor. The Bonati system was designed for spinal surgery and has been promoted only for that purpose.
Rather than a minimum 20 cm incision as in traditional (open) cholecystectomy, four incisions of 0.5–1.0 cm, or more recently a single incision of 1.5–2.0 cm, will be sufficient to perform a laparoscopic removal of a gallbladder. Since the gallbladder is similar to a small balloon that stores and releases bile, it can usually be removed from the abdomen by suctioning out the bile and then removing the deflated gallbladder through the 1 cm incision at the patient's navel. The length of postoperative stay in the hospital is minimal, and same-day discharges are possible in cases of early morning procedures.
In certain advanced laparoscopic procedures, where the size of the specimen being removed would be too large to pull out through a trocar site (as would be done with a gallbladder), an incision larger than 10 mm must be made.
The most common of these procedures are removal of all or part of the colon (colectomy), or removal of the kidney (nephrectomy). Some surgeons perform these procedures completely laparoscopically, making the larger incision toward the end of the procedure for specimen removal, or, in the case of a colectomy, to also prepare the remaining healthy bowel to be reconnected (create an anastomosis).
Many other surgeons feel that since they will have to make a larger incision for specimen removal anyway, they might as well use this incision to have their hand in the operative field during the procedure to aid as a retractor, dissector, and to be able to feel differing tissue densities (palpate), as they would in open surgery. This technique is called hand-assist laparoscopy.
Since they will still be working with scopes and other laparoscopic instruments, CO2 will have to be maintained in the patient's abdomen, so a device known as a hand access port (a sleeve with a seal that allows passage of the hand) must be used.
Surgeons who choose this hand-assist technique feel it reduces operative time significantly versus the straight laparoscopic approach. It also gives them more options in dealing with unexpected adverse events (e.g. uncontrolled bleeding) that may otherwise require creating a much larger incision and converting to a fully open surgical procedure.
Conceptually, the laparoscopic approach is intended to minimize post-operative pain and speed up recovery times, while maintaining an enhanced visual field for surgeons.
Due to improved patient outcomes, in the last two decades, laparoscopic surgery has been adopted by various surgical sub-specialties including gastrointestinal surgery (including bariatric procedures for morbid obesity), gynecologic surgery and urology.
Based on numerous prospective randomized controlled trials, the approach has proven to be beneficial in reducing post-operative morbidities such as wound infections and incisional hernias (especially in morbidly obese patients), and is now deemed safe when applied to surgery for cancers such as cancer of colon.
The restricted vision, the difficulty in handling of the instruments (new hand-eye coordination skills are needed), the lack of tactile perception and the limited working area are factors which add to the technical complexity of this surgical approach. For these reasons, minimally invasive surgery has emerged as a highly competitive new sub-specialty within various fields of surgery.
Surgical residents who wish to focus on this area of surgery gain additional laparoscopic surgery training during one or two years of fellowship after completing their basic surgical residency. In OB-GYN residency programs, the average laparoscopy-to-laparotomy quotient (LPQ) is 0.55.
The first transatlantic surgery (Lindbergh operation) ever performed was a laparoscopic gallbladder removal.
Laparoscopic techniques have also been developed in the field of veterinary medicine. Due to the relative high cost of the equipment required, however, it has not become commonplace in most traditional practices today but rather limited to specialty-type practices. Many of the same surgeries performed in humans can be applied to animal cases – everything from an egg-bound tortoise to a German Shepherd can benefit from MIS.
A paper published in JAVMA (Journal of the American Veterinary Medical Association) in 2005 showed that dogs spayed laparoscopically experienced significantly less pain (65%) than those that were spayed with traditional "open" methods.
Arthroscopy, thoracoscopy, cystoscopy are all performed in veterinary medicine today. The University of Georgia School of Veterinary Medicine and Colorado State University's School of Veterinary Medicine are two of the main centers where veterinary laparoscopy got started and have excellent training programs for veterinarians interested in getting started in MIS.
Advantages:
There are a number of advantages to the patient with laparoscopic surgery versus an open procedure. These include:
- Reduced hemorrhaging, which reduces the chance of needing a blood transfusion.
- Smaller incision, which reduces pain and shortens recovery time, as well as resulting in less post-operative scarring.
- Less pain, leading to less pain medication needed.
- Although procedure times are usually slightly longer, hospital stay is less, and often with a same day discharge which leads to a faster return to everyday living.
- Reduced exposure of internal organs to possible external contaminants thereby reduced risk of acquiring infections.
- There are more indications for laparoscopic surgery in gastrointestinal emergencies as the field develops.
Although laparoscopy in adult age group is widely accepted, its advantages in pediatric age group is questioned. Benefits of laparoscopy appears to recede with younger age. Efficacy of laparoscopy is inferior to open surgery in certain conditions such as pyloromyotomy for Infantile hypertrophic pyloric stenosis. Although laparoscopic appendectomy has lesser wound problems than open surgery, the former is associated with more intra-abdominal abscesses.
Disadvantages:
While laparoscopic surgery is clearly advantageous in terms of patient outcomes, the procedure is more difficult from the surgeon's perspective when compared to traditional, open surgery:
- The surgeon has limited range of motion at the surgical site resulting in a loss of dexterity.
- Poor depth perception.
- Surgeons must use tools to interact with tissue rather than manipulate it directly with their hands. This results in an inability to accurately judge how much force is being applied to tissue as well as a risk of damaging tissue by applying more force than necessary. This limitation also reduces tactile sensation, making it more difficult for the surgeon to feel tissue (sometimes an important diagnostic tool, such as when palpating for tumors) and making delicate operations such as tying sutures more difficult.
- The tool endpoints move in the opposite direction to the surgeon's hands due to the pivot point, making laparoscopic surgery a non-intuitive motor skill that is difficult to learn. This is called the Fulcrum effect.
- Some surgeries (carpal tunnel for instance) generally turn out better for the patient when the area can be opened up, allowing the surgeon to see "the whole picture" surrounding physiology, to better address the issue at hand. In this regard, keyhole surgery can be a disadvantage.
Risks:
Some of the risks are briefly described below:
- The most significant risks are from trocar injuries during insertion into the abdominal cavity, as the trocar is typically inserted blindly. Injuries include abdominal wall hematoma, umbilical hernias, umbilical wound infection, and penetration of blood vessels or small or large bowel.
The risk of such injuries is increased in patients who have a low body mass index or have a history of prior abdominal surgery. While these injuries are rare, significant complications can occur, and they are primarily related to the umbilical insertion site. Vascular injuries can result in hemorrhage that may be life-threatening. Injuries to the bowel can cause a delayed peritonitis. It is very important that these injuries be recognized as early as possible.
- Some patients have sustained electrical burns unseen by surgeons who are working with electrodes that leak current into surrounding tissue. The resulting injuries can result in perforated organs and can also lead to peritonitis. This risk is eliminated by utilizing active electrode monitoring.
- There may be an increased risk of hypothermia and peritoneal trauma due to increased exposure to cold, dry gases during insufflation. The use of Surgical Humidification therapy, which is the use of heated and humidified CO2 for insufflation, has been shown to reduce this risk.
- Many patients with existing pulmonary disorders may not tolerate pneumoperitoneum (gas in the abdominal cavity), resulting in a need for conversion to open surgery after the initial attempt at laparoscopic approach.
- Not all of the CO2 introduced into the abdominal cavity is removed through the incisions during surgery. Gas tends to rise, and when a pocket of CO2 rises in the abdomen, it pushes against the diaphragm (the muscle that separates the abdominal from the thoracic cavities and facilitates breathing), and can exert pressure on the phrenic nerve. This produces a sensation of pain that may extend to the patient's shoulders. For an appendectomy, the right shoulder can be particularly painful. In some cases this can also cause considerable pain when breathing. In all cases, however, the pain is transient, as the body tissues will absorb the CO2 and eliminate it through respiration.
- Coagulation disorders and dense adhesions (scar tissue) from previous abdominal surgery may pose added risk for laparoscopic surgery and are considered relative contra-indications for this approach.
- Intra-abdominal adhesion formation is a risk associated with both laparoscopic and open surgery and remains a significant, unresolved problem. Adhesions are fibrous deposits that connect tissue to organ post surgery. Generally, they occur in 50-100% of all abdominal surgeries, with the risk of developing adhesions being the same for both procedures. Complications of adhesions include chronic pelvic pain, bowel obstruction, and female infertility. In particular, small bowel obstruction poses the most significant problem. The use of surgical humidification therapy during laparoscopic surgery may minimize the incidence of adhesion formation. Other techniques to reduce adhesion formation include the use of physical barriers such as films or gels, or broad-coverage fluid agents to separate tissues during healing following surgery.
Robotic laparoscopic surgery:
Main article: Robotic surgery
The process of minimally invasive surgery has been augmented by specialized tools for decades. For example, TransEnterix of Durham, North Carolina received U.S. Food and Drug Administration approval in October 2009 for its SPIDER Surgical System using flexible instruments and one incision in the navel area instead of several, allowing quicker healing for patients. Dr. Richard Stac of Duke University developed the process.
In recent years, electronic tools have been developed to aid surgeons. Some of the features include:
- Visual magnification — use of a large viewing screen improves visibility
- Stabilization — Electromechanical damping of vibrations, due to machinery or shaky human hands
- Simulators — use of specialized virtual reality training tools to improve physicians' proficiency in surgery
- Reduced number of incisions
There has been a distinct lack of disclosure regarding nano-scale developments in keyhole surgery and remote medicine, a "disparity of disclosure" which does not correlate with the rapid advancements in both the medical and nanotechnology fields over the last two decades.
Robotic surgery has been touted as a solution to underdeveloped nations, whereby a single central hospital can operate several remote machines at distant locations. The potential for robotic surgery has had strong military interest as well, with the intention of providing mobile medical care while keeping trained doctors safe from battle.
Non-robotic hand guided assistance systems:
There are also user-friendly non robotic assistance systems that are single hand guided devices with a high potential to save time and money. These assistance devices are not bound by the restrictions of common medical robotic systems. The systems enhance the manual possibilities of the surgeon and his/her team, regarding the need of replacing static holding force during the intervention.
Some of the features are:
- The stabilization of the camera picture because the whole static workload is conveyed by the assistance system.
- Some systems enable a fast repositioning and very short time for fixation of less than 0.02 seconds at the desired position. Some systems are lightweight constructions (18 kg) and can withstand a force of 20 N in any position and direction.
- The benefit – a physically relaxed intervention team can work concentrated on the main goals during the intervention.
- The potentials of these systems enhance the possibilities of the mobile medical care with those lightweight assistance systems. These assistance systems meet the demands of true solo surgery assistance systems and are robust, versatile, and easy to use.
Click on any of the following blue hyperlinks for more about Laparoscopic Surgery:
- History
- See also:
- Arthroscopic surgery
- Percutaneous (surgery)
- Invasiveness of surgical procedures
- Natural orifice translumenal endoscopic surgery (NOTES)
- Revision weight loss surgery
- Single port laparoscopy
- Feder, Barnaby J., "Surgical Device Poses a Rare but Serious Peril" The New York Times, March 17, 2006
- Laparoscopy web information
- World Association of Laparoscopic Surgeons
- World Journal of Laparoscopic Surgery
Eye Care Professional
YouTube Video about Eye Health: What Are Cataracts?
Pictured Below: Illustration of the eye and its parts: 1. vitreous body; 2. ora serrata; 3. ciliary muscle; 4. ciliary zonules; 5. Schlemm's canal; 6. pupil; 7. anterior chamber; 8. cornea; 9. iris; 10. lens cortex; 11. lens nucleus; 12. ciliary process; 13. conjunctiva; 14. inferior oblique muscle; 15. inferior rectus muscle; 16. medial rectus muscle; 17. retinal arteries and veins; 18. optic disc; 19. dura mater; 20. central retinal artery 21. central retinal vein; 22. optic nerve; 23. vorticose vein; 24. bulbar sheath; 25. macula; 26. fovea; 27. sclera; 28. choroid 29. superior rectus muscle
An eye care professional (ECP) is an individual who provides a service related to the eyes or vision. It is any healthcare worker involved in eye care, from one with a small amount of post-secondary training to practitioners with a doctoral level of education.
Optometrist:
Main article: Optometry
The World Council of Optometry, a member of the World Health
Organisation, defines optometrists as “…the primary healthcare practitioners of the eye and visual system who provide comprehensive eye and vision care, which includes refraction and dispensing, detection/diagnosis and management of disease in the eye, and the rehabilitation of conditions of the visual system.”
A Doctor of Optometry (OD) attends four years of college, four years of optometry school and then an optional one-year residency. Optometrists undergo extensive and intensive refractive and medical training mainly pertaining to the eye and the entrance criteria to attend optometry school is also highly competitive. An OD is fully qualified to treat eye diseases and disorders and specializes in optics and vision correction. Permissions granted by an optometric license vary by location.
Ophthalmologist:
Main article: Ophthalmology
Ophthalmologists are “…medical and osteopathic doctors who provide comprehensive eye care, including medical, surgical and optical care.” In the US, this requires four years of college, four years of medical school, one year general internship, three years of residency, then optional fellowship for 1 to 2 years (typically 12–14 years of education after high school).
An ophthalmologist can perform all the tests an optometrist can and in addition is a fully qualified medical doctor and surgeon. Ophthalmologists undergo extensive and intensive medical and surgical exams to qualify and entrance criteria to a training program is highly competitive. Some ophthalmologists receive additional advanced training (or fellowship) in specific areas of ophthalmology, such as retina, cornea, glaucoma, laser vision correction, pediatric ophthalmology, uveitis, pathology, or neuro-ophthalmology.
Click on any of the following blue hyperlinks for more about Eye Care Professionals:
Optometrist:
Main article: Optometry
The World Council of Optometry, a member of the World Health
Organisation, defines optometrists as “…the primary healthcare practitioners of the eye and visual system who provide comprehensive eye and vision care, which includes refraction and dispensing, detection/diagnosis and management of disease in the eye, and the rehabilitation of conditions of the visual system.”
A Doctor of Optometry (OD) attends four years of college, four years of optometry school and then an optional one-year residency. Optometrists undergo extensive and intensive refractive and medical training mainly pertaining to the eye and the entrance criteria to attend optometry school is also highly competitive. An OD is fully qualified to treat eye diseases and disorders and specializes in optics and vision correction. Permissions granted by an optometric license vary by location.
- In the United States and Canada, the standard education is four years of college and four years of optometry school at an accredited Doctor of Optometry (OD) program. An additional one to two years of residency, fellowship and/or specialty training is required to qualify for certain positions. All optometry colleges in the U.S. currently provide training in the diagnosis and treatment of eye diseases and level 1 in office surgical procedures.
- In the United States, optometrists are defined as physicians under Medicare, but laws pertaining to optometry vary by state.
- All states allow treatment of eye diseases, including the use of topical pharmaceuticals (by properly licensed optometrists)
- 48/50 states allow prescription of oral medications to treat eye diseases
- Many states allow optometrists to perform injections in and around the eye
- Oklahoma, Kentucky, and Louisiana allow optometrists to perform certain laser surgeries.
- Outside of the United States, Canada, United Kingdom, Australia and Philippines, optometrists are often limited in their use of pharmaceuticals. In most of these countries, optometry is either a 4-year or 5-year college degree and they are not classified as doctors.
Ophthalmologist:
Main article: Ophthalmology
Ophthalmologists are “…medical and osteopathic doctors who provide comprehensive eye care, including medical, surgical and optical care.” In the US, this requires four years of college, four years of medical school, one year general internship, three years of residency, then optional fellowship for 1 to 2 years (typically 12–14 years of education after high school).
An ophthalmologist can perform all the tests an optometrist can and in addition is a fully qualified medical doctor and surgeon. Ophthalmologists undergo extensive and intensive medical and surgical exams to qualify and entrance criteria to a training program is highly competitive. Some ophthalmologists receive additional advanced training (or fellowship) in specific areas of ophthalmology, such as retina, cornea, glaucoma, laser vision correction, pediatric ophthalmology, uveitis, pathology, or neuro-ophthalmology.
Click on any of the following blue hyperlinks for more about Eye Care Professionals:
- Other Types
- Distinction between ophthalmologists, optometrists and orthoptists
- International organizations
- European Council of Optometry and Optics
- International Agency for the Prevention of Blindness
- International Council of Ophthalmology
- International Orthoptic Association
- World Council of Optometry
- World Optometry Foundation
- See also:
- American Optometric Association
- American Academy of Optometry
- American Association for Pediatric Ophthalmology and Strabismus
- American Academy of Ophthalmology
- College of Optometrists
- College of Optometrists in Vision Development
- Joint Commission on Allied Health Personnel in Ophthalmology
- Optometric Extension Program
- The Institute of Optometry
- Worshipful Company of Spectacle Makers
Eye surgery, also known as ocular surgery, is surgery performed on the eye or its adnexa, typically by an ophthalmologist.
The eye is a fragile organ, and requires extreme care before, during, and after a surgical procedure. An expert eye surgeon is responsible for selecting the appropriate surgical procedure for the patient, and for taking the necessary safety precautions. Mentions of eye surgery can be found in several ancient texts. Today it continues to be a widely practiced type of surgery, having developed various techniques for treating eye problems.
Preparation and precautions:
Main article: Anaesthesia for ocular surgery
Since the eye is heavily supplied by nerves, anesthesia is essential. Local anesthesia is most commonly used. Topical anesthesia using lidocaine topical gel are often used for quick procedures. Since topical anesthesia requires cooperation from the patient, general anesthesia is often used for children, traumatic eye injuries, major orbitotomies and for apprehensive patients.
The physician administering anesthesia, or a nurse anesthetist or anesthetist assistant with expertise in anesthesia of the eye, monitors the patient's cardiovascular status. Sterile precautions are taken to prepare the area for surgery and lower the risk of infection. These precautions include the use of antiseptics, such as povidone-iodine, and sterile drapes, gowns and gloves.
Laser eye surgery:
Although the terms laser eye surgery and refractive surgery are commonly used as if they were interchangeable, this is not the case. Lasers may be used to treat nonrefractive conditions (e.g. to seal a retinal tear).
Laser eye surgery or laser corneal surgery is a medical procedure that uses a laser to reshape the surface of the eye. This is done to correct myopia (short-sightedness), hypermetropia (long sightedness) and astigmatism (uneven curvature of the eye's surface). It is important to note that refractive surgery is not compatible with everyone, and rarely people may find that eyewear is still needed after surgery.
Recent developments also include procedures that can change eye color from brown to blue.
Cataract surgery:
Main article: Cataract surgery
A cataract is an opacification or cloudiness of the eye's crystalline lens due to aging, disease, or trauma that typically prevents light from forming a clear image on the retina. If visual loss is significant, surgical removal of the lens may be warranted, with lost optical power usually replaced with a plastic intraocular lens (IOL). Owing to the high prevalence of cataracts, cataract extraction is the most common eye surgery. Rest after surgery is recommended.
Glaucoma surgery:
Main article: Glaucoma surgery
Glaucoma is a group of diseases affecting the optic nerve that results in vision loss and is frequently characterized by raised intraocular pressure (IOP).
There are many types of glaucoma surgery, and variations or combinations of those types, that facilitate the escape of excess aqueous humor from the eye to lower intraocular pressure, and a few that lower IOP by decreasing the production of aqueous humor.
Canaloplasty:
Canaloplasty is an advanced, nonpenetrating procedure designed to enhance drainage through the eye’s natural drainage system to provide sustained reduction of IOP. Canaloplasty utilizes microcatheter technology in a simple and minimally invasive procedure. To perform a canaloplasty, an Ophthalmologist creates a tiny incision to gain access to a canal in the eye.
A microcatheter circumnavigates the canal around the iris, enlarging the main drainage channel and its smaller collector channels through the injection of a sterile, gel-like material called viscoelastic. The catheter is then removed and a suture is placed within the canal and tightened. By opening up the canal, the pressure inside the eye can be reduced.
Refractive surgery:
Main article: Refractive surgery
Refractive surgery aims to correct errors of refraction in the eye, reducing or eliminating the need for corrective lenses
Corneal surgery:
Corneal surgery includes most refractive surgery as well as the following:
Vitreo-retinal surgery:
Vitreo-retinal surgery includes the following:
Eye muscle surgery:
Main article: Strabismus surgery
With approximately 1.2 million procedures each year, extraocular muscle surgery is the third most common eye surgery in the United States.
Click on any of the following blue hyperlinks for more about Eye Surgery:
The eye is a fragile organ, and requires extreme care before, during, and after a surgical procedure. An expert eye surgeon is responsible for selecting the appropriate surgical procedure for the patient, and for taking the necessary safety precautions. Mentions of eye surgery can be found in several ancient texts. Today it continues to be a widely practiced type of surgery, having developed various techniques for treating eye problems.
Preparation and precautions:
Main article: Anaesthesia for ocular surgery
Since the eye is heavily supplied by nerves, anesthesia is essential. Local anesthesia is most commonly used. Topical anesthesia using lidocaine topical gel are often used for quick procedures. Since topical anesthesia requires cooperation from the patient, general anesthesia is often used for children, traumatic eye injuries, major orbitotomies and for apprehensive patients.
The physician administering anesthesia, or a nurse anesthetist or anesthetist assistant with expertise in anesthesia of the eye, monitors the patient's cardiovascular status. Sterile precautions are taken to prepare the area for surgery and lower the risk of infection. These precautions include the use of antiseptics, such as povidone-iodine, and sterile drapes, gowns and gloves.
Laser eye surgery:
Although the terms laser eye surgery and refractive surgery are commonly used as if they were interchangeable, this is not the case. Lasers may be used to treat nonrefractive conditions (e.g. to seal a retinal tear).
Laser eye surgery or laser corneal surgery is a medical procedure that uses a laser to reshape the surface of the eye. This is done to correct myopia (short-sightedness), hypermetropia (long sightedness) and astigmatism (uneven curvature of the eye's surface). It is important to note that refractive surgery is not compatible with everyone, and rarely people may find that eyewear is still needed after surgery.
Recent developments also include procedures that can change eye color from brown to blue.
Cataract surgery:
Main article: Cataract surgery
A cataract is an opacification or cloudiness of the eye's crystalline lens due to aging, disease, or trauma that typically prevents light from forming a clear image on the retina. If visual loss is significant, surgical removal of the lens may be warranted, with lost optical power usually replaced with a plastic intraocular lens (IOL). Owing to the high prevalence of cataracts, cataract extraction is the most common eye surgery. Rest after surgery is recommended.
Glaucoma surgery:
Main article: Glaucoma surgery
Glaucoma is a group of diseases affecting the optic nerve that results in vision loss and is frequently characterized by raised intraocular pressure (IOP).
There are many types of glaucoma surgery, and variations or combinations of those types, that facilitate the escape of excess aqueous humor from the eye to lower intraocular pressure, and a few that lower IOP by decreasing the production of aqueous humor.
Canaloplasty:
Canaloplasty is an advanced, nonpenetrating procedure designed to enhance drainage through the eye’s natural drainage system to provide sustained reduction of IOP. Canaloplasty utilizes microcatheter technology in a simple and minimally invasive procedure. To perform a canaloplasty, an Ophthalmologist creates a tiny incision to gain access to a canal in the eye.
A microcatheter circumnavigates the canal around the iris, enlarging the main drainage channel and its smaller collector channels through the injection of a sterile, gel-like material called viscoelastic. The catheter is then removed and a suture is placed within the canal and tightened. By opening up the canal, the pressure inside the eye can be reduced.
Refractive surgery:
Main article: Refractive surgery
Refractive surgery aims to correct errors of refraction in the eye, reducing or eliminating the need for corrective lenses
- Keratomilleusis is a method of reshaping the cornea surface to change its optical power. A disc of cornea is shaved off, quickly frozen, lathe-ground, then returned to its original power.
- Automated lamellar keratoplasty (ALK)
- Laser assisted in-situ keratomileusis (LASIK)
- Laser assisted sub-epithelial keratomileusis (LASEK), a.k.a. Epi-LASIK
- Photorefractive keratectomy (PRK)
- Laser thermal keratoplasty (LTK)
- Conductive keratoplasty (CK) uses radio frequency waves to shrink corneal collagen. It is used to treat mild to moderate hyperopia.
- Limbal relaxing incisions (LRI) to correct minor astigmatism
- Astigmatic keratotomy (AK), a.k.a. Arcuate keratotomy or Transverse keratotomy
- Radial keratotomy (RK)
- Hexagonal keratotomy (HK)
- Epikeratophakia is the removal of the corneal epithelium and replacement with a lathe cut corneal button.
- Intracorneal rings (ICRs), or corneal ring segments
- Implantable contact lenses
- Presbyopia reversal
- Anterior ciliary sclerotomy (ACS)
- Scleral reinforcement surgery for the mitigation of degenerative myopia
Corneal surgery:
Corneal surgery includes most refractive surgery as well as the following:
- Corneal transplant surgery, is used to remove a cloudy/diseased cornea and replace it with a clear donor cornea.
- Penetrating keratoplasty (PK)
- Keratoprosthesis (KKPro)
- Phototherapeutic keratectomy (PTK)
- Pterygium excision
- Corneal tattooing
- Osteo-Odonto-Keratoprosthesis (OOKP), in which support for an artificial cornea is created from a tooth and its surrounding jawbone. This is a still-experimental procedure used for patients with severely damaged eyes, generally from burns.
- Eye color change surgery through an iris implant, known as Brightocular, or stripping away the top layer of eye pigment, known as the Stroma procedure.
Vitreo-retinal surgery:
Vitreo-retinal surgery includes the following:
- Vitrectomy
- Anterior vitrectomy is the removal of the front portion of vitreous tissue. It is used for preventing or treating vitreous loss during cataract or corneal surgery, or to remove misplaced vitreous in conditions such as aphakia pupillary block glaucoma.
- Pars plana vitrectomy (PPV), or trans pars plana vitrectomy (TPPV), is a procedure to remove vitreous opacities and membranes through a pars plana incision. It is frequently combined with other intraocular procedures for the treatment of giant retinal tears, tractional retinal detachments, and posterior vitreous detachments.
- Pan retinal photocoagulation (PRP) is a type of photocoagulation therapy used in the treatment of diabetic retinopathy.
- Retinal detachment repair
- Ignipuncture is an obsolete procedure that involves cauterization of the retina with a very hot pointed instrument.
- A scleral buckle is used in the repair of a retinal detachment to indent or "buckle" the sclera inward, usually by sewing a piece of preserved sclera or silicone rubber to its surface.
- Laser photocoagulation, or photocoagulation therapy, is the use of a laser to seal a retinal tear.
- Pneumatic retinopexy
- Retinal cryopexy, or retinal cryotherapy, is a procedure that uses intense cold to induce a chorioretinal scar and to destroy retinal or choroidal tissue.[23]
- Macular hole repair
- Partial lamellar sclerouvectomy
- Partial lamellar sclerocyclochoroidectomy
- Partial lamellar sclerochoroidectomy
- Posterior sclerotomy is an opening made into the vitreous through the sclera, as for detached retina or the removal of a foreign body.
- Radial optic neurotomy
- macular translocation surgery
- through 360 degree retinotomy
- through scleral imbrication technique
Eye muscle surgery:
Main article: Strabismus surgery
With approximately 1.2 million procedures each year, extraocular muscle surgery is the third most common eye surgery in the United States.
- Eye muscle surgery typically corrects strabismus and includes the following:
- Loosening / weakening procedures
- Recession involves moving the insertion of a muscle posteriorly towards its origin.
- Myectomy
- Myotomy
- Tenectomy
- Tenotomy
- Tightening / strengthening procedures
- Resection
- Tucking
- Advancement is the movement of an eye muscle from its original place of attachment on the eyeball to a more forward position.
- Transposition / repositioning procedures
- Adjustable suture surgery is a method of reattaching an extraocular muscle by means of a stitch that can be shortened or lengthened within the first post-operative day, to obtain better ocular alignment
- Loosening / weakening procedures
Click on any of the following blue hyperlinks for more about Eye Surgery:
- Oculoplastic surgery
- Eyelid surgery
Orbital surgery
Other oculoplastic surgery
- Eyelid surgery
- Surgery involving the lacrimal apparatus
- Eye removal
- Other surgery
LASIK Eye Surgery
YouTube Video of LASIK Eye Surgery Procedure
Pictured Below: LASIK eye surgery: What you can expect (by the Mayo Clinic)
LASIK or Lasik (laser-assisted in situ keratomileusis), commonly referred to as laser eye surgery or laser vision correction, is a type of refractive surgery for the correction of myopia, hyperopia, and astigmatism.
The LASIK surgery is performed by an ophthalmologist who uses a laser or microkeratome to reshape the eye's cornea in order to improve visual acuity. For most people, LASIK provides a long-lasting alternative to eyeglasses or contact lenses.
LASIK is most similar to another surgical corrective procedure, photorefractive keratectomy (PRK), and both represent advances over radial keratotomy in the surgical treatment of refractive errors of vision.
For patients with moderate to high myopia or thin corneas which cannot be treated with LASIK and PRK, the phakic intraocular lens is an alternative. As of 2011, over 11 million LASIK procedures had been performed in the United States and as of 2009 over 28 million have been performed worldwide.
Click on the following blue hyperlinks for more about LASIK Eye Surgery:
The LASIK surgery is performed by an ophthalmologist who uses a laser or microkeratome to reshape the eye's cornea in order to improve visual acuity. For most people, LASIK provides a long-lasting alternative to eyeglasses or contact lenses.
LASIK is most similar to another surgical corrective procedure, photorefractive keratectomy (PRK), and both represent advances over radial keratotomy in the surgical treatment of refractive errors of vision.
For patients with moderate to high myopia or thin corneas which cannot be treated with LASIK and PRK, the phakic intraocular lens is an alternative. As of 2011, over 11 million LASIK procedures had been performed in the United States and as of 2009 over 28 million have been performed worldwide.
Click on the following blue hyperlinks for more about LASIK Eye Surgery:
- Effectiveness
- Risks
- Process
- Wavefront-guided
- Topography-assisted
- History
- Further research
- Comparison to photorefractive keratectomy
Macular Degeneration and its Treatment
YouTube Video Animation: Detecting age-related macular degeneration through a dilated eye exam by the National Eye Institute NIH
Pictured (L) Normal vision; (R) The same view with age-related macular degeneration (National Eye Institute)
Macular degeneration, also known as age-related macular degeneration (AMD or ARMD), is a medical condition which may result in blurred or no vision in the center of the visual field. Early on there are often no symptoms. Over time, however, some people experience a gradual worsening of vision that may affect one or both eyes.
While it does not result in complete blindness, loss of central vision can make it hard to recognize faces, drive, read, or perform other activities of daily life. Visual hallucinations may also occur and these do not represent a mental illness.
Macular degeneration typically occurs in older people. Genetic factors and smoking also play a role. It is due to damage to the macula of the retina. Diagnosis is by a complete eye exam. The severity is divided into early, intermediate, and late types. The late type is additionally divided into "dry" and "wet" forms with the dry form making up 90% of cases.
Prevention includes exercising, eating well, and not smoking. Antioxidant vitamins and minerals do not appear to be useful for prevention. There is no cure or treatment that returns vision already lost. In the wet form, anti-VEGF medication injected into the eye or less commonly laser coagulation or photodynamic therapy may slow worsening. Supplements in those who already have the disease may slow progression.
In 2015 it affected 6.2 million people globally. In 2013 it was the fourth most common cause of blindness after cataracts, preterm birth, and glaucoma. It most commonly occurs in people over the age of fifty and in the United States is the most common cause of vision loss in this age group. About 0.4% of people between 50 and 60 have the disease, while it occurs in 0.7% of people 60 to 70, 2.3% of those 70 to 80, and nearly 12% of people over 80 years old.
Signs and symptoms of macular degeneration include:
Visual symptoms:
Macular degeneration by itself will not lead to total blindness. For that matter, only a very small number of people with visual impairment are totally blind. In almost all cases, some vision remains, mainly peripheral. Other complicating conditions may possibly lead to such an acute condition (severe stroke or trauma, untreated glaucoma, etc.), but few macular degeneration patients experience total visual loss.
The area of the macula comprises only about 2.1% of the retina, and the remaining 97.9% (the peripheral field) remains unaffected by the disease. Even though the macula provides such a small fraction of the visual field, almost half of the visual cortex is devoted to processing macular information.
The loss of central vision profoundly affects visual functioning. It is quite difficult, for example, to read without central vision. Pictures that attempt to depict the central visual loss of macular degeneration with a black spot do not really do justice to the devastating nature of the visual loss. This can be demonstrated by printing letters six inches high on a piece of paper and attempting to identify them while looking straight ahead and holding the paper slightly to the side. Most people find this difficult to do.
Risk Factors:
Environment and lifestyle:
Genetics:
Recurrence ratios for siblings of an affected individual are three- to sixfold higher than in the general population. Genetic linkage analysis has identified 5 sets of gene variants at three locations on different chromosomes (1, 6 and 10) as explaining at least 50% of the risk.
These genes have roles regulating immune response, inflammatory processes and homeostasis of the retina. Variants of these genes give rise to different kinds of dysfunction in these processes. Over time, this results in accumulation of intracellular and extracellular metabolic debris. This can cause scarring of the retina or breakdown of its vascularization.
Genetic tests are available for some of these gene variations. However, pathogenesis of macular degeneration is a complex interaction between genetics, environment and lifestyle, and presence of unfavorable genetic factors doesn't necessarily predict progression to disease.
The three loci where identified gene variants are found are designated:
Specific genes:
Mitochondrial related gene polymorphisms such as that in the MT-ND2 molecule, predicts wet AMD.
Click on any of the following blue hyperlinks for more about Macular Degeneration:
While it does not result in complete blindness, loss of central vision can make it hard to recognize faces, drive, read, or perform other activities of daily life. Visual hallucinations may also occur and these do not represent a mental illness.
Macular degeneration typically occurs in older people. Genetic factors and smoking also play a role. It is due to damage to the macula of the retina. Diagnosis is by a complete eye exam. The severity is divided into early, intermediate, and late types. The late type is additionally divided into "dry" and "wet" forms with the dry form making up 90% of cases.
Prevention includes exercising, eating well, and not smoking. Antioxidant vitamins and minerals do not appear to be useful for prevention. There is no cure or treatment that returns vision already lost. In the wet form, anti-VEGF medication injected into the eye or less commonly laser coagulation or photodynamic therapy may slow worsening. Supplements in those who already have the disease may slow progression.
In 2015 it affected 6.2 million people globally. In 2013 it was the fourth most common cause of blindness after cataracts, preterm birth, and glaucoma. It most commonly occurs in people over the age of fifty and in the United States is the most common cause of vision loss in this age group. About 0.4% of people between 50 and 60 have the disease, while it occurs in 0.7% of people 60 to 70, 2.3% of those 70 to 80, and nearly 12% of people over 80 years old.
Signs and symptoms of macular degeneration include:
Visual symptoms:
- Distorted vision in the form of metamorphopsia, in which a grid of straight lines appears wavy and parts of the grid may appear blank: Patients often first notice this when looking at things like miniblinds in their home or telephone poles while driving. There may also be central scotomas, shadows or missing areas of vision
- Slow recovery of visual function after exposure to bright light (photostress test)
- Visual acuity drastically decreasing (two levels or more), e.g.: 20/20 to 20/80
- Blurred vision: Those with nonexudative macular degeneration may be asymptomatic or notice a gradual loss of central vision, whereas those with exudative macular degeneration often notice a rapid onset of vision loss (often caused by leakage and bleeding of abnormal blood vessels).
- Trouble discerning colors, specifically dark ones from dark ones and light ones from light ones
- A loss in contrast sensitivity
Macular degeneration by itself will not lead to total blindness. For that matter, only a very small number of people with visual impairment are totally blind. In almost all cases, some vision remains, mainly peripheral. Other complicating conditions may possibly lead to such an acute condition (severe stroke or trauma, untreated glaucoma, etc.), but few macular degeneration patients experience total visual loss.
The area of the macula comprises only about 2.1% of the retina, and the remaining 97.9% (the peripheral field) remains unaffected by the disease. Even though the macula provides such a small fraction of the visual field, almost half of the visual cortex is devoted to processing macular information.
The loss of central vision profoundly affects visual functioning. It is quite difficult, for example, to read without central vision. Pictures that attempt to depict the central visual loss of macular degeneration with a black spot do not really do justice to the devastating nature of the visual loss. This can be demonstrated by printing letters six inches high on a piece of paper and attempting to identify them while looking straight ahead and holding the paper slightly to the side. Most people find this difficult to do.
Risk Factors:
- Aging: Advanced age is the strongest predictor of AMD, particularly over 50.[9]
- Family history:
Environment and lifestyle:
- Smoking: Smoking tobacco increases the risk of AMD by two to three times that of someone who has never smoked, and may be the most important modifiable factor in its prevention. A review of previous studies found "a strong association between current smoking and AMD. ... Cigarette smoking is likely to have toxic effects on the retina."
- Hypertension (high blood pressure): In the ALIENOR study 2013, early and late AMD were not significantly associated with systolic or diastolic BP, hypertension, or use of antihypertensive medications, but elevated pulse pressure ((PP) systolic BP minus diastolic BP) was significantly associated with an increased risk of late AMD.
- Atherosclerosis:
- High cholesterol: Elevated cholesterol may increase the risk of AMD.
- Obesity: Abdominal obesity is a risk factor, especially among men.
- Fat intake: Consuming high amounts of certain fats including saturated fats, trans fats and omega-6 fatty acids likely contributes to AMD, while monounsaturated fats are potentially protective. In particular, ω-3 fatty acids may decrease the risk of AMD.
- Exposure to sunlight, especially blue light: Evidence is conflicting as to whether exposure to sunlight contributes to the development of macular degeneration. A recent study on 446 subjects found it does not. Other research, however, has shown high-energy visible light may contribute to AMD.
Genetics:
Recurrence ratios for siblings of an affected individual are three- to sixfold higher than in the general population. Genetic linkage analysis has identified 5 sets of gene variants at three locations on different chromosomes (1, 6 and 10) as explaining at least 50% of the risk.
These genes have roles regulating immune response, inflammatory processes and homeostasis of the retina. Variants of these genes give rise to different kinds of dysfunction in these processes. Over time, this results in accumulation of intracellular and extracellular metabolic debris. This can cause scarring of the retina or breakdown of its vascularization.
Genetic tests are available for some of these gene variations. However, pathogenesis of macular degeneration is a complex interaction between genetics, environment and lifestyle, and presence of unfavorable genetic factors doesn't necessarily predict progression to disease.
The three loci where identified gene variants are found are designated:
- Complement Factor H (CFH) on chromosome 1 at location 1q31.3
- HTRA serine peptidase 1/Age Related Maculopathy Susceptibility 2 (HTRA1/ARMS2) on chromosome 10 at location 10q26
- Complement Factor B/Complement Component 2 (CFB/CC2) on chromosome 6 at 6p21.3
Specific genes:
- Polymorphisms in genes for complement system proteins: The genes for the complement system proteins factor H (CFH), factor B (CFB) and factor 3 (C3) are strongly associated with a person's risk for developing AMD. CFH is involved in inhibiting the inflammatory response. The mutation in CFH (Y402H) results in reduced ability of CFH to regulate complement on critical surfaces such as the retina and leads to increased inflammatory response within the macula. Absence of the complement factor H-related genes R3 and R1 protects against AMD. Two independent studies in 2007 showed a certain common mutation Arg80Gly in the C3 gene, which is a central protein of the complement system, is strongly associated with the occurrence of AMD. The authors of both papers consider their study to underscore the influence of the complement pathway in the pathogenesis of this disease.
- In two 2006 studies, another gene that has implications for the disease, called HTRA1 (encoding a secreted serine protease), was identified.
- Six mutations of the gene SERPING1 (Serpin Peptidase Inhibitor, Clade G (C1 Inhibitor), Member 1) are associated with AMD. Mutations in this gene can also cause hereditary angioedema.
- Fibulin-5 mutation: Rare forms of the disease are caused by genetic defects in fibulin-5, in an autosomal dominant manner. In 2004, Stone et al. performed a screen on 402 AMD patients and revealed a statistically significant correlation between mutations in fibulin-5 and incidence of the disease.
Mitochondrial related gene polymorphisms such as that in the MT-ND2 molecule, predicts wet AMD.
Click on any of the following blue hyperlinks for more about Macular Degeneration:
- Pathophysiology
- Stages
Oxidative stress
- Stages
- Diagnosis
- Prevention
- Management
- Dry AMD
Wet AMD
Adaptive devices
- Dry AMD
- Epidemiology
- Research directions
- Other types
- Notable cases
- See also:
Gastric Bypass Surgery as a surgical means for reducing hunger for curing obesity
YouTube Video: Gastric Bypass Surgery Procedure (Animation)
Pictured: a Diagram of a Gastric Bypass, Courtesy of Lina Wolf - Own work, CC BY-SA 3.0
Gastric bypass surgery refers to a surgical procedure in which the stomach is divided into a small upper pouch and a much larger lower "remnant" pouch and then the small intestine is rearranged to connect to both.
Surgeons have developed several different ways to reconnect the intestine, thus leading to several different gastric bypass (GBP) procedures. Any GBP leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food.
The operation is prescribed to treat morbid obesity (defined as a body mass index greater than 40), type 2 diabetes, hypertension, sleep apnea, and other comorbid conditions.
Bariatric surgery is the term encompassing allof the surgical treatments for morbid obesity, not just gastric bypasses, which make up only one class of such operations. The resulting weight loss, typically dramatic, markedly reduces comorbidities.
The long-term mortality rate of gastric bypass patients has been shown to be reduced by up to 40%. As with all surgery, complications may occur. A study from 2005 to 2006 revealed that 15% of patients experience complications as a result of gastric bypass, and 0.5% of patients died within six months of surgery due to complications.
Uses:
Gastric bypass is indicated for the surgical treatment of morbid obesity, a diagnosis which is made when the patient is seriously obese, has been unable to achieve satisfactory and sustained weight loss by dietary efforts, and suffers from comorbid conditions which are either life-threatening or a serious impairment to the quality of life.
Prior to 1991, clinicians interpreted serious obesity as weighing at least 100 pounds (45 kg) more than the "ideal body weight", an actuarially-determined body-weight at which one was estimated to be likely to live the longest, as determined by the life-insurance industry. This criterion failed for persons of short stature.
In 1991, the National Institutes of Health (NIH) sponsored a consensus panel whose recommendations have set the current standard for consideration of surgical treatment, the body mass index (BMI). The BMI is defined as the body weight (in kilograms), divided by the square of the height (in meters). The result is expressed as a number in units of kilograms per square meter.
In healthy adults, BMI ranges from 18.5 to 24.9, with a BMI above 30 being considered obese, and a BMI less than 18.5 considered underweight. (BMI is by itself not a reliable index of obesity: serious bodybuilders or strength athletes have BMIs in the obesity range while having relatively little body fat.)
The Consensus Panel of the National Institutes of Health (NIH) recommended the following criteria for consideration of bariatric surgery, including gastric bypass procedures:
The Consensus Panel also emphasized the necessity of multidisciplinary care of the bariatric surgical patient by a team of physicians and therapists to manage associated comorbidities and nutrition, physical activity, behavior, and psychological needs. The surgical procedure is best regarded as a tool which enables the patient to alter lifestyle and eating habits, and to achieve effective and permanent management of obesity and eating behavior.
Since 1991, major developments in the field of bariatric surgery, particularly laparoscopy, have outdated some of the conclusions of the NIH panel. In 2004 the American Society for Bariatric Surgery (ASBS) sponsored a consensus conference which updated the evidence and the conclusions of the NIH panel. This conference, composed of physicians and scientists of both surgical and non-surgical disciplines, reached several conclusions, including:
Click on any of the following blue hyperlinks for more about Gastric Bypass Surgery:
Surgeons have developed several different ways to reconnect the intestine, thus leading to several different gastric bypass (GBP) procedures. Any GBP leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food.
The operation is prescribed to treat morbid obesity (defined as a body mass index greater than 40), type 2 diabetes, hypertension, sleep apnea, and other comorbid conditions.
Bariatric surgery is the term encompassing allof the surgical treatments for morbid obesity, not just gastric bypasses, which make up only one class of such operations. The resulting weight loss, typically dramatic, markedly reduces comorbidities.
The long-term mortality rate of gastric bypass patients has been shown to be reduced by up to 40%. As with all surgery, complications may occur. A study from 2005 to 2006 revealed that 15% of patients experience complications as a result of gastric bypass, and 0.5% of patients died within six months of surgery due to complications.
Uses:
Gastric bypass is indicated for the surgical treatment of morbid obesity, a diagnosis which is made when the patient is seriously obese, has been unable to achieve satisfactory and sustained weight loss by dietary efforts, and suffers from comorbid conditions which are either life-threatening or a serious impairment to the quality of life.
Prior to 1991, clinicians interpreted serious obesity as weighing at least 100 pounds (45 kg) more than the "ideal body weight", an actuarially-determined body-weight at which one was estimated to be likely to live the longest, as determined by the life-insurance industry. This criterion failed for persons of short stature.
In 1991, the National Institutes of Health (NIH) sponsored a consensus panel whose recommendations have set the current standard for consideration of surgical treatment, the body mass index (BMI). The BMI is defined as the body weight (in kilograms), divided by the square of the height (in meters). The result is expressed as a number in units of kilograms per square meter.
In healthy adults, BMI ranges from 18.5 to 24.9, with a BMI above 30 being considered obese, and a BMI less than 18.5 considered underweight. (BMI is by itself not a reliable index of obesity: serious bodybuilders or strength athletes have BMIs in the obesity range while having relatively little body fat.)
The Consensus Panel of the National Institutes of Health (NIH) recommended the following criteria for consideration of bariatric surgery, including gastric bypass procedures:
- people who have a BMI of 40 or higher
- people with a BMI of 35 or higher with one or more related comorbid conditions
The Consensus Panel also emphasized the necessity of multidisciplinary care of the bariatric surgical patient by a team of physicians and therapists to manage associated comorbidities and nutrition, physical activity, behavior, and psychological needs. The surgical procedure is best regarded as a tool which enables the patient to alter lifestyle and eating habits, and to achieve effective and permanent management of obesity and eating behavior.
Since 1991, major developments in the field of bariatric surgery, particularly laparoscopy, have outdated some of the conclusions of the NIH panel. In 2004 the American Society for Bariatric Surgery (ASBS) sponsored a consensus conference which updated the evidence and the conclusions of the NIH panel. This conference, composed of physicians and scientists of both surgical and non-surgical disciplines, reached several conclusions, including:
- bariatric surgery is the most effective treatment for morbid obesity
- gastric bypass is one of four types of operations for morbid obesity
- laparoscopic surgery is equally effective and as safe as open surgery
- patients should undergo comprehensive preoperative evaluation and have multi-disciplinary support for optimum outcome
Click on any of the following blue hyperlinks for more about Gastric Bypass Surgery:
- Surgical techniques
- Physiology
- Complications
- Results and health benefits of gastric bypass
- Cost of gastric bypass
- Living with gastric bypass
- Surgeon accreditation
- See also:
- Adjustable gastric banding surgery
- Duodenal Switch surgery
- Roux-en-Y anastomosis
- Vagotomy—Cutting of the vagus nerve to reduce the feeling of hunger
- StomaphyX—Revisional, natural orifice procedure for patients that have regained weight after gastric bypass
- American Society for Bariatric Surgery
- ASBS Consensus Conference Statement – 2004
- NIH – Gastrointestinal Surgery for Obesity
- NIH Medline Plus – Multiple Links to articles, videos about bariatric surgery
- Metabolic & Weight Loss Surgical Procedures Gallery - Including information on bariatric surgery
Diseases that have been eliminated from the United States
YouTube Video: Eradicating Polio: Reaching the Last Child by Harvard University
Pictured: Impact of diseases which have since been eradicated from the United States: (L) Small Pox, (C) Yellow Fever and (R) Malaria
This is a list of diseases known (or declared) to have been eliminated from the United States, either permanently or at one time.
Most of the diseases listed were eliminated after coordinated public health campaigns. (Since some diseases can be eliminated and then reintroduced at a later time, such diseases are still eligible for the list, but with the fact of reintroduction noted.) Some entries are based on formal public health declarations, others are based on reliable information in the medical or public health literature.
Since some diseases can be eliminated, but subsequently reimported without transmitting additional endemic cases, these are noted in a dedicated column. Although no fixed rule always applies, many infectious diseases (e.g., measles) are considered eliminated when no cases have been reported to public health authorities for at least 12 months.
(NB: In recent years, "elimination" is the preferred term for "regional eradication" of a disease; the term "eradication" is reserved for the reduction of an infectious disease's global prevalence to zero.)
Click on any of the following blue hyperlinks for a list of diseases eradicated in the United States:
Possible Future Eradications:
Various public health projects are ongoing with a goal of eliminating diseases from the country. Note that several infectious diseases in the United States, not on the above list, are considered close to elimination (98-99% reductions): e.g.,
Other disease pathogens (e.g., those of anthrax and rabies) have been almost entirely eliminated from humans in the US, but remain as hazards in the environment and so cannot accurately be described as eliminated.
The stated goal of "eradication" of hookworm from the southeast US (1915-20) was not achieved, although the hookworm-infection rate of that region did drop by more than half:
Most of the diseases listed were eliminated after coordinated public health campaigns. (Since some diseases can be eliminated and then reintroduced at a later time, such diseases are still eligible for the list, but with the fact of reintroduction noted.) Some entries are based on formal public health declarations, others are based on reliable information in the medical or public health literature.
Since some diseases can be eliminated, but subsequently reimported without transmitting additional endemic cases, these are noted in a dedicated column. Although no fixed rule always applies, many infectious diseases (e.g., measles) are considered eliminated when no cases have been reported to public health authorities for at least 12 months.
(NB: In recent years, "elimination" is the preferred term for "regional eradication" of a disease; the term "eradication" is reserved for the reduction of an infectious disease's global prevalence to zero.)
Click on any of the following blue hyperlinks for a list of diseases eradicated in the United States:
- Yellow fever
- Smallpox
- Babesia bovis babesiosis (Cattle disease; occasionally infects humans)
- Malaria (See National Malaria Eradication Program)
- Poliomyelitis ( see Poliomyelitis eradication)
- Measles After widespread national vaccination efforts.
- Diphtheria (After widespread national vaccination efforts.)
Possible Future Eradications:
Various public health projects are ongoing with a goal of eliminating diseases from the country. Note that several infectious diseases in the United States, not on the above list, are considered close to elimination (98-99% reductions): e.g.,
Other disease pathogens (e.g., those of anthrax and rabies) have been almost entirely eliminated from humans in the US, but remain as hazards in the environment and so cannot accurately be described as eliminated.
The stated goal of "eradication" of hookworm from the southeast US (1915-20) was not achieved, although the hookworm-infection rate of that region did drop by more than half:
- In 1954, Congressional funds were first approved for a Cooperative State-Federal Brucellosis Eradication Program to eliminate the disease from the country. (Brucellosis is a problem mainly in livestock. In 1956, there were 124,000 affected herds found by testing in the US. By 1992, the number had dropped to 700 herds and the number of affected, domestic herds has declined to single digits since then.)
- The CDC Division of TB Elimination has a goal of controlling tuberculosis and eliminating it from the United States by minimizing the likelihood of Mycobacterium tuberculosis transmission, which will prevent the occurrence of new cases.
- The Oral Rabies Vaccine (ORV) Program has a goal of preventing the spread of raccoon variant rabies and eventually eliminating it from the United States.
- There has been an effort for several years to eliminate syphilis from the US. The rate of infection decreased through the 1990s, and in 2000 it was the lowest since reporting began in 1941, leading the US Surgeon General to issue a plan to eliminate the disease from the country. It has been staging a comeback, however, increasing each year since 2001.
Jonas Salk
YouTube Video about Jonas Salk and the Polio Vaccine
Pictured: Jonas Salk on the cover of Time Magazine, March 29, 1954
Jonas Edward Salk (October 28, 1914 – June 23, 1995) was an American medical researcher and virologist. He discovered and developed one of the first successful polio vaccines.
Born in New York City, he attended New York University School of Medicine, later choosing to do medical research instead of becoming a practicing physician. In 1939, after earning his medical degree, Salk began an internship as a physician scientist at Mount Sinai Hospital.
Two years later he was granted a fellowship at the University of Michigan, where he would study flu viruses with his mentor Thomas Francis, Jr..
Until 1955, when the Salk vaccine was introduced, polio was considered one of the most frightening public health problems in the world. In the postwar United States, annual epidemics were increasingly devastating.
The 1952 U.S. epidemic was the worst outbreak in the nation's history. Of nearly 58,000 cases reported that year, 3,145 people died and 21,269 were left with mild to disabling paralysis, with most of its victims being children. The "public reaction was to a plague", said historian William L. O'Neill. "Citizens of urban areas were to be terrified every summer when this frightful visitor returned."
According to a 2009 PBS documentary, "Apart from the atomic bomb, America's greatest fear was polio." As a result, scientists were in a frantic race to find a way to prevent or cure the disease. In 1938, U.S. President Franklin D. Roosevelt, the world's most recognized victim of the disease, had founded the National Foundation for Infantile Paralysis (known as March of Dimes Foundation since 2007), an organization that would fund the development of a vaccine.
In 1947, Salk accepted an appointment to the University of Pittsburgh School of Medicine. In 1948, he undertook a project funded by the National Foundation for Infantile Paralysis to determine the number of different types of polio virus. Salk saw an opportunity to extend this project towards developing a vaccine against polio, and, together with the skilled research team he assembled, devoted himself to this work for the next seven years.
The field trial set up to test the Salk vaccine was, according to O'Neill, "the most elaborate program of its kind in history, involving 20,000 physicians and public health officers, 64,000 school personnel, and 220,000 volunteers." Over 1,800,000 school children took part in the trial.
When news of the vaccine's success was made public on April 12, 1955, Salk was hailed as a "miracle worker" and the day almost became a national holiday. Around the world, an immediate rush to vaccinate began, with countries including Canada, Sweden, Denmark, Norway, West Germany, the Netherlands, Switzerland, and Belgium planning to begin polio immunization campaigns using Salk's vaccine.
Salk campaigned for mandatory vaccination, claiming that public health should be considered a "moral commitment." His sole focus had been to develop a safe and effective vaccine as rapidly as possible, with no interest in personal profit. When asked who owned the patent to it, Salk said, "Well, the people I would say. There is no patent. Could you patent the sun?"
In 1960, he founded the Salk Institute for Biological Studies in La Jolla, California, which is today a center for medical and scientific research. He continued to conduct research and publish books, including Man Unfolding (1972), The Survival of the Wisest (1973), World Population and Human Values: A New Reality (1981), and Anatomy of Reality: Merging of Intuition and Reason (1983). Salk's last years were spent searching for a vaccine against HIV. His personal papers are stored at the University of California, San Diego Library.
Click here for more about Jonas Salk.
Born in New York City, he attended New York University School of Medicine, later choosing to do medical research instead of becoming a practicing physician. In 1939, after earning his medical degree, Salk began an internship as a physician scientist at Mount Sinai Hospital.
Two years later he was granted a fellowship at the University of Michigan, where he would study flu viruses with his mentor Thomas Francis, Jr..
Until 1955, when the Salk vaccine was introduced, polio was considered one of the most frightening public health problems in the world. In the postwar United States, annual epidemics were increasingly devastating.
The 1952 U.S. epidemic was the worst outbreak in the nation's history. Of nearly 58,000 cases reported that year, 3,145 people died and 21,269 were left with mild to disabling paralysis, with most of its victims being children. The "public reaction was to a plague", said historian William L. O'Neill. "Citizens of urban areas were to be terrified every summer when this frightful visitor returned."
According to a 2009 PBS documentary, "Apart from the atomic bomb, America's greatest fear was polio." As a result, scientists were in a frantic race to find a way to prevent or cure the disease. In 1938, U.S. President Franklin D. Roosevelt, the world's most recognized victim of the disease, had founded the National Foundation for Infantile Paralysis (known as March of Dimes Foundation since 2007), an organization that would fund the development of a vaccine.
In 1947, Salk accepted an appointment to the University of Pittsburgh School of Medicine. In 1948, he undertook a project funded by the National Foundation for Infantile Paralysis to determine the number of different types of polio virus. Salk saw an opportunity to extend this project towards developing a vaccine against polio, and, together with the skilled research team he assembled, devoted himself to this work for the next seven years.
The field trial set up to test the Salk vaccine was, according to O'Neill, "the most elaborate program of its kind in history, involving 20,000 physicians and public health officers, 64,000 school personnel, and 220,000 volunteers." Over 1,800,000 school children took part in the trial.
When news of the vaccine's success was made public on April 12, 1955, Salk was hailed as a "miracle worker" and the day almost became a national holiday. Around the world, an immediate rush to vaccinate began, with countries including Canada, Sweden, Denmark, Norway, West Germany, the Netherlands, Switzerland, and Belgium planning to begin polio immunization campaigns using Salk's vaccine.
Salk campaigned for mandatory vaccination, claiming that public health should be considered a "moral commitment." His sole focus had been to develop a safe and effective vaccine as rapidly as possible, with no interest in personal profit. When asked who owned the patent to it, Salk said, "Well, the people I would say. There is no patent. Could you patent the sun?"
In 1960, he founded the Salk Institute for Biological Studies in La Jolla, California, which is today a center for medical and scientific research. He continued to conduct research and publish books, including Man Unfolding (1972), The Survival of the Wisest (1973), World Population and Human Values: A New Reality (1981), and Anatomy of Reality: Merging of Intuition and Reason (1983). Salk's last years were spent searching for a vaccine against HIV. His personal papers are stored at the University of California, San Diego Library.
Click here for more about Jonas Salk.
Nanomedicine
YouTube Video: Nanomedicines -- The way of the future?
Pictured: what are the differences between nanomedicine and common medicine?
Nanomedicine is the medical application of nanotechnology. Nanomedicine ranges from the medical applications of nanomaterials and biological devices, to nanoelectronic biosensors, and even possible future applications of molecular nanotechnology such as biological machines.
Current problems for nanomedicine involve understanding the issues related to toxicity and environmental impact of nanoscale materials (materials whose structure is on the scale of nanometers, i.e. billionths of a meter).
Functionalities can be added to nanomaterials by interfacing them with biological molecules or structures. The size of nanomaterials is similar to that of most biological molecules and structures; therefore, nanomaterials can be useful for both in vivo and in vitro biomedical research and applications.
Thus far, the integration of nanomaterials with biology has led to the development of diagnostic devices, contrast agents, analytical tools, physical therapy applications, and drug delivery vehicles.
Nanomedicine seeks to deliver a valuable set of research tools and clinically useful devices in the near future. The National Nanotechnology Initiative expects new commercial applications in the pharmaceutical industry that may include advanced drug delivery systems, new therapies, and in vivo imaging. Nanomedicine research is receiving funding from the US National Institutes of Health Common Fund program, supporting four nanomedicine development centers.
Nanomedicine sales reached $16 billion in 2015, with a minimum of $3.8 billion in nanotechnology R&D being invested every year. Global funding for emerging nanotechnology increased by 45% per year in recent years, with product sales exceeding $1 trillion in 2013. As the nanomedicine industry continues to grow, it is expected to have a significant impact on the economy.
Drug Delivery:
Nanotechnology has provided the possibility of delivering drugs to specific cells using nanoparticles. The overall drug consumption and side-effects may be lowered significantly by depositing the active agent in the morbid region only and in no higher dose than needed.
Targeted drug delivery is intended to reduce the side effects of drugs with concomitant decreases in consumption and treatment expenses. Drug delivery focuses on maximizing bioavailability, both at specific places in the body and over a period of time.
This can potentially be achieved by molecular targeting by nanoengineered devices. A benefit of using nanoscale for medical technologies is that smaller devices are less invasive and can possibly be implanted inside the body, plus biochemical reaction times are much shorter.
These devices are faster and more sensitive than typical drug delivery. The efficacy of drug delivery through nanomedicine is largely based upon: a) efficient encapsulation of the drugs, b) successful delivery of drug to the targeted region of the body, and c) successful release of the drug.
Drug delivery systems, lipid- or polymer-based nanoparticles, can be designed to improve the pharmacokinetics and biodistribution of the drug. However, the pharmacokinetics and pharmacodynamics of nanomedicine is highly variable among different patients. When designed to avoid the body's defence mechanisms, nanoparticles have beneficial properties that can be used to improve drug delivery.
Complex drug delivery mechanisms are being developed, including the ability to get drugs through cell membranes and into cell cytoplasm. Triggered response is one way for drug molecules to be used more efficiently. Drugs are placed in the body and only activate on encountering a particular signal. For example, a drug with poor solubility will be replaced by a drug delivery system where both hydrophilic and hydrophobic environments exist, improving the solubility.
Drug delivery systems may also be able to prevent tissue damage through regulated drug release; reduce drug clearance rates; or lower the volume of distribution and reduce the effect on non-target tissue. However, the biodistribution of these nanoparticles is still imperfect due to the complex host's reactions to nano- and microsized materials and the difficulty in targeting specific organs in the body.
Nevertheless, a lot of work is still ongoing to optimize and better understand the potential and limitations of nanoparticulate systems. While advancement of research proves that targeting and distribution can be augmented by nanoparticles, the dangers of nanotoxicity become an important next step in further understanding of their medical uses.
Nanoparticles are under research for their potential to decrease antibiotic resistance or for various antimicrobial uses. Nanoparticles might also used to circumvent multidrug resistance (MDR) mechanisms.
Systems under research:
Two forms of nanomedicine that have already been tested in mice and are awaiting human testing will use gold nanoshells to help diagnose and treat cancer, along with liposomes as vaccine adjuvants and drug transport vehicles.
Similarly, drug detoxification is also another application for nanomedicine which has shown promising results in rats. Advances in Lipid nanotechnology was also instrumental in engineering medical nanodevices and novel drug delivery systems as well as in developing sensing applications. Another example can be found in dendrimers and nanoporous materials. Another example is to use block co-polymers, which form micelles for drug encapsulation.
Polymeric nanoparticles are a competing technology to lipidic (based mainly on Phospholipids) nanoparticles. There is an additional risk of toxicity associated with polymers not widely studied or understood. The major advantages of polymers is stability, lower cost and predictable characterization. However, in the patient's body this very stability (slow degradation) is a negative factor.
Phospholipids on the other hand are membrane lipids (already present in the body and surrounding each cell), have a GRAS (Generally Recognised As Safe) status from FDA and are derived from natural sources without any complex chemistry involved. They are not metabolised but rather absorbed by the body and the degradation products are themselves nutrients (fats or micronutrients).
Protein and peptides exert multiple biological actions in the human body and they have been identified as showing great promise for treatment of various diseases and disorders. These macromolecules are called biopharmaceuticals. Targeted and/or controlled delivery of these biopharmaceuticals using nanomaterials like nanoparticles and Dendrimers is an emerging field called nanobiopharmaceutics, and these products are called nanobiopharmaceuticals.
Another highly efficient system for microRNA delivery for example are nanoparticles formed by the self-assembly of two different microRNAs deregulated in cancer.
Another vision is based on small electromechanical systems; nanoelectromechanical systems are being investigated for the active release of drugs. Some potentially important applications include cancer treatment with iron nanoparticles or gold shells.
Nanotechnology is also opening up new opportunities in implantable delivery systems, which are often preferable to the use of injectable drugs, because the latter frequently display first-order kinetics (the blood concentration goes up rapidly, but drops exponentially over time).
This rapid rise may cause difficulties with toxicity, and drug efficacy can diminish as the drug concentration falls below the targeted range.
Applications:
Some nanotechnology-based drugs that are commercially available or in human clinical trials include:
Cancer:
Existing and potential drug nanocarriers have been reviewed.
Nanoparticles have high surface area to volume ratio. This allows for many functional groups to be attached to a nanoparticle, which can seek out and bind to certain tumor cells. Additionally, the small size of nanoparticles (10 to 100 nanometers), allows them to preferentially accumulate at tumor sites (because tumors lack an effective lymphatic drainage system). Limitations to conventional cancer chemotherapy include drug resistance, lack of selectivity, and lack of solubility. Nanoparticles have the potential to overcome these problems.
In photodynamic therapy, a particle is placed within the body and is illuminated with light from the outside. The light gets absorbed by the particle and if the particle is metal, energy from the light will heat the particle and surrounding tissue.
Light may also be used to produce high energy oxygen molecules which will chemically react with and destroy most organic molecules that are next to them (like tumors). This therapy is appealing for many reasons. It does not leave a "toxic trail" of reactive molecules throughout the body (chemotherapy) because it is directed where only the light is shined and the particles exist.
Photodynamic therapy has potential for a noninvasive procedure for dealing with diseases, growth and tumors. Kanzius RF therapy is one example of such therapy (nanoparticle hyperthermia) . Also, gold nanoparticles have the potential to join numerous therapeutic functions into a single platform, by targeting specific tumor cells, tissues and organs.
Imaging:
In vivo imaging is another area where tools and devices are being developed. Using nanoparticle contrast agents, images such as ultrasound and MRI have a favorable distribution and improved contrast. In cardiovascular imaging, nanoparticles have potential to aid visualization of blood pooling, ischemia, angiogenesis, atherosclerosis, and focal areas where inflammation is present.
The small size of nanoparticles endows them with properties that can be very useful in oncology, particularly in imaging. Quantum dots (nanoparticles with quantum confinement properties, such as size-tunable light emission), when used in conjunction with MRI (magnetic resonance imaging), can produce exceptional images of tumor sites.
Nanoparticles of cadmium selenide (quantum dots) glow when exposed to ultraviolet light. When injected, they seep into cancer tumors. The surgeon can see the glowing tumor, and use it as a guide for more accurate tumor removal.These nanoparticles are much brighter than organic dyes and only need one light source for excitation.
This means that the use of fluorescent quantum dots could produce a higher contrast image and at a lower cost than today's organic dyes used as contrast media. The downside, however, is that quantum dots are usually made of quite toxic elements, but this concern may be addressed by use of fluorescent dopants.
Tracking movement can help determine how well drugs are being distributed or how substances are metabolized. It is difficult to track a small group of cells throughout the body, so scientists used to dye the cells. These dyes needed to be excited by light of a certain wavelength in order for them to light up.
While different color dyes absorb different frequencies of light, there was a need for as many light sources as cells. A way around this problem is with luminescent tags. These tags are quantum dots attached to proteins that penetrate cell membranes. The dots can be random in size, can be made of bio-inert material, and they demonstrate the nanoscale property that color is size-dependent.
As a result, sizes are selected so that the frequency of light used to make a group of quantum dots fluoresce is an even multiple of the frequency required to make another group incandesce. Then both groups can be lit with a single light source. They have also found a way to insert nanoparticles into the affected parts of the body so that those parts of the body will glow showing the tumor growth or shrinkage or also organ trouble.
Sensing:
Main article: Nanosensor
Nanotechnology-on-a-chip is one more dimension of lab-on-a-chip technology. Magnetic nanoparticles, bound to a suitable antibody, are used to label specific molecules, structures or microorganisms. Gold nanoparticles tagged with short segments of DNA can be used for detection of genetic sequence in a sample.
Multicolor optical coding for biological assays has been achieved by embedding different-sized quantum dots into polymeric microbeads. Nanopore technology for analysis of nucleic acids converts strings of nucleotides directly into electronic signatures.
Sensor test chips containing thousands of nanowires, able to detect proteins and other biomarkers left behind by cancer cells, could enable the detection and diagnosis of cancer in the early stages from a few drops of a patient's blood. Nanotechnology is helping to advance the use of arthroscopes, which are pencil-sized devices that are used in surgeries with lights and cameras so surgeons can do the surgeries with smaller incisions. The smaller the incisions the faster the healing time which is better for the patients. It is also helping to find a way to make an arthroscope smaller than a strand of hair.
Research on nanoelectronics-based cancer diagnostics could lead to tests that can be done in pharmacies. The results promise to be highly accurate and the product promises to be inexpensive. They could take a very small amount of blood and detect cancer anywhere in the body in about five minutes, with a sensitivity that is a thousand times better than in a conventional laboratory test.
These devices that are built with nanowires to detect cancer proteins; each nanowire detector is primed to be sensitive to a different cancer marker. The biggest advantage of the nanowire detectors is that they could test for anywhere from ten to one hundred similar medical conditions without adding cost to the testing device.
Nanotechnology has also helped to personalize oncology for the detection, diagnosis, and treatment of cancer. It is now able to be tailored to each individual’s tumor for better performance. They have found ways that they will be able to target a specific part of the body that is being affected by cancer.
Blood purification:
Magnetic micro particles are proven research instruments for the separation of cells and proteins from complex media. The technology is available under the name Magnetic-activated cell sorting or Dynabeads among others.
More recently it was shown in animal models that magnetic nanoparticles can be used for the removal of various noxious compounds including toxins, pathogens, and proteins from whole blood in an extracorporeal circuit similar to dialysis.
In contrast to dialysis, which works on the principle of the size related diffusion of solutes and ultrafiltration of fluid across a semi-permeable membrane, the purification with nanoparticles allows specific targeting of substances. Additionally larger compounds which are commonly not dialyzable can be removed.
The purification process is based on functionalized iron oxide or carbon coated metal nanoparticles with ferromagnetic or superparamagnetic properties. Binding agents such as proteins, antibodies, antibiotics, or synthetic ligands are covalently linked to the particle surface. These binding agents are able to interact with target species forming an agglomerate.
Applying an external magnetic field gradient allows exerting a force on the nanoparticles. Hence the particles can be separated from the bulk fluid, thereby cleaning it from the contaminants.
The small size (< 100 nm) and large surface area of functionalized nanomagnets leads to advantageous properties compared to hemoperfusion, which is a clinically used technique for the purification of blood and is based on surface adsorption.
These advantages are high loading and accessibility of the binding agents, high selectivity towards the target compound, fast diffusion, small hydrodynamic resistance, and low dosage.
This approach offers new therapeutic possibilities for the treatment of systemic infections such as sepsis by directly removing the pathogen. It can also be used to selectively remove cytokines or endotoxins or for the dialysis of compounds which are not accessible by traditional dialysis methods. However the technology is still in a preclinical phase and first clinical trials are not expected before 2017.
Tissue engineering:
Nanotechnology may be used as part of tissue engineering to help reproduce or repair or reshape damaged tissue using suitable nanomaterial-based scaffolds and growth factors. Tissue engineering if successful may replace conventional treatments like organ transplants or artificial implants.
Nanoparticles such as graphene, carbon nanotubes, molybdenum disulfide and tungsten disulfide are being used as reinforcing agents to fabricate mechanically strong biodegradable polymeric nanocomposites for bone tissue engineering applications. The addition of these nanoparticles in the polymer matrix at low concentrations (~0.2 weight %) leads to significant improvements in the compressive and flexural mechanical properties of polymeric nanocomposites.
Potentially, these nanocomposites may be used as a novel, mechanically strong, light weight composite as bone implants.
For example, a flesh welder was demonstrated to fuse two pieces of chicken meat into a single piece using a suspension of gold-coated nanoshells activated by an infrared laser. This could be used to weld arteries during surgery. Another example is nanonephrology, the use of nanomedicine on the kidney.
Medical devices:
Neuro-electronic interfacing is a visionary goal dealing with the construction of nanodevices that will permit computers to be joined and linked to the nervous system. This idea requires the building of a molecular structure that will permit control and detection of nerve impulses by an external computer.
A refuelable strategy implies energy is refilled continuously or periodically with external sonic, chemical, tethered, magnetic, or biological electrical sources, while a nonrefuelable strategy implies that all power is drawn from internal energy storage which would stop when all energy is drained.
A nanoscale enzymatic biofuel cell for self-powered nanodevices have been developed that uses glucose from biofluids including human blood and watermelons. One limitation to this innovation is the fact that electrical interference or leakage or overheating from power consumption is possible.
The wiring of the structure is extremely difficult because they must be positioned precisely in the nervous system. The structures that will provide the interface must also be compatible with the body's immune system.
Molecular nanotechnology is a speculative subfield of nanotechnology regarding the possibility of engineering molecular assemblers, machines which could re-order matter at a molecular or atomic scale.
Nanomedicine would make use of these nanorobots, introduced into the body, to repair or detect damages and infections. Molecular nanotechnology is highly theoretical, seeking to anticipate what inventions nanotechnology might yield and to propose an agenda for future inquiry.
The proposed elements of molecular nanotechnology, such as molecular assemblers and nanorobots are far beyond current capabilities. Future advances in nanomedicine could give rise to life extension through the repair of many processes thought to be responsible for aging.
K. Eric Drexler, one of the founders of nanotechnology, postulated cell repair machines, including ones operating within cells and utilizing as yet hypothetical molecular machines, in his 1986 book Engines of Creation, with the first technical discussion of medical nanorobots by Robert Freitas appearing in 1999.
Raymond Kurzweil, a futurist and transhumanist, stated in his book The Singularity Is Near that he believes that advanced medical nanorobotics could completely remedy the effects of aging by 2030.
According to Richard Feynman, it was his former graduate student and collaborator Albert Hibbs who originally suggested to him (circa 1959) the idea of a medical use for Feynman's theoretical micromachines (see nanotechnology). Hibbs suggested that certain repair machines might one day be reduced in size to the point that it would, in theory, be possible to (as Feynman put it) "swallow the doctor". The idea was incorporated into Feynman's 1959 essay There's Plenty of Room at the Bottom.
See Also:
Current problems for nanomedicine involve understanding the issues related to toxicity and environmental impact of nanoscale materials (materials whose structure is on the scale of nanometers, i.e. billionths of a meter).
Functionalities can be added to nanomaterials by interfacing them with biological molecules or structures. The size of nanomaterials is similar to that of most biological molecules and structures; therefore, nanomaterials can be useful for both in vivo and in vitro biomedical research and applications.
Thus far, the integration of nanomaterials with biology has led to the development of diagnostic devices, contrast agents, analytical tools, physical therapy applications, and drug delivery vehicles.
Nanomedicine seeks to deliver a valuable set of research tools and clinically useful devices in the near future. The National Nanotechnology Initiative expects new commercial applications in the pharmaceutical industry that may include advanced drug delivery systems, new therapies, and in vivo imaging. Nanomedicine research is receiving funding from the US National Institutes of Health Common Fund program, supporting four nanomedicine development centers.
Nanomedicine sales reached $16 billion in 2015, with a minimum of $3.8 billion in nanotechnology R&D being invested every year. Global funding for emerging nanotechnology increased by 45% per year in recent years, with product sales exceeding $1 trillion in 2013. As the nanomedicine industry continues to grow, it is expected to have a significant impact on the economy.
Drug Delivery:
Nanotechnology has provided the possibility of delivering drugs to specific cells using nanoparticles. The overall drug consumption and side-effects may be lowered significantly by depositing the active agent in the morbid region only and in no higher dose than needed.
Targeted drug delivery is intended to reduce the side effects of drugs with concomitant decreases in consumption and treatment expenses. Drug delivery focuses on maximizing bioavailability, both at specific places in the body and over a period of time.
This can potentially be achieved by molecular targeting by nanoengineered devices. A benefit of using nanoscale for medical technologies is that smaller devices are less invasive and can possibly be implanted inside the body, plus biochemical reaction times are much shorter.
These devices are faster and more sensitive than typical drug delivery. The efficacy of drug delivery through nanomedicine is largely based upon: a) efficient encapsulation of the drugs, b) successful delivery of drug to the targeted region of the body, and c) successful release of the drug.
Drug delivery systems, lipid- or polymer-based nanoparticles, can be designed to improve the pharmacokinetics and biodistribution of the drug. However, the pharmacokinetics and pharmacodynamics of nanomedicine is highly variable among different patients. When designed to avoid the body's defence mechanisms, nanoparticles have beneficial properties that can be used to improve drug delivery.
Complex drug delivery mechanisms are being developed, including the ability to get drugs through cell membranes and into cell cytoplasm. Triggered response is one way for drug molecules to be used more efficiently. Drugs are placed in the body and only activate on encountering a particular signal. For example, a drug with poor solubility will be replaced by a drug delivery system where both hydrophilic and hydrophobic environments exist, improving the solubility.
Drug delivery systems may also be able to prevent tissue damage through regulated drug release; reduce drug clearance rates; or lower the volume of distribution and reduce the effect on non-target tissue. However, the biodistribution of these nanoparticles is still imperfect due to the complex host's reactions to nano- and microsized materials and the difficulty in targeting specific organs in the body.
Nevertheless, a lot of work is still ongoing to optimize and better understand the potential and limitations of nanoparticulate systems. While advancement of research proves that targeting and distribution can be augmented by nanoparticles, the dangers of nanotoxicity become an important next step in further understanding of their medical uses.
Nanoparticles are under research for their potential to decrease antibiotic resistance or for various antimicrobial uses. Nanoparticles might also used to circumvent multidrug resistance (MDR) mechanisms.
Systems under research:
Two forms of nanomedicine that have already been tested in mice and are awaiting human testing will use gold nanoshells to help diagnose and treat cancer, along with liposomes as vaccine adjuvants and drug transport vehicles.
Similarly, drug detoxification is also another application for nanomedicine which has shown promising results in rats. Advances in Lipid nanotechnology was also instrumental in engineering medical nanodevices and novel drug delivery systems as well as in developing sensing applications. Another example can be found in dendrimers and nanoporous materials. Another example is to use block co-polymers, which form micelles for drug encapsulation.
Polymeric nanoparticles are a competing technology to lipidic (based mainly on Phospholipids) nanoparticles. There is an additional risk of toxicity associated with polymers not widely studied or understood. The major advantages of polymers is stability, lower cost and predictable characterization. However, in the patient's body this very stability (slow degradation) is a negative factor.
Phospholipids on the other hand are membrane lipids (already present in the body and surrounding each cell), have a GRAS (Generally Recognised As Safe) status from FDA and are derived from natural sources without any complex chemistry involved. They are not metabolised but rather absorbed by the body and the degradation products are themselves nutrients (fats or micronutrients).
Protein and peptides exert multiple biological actions in the human body and they have been identified as showing great promise for treatment of various diseases and disorders. These macromolecules are called biopharmaceuticals. Targeted and/or controlled delivery of these biopharmaceuticals using nanomaterials like nanoparticles and Dendrimers is an emerging field called nanobiopharmaceutics, and these products are called nanobiopharmaceuticals.
Another highly efficient system for microRNA delivery for example are nanoparticles formed by the self-assembly of two different microRNAs deregulated in cancer.
Another vision is based on small electromechanical systems; nanoelectromechanical systems are being investigated for the active release of drugs. Some potentially important applications include cancer treatment with iron nanoparticles or gold shells.
Nanotechnology is also opening up new opportunities in implantable delivery systems, which are often preferable to the use of injectable drugs, because the latter frequently display first-order kinetics (the blood concentration goes up rapidly, but drops exponentially over time).
This rapid rise may cause difficulties with toxicity, and drug efficacy can diminish as the drug concentration falls below the targeted range.
Applications:
Some nanotechnology-based drugs that are commercially available or in human clinical trials include:
- Abraxane, approved by the U.S. Food and Drug Administration (FDA) to treat breast cancer, non-small- cell lung cancer (NSCLC) and pancreatic cancer, is the nanoparticle albumin bound paclitaxel.
- Doxil was originally approved by the FDA for the use on HIV-related Kaposi's sarcoma. It is now being used to also treat ovarian cancer and multiple myeloma. The drug is encased in liposomes, which helps to extend the life of the drug that is being distributed. Liposomes are self-assembling, spherical, closed colloidal structures that are composed of lipid bilayers that surround an aqueous space. The liposomes also help to increase the functionality and it helps to decrease the damage that the drug does to the heart muscles specifically.
- Onivyde, liposome encapsulated irinotecan to treat metastatic pancreatic cancer, was approved by FDA in October 2015.
- C-dots (Cornell dots) are the smallest silica-based nanoparticles with the size <10 nm. The particles are infused with organic dye which will light up with fluorescence. Clinical trial is underway since 2011 to use the C-dots as diagnostic tool to assist surgeons to identify the location of tumor cells.
- An early phase clinical trial using the platform of ‘Minicell’ nanoparticle for drug delivery have been tested on patients with advanced and untreatable cancer. Built from the membranes of mutant bacteria, the minicells were loaded with paclitaxel and coated with cetuximab, antibodies that bind the epidermal growth factor receptor (EGFR) which is often overexpressed in a number of cancers, as a 'homing' device to the tumor cells. The tumor cells recognize the bacteria from which the minicells have been derived, regard it as invading microorganism and engulf it. Once inside, the payload of anti-cancer drug kills the tumor cells. Measured at 400 nanometers, the minicell is bigger than synthetic particles developed for drug delivery. The researchers indicated that this larger size gives the minicells a better profile in side-effects because the minicells will preferentially leak out of the porous blood vessels around the tumor cells and do not reach the liver, digestive system and skin. This Phase 1 clinical trial demonstrated that this treatment is well tolerated by the patients. As a platform technology, the minicell drug delivery system can be used to treat a number of different cancers with different anti-cancer drugs with the benefit of lower dose and less side-effects.
- In 2014, a Phase 3 clinical trial for treating inflammation and pain after cataract surgery, and a Phase 2 trial for treating dry eye disease were initiated using nanoparticle loteprednol etabonate. In 2015, the product, KPI-121 was found to produce statistically significant positive results for the post-surgery treatment.
Cancer:
Existing and potential drug nanocarriers have been reviewed.
Nanoparticles have high surface area to volume ratio. This allows for many functional groups to be attached to a nanoparticle, which can seek out and bind to certain tumor cells. Additionally, the small size of nanoparticles (10 to 100 nanometers), allows them to preferentially accumulate at tumor sites (because tumors lack an effective lymphatic drainage system). Limitations to conventional cancer chemotherapy include drug resistance, lack of selectivity, and lack of solubility. Nanoparticles have the potential to overcome these problems.
In photodynamic therapy, a particle is placed within the body and is illuminated with light from the outside. The light gets absorbed by the particle and if the particle is metal, energy from the light will heat the particle and surrounding tissue.
Light may also be used to produce high energy oxygen molecules which will chemically react with and destroy most organic molecules that are next to them (like tumors). This therapy is appealing for many reasons. It does not leave a "toxic trail" of reactive molecules throughout the body (chemotherapy) because it is directed where only the light is shined and the particles exist.
Photodynamic therapy has potential for a noninvasive procedure for dealing with diseases, growth and tumors. Kanzius RF therapy is one example of such therapy (nanoparticle hyperthermia) . Also, gold nanoparticles have the potential to join numerous therapeutic functions into a single platform, by targeting specific tumor cells, tissues and organs.
Imaging:
In vivo imaging is another area where tools and devices are being developed. Using nanoparticle contrast agents, images such as ultrasound and MRI have a favorable distribution and improved contrast. In cardiovascular imaging, nanoparticles have potential to aid visualization of blood pooling, ischemia, angiogenesis, atherosclerosis, and focal areas where inflammation is present.
The small size of nanoparticles endows them with properties that can be very useful in oncology, particularly in imaging. Quantum dots (nanoparticles with quantum confinement properties, such as size-tunable light emission), when used in conjunction with MRI (magnetic resonance imaging), can produce exceptional images of tumor sites.
Nanoparticles of cadmium selenide (quantum dots) glow when exposed to ultraviolet light. When injected, they seep into cancer tumors. The surgeon can see the glowing tumor, and use it as a guide for more accurate tumor removal.These nanoparticles are much brighter than organic dyes and only need one light source for excitation.
This means that the use of fluorescent quantum dots could produce a higher contrast image and at a lower cost than today's organic dyes used as contrast media. The downside, however, is that quantum dots are usually made of quite toxic elements, but this concern may be addressed by use of fluorescent dopants.
Tracking movement can help determine how well drugs are being distributed or how substances are metabolized. It is difficult to track a small group of cells throughout the body, so scientists used to dye the cells. These dyes needed to be excited by light of a certain wavelength in order for them to light up.
While different color dyes absorb different frequencies of light, there was a need for as many light sources as cells. A way around this problem is with luminescent tags. These tags are quantum dots attached to proteins that penetrate cell membranes. The dots can be random in size, can be made of bio-inert material, and they demonstrate the nanoscale property that color is size-dependent.
As a result, sizes are selected so that the frequency of light used to make a group of quantum dots fluoresce is an even multiple of the frequency required to make another group incandesce. Then both groups can be lit with a single light source. They have also found a way to insert nanoparticles into the affected parts of the body so that those parts of the body will glow showing the tumor growth or shrinkage or also organ trouble.
Sensing:
Main article: Nanosensor
Nanotechnology-on-a-chip is one more dimension of lab-on-a-chip technology. Magnetic nanoparticles, bound to a suitable antibody, are used to label specific molecules, structures or microorganisms. Gold nanoparticles tagged with short segments of DNA can be used for detection of genetic sequence in a sample.
Multicolor optical coding for biological assays has been achieved by embedding different-sized quantum dots into polymeric microbeads. Nanopore technology for analysis of nucleic acids converts strings of nucleotides directly into electronic signatures.
Sensor test chips containing thousands of nanowires, able to detect proteins and other biomarkers left behind by cancer cells, could enable the detection and diagnosis of cancer in the early stages from a few drops of a patient's blood. Nanotechnology is helping to advance the use of arthroscopes, which are pencil-sized devices that are used in surgeries with lights and cameras so surgeons can do the surgeries with smaller incisions. The smaller the incisions the faster the healing time which is better for the patients. It is also helping to find a way to make an arthroscope smaller than a strand of hair.
Research on nanoelectronics-based cancer diagnostics could lead to tests that can be done in pharmacies. The results promise to be highly accurate and the product promises to be inexpensive. They could take a very small amount of blood and detect cancer anywhere in the body in about five minutes, with a sensitivity that is a thousand times better than in a conventional laboratory test.
These devices that are built with nanowires to detect cancer proteins; each nanowire detector is primed to be sensitive to a different cancer marker. The biggest advantage of the nanowire detectors is that they could test for anywhere from ten to one hundred similar medical conditions without adding cost to the testing device.
Nanotechnology has also helped to personalize oncology for the detection, diagnosis, and treatment of cancer. It is now able to be tailored to each individual’s tumor for better performance. They have found ways that they will be able to target a specific part of the body that is being affected by cancer.
Blood purification:
Magnetic micro particles are proven research instruments for the separation of cells and proteins from complex media. The technology is available under the name Magnetic-activated cell sorting or Dynabeads among others.
More recently it was shown in animal models that magnetic nanoparticles can be used for the removal of various noxious compounds including toxins, pathogens, and proteins from whole blood in an extracorporeal circuit similar to dialysis.
In contrast to dialysis, which works on the principle of the size related diffusion of solutes and ultrafiltration of fluid across a semi-permeable membrane, the purification with nanoparticles allows specific targeting of substances. Additionally larger compounds which are commonly not dialyzable can be removed.
The purification process is based on functionalized iron oxide or carbon coated metal nanoparticles with ferromagnetic or superparamagnetic properties. Binding agents such as proteins, antibodies, antibiotics, or synthetic ligands are covalently linked to the particle surface. These binding agents are able to interact with target species forming an agglomerate.
Applying an external magnetic field gradient allows exerting a force on the nanoparticles. Hence the particles can be separated from the bulk fluid, thereby cleaning it from the contaminants.
The small size (< 100 nm) and large surface area of functionalized nanomagnets leads to advantageous properties compared to hemoperfusion, which is a clinically used technique for the purification of blood and is based on surface adsorption.
These advantages are high loading and accessibility of the binding agents, high selectivity towards the target compound, fast diffusion, small hydrodynamic resistance, and low dosage.
This approach offers new therapeutic possibilities for the treatment of systemic infections such as sepsis by directly removing the pathogen. It can also be used to selectively remove cytokines or endotoxins or for the dialysis of compounds which are not accessible by traditional dialysis methods. However the technology is still in a preclinical phase and first clinical trials are not expected before 2017.
Tissue engineering:
Nanotechnology may be used as part of tissue engineering to help reproduce or repair or reshape damaged tissue using suitable nanomaterial-based scaffolds and growth factors. Tissue engineering if successful may replace conventional treatments like organ transplants or artificial implants.
Nanoparticles such as graphene, carbon nanotubes, molybdenum disulfide and tungsten disulfide are being used as reinforcing agents to fabricate mechanically strong biodegradable polymeric nanocomposites for bone tissue engineering applications. The addition of these nanoparticles in the polymer matrix at low concentrations (~0.2 weight %) leads to significant improvements in the compressive and flexural mechanical properties of polymeric nanocomposites.
Potentially, these nanocomposites may be used as a novel, mechanically strong, light weight composite as bone implants.
For example, a flesh welder was demonstrated to fuse two pieces of chicken meat into a single piece using a suspension of gold-coated nanoshells activated by an infrared laser. This could be used to weld arteries during surgery. Another example is nanonephrology, the use of nanomedicine on the kidney.
Medical devices:
Neuro-electronic interfacing is a visionary goal dealing with the construction of nanodevices that will permit computers to be joined and linked to the nervous system. This idea requires the building of a molecular structure that will permit control and detection of nerve impulses by an external computer.
A refuelable strategy implies energy is refilled continuously or periodically with external sonic, chemical, tethered, magnetic, or biological electrical sources, while a nonrefuelable strategy implies that all power is drawn from internal energy storage which would stop when all energy is drained.
A nanoscale enzymatic biofuel cell for self-powered nanodevices have been developed that uses glucose from biofluids including human blood and watermelons. One limitation to this innovation is the fact that electrical interference or leakage or overheating from power consumption is possible.
The wiring of the structure is extremely difficult because they must be positioned precisely in the nervous system. The structures that will provide the interface must also be compatible with the body's immune system.
Molecular nanotechnology is a speculative subfield of nanotechnology regarding the possibility of engineering molecular assemblers, machines which could re-order matter at a molecular or atomic scale.
Nanomedicine would make use of these nanorobots, introduced into the body, to repair or detect damages and infections. Molecular nanotechnology is highly theoretical, seeking to anticipate what inventions nanotechnology might yield and to propose an agenda for future inquiry.
The proposed elements of molecular nanotechnology, such as molecular assemblers and nanorobots are far beyond current capabilities. Future advances in nanomedicine could give rise to life extension through the repair of many processes thought to be responsible for aging.
K. Eric Drexler, one of the founders of nanotechnology, postulated cell repair machines, including ones operating within cells and utilizing as yet hypothetical molecular machines, in his 1986 book Engines of Creation, with the first technical discussion of medical nanorobots by Robert Freitas appearing in 1999.
Raymond Kurzweil, a futurist and transhumanist, stated in his book The Singularity Is Near that he believes that advanced medical nanorobotics could completely remedy the effects of aging by 2030.
According to Richard Feynman, it was his former graduate student and collaborator Albert Hibbs who originally suggested to him (circa 1959) the idea of a medical use for Feynman's theoretical micromachines (see nanotechnology). Hibbs suggested that certain repair machines might one day be reduced in size to the point that it would, in theory, be possible to (as Feynman put it) "swallow the doctor". The idea was incorporated into Feynman's 1959 essay There's Plenty of Room at the Bottom.
See Also:
- Colloidal gold
- Gold nanobeacon
- Heart nanotechnology
- IEEE P1906.1 – Recommended Practice for Nanoscale and Molecular Communication Framework
- Impalefection
- Monitoring (medicine)
- Nanobiotechnology
- Nanoparticle–biomolecule conjugate
- Nanosensor
- Nanozymes
- Nanotechnology in fiction
- Photodynamic therapy
- Top-down and bottom-up design
Medical Research and Funding
YouTube Video: National Institute of Health Mission - It's About Life
Pictured: R&D in the FY 2014 Omnibus: The National Institutes of Health
Biomedical research (or experimental medicine) encompasses a wide array of research from "basic research" (also called bench science or bench research), involving the elucidation of more fundamental scientific principles, to clinical research, which is distinguished by the involvement of patients.
Within this spectrum is applied research, or translational research conducted to aid and support the development of knowledge in the field of medicine, and pre-clinical research, for example involving animals.
Both clinical and pre-clinical research phases exist in the pharmaceutical industry's drug development pipelines, where the clinical phase is denoted by the term clinical trial.
However, only part of the clinical or pre-clinical research is oriented towards a specific pharmaceutical purpose. The need for fundamental and mechanistic understanding, diagnostics, medical devices and non-pharmaceutical therapies means that pharmaceutical research is only a small part of medical research.
The increased longevity of humans over the past century can be significantly attributed to advances resulting from medical research. Among the major benefits of medical research have been the following:
New, beneficial tests and treatments are expected as a result of the Human Genome Project. Many challenges remain, however, including the appearance of antibiotic resistance and the obesity epidemic.
Most of the research in the field is pursued by biomedical scientists, however significant contributions are made by other biologists, as well as chemists and physicists. Medical research, done on humans, has to strictly follow the medical ethics as sanctioned in the Declaration of Helsinki and elsewhere. In all cases, the research ethics has to be respected.
Phases of Medical Research:
Basic Medical Research:
Areas tackled in the most fundamental parts of medical research include cellular and molecular biology, medical genetics, immunology, neuroscience, and psychology.
Researchers, mainly in universities or government-funded research institutes, aim to establish an understanding of the cellular, molecular and physiological mechanisms underpinning human health and disease.
Since many organisms share a common evolutionary history with humans and hence common features and systems, the basic end of medical research these days shades into basic biology.
Preclinical research:
Pre-clinical research covers research that prepares the ground for clinical research with patients. Typically the work requires no ethical approval (though work with animals does), is supervised by scientists rather than medical doctors, and is carried out in a university or company rather than a hospital.
Clinical research:
Clinical research is carried out with patients. It is generally supervised by doctors in a medical setting such as a hospital and requires ethical approval.
Click on any of the following for more about Medical Research:
Within this spectrum is applied research, or translational research conducted to aid and support the development of knowledge in the field of medicine, and pre-clinical research, for example involving animals.
Both clinical and pre-clinical research phases exist in the pharmaceutical industry's drug development pipelines, where the clinical phase is denoted by the term clinical trial.
However, only part of the clinical or pre-clinical research is oriented towards a specific pharmaceutical purpose. The need for fundamental and mechanistic understanding, diagnostics, medical devices and non-pharmaceutical therapies means that pharmaceutical research is only a small part of medical research.
The increased longevity of humans over the past century can be significantly attributed to advances resulting from medical research. Among the major benefits of medical research have been the following:
- vaccines for measles and polio,
- insulin treatment for diabetes,
- classes of antibiotics for treating a host of maladies,
- medication for high blood pressure,
- improved treatments for AIDS,
- statins and other treatments for atherosclerosis,
- new surgical techniques such as microsurgery,
- and increasingly successful treatments for cancer.
New, beneficial tests and treatments are expected as a result of the Human Genome Project. Many challenges remain, however, including the appearance of antibiotic resistance and the obesity epidemic.
Most of the research in the field is pursued by biomedical scientists, however significant contributions are made by other biologists, as well as chemists and physicists. Medical research, done on humans, has to strictly follow the medical ethics as sanctioned in the Declaration of Helsinki and elsewhere. In all cases, the research ethics has to be respected.
Phases of Medical Research:
Basic Medical Research:
Areas tackled in the most fundamental parts of medical research include cellular and molecular biology, medical genetics, immunology, neuroscience, and psychology.
Researchers, mainly in universities or government-funded research institutes, aim to establish an understanding of the cellular, molecular and physiological mechanisms underpinning human health and disease.
Since many organisms share a common evolutionary history with humans and hence common features and systems, the basic end of medical research these days shades into basic biology.
Preclinical research:
Pre-clinical research covers research that prepares the ground for clinical research with patients. Typically the work requires no ethical approval (though work with animals does), is supervised by scientists rather than medical doctors, and is carried out in a university or company rather than a hospital.
Clinical research:
Clinical research is carried out with patients. It is generally supervised by doctors in a medical setting such as a hospital and requires ethical approval.
Click on any of the following for more about Medical Research:
Francis Collins, Lead Scientist of the Genome Project
YouTube Video: Francis Collins - The Language of God: A Scientist Presents Evidence of Belief
Francis Sellers Collins (born April 14, 1950) is an American physician-geneticist noted for his discoveries of disease genes and his leadership of the Human Genome Project. He is director of the National Institutes of Health (NIH) in Bethesda, Maryland, USA.
Before being appointed director of the NIH, Collins led the Human Genome Project and other genomics research initiatives as director of the National Human Genome Research Institute (NHGRI), one of the 27 institutes and centers at NIH.
Before joining NHGRI, he earned a reputation as a gene hunter at the University of Michigan.
He has been elected to the Institute of Medicine and the National Academy of Sciences, and has received the Presidential Medal of Freedom and the National Medal of Science.
Collins also has written a number of books on science, medicine, and religion, including the New York Times bestseller, The Language of God: A Scientist Presents Evidence for Belief.
After leaving the helm of NHGRI and before becoming director of the NIH, he founded and
served as president of The BioLogos Foundation, which promotes discourse on the relationship between science and religion and advocates the perspective that belief in Christianity can be reconciled with acceptance of evolution and science, especially through the advancement of evolutionary creation.
In 2009, Pope Benedict XVI appointed Collins to the Pontifical Academy of Sciences.
Click on any of the following blue hyperlinks for more about Francis Collins:
Before being appointed director of the NIH, Collins led the Human Genome Project and other genomics research initiatives as director of the National Human Genome Research Institute (NHGRI), one of the 27 institutes and centers at NIH.
Before joining NHGRI, he earned a reputation as a gene hunter at the University of Michigan.
He has been elected to the Institute of Medicine and the National Academy of Sciences, and has received the Presidential Medal of Freedom and the National Medal of Science.
Collins also has written a number of books on science, medicine, and religion, including the New York Times bestseller, The Language of God: A Scientist Presents Evidence for Belief.
After leaving the helm of NHGRI and before becoming director of the NIH, he founded and
served as president of The BioLogos Foundation, which promotes discourse on the relationship between science and religion and advocates the perspective that belief in Christianity can be reconciled with acceptance of evolution and science, especially through the advancement of evolutionary creation.
In 2009, Pope Benedict XVI appointed Collins to the Pontifical Academy of Sciences.
Click on any of the following blue hyperlinks for more about Francis Collins:
Vaccines, including a List of Vaccine-preventable Diseases
YouTube Video: How do vaccines prevent disease? by Harvard University
Pictured: Avian flu vaccine development by reverse genetics techniques.
Click here for a List of Vaccine-preventable Diseases.
A vaccine is a biological preparation that provides active acquired immunity to a particular disease. A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins, or one of its surface proteins.
The agent stimulates the body's immune system to recognize the agent as a threat, destroy it, recognize and destroy any of these microorganisms that it later encounters. Vaccines can be prophylactic (example: to prevent or ameliorate the effects of a future infection by a natural or "wild" pathogen), or therapeutic (e.g., vaccines against cancer are being investigated).
The effectiveness of vaccination has been widely studied and verified; for example, the influenza vaccine, the HPV vaccine, and the chicken pox vaccine. The World Health Organization (WHO) reports that licensed vaccines are currently available for twenty-five different preventable infections.
The administration of vaccines is called vaccination. Vaccination is the most effective method of preventing infectious diseases; widespread immunity due to vaccination is largely responsible for the worldwide eradication of smallpox and the restriction of diseases such as polio, measles, and tetanus from much of the world.
The terms vaccine and vaccination are derived from Variolae vaccinae (smallpox of the cow), the term devised by Edward Jenner to denote cowpox. He used it in 1798 in the long title of his Inquiry into the Variolae vaccinae known as the Cow Pox, in which he described the protective effect of cowpox against smallpox.
In 1881, to honor Jenner, Louis Pasteur proposed that the terms should be extended to cover the new protective inoculations then being developed.
How Vaccines Work:
Generically, the process of artificial induction of immunity, in an effort to protect against infectious disease, works by 'priming' the immune system with an 'immunogen'. Stimulating immune responses with an infectious agent is known as immunization. Vaccination includes various ways of administering immunogens.
Some vaccines are administered after the patient already has contracted a disease. Vaccines given after exposure to smallpox, within the first three days, are reported to attenuate the disease considerably, and vaccination up to a week after exposure probably offers some protection from disease or may reduce the severity of disease.
The first rabies immunization was given by Louis Pasteur to a child after he was bitten by a rabid dog. Since then, it has been found that, in people with healthy immune systems, four doses of rabies vaccine over 14 days, wound care, and treatment of the bite with rabies immune globulin, commenced as soon as possible after exposure, is effective in preventing rabies in humans.
Other examples include experimental AIDS, cancer and Alzheimer's disease vaccines. Such immunizations aim to trigger an immune response more rapidly and with less harm than natural infection.
Most vaccines are given by hypodermic injection as they are not absorbed reliably through the intestines. Live attenuated polio, some typhoid, and some cholera vaccines are given orally to produce immunity in the bowel. While vaccination provides a lasting effect, it usually takes several weeks to develop, while passive immunity (the transfer of antibodies) has immediate effect.
Vaccination versus inoculation:
The term inoculation is often used interchangeably with vaccination. However, some argue that the terms are not synonymous. Dr Byron Plant explains: "Vaccination is the more commonly used term, which actually consists of a 'safe' injection of a sample taken from a cow suffering from cowpox... Inoculation, a practice probably as old as the disease itself, is the injection of the variola virus taken from a pustule or scab of a smallpox sufferer into the superficial layers of the skin, commonly on the upper arm of the subject.
Often inoculation was done 'arm to arm' or less effectively 'scab to arm'..." Inoculation oftentimes caused the patient to become infected with smallpox, and in some cases the infection turned into a severe case.
Vaccinations began in the 18th century with the work of Edward Jenner and the smallpox vaccine.
Effectiveness:
Vaccines have historically been the most effective means to fight and eradicate infectious diseases. Limitations to their effectiveness, nevertheless, exist. Sometimes, protection fails because the host's immune system simply does not respond adequately or at all. Lack of response commonly results from clinical factors such as diabetes, steroid use, HIV infection or age. It also might fail for genetic reasons if the host's immune system includes no strains of B cells that can generate antibodies suited to reacting effectively and binding to the antigens associated with the pathogen.
Even if the host does develop antibodies, protection might not be adequate; immunity might develop too slowly to be effective in time, the antibodies might not disable the pathogen completely, or there might be multiple strains of the pathogen, not all of which are equally susceptible to the immune reaction.
However, even a partial, late, or weak immunity, such as a one resulting from cross-immunity to a strain other than the target strain, may mitigate an infection, resulting in a lower mortality rate, lower morbidity, and faster recovery.
Adjuvants commonly are used to boost immune response, particularly for older people (50–75 years and up), whose immune response to a simple vaccine may have weakened.
The efficacy or performance of the vaccine is dependent on a number of factors:
If a vaccinated individual does develop the disease vaccinated against (breakthrough infection), the disease is likely to be less virulent than in unvaccinated victims.
The following are important considerations in the effectiveness of a vaccination program:
In 1958, there were 763,094 cases of measles in the United States; 552 deaths resulted. After the introduction of new vaccines, the number of cases dropped to fewer than 150 per year (median of 56). In early 2008, there were 64 suspected cases of measles. Fifty-four of those infections were associated with importation from another country, although only 13% were actually acquired outside the United States; 63 of the 64 individuals either had never been vaccinated against measles or were uncertain whether they had been vaccinated.
Vaccines have contributed to the eradication of smallpox, one of the most contagious and deadly diseases in humans. Other diseases such as rubella, polio, measles, mumps, chickenpox, and typhoid are nowhere near as common as they were a hundred years ago.
As long as the vast majority of people are vaccinated, it is much more difficult for an outbreak of disease to occur, let alone spread. This effect is called herd immunity. Polio, which is transmitted only between humans, is targeted by an extensive eradication campaign that has seen endemic polio restricted to only parts of three countries (Afghanistan, Nigeria, and Pakistan).
However, the difficulty of reaching all children as well as cultural misunderstandings have caused the anticipated eradication date to be missed several times.
Vaccines also help prevent the development of antibiotic resistance. For example, by greatly reducing the incidence of pneumonia caused by Streptococcus pneumoniae, vaccine programs have greatly reduced the prevalence of infections resistant to penicillin or other first-line antibiotics.
Adverse Effects:
Vaccination given during childhood is generally safe. Adverse effects if any are generally mild. The rate of side effects depends on the vaccine in question. Some common side effects include fever, pain around the injection site, and muscle aches. Additionally, some individuals may be allergic to ingredients in the vaccine. MMR vaccine is rarely associated with febrile seizures.
Severe side effects are extremely rare. Varicella vaccine is rarely associated with complications in immunodeficient individuals and rotavirus vaccines are moderately associated with intussusception.
Types of Vaccines:
Vaccines are dead or inactivated organisms or purified products derived from them.
There are several types of vaccines in use. These represent different strategies used to try to reduce the risk of illness while retaining the ability to induce a beneficial immune response.
Inactivated:
Main article: Inactivated vaccine
Some vaccines contain inactivated, but previously virulent, micro-organisms that have been destroyed with chemicals, heat, or radiation. Examples include the polio vaccine, hepatitis A vaccine, rabies vaccine and some influenza vaccines.
Attenuated:
Main article: Attenuated vaccine
Some vaccines contain live, attenuated microorganisms. Many of these are active viruses that have been cultivated under conditions that disable their virulent properties, or that use closely related but less dangerous organisms to produce a broad immune response. Although most attenuated vaccines are viral, some are bacterial in nature.
Examples include the viral diseases yellow fever, measles, mumps, and rubella, and the bacterial disease typhoid.
The live Mycobacterium tuberculosis vaccine developed by Calmette and Guérin is not made of a contagious strain but contains a virulently modified strain called "BCG" used to elicit an immune response to the vaccine.
The live attenuated vaccine containing strain Yersinia pestis EV is used for plague immunization. Attenuated vaccines have some advantages and disadvantages. They typically provoke more durable immunological responses and are the preferred type for healthy adults. But they may not be safe for use in immunocompromised individuals, and may rarely mutate to a virulent form and cause disease.
Toxoid:
Toxoid vaccines are made from inactivated toxic compounds that cause illness rather than the micro-organism. Examples of toxoid-based vaccines include tetanus and diphtheria. Toxoid vaccines are known for their efficacy. Not all toxoids are for micro-organisms; for example, Crotalus atrox toxoid is used to vaccinate dogs against rattlesnake bites.
Subunit:
Protein subunit – rather than introducing an inactivated or attenuated micro-organism to an immune system (which would constitute a "whole-agent" vaccine), a fragment of it can create an immune response.
Examples include the subunit vaccine against Hepatitis B virus that is composed of only the surface proteins of the virus (previously extracted from the blood serum of chronically infected patients, but now produced by recombination of the viral genes into yeast), the virus-like particle (VLP) vaccine against human papillomavirus (HPV) that is composed of the viral major capsid protein, and the hemagglutinin and neuraminidase subunits of the influenza virus. Subunit vaccine is being used for plague immunization.
Conjugate:
Conjugate – certain bacteria have polysaccharide outer coats that are poorly immunogenic. By linking these outer coats to proteins (e.g., toxins), the immune system can be led to recognize the polysaccharide as if it were a protein antigen. This approach is used in the Haemophilus influenzae type B vaccine
Experimental:
A number of innovative vaccines are also in development and in use:
While most vaccines are created using inactivated or attenuated compounds from micro-organisms, synthetic vaccines are composed mainly or wholly of synthetic peptides, carbohydrates, or antigens.
Valence:
Vaccines may be monovalent (also called univalent) or multivalent (also called polyvalent). A monovalent vaccine is designed to immunize against a single antigen or single microorganism. A multivalent or polyvalent vaccine is designed to immunize against two or more strains of the same microorganism, or against two or more microorganisms. The valency of a multivalent vaccine may be denoted with a Greek or Latin prefix (e.g., tetravalent or quadrivalent). In certain cases, a monovalent vaccine may be preferable for rapidly developing a strong immune response.[
Heterotypic:
Also known as heterologous or "Jennerian" vaccines, these are vaccines that are pathogens of other animals that either do not cause disease or cause mild disease in the organism being treated. The classic example is Jenner's use of cowpox to protect against smallpox. A current example is the use of BCG vaccine made from Mycobacterium bovis to protect against human tuberculosis
Routes of administration:
See also: Vaccination schedule
A vaccine administration may be oral, by injection (intramuscular, intradermal, subcutaneous), by puncture, transdermal or intranasal. Several recent clinical trials have aimed to deliver the vaccines via mucosal surfaces to be up-taken by the common mucosal immunity system, thus avoiding the need for injections.
Click on any of the following blue hyperlinks for more about Vaccines:
A vaccine is a biological preparation that provides active acquired immunity to a particular disease. A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins, or one of its surface proteins.
The agent stimulates the body's immune system to recognize the agent as a threat, destroy it, recognize and destroy any of these microorganisms that it later encounters. Vaccines can be prophylactic (example: to prevent or ameliorate the effects of a future infection by a natural or "wild" pathogen), or therapeutic (e.g., vaccines against cancer are being investigated).
The effectiveness of vaccination has been widely studied and verified; for example, the influenza vaccine, the HPV vaccine, and the chicken pox vaccine. The World Health Organization (WHO) reports that licensed vaccines are currently available for twenty-five different preventable infections.
The administration of vaccines is called vaccination. Vaccination is the most effective method of preventing infectious diseases; widespread immunity due to vaccination is largely responsible for the worldwide eradication of smallpox and the restriction of diseases such as polio, measles, and tetanus from much of the world.
The terms vaccine and vaccination are derived from Variolae vaccinae (smallpox of the cow), the term devised by Edward Jenner to denote cowpox. He used it in 1798 in the long title of his Inquiry into the Variolae vaccinae known as the Cow Pox, in which he described the protective effect of cowpox against smallpox.
In 1881, to honor Jenner, Louis Pasteur proposed that the terms should be extended to cover the new protective inoculations then being developed.
How Vaccines Work:
Generically, the process of artificial induction of immunity, in an effort to protect against infectious disease, works by 'priming' the immune system with an 'immunogen'. Stimulating immune responses with an infectious agent is known as immunization. Vaccination includes various ways of administering immunogens.
Some vaccines are administered after the patient already has contracted a disease. Vaccines given after exposure to smallpox, within the first three days, are reported to attenuate the disease considerably, and vaccination up to a week after exposure probably offers some protection from disease or may reduce the severity of disease.
The first rabies immunization was given by Louis Pasteur to a child after he was bitten by a rabid dog. Since then, it has been found that, in people with healthy immune systems, four doses of rabies vaccine over 14 days, wound care, and treatment of the bite with rabies immune globulin, commenced as soon as possible after exposure, is effective in preventing rabies in humans.
Other examples include experimental AIDS, cancer and Alzheimer's disease vaccines. Such immunizations aim to trigger an immune response more rapidly and with less harm than natural infection.
Most vaccines are given by hypodermic injection as they are not absorbed reliably through the intestines. Live attenuated polio, some typhoid, and some cholera vaccines are given orally to produce immunity in the bowel. While vaccination provides a lasting effect, it usually takes several weeks to develop, while passive immunity (the transfer of antibodies) has immediate effect.
Vaccination versus inoculation:
The term inoculation is often used interchangeably with vaccination. However, some argue that the terms are not synonymous. Dr Byron Plant explains: "Vaccination is the more commonly used term, which actually consists of a 'safe' injection of a sample taken from a cow suffering from cowpox... Inoculation, a practice probably as old as the disease itself, is the injection of the variola virus taken from a pustule or scab of a smallpox sufferer into the superficial layers of the skin, commonly on the upper arm of the subject.
Often inoculation was done 'arm to arm' or less effectively 'scab to arm'..." Inoculation oftentimes caused the patient to become infected with smallpox, and in some cases the infection turned into a severe case.
Vaccinations began in the 18th century with the work of Edward Jenner and the smallpox vaccine.
Effectiveness:
Vaccines have historically been the most effective means to fight and eradicate infectious diseases. Limitations to their effectiveness, nevertheless, exist. Sometimes, protection fails because the host's immune system simply does not respond adequately or at all. Lack of response commonly results from clinical factors such as diabetes, steroid use, HIV infection or age. It also might fail for genetic reasons if the host's immune system includes no strains of B cells that can generate antibodies suited to reacting effectively and binding to the antigens associated with the pathogen.
Even if the host does develop antibodies, protection might not be adequate; immunity might develop too slowly to be effective in time, the antibodies might not disable the pathogen completely, or there might be multiple strains of the pathogen, not all of which are equally susceptible to the immune reaction.
However, even a partial, late, or weak immunity, such as a one resulting from cross-immunity to a strain other than the target strain, may mitigate an infection, resulting in a lower mortality rate, lower morbidity, and faster recovery.
Adjuvants commonly are used to boost immune response, particularly for older people (50–75 years and up), whose immune response to a simple vaccine may have weakened.
The efficacy or performance of the vaccine is dependent on a number of factors:
- the disease itself (for some diseases vaccination performs better than for others)
- the strain of vaccine (some vaccines are specific to, or at least most effective against, particular strains of the disease)
- whether the vaccination schedule has been properly observed.
- idiosyncratic response to vaccination; some individuals are "non-responders" to certain vaccines, meaning that they do not generate antibodies even after being vaccinated correctly.
- assorted factors such as ethnicity, age, or genetic predisposition.
If a vaccinated individual does develop the disease vaccinated against (breakthrough infection), the disease is likely to be less virulent than in unvaccinated victims.
The following are important considerations in the effectiveness of a vaccination program:
- careful modeling to anticipate the impact that an immunization campaign will have on the epidemiology of the disease in the medium to long term
- ongoing surveillance for the relevant disease following introduction of a new vaccine
- maintenance of high immunization rates, even when a disease has become rare.
In 1958, there were 763,094 cases of measles in the United States; 552 deaths resulted. After the introduction of new vaccines, the number of cases dropped to fewer than 150 per year (median of 56). In early 2008, there were 64 suspected cases of measles. Fifty-four of those infections were associated with importation from another country, although only 13% were actually acquired outside the United States; 63 of the 64 individuals either had never been vaccinated against measles or were uncertain whether they had been vaccinated.
Vaccines have contributed to the eradication of smallpox, one of the most contagious and deadly diseases in humans. Other diseases such as rubella, polio, measles, mumps, chickenpox, and typhoid are nowhere near as common as they were a hundred years ago.
As long as the vast majority of people are vaccinated, it is much more difficult for an outbreak of disease to occur, let alone spread. This effect is called herd immunity. Polio, which is transmitted only between humans, is targeted by an extensive eradication campaign that has seen endemic polio restricted to only parts of three countries (Afghanistan, Nigeria, and Pakistan).
However, the difficulty of reaching all children as well as cultural misunderstandings have caused the anticipated eradication date to be missed several times.
Vaccines also help prevent the development of antibiotic resistance. For example, by greatly reducing the incidence of pneumonia caused by Streptococcus pneumoniae, vaccine programs have greatly reduced the prevalence of infections resistant to penicillin or other first-line antibiotics.
Adverse Effects:
Vaccination given during childhood is generally safe. Adverse effects if any are generally mild. The rate of side effects depends on the vaccine in question. Some common side effects include fever, pain around the injection site, and muscle aches. Additionally, some individuals may be allergic to ingredients in the vaccine. MMR vaccine is rarely associated with febrile seizures.
Severe side effects are extremely rare. Varicella vaccine is rarely associated with complications in immunodeficient individuals and rotavirus vaccines are moderately associated with intussusception.
Types of Vaccines:
Vaccines are dead or inactivated organisms or purified products derived from them.
There are several types of vaccines in use. These represent different strategies used to try to reduce the risk of illness while retaining the ability to induce a beneficial immune response.
Inactivated:
Main article: Inactivated vaccine
Some vaccines contain inactivated, but previously virulent, micro-organisms that have been destroyed with chemicals, heat, or radiation. Examples include the polio vaccine, hepatitis A vaccine, rabies vaccine and some influenza vaccines.
Attenuated:
Main article: Attenuated vaccine
Some vaccines contain live, attenuated microorganisms. Many of these are active viruses that have been cultivated under conditions that disable their virulent properties, or that use closely related but less dangerous organisms to produce a broad immune response. Although most attenuated vaccines are viral, some are bacterial in nature.
Examples include the viral diseases yellow fever, measles, mumps, and rubella, and the bacterial disease typhoid.
The live Mycobacterium tuberculosis vaccine developed by Calmette and Guérin is not made of a contagious strain but contains a virulently modified strain called "BCG" used to elicit an immune response to the vaccine.
The live attenuated vaccine containing strain Yersinia pestis EV is used for plague immunization. Attenuated vaccines have some advantages and disadvantages. They typically provoke more durable immunological responses and are the preferred type for healthy adults. But they may not be safe for use in immunocompromised individuals, and may rarely mutate to a virulent form and cause disease.
Toxoid:
Toxoid vaccines are made from inactivated toxic compounds that cause illness rather than the micro-organism. Examples of toxoid-based vaccines include tetanus and diphtheria. Toxoid vaccines are known for their efficacy. Not all toxoids are for micro-organisms; for example, Crotalus atrox toxoid is used to vaccinate dogs against rattlesnake bites.
Subunit:
Protein subunit – rather than introducing an inactivated or attenuated micro-organism to an immune system (which would constitute a "whole-agent" vaccine), a fragment of it can create an immune response.
Examples include the subunit vaccine against Hepatitis B virus that is composed of only the surface proteins of the virus (previously extracted from the blood serum of chronically infected patients, but now produced by recombination of the viral genes into yeast), the virus-like particle (VLP) vaccine against human papillomavirus (HPV) that is composed of the viral major capsid protein, and the hemagglutinin and neuraminidase subunits of the influenza virus. Subunit vaccine is being used for plague immunization.
Conjugate:
Conjugate – certain bacteria have polysaccharide outer coats that are poorly immunogenic. By linking these outer coats to proteins (e.g., toxins), the immune system can be led to recognize the polysaccharide as if it were a protein antigen. This approach is used in the Haemophilus influenzae type B vaccine
Experimental:
A number of innovative vaccines are also in development and in use:
- Dendritic cell vaccines combine dendritic cells with antigens in order to present the antigens to the body's white blood cells, thus stimulating an immune reaction. These vaccines have shown some positive preliminary results for treating brain tumors and are also tested in malignant melanoma.
- Recombinant Vector – by combining the physiology of one micro-organism and the DNA of the other, immunity can be created against diseases that have complex infection processes
- DNA vaccination – an alternative, experimental approach to vaccination called DNA vaccination, created from an infectious agent's DNA, is under development. The proposed mechanism is the insertion (and expression, enhanced by the use of electroporation, triggering immune system recognition) of viral or bacterial DNA into human or animal cells. Some cells of the immune system that recognize the proteins expressed will mount an attack against these proteins and cells expressing them. Because these cells live for a very long time, if the pathogen that normally expresses these proteins is encountered at a later time, they will be attacked instantly by the immune system. One potential advantage of DNA vaccines is that they are very easy to produce and store. As of 2015, DNA vaccination is still experimental and is not approved for human use.
- T-cell receptor peptide vaccines are under development for several diseases using models of Valley Fever, stomatitis, and atopic dermatitis. These peptides have been shown to modulate cytokine production and improve cell-mediated immunity.
- Targeting of identified bacterial proteins that are involved in complement inhibition would neutralize the key bacterial virulence mechanism.
While most vaccines are created using inactivated or attenuated compounds from micro-organisms, synthetic vaccines are composed mainly or wholly of synthetic peptides, carbohydrates, or antigens.
Valence:
Vaccines may be monovalent (also called univalent) or multivalent (also called polyvalent). A monovalent vaccine is designed to immunize against a single antigen or single microorganism. A multivalent or polyvalent vaccine is designed to immunize against two or more strains of the same microorganism, or against two or more microorganisms. The valency of a multivalent vaccine may be denoted with a Greek or Latin prefix (e.g., tetravalent or quadrivalent). In certain cases, a monovalent vaccine may be preferable for rapidly developing a strong immune response.[
Heterotypic:
Also known as heterologous or "Jennerian" vaccines, these are vaccines that are pathogens of other animals that either do not cause disease or cause mild disease in the organism being treated. The classic example is Jenner's use of cowpox to protect against smallpox. A current example is the use of BCG vaccine made from Mycobacterium bovis to protect against human tuberculosis
Routes of administration:
See also: Vaccination schedule
A vaccine administration may be oral, by injection (intramuscular, intradermal, subcutaneous), by puncture, transdermal or intranasal. Several recent clinical trials have aimed to deliver the vaccines via mucosal surfaces to be up-taken by the common mucosal immunity system, thus avoiding the need for injections.
Click on any of the following blue hyperlinks for more about Vaccines:
- Nomenclature
- Developing immunity
- Schedule
- History including Timeline
- Society and culture
- Opposition
Economics of development
Patents
- Opposition
- Production
- Excipients
Role of preservatives
- Excipients
- Delivery systems including Plasmids
- Veterinary medicine
- DIVA vaccines
- First DIVA vaccines
Use in practice
Other DIVA vaccines (under development)
- First DIVA vaccines
- Trends
- See also:
- Coalition for Epidemic Preparedness Innovations
- Flying syringe
- The Horse Named Jim
- Immunization registry
- Immunotherapy
- List of vaccine ingredients
- List of vaccine topics
- Non-specific effect of vaccines
- OPV AIDS hypothesis
- Reverse vaccinology
- TA-CD
- Virosome
- Vaccinov
- WHO Vaccine preventable diseases and immunization
- World Health Organization position papers on vaccines
- The History of Vaccines, from the College of Physicians of Philadelphia
Microsurgery including Robot-assisted Surgery
YouTube Video: Robotic Micro Surgery
Pictured: Robotic Micro Surgery
Microsurgery:
Microsurgery is a general term for surgery requiring an operating microscope. The most obvious developments have been procedures developed to allow anastomosis of successively smaller blood vessels and nerves (typically 1 mm in diameter) which have allowed transfer of tissue from one part of the body to another and re-attachment of severed parts.
Microsurgical techniques are utilized by several specialties today, such as:
Free Tissue Transfer:
Main article: free flap
Free tissue transfer is a surgical reconstructive procedure using microsurgery. A region of "donor" tissue is selected that can be isolated on a feeding artery and vein; this tissue is usually a composite of several tissue types (e.g., skin, muscle, fat, bone).
Common donor regions include the rectus abdominis muscle, latissimus dorsi muscle, fibula, radial forearm bone and skin, and lateral arm skin. The composite tissue is transferred (moved as a free flap of tissue) to the region on the patient requiring reconstruction (e.g., mandible after oral cancer resection, breast after cancer resection, traumatic tissue loss, congenital tissue absence).
The vessels that supply the free flap are anastomosed with microsurgery to matching vessels (artery and vein) in the reconstructive site. The procedure was first done in the early 1970s and has become a popular "one-stage" (single operation) procedure for many surgical reconstructive applications.
Replantation:
Replantation is the reattachment of a completely detached body part.
Fingers and thumbs are the most common but the ear, scalp, nose, face, arm and penis have all been replanted.
Generally replantation involves restoring blood flow through arteries and veins, restoring the bony skeleton and connecting tendons and nerves as required.
Robert Malt and Charles Mckhann reported the first replantation two human upper extremities by microvascular means in 1964 with the first arm replanted in a child after a train injury in 1962 in Boston.
Initially, when the techniques were developed to make replantation possible, success was defined in terms of a survival of the amputated part alone. However, as more experience was gained in this field, surgeons specializing in replantation began to understand that survival of the amputated piece was not enough to ensure success of the replant.
In this way, functional demands of the amputated specimen became paramount in guiding which amputated pieces should and should not be replanted. Additional concerns about the patients ability to tolerate the long rehabilitation process that is necessary after replantation both on physical and psychological levels also became important.
So, when fingers are amputated, for instance, a replantation surgeon must seriously consider the contribution of the finger to the overall function of the hand. In this way, every attempt will be made to salvage an amputated thumb, since a great deal of hand function is dependent on the thumb, while an index finger or small finger may not be replanted, depending on the individual needs of the patient and the ability of the patient to tolerate a long surgery and a long course of rehabilitation.
However, if an amputated specimen is not able to be replanted to its original location entirely, this does not mean that the specimen is unreplantable. In fact, replantation surgeons have learned that only a piece or a portion may be necessary to obtain a functional result, or especially in the case of multiple amputated fingers, a finger or fingers may be transposed to a more useful location to obtain a more functional result. This concept is called "spare parts" surgery.
Transplantation:
Microsurgical techniques have played a crucial role in the development of transplantation immunological research because it allowed the use of rodents models, which are more appropriate for transplantation research (there are more reagents, monoclonal antibodies, knockout animals, and other immunological tools for mice and rats than other species).
Before it was introduced, transplant immunology was studied in rodents using the skin transplantation model, which is limited by the fact that it is not vascularized. Thus, microsurgery represents the link between surgery and transplant immunological research.
The first microsurgical experiments (porto-caval anastomosis in the rat) were performed by Dr. Sun Lee (pioneer of microsurgery) at the University of Pittsburgh in 1958. After a short time, many models of organ transplants in rat and mice have been established.
Today, virtually every rat or mouse organ can be transplanted with relative high success rate. Microsurgery was also important to develop new techniques of transplantation, that would be later performed in humans. In addition, it allows reconstruction of small arteries in clinical organ transplantation (e.g. accessory arteries in cadaver liver transplantation, polar arteries in renal transplantation and in living liver donor transplantation)
Treatment of Infertility:
Microsurgery has been used to treat several pathologic conditions leading to infertility such as tubal obstructions, vas deferens obstructions and varicocele which is one of the most frequent cause of male infertility.
Microsurgical drainages by placing micro vascular bypasses between spermatic and inferior epigastric veins as proposed by Flati et al. have been successfully performed in treating male infertility due to varicocele. Microsurgical treatment has been shown to significantly improve fertility rate also in patients with recurrent varicocele who had previously undergone non microsurgical treatments.
Click on any of the following blue hyperlinks for more about Microsurgery:
___________________________________________________________________________
Robot-assisted Surgery:
Robotic surgery, computer-assisted surgery, and robotically-assisted surgery are terms for technological developments that use robotic systems to aid in surgical procedures. Robotically-assisted surgery was developed to overcome the limitations of pre-existing minimally-invasive surgical procedures and to enhance the capabilities of surgeons performing open surgery.
In the case of robotically-assisted minimally-invasive surgery, instead of directly moving the instruments, the surgeon uses one of two methods to control the instruments; either a direct telemanipulator or through computer control.
A telemanipulator is a remote manipulator that allows the surgeon to perform the normal movements associated with the surgery while the robotic arms carry out those movements using end-effectors and manipulators to perform the actual surgery on the patient.
In computer-controlled systems the surgeon uses a computer to control the robotic arms and its end-effectors, though these systems can also still use telemanipulators for their input. One advantage of using the computerised method is that the surgeon does not have to be present, but can be anywhere in the world, leading to the possibility for remote surgery.
In the case of enhanced open surgery, autonomous instruments (in familiar configurations) replace traditional steel tools, performing certain actions (such as rib spreading) with much smoother, feedback-controlled motions than could be achieved by a human hand.
The main object of such smart instruments is to reduce or eliminate the tissue trauma traditionally associated with open surgery without requiring more than a few minutes' training on the part of surgeons. This approach seeks to improve open surgeries, particularly cardio-thoracic, that have so far not benefited from minimally-invasive techniques.
Robotic surgery has been criticized for its expense, by one estimate costing $1,500 to $2000 more per patient.
Comparison to Traditional Methods:
Major advances aided by surgical robots have been remote surgery, minimally invasive surgery and unmanned surgery. Due to robotic use, the surgery is done with precision, miniaturization, smaller incisions; decreased blood loss, less pain, and quicker healing time. Articulation beyond normal manipulation and three-dimensional magnification helps resulting in improved ergonomics.
Due to these techniques there is a reduced duration of hospital stays, blood loss, transfusions, and use of pain medication. The existing open surgery technique has many flaws like limited access to surgical area, long recovery time, long hours of operation, blood loss, surgical scars and marks.
The robot normally costs $1,390,000 and while its disposable supply cost is normally $1,500 per procedure, the cost of the procedure is higher. Additional surgical training is needed to operate the system.
Numerous feasibility studies have been done to determine whether the purchase of such systems are worthwhile. As it stands, opinions differ dramatically. Surgeons report that, although the manufacturers of such systems provide training on this new technology, the learning phase is intensive and surgeons must operate on twelve to eighteen patients before they adapt.
During the training phase, minimally invasive operations can take up to twice as long as traditional surgery, leading to operating room tie ups and surgical staffs keeping patients under anesthesia for longer periods. Patient surveys indicate they chose the procedure based on expectations of decreased morbidity, improved outcomes, reduced blood loss and less pain. Higher expectations may explain higher rates of dissatisfaction and regret.
Compared with other minimally invasive surgery approaches, robot-assisted surgery gives the surgeon better control over the surgical instruments and a better view of the surgical site. In addition, surgeons no longer have to stand throughout the surgery and do not tire as quickly. Naturally occurring hand tremors are filtered out by the robot's computer software.
Finally, the surgical robot can continuously be used by rotating surgery teams.
Critics of the system, including the American Congress of Obstetricians and Gynecologists, say there is a steep learning curve for surgeons who adopt use of the system and that there's a lack of studies that indicate long-term results are superior to results following traditional laparoscopic surgery. Articles in the newly created Journal of Robotic Surgery tend to report on one surgeon's experience.
A Medicare study found that some procedures that have traditionally been performed with large incisions can be converted to "minimally invasive" endoscopic procedures with the use of the Da Vinci Surgical System, shortening length-of-stay in the hospital and reducing recovery times. But because of the hefty cost of the robotic system it is not clear that it is cost-effective for hospitals and physicians despite any benefits to patients since there is no additional reimbursement paid by the government or insurance companies when the system is used.
Robot-assisted pancreatectomies have been found to be associated with "longer operating time, lower estimated blood loss, a higher spleen-preservation rate, and shorter hospital stay[s]" than laparoscopic pancreatectomies; there was "no significant difference in transfusion, conversion to open surgery, overall complications, severe complications, pancreatic fistula, severe pancreatic fistula, ICU stay, total cost, and 30-day mortality between the two groups."
For surgical removal of the uterus and cervix for early cervical cancer, robotic and laparoscopic surgery resulted in similar outcomes with respect to the cancer.
Click on any of the following blue hyperlinks for more about Robot-assisted Surgery:
Microsurgery is a general term for surgery requiring an operating microscope. The most obvious developments have been procedures developed to allow anastomosis of successively smaller blood vessels and nerves (typically 1 mm in diameter) which have allowed transfer of tissue from one part of the body to another and re-attachment of severed parts.
Microsurgical techniques are utilized by several specialties today, such as:
- general surgery,
- ophthalmology,
- orthopedic surgery,
- gynecological surgery,
- otolaryngology,
- neurosurgery,
- oral and maxillofacial surgery,
- plastic surgery,
- podiatric surgery
- and pediatric surgery.
Free Tissue Transfer:
Main article: free flap
Free tissue transfer is a surgical reconstructive procedure using microsurgery. A region of "donor" tissue is selected that can be isolated on a feeding artery and vein; this tissue is usually a composite of several tissue types (e.g., skin, muscle, fat, bone).
Common donor regions include the rectus abdominis muscle, latissimus dorsi muscle, fibula, radial forearm bone and skin, and lateral arm skin. The composite tissue is transferred (moved as a free flap of tissue) to the region on the patient requiring reconstruction (e.g., mandible after oral cancer resection, breast after cancer resection, traumatic tissue loss, congenital tissue absence).
The vessels that supply the free flap are anastomosed with microsurgery to matching vessels (artery and vein) in the reconstructive site. The procedure was first done in the early 1970s and has become a popular "one-stage" (single operation) procedure for many surgical reconstructive applications.
Replantation:
Replantation is the reattachment of a completely detached body part.
Fingers and thumbs are the most common but the ear, scalp, nose, face, arm and penis have all been replanted.
Generally replantation involves restoring blood flow through arteries and veins, restoring the bony skeleton and connecting tendons and nerves as required.
Robert Malt and Charles Mckhann reported the first replantation two human upper extremities by microvascular means in 1964 with the first arm replanted in a child after a train injury in 1962 in Boston.
Initially, when the techniques were developed to make replantation possible, success was defined in terms of a survival of the amputated part alone. However, as more experience was gained in this field, surgeons specializing in replantation began to understand that survival of the amputated piece was not enough to ensure success of the replant.
In this way, functional demands of the amputated specimen became paramount in guiding which amputated pieces should and should not be replanted. Additional concerns about the patients ability to tolerate the long rehabilitation process that is necessary after replantation both on physical and psychological levels also became important.
So, when fingers are amputated, for instance, a replantation surgeon must seriously consider the contribution of the finger to the overall function of the hand. In this way, every attempt will be made to salvage an amputated thumb, since a great deal of hand function is dependent on the thumb, while an index finger or small finger may not be replanted, depending on the individual needs of the patient and the ability of the patient to tolerate a long surgery and a long course of rehabilitation.
However, if an amputated specimen is not able to be replanted to its original location entirely, this does not mean that the specimen is unreplantable. In fact, replantation surgeons have learned that only a piece or a portion may be necessary to obtain a functional result, or especially in the case of multiple amputated fingers, a finger or fingers may be transposed to a more useful location to obtain a more functional result. This concept is called "spare parts" surgery.
Transplantation:
Microsurgical techniques have played a crucial role in the development of transplantation immunological research because it allowed the use of rodents models, which are more appropriate for transplantation research (there are more reagents, monoclonal antibodies, knockout animals, and other immunological tools for mice and rats than other species).
Before it was introduced, transplant immunology was studied in rodents using the skin transplantation model, which is limited by the fact that it is not vascularized. Thus, microsurgery represents the link between surgery and transplant immunological research.
The first microsurgical experiments (porto-caval anastomosis in the rat) were performed by Dr. Sun Lee (pioneer of microsurgery) at the University of Pittsburgh in 1958. After a short time, many models of organ transplants in rat and mice have been established.
Today, virtually every rat or mouse organ can be transplanted with relative high success rate. Microsurgery was also important to develop new techniques of transplantation, that would be later performed in humans. In addition, it allows reconstruction of small arteries in clinical organ transplantation (e.g. accessory arteries in cadaver liver transplantation, polar arteries in renal transplantation and in living liver donor transplantation)
Treatment of Infertility:
Microsurgery has been used to treat several pathologic conditions leading to infertility such as tubal obstructions, vas deferens obstructions and varicocele which is one of the most frequent cause of male infertility.
Microsurgical drainages by placing micro vascular bypasses between spermatic and inferior epigastric veins as proposed by Flati et al. have been successfully performed in treating male infertility due to varicocele. Microsurgical treatment has been shown to significantly improve fertility rate also in patients with recurrent varicocele who had previously undergone non microsurgical treatments.
Click on any of the following blue hyperlinks for more about Microsurgery:
___________________________________________________________________________
Robot-assisted Surgery:
Robotic surgery, computer-assisted surgery, and robotically-assisted surgery are terms for technological developments that use robotic systems to aid in surgical procedures. Robotically-assisted surgery was developed to overcome the limitations of pre-existing minimally-invasive surgical procedures and to enhance the capabilities of surgeons performing open surgery.
In the case of robotically-assisted minimally-invasive surgery, instead of directly moving the instruments, the surgeon uses one of two methods to control the instruments; either a direct telemanipulator or through computer control.
A telemanipulator is a remote manipulator that allows the surgeon to perform the normal movements associated with the surgery while the robotic arms carry out those movements using end-effectors and manipulators to perform the actual surgery on the patient.
In computer-controlled systems the surgeon uses a computer to control the robotic arms and its end-effectors, though these systems can also still use telemanipulators for their input. One advantage of using the computerised method is that the surgeon does not have to be present, but can be anywhere in the world, leading to the possibility for remote surgery.
In the case of enhanced open surgery, autonomous instruments (in familiar configurations) replace traditional steel tools, performing certain actions (such as rib spreading) with much smoother, feedback-controlled motions than could be achieved by a human hand.
The main object of such smart instruments is to reduce or eliminate the tissue trauma traditionally associated with open surgery without requiring more than a few minutes' training on the part of surgeons. This approach seeks to improve open surgeries, particularly cardio-thoracic, that have so far not benefited from minimally-invasive techniques.
Robotic surgery has been criticized for its expense, by one estimate costing $1,500 to $2000 more per patient.
Comparison to Traditional Methods:
Major advances aided by surgical robots have been remote surgery, minimally invasive surgery and unmanned surgery. Due to robotic use, the surgery is done with precision, miniaturization, smaller incisions; decreased blood loss, less pain, and quicker healing time. Articulation beyond normal manipulation and three-dimensional magnification helps resulting in improved ergonomics.
Due to these techniques there is a reduced duration of hospital stays, blood loss, transfusions, and use of pain medication. The existing open surgery technique has many flaws like limited access to surgical area, long recovery time, long hours of operation, blood loss, surgical scars and marks.
The robot normally costs $1,390,000 and while its disposable supply cost is normally $1,500 per procedure, the cost of the procedure is higher. Additional surgical training is needed to operate the system.
Numerous feasibility studies have been done to determine whether the purchase of such systems are worthwhile. As it stands, opinions differ dramatically. Surgeons report that, although the manufacturers of such systems provide training on this new technology, the learning phase is intensive and surgeons must operate on twelve to eighteen patients before they adapt.
During the training phase, minimally invasive operations can take up to twice as long as traditional surgery, leading to operating room tie ups and surgical staffs keeping patients under anesthesia for longer periods. Patient surveys indicate they chose the procedure based on expectations of decreased morbidity, improved outcomes, reduced blood loss and less pain. Higher expectations may explain higher rates of dissatisfaction and regret.
Compared with other minimally invasive surgery approaches, robot-assisted surgery gives the surgeon better control over the surgical instruments and a better view of the surgical site. In addition, surgeons no longer have to stand throughout the surgery and do not tire as quickly. Naturally occurring hand tremors are filtered out by the robot's computer software.
Finally, the surgical robot can continuously be used by rotating surgery teams.
Critics of the system, including the American Congress of Obstetricians and Gynecologists, say there is a steep learning curve for surgeons who adopt use of the system and that there's a lack of studies that indicate long-term results are superior to results following traditional laparoscopic surgery. Articles in the newly created Journal of Robotic Surgery tend to report on one surgeon's experience.
A Medicare study found that some procedures that have traditionally been performed with large incisions can be converted to "minimally invasive" endoscopic procedures with the use of the Da Vinci Surgical System, shortening length-of-stay in the hospital and reducing recovery times. But because of the hefty cost of the robotic system it is not clear that it is cost-effective for hospitals and physicians despite any benefits to patients since there is no additional reimbursement paid by the government or insurance companies when the system is used.
Robot-assisted pancreatectomies have been found to be associated with "longer operating time, lower estimated blood loss, a higher spleen-preservation rate, and shorter hospital stay[s]" than laparoscopic pancreatectomies; there was "no significant difference in transfusion, conversion to open surgery, overall complications, severe complications, pancreatic fistula, severe pancreatic fistula, ICU stay, total cost, and 30-day mortality between the two groups."
For surgical removal of the uterus and cervix for early cervical cancer, robotic and laparoscopic surgery resulted in similar outcomes with respect to the cancer.
Click on any of the following blue hyperlinks for more about Robot-assisted Surgery:
- Uses:
- Miniature robotics
- History
- See also:
Reconstructive Surgery
YouTube Video: Plastic Surgery - Face Reconstruction - BBC Worldwide
Pictured: How a Severely Burned Former Firefighter Is Doing 1 Year After Face Transplant Surgery by ABC News
Reconstructive surgery is, in its broadest sense, the use of surgery to restore the form and function of the body; maxillo-facial surgeons, plastic surgeons and otolaryngologists do reconstructive surgery on faces after trauma and to reconstruct the head and neck after cancer.
Other branches of surgery (e.g., general surgery, gynecological surgery, pediatric surgery, cosmetic surgery, podiatric surgery) also perform some reconstructive procedures.
The common feature is that the operation attempts to restore the anatomy or the function of the body part to normal.
Reconstructive surgeons use the concept of a reconstructive ladder to manage increasingly complex wounds. This ranges from very simple techniques such as primary closure and dressings to more complex skin grafts, tissue expansion and free flaps.
Cosmetic surgery procedures include breast enhancement, reduction and lift, face lift, forehead lift, upper and lower eyelid surgery (blepharoplasty), laser skin resurfacing (laser resurfacing), chemical peel, nose reshaping (rhinoplasty), reconstruction liposuction, nasal reconstruction using the paramedian flap, as well as tummy tuck (abdominoplasty).
Many of these procedures are constantly being improved.
In 2010 only 10 research papers were identified which looked at reconstructive surgery after massive weight loss.
Use of implants and biomaterials:
Biomaterials are, in their simplest form, plastic implants used to correct or replace damaged body parts. Biomaterials were not used for reconstructive purposes until after World War II due to the new and improved technology and the tremendous need for the correction of damaged body parts that could replace transplantation.
The process involves scientific and medical research to ensure that the biomaterials are biocompatible and that they can assume the mechanical and functioning roles of the components they are replacing.
A successful implantation can best be achieved by a team that understands not only the anatomical, physiological, biochemical, and pathological aspects of the problem, but also comprehends bioengineering. Cellular and tissue engineering is crucial to know for reconstructive procedures.
An overview on the standardization and control of biomedical devices has recently been gathered by D. G. Singleton. Papers have covered in depth the U.S. Food and Drug Administration (FDA) Premarket Approval Process (J. L. Ely) and FDA regulations governing Class III devices.
Two papers have described how the National Bureau of Standards, American Dental Association, National Institute of Dental Research, and private dental companies have collaborated in a number of important advances in dental materials, devices, and analytical systems.
Other branches of surgery (e.g., general surgery, gynecological surgery, pediatric surgery, cosmetic surgery, podiatric surgery) also perform some reconstructive procedures.
The common feature is that the operation attempts to restore the anatomy or the function of the body part to normal.
Reconstructive surgeons use the concept of a reconstructive ladder to manage increasingly complex wounds. This ranges from very simple techniques such as primary closure and dressings to more complex skin grafts, tissue expansion and free flaps.
Cosmetic surgery procedures include breast enhancement, reduction and lift, face lift, forehead lift, upper and lower eyelid surgery (blepharoplasty), laser skin resurfacing (laser resurfacing), chemical peel, nose reshaping (rhinoplasty), reconstruction liposuction, nasal reconstruction using the paramedian flap, as well as tummy tuck (abdominoplasty).
Many of these procedures are constantly being improved.
In 2010 only 10 research papers were identified which looked at reconstructive surgery after massive weight loss.
Use of implants and biomaterials:
Biomaterials are, in their simplest form, plastic implants used to correct or replace damaged body parts. Biomaterials were not used for reconstructive purposes until after World War II due to the new and improved technology and the tremendous need for the correction of damaged body parts that could replace transplantation.
The process involves scientific and medical research to ensure that the biomaterials are biocompatible and that they can assume the mechanical and functioning roles of the components they are replacing.
A successful implantation can best be achieved by a team that understands not only the anatomical, physiological, biochemical, and pathological aspects of the problem, but also comprehends bioengineering. Cellular and tissue engineering is crucial to know for reconstructive procedures.
An overview on the standardization and control of biomedical devices has recently been gathered by D. G. Singleton. Papers have covered in depth the U.S. Food and Drug Administration (FDA) Premarket Approval Process (J. L. Ely) and FDA regulations governing Class III devices.
Two papers have described how the National Bureau of Standards, American Dental Association, National Institute of Dental Research, and private dental companies have collaborated in a number of important advances in dental materials, devices, and analytical systems.
Vascular Surgery
YouTube Video: What is Vascular Surgery?
Pictured: Illustration of the major arteries and veins comprising the human vascular system
Vascular surgery is a surgical subspecialty in which diseases of the vascular system, or arteries, veins and lymphatic circulation, are managed by medical therapy, minimally-invasive catheter procedures, and surgical reconstruction.
The specialty evolved from general and cardiac surgery as well as minimally invasive techniques pioneered by interventional radiology.
The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system except those of the heart and brain. Cardiothoracic surgeons and interventional cardiologists manage diseases of the heart vessels.
Neurosurgeons and interventional neuroradiologists surgically manage diseases of the vessels in the brain (e.g., intracranial aneurysms).
Scope:
Vascular surgery encompasses surgery of the aorta, carotid arteries, and lower extremities, including the iliac, femoral, and tibial arteries. Vascular surgery also involves surgery of veins, for conditions such as May–Thurner syndrome and for varicose veins. In some regions, vascular surgery also includes dialysis access surgery and transplant surgery.
Click here for the main disease categories and procedures associated with the vascular system.
Click on the following for more about Vascular Surgery:
The specialty evolved from general and cardiac surgery as well as minimally invasive techniques pioneered by interventional radiology.
The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system except those of the heart and brain. Cardiothoracic surgeons and interventional cardiologists manage diseases of the heart vessels.
Neurosurgeons and interventional neuroradiologists surgically manage diseases of the vessels in the brain (e.g., intracranial aneurysms).
Scope:
Vascular surgery encompasses surgery of the aorta, carotid arteries, and lower extremities, including the iliac, femoral, and tibial arteries. Vascular surgery also involves surgery of veins, for conditions such as May–Thurner syndrome and for varicose veins. In some regions, vascular surgery also includes dialysis access surgery and transplant surgery.
Click here for the main disease categories and procedures associated with the vascular system.
Click on the following for more about Vascular Surgery:
- History
- Investigations including Major trials
- Training
- See also
- Society for Vascular Surgery, the major American professional society
- Ischemia-repurfusion injuries of the appendicular musculoskeletal system
- Society for Vascular Surgery (U.S.)
- International Society for Vascular Surgery
Laser Technology in Medicine
YouTube Video of Laser Treatment for Lung Cancer Victims
Pictured: Example Laser Application in Dentistry
Laser medicine consists in the use of lasers in medical diagnosis, treatments, or therapies, such as laser photodynamic therapy.
Lasers used in medicine include in principle any type of laser, but especially:
Applications in Medicine:
Examples of procedures, practices, devices, and specialties where lasers are utilized include:
See Also:
Lasers used in medicine include in principle any type of laser, but especially:
- CO2 lasers, used to cut, vaporize, ablate and photo-coagulate soft tissue.
- diode lasers
- dye lasers
- excimer lasers
- fiber lasers
- gas lasers
- free electron lasers
- semiconductor diode lasers
Applications in Medicine:
Examples of procedures, practices, devices, and specialties where lasers are utilized include:
- angioplasty
- cancer diagnosis
- cancer treatment
- cosmetic dermatology such as scar revision, skin resurfacing, laser hair removal, tattoo removal
- dermatology, to treat melanoma
- frenectomy
- lithotripsy,
- laser mammography
- medical imaging
- microscopy
- ophthalmology (includes Lasik and laser photocoagulation)
- optical coherence tomography
- optogenetics
- prostatectomy
- plastic surgery, in laser liposuction
- surgery, to ablate and cauterize tissue
See Also:
- Dental laser
- Endovenous laser therapy
- Laser-assisted new attachment procedure
- Laser scalpel
- Laser surgery
- Light therapy
- Low level laser therapy
- Photodynamic therapy
- Photomedicine
- Soft-tissue laser surgery
Medical Robots
YouTube Video: da Vinci Robot Stitches a Grape Back Together
Pictured: A laparoscopic robotic surgery machine. Patient-side cart of the da Vinci surgical system.
A medical robot is a robot used in the medical sciences. They include, but are not limited to, surgical robots. These are in most telemanipulators, which use the surgeon's actions on one side to control the "effector" on the other side.
Types of Medical Robots:
Surgical robots: These robots either allow surgical operations to be carried out with greater precision than an unaided human surgeon, or allow remote surgery where a human surgeon is not physically present with the patient.
Rehabilitation robots: This group facilitates and supports the lives of infirm, elderly people, or those with dysfunction of body parts effecting movement. These robots are also used for rehabilitation and related procedures, such as training and therapy.
Biorobots: A group of robots designed to imitate the cognition of humans and animals.
Telepresence robots: Allow off-site medical professionals to move, look around, communicate, and participate from remote locations.
Pharmacy automation: Robotic systems to dispense oral solids in a retail pharmacy setting or preparing sterile IV admixtures in a hospital pharmacy setting.
Disinfection robot: has the capability to disinfect a whole room in mere minutes, generally using ultraviolet light technology. They are being used to fight Ebola virus disease. Pulsed light (PL) is a technique to decontaminate surfaces by killing MOs using pulses of an intense broad spectrum, rich in UV-C light. UV-C is the portion of the electromagnetic spectrum corresponding to the band between 200 and 280 nm. PL works with Xenon flash lamps that can produce flashes several times per second. Disinfection robots use pulsed UV light.
See also:
Types of Medical Robots:
Surgical robots: These robots either allow surgical operations to be carried out with greater precision than an unaided human surgeon, or allow remote surgery where a human surgeon is not physically present with the patient.
Rehabilitation robots: This group facilitates and supports the lives of infirm, elderly people, or those with dysfunction of body parts effecting movement. These robots are also used for rehabilitation and related procedures, such as training and therapy.
Biorobots: A group of robots designed to imitate the cognition of humans and animals.
Telepresence robots: Allow off-site medical professionals to move, look around, communicate, and participate from remote locations.
Pharmacy automation: Robotic systems to dispense oral solids in a retail pharmacy setting or preparing sterile IV admixtures in a hospital pharmacy setting.
Disinfection robot: has the capability to disinfect a whole room in mere minutes, generally using ultraviolet light technology. They are being used to fight Ebola virus disease. Pulsed light (PL) is a technique to decontaminate surfaces by killing MOs using pulses of an intense broad spectrum, rich in UV-C light. UV-C is the portion of the electromagnetic spectrum corresponding to the band between 200 and 280 nm. PL works with Xenon flash lamps that can produce flashes several times per second. Disinfection robots use pulsed UV light.
See also:
- Medical Robots Conference
- Where Are the Elder Care Robots?
- Notable Chinese Firms Emerging in Medical Robots Sector (IEEE)
A woman with a transplanted uterus just gave birth — a first for the U.S. by the Washington Post (December 3, 2017)
YouTube Video: A woman with a transplanted uterus just gave birth
Pictured: The first baby born as a result of a womb transplant in the United States lies in the neonatal unit at Baylor University Medical Center in Dallas. (Baylor University Medical Center via AP)
For women with uterine factor infertility who want to be mothers, the calculus has always been heartbreakingly simple: No uterus means no pregnancy.
The equation changed drastically in 2014, when Swedish doctors delivered a healthy 3.9-pound baby that was the result of a successful uterus transplant.
Now, doctors at Baylor University say a woman born without a uterus has delivered a baby after a successful transplant, the first time the surgery has worked outside of the Swedish hospital that pioneered the procedure.
The success marked another step forward for transplant surgery aimed at improving a person’s life, not just saving it. Doctors have performed penis transplants for wounded troops, given a young boy two new hands and given a new nose, lips, palate, eyelids and jaw to a woman who was gruesomely disfigured after she was shot in the face.
The fact that the uterus transplant success in Sweden can be replicated is a promising sign for thousands of women who have been unable to conceive. And doctors at Baylor have sought to expand the limits of the procedure, using donated uteri that didn’t come from family members and, in some cases, organs that came from cadavers.
“To make the field grow and expand and have the procedure come out to more women, it has to be reproduced,” said Liza Johannesson, a uterus transplant surgeon who left the Swedish team to join Baylor’s group, told the New York Times. “It was a very exciting birth. I’ve seen so many births and delivered so many babies, but this was a very special one.”
Baylor’s clinical trial was designed to include 10 women. Eight, including the new mother, have received the transplants so far. One recipient is pregnant, and two are trying to conceive. Four others had transplants that failed, and the organs had to be surgically removed.
[A 2-year-old’s kidney transplant was put on hold — after his donor father’s probation violation]
The surgeries differ from other transplants in one major way: They’re not intended to be permanent. Instead, they give a woman enough time to conceive a child. In vitro fertilized eggs are transferred to the woman’s womb, and after the baby is born, the uterus is removed via surgery.
That means the patient doesn’t have to spend a lifetime taking powerful drugs that suppress her immune system, which would put her at risk for dangerous long-term complications.
The university hasn’t released the names of the mother or the baby, saying they chose to remain anonymous.
But according to Tech Times, the donor uterus came from Taylor Siler, a Dallas nurse who has two children. She said she wanted to offer another woman a chance to give birth.
While this most recent birth is a step forward, uterine transplantation surgery is still in its very early days, and doctors conceded that there had been setbacks, particularly with the earliest volunteers.
In February 2016, Lindsey McFarland became the first woman to receive a uterus transplant in the United States. The organ came from a dead donor and was implanted during a nine-hour surgery.
Her story gave a sense of just how tenuous the nascent surgery is. She had to have her transplanted uterus removed after coming down with a yeast infection.
According to Newsweek, most of the women in Baylor’s trial had Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, which makes pregnancy and giving birth impossible.
And for most of their lives many had been told that they wouldn’t be able to have children.
“We do transplants all day long,” Giuliano Tesla, who heads the uterus transplant clinical trial at Baylor University Medical Center, told Time magazine. “This is not the same thing. I totally underestimated what this type of transplant does for these women. What I’ve learned emotionally, I do not have the words to describe.”
The equation changed drastically in 2014, when Swedish doctors delivered a healthy 3.9-pound baby that was the result of a successful uterus transplant.
Now, doctors at Baylor University say a woman born without a uterus has delivered a baby after a successful transplant, the first time the surgery has worked outside of the Swedish hospital that pioneered the procedure.
The success marked another step forward for transplant surgery aimed at improving a person’s life, not just saving it. Doctors have performed penis transplants for wounded troops, given a young boy two new hands and given a new nose, lips, palate, eyelids and jaw to a woman who was gruesomely disfigured after she was shot in the face.
The fact that the uterus transplant success in Sweden can be replicated is a promising sign for thousands of women who have been unable to conceive. And doctors at Baylor have sought to expand the limits of the procedure, using donated uteri that didn’t come from family members and, in some cases, organs that came from cadavers.
“To make the field grow and expand and have the procedure come out to more women, it has to be reproduced,” said Liza Johannesson, a uterus transplant surgeon who left the Swedish team to join Baylor’s group, told the New York Times. “It was a very exciting birth. I’ve seen so many births and delivered so many babies, but this was a very special one.”
Baylor’s clinical trial was designed to include 10 women. Eight, including the new mother, have received the transplants so far. One recipient is pregnant, and two are trying to conceive. Four others had transplants that failed, and the organs had to be surgically removed.
[A 2-year-old’s kidney transplant was put on hold — after his donor father’s probation violation]
The surgeries differ from other transplants in one major way: They’re not intended to be permanent. Instead, they give a woman enough time to conceive a child. In vitro fertilized eggs are transferred to the woman’s womb, and after the baby is born, the uterus is removed via surgery.
That means the patient doesn’t have to spend a lifetime taking powerful drugs that suppress her immune system, which would put her at risk for dangerous long-term complications.
The university hasn’t released the names of the mother or the baby, saying they chose to remain anonymous.
But according to Tech Times, the donor uterus came from Taylor Siler, a Dallas nurse who has two children. She said she wanted to offer another woman a chance to give birth.
While this most recent birth is a step forward, uterine transplantation surgery is still in its very early days, and doctors conceded that there had been setbacks, particularly with the earliest volunteers.
In February 2016, Lindsey McFarland became the first woman to receive a uterus transplant in the United States. The organ came from a dead donor and was implanted during a nine-hour surgery.
Her story gave a sense of just how tenuous the nascent surgery is. She had to have her transplanted uterus removed after coming down with a yeast infection.
According to Newsweek, most of the women in Baylor’s trial had Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, which makes pregnancy and giving birth impossible.
And for most of their lives many had been told that they wouldn’t be able to have children.
“We do transplants all day long,” Giuliano Tesla, who heads the uterus transplant clinical trial at Baylor University Medical Center, told Time magazine. “This is not the same thing. I totally underestimated what this type of transplant does for these women. What I’ve learned emotionally, I do not have the words to describe.”
Corneal Transplants
YouTube Video of Corneal Transplant Surgery
Corneal transplantation, also known as corneal grafting, is a surgical procedure where a damaged or diseased cornea is replaced by donated corneal tissue (the graft). When the entire cornea is replaced it is known as penetrating keratoplasty and when only part of the cornea is replaced it is known as lamellar keratoplasty.
Keratoplasty simply means surgery to the cornea. The graft is taken from a recently dead individual with no known diseases or other factors that may affect the chance of survival of the donated tissue or the health of the recipient.
The cornea is the transparent front part of the eye that covers the iris, pupil and anterior chamber. The surgical procedure is performed by ophthalmologists, physicians who specialize in eyes, and is often done on an outpatient basis. Donors can be of any age, as is shown in the case of Janis Babson, who donated her eyes at age 10. The corneal transplantation is performed when medicines, keratoconus conservative surgery and cross-linking cannot heal the cornea anymore.
Medical uses:
Indications include the following:
Risks:
The risks are similar to other intraocular procedures, but additionally include graft rejection (lifelong), detachment or displacement of lamellar transplants and primary graft failure.
There is also a risk of infection. Since the cornea has no blood vessels (it takes its nutrients from the aqueous humor) it heals much more slowly than a cut on the skin. While the wound is healing, it is possible that it might become infected by various microorganisms.
This risk is minimized by antibiotic prophylaxis (using antibiotic eyedrops, even when no infection exists).
There is a risk of cornea rejection, which occurs in about 20% of cases. Graft failure can occur at any time after the cornea has been transplanted, even years or decades later. The causes can vary, though it is usually due to new injury or illness. Treatment can be either medical or surgical, depending on the individual case. An early, technical cause of failure may be an excessively tight stitch cheesewiring through the sclera.
Procedures:
On the day of the surgery, the patient arrives to either a hospital or an outpatient surgery center, where the procedure will be performed. The patient is given a brief physical examination by the surgical team and is taken to the operating room. In the operating room, the patient lies down on an operating table and is either given general anesthesia, or local anesthesia and a sedative.
With anesthesia induced, the surgical team prepares the eye to be operated on and drapes the face around the eye. An eyelid speculum is placed to keep the lids open, and some lubrication is placed on the eye to prevent drying. In children, a metal ring is stitched to the sclera which will provide support of the sclera during the procedure.
Pre-operative examination:
In most instances, the person will meet with their ophthalmologist for an examination in the weeks or months preceding the surgery. During the exam, the ophthalmologist will examine the eye and diagnose the condition. The doctor will then discuss the condition with the patient, including the different treatment options available.
The doctor will also discuss the risks and benefits of the various options. If the patient elects to proceed with the surgery, the doctor will have the patient sign an informed consent form.
The doctor might also perform a physical examination and order lab tests, such as blood work, X-rays, or an EKG.
The surgery date and time will also be set, and the patient will be told where the surgery will take place. Within the United States, the supply of corneas is sufficient to meet the demand for surgery and research purposes. Therefore, unlike other tissues for transplantation, delays and shortages are not usually an issue.
Penetrating keratoplasty:
A trephine (a circular cutting device), which removes a circular disc of cornea, is used by the surgeon to cut the donor cornea. A second trephine is then used to remove a similar-sized portion of the patient's cornea. The donor tissue is then sewn in place with sutures.
Antibiotic eyedrops are placed, the eye is patched, and the patient is taken to a recovery area while the effects of the anesthesia wear off. The patient typically goes home following this and sees the doctor the following day for the first postoperative appointment.
Lamellar keratoplasty:
Lamellar keratoplasty encompasses several techniques which selectively replace diseased layers of the cornea while leaving healthy layers in place. The chief advantage is improved tectonic integrity of the eye. Disadvantages include the technically challenging nature of these procedures, which replace portions of a structure only 500 µm thick, and reduced optical performance of the donor/recipient interface compared to full-thickness keratoplasty.
Deep anterior lamellar keratoplasty:
In this procedure, the anterior layers of the central cornea are removed and replaced with donor tissue. Endothelial cells and the Descemets membrane are left in place. This technique is used in cases of anterior corneal opacifications, scars, and ectatic diseases such as keratoconus.
Endothelial keratoplasty:
Endothelial keratoplasty replaces the patient's endothelium with a transplanted disc of posterior stroma/Descemets/endothelium (DSEK) or Descemets/endothelium (DMEK).
This relatively new procedure has revolutionized treatment of disorders of the innermost layer of the cornea (endothelium). Unlike a full-thickness corneal transplant, the surgery can be performed with one or no sutures. Patients may recover functional vision in days to weeks, as opposed to up to a year with full thickness transplants.
However, an Australian study has shown that despite its benefits, the loss of endothelial cells that maintain transparency is much higher in DSEK compared to a full-thickness corneal transplant. The reason may be greater tissue manipulation during surgery, the study concluded.
During surgery the patient's corneal endothelium is removed and replaced with donor tissue. With DSEK, the donor includes a thin layer of stroma, as well as endothelium, and is commonly 100–150 µm thick. With DMEK, only the endothelium is transplanted. In the immediate postoperative period the donor tissue is held in position with an air bubble placed inside the eye (the anterior chamber). The tissue self-adheres in a short period and the air is adsorbed into the surrounding tissues.
Complications include displacement of the donor tissue requiring repositioning ("refloating"). This is more common with DMEK than DSEK. Folds in the donor tissue may reduce the quality of vision, requiring repair. Rejection of the donor tissue may require repeating the procedure. Gradual reduction in endothelial cell density over time can lead to loss of clarity and require repeating the procedure.
Patients with endothelial transplants frequently achieve best corrected vision in the 20/30 to 20/40 range, although some reach 20/20. Optical irregularity at the graft/host interface may limit vision below 20/20.
Synthetic corneas:
Main article: Keratoprosthesis
Boston keratoprosthesis:
The Boston keratoprosthesis is the most widely used synthetic cornea to date with over 900 procedures performed worldwide in 2008. The Boston KPro was developed at the Massachusetts Eye and Ear Infirmary under the leadership of Claes Dohlman, MD, PhD.
AlphaCor:
In cases where there have been several graft failures or the risk for keratoplasty is high, synthetic corneas can substitute successfully for donor corneas. Such a device contains a peripheral skirt and a transparent central region.
These two parts are connected on a molecular level by an interpenetrating polymer network, made from poly-2-hydroxyethyl methacrylate (pHEMA). AlphaCor is a U.S. FDA-approved type of synthetic cornea measuring 7.0 mm in diameter and 0.5 mm in thickness. The main advantages of synthetic corneas are that they are biocompatible, and the network between the parts and the device prevents complications that could arise at their interface. The probability of retention in one large study was estimated at 62% at 2 years follow-up.
Osteo-Odonto-Keratoprosthesis:
Main article: Osteo-Odonto-Keratoprosthesis
In a very rare and complex multi-step surgical procedure, employed to help the most disabled patients, a lamina of the person's tooth is grafted into the eye, with an artificial lens installed in the transplanted piece.
Prognosis:
The prognosis for visual restoration and maintenance of ocular health with corneal transplants is generally very good. Risks for failure or guarded prognoses are multifactorial. The type of transplant, the disease state requiring the procedure, the health of the other parts of the recipient eye and even the health of the donor tissue may all confer a more or less favorable prognosis.
The majority of corneal transplants result in significant improvement in visual function for many years or a lifetime. In cases of rejection or transplant failure, the surgery can generally be repeated.
Alternatives:
Contact lenses:
Different types of contact lenses may be used to delay or eliminate the need for corneal transplantation in corneal disorders.
Phototherapeutic keratectomy:
Diseases that only affect the surface of the cornea can be treated with an operation called phototherapeutic keratectomy (PTK). With the precision of an excimer laser and a modulating agent coating the eye, irregularities on the surface can be removed. However, in most of the cases where corneal transplantation is recommended, PTK would not be effective.
Intrastromal corneal ring segments:
In corneal disorders where vision correction is not possible by using contact lenses, intrastromal corneal ring segments may be used to flatten the cornea, which is intended to relieve the nearsightedness and astigmatism.
In this procedure, an ophthalmologist makes an incision in the cornea of the eye, and inserts two crescent or semi-circular shaped ring segments between the layers of the corneal stroma, one on each side of the pupil.
Intrastromal corneal rings were approved in 2004 by the Food and Drug Administration for people with keratoconus who cannot adequately correct their vision with glasses or contact lenses. They were approved under the Humanitarian Device Exemption, which means the manufacturer did not have to demonstrate effectiveness.
Corneal collagen cross-linking:
Corneal collagen cross-linking may delay or eliminate the need for corneal transplantation in keratoconus and post-LASIK ectasia, however as of 2015 it is lacking sufficient evidence to determine if it is useful in keratoconus.
Epidemiology:
Corneal transplant is one of the most common transplant procedures. Although approximately 100,000 procedures are performed worldwide each year, some estimates report that 10,000,000 people are affected by various disorders that would benefit from corneal transplantation.
In Australia, approximately 1,500 grafts are performed each year. According to the NHS Blood and Transplant, over 2,300 corneal transplant procedures are performed each year in the United Kingdom. Between April 1, 2005 and March 31, 2006, 2,503 people received corneal transplants in the UK.
Click on any of the following blue hyperlinks for more about Corneal Transplants:
Keratoplasty simply means surgery to the cornea. The graft is taken from a recently dead individual with no known diseases or other factors that may affect the chance of survival of the donated tissue or the health of the recipient.
The cornea is the transparent front part of the eye that covers the iris, pupil and anterior chamber. The surgical procedure is performed by ophthalmologists, physicians who specialize in eyes, and is often done on an outpatient basis. Donors can be of any age, as is shown in the case of Janis Babson, who donated her eyes at age 10. The corneal transplantation is performed when medicines, keratoconus conservative surgery and cross-linking cannot heal the cornea anymore.
Medical uses:
Indications include the following:
- Optical: To improve visual acuity by replacing the opaque or distorted host tissue by clear healthy donor tissue. The most common indication in this category is pseudophakic bullous keratopathy, followed by keratoconus, corneal degeneration, keratoglobus and dystrophy, as well as scarring due to keratitis and trauma.
- Tectonic/reconstructive: To preserve corneal anatomy and integrity in patients with stromal thinning and descemetoceles, or to reconstruct the anatomy of the eye, e.g. after corneal perforation.
- Therapeutic: To remove inflamed corneal tissue unresponsive to treatment by antibiotics or anti-virals.
- Cosmetic: To improve the appearance of patients with corneal scars that have given a whitish or opaque hue to the cornea.
Risks:
The risks are similar to other intraocular procedures, but additionally include graft rejection (lifelong), detachment or displacement of lamellar transplants and primary graft failure.
There is also a risk of infection. Since the cornea has no blood vessels (it takes its nutrients from the aqueous humor) it heals much more slowly than a cut on the skin. While the wound is healing, it is possible that it might become infected by various microorganisms.
This risk is minimized by antibiotic prophylaxis (using antibiotic eyedrops, even when no infection exists).
There is a risk of cornea rejection, which occurs in about 20% of cases. Graft failure can occur at any time after the cornea has been transplanted, even years or decades later. The causes can vary, though it is usually due to new injury or illness. Treatment can be either medical or surgical, depending on the individual case. An early, technical cause of failure may be an excessively tight stitch cheesewiring through the sclera.
Procedures:
On the day of the surgery, the patient arrives to either a hospital or an outpatient surgery center, where the procedure will be performed. The patient is given a brief physical examination by the surgical team and is taken to the operating room. In the operating room, the patient lies down on an operating table and is either given general anesthesia, or local anesthesia and a sedative.
With anesthesia induced, the surgical team prepares the eye to be operated on and drapes the face around the eye. An eyelid speculum is placed to keep the lids open, and some lubrication is placed on the eye to prevent drying. In children, a metal ring is stitched to the sclera which will provide support of the sclera during the procedure.
Pre-operative examination:
In most instances, the person will meet with their ophthalmologist for an examination in the weeks or months preceding the surgery. During the exam, the ophthalmologist will examine the eye and diagnose the condition. The doctor will then discuss the condition with the patient, including the different treatment options available.
The doctor will also discuss the risks and benefits of the various options. If the patient elects to proceed with the surgery, the doctor will have the patient sign an informed consent form.
The doctor might also perform a physical examination and order lab tests, such as blood work, X-rays, or an EKG.
The surgery date and time will also be set, and the patient will be told where the surgery will take place. Within the United States, the supply of corneas is sufficient to meet the demand for surgery and research purposes. Therefore, unlike other tissues for transplantation, delays and shortages are not usually an issue.
Penetrating keratoplasty:
A trephine (a circular cutting device), which removes a circular disc of cornea, is used by the surgeon to cut the donor cornea. A second trephine is then used to remove a similar-sized portion of the patient's cornea. The donor tissue is then sewn in place with sutures.
Antibiotic eyedrops are placed, the eye is patched, and the patient is taken to a recovery area while the effects of the anesthesia wear off. The patient typically goes home following this and sees the doctor the following day for the first postoperative appointment.
Lamellar keratoplasty:
Lamellar keratoplasty encompasses several techniques which selectively replace diseased layers of the cornea while leaving healthy layers in place. The chief advantage is improved tectonic integrity of the eye. Disadvantages include the technically challenging nature of these procedures, which replace portions of a structure only 500 µm thick, and reduced optical performance of the donor/recipient interface compared to full-thickness keratoplasty.
Deep anterior lamellar keratoplasty:
In this procedure, the anterior layers of the central cornea are removed and replaced with donor tissue. Endothelial cells and the Descemets membrane are left in place. This technique is used in cases of anterior corneal opacifications, scars, and ectatic diseases such as keratoconus.
Endothelial keratoplasty:
Endothelial keratoplasty replaces the patient's endothelium with a transplanted disc of posterior stroma/Descemets/endothelium (DSEK) or Descemets/endothelium (DMEK).
This relatively new procedure has revolutionized treatment of disorders of the innermost layer of the cornea (endothelium). Unlike a full-thickness corneal transplant, the surgery can be performed with one or no sutures. Patients may recover functional vision in days to weeks, as opposed to up to a year with full thickness transplants.
However, an Australian study has shown that despite its benefits, the loss of endothelial cells that maintain transparency is much higher in DSEK compared to a full-thickness corneal transplant. The reason may be greater tissue manipulation during surgery, the study concluded.
During surgery the patient's corneal endothelium is removed and replaced with donor tissue. With DSEK, the donor includes a thin layer of stroma, as well as endothelium, and is commonly 100–150 µm thick. With DMEK, only the endothelium is transplanted. In the immediate postoperative period the donor tissue is held in position with an air bubble placed inside the eye (the anterior chamber). The tissue self-adheres in a short period and the air is adsorbed into the surrounding tissues.
Complications include displacement of the donor tissue requiring repositioning ("refloating"). This is more common with DMEK than DSEK. Folds in the donor tissue may reduce the quality of vision, requiring repair. Rejection of the donor tissue may require repeating the procedure. Gradual reduction in endothelial cell density over time can lead to loss of clarity and require repeating the procedure.
Patients with endothelial transplants frequently achieve best corrected vision in the 20/30 to 20/40 range, although some reach 20/20. Optical irregularity at the graft/host interface may limit vision below 20/20.
Synthetic corneas:
Main article: Keratoprosthesis
Boston keratoprosthesis:
The Boston keratoprosthesis is the most widely used synthetic cornea to date with over 900 procedures performed worldwide in 2008. The Boston KPro was developed at the Massachusetts Eye and Ear Infirmary under the leadership of Claes Dohlman, MD, PhD.
AlphaCor:
In cases where there have been several graft failures or the risk for keratoplasty is high, synthetic corneas can substitute successfully for donor corneas. Such a device contains a peripheral skirt and a transparent central region.
These two parts are connected on a molecular level by an interpenetrating polymer network, made from poly-2-hydroxyethyl methacrylate (pHEMA). AlphaCor is a U.S. FDA-approved type of synthetic cornea measuring 7.0 mm in diameter and 0.5 mm in thickness. The main advantages of synthetic corneas are that they are biocompatible, and the network between the parts and the device prevents complications that could arise at their interface. The probability of retention in one large study was estimated at 62% at 2 years follow-up.
Osteo-Odonto-Keratoprosthesis:
Main article: Osteo-Odonto-Keratoprosthesis
In a very rare and complex multi-step surgical procedure, employed to help the most disabled patients, a lamina of the person's tooth is grafted into the eye, with an artificial lens installed in the transplanted piece.
Prognosis:
The prognosis for visual restoration and maintenance of ocular health with corneal transplants is generally very good. Risks for failure or guarded prognoses are multifactorial. The type of transplant, the disease state requiring the procedure, the health of the other parts of the recipient eye and even the health of the donor tissue may all confer a more or less favorable prognosis.
The majority of corneal transplants result in significant improvement in visual function for many years or a lifetime. In cases of rejection or transplant failure, the surgery can generally be repeated.
Alternatives:
Contact lenses:
Different types of contact lenses may be used to delay or eliminate the need for corneal transplantation in corneal disorders.
Phototherapeutic keratectomy:
Diseases that only affect the surface of the cornea can be treated with an operation called phototherapeutic keratectomy (PTK). With the precision of an excimer laser and a modulating agent coating the eye, irregularities on the surface can be removed. However, in most of the cases where corneal transplantation is recommended, PTK would not be effective.
Intrastromal corneal ring segments:
In corneal disorders where vision correction is not possible by using contact lenses, intrastromal corneal ring segments may be used to flatten the cornea, which is intended to relieve the nearsightedness and astigmatism.
In this procedure, an ophthalmologist makes an incision in the cornea of the eye, and inserts two crescent or semi-circular shaped ring segments between the layers of the corneal stroma, one on each side of the pupil.
Intrastromal corneal rings were approved in 2004 by the Food and Drug Administration for people with keratoconus who cannot adequately correct their vision with glasses or contact lenses. They were approved under the Humanitarian Device Exemption, which means the manufacturer did not have to demonstrate effectiveness.
Corneal collagen cross-linking:
Corneal collagen cross-linking may delay or eliminate the need for corneal transplantation in keratoconus and post-LASIK ectasia, however as of 2015 it is lacking sufficient evidence to determine if it is useful in keratoconus.
Epidemiology:
Corneal transplant is one of the most common transplant procedures. Although approximately 100,000 procedures are performed worldwide each year, some estimates report that 10,000,000 people are affected by various disorders that would benefit from corneal transplantation.
In Australia, approximately 1,500 grafts are performed each year. According to the NHS Blood and Transplant, over 2,300 corneal transplant procedures are performed each year in the United Kingdom. Between April 1, 2005 and March 31, 2006, 2,503 people received corneal transplants in the UK.
Click on any of the following blue hyperlinks for more about Corneal Transplants:
- History
- Research
- Society and culture
- Facts About the Cornea and Corneal Disease The National Eye Institute (NEI)
Virtual Healthcare: The future of Medicine? YouTube Video: This Is What The Future Of Health Care Looks Like Pictured below: The eHealth Enhanced Chronic Care Model: A Theory Derivation Approach
eHealth (also written e-health) is a relatively recent healthcare practice supported by electronic processes and communication, dating back to at least 1999. Usage of the term varies. A study in 2005 found 51 unique definitions.
Some argue that it is interchangeable with health informatics with a broad definition covering electronic/digital processes in health while others use it in the narrower sense of healthcare practice using the Internet.
It can also include health applications and links on mobile phones, referred to as mHealth or m-Health. Since about 2011, the increasing recognition of the need for better cyber-security and regulation may result in the need for these specialized resources to develop safer eHealth solutions that can withstand these growing threats.
The term can encompass a range of services or systems that are at the edge of medicine/healthcare and information technology, including:
Several authors have noted the variable usage in the term, from being specific to the use of the Internet in healthcare to being generally around any use of computers in healthcare.
Various authors have considered the evolution of the term and its usage and how this maps to changes in health informatics and healthcare generally.Oh et al., in a 2005 systematic review of the term's usage, offered the definition of eHealth as a set of technological themes in health today, more specifically based on commerce, activities, stakeholders, outcomes, locations, or perspectives.
One thing that all sources seem to agree on is that e-Health initiatives do not originate with the patient, though the patient may be a member of a patient organization that seeks to do this, as in the e-Patient movement.
Click on any of the following blue hyperlinks for more about eHealth:
Telemedicine is the use of telecommunication and information technology to provide clinical health care from a distance. It has been used to overcome distance barriers and to improve access to medical services that would often not be consistently available in distant rural communities. It is also used to save lives in critical care and emergency situations.
Although there were distant precursors to telemedicine, it is essentially a product of 20th century telecommunication and information technologies. These technologies permit communications between patient and medical staff with both convenience and fidelity, as well as the transmission of medical, imaging and health informatics data from one site to another.
Early forms of telemedicine achieved with telephone and radio have been supplemented with videotelephony, advanced diagnostic methods supported by distributed client/server applications, and additionally with telemedical devices to support in-home care.
The definition of telemedicine is somewhat controversial. Some definitions (such as the definition given by the World Health Organization) include all aspects of healthcare including preventive care. The American Telemedicine Association uses the terms telemedicine and telehealth interchangeably, although it acknowledges that telehealth is sometimes used more broadly for remote health not involving active clinical treatments.
eHealth is another related term, used particularly in the U.K. and Europe, as an umbrella term that includes telehealth, electronic medical records, and other components of health information technology.
Benefits and Drawbacks:
Telemedicine can be beneficial to patients in isolated communities and remote regions, who can receive care from doctors or specialists far away without the patient having to travel to visit them.
Recent developments in mobile collaboration technology can allow healthcare professionals in multiple locations to share information and discuss patient issues as if they were in the same place.
Remote patient monitoring through mobile technology can reduce the need for outpatient visits and enable remote prescription verification and drug administration oversight, potentially significantly reducing the overall cost of medical care. Telemedicine can also facilitate medical education by allowing workers to observe experts in their fields and share best practices more easily.
Telemedicine can eliminate the possible transmission of infectious diseases or parasites between patients and medical staff. This is particularly an issue where MRSA is a concern. Additionally, some patients who feel uncomfortable in a doctors office may do better remotely. For example, white coat syndrome may be avoided. Patients who are home-bound and would otherwise require an ambulance to move them to a clinic are also a consideration.
The downsides of telemedicine include the cost of telecommunication and data management equipment and of technical training for medical personnel who will employ it. Virtual medical treatment also entails potentially decreased human interaction between medical professionals and patients, an increased risk of error when medical services are delivered in the absence of a registered professional, and an increased risk that protected health information may be compromised through electronic storage and transmission.
There is also a concern that telemedicine may actually decrease time efficiency due to the difficulties of assessing and treating patients through virtual interactions; for example, it has been estimated that a teledermatology consultation can take up to thirty minutes, whereas fifteen minutes is typical for a traditional consultation.
Additionally, potentially poor quality of transmitted records, such as images or patient progress reports, and decreased access to relevant clinical information are quality assurance risks that can compromise the quality and continuity of patient care for the reporting doctor.
Other obstacles to the implementation of telemedicine include unclear legal regulation for some telemedical practices and difficulty claiming reimbursement from insurers or government programs in some fields.
Another disadvantage of telemedicine is the inability to start treatment immediately. For example, a patient suffering from a bacterial infection might be given an antibiotic hypodermic injection in the clinic, and observed for any reaction, before that antibiotic is prescribed in pill form.
Click on any of the following blue hyperlinks for more about Telemedicine:
Digital health is the convergence of digital and genomic technologies with health, healthcare, living, and society to enhance the efficiency of healthcare delivery and make medicines more personalized and precise.
The discipline involves the use of information and communication technologies to help address the health problems and challenges faced by patients. These technologies include both hardware and software solutions and services, including telemedicine, web-based analysis, email, mobile phones and applications, text messages, and clinic or remote monitoring sensors.
Generally, digital health is concerned about the development of interconnected health systems to improve the use of computational technologies, smart devices, computational analysis techniques and communication media to aid healthcare professionals and patients manage illnesses and health risks, as well as promote health and wellbeing.
Digital health is a multi-disciplinary domain which involves many stakeholders, including clinicians, researchers and scientists with a wide range of expertise in healthcare, engineering, social sciences, public health, health economics and management.
Elements:
As an outgrowth of the Digital Revolution characterized by "the mass production and widespread use of digital logic circuits, and its derived technologies, including the computer, digital cellular phone, and the Internet," key elements of digital health include wireless devices, hardware sensors and software sensing technologies, microprocessors and integrated circuits, the Internet, social networking, mobile/cellular networks and body area networks, health information technology, genomics, and personal genetic information.
Domains:
Various domains span digital health. These include Healthcare technology assessment and monitoring to prevent, diagnose or treat diseases, monitoring of patients, or for rehabilitation or long-term care.
Such technologies include Assistive technologies and rehabilitation robotics for people with disabilities so as to aid in their independence to perform daily tasks, unobtrusive monitoring sensors and wearable devices.
Clinical decision support aids clinicians at the point of care, including diagnosis, analysis and interpretation of patient-related data.Computational simulations, modeling and machine learning approaches can model health-related outcomes. E-health delivers health information and services to enable data transmition, storage and retrievial for clinical, educational and administrative purposes.
Health systems engineering applications in health care systems, includes knowledge discovery, decision making, optimization, human factors engineering, quality engineering, and information technology and communication. Human-computer-environment interactions Human-computer interaction principles tend to be based around user-centered, experience-centered or activity-centered designs.
Virtual reality, video gaming rehabilitation, and serious games to provide a social and interactive experience for healthcare student and patient education. Speech and hearing systems for natural language processing, speech recognition techniques, and medical devices can aid in speech and hearing (e.g. cochlear implants).Telehealth, telemedicine, telecare, telecoaching and telerehabilitation provide various forms of patient care remotely at a distance.
Implementation:
National digital programs exist to support healthcare, such as those of Canada Health Infoway built on core systems of patient and provider registries, clinical and diagnostic imaging systems, clinical reports and immunizations. By 2014, 75% of Canadian physicians were using electronic medical records.
In Uganda and Mozambique, partnerships between patients with cell phones, local and regional governments, technologists, non-governmental organizations, academia, and industry have enabled mHealth solutions.
Innovation cycle:
The innovation process for digital health is an iterative cycle for technological solutions classified into five main activity processes beginning from the identification of the healthcare problem, research, digital solution, evaluating the solution to implementation in working clinical practices.
___________________________________________________________________________
Online doctor is a term that emerged during the 2000s, used by both the media and academics, to describe a generation of physicians and health practitioners who deliver healthcare, including drug prescription, over the internet.
Emergence of online doctors:
In the 2000s, many people came to treat the internet as a first, or at least a major, source of information and communication. Health advice is now the second-most popular topic, after pornography, that people search for on the internet.
With the advent of broadband and videoconferencing, many individuals have turned to online doctors to receive online consultations and purchase prescription drugs. Use of this technology has many advantages for both the doctor and the patient, including cost savings, convenience, accessibility, and improved privacy and communication.
In the US, a 2006 study found that searching for information on prescription or over-the-counter drugs was the fifth most popular search topic, and a 2004 study found that 4% of Americans had purchased prescription medications online.
A 2009 survey conducted by Geneva-based Health On the Net Foundation found one-in-ten Europeans buys medicines from websites and one-third claim to use online consultation.
In Germany, approximately seven million people buy from mail-order pharmacies, and mail-order sales account for approximately 8–10% of total pharmaceutical sales.
In 2008, the Royal Pharmaceutical Society of Great Britain reported that approximately two million people in Great Britain were regularly purchasing pharmaceuticals online (both with a prescription from registered online UK doctors and without prescriptions from other websites).
A recent survey commissioned by Pfizer, the Medicines and Healthcare products Regulatory Agency, RPSGB, the Patients Association and HEART UK found that 15% of the British adults asked had bought a prescription-only medicine online.
In developed countries, many online doctors prescribe so-called ‘lifestyle drugs’, such as for weight loss, hair loss or erectile dysfunction. The RPSGB has identified the most popular products prescribed online as Prozac (an antidepressant), Viagra (for erectile dysfunction), Valium (a tranquiliser), Ritalin (a psychostimulant), Serostim (a synthetic growth hormone) and Provigil (a psychostimulant).
A study in the USA has also shown that antibiotics are commonly available online without prescription.
Potential Harm:
Traditionalist critics of online doctors argue that an online doctor cannot provide proper examinations or diagnosis either by email or video call. Such consultations, they argue, will always be dangerous, with the potential for serious disease to be missed. There are also concerns that the absence of proximity leads to treatment by unqualified doctors or patients using false information to secure dangerous drugs.
Proponents argue there is little difference between an e-mail consultation and the sort of telephone assessment and advice that doctors regularly make out of hours or in circumstances where doctors cannot physically examine a patient (e.g., jungle medicine).
Laurence Buckman, chairman of the British Medical Association’s GPs’ committee, says that online consultations make life easier for doctors and patients when used properly. "Many GPs will be very happy with it and it could be useful. When it’s a regular patient you know well, it follows on from telephone consulting.
Voice is essential, vision is desirable. The problem comes when I don’t know the patient". Niall Dickson, chief executive of the General Medical Council, says: "We trust doctors to use their judgement to decide whether they should see a patient in person. Online consultations will be appropriate for some patients, whereas other patients will need a physical examination or may benefit from seeing their doctor in person".
Past and Future Developments
The first medical consulting website in the US was WebMD, founded in 1996 by Jim Clark (one of the founders of Netscape) and Pavan Nigam as Healthscape. Currently, its website carries information regarding health and health care, including a symptom checklist, pharmacy information, drug information, blogs of physicians with specific topics, and a place to store personal medical information.
As of February 2011, WebMD’s network of sites reaches an average of 86.4 million visitors per month and is the leading health portal in the United States.
Other popular US healthcare and medical consulting sites include the following:
Many have experienced dramatic growth. (Healthline, launched in 2005, grew by 269% to 2.7 million average monthly unique visitors in Q1 2007 from 0.8 million average monthly unique visitors in Q1 2006).
Niche consulting sites are also popular including SeniorNet, which deals with age-related syndromes and 4collegewomen.org and GirlsHealth.gov, which target young women.
Several American online doctor companies, including Sherpaa, MDlive, Teladoc, First Stop Health, American Well, WebDoc247, MeMD, and Ringadoc, provide consultations with doctors over the phone or the Internet. Prominent San Francisco-based venture capital firm Founders Fund called such services "extraordinarily fast" and predicted that they will "bring relief to thousands of people with immediate medical needs".
In the UK, e-med was the first online health site to offer both a diagnosis and prescriptions to patients over the Internet. It was established in March 2000 by Dr. Julian Eden, In 2010, DrThom claimed to have 100,000 patients visit their site
NHS Direct (currently NHS Choices) is the free health advice and information service provided by the National Health Service (NHS) for residents and visitors in the UK, with advice offered 24 hours a day via telephone and web contact.
Over 1.5 million patients visit the website every month. More recently, a number of online doctors have emerged in the country, firms such as Now Healthcare Group, Dr Fox Pharmacy, Push Doctor and Lloyds Pharmacy offer consultation and prescriptions via the Internet.
In Australia HealthDirect is the free health advice and information service provided by the government with advice offered 24 hours a day via telephone. Medicare began funding online consultations for specialists on 1 July 2011 which has seen a slow but steady increase in volumes.
New advances in digital information technology mean that in future online doctors and healthcare websites may offer advanced scanning and diagnostic services over the internet.
The Nuffield Council on Bioethics identifies such services as direct-to-consumer body imaging (such as CT and MRI scans) and personal genetic profiling for individual susceptibility to disease. Professor Sir Bruce Keogh, the medical director of the UK NHS, is drawing up plans to introduce online consultations via Skype and has said IT will "completely change the way [doctors] deliver medicine".
This concept is gaining more importance and there are some companies who started cashing on it, few companies like Zocdoc have started providing online doctor booking service.
See also:
Some argue that it is interchangeable with health informatics with a broad definition covering electronic/digital processes in health while others use it in the narrower sense of healthcare practice using the Internet.
It can also include health applications and links on mobile phones, referred to as mHealth or m-Health. Since about 2011, the increasing recognition of the need for better cyber-security and regulation may result in the need for these specialized resources to develop safer eHealth solutions that can withstand these growing threats.
The term can encompass a range of services or systems that are at the edge of medicine/healthcare and information technology, including:
- Electronic health record: enabling the communication of patient data between different healthcare professionals (GPs, specialists etc.);
- Computerized physician order entry: a means of requesting diagnostic tests and treatments electronically and receiving the results
- ePrescribing: access to prescribing options, printing prescriptions to patients and sometimes electronic transmission of prescriptions from doctors to pharmacists
- Clinical decision support system: providing information electronically about protocols and standards for healthcare professionals to use in diagnosing and treating patients.
- Telemedicine: physical and psychological diagnosis and treatments at a distance, including telemonitoring of patients functions;
- Consumer health informatics: use of electronic resources on medical topics by healthy individuals or patients;
- Health knowledge management: e.g. in an overview of latest medical journals, best practice guidelines or epidemiological tracking (examples include physician resources such as Medscape and MDLinx);
- Virtual healthcare teams: consisting of healthcare professionals who collaborate and share information on patients through digital equipment (for transmural care);
- mHealth or m-Health: includes the use of mobile devices in collecting aggregate and patient-level health data, providing healthcare information to practitioners, researchers, and patients, real-time monitoring of patient vitals, and direct provision of care (via mobile telemedicine);
- Medical research using grids: powerful computing and data management capabilities to handle large amounts of heterogeneous data.
- Health informatics / healthcare information systems: also often refer to software solutions for appointment scheduling, patient data management, work schedule management and other administrative tasks surrounding health
Several authors have noted the variable usage in the term, from being specific to the use of the Internet in healthcare to being generally around any use of computers in healthcare.
Various authors have considered the evolution of the term and its usage and how this maps to changes in health informatics and healthcare generally.Oh et al., in a 2005 systematic review of the term's usage, offered the definition of eHealth as a set of technological themes in health today, more specifically based on commerce, activities, stakeholders, outcomes, locations, or perspectives.
One thing that all sources seem to agree on is that e-Health initiatives do not originate with the patient, though the patient may be a member of a patient organization that seeks to do this, as in the e-Patient movement.
Click on any of the following blue hyperlinks for more about eHealth:
- eHealth literacy
- Data exchange
- Early adopters
- E-mental health
- Cybermedicine
- Self-monitoring healthcare devices
- Evaluation
- In developing countries
- See also:
- Center for Telehealth and E-Health Law
- eHealthInsurance
- EUDRANET
- European Institute for Health Records
- Health 2.0
- Health blog
- Technology and mental health issues
- Telehealth
- "ehealth news". ehealth.
- "NorthWest EHealth". NWEH.
- "The eHeatlhQ Seal". Internet Medical Society.
- "Virtual Healthcare Trends". Anna Maria Online. Anna Maria College.
- "The Digital Health Care Environment". Saint Joseph's University.
Telemedicine is the use of telecommunication and information technology to provide clinical health care from a distance. It has been used to overcome distance barriers and to improve access to medical services that would often not be consistently available in distant rural communities. It is also used to save lives in critical care and emergency situations.
Although there were distant precursors to telemedicine, it is essentially a product of 20th century telecommunication and information technologies. These technologies permit communications between patient and medical staff with both convenience and fidelity, as well as the transmission of medical, imaging and health informatics data from one site to another.
Early forms of telemedicine achieved with telephone and radio have been supplemented with videotelephony, advanced diagnostic methods supported by distributed client/server applications, and additionally with telemedical devices to support in-home care.
The definition of telemedicine is somewhat controversial. Some definitions (such as the definition given by the World Health Organization) include all aspects of healthcare including preventive care. The American Telemedicine Association uses the terms telemedicine and telehealth interchangeably, although it acknowledges that telehealth is sometimes used more broadly for remote health not involving active clinical treatments.
eHealth is another related term, used particularly in the U.K. and Europe, as an umbrella term that includes telehealth, electronic medical records, and other components of health information technology.
Benefits and Drawbacks:
Telemedicine can be beneficial to patients in isolated communities and remote regions, who can receive care from doctors or specialists far away without the patient having to travel to visit them.
Recent developments in mobile collaboration technology can allow healthcare professionals in multiple locations to share information and discuss patient issues as if they were in the same place.
Remote patient monitoring through mobile technology can reduce the need for outpatient visits and enable remote prescription verification and drug administration oversight, potentially significantly reducing the overall cost of medical care. Telemedicine can also facilitate medical education by allowing workers to observe experts in their fields and share best practices more easily.
Telemedicine can eliminate the possible transmission of infectious diseases or parasites between patients and medical staff. This is particularly an issue where MRSA is a concern. Additionally, some patients who feel uncomfortable in a doctors office may do better remotely. For example, white coat syndrome may be avoided. Patients who are home-bound and would otherwise require an ambulance to move them to a clinic are also a consideration.
The downsides of telemedicine include the cost of telecommunication and data management equipment and of technical training for medical personnel who will employ it. Virtual medical treatment also entails potentially decreased human interaction between medical professionals and patients, an increased risk of error when medical services are delivered in the absence of a registered professional, and an increased risk that protected health information may be compromised through electronic storage and transmission.
There is also a concern that telemedicine may actually decrease time efficiency due to the difficulties of assessing and treating patients through virtual interactions; for example, it has been estimated that a teledermatology consultation can take up to thirty minutes, whereas fifteen minutes is typical for a traditional consultation.
Additionally, potentially poor quality of transmitted records, such as images or patient progress reports, and decreased access to relevant clinical information are quality assurance risks that can compromise the quality and continuity of patient care for the reporting doctor.
Other obstacles to the implementation of telemedicine include unclear legal regulation for some telemedical practices and difficulty claiming reimbursement from insurers or government programs in some fields.
Another disadvantage of telemedicine is the inability to start treatment immediately. For example, a patient suffering from a bacterial infection might be given an antibiotic hypodermic injection in the clinic, and observed for any reaction, before that antibiotic is prescribed in pill form.
Click on any of the following blue hyperlinks for more about Telemedicine:
- History
- Types
- Specialist care delivery
- Licensure
- U.S. licensing and regulatory issues
- Companies
- Advanced and experimental services
- Enabling technologies
- Developing countries
- See also:
Digital health is the convergence of digital and genomic technologies with health, healthcare, living, and society to enhance the efficiency of healthcare delivery and make medicines more personalized and precise.
The discipline involves the use of information and communication technologies to help address the health problems and challenges faced by patients. These technologies include both hardware and software solutions and services, including telemedicine, web-based analysis, email, mobile phones and applications, text messages, and clinic or remote monitoring sensors.
Generally, digital health is concerned about the development of interconnected health systems to improve the use of computational technologies, smart devices, computational analysis techniques and communication media to aid healthcare professionals and patients manage illnesses and health risks, as well as promote health and wellbeing.
Digital health is a multi-disciplinary domain which involves many stakeholders, including clinicians, researchers and scientists with a wide range of expertise in healthcare, engineering, social sciences, public health, health economics and management.
Elements:
As an outgrowth of the Digital Revolution characterized by "the mass production and widespread use of digital logic circuits, and its derived technologies, including the computer, digital cellular phone, and the Internet," key elements of digital health include wireless devices, hardware sensors and software sensing technologies, microprocessors and integrated circuits, the Internet, social networking, mobile/cellular networks and body area networks, health information technology, genomics, and personal genetic information.
Domains:
Various domains span digital health. These include Healthcare technology assessment and monitoring to prevent, diagnose or treat diseases, monitoring of patients, or for rehabilitation or long-term care.
Such technologies include Assistive technologies and rehabilitation robotics for people with disabilities so as to aid in their independence to perform daily tasks, unobtrusive monitoring sensors and wearable devices.
Clinical decision support aids clinicians at the point of care, including diagnosis, analysis and interpretation of patient-related data.Computational simulations, modeling and machine learning approaches can model health-related outcomes. E-health delivers health information and services to enable data transmition, storage and retrievial for clinical, educational and administrative purposes.
Health systems engineering applications in health care systems, includes knowledge discovery, decision making, optimization, human factors engineering, quality engineering, and information technology and communication. Human-computer-environment interactions Human-computer interaction principles tend to be based around user-centered, experience-centered or activity-centered designs.
Virtual reality, video gaming rehabilitation, and serious games to provide a social and interactive experience for healthcare student and patient education. Speech and hearing systems for natural language processing, speech recognition techniques, and medical devices can aid in speech and hearing (e.g. cochlear implants).Telehealth, telemedicine, telecare, telecoaching and telerehabilitation provide various forms of patient care remotely at a distance.
Implementation:
National digital programs exist to support healthcare, such as those of Canada Health Infoway built on core systems of patient and provider registries, clinical and diagnostic imaging systems, clinical reports and immunizations. By 2014, 75% of Canadian physicians were using electronic medical records.
In Uganda and Mozambique, partnerships between patients with cell phones, local and regional governments, technologists, non-governmental organizations, academia, and industry have enabled mHealth solutions.
Innovation cycle:
The innovation process for digital health is an iterative cycle for technological solutions classified into five main activity processes beginning from the identification of the healthcare problem, research, digital solution, evaluating the solution to implementation in working clinical practices.
___________________________________________________________________________
Online doctor is a term that emerged during the 2000s, used by both the media and academics, to describe a generation of physicians and health practitioners who deliver healthcare, including drug prescription, over the internet.
Emergence of online doctors:
In the 2000s, many people came to treat the internet as a first, or at least a major, source of information and communication. Health advice is now the second-most popular topic, after pornography, that people search for on the internet.
With the advent of broadband and videoconferencing, many individuals have turned to online doctors to receive online consultations and purchase prescription drugs. Use of this technology has many advantages for both the doctor and the patient, including cost savings, convenience, accessibility, and improved privacy and communication.
In the US, a 2006 study found that searching for information on prescription or over-the-counter drugs was the fifth most popular search topic, and a 2004 study found that 4% of Americans had purchased prescription medications online.
A 2009 survey conducted by Geneva-based Health On the Net Foundation found one-in-ten Europeans buys medicines from websites and one-third claim to use online consultation.
In Germany, approximately seven million people buy from mail-order pharmacies, and mail-order sales account for approximately 8–10% of total pharmaceutical sales.
In 2008, the Royal Pharmaceutical Society of Great Britain reported that approximately two million people in Great Britain were regularly purchasing pharmaceuticals online (both with a prescription from registered online UK doctors and without prescriptions from other websites).
A recent survey commissioned by Pfizer, the Medicines and Healthcare products Regulatory Agency, RPSGB, the Patients Association and HEART UK found that 15% of the British adults asked had bought a prescription-only medicine online.
In developed countries, many online doctors prescribe so-called ‘lifestyle drugs’, such as for weight loss, hair loss or erectile dysfunction. The RPSGB has identified the most popular products prescribed online as Prozac (an antidepressant), Viagra (for erectile dysfunction), Valium (a tranquiliser), Ritalin (a psychostimulant), Serostim (a synthetic growth hormone) and Provigil (a psychostimulant).
A study in the USA has also shown that antibiotics are commonly available online without prescription.
Potential Harm:
Traditionalist critics of online doctors argue that an online doctor cannot provide proper examinations or diagnosis either by email or video call. Such consultations, they argue, will always be dangerous, with the potential for serious disease to be missed. There are also concerns that the absence of proximity leads to treatment by unqualified doctors or patients using false information to secure dangerous drugs.
Proponents argue there is little difference between an e-mail consultation and the sort of telephone assessment and advice that doctors regularly make out of hours or in circumstances where doctors cannot physically examine a patient (e.g., jungle medicine).
Laurence Buckman, chairman of the British Medical Association’s GPs’ committee, says that online consultations make life easier for doctors and patients when used properly. "Many GPs will be very happy with it and it could be useful. When it’s a regular patient you know well, it follows on from telephone consulting.
Voice is essential, vision is desirable. The problem comes when I don’t know the patient". Niall Dickson, chief executive of the General Medical Council, says: "We trust doctors to use their judgement to decide whether they should see a patient in person. Online consultations will be appropriate for some patients, whereas other patients will need a physical examination or may benefit from seeing their doctor in person".
Past and Future Developments
The first medical consulting website in the US was WebMD, founded in 1996 by Jim Clark (one of the founders of Netscape) and Pavan Nigam as Healthscape. Currently, its website carries information regarding health and health care, including a symptom checklist, pharmacy information, drug information, blogs of physicians with specific topics, and a place to store personal medical information.
As of February 2011, WebMD’s network of sites reaches an average of 86.4 million visitors per month and is the leading health portal in the United States.
Other popular US healthcare and medical consulting sites include the following:
- NIH.gov,
- MSN Health,
- Doctorspring,
- MdLive,
- Justdoc,
- Yahoo! Health,
- EverydayHealth,
- WomensHealth.gov,
- MayoClinic,
- Doctor Vista,
Many have experienced dramatic growth. (Healthline, launched in 2005, grew by 269% to 2.7 million average monthly unique visitors in Q1 2007 from 0.8 million average monthly unique visitors in Q1 2006).
Niche consulting sites are also popular including SeniorNet, which deals with age-related syndromes and 4collegewomen.org and GirlsHealth.gov, which target young women.
Several American online doctor companies, including Sherpaa, MDlive, Teladoc, First Stop Health, American Well, WebDoc247, MeMD, and Ringadoc, provide consultations with doctors over the phone or the Internet. Prominent San Francisco-based venture capital firm Founders Fund called such services "extraordinarily fast" and predicted that they will "bring relief to thousands of people with immediate medical needs".
In the UK, e-med was the first online health site to offer both a diagnosis and prescriptions to patients over the Internet. It was established in March 2000 by Dr. Julian Eden, In 2010, DrThom claimed to have 100,000 patients visit their site
NHS Direct (currently NHS Choices) is the free health advice and information service provided by the National Health Service (NHS) for residents and visitors in the UK, with advice offered 24 hours a day via telephone and web contact.
Over 1.5 million patients visit the website every month. More recently, a number of online doctors have emerged in the country, firms such as Now Healthcare Group, Dr Fox Pharmacy, Push Doctor and Lloyds Pharmacy offer consultation and prescriptions via the Internet.
In Australia HealthDirect is the free health advice and information service provided by the government with advice offered 24 hours a day via telephone. Medicare began funding online consultations for specialists on 1 July 2011 which has seen a slow but steady increase in volumes.
New advances in digital information technology mean that in future online doctors and healthcare websites may offer advanced scanning and diagnostic services over the internet.
The Nuffield Council on Bioethics identifies such services as direct-to-consumer body imaging (such as CT and MRI scans) and personal genetic profiling for individual susceptibility to disease. Professor Sir Bruce Keogh, the medical director of the UK NHS, is drawing up plans to introduce online consultations via Skype and has said IT will "completely change the way [doctors] deliver medicine".
This concept is gaining more importance and there are some companies who started cashing on it, few companies like Zocdoc have started providing online doctor booking service.
See also:
- e-Patient
- Health informatics
- mHealth
- Telehealth
- NHS Choices The UK government's medical advice and treatment portal
- FSMB Federation of State Medical Boards, body of the state medical boards that regulate online doctors in the US
- CQC Quality Care Commission Board, body that regulates online doctors in the UK
Assistive Technology
YouTube Video about Mackenzie's Voice: Living with Cerebral Palsy
YouTube Video about Assistive Technology in Action - Meet Elle
Pictured below: Assistive Devices and their Use
Assistive technology is an umbrella term that includes assistive, adaptive, and rehabilitative devices for people with disabilities while also including the process used in selecting, locating, and using them.
People who have disabilities often have difficulty performing activities of daily living (ADLs) independently, or even with assistance. ADLs are self-care activities that include toileting, mobility (ambulation), eating, bathing, dressing and grooming. Assistive technology can ameliorate the effects of disabilities that limit the ability to perform ADLs.
Assistive technology promotes greater independence by enabling people to perform tasks they were formerly unable to accomplish, or had great difficulty accomplishing, by providing enhancements to, or changing methods of interacting with, the technology needed to accomplish such tasks.
For example, wheelchairs provide independent mobility for those who cannot walk, while assistive eating devices can enable people who cannot feed themselves to do so.
Due to assistive technology, people with disabilities have an opportunity of a more positive and easygoing lifestyle, with an increase in "social participation," "security and control," and a greater chance to "reduce institutional costs without significantly increasing household expenses."
Adaptive Technology:
The term adaptive technology is often used as the synonym for assistive technology; however, they are different terms. Assistive technology refers to "any item, piece of equipment, or product system, whether acquired commercially, modified, or customized, that is used to increase, maintain, or improve functional capabilities of individuals with disabilities", while adaptive technology covers items that are specifically designed for persons with disabilities and would seldom be used by non-disabled persons.
In other words, "assistive technology is any object or system that increases or maintains the capabilities of people with disabilities," while adaptive technology is "any object or system that is specifically designed for the purpose of increasing or maintaining the capabilities of people with disabilities." Consequently, adaptive technology is a subset of assistive technology. Adaptive technology often refers specifically to electronic and information technology access.
Mobility impairments:
Wheelchairs:
Main article: Wheelchair
Wheelchairs are devices that can be manually propelled or electrically propelled, and that include a seating system and are designed to be a substitute for the normal mobility that most people enjoy.
Wheelchairs and other mobility devices allow people to perform mobility-related activities of daily living which include feeding, toileting, dressing, grooming, and bathing. The devices come in a number of variations where they can be propelled either by hand or by motors where the occupant uses electrical controls to manage motors and seating control actuators through a joystick, sip-and-puff control, or other input devices.
Often there are handles behind the seat for someone else to do the pushing or input devices for caregivers. Wheelchairs are used by people for whom walking is difficult or impossible due to illness, injury, or disability. People with both sitting and walking disability often need to use a wheelchair or walker.
Transfer devices:
Main article: Patient lift
Patient transfer devices generally allow patients with impaired mobility to be moved by caregivers between beds, wheelchairs, commodes, toilets, chairs, stretchers, shower benches, automobiles, swimming pools, and other patient support systems (i.e., radiology, surgical, or examining tables).
The most common devices are Patient lifts (for vertical transfer), Transfer benches, stretcher or convertible chairs (for lateral, supine transfer), sit-to-stand lifts (for moving patients from one seated position to another i.e., from wheelchairs to commodes), air bearing inflatable mattresses (for supine transfer i.e., transfer from a gurney to an operating room table), and sliding boards (usually used for transfer from a bed to a wheelchair).
Highly dependent patients who cannot assist their caregiver in moving them often require a Patient lift (a floor or ceiling-suspended sling lift) which though invented in 1955 and in common use since the early 1960s is still considered the state-of-the-art transfer device by OSHA and the American Nursing Association.
Walkers:
Main article: Walker
A walker or walking frame or Rollator is a tool for disabled people who need additional support to maintain balance or stability while walking. It consists of a frame that is about waist high, approximately twelve inches deep and slightly wider than the user. Walkers are also available in other sizes, such as for children, or for heavy people. Modern walkers are height-adjustable.
The front two legs of the walker may or may not have wheels attached depending on the strength and abilities of the person using it. It is also common to see caster wheels or glides on the back legs of a walker with wheels on the front.
Prosthesis:
Main article: Prosthesis
A prosthesis, prosthetic, or prosthetic limb is a device that replaces a missing body part. It is part of the field of biomechatronics, the science of using mechanical devices with human muscle, skeleton, and nervous systems to assist or enhance motor control lost by trauma, disease, or defect. Prostheses are typically used to replace parts lost by injury (traumatic) or missing from birth (congenital) or to supplement defective body parts.
Inside the body, artificial heart valves are in common use with artificial hearts and lungs seeing less common use but under active technology development. Other medical devices and aids that can be considered prosthetics include hearing aids, artificial eyes, palatal obturator, gastric bands, and dentures.
Prostheses are specifically not orthoses, although given certain circumstances a prosthesis might end up performing some or all of the same functionary benefits as an orthosis.
Prostheses are technically the complete finished item. For instance, a C-Leg knee alone is not a prosthesis, but only a prosthetic component. The complete prosthesis would consist of the attachment system to the residual limb — usually a "socket", and all the attachment hardware components all the way down to and including the terminal device. Keep this in mind as nomenclature is often interchanged.
The terms "prosthetic" and "orthotic" are adjectives used to describe devices such as a prosthetic knee. The terms "prosthetics" and "orthotics" are used to describe the respective allied health fields.
Visual impairments:
Main article: Blindness § Management
Many people with serious visual impairments live independently, using a wide range of tools and techniques. Examples of assistive technology for visually impairment include screen readers, screen magnifiers, Braille embossers, desktop video magnifiers, and voice recorders.
Screen readers:
Main article: Screen reader
Screen readers are used to help the visually impaired to easily access electronic information. These software programs run on a computer in order to convey the displayed information through voice (text-to-speech) or braille (refreshable braille displays) in combination with magnification for low vision users in some cases. There are a variety of platforms and applications available for a variety of costs with differing feature sets.
One example of screen readers is Apple VoiceOver. This software is provided free of charge on all Apple devices. Apple VoiceOver includes the option to magnify the screen, control the keyboard, and provide verbal descriptions to describe what is happening on the screen. There are thirty languages to select from. It also has the capacity to read aloud file content, as well as web pages, E-mail messages, and word processing files.
Braille and braille embossers:
Main article: Braille
Braille is a system of raised dots formed into units called braille cells. A full braille cell is made up of six dots, with two parallel rows of three dots, but other combinations and quantities of dots represent other letters, numbers, punctuation marks, or words. People can then use their fingers to read the code of raised dots.
A braille embosser is, simply put, a printer for braille. Instead of a standard printer adding ink onto a page, the braille embosser imprints the raised dots of braille onto a page. Some braille embossers combine both braille and ink so the documents can be read with either sight or touch.
Refreshable braille display:
Main article: Refreshable braille display
A refreshable braille display or braille terminal is an electro-mechanical device for displaying braille characters, usually by means of round-tipped pins raised through holes in a flat surface. Computer users who cannot use a computer monitor use it to read a braille output version of the displayed text.
Desktop video magnifier:
Main article: Video magnifier
Desktop video magnifiers are electronic devices that use a camera and a display screen to perform digital magnification of printed materials. They enlarge printed pages for those with low vision. A camera connects to a monitor that displays real-time images, and the user can control settings such as magnification, focus, contrast, underlining, highlighting, and other screen preferences. They come in a variety of sizes and styles; some are small and portable with handheld cameras, while others are much larger and mounted on a fixed stand.
Screen magnification software:
Main article: Screen magnifier
A screen magnifier is software that interfaces with a computer's graphical output to present enlarged screen content. It allows users to enlarge the texts and graphics on their computer screens for easier viewing.
Similar to desktop video magnifiers, this technology assists people with low vision. After the user loads the software into their computer's memory, it serves as a kind of "computer magnifying glass." Wherever the computer cursor moves, it enlarges the area around it. This allows greater computer accessibility for a wide range of visual abilities.
Large-print and tactile keyboards:
A large-print keyboard has large letters printed on the keys. On the keyboard shown, the round buttons at the top control software which can magnify the screen (zoom in), change the background color of the screen, or make the mouse cursor on the screen larger. The "bump dots" on the keys, installed in this case by the organization using the keyboards, help the user find the right keys in a tactile way.
Navigation Assistance
Assistive technology for navigation has exploded on the IEEE Xplore database since 2000, with over 7,500 engineering articles written on assistive technologies and visual impairment in the past 25 years, and over 1,300 articles on solving the problem of navigation for people who are blind or visually impaired.
As well, over 600 articles on augmented reality and visual impairment have appeared in the engineering literature since 2000. Most of these articles were published within the past 5 years, and the number of articles in this area is increasing every year.
GPS, accelerometers, gyroscopes, and cameras can pinpoint the exact location of the user and provide information on what’s in the immediate vicinity, and assistance in getting to a destination.
Wearable Technology:
Main article: Wearable technology
Wearable technology are smart electronic devices that can be worn on the body as an implant or an accessory. New technologies are exploring how the visually impaired can receive visual information through wearable devices.
Some wearable devices for visual impairment include:
Personal emergency response systems:
Main article: Telecare
Personal emergency response systems (PERS), or Telecare (UK term), are a particular sort of assistive technology that use electronic sensors connected to an alarm system to help caregivers manage risk and help vulnerable people stay independent at home longer.
An example would be the systems being put in place for senior people such as fall detectors, thermometers (for hypothermia risk), flooding and unlit gas sensors (for people with mild dementia). Notably, these alerts can be customized to the particular person's risks. When the alert is triggered, a message is sent to a caregiver or contact center who can respond appropriately.
Accessibility software:
Main article: Computer accessibility
In human–computer interaction, computer accessibility (also known as accessible computing) refers to the accessibility of a computer system to all people, regardless of disability or severity of impairment, examples include web accessibility guidelines.
Another approach is for the user to present a token to the computer terminal, such as a smart card, that has configuration information to adjust the computer speed, text size, etc. to their particular needs. This is useful where users want to access public computer based terminals in Libraries, ATM, Information kiosks etc.
The concept is encompassed by the CEN EN 1332-4 Identification Card Systems - Man-Machine Interface. This development of this standard has been supported in Europe by SNAPI and has been successfully incorporated into the Lasseo specifications, but with limited success due to the lack of interest from public computer terminal suppliers.
Hearing impairments:
Main article: Assistive Technology for Deaf and Hard of Hearing
The deaf or hard of hearing community has a difficult time to communicate and perceive information as compared to hearing individuals. Thus, these individuals often rely on visual and tactile mediums for receiving and communicating information.
The use of assistive technology and devices provides this community with various solutions to their problems by providing higher sound (for those who are hard of hearing), tactile feedback, visual cues and improved technology access.
Individuals who are deaf or hard of hearing utilize a variety of assistive technologies that provide them with improved access to information in numerous environments. Most devices either provide amplified sound or alternate ways to access information through vision and/or vibration.
These technologies can be grouped into three general categories: Hearing Technology, alerting devices, and communication support.
Hearing aids:
Main article: Hearing aid
A hearing aid or deaf aid is an electroacoustic device which is designed to amplify sound for the wearer, usually with the aim of making speech more intelligible, and to correct impaired hearing as measured by audiometry.
This type of assistive technology helps people with hearing loss participate more fully in their communities by allowing them to hear more clearly. They amplify any and all sound waves through use of a microphone, amplifier, and speaker. There is a wide variety of hearing aids available, including digital, in-the-ear, in-the-canal, behind-the-ear, and on-the-body aids.
Assistive listening devices:
Main article: Assistive listening device
Assistive listening devices include FM, infrared, and loop assistive listening devices. This type of technology allows people with hearing difficulties to focus on a speaker or subject by getting rid of extra background noises and distractions, making places like auditoriums, classrooms, and meetings much easier to participate in.
The assistive listening device usually uses a microphone to capture an audio source near to its origin and broadcast it wirelessly over an FM (Frequency Modulation) transmission, IR (Infra Red) transmission, IL (Induction Loop) transmission, or other transmission methods.
The person who is listening may use an FM/IR/IL Receiver to tune into the signal and listen at his/her preferred volume.
Amplified telephone equipment:
Main article: Telecommunications device for the deaf#Other devices for the deaf or hard of hearing
This type of assistive technology allows users to amplify the volume and clarity of their phone calls so that they can easily partake in this medium of communication. There are also options to adjust the frequency and tone of a call to suit their individual hearing needs.
Additionally, there is a wide variety of amplified telephones to choose from, with different degrees of amplification. For example, a phone with 26 to 40 decibel is generally sufficient for mild hearing loss, while a phone with 71 to 90 decibel is better for more severe hearing loss.
Augmentative and alternative communication:
Main article: Augmentative and alternative communication
Augmentative and alternative communication (AAC) is an umbrella term that encompasses methods of communication for those with impairments or restrictions on the production or comprehension of spoken or written language.
AAC systems are extremely diverse and depend on the capabilities of the user. They may be as basic as pictures on a board that are used to request food, drink, or other care; or they can be advanced speech generating devices, based on speech synthesis, that are capable of storing hundreds of phrases and words.
Cognitive impairments:
Main article: Cognitive orthotics
Assistive Technology for Cognition (ATC) is the use of technology (usually high tech) to augment and assist cognitive processes such as attention, memory, self-regulation, navigation, emotion recognition and management, planning, and sequencing activity.
Systematic reviews of the field have found that the number of ATC are growing rapidly, but have focused on memory and planning, that there is emerging evidence for efficacy, that a lot of scope exists to develop new ATC.
Examples of ATC include: NeuroPage which prompts users about meetings, Wakamaru, which provides companionship and reminds users to take medicine and calls for help if something is wrong, and telephone Reassurance systems.
Memory aids:
Memory aids are any type of assistive technology that helps a user learn and remember certain information. Many memory aids are used for cognitive impairments such as reading, writing, or organizational difficulties.
For example, a Smartpen records handwritten notes by creating both a digital copy and an audio recording of the text. Users simply tap certain parts of their notes, the pen saves it, and reads it back to them. From there, the user can also download their notes onto a computer for increased accessibility. Digital voice recorders are also used to record "in the moment" information for fast and easy recall at a later time.
Educational software:
Main article: Educational software
Educational software is software that assists people with reading, learning, comprehension, and organizational difficulties. Any accommodation software such as text readers, notetakers, text enlargers, organization tools, word predictions, and talking word processors falls under the category of educational software.
Eating Impairments:
Main article: Assistive eating devices
Adaptive eating devices include items commonly used by the general population like spoons and forks and plates. However they become assistive technology when they are modified to accommodate the needs of people who have difficultly using standard cutlery due to a disabling condition.
Common modifications include increasing the size of the utensil handle to make it easier to grasp. Plates and bowls may have a guard on the edge that stops food being pushed off of the dish when it is being scooped. More sophisticated equipment for eating includes manual and powered feeding devices. These devices support those who have little or no hand and arm function and enable them to eat independently.
In Sports:
Assistive technology in sports is an area of technology design that is growing. Assistive technology is the array of new devices created to enable sports enthusiasts who have disabilities to play. Assistive technology may be used in adaptive sports, where an existing sport is modified to enable players with a disability to participate; or, assistive technology may be used to invent completely new sports with athletes with disabilities exclusively in mind.
An increasing number of people with disabilities are participating in sports, leading to the development of new assistive technology. Assistive technology devices can be simple, or "low-tech", or they may use highly advanced technology. "Low-tech" devices can include velcro gloves and adaptive bands and tubes. "High-tech" devices can include all-terrain wheelchairs and adaptive bicycles.
Accordingly, assistive technology can be found in sports ranging from local community recreation to the elite Paralympic Games. More complex assistive technology devices have been developed over time, and as a result, sports for people with disabilities "have changed from being a clinical therapeutic tool to an increasingly competition-oriented activity".
In Education:
In the United States there are two major pieces of legislation that govern the use of assistive technology within the school system.
The first is Section 504 of the Rehabilitation Act of 1973 and the second being the Individuals with Disabilities Education Act (IDEA) which was first enacted in 1975 under the name The Education for All Handicapped Children Act.
In 2004, during the reauthorization period for IDEA, the National Instructional Material Access Center (NIMAC) was created which provided a repository of accessible text including publisher's textbooks to students with a qualifying disability. Files provided are in XML format and used as a starting platform for braille readers, screen readers, and other digital text software.
IDEA defines assistive technology as follows: "any item, piece of equipment, or product system, whether acquired commercially off the shelf, modified, or customized, that is used to increase, maintain, or improve functional capabilities of a child with a disability. (B) Exception.--The term does not include a medical device that is surgically implanted, or the replacement of such device."
Assistive technology in this area is broken down into low, mid, and high tech categories. Low tech encompasses equipment that is often low cost and does not include batteries or requires charging. Examples include adapted paper and pencil grips for writing or masks and color overlays for reading.
Mid tech supports used in the school setting include the use of handheld spelling dictionaries and portable word processors used to keyboard writing. High tech supports involve the use of tablet devices and computers with accompanying software. Software supports for writing include the use of auditory feedback while keyboarding, word prediction for spelling, and speech to text.
Supports for reading include the use of text to speech (TTS) software and font modification via access to digital text. Limited supports are available for math instruction and mostly consist of grid based software to allow younger students to keyboard equations and auditory feedback of more complex equations using MathML and Daisy.
Computer Accessibility:
Main article: Computer accessibility
One of the largest problems that affect people with disabilities is discomfort with prostheses. An experiment performed in Massachusetts utilized 20 people with various sensors attached to their arms. The subjects tried different arm exercises, and the sensors recorded their movements. All of the data helped engineers develop new engineering concepts for prosthetics.
Assistive technology may attempt to improve the ergonomics of the devices themselves such as Dvorak and other alternative keyboard layouts, which offer more ergonomic layouts of the keys.
Assistive technology devices have been created to enable people with disabilities to use modern touch screen mobile computers such as the iPad, iPhone and iPod touch. The Pererro is a plug and play adapter for iOS devices which uses the built in Apple VoiceOver feature in combination with a basic switch.
This brings touch screen technology to those who were previously unable to use it. Apple, with the release of iOS 7 had introduced the ability to navigate apps using switch control. Switch access could be activated either through an external bluetooth connected switch, single touch of the screen, or use of right and left head turns using the device's camera.
Additional accessibility features include the use of Assistive Touch which allows a user to access multi-touch gestures through pre-programmed onscreen buttons.
For users with physical disabilities a large variety of switches are available and customizable to the user's needs varying in size, shape, or amount of pressure required for activation. Switch access may be placed near any area of the body which has consistent and reliable mobility and less subject to fatigue. Common sites include the hands, head, and feet.
Eye gaze and head mouse systems can also be used as an alternative mouse navigation. A user may utilize single or multiple switch sites and the process often involves a scanning through items on a screen and activating the switch once the desired object is highlighted.
Home Automation:
The form of home automation called assistive domotics focuses on making it possible for elderly and disabled people to live independently. Home automation is becoming a viable option for the elderly and disabled who would prefer to stay in their own homes rather than move to a healthcare facility.
This field uses much of the same technology and equipment as home automation for security, entertainment, and energy conservation but tailors it towards elderly and disabled users. For example, automated prompts and reminders utilize motion sensors and pre-recorded audio messages; an automated prompt in the kitchen may remind the resident to turn off the oven, and one by the front door may remind the resident to lock the door.
Impacts:
Overall, assistive technology aims to allow people with disabilities to "participate more fully in all aspects of life (home, school, and community)" and increases their opportunities for "education, social interactions, and potential for meaningful employment". It creates greater independence and control for disabled individuals.
For example, in one study of 1,342 infants, toddlers and preschoolers, all with some kind of developmental, physical, sensory, or cognitive disability, the use of assistive technology created improvements in child development.
These included improvements in "cognitive, social, communication, literacy, motor, adaptive, and increases in engagement in learning activities". Additionally, it has been found to lighten caregiver load. Both family and professional caregivers benefit from assistive technology.
Through its use, the time that a family member or friend would need to care for a patient significantly decreases. However, studies show that care time for a professional caregiver increases when assistive technology is used. Nonetheless, their work load is significantly easier as the assistive technology frees them of having to perform certain tasks
See Also:
People who have disabilities often have difficulty performing activities of daily living (ADLs) independently, or even with assistance. ADLs are self-care activities that include toileting, mobility (ambulation), eating, bathing, dressing and grooming. Assistive technology can ameliorate the effects of disabilities that limit the ability to perform ADLs.
Assistive technology promotes greater independence by enabling people to perform tasks they were formerly unable to accomplish, or had great difficulty accomplishing, by providing enhancements to, or changing methods of interacting with, the technology needed to accomplish such tasks.
For example, wheelchairs provide independent mobility for those who cannot walk, while assistive eating devices can enable people who cannot feed themselves to do so.
Due to assistive technology, people with disabilities have an opportunity of a more positive and easygoing lifestyle, with an increase in "social participation," "security and control," and a greater chance to "reduce institutional costs without significantly increasing household expenses."
Adaptive Technology:
The term adaptive technology is often used as the synonym for assistive technology; however, they are different terms. Assistive technology refers to "any item, piece of equipment, or product system, whether acquired commercially, modified, or customized, that is used to increase, maintain, or improve functional capabilities of individuals with disabilities", while adaptive technology covers items that are specifically designed for persons with disabilities and would seldom be used by non-disabled persons.
In other words, "assistive technology is any object or system that increases or maintains the capabilities of people with disabilities," while adaptive technology is "any object or system that is specifically designed for the purpose of increasing or maintaining the capabilities of people with disabilities." Consequently, adaptive technology is a subset of assistive technology. Adaptive technology often refers specifically to electronic and information technology access.
Mobility impairments:
Wheelchairs:
Main article: Wheelchair
Wheelchairs are devices that can be manually propelled or electrically propelled, and that include a seating system and are designed to be a substitute for the normal mobility that most people enjoy.
Wheelchairs and other mobility devices allow people to perform mobility-related activities of daily living which include feeding, toileting, dressing, grooming, and bathing. The devices come in a number of variations where they can be propelled either by hand or by motors where the occupant uses electrical controls to manage motors and seating control actuators through a joystick, sip-and-puff control, or other input devices.
Often there are handles behind the seat for someone else to do the pushing or input devices for caregivers. Wheelchairs are used by people for whom walking is difficult or impossible due to illness, injury, or disability. People with both sitting and walking disability often need to use a wheelchair or walker.
Transfer devices:
Main article: Patient lift
Patient transfer devices generally allow patients with impaired mobility to be moved by caregivers between beds, wheelchairs, commodes, toilets, chairs, stretchers, shower benches, automobiles, swimming pools, and other patient support systems (i.e., radiology, surgical, or examining tables).
The most common devices are Patient lifts (for vertical transfer), Transfer benches, stretcher or convertible chairs (for lateral, supine transfer), sit-to-stand lifts (for moving patients from one seated position to another i.e., from wheelchairs to commodes), air bearing inflatable mattresses (for supine transfer i.e., transfer from a gurney to an operating room table), and sliding boards (usually used for transfer from a bed to a wheelchair).
Highly dependent patients who cannot assist their caregiver in moving them often require a Patient lift (a floor or ceiling-suspended sling lift) which though invented in 1955 and in common use since the early 1960s is still considered the state-of-the-art transfer device by OSHA and the American Nursing Association.
Walkers:
Main article: Walker
A walker or walking frame or Rollator is a tool for disabled people who need additional support to maintain balance or stability while walking. It consists of a frame that is about waist high, approximately twelve inches deep and slightly wider than the user. Walkers are also available in other sizes, such as for children, or for heavy people. Modern walkers are height-adjustable.
The front two legs of the walker may or may not have wheels attached depending on the strength and abilities of the person using it. It is also common to see caster wheels or glides on the back legs of a walker with wheels on the front.
Prosthesis:
Main article: Prosthesis
A prosthesis, prosthetic, or prosthetic limb is a device that replaces a missing body part. It is part of the field of biomechatronics, the science of using mechanical devices with human muscle, skeleton, and nervous systems to assist or enhance motor control lost by trauma, disease, or defect. Prostheses are typically used to replace parts lost by injury (traumatic) or missing from birth (congenital) or to supplement defective body parts.
Inside the body, artificial heart valves are in common use with artificial hearts and lungs seeing less common use but under active technology development. Other medical devices and aids that can be considered prosthetics include hearing aids, artificial eyes, palatal obturator, gastric bands, and dentures.
Prostheses are specifically not orthoses, although given certain circumstances a prosthesis might end up performing some or all of the same functionary benefits as an orthosis.
Prostheses are technically the complete finished item. For instance, a C-Leg knee alone is not a prosthesis, but only a prosthetic component. The complete prosthesis would consist of the attachment system to the residual limb — usually a "socket", and all the attachment hardware components all the way down to and including the terminal device. Keep this in mind as nomenclature is often interchanged.
The terms "prosthetic" and "orthotic" are adjectives used to describe devices such as a prosthetic knee. The terms "prosthetics" and "orthotics" are used to describe the respective allied health fields.
Visual impairments:
Main article: Blindness § Management
Many people with serious visual impairments live independently, using a wide range of tools and techniques. Examples of assistive technology for visually impairment include screen readers, screen magnifiers, Braille embossers, desktop video magnifiers, and voice recorders.
Screen readers:
Main article: Screen reader
Screen readers are used to help the visually impaired to easily access electronic information. These software programs run on a computer in order to convey the displayed information through voice (text-to-speech) or braille (refreshable braille displays) in combination with magnification for low vision users in some cases. There are a variety of platforms and applications available for a variety of costs with differing feature sets.
One example of screen readers is Apple VoiceOver. This software is provided free of charge on all Apple devices. Apple VoiceOver includes the option to magnify the screen, control the keyboard, and provide verbal descriptions to describe what is happening on the screen. There are thirty languages to select from. It also has the capacity to read aloud file content, as well as web pages, E-mail messages, and word processing files.
Braille and braille embossers:
Main article: Braille
Braille is a system of raised dots formed into units called braille cells. A full braille cell is made up of six dots, with two parallel rows of three dots, but other combinations and quantities of dots represent other letters, numbers, punctuation marks, or words. People can then use their fingers to read the code of raised dots.
A braille embosser is, simply put, a printer for braille. Instead of a standard printer adding ink onto a page, the braille embosser imprints the raised dots of braille onto a page. Some braille embossers combine both braille and ink so the documents can be read with either sight or touch.
Refreshable braille display:
Main article: Refreshable braille display
A refreshable braille display or braille terminal is an electro-mechanical device for displaying braille characters, usually by means of round-tipped pins raised through holes in a flat surface. Computer users who cannot use a computer monitor use it to read a braille output version of the displayed text.
Desktop video magnifier:
Main article: Video magnifier
Desktop video magnifiers are electronic devices that use a camera and a display screen to perform digital magnification of printed materials. They enlarge printed pages for those with low vision. A camera connects to a monitor that displays real-time images, and the user can control settings such as magnification, focus, contrast, underlining, highlighting, and other screen preferences. They come in a variety of sizes and styles; some are small and portable with handheld cameras, while others are much larger and mounted on a fixed stand.
Screen magnification software:
Main article: Screen magnifier
A screen magnifier is software that interfaces with a computer's graphical output to present enlarged screen content. It allows users to enlarge the texts and graphics on their computer screens for easier viewing.
Similar to desktop video magnifiers, this technology assists people with low vision. After the user loads the software into their computer's memory, it serves as a kind of "computer magnifying glass." Wherever the computer cursor moves, it enlarges the area around it. This allows greater computer accessibility for a wide range of visual abilities.
Large-print and tactile keyboards:
A large-print keyboard has large letters printed on the keys. On the keyboard shown, the round buttons at the top control software which can magnify the screen (zoom in), change the background color of the screen, or make the mouse cursor on the screen larger. The "bump dots" on the keys, installed in this case by the organization using the keyboards, help the user find the right keys in a tactile way.
Navigation Assistance
Assistive technology for navigation has exploded on the IEEE Xplore database since 2000, with over 7,500 engineering articles written on assistive technologies and visual impairment in the past 25 years, and over 1,300 articles on solving the problem of navigation for people who are blind or visually impaired.
As well, over 600 articles on augmented reality and visual impairment have appeared in the engineering literature since 2000. Most of these articles were published within the past 5 years, and the number of articles in this area is increasing every year.
GPS, accelerometers, gyroscopes, and cameras can pinpoint the exact location of the user and provide information on what’s in the immediate vicinity, and assistance in getting to a destination.
Wearable Technology:
Main article: Wearable technology
Wearable technology are smart electronic devices that can be worn on the body as an implant or an accessory. New technologies are exploring how the visually impaired can receive visual information through wearable devices.
Some wearable devices for visual impairment include:
Personal emergency response systems:
Main article: Telecare
Personal emergency response systems (PERS), or Telecare (UK term), are a particular sort of assistive technology that use electronic sensors connected to an alarm system to help caregivers manage risk and help vulnerable people stay independent at home longer.
An example would be the systems being put in place for senior people such as fall detectors, thermometers (for hypothermia risk), flooding and unlit gas sensors (for people with mild dementia). Notably, these alerts can be customized to the particular person's risks. When the alert is triggered, a message is sent to a caregiver or contact center who can respond appropriately.
Accessibility software:
Main article: Computer accessibility
In human–computer interaction, computer accessibility (also known as accessible computing) refers to the accessibility of a computer system to all people, regardless of disability or severity of impairment, examples include web accessibility guidelines.
Another approach is for the user to present a token to the computer terminal, such as a smart card, that has configuration information to adjust the computer speed, text size, etc. to their particular needs. This is useful where users want to access public computer based terminals in Libraries, ATM, Information kiosks etc.
The concept is encompassed by the CEN EN 1332-4 Identification Card Systems - Man-Machine Interface. This development of this standard has been supported in Europe by SNAPI and has been successfully incorporated into the Lasseo specifications, but with limited success due to the lack of interest from public computer terminal suppliers.
Hearing impairments:
Main article: Assistive Technology for Deaf and Hard of Hearing
The deaf or hard of hearing community has a difficult time to communicate and perceive information as compared to hearing individuals. Thus, these individuals often rely on visual and tactile mediums for receiving and communicating information.
The use of assistive technology and devices provides this community with various solutions to their problems by providing higher sound (for those who are hard of hearing), tactile feedback, visual cues and improved technology access.
Individuals who are deaf or hard of hearing utilize a variety of assistive technologies that provide them with improved access to information in numerous environments. Most devices either provide amplified sound or alternate ways to access information through vision and/or vibration.
These technologies can be grouped into three general categories: Hearing Technology, alerting devices, and communication support.
Hearing aids:
Main article: Hearing aid
A hearing aid or deaf aid is an electroacoustic device which is designed to amplify sound for the wearer, usually with the aim of making speech more intelligible, and to correct impaired hearing as measured by audiometry.
This type of assistive technology helps people with hearing loss participate more fully in their communities by allowing them to hear more clearly. They amplify any and all sound waves through use of a microphone, amplifier, and speaker. There is a wide variety of hearing aids available, including digital, in-the-ear, in-the-canal, behind-the-ear, and on-the-body aids.
Assistive listening devices:
Main article: Assistive listening device
Assistive listening devices include FM, infrared, and loop assistive listening devices. This type of technology allows people with hearing difficulties to focus on a speaker or subject by getting rid of extra background noises and distractions, making places like auditoriums, classrooms, and meetings much easier to participate in.
The assistive listening device usually uses a microphone to capture an audio source near to its origin and broadcast it wirelessly over an FM (Frequency Modulation) transmission, IR (Infra Red) transmission, IL (Induction Loop) transmission, or other transmission methods.
The person who is listening may use an FM/IR/IL Receiver to tune into the signal and listen at his/her preferred volume.
Amplified telephone equipment:
Main article: Telecommunications device for the deaf#Other devices for the deaf or hard of hearing
This type of assistive technology allows users to amplify the volume and clarity of their phone calls so that they can easily partake in this medium of communication. There are also options to adjust the frequency and tone of a call to suit their individual hearing needs.
Additionally, there is a wide variety of amplified telephones to choose from, with different degrees of amplification. For example, a phone with 26 to 40 decibel is generally sufficient for mild hearing loss, while a phone with 71 to 90 decibel is better for more severe hearing loss.
Augmentative and alternative communication:
Main article: Augmentative and alternative communication
Augmentative and alternative communication (AAC) is an umbrella term that encompasses methods of communication for those with impairments or restrictions on the production or comprehension of spoken or written language.
AAC systems are extremely diverse and depend on the capabilities of the user. They may be as basic as pictures on a board that are used to request food, drink, or other care; or they can be advanced speech generating devices, based on speech synthesis, that are capable of storing hundreds of phrases and words.
Cognitive impairments:
Main article: Cognitive orthotics
Assistive Technology for Cognition (ATC) is the use of technology (usually high tech) to augment and assist cognitive processes such as attention, memory, self-regulation, navigation, emotion recognition and management, planning, and sequencing activity.
Systematic reviews of the field have found that the number of ATC are growing rapidly, but have focused on memory and planning, that there is emerging evidence for efficacy, that a lot of scope exists to develop new ATC.
Examples of ATC include: NeuroPage which prompts users about meetings, Wakamaru, which provides companionship and reminds users to take medicine and calls for help if something is wrong, and telephone Reassurance systems.
Memory aids:
Memory aids are any type of assistive technology that helps a user learn and remember certain information. Many memory aids are used for cognitive impairments such as reading, writing, or organizational difficulties.
For example, a Smartpen records handwritten notes by creating both a digital copy and an audio recording of the text. Users simply tap certain parts of their notes, the pen saves it, and reads it back to them. From there, the user can also download their notes onto a computer for increased accessibility. Digital voice recorders are also used to record "in the moment" information for fast and easy recall at a later time.
Educational software:
Main article: Educational software
Educational software is software that assists people with reading, learning, comprehension, and organizational difficulties. Any accommodation software such as text readers, notetakers, text enlargers, organization tools, word predictions, and talking word processors falls under the category of educational software.
Eating Impairments:
Main article: Assistive eating devices
Adaptive eating devices include items commonly used by the general population like spoons and forks and plates. However they become assistive technology when they are modified to accommodate the needs of people who have difficultly using standard cutlery due to a disabling condition.
Common modifications include increasing the size of the utensil handle to make it easier to grasp. Plates and bowls may have a guard on the edge that stops food being pushed off of the dish when it is being scooped. More sophisticated equipment for eating includes manual and powered feeding devices. These devices support those who have little or no hand and arm function and enable them to eat independently.
In Sports:
Assistive technology in sports is an area of technology design that is growing. Assistive technology is the array of new devices created to enable sports enthusiasts who have disabilities to play. Assistive technology may be used in adaptive sports, where an existing sport is modified to enable players with a disability to participate; or, assistive technology may be used to invent completely new sports with athletes with disabilities exclusively in mind.
An increasing number of people with disabilities are participating in sports, leading to the development of new assistive technology. Assistive technology devices can be simple, or "low-tech", or they may use highly advanced technology. "Low-tech" devices can include velcro gloves and adaptive bands and tubes. "High-tech" devices can include all-terrain wheelchairs and adaptive bicycles.
Accordingly, assistive technology can be found in sports ranging from local community recreation to the elite Paralympic Games. More complex assistive technology devices have been developed over time, and as a result, sports for people with disabilities "have changed from being a clinical therapeutic tool to an increasingly competition-oriented activity".
In Education:
In the United States there are two major pieces of legislation that govern the use of assistive technology within the school system.
The first is Section 504 of the Rehabilitation Act of 1973 and the second being the Individuals with Disabilities Education Act (IDEA) which was first enacted in 1975 under the name The Education for All Handicapped Children Act.
In 2004, during the reauthorization period for IDEA, the National Instructional Material Access Center (NIMAC) was created which provided a repository of accessible text including publisher's textbooks to students with a qualifying disability. Files provided are in XML format and used as a starting platform for braille readers, screen readers, and other digital text software.
IDEA defines assistive technology as follows: "any item, piece of equipment, or product system, whether acquired commercially off the shelf, modified, or customized, that is used to increase, maintain, or improve functional capabilities of a child with a disability. (B) Exception.--The term does not include a medical device that is surgically implanted, or the replacement of such device."
Assistive technology in this area is broken down into low, mid, and high tech categories. Low tech encompasses equipment that is often low cost and does not include batteries or requires charging. Examples include adapted paper and pencil grips for writing or masks and color overlays for reading.
Mid tech supports used in the school setting include the use of handheld spelling dictionaries and portable word processors used to keyboard writing. High tech supports involve the use of tablet devices and computers with accompanying software. Software supports for writing include the use of auditory feedback while keyboarding, word prediction for spelling, and speech to text.
Supports for reading include the use of text to speech (TTS) software and font modification via access to digital text. Limited supports are available for math instruction and mostly consist of grid based software to allow younger students to keyboard equations and auditory feedback of more complex equations using MathML and Daisy.
Computer Accessibility:
Main article: Computer accessibility
One of the largest problems that affect people with disabilities is discomfort with prostheses. An experiment performed in Massachusetts utilized 20 people with various sensors attached to their arms. The subjects tried different arm exercises, and the sensors recorded their movements. All of the data helped engineers develop new engineering concepts for prosthetics.
Assistive technology may attempt to improve the ergonomics of the devices themselves such as Dvorak and other alternative keyboard layouts, which offer more ergonomic layouts of the keys.
Assistive technology devices have been created to enable people with disabilities to use modern touch screen mobile computers such as the iPad, iPhone and iPod touch. The Pererro is a plug and play adapter for iOS devices which uses the built in Apple VoiceOver feature in combination with a basic switch.
This brings touch screen technology to those who were previously unable to use it. Apple, with the release of iOS 7 had introduced the ability to navigate apps using switch control. Switch access could be activated either through an external bluetooth connected switch, single touch of the screen, or use of right and left head turns using the device's camera.
Additional accessibility features include the use of Assistive Touch which allows a user to access multi-touch gestures through pre-programmed onscreen buttons.
For users with physical disabilities a large variety of switches are available and customizable to the user's needs varying in size, shape, or amount of pressure required for activation. Switch access may be placed near any area of the body which has consistent and reliable mobility and less subject to fatigue. Common sites include the hands, head, and feet.
Eye gaze and head mouse systems can also be used as an alternative mouse navigation. A user may utilize single or multiple switch sites and the process often involves a scanning through items on a screen and activating the switch once the desired object is highlighted.
Home Automation:
The form of home automation called assistive domotics focuses on making it possible for elderly and disabled people to live independently. Home automation is becoming a viable option for the elderly and disabled who would prefer to stay in their own homes rather than move to a healthcare facility.
This field uses much of the same technology and equipment as home automation for security, entertainment, and energy conservation but tailors it towards elderly and disabled users. For example, automated prompts and reminders utilize motion sensors and pre-recorded audio messages; an automated prompt in the kitchen may remind the resident to turn off the oven, and one by the front door may remind the resident to lock the door.
Impacts:
Overall, assistive technology aims to allow people with disabilities to "participate more fully in all aspects of life (home, school, and community)" and increases their opportunities for "education, social interactions, and potential for meaningful employment". It creates greater independence and control for disabled individuals.
For example, in one study of 1,342 infants, toddlers and preschoolers, all with some kind of developmental, physical, sensory, or cognitive disability, the use of assistive technology created improvements in child development.
These included improvements in "cognitive, social, communication, literacy, motor, adaptive, and increases in engagement in learning activities". Additionally, it has been found to lighten caregiver load. Both family and professional caregivers benefit from assistive technology.
Through its use, the time that a family member or friend would need to care for a patient significantly decreases. However, studies show that care time for a professional caregiver increases when assistive technology is used. Nonetheless, their work load is significantly easier as the assistive technology frees them of having to perform certain tasks
See Also:
- Accessibility
- Augmentative and alternative communication
- Braille technology
- Design for All (in ICT)
- Durable medical equipment
- Matching Person & Technology Model
- OATS: Open Source Assistive Technology Software
- Occupational Therapy
- Transgenerational design
- Universal access to education
Health Technology in the United States
- YouTube Video of the Best Medical Breakthroughs in 2021 by the Cleveland Clinic
- YouTube Video of 5 Medical Breakthroughs Shaping the Future of Health by WebMD
- Click here for a List of FDA-approved Drugs covering Hematology/Oncology (Cancer) Approvals & Safety Notifications.
- Click here for a list of FDA-approved Novel Drugs for 2018
Health technology is defined by the World Health Organization as the "application of organized knowledge and skills in the form of devices, medicines, vaccines, procedures and systems developed to solve a health problem and improve quality of lives". This includes the pharmaceuticals, devices, procedures, organizational systems used in health care, and computer-supported information systems. In the United States, these technologies involve standardized physical objects as well as traditional and designed social means and methods to treat or care for patients.
Medical Technology:
Medical technology, or "medtech", encompasses a wide range of healthcare products and is used to treat diseases and medical conditions affecting humans.
Such technologies (applications of medical science) are intended to improve the quality of healthcare delivered through earlier diagnosis, less invasive treatment options and reduction in hospital stays and rehabilitation times.
Recent advances in medical technology have also focused on cost reduction. Medical technology may broadly include medical devices, information technology, biotech, and healthcare services.
The impacts of medical technology involve social and ethical issues. For example, physicians can seek objective information from technology rather than read subjective patient reports.
A major driver of the sector's growth is the consumerization of medtech. Supported by the widespread availability of smartphones and tablets, providers are able to reach a large audience at low cost, a trend that stands to be consolidated as wearable technologies spread throughout the market.
In the past 5 years running up to the end of 2015, venture funding has grown 200%, allowing US$11.7 billion to flow into health tech businesses from over 30,000 investors in the space.
The over-dependence on the use of technology in every step of the treatment process can result in severe economic burdens to families and individuals.
There has been an unprecedented rise in the utilization of automated clinical laboratories and CT scanners without any proof that they are necessary and beneficial to the individuals and families.
Education
Companies such as Surgical Theater, provide new technology capable of capturing 3D virtual images of patients' brains to use as practice for operations. 3D printing allows medical companies to produce prototypes to practice on before an operation created with artificial tissue.
Medical virtual reality provides doctors multiple surgical scenarios that could happen and allows them to practice and prepare themselves for these situations. It also permits medical students a hands on experience of different procedures without the consequences of making potential mistakes.
ORamaVR is one of the leading companies that employs such medical virtual reality technologies to transform medical education (knowledge) and training (skills) in order to improve patient outcomes, reduce surgical errors and training time and democratise medical education and training.
Privacy of health data:
Phones that can track one's whereabouts, steps and more can serve as medical devices, and medical devices have much the same effect as these phones. In the research article, Privacy Attitudes among Early Adopters of Emerging Health Technologies by Cynthia Cheung, Matthew Bietz, Kevin Patrick and Cinnamon Bloss discovered people were willing to share personal data for scientific advancements, although they still expressed uncertainty about who would have access to their data. People are naturally cautious about giving out sensitive personal information.
In 2015 the Medical Access and CHIP Reauthorization Act (MACRA) was passed which will be put into play in 2018 pushing towards electronic health records. Health Information Technology: Integration, Patient Empowerment, and Security by K. Marvin provided multiple different polls based on people's views on different types of technology entering the medical field most answers where responded with somewhat likely and very few completely disagreed on technology being used in medicine.
Marvin discusses the maintenance required to protect medical data and technology against cyber attacks as well as providing a proper data backup system for the information.
Patient Protection and Affordable Care Act (ACA) also known as Obamacare and health information technology health care is entering the digital era. Although with this development it needs to be protected.
Both health information and financial information now made digital within the health industry might become a larger target for cybercrime. Even with multiple different types of safeguards hackers some how still find their way in so the security that is in place needs to constantly be updated to prevent these breaches.
Allied Professions:
The term medical technology may also refer to the duties performed by clinical laboratory professionals in various settings within the public and private sectors.
The work of these professionals encompass clinical applications that include:
- chemistry,
- genetics,
- hematology,
- immunohematology (blood bank),
- immunology,
- microbiology,
- serology,
- urinalysis,
- and miscellaneous body fluid analysis.
Depending on location, educational level and certifying body, these professionals may be referred to as biomedical scientists, medical laboratory scientists (MLS), medical technologists (MT), medical laboratory technologists and medical laboratory technicians
Technology Testing:
All medical equipment introduced commercially must meet both United States and international regulations. The devices are tested on their material, effects on the human body, all components including devices that have other devices included with them, and the mechanical aspects.
Medical device user fee and modernization act of 2002 was created to make the FDA hurry up on their approval process of medical technology. By introducing sponsor user fees for a faster review time with predetermined performance target for review time:
36 devices and apps were approved by the FDA in 2016.
Types of Technology:
Medical technology has evolved into smaller portable devices, e.g., smartphones, touchscreens, tablets, laptops, digital ink, voice and face recognition and more.
With this technology, the following innovations came to exist:
- electronic health records (EHR),
- health information exchange (HIE),
- Nationwide Health Information Network (NwHIN),
- personal health records (PHRs),
- patient portals,
- nanomedicine,
- genome-based personalized medicine,
- Geographical Positioning System (GPS),
- radio frequency identification (RFID),
- telemedicine,
- clinical decision support (CDS),
- mobile home health care
- and cloud computing came to exist.
3D printing can be used to produce specialized splints, prostheses, parts for medical devices and inert implants. The end goal of 3D printing is being able to print out customized replaceable body parts
Assessment:
The concept of health technology assessment (HTA) was first coined in 1967 by the U.S. Congress in response to the increasing need to address the unintended and potential consequences of health technology, along with its prominent role in society. It was further institutionalized with the establishment of the congressional Office of Technology Assessment (OTA) in 1972-1973.
HTA is defined as a comprehensive form of policy research that examines short- and long-term consequences of the application of technology, including benefits, costs, and risks.
Due to the broad scope of technology assessment, it requires the participation of individuals besides scientists and health care practitioners such as managers and even the consumers.
There are several American organizations that provide health technology assessments and these include the Centers for Medicare and Medicaid Services (CMS) and the Veterans Administration through its VA Technology Assessment Program (VATAP). The models adopted by these institutions vary, although they focus on whether a medical technology being offered is therapeutically relevant. A study conducted in 2007 noted that the assessments still did not use formal economic analyses.
Aside from its development, however, assessment in the health technology industry has been viewed as sporadic and fragmented Issues such as the determination of products that needed to be developed, cost, and access, among others, also emerged. These - some argue - need to be included in the assessment since health technology is never purely a matter of science but also of beliefs, values, and ideologies.
One of the mechanisms being suggested – either as an element of- or an alternative to the current TAs is bioethics, which is also referred to as the "fourth-generation" evaluation framework.
There are at least two dimensions to an ethical HTA. The first involves the incorporation of ethics in the methodological standards employed to assess technologies while the second is concerned with the use of ethical framework in research and judgment on the part of the researchers who produce information used in the industry.
Monitoring One's Health:
Smartphones, tablets, and wearable computers have allowed people to monitor their own health. These devices run numerous applications that are designed to provide simple health services and the monitoring of one's health.
An example of this is Fitbit, a fitness tracker that is worn on the user's wrist. This wearable technology allows people to track their steps, heart rate, floors climbed, miles walked, active minutes, and even sleep patterns. The data collected and analyzed allow users not just to keep track of their own health but also help manage it, particularly through its capability to identify health risk factors.
There is also the case of the Internet, which serves as a repository of information and expert content that can be used to "self-diagnose" instead of going to their doctor. For instance, one need only enumerate symptoms as search parameters at Google and the search engine could identify the illness from the list of contents uploaded to the world wide web, particularly those provided by expert/medical sources.
These advance may eventually have some effect on doctor visits from patients and change the role of the health professionals from "gatekeeper to secondary care to facilitator of information interpretation and decision-making." Apart from basic services provided by Google in Search, there are also companies such as WebMD or Infermedica with its product Symptomate that already offer dedicated symptom-checking apps
Careers:
There are numerous careers to choose from in health technology in the USA. Listed below are some job titles and average salaries.
- Athletic Trainer, Salary: $41,340. Athletic trainers treat athletes and other individuals who have sustained injuries. They also teach people how to prevent injuries. They perform their job under the supervision of physicians.
- Dental Hygienist, Salary: $67,340. Dental hygienists provide preventative dental care and teach patients how to maintain good oral health. They usually work under dentists' supervision.
- Laboratory Technicians and Technologists, Salary: $51,770. Lab technicians and technologists perform laboratory tests and procedures. Technicians work under the supervision of a laboratory technologist or a laboratory manager.
- Nuclear Medicine Technologist, Salary: $67,910. Nuclear medicine technologists prepare and administer radiopharmaceuticals, radioactive drugs, to patients in order to treat or diagnose diseases.
- Pharmacy Technician, Salary: $28,070. Pharmacy technicians assist pharmacists with the preparation of prescription medications for customers.
Health Updates from AARP Magazine, October/November 2018 Issue YouTube Videos: Pictured below:
(L) Belinda Smith with her battery-operated “heart”
(R) CAR T-cell therapy helped eliminate tumors on Marge Jacques' neck.
(L) Belinda Smith with her battery-operated “heart”
(R) CAR T-cell therapy helped eliminate tumors on Marge Jacques' neck.
Heart Pump gives Patients More Time:
by Sari Harrar
BELINDA SMITH needed a new heart. Congestive heart failure had reduced the pumping power of her own ticker by 90 percent. “I needed a heart transplant, but I couldn’t wait that long,” recalls Smith, now 50, a mother of four from Dayton, Ohio. “Doctors gave me less than a year to live.” New hearts aren’t easy to come by.
There are about 4,000 people awaiting transplants, but just 2,500 donor hearts are available each year in the U.S. For people like Smith, though, there’s new hope: a battery-powered implant that plugs into the wall at night. Smith’s life was saved by one of these left ventricular assist devices (LVADs), which doctors installed in her chest in 2017. “It does the work my heart can’t do, pumping blood out into my body,” Smith explains. “I can do almost everything I did before — I just can’t get the cord and batteries wet. I have a waterproof bag for taking a shower, but I can’t go swimming.”
Her LVAD is the size of a D battery and weighs less than a pound.
During the day it runs on a battery pack attached to a power cord extending through her chest wall. “I carry two tote bags whenever I leave my apartment — with my controller, extra batteries, a car charger and an extra pump. If the batteries ever run out, I’ve got less than five minutes to plug in new ones,” she notes. “When I’m going to sleep, I plug myself into a wall outlet with a 25-foot power cord.” LVADs pump blood continuously; users don’t have a heartbeat. “You have to wear a medical-alert bracelet so EMTs don’t think you’re dead or try to give you CPR. That would crush the pump,” Smith says. “But I can hear the sound of the pump when I put my head on my arm at night. It purrs.”
Smith hopes to get a spot on a heart-transplant list soon. But for thousands of adults with heart failure, an LVAD is their future. The Food and Drug Administration last fall approved the first LVAD as a “destination therapy” for indefinite use for people with end-stage heart failure who aren’t candidates for a heart transplant.
“For more and more people, LVADs are a long-term option,” says Smith’s cardiologist, Hareeprasad R. Vongooru. “For someone with severe heart failure whose one-year survival odds are as low as 25 percent, this is a new lease on life.”
In-Artery Sensor Tracks Heart Failure:
For 25 percent of the 5.7 million Americans with congestive heart failure, the heart’s ability to pump blood is dangerously weak. Just walking across the room leaves them breathless. The risk of dying within a year is as high as 15 percent. Catching signs of worsening heart failure early is crucial, so a daily weigh-in to check for water-weight gain is required.
Now the first miniature sensor for this purpose picks up heart changes sooner, by sensing blood pressure shifts inside the pulmonary artery. The device, called CardioMEMS, has cut the risk of death by a respectable 30 percent in people with severe heart failure, according to a brand-new study of 2,174 people presented at the American College of Cardiology’s 67th annual Scientific Session & Expo this year.
The wireless sensor, about the size of a half-inch piece of spaghetti, transmits a constant stream of data to a website monitored by a health care practitioner who can quickly recommend medication adjustments.
On the Horizon: Heart Failure Treatment:
"The big push is prevention. That means giving people not just aspirin and cholesterol-lowering statins but also beta-blockers, ACE inhibitors and the diuretic Aldactone (spironolactone), all of which help protect heart muscle after a heart attack. Though these drugs are recognized for helping to prevent heart failure, they are not always given to people after a heart attack. The other important push is controlling high blood pressure. Even in older adults, keeping blood pressure at a healthy level can reduce the risk for heart failure."
— HAREEPRASAD R. VONGOORU, cardiologist and assistant professor of cardiovascular health and disease at the University of Cincinnati
___________________________________________________________________________
New Weapons in Fight Against Cancer
CAR T-cell therapy, gene testing can help beat this deadly disease
by Sari Harrar, AARP The Magazine, October/November 2018
MARGE JACQUES battled non-Hodgkin’s lymphoma for 15 years, but the white blood cell cancer kept coming back despite multidrug chemotherapy cocktails, liquid radiation and even stem cell therapy. “It returned every two years. In 2014 I had lumps all down my neck, because there were tumors in my lymph glands,” says Jacques, now 63. “I cried as I drove to see my oncologist in Philadelphia. Then he told me there was something new to try.”
Jacques became one of the first American adults to get CAR T-cell therapy — the nation’s first personalized cellular cancer treatment — for her specific cancer, diffuse large B-cell lymphoma. The treatment removed some of her T cells, which are the immune system’s frontline killers. The cells were then genetically modified to produce a receptor that will attach to cancer cells and attack them.
Miraculously, Jacques’ cancer went into remission. “Slowly, the tumors shrank. Blood tests and scans showed it was gone,” she adds. Even better: It has not returned, and she is back to enjoying life. “Throughout my years with cancer, I never felt sorry for myself. But it’s a rocky road,” says this single mother and project manager from Collegeville, Pa. “Humor, family and friends got me through all this.”
Today the groundbreaking treatment is available commercially. In October 2017 and May 2018, the Food and Drug Administration (FDA) approved two CAR T-cell drugs for patients such as Jacques, whose diffuse large B-cell lymphoma doesn’t respond to other treatments.
Experts expect that these drugs, which are covered by Medicare, will be deployed against a variety of cancers in the future. “This is a spectacular new therapy,” notes Jacques’ oncologist, CAR T-cell researcher Stephen J. Schuster, director of the lymphoma program at the University of Pennsylvania. “It’s saving the lives of people whose prognosis was measured in months, not years. In studies, 50 percent respond and about 1 in 3 are long-term, disease-free survivors.”
Mega Gene Test Checks for Targeted Cancer Treatment:
Designated a breakthrough by the FDA when it was approved in late 2017, FoundationOne CDx is one-stop shopping for gene-based treatments. Just one test can check for mutations in 324 genes involved in cancer growth, allowing oncologists to identify the most promising treatments quickly. The FDA recently approved a similar test from Memorial Sloan Kettering Cancer Center in New York City; it’s called MSK-Impact, and it looks for mutations in 468 genes.
On the Horizon: Cancer Treatment:
"From August 2017 through July 2018, the FDA approved 14 new anticancer therapeutics. These include nine molecularly targeted therapeutics, part of the new wave of precision medicines, as well as two targeted forms of radiotherapy and two new CAR T-cell therapies.
There are preclinical studies of vaccines that target oncogenes (early genetic changes that initiate cancers). We expect to see these tested in the next few years in individuals who are at high risk for cancer development."
— ELIZABETH M. JAFFEE, oncologist and president of the American Association for Cancer Research
by Sari Harrar
BELINDA SMITH needed a new heart. Congestive heart failure had reduced the pumping power of her own ticker by 90 percent. “I needed a heart transplant, but I couldn’t wait that long,” recalls Smith, now 50, a mother of four from Dayton, Ohio. “Doctors gave me less than a year to live.” New hearts aren’t easy to come by.
There are about 4,000 people awaiting transplants, but just 2,500 donor hearts are available each year in the U.S. For people like Smith, though, there’s new hope: a battery-powered implant that plugs into the wall at night. Smith’s life was saved by one of these left ventricular assist devices (LVADs), which doctors installed in her chest in 2017. “It does the work my heart can’t do, pumping blood out into my body,” Smith explains. “I can do almost everything I did before — I just can’t get the cord and batteries wet. I have a waterproof bag for taking a shower, but I can’t go swimming.”
Her LVAD is the size of a D battery and weighs less than a pound.
During the day it runs on a battery pack attached to a power cord extending through her chest wall. “I carry two tote bags whenever I leave my apartment — with my controller, extra batteries, a car charger and an extra pump. If the batteries ever run out, I’ve got less than five minutes to plug in new ones,” she notes. “When I’m going to sleep, I plug myself into a wall outlet with a 25-foot power cord.” LVADs pump blood continuously; users don’t have a heartbeat. “You have to wear a medical-alert bracelet so EMTs don’t think you’re dead or try to give you CPR. That would crush the pump,” Smith says. “But I can hear the sound of the pump when I put my head on my arm at night. It purrs.”
Smith hopes to get a spot on a heart-transplant list soon. But for thousands of adults with heart failure, an LVAD is their future. The Food and Drug Administration last fall approved the first LVAD as a “destination therapy” for indefinite use for people with end-stage heart failure who aren’t candidates for a heart transplant.
“For more and more people, LVADs are a long-term option,” says Smith’s cardiologist, Hareeprasad R. Vongooru. “For someone with severe heart failure whose one-year survival odds are as low as 25 percent, this is a new lease on life.”
In-Artery Sensor Tracks Heart Failure:
For 25 percent of the 5.7 million Americans with congestive heart failure, the heart’s ability to pump blood is dangerously weak. Just walking across the room leaves them breathless. The risk of dying within a year is as high as 15 percent. Catching signs of worsening heart failure early is crucial, so a daily weigh-in to check for water-weight gain is required.
Now the first miniature sensor for this purpose picks up heart changes sooner, by sensing blood pressure shifts inside the pulmonary artery. The device, called CardioMEMS, has cut the risk of death by a respectable 30 percent in people with severe heart failure, according to a brand-new study of 2,174 people presented at the American College of Cardiology’s 67th annual Scientific Session & Expo this year.
The wireless sensor, about the size of a half-inch piece of spaghetti, transmits a constant stream of data to a website monitored by a health care practitioner who can quickly recommend medication adjustments.
On the Horizon: Heart Failure Treatment:
"The big push is prevention. That means giving people not just aspirin and cholesterol-lowering statins but also beta-blockers, ACE inhibitors and the diuretic Aldactone (spironolactone), all of which help protect heart muscle after a heart attack. Though these drugs are recognized for helping to prevent heart failure, they are not always given to people after a heart attack. The other important push is controlling high blood pressure. Even in older adults, keeping blood pressure at a healthy level can reduce the risk for heart failure."
— HAREEPRASAD R. VONGOORU, cardiologist and assistant professor of cardiovascular health and disease at the University of Cincinnati
___________________________________________________________________________
New Weapons in Fight Against Cancer
CAR T-cell therapy, gene testing can help beat this deadly disease
by Sari Harrar, AARP The Magazine, October/November 2018
MARGE JACQUES battled non-Hodgkin’s lymphoma for 15 years, but the white blood cell cancer kept coming back despite multidrug chemotherapy cocktails, liquid radiation and even stem cell therapy. “It returned every two years. In 2014 I had lumps all down my neck, because there were tumors in my lymph glands,” says Jacques, now 63. “I cried as I drove to see my oncologist in Philadelphia. Then he told me there was something new to try.”
Jacques became one of the first American adults to get CAR T-cell therapy — the nation’s first personalized cellular cancer treatment — for her specific cancer, diffuse large B-cell lymphoma. The treatment removed some of her T cells, which are the immune system’s frontline killers. The cells were then genetically modified to produce a receptor that will attach to cancer cells and attack them.
Miraculously, Jacques’ cancer went into remission. “Slowly, the tumors shrank. Blood tests and scans showed it was gone,” she adds. Even better: It has not returned, and she is back to enjoying life. “Throughout my years with cancer, I never felt sorry for myself. But it’s a rocky road,” says this single mother and project manager from Collegeville, Pa. “Humor, family and friends got me through all this.”
Today the groundbreaking treatment is available commercially. In October 2017 and May 2018, the Food and Drug Administration (FDA) approved two CAR T-cell drugs for patients such as Jacques, whose diffuse large B-cell lymphoma doesn’t respond to other treatments.
Experts expect that these drugs, which are covered by Medicare, will be deployed against a variety of cancers in the future. “This is a spectacular new therapy,” notes Jacques’ oncologist, CAR T-cell researcher Stephen J. Schuster, director of the lymphoma program at the University of Pennsylvania. “It’s saving the lives of people whose prognosis was measured in months, not years. In studies, 50 percent respond and about 1 in 3 are long-term, disease-free survivors.”
Mega Gene Test Checks for Targeted Cancer Treatment:
Designated a breakthrough by the FDA when it was approved in late 2017, FoundationOne CDx is one-stop shopping for gene-based treatments. Just one test can check for mutations in 324 genes involved in cancer growth, allowing oncologists to identify the most promising treatments quickly. The FDA recently approved a similar test from Memorial Sloan Kettering Cancer Center in New York City; it’s called MSK-Impact, and it looks for mutations in 468 genes.
On the Horizon: Cancer Treatment:
"From August 2017 through July 2018, the FDA approved 14 new anticancer therapeutics. These include nine molecularly targeted therapeutics, part of the new wave of precision medicines, as well as two targeted forms of radiotherapy and two new CAR T-cell therapies.
There are preclinical studies of vaccines that target oncogenes (early genetic changes that initiate cancers). We expect to see these tested in the next few years in individuals who are at high risk for cancer development."
— ELIZABETH M. JAFFEE, oncologist and president of the American Association for Cancer Research
Regenerative Medicine including Tissue Engineering by Mooney Lab Laboratory for Cell and Tissue Engineering (Harvard University)
YouTube Video: Healing from Within: The Promise of Regenerative Medicine (Mayo Clinic)
Pictured below: Tissue Engineering and Regenerative Medicine (see further amplification by Mooney Labs following image)
Tissue Engineering and Regenerative Medicine by Mooney Lab
Laboratory for Cell and Tissue Engineering (Harvard University): "There is a tremendous need for new strategies to promote the regeneration of musculoskeletal, skin, vascular and dental/oral/craniofacial tissues, due to the large number of patients suffering from disease or trauma to these tissues.."
Regenerative Medicine by Wikipedia:
Regenerative medicine is a branch of translational research in tissue engineering and molecular biology which deals with the "process of replacing, engineering or regenerating human cells, tissues or organs to restore or establish normal function". This field holds the promise of engineering damaged tissues and organs by stimulating the body's own repair mechanisms to functionally heal previously irreparable tissues or organs.
Regenerative medicine also includes the possibility of growing tissues and organs in the laboratory and implanting them when the body cannot heal itself. If a regenerated organ's cells would be derived from the patient's own tissue or cells, this would potentially solve the problem of the shortage of organs available for donation, and the problem of organ transplant rejection.
Some of the biomedical approaches within the field of regenerative medicine may involve the use of stem cells. Examples include the injection of stem cells or progenitor cells obtained through directed differentiation (cell therapies); the induction of regeneration by biologically active molecules administered alone or as a secretion by infused cells (immunomodulation therapy); and transplantation of in vitro grown organs and tissues (tissue engineering).
Click on any of the following blue hyperlinks for more about Regenerative Medicine:
Laboratory for Cell and Tissue Engineering (Harvard University): "There is a tremendous need for new strategies to promote the regeneration of musculoskeletal, skin, vascular and dental/oral/craniofacial tissues, due to the large number of patients suffering from disease or trauma to these tissues.."
Regenerative Medicine by Wikipedia:
Regenerative medicine is a branch of translational research in tissue engineering and molecular biology which deals with the "process of replacing, engineering or regenerating human cells, tissues or organs to restore or establish normal function". This field holds the promise of engineering damaged tissues and organs by stimulating the body's own repair mechanisms to functionally heal previously irreparable tissues or organs.
Regenerative medicine also includes the possibility of growing tissues and organs in the laboratory and implanting them when the body cannot heal itself. If a regenerated organ's cells would be derived from the patient's own tissue or cells, this would potentially solve the problem of the shortage of organs available for donation, and the problem of organ transplant rejection.
Some of the biomedical approaches within the field of regenerative medicine may involve the use of stem cells. Examples include the injection of stem cells or progenitor cells obtained through directed differentiation (cell therapies); the induction of regeneration by biologically active molecules administered alone or as a secretion by infused cells (immunomodulation therapy); and transplantation of in vitro grown organs and tissues (tissue engineering).
Click on any of the following blue hyperlinks for more about Regenerative Medicine:
Mayo Clinic
- YouTube Video: Telemedicine Advances-Mayo Clinic
- YouTube Video: Mayo Clinic Minute: The Mayo Clinic Diet
- YouTube Video and theMayo Clinic Minute: What to Eat for Brain Health
The Mayo Clinic is a nonprofit academic medical center based in Rochester, Minnesota, focused on integrated clinical practice, education, and research. It employs more than 4,500 physicians and scientists, along with another 58,400 administrative and allied health staff.
The practice specializes in treating difficult cases through tertiary care and destination medicine. It is home to the highly ranked Mayo Clinic Alix School of Medicine in addition to many of the largest, best regarded residency education programs in the United States. It spends over $660 million a year on research and has more than 3,000 full-time research personnel.
William Worrall Mayo settled his family in Rochester in 1864 and opened a sole proprietorship medical practice that evolved under his sons, Will and Charlie Mayo, into Mayo Clinic.
Today, in addition to its flagship hospital in Rochester, Mayo Clinic has major campuses in Arizona and Florida. The Mayo Clinic Health System also operates affiliated facilities throughout Minnesota, Wisconsin, and Iowa.
Mayo Clinic is ranked number 1 in the United States on the 2018–2019 U.S. News & World Report Best Hospitals Honor Roll, maintaining a position at or near the top for more than 27 years. It has been on the list of "100 Best Companies to Work For" published by Fortune magazine for fourteen consecutive years, and has continued to achieve this ranking through 2017.
Core Operations:
Patient care:
Each year, more than 1.3 million different patients from all 50 states and from more than 150 countries are seen at one of the Mayo Clinic facilities. Mayo Clinic offers highly specialized medical care, and a large portion of the patient population are referrals from smaller clinics and hospitals across the upper Midwest and the United States.
Mayo Clinic physicians are paid a fixed salary, which is not linked to patient volume (relative value units) or income from fee-for-service payments. This practice is thought to decrease the monetary motivation to see patients in excessive numbers and increase the incentive to spend more time with individuals. Salaries are determined by the marketplace salaries for physicians in comparable large group practices.
Research:
Mayo Clinic researchers contribute to the understanding of disease processes, best clinical practices, and translation of findings from the laboratory to the clinical practice. Nearly 600 doctoral level physicians and research scientists are employed, with an additional 3,400 other health personnel and students with appointments in research.
In 2015, more than 2,700 research protocols were reviewed by the Mayo Clinic Institutional review board and 11,000 ongoing human research studies. These research initiatives led to more than 7,300 research publications and review articles in peer-review journals.[6]
Education:
Main article: Mayo Clinic College of Medicine and Science
The Mayo Clinic College of Medicine and Science (MCCMS), established in 1915, offers educational programs embedded in Mayo Clinic's clinical practice and biomedical research activities.
MCCMS consists of five accredited schools, including the M.D. degree-granting Mayo Clinic Alix School of Medicine as well as the master's and Ph.D. degree-granting Mayo Clinic Graduate School of Biomedical Sciences.
The Mayo Clinic School of Health Sciences offers training for about 50 health sciences career fields. The Mayo Clinic School of Graduate Medical Education runs over 270 residences and fellowships in all medical and surgical specialties. The Mayo Clinic School of Continuous Professional Development delivers continuing education courses aimed at practicing medical professionals.
Innovation:
Mayo Clinic has adopted more than 15,000 mobile devices from Apple for patient care; including the iPad, iPad Mini and iPhone. Mayo Clinic then created an app for these devices called Synthesis Mobile, which integrated hundreds of their health systems. For Mayo Clinic Care Network members, more apps were created to help patients see their medical records or ask clinicians for assistance.
In 2014, Mayo Clinic was developing an app for Apple's HealthKit to help users maintain healthy lifestyles and warn of certain health signs that need attention.
Mayo Clinic, in collaboration with real estate firm Delos Living, launched the Well Living Lab in September 2015. This research facility is designed to simulate real-world, non-hospital environments to allow Mayo Clinic researchers to study the interaction between indoor spaces and human health.
The Mayo Clinic Center for Innovation, established in 2008, was one of the pioneers of innovation in healthcare. It has since worked on over 270 projects and is often looked to as a role model for using design in healthcare.
In March 2018, Mayo Clinic and Mytonomy, a healthcare education system company, partnered to provide video content for cancer patients. The video content is used to address important questions and answers and designed to aid in the decision-making process between patient and doctor.
Click on any of the following blue hyperlinks for more about the Mayo Clinic:
The practice specializes in treating difficult cases through tertiary care and destination medicine. It is home to the highly ranked Mayo Clinic Alix School of Medicine in addition to many of the largest, best regarded residency education programs in the United States. It spends over $660 million a year on research and has more than 3,000 full-time research personnel.
William Worrall Mayo settled his family in Rochester in 1864 and opened a sole proprietorship medical practice that evolved under his sons, Will and Charlie Mayo, into Mayo Clinic.
Today, in addition to its flagship hospital in Rochester, Mayo Clinic has major campuses in Arizona and Florida. The Mayo Clinic Health System also operates affiliated facilities throughout Minnesota, Wisconsin, and Iowa.
Mayo Clinic is ranked number 1 in the United States on the 2018–2019 U.S. News & World Report Best Hospitals Honor Roll, maintaining a position at or near the top for more than 27 years. It has been on the list of "100 Best Companies to Work For" published by Fortune magazine for fourteen consecutive years, and has continued to achieve this ranking through 2017.
Core Operations:
Patient care:
Each year, more than 1.3 million different patients from all 50 states and from more than 150 countries are seen at one of the Mayo Clinic facilities. Mayo Clinic offers highly specialized medical care, and a large portion of the patient population are referrals from smaller clinics and hospitals across the upper Midwest and the United States.
Mayo Clinic physicians are paid a fixed salary, which is not linked to patient volume (relative value units) or income from fee-for-service payments. This practice is thought to decrease the monetary motivation to see patients in excessive numbers and increase the incentive to spend more time with individuals. Salaries are determined by the marketplace salaries for physicians in comparable large group practices.
Research:
Mayo Clinic researchers contribute to the understanding of disease processes, best clinical practices, and translation of findings from the laboratory to the clinical practice. Nearly 600 doctoral level physicians and research scientists are employed, with an additional 3,400 other health personnel and students with appointments in research.
In 2015, more than 2,700 research protocols were reviewed by the Mayo Clinic Institutional review board and 11,000 ongoing human research studies. These research initiatives led to more than 7,300 research publications and review articles in peer-review journals.[6]
Education:
Main article: Mayo Clinic College of Medicine and Science
The Mayo Clinic College of Medicine and Science (MCCMS), established in 1915, offers educational programs embedded in Mayo Clinic's clinical practice and biomedical research activities.
MCCMS consists of five accredited schools, including the M.D. degree-granting Mayo Clinic Alix School of Medicine as well as the master's and Ph.D. degree-granting Mayo Clinic Graduate School of Biomedical Sciences.
The Mayo Clinic School of Health Sciences offers training for about 50 health sciences career fields. The Mayo Clinic School of Graduate Medical Education runs over 270 residences and fellowships in all medical and surgical specialties. The Mayo Clinic School of Continuous Professional Development delivers continuing education courses aimed at practicing medical professionals.
Innovation:
Mayo Clinic has adopted more than 15,000 mobile devices from Apple for patient care; including the iPad, iPad Mini and iPhone. Mayo Clinic then created an app for these devices called Synthesis Mobile, which integrated hundreds of their health systems. For Mayo Clinic Care Network members, more apps were created to help patients see their medical records or ask clinicians for assistance.
In 2014, Mayo Clinic was developing an app for Apple's HealthKit to help users maintain healthy lifestyles and warn of certain health signs that need attention.
Mayo Clinic, in collaboration with real estate firm Delos Living, launched the Well Living Lab in September 2015. This research facility is designed to simulate real-world, non-hospital environments to allow Mayo Clinic researchers to study the interaction between indoor spaces and human health.
The Mayo Clinic Center for Innovation, established in 2008, was one of the pioneers of innovation in healthcare. It has since worked on over 270 projects and is often looked to as a role model for using design in healthcare.
In March 2018, Mayo Clinic and Mytonomy, a healthcare education system company, partnered to provide video content for cancer patients. The video content is used to address important questions and answers and designed to aid in the decision-making process between patient and doctor.
Click on any of the following blue hyperlinks for more about the Mayo Clinic:
Breakthrough Medical Therapy (FDA)
- YouTube Video: Breakthrough Therapy (FDA December 2015)
- YouTube Video: FDA Approves Breakthrough Cancer Treatment
Breakthrough therapy is a United States Food and Drug Administration designation that expedites drug development that was created by Congress under Section 902 of the 9 July 2012 Food and Drug Administration Safety and Innovation Act.
The FDA's "breakthrough therapy" designation is not intended to imply that a drug is actually a "breakthrough" or that there is high-quality evidence of treatment efficacy for a particular condition; rather, it allows the FDA to grant priority review to drug candidates if preliminary clinical trials indicate that the therapy may offer substantial treatment advantages over existing options for patients with serious or life-threatening diseases.
The FDA has other mechanisms for expediting the review and approval process for promising drugs, including fast track designation, accelerated approval, and priority review.
Requirements:
A breakthrough therapy designation can be assigned to a drug if "it is a drug which is intended alone or in combination with one or more other drugs to treat a serious or life threatening disease or condition" and if the preliminary clinical evidence indicates that the drug may demonstrate substantial improvement over existing therapies on one or more clinically significant endpoints, such as substantial treatment effects observed early in clinical development."
Requests are reviewed by the Center for Drug Evaluation and Research (CDER) and the Center for Biologics Evaluation and Research (CBER). CDER receives approximately 100 requests per year for breakthrough designation. Historically, about one third were approved. CBER receives 15–30 requests per year.
Sponsors must apply for breakthrough status separately for each indication they intend to label the drug for.
Breakthrough designation applications are submitted as an amendment to the IND applications before the initiation of clinical trials.
Incentives:
Drugs that have been granted breakthrough status are given priority review. The FDA works with the sponsor of the drug application to expedite the approval process. This expedited process can include rolling reviews, smaller clinical trials, and alternative trial designs.
Issues:
Critics have said that the name is misleading and provides companies that obtain a breakthrough designation for a drug candidate with a marketing advantage that may be undeserved.
The FDA acknowledges that the name "breakthrough therapy" may be misleading. It was never meant to imply that these drugs are actually “breakthroughs,” and it does not ensure that they will provide clinical benefit, but still critics complain that they are based on preliminary evidence, including changes in surrogate markers such as laboratory measurements, that often don't reflect "meaningful clinical benefit."
The FDA guidance states: "Not all products designated as breakthrough therapies ultimately will be shown to have the substantial improvement over available therapies suggested by the preliminary clinical evidence at the time of designation. If the designation is no longer supported by subsequent data, FDA may rescind the designation."
See also:
The FDA's "breakthrough therapy" designation is not intended to imply that a drug is actually a "breakthrough" or that there is high-quality evidence of treatment efficacy for a particular condition; rather, it allows the FDA to grant priority review to drug candidates if preliminary clinical trials indicate that the therapy may offer substantial treatment advantages over existing options for patients with serious or life-threatening diseases.
The FDA has other mechanisms for expediting the review and approval process for promising drugs, including fast track designation, accelerated approval, and priority review.
Requirements:
A breakthrough therapy designation can be assigned to a drug if "it is a drug which is intended alone or in combination with one or more other drugs to treat a serious or life threatening disease or condition" and if the preliminary clinical evidence indicates that the drug may demonstrate substantial improvement over existing therapies on one or more clinically significant endpoints, such as substantial treatment effects observed early in clinical development."
Requests are reviewed by the Center for Drug Evaluation and Research (CDER) and the Center for Biologics Evaluation and Research (CBER). CDER receives approximately 100 requests per year for breakthrough designation. Historically, about one third were approved. CBER receives 15–30 requests per year.
Sponsors must apply for breakthrough status separately for each indication they intend to label the drug for.
Breakthrough designation applications are submitted as an amendment to the IND applications before the initiation of clinical trials.
Incentives:
Drugs that have been granted breakthrough status are given priority review. The FDA works with the sponsor of the drug application to expedite the approval process. This expedited process can include rolling reviews, smaller clinical trials, and alternative trial designs.
Issues:
Critics have said that the name is misleading and provides companies that obtain a breakthrough designation for a drug candidate with a marketing advantage that may be undeserved.
The FDA acknowledges that the name "breakthrough therapy" may be misleading. It was never meant to imply that these drugs are actually “breakthroughs,” and it does not ensure that they will provide clinical benefit, but still critics complain that they are based on preliminary evidence, including changes in surrogate markers such as laboratory measurements, that often don't reflect "meaningful clinical benefit."
The FDA guidance states: "Not all products designated as breakthrough therapies ultimately will be shown to have the substantial improvement over available therapies suggested by the preliminary clinical evidence at the time of designation. If the designation is no longer supported by subsequent data, FDA may rescind the designation."
See also:
- Official FDA Website
- List of drugs granted breakthrough therapy designation
- FDA Fast Track Development Program
- Priority review (FDA)
- Orphan drug
Mental Health including Body Image and Self-Esteem
YouTube Video: To reach beyond your limits by training your mind
(By Marisa Peer | TEDxKCS)
Pictured: Negative perceptions of Mental Health, Body Image and Self-esteem
YouTube Video: To reach beyond your limits by training your mind
(By Marisa Peer | TEDxKCS)
Pictured: Negative perceptions of Mental Health, Body Image and Self-esteem
Mental health is a level of psychological well-being, or an absence of mental illness. It is the "psychological state of someone who is functioning at a satisfactory level of emotional and behavioral adjustment". From the perspective of positive psychology or holism, mental health may include an individual's ability to enjoy life, and create a balance between life activities and efforts to achieve psychological resilience.
According to the World Health Organization (WHO), mental health includes "subjective well-being, perceived self-efficacy, autonomy, competence, inter-generational dependence, and self-actualization of one's intellectual and emotional potential, among others."
The WHO further states that the well-being of an individual is encompassed in the realization of their abilities, coping with normal stresses of life, productive work and contribution to their community. Cultural differences, subjective assessments, and competing professional theories all affect how "mental health" is defined. A widely accepted definition of health by mental health specialists is psychoanalyst Sigmund Freud's definition: the capacity "to work and to love".
Mental Health and Mental Illness:
According to the U.S. surgeon general (1999), mental health is the successful performance of mental function, resulting in productive activities, fulfilling relationships with other people, and providing the ability to adapt to change and cope with adversity. The term mental illness refers collectively to all diagnosable mental disorders—health conditions characterized by alterations in thinking, mood, or behavior associated with distress or impaired functioning.
A person struggling with their mental health may experience stress, depression, anxiety, relationship problems, grief, addiction, ADHD or learning disabilities, mood disorders, or other mental illnesses of varying degrees.
Therapists, psychiatrists, psychologists, social workers, nurse practitioners or physicians can help manage mental illness with treatments such as therapy, counseling, or medication.
Click on any of the following blue hyperlinks for more about Mental Health:
Body Image is a person's perception of the aesthetics or sexual attractiveness of their own body. The phrase body image was first coined by the Austrian neurologist and psychoanalyst Paul Schilder in his book The Image and Appearance of the Human Body (1935).
Human society has at all times placed great value on beauty of the human body, but a person's perception of their own body may not correspond to society's standards.
The concept of body image is used in a number of disciplines, including psychology, medicine, psychiatry, psychoanalysis, philosophy and cultural and feminist studies. The term is also often used in the media. Across these disciplines and media there is no consensus definition.
A person's body image is thought to be, in part, a product of their personal experiences, personality, and various social and cultural forces. A person's sense of their own physical appearance, usually in relation to others or in relation to some cultural "ideal," can shape their body image. A person's perception of their appearance can be different from how others actually perceive them.
Research suggests that exposure to mass media depicting the thin-ideal body may be linked to body image disturbance in women. This meta-analysis examined experimental and correlational studies testing the links between media exposure to body dissatisfaction, internalization of the thin ideal, and eating behaviors and beliefs with a sample of 77 studies that yielded 141 effect sizes.
Effects for some outcome variables were moderated by publication year and study design. The findings support the notion that exposure to media images depicting the thin-ideal body is related to body image concerns for women.
A 2007 report by the American Psychological Association found that a culture-wide sexualization of girls and women was contributing to increased female anxiety associated with body image.
Similar findings associated with body image were found by an Australian government Senate Standing Committee report on the sexualization of children in the media. However, other scholars have expressed concern that these claims are not based on solid data.
Body image can have a wide range of psychological effects and physical effects. Throughout history, it has been extremely difficult for people to live up to the standards of society and what they believe the ideal body is.
There are many factors that lead to a person’s body image, some of these include: family dynamics, mental illness, biological predispositions and environmental causes for obesity or malnutrition, and cultural expectations (e.g., media and politics).
People who are both underweight and overweight can have poor body image. However, because people are constantly told and shown the cosmetic appeal of weight loss and are warned about the risks of obesity, those who are normal or overweight on the BMI scale have higher risks of poor body image.
This is something that can lead to a change in a person's body image. Often, people who have a low body image will try to alter their bodies in some way, such as by dieting or undergoing cosmetic surgery.
Click on any of the following blue hyperlinks for more about Body Image:
Self-esteem:
In sociology and psychology, self-esteem reflects a person's overall subjective emotional evaluation of his or her own worth. It is a judgment of oneself as well as an attitude toward the self. Self-esteem encompasses beliefs about oneself, (for example, "I am competent", "I am worthy"), as well as emotional states, such as triumph, despair, pride, and shame.
Smith and Mackie (2007) defined it by saying "The self-concept is what we think about the self; self-esteem, is the positive or negative evaluations of the self, as in how we feel about it.".
Self-esteem is attractive as a social psychological construct because researchers have conceptualized it as an influential predictor of certain outcomes, such as academic achievement, happiness, satisfaction in marriage and relationships, and criminal behavior.
Self-esteem can apply specifically to a particular dimension (for example, "I believe I am a good writer and feel happy about that") or a global extent (for example, "I believe I am a bad person, and feel bad about myself in general").
Psychologists usually regard self-esteem as an enduring personality characteristic ("trait" self-esteem), though normal, short-term variations ("state" self-esteem) also exist. Synonyms or near-synonyms of self-esteem include: self-worth, self-regard, self-respect, and self-integrity
Click on any of the following blue hyperlinks for more about Self Esteem:
According to the World Health Organization (WHO), mental health includes "subjective well-being, perceived self-efficacy, autonomy, competence, inter-generational dependence, and self-actualization of one's intellectual and emotional potential, among others."
The WHO further states that the well-being of an individual is encompassed in the realization of their abilities, coping with normal stresses of life, productive work and contribution to their community. Cultural differences, subjective assessments, and competing professional theories all affect how "mental health" is defined. A widely accepted definition of health by mental health specialists is psychoanalyst Sigmund Freud's definition: the capacity "to work and to love".
Mental Health and Mental Illness:
According to the U.S. surgeon general (1999), mental health is the successful performance of mental function, resulting in productive activities, fulfilling relationships with other people, and providing the ability to adapt to change and cope with adversity. The term mental illness refers collectively to all diagnosable mental disorders—health conditions characterized by alterations in thinking, mood, or behavior associated with distress or impaired functioning.
A person struggling with their mental health may experience stress, depression, anxiety, relationship problems, grief, addiction, ADHD or learning disabilities, mood disorders, or other mental illnesses of varying degrees.
Therapists, psychiatrists, psychologists, social workers, nurse practitioners or physicians can help manage mental illness with treatments such as therapy, counseling, or medication.
Click on any of the following blue hyperlinks for more about Mental Health:
- History
- Significance
- Perspectives
- Mental well-being
- Children and young adults
- Prevention
- Cultural and religious considerations
- Emotional improvement
- Emotional issues
- Treatment
- Activity therapies
- Biofeedback
- Expressive therapies
- Group therapy
- Psychotherapy
- Meditation
- Spiritual counseling
- Social work in mental health Prevalence and programs
- Roles and functions
- History
- United States
- Canada
- India
- Australia
- See also:
- Ethnopsychopharmacology
- Health
- Mental environment
- Reason
- Sanity
- Technology and mental health issues
- World Mental Health Day
- Related disciplines and specialties
- Mental health in different occupations and regions
- National Institute of Mental Health (United States)
- The National Mental Health Development Unit (NMHDU), England
- Health-EU Portal Mental Health in the EU
Body Image is a person's perception of the aesthetics or sexual attractiveness of their own body. The phrase body image was first coined by the Austrian neurologist and psychoanalyst Paul Schilder in his book The Image and Appearance of the Human Body (1935).
Human society has at all times placed great value on beauty of the human body, but a person's perception of their own body may not correspond to society's standards.
The concept of body image is used in a number of disciplines, including psychology, medicine, psychiatry, psychoanalysis, philosophy and cultural and feminist studies. The term is also often used in the media. Across these disciplines and media there is no consensus definition.
A person's body image is thought to be, in part, a product of their personal experiences, personality, and various social and cultural forces. A person's sense of their own physical appearance, usually in relation to others or in relation to some cultural "ideal," can shape their body image. A person's perception of their appearance can be different from how others actually perceive them.
Research suggests that exposure to mass media depicting the thin-ideal body may be linked to body image disturbance in women. This meta-analysis examined experimental and correlational studies testing the links between media exposure to body dissatisfaction, internalization of the thin ideal, and eating behaviors and beliefs with a sample of 77 studies that yielded 141 effect sizes.
Effects for some outcome variables were moderated by publication year and study design. The findings support the notion that exposure to media images depicting the thin-ideal body is related to body image concerns for women.
A 2007 report by the American Psychological Association found that a culture-wide sexualization of girls and women was contributing to increased female anxiety associated with body image.
Similar findings associated with body image were found by an Australian government Senate Standing Committee report on the sexualization of children in the media. However, other scholars have expressed concern that these claims are not based on solid data.
Body image can have a wide range of psychological effects and physical effects. Throughout history, it has been extremely difficult for people to live up to the standards of society and what they believe the ideal body is.
There are many factors that lead to a person’s body image, some of these include: family dynamics, mental illness, biological predispositions and environmental causes for obesity or malnutrition, and cultural expectations (e.g., media and politics).
People who are both underweight and overweight can have poor body image. However, because people are constantly told and shown the cosmetic appeal of weight loss and are warned about the risks of obesity, those who are normal or overweight on the BMI scale have higher risks of poor body image.
This is something that can lead to a change in a person's body image. Often, people who have a low body image will try to alter their bodies in some way, such as by dieting or undergoing cosmetic surgery.
Click on any of the following blue hyperlinks for more about Body Image:
- Media Impact
- On women and in general
- On men
- On fashion industry
- Social media and disorders
- Measurement
- Figure preferences
- Video projection techniques
- Questionnaires
- Gender differences
- Weight
- Race
- See also:
Self-esteem:
In sociology and psychology, self-esteem reflects a person's overall subjective emotional evaluation of his or her own worth. It is a judgment of oneself as well as an attitude toward the self. Self-esteem encompasses beliefs about oneself, (for example, "I am competent", "I am worthy"), as well as emotional states, such as triumph, despair, pride, and shame.
Smith and Mackie (2007) defined it by saying "The self-concept is what we think about the self; self-esteem, is the positive or negative evaluations of the self, as in how we feel about it.".
Self-esteem is attractive as a social psychological construct because researchers have conceptualized it as an influential predictor of certain outcomes, such as academic achievement, happiness, satisfaction in marriage and relationships, and criminal behavior.
Self-esteem can apply specifically to a particular dimension (for example, "I believe I am a good writer and feel happy about that") or a global extent (for example, "I believe I am a bad person, and feel bad about myself in general").
Psychologists usually regard self-esteem as an enduring personality characteristic ("trait" self-esteem), though normal, short-term variations ("state" self-esteem) also exist. Synonyms or near-synonyms of self-esteem include: self-worth, self-regard, self-respect, and self-integrity
Click on any of the following blue hyperlinks for more about Self Esteem:
- History
- Effect on public policy
- Theories
- Measurement
- Development across lifespan
- Types
- Importance
- Neuroscience
- Criticism and controversy
- See also:
- Assertiveness
- Blue Eyed
- Clinical depression
- Dunning–Kruger effect
- Emotional competence
- Fear of negative evaluation
- Gumption trap
- Hubris
- Identity
- Inner critic
- Invisible support
- List of confidence tricks
- Optimism bias
- Outline of self
- Overconfidence effect
- Passiveness
- Performance anxiety
- Self-awareness
- Self-compassion
- Self-esteem functions
- Self-esteem instability
- Self-evaluation maintenance theory
- Self image
- Shyness
- Social anxiety
- Social phobia
- Suicide prevention
Crohn's Disease
- YouTube Video: What is Crohn's Disease?
- YouTube Video: Crohns or Colitis? - Mayo Clinic
- YouTube Video: Living with Crohn's Disease - BBC News
Crohn's disease is a type of inflammatory bowel disease (IBD) that may affect any part of the gastrointestinal tract from mouth to anus. Signs and symptoms often include abdominal pain, diarrhea (which may be bloody if inflammation is severe), fever, and weight loss.
Other complications may occur outside the gastrointestinal tract and include anemia, skin rashes, arthritis, inflammation of the eye, and tiredness. The skin rashes may be due to infections as well as pyoderma gangrenosum or erythema nodosum. Bowel obstruction may occur as a complication of chronic inflammation, and those with the disease are at greater risk of bowel cancer.
While the cause of Crohn's disease is unknown, it is believed to be due to a combination of environmental, immune, and bacterial factors in genetically susceptible individuals. It results in a chronic inflammatory disorder, in which the body's immune system attacks the gastrointestinal tract, possibly targeting microbial antigens.
While Crohn's is an immune-related disease, it does not appear to be an autoimmune disease (in that the immune system is not being triggered by the body itself). The exact underlying immune problem is not clear; however, it may be an immunodeficiency state.
About half of the overall risk is related to genetics with more than 70 genes having been found to be involved. Tobacco smokers are twice as likely to develop Crohn's disease as nonsmokers. It also often begins after gastroenteritis.
Diagnosis is based on a number of findings including biopsy and appearance of the bowel wall, medical imaging and description of the disease. Other conditions that can present similarly include irritable bowel syndrome and Behçet's disease.
There are no medications or surgical procedures that can cure Crohn's disease. Treatment options are intended to help with symptoms, maintain remission, and prevent relapse. In those newly diagnosed, a corticosteroid may be used for a brief period of time to rapidly improve symptoms alongside another medication such as either methotrexate or a thiopurine used to prevent recurrence.
Stopping smoking is recommended in people with Crohn's disease.
One in five people with the disease is admitted to hospital each year, and half of those with the disease will require surgery for the disease at some point over a ten-year period. While surgery should be used as little as possible, it is necessary to address some abscesses, certain bowel obstructions, and cancers. Checking for bowel cancer via colonoscopy is recommended every few years, starting eight years after the disease has begun.
Crohn's disease affects about 3.2 per 1,000 people in Europe and North America. It is less common in Asia and Africa. It has historically been more common in the developed world. Rates have, however, been increasing, particularly in the developing world, since the 1970s.
Inflammatory bowel disease resulted in 47,400 deaths in 2015 and those with Crohn's disease have a slightly reduced life expectancy. It tends to start in the teens and twenties, although it can occur at any age.
Males and females are equally affected. The disease was named after gastroenterologist Burrill Bernard Crohn, who in 1932, together with two other colleagues at Mount Sinai Hospital in New York, described a series of patients with inflammation of the terminal ileum of the small intestine, the area most commonly affected by the illness.
Click on any of the following blue hyperlinks for more about Crohn's Disease:
Other complications may occur outside the gastrointestinal tract and include anemia, skin rashes, arthritis, inflammation of the eye, and tiredness. The skin rashes may be due to infections as well as pyoderma gangrenosum or erythema nodosum. Bowel obstruction may occur as a complication of chronic inflammation, and those with the disease are at greater risk of bowel cancer.
While the cause of Crohn's disease is unknown, it is believed to be due to a combination of environmental, immune, and bacterial factors in genetically susceptible individuals. It results in a chronic inflammatory disorder, in which the body's immune system attacks the gastrointestinal tract, possibly targeting microbial antigens.
While Crohn's is an immune-related disease, it does not appear to be an autoimmune disease (in that the immune system is not being triggered by the body itself). The exact underlying immune problem is not clear; however, it may be an immunodeficiency state.
About half of the overall risk is related to genetics with more than 70 genes having been found to be involved. Tobacco smokers are twice as likely to develop Crohn's disease as nonsmokers. It also often begins after gastroenteritis.
Diagnosis is based on a number of findings including biopsy and appearance of the bowel wall, medical imaging and description of the disease. Other conditions that can present similarly include irritable bowel syndrome and Behçet's disease.
There are no medications or surgical procedures that can cure Crohn's disease. Treatment options are intended to help with symptoms, maintain remission, and prevent relapse. In those newly diagnosed, a corticosteroid may be used for a brief period of time to rapidly improve symptoms alongside another medication such as either methotrexate or a thiopurine used to prevent recurrence.
Stopping smoking is recommended in people with Crohn's disease.
One in five people with the disease is admitted to hospital each year, and half of those with the disease will require surgery for the disease at some point over a ten-year period. While surgery should be used as little as possible, it is necessary to address some abscesses, certain bowel obstructions, and cancers. Checking for bowel cancer via colonoscopy is recommended every few years, starting eight years after the disease has begun.
Crohn's disease affects about 3.2 per 1,000 people in Europe and North America. It is less common in Asia and Africa. It has historically been more common in the developed world. Rates have, however, been increasing, particularly in the developing world, since the 1970s.
Inflammatory bowel disease resulted in 47,400 deaths in 2015 and those with Crohn's disease have a slightly reduced life expectancy. It tends to start in the teens and twenties, although it can occur at any age.
Males and females are equally affected. The disease was named after gastroenterologist Burrill Bernard Crohn, who in 1932, together with two other colleagues at Mount Sinai Hospital in New York, described a series of patients with inflammation of the terminal ileum of the small intestine, the area most commonly affected by the illness.
Click on any of the following blue hyperlinks for more about Crohn's Disease:
- Signs and symptoms
- Cause
- Pathophysiology
- Diagnosis
- Management
- Prognosis
- Epidemiology
- History
- Research
- See also:
DNA (DeoxyriboNucleic Acid) including a List of Human Genes
YouTube Video: What is DNA and How Does it Work?
Pictured: The structure of the DNA double helix. The atoms in the structure are color-coded by element and the detailed structure of two base pairs are shown in the bottom right.
YouTube Video: What is DNA and How Does it Work?
Pictured: The structure of the DNA double helix. The atoms in the structure are color-coded by element and the detailed structure of two base pairs are shown in the bottom right.
Deoxyribonucleic acid (DNA) is a molecule that carries most of the genetic instructions used in the growth, development, functioning and reproduction of all known living organisms and many viruses.
DNA and RNA are nucleic acids; alongside proteins and complex carbohydrates, they are one of the three major types of macro molecule that are essential for all known forms of life.
Most DNA molecules consist of two biopolymer strands coiled around each other to form a double helix. The two DNA strands are known as polynucleotides since they are composed of simpler units called nucleotides.
Each nucleotide is composed of a nitrogen-containing nucleobase—either cytosine (C), guanine (G), adenine (A), or thymine (T)—as well as a sugar called deoxyribose and a phosphate group.
The nucleotides are joined to one another in a chain by covalent bonds between the sugar of one nucleotide and the phosphate of the next, resulting in an alternating sugar-phosphate backbone.
According to base pairing rules (A with T, and C with G), hydrogen bonds bind the nitrogenous bases of the two separate polynucleotide strands to make double-stranded DNA.
The total amount of related DNA base pairs on Earth is estimated at 5.0 x 1037, and weighs 50 billion tons. In comparison, the total mass of the biosphere has been estimated to be as much as 4 TtC (trillion tons of carbon).
DNA stores biological information. The DNA backbone is resistant to cleavage, and both strands of the double-stranded structure store the same biological information. Biological information is replicated as the two strands are separated. A significant portion of DNA (more than 98% for humans) is non-coding, meaning that these sections do not serve as patterns for protein sequences.
The two strands of DNA run in opposite directions to each other and are therefore anti-parallel. Attached to each sugar is one of four types of nucleobases (informally, bases). It is the sequence of these four nucleobases along the backbone that encodes biological information.
Under the genetic code, RNA strands are translated to specify the sequence of amino acids within proteins. These RNA strands are initially created using DNA strands as a template in a process called transcription.
Within cells, DNA is organized into long structures called chromosomes. During cell division these chromosomes are duplicated in the process of DNA replication, providing each cell its own complete set of chromosomes.
Eukaryotic organisms (animals, plants, fungi, and protists) store most of their DNA inside the cell nucleus and some of their DNA in organelles, such as mitochondria or chloroplasts.
In contrast, prokaryotes (bacteria and archaea) store their DNA only in the cytoplasm. Within the chromosomes, chromatin proteins such as histones compact and organize DNA. These compact structures guide the interactions between DNA and other proteins, helping control which parts of the DNA are transcribed.
DNA was first isolated by Friedrich Miescher in 1869. Its molecular structure was identified by James Watson and Francis Crick in 1953, whose model-building efforts were guided by X-ray diffraction data acquired by Rosalind Franklin.
DNA is used by researchers as a molecular tool to explore physical laws and theories, such as the ergodic theorem and the theory of elasticity. The unique material properties of DNA have made it an attractive molecule for material scientists and engineers interested in micro- and nano-fabrication. Among notable advances in this field are DNA origami and DNA-based hybrid materials.
Click here for further amplification.
____________________________________________________________
A List of Human Genes
The human genome is the complete set of nucleic acid sequences for humans, encoded as DNA within the 23 chromosome pairs in cell nuclei and in a small DNA molecule found within individual mitochondria.
Human genomes include both protein-coding DNA genes and noncoding DNA. Haploid human genomes, which are contained in germ cells (the egg and sperm gamete cells created in the meiosis phase of sexual reproduction before fertilization creates a zygote) consist of three billion DNA base pairs, while diploid genomes (found in somatic cells) have twice the DNA content.
While there are significant differences among the genomes of human individuals (on the order of 0.1%), these are considerably smaller than the differences between humans and their closest living relatives, the chimpanzees (approximately 4%) and bonobos.
Below is a List human genes by chromosome:
DNA and RNA are nucleic acids; alongside proteins and complex carbohydrates, they are one of the three major types of macro molecule that are essential for all known forms of life.
Most DNA molecules consist of two biopolymer strands coiled around each other to form a double helix. The two DNA strands are known as polynucleotides since they are composed of simpler units called nucleotides.
Each nucleotide is composed of a nitrogen-containing nucleobase—either cytosine (C), guanine (G), adenine (A), or thymine (T)—as well as a sugar called deoxyribose and a phosphate group.
The nucleotides are joined to one another in a chain by covalent bonds between the sugar of one nucleotide and the phosphate of the next, resulting in an alternating sugar-phosphate backbone.
According to base pairing rules (A with T, and C with G), hydrogen bonds bind the nitrogenous bases of the two separate polynucleotide strands to make double-stranded DNA.
The total amount of related DNA base pairs on Earth is estimated at 5.0 x 1037, and weighs 50 billion tons. In comparison, the total mass of the biosphere has been estimated to be as much as 4 TtC (trillion tons of carbon).
DNA stores biological information. The DNA backbone is resistant to cleavage, and both strands of the double-stranded structure store the same biological information. Biological information is replicated as the two strands are separated. A significant portion of DNA (more than 98% for humans) is non-coding, meaning that these sections do not serve as patterns for protein sequences.
The two strands of DNA run in opposite directions to each other and are therefore anti-parallel. Attached to each sugar is one of four types of nucleobases (informally, bases). It is the sequence of these four nucleobases along the backbone that encodes biological information.
Under the genetic code, RNA strands are translated to specify the sequence of amino acids within proteins. These RNA strands are initially created using DNA strands as a template in a process called transcription.
Within cells, DNA is organized into long structures called chromosomes. During cell division these chromosomes are duplicated in the process of DNA replication, providing each cell its own complete set of chromosomes.
Eukaryotic organisms (animals, plants, fungi, and protists) store most of their DNA inside the cell nucleus and some of their DNA in organelles, such as mitochondria or chloroplasts.
In contrast, prokaryotes (bacteria and archaea) store their DNA only in the cytoplasm. Within the chromosomes, chromatin proteins such as histones compact and organize DNA. These compact structures guide the interactions between DNA and other proteins, helping control which parts of the DNA are transcribed.
DNA was first isolated by Friedrich Miescher in 1869. Its molecular structure was identified by James Watson and Francis Crick in 1953, whose model-building efforts were guided by X-ray diffraction data acquired by Rosalind Franklin.
DNA is used by researchers as a molecular tool to explore physical laws and theories, such as the ergodic theorem and the theory of elasticity. The unique material properties of DNA have made it an attractive molecule for material scientists and engineers interested in micro- and nano-fabrication. Among notable advances in this field are DNA origami and DNA-based hybrid materials.
Click here for further amplification.
____________________________________________________________
A List of Human Genes
The human genome is the complete set of nucleic acid sequences for humans, encoded as DNA within the 23 chromosome pairs in cell nuclei and in a small DNA molecule found within individual mitochondria.
Human genomes include both protein-coding DNA genes and noncoding DNA. Haploid human genomes, which are contained in germ cells (the egg and sperm gamete cells created in the meiosis phase of sexual reproduction before fertilization creates a zygote) consist of three billion DNA base pairs, while diploid genomes (found in somatic cells) have twice the DNA content.
While there are significant differences among the genomes of human individuals (on the order of 0.1%), these are considerably smaller than the differences between humans and their closest living relatives, the chimpanzees (approximately 4%) and bonobos.
Below is a List human genes by chromosome:
- Chromosome 1 (human)
- Chromosome 2 (human)
- Chromosome 3 (human)
- Chromosome 4 (human)
- Chromosome 5 (human)
- Chromosome 6 (human)
- Chromosome 7 (human)
- Chromosome 8 (human)
- Chromosome 9 (human)
- Chromosome 10 (human)
- Chromosome 11 (human)
- Chromosome 12 (human)
- Chromosome 13 (human)
- Chromosome 14 (human)
- Chromosome 15 (human)
- Chromosome 16 (human)
- Chromosome 17 (human)
- Chromosome 18 (human)
- Chromosome 19 (human)
- Chromosome 20 (human)
- Chromosome 21 (human)
- Chromosome 22 (human)
- Chromosome X (human)
- Chromosome Y (human)
Genetics is the study of genes, genetic variation, and heredity in living organisms. It is generally considered a field of biology, but it intersects frequently with many of the life sciences and is strongly linked with the study of information systems.
The father of genetics is Gregor Mendel, a late 19th-century scientist and Augustinian friar. Mendel studied 'trait inheritance', patterns in the way traits were handed down from parents to offspring. He observed that organisms (pea plants) inherit traits by way of discrete "units of inheritance". This term, still used today, is a somewhat ambiguous definition of what is referred to as a gene.
Trait inheritance and molecular inheritance mechanisms of genes are still primary principles of genetics in the 21st century, but modern genetics has expanded beyond inheritance to studying the function and behavior of genes.
Gene structure and function, variation, and distribution are studied within the context of the cell, the organism (e.g. dominance) and within the context of a population. Genetics has given rise to a number of sub-fields including epigenetics and population genetics.
Organisms studied within the broad field span the domain of life, including bacteria, plants, animals, and humans.
Genetic processes work in combination with an organism's environment and experiences to influence development and behavior, often referred to as nature versus nurture. The intra- or extra-cellular environment of a cell or organism may switch gene transcription on or off. A classic example is two seeds of genetically identical corn, one placed in a temperate climate and one in an arid climate.
While the average height of the two corn stalks may be genetically determined to be equal, the one in the arid climate only grows to half the height of the one in the temperate climate due to lack of water and nutrients in its environment.
For amplification, click on any of the following:
The father of genetics is Gregor Mendel, a late 19th-century scientist and Augustinian friar. Mendel studied 'trait inheritance', patterns in the way traits were handed down from parents to offspring. He observed that organisms (pea plants) inherit traits by way of discrete "units of inheritance". This term, still used today, is a somewhat ambiguous definition of what is referred to as a gene.
Trait inheritance and molecular inheritance mechanisms of genes are still primary principles of genetics in the 21st century, but modern genetics has expanded beyond inheritance to studying the function and behavior of genes.
Gene structure and function, variation, and distribution are studied within the context of the cell, the organism (e.g. dominance) and within the context of a population. Genetics has given rise to a number of sub-fields including epigenetics and population genetics.
Organisms studied within the broad field span the domain of life, including bacteria, plants, animals, and humans.
Genetic processes work in combination with an organism's environment and experiences to influence development and behavior, often referred to as nature versus nurture. The intra- or extra-cellular environment of a cell or organism may switch gene transcription on or off. A classic example is two seeds of genetically identical corn, one placed in a temperate climate and one in an arid climate.
While the average height of the two corn stalks may be genetically determined to be equal, the one in the arid climate only grows to half the height of the one in the temperate climate due to lack of water and nutrients in its environment.
For amplification, click on any of the following:
- The gene
- History
- Features of inheritance
- Molecular basis for inheritance
- Gene expression
- Genetic change
- Society and culture
- See also:
Mental Disorders, including a List of Mental Disorders
YouTube Video: The Truth about Mental Health Disorders
Pictured: Common Mental Disorders for (L) Adults and (R) Children
YouTube Video: The Truth about Mental Health Disorders
Pictured: Common Mental Disorders for (L) Adults and (R) Children
Click here for a List of Mental Disorders.
A mental disorder, also called a mental illness or psychiatric disorder, is a behavioral or mental pattern that may cause suffering or a poor ability to function in life.
Such features may be persistent, relapsing and remitting, or occur as a single episode. Many disorders have been described, with signs and symptoms that vary widely between specific disorders. Such disorders may be diagnosed by a mental health professional.
The causes of mental disorders are often unclear. Theories may incorporate findings from a range of fields. Mental disorders are usually defined by a combination of how a person behaves, feels, perceives, or thinks.
This may be associated with particular regions or functions of the brain, often in a social context. A mental disorder is one aspect of mental health. Cultural and religious beliefs, as well as social norms, should be taken into account when making a diagnosis.
Services are based in psychiatric hospitals or in the community, and assessments are carried out by psychiatrists, psychologists, and clinical social workers, using various methods but often relying on observation and questioning.
Treatments are provided by various mental health professionals. Psychotherapy and psychiatric medication are two major treatment options.
Other treatments include social interventions, peer support, and self-help. In a minority of cases there might be involuntary detention or treatment. Prevention programs have been shown to reduce depression.
Common mental disorders include depression, which affects about 400 million, dementia which affects about 35 million, and schizophrenia, which affects about 21 million people globally.
Stigma and discrimination can add to the suffering and disability associated with mental disorders, leading to various social movements attempting to increase understanding and challenge social exclusion.
The definition and classification of mental disorders are key issues for researchers as well as service providers and those who may be diagnosed. For a mental state to classify as a disorder, it generally needs to cause dysfunction. Most international clinical documents use the term mental "disorder", while "illness" is also common. It has been noted that using the term "mental" (i.e., of the mind) is not necessarily meant to imply separateness from brain or body.
According to DSM-IV, a mental disorder is a psychological syndrome or pattern which is associated with distress (e.g. via a painful symptom), disability (impairment in one or more important areas of functioning), increased risk of death, or causes a significant loss of autonomy; however it excludes normal responses such as grief from loss of a loved one, and also excludes deviant behavior for political, religious, or societal reasons not arising from a dysfunction in the individual.
DSM-IV precedes the definition with caveats, stating that, as in the case with many medical terms, mental disorder "lacks a consistent operational definition that covers all situations", noting that different levels of abstraction can be used for medical definitions, including pathology, symptomology, deviance from a normal range, or etiology, and that the same is true for mental disorders, so that sometimes one type of definition is appropriate, and sometimes another, depending on the situation.
In 2013, the American Psychiatric Association (APA) redefined mental disorders in the DSM-5 as "a syndrome characterized by clinically significant disturbance in an individual's cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning.”
Click on any of the following blue hyperlinks for more about Mental Disorders:
A mental disorder, also called a mental illness or psychiatric disorder, is a behavioral or mental pattern that may cause suffering or a poor ability to function in life.
Such features may be persistent, relapsing and remitting, or occur as a single episode. Many disorders have been described, with signs and symptoms that vary widely between specific disorders. Such disorders may be diagnosed by a mental health professional.
The causes of mental disorders are often unclear. Theories may incorporate findings from a range of fields. Mental disorders are usually defined by a combination of how a person behaves, feels, perceives, or thinks.
This may be associated with particular regions or functions of the brain, often in a social context. A mental disorder is one aspect of mental health. Cultural and religious beliefs, as well as social norms, should be taken into account when making a diagnosis.
Services are based in psychiatric hospitals or in the community, and assessments are carried out by psychiatrists, psychologists, and clinical social workers, using various methods but often relying on observation and questioning.
Treatments are provided by various mental health professionals. Psychotherapy and psychiatric medication are two major treatment options.
Other treatments include social interventions, peer support, and self-help. In a minority of cases there might be involuntary detention or treatment. Prevention programs have been shown to reduce depression.
Common mental disorders include depression, which affects about 400 million, dementia which affects about 35 million, and schizophrenia, which affects about 21 million people globally.
Stigma and discrimination can add to the suffering and disability associated with mental disorders, leading to various social movements attempting to increase understanding and challenge social exclusion.
The definition and classification of mental disorders are key issues for researchers as well as service providers and those who may be diagnosed. For a mental state to classify as a disorder, it generally needs to cause dysfunction. Most international clinical documents use the term mental "disorder", while "illness" is also common. It has been noted that using the term "mental" (i.e., of the mind) is not necessarily meant to imply separateness from brain or body.
According to DSM-IV, a mental disorder is a psychological syndrome or pattern which is associated with distress (e.g. via a painful symptom), disability (impairment in one or more important areas of functioning), increased risk of death, or causes a significant loss of autonomy; however it excludes normal responses such as grief from loss of a loved one, and also excludes deviant behavior for political, religious, or societal reasons not arising from a dysfunction in the individual.
DSM-IV precedes the definition with caveats, stating that, as in the case with many medical terms, mental disorder "lacks a consistent operational definition that covers all situations", noting that different levels of abstraction can be used for medical definitions, including pathology, symptomology, deviance from a normal range, or etiology, and that the same is true for mental disorders, so that sometimes one type of definition is appropriate, and sometimes another, depending on the situation.
In 2013, the American Psychiatric Association (APA) redefined mental disorders in the DSM-5 as "a syndrome characterized by clinically significant disturbance in an individual's cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning.”
Click on any of the following blue hyperlinks for more about Mental Disorders:
- Classifications
- Disorders
- Signs and symptoms
- Causes
- Drugs
Genetics
Models
- Drugs
- Diagnosis
- Prevention
- Depression
Anxiety
Psychosis
Mental health strategies
Prevention programmes
Targeted vs universal
- Depression
- Management
- Psychotherapy
Medication
Other
- Psychotherapy
- Epidemiology
- History
- Ancient civilizations
Europe
Europe and the U.S.
- Ancient civilizations
- Society and culture
- Religion
Movements
Cultural bias
Laws and policies
Perception and discrimination
- Religion
- Mental health
- See also:
- Erving Goffman
- Mental illness portrayed in media
- Mental illness in American prisons
- National Institute of Mental Health
- Psychological evaluation
- Parity of esteem
- NIMH.NIH.gov – National Institute of Mental Health
- International Committee of Women Leaders on Mental Health
- Psychology Dictionary
- Metapsychology Online Reviews: Mental Health
- The New York Times: Mental Health & Disorders
- The Guardian: Mental Health
- Perring, Christian (22 February 2010). "Mental Illness". Stanford Encyclopedia of Philosophy.
- "Insane, Statistics of". Encyclopedia Americana. 1920.
- Adverse Childhood Experiences: Risk Factors for Substance Misuse and Mental Health Dr. Robert Anda of the U.S. Centers for Disease Control describes the relation between childhood adversity and mental health (video)
Cancer, including a List of Different Cancers as well as Treatment Options
YouTube Video: Cancer treatment drug heading for US approval (by CNN 7-13-17)
Pictured: (L) Symptoms of cancer metastasis depend on the location of the tumor. (Courtesy of Mikael Häggström); (R) The incidence of lung cancer is highly correlated with smoking. (Courtesy of Sakurambo - Vectorized version of Image:Cancer smoking lung cancer correlation from NIH.png, originally published on the nih.gov)
YouTube Video: Cancer treatment drug heading for US approval (by CNN 7-13-17)
Pictured: (L) Symptoms of cancer metastasis depend on the location of the tumor. (Courtesy of Mikael Häggström); (R) The incidence of lung cancer is highly correlated with smoking. (Courtesy of Sakurambo - Vectorized version of Image:Cancer smoking lung cancer correlation from NIH.png, originally published on the nih.gov)
Click here for a List of Different forms of Cancer.
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. Not all tumors are cancerous; benign tumors do not spread to other parts of the body.
Possible signs and symptoms include a lump, abnormal bleeding, prolonged cough, unexplained weight loss, and a change in bowel movements. While these symptoms may indicate cancer, they may have other causes. Over 100 types of cancers affect humans.
Tobacco use is the cause of about 22% of cancer deaths. Another 10% is due to obesity, poor diet, lack of physical activity, and excessive drinking of alcohol.
Other factors include certain infections, exposure to ionizing radiation and environmental pollutants.
In the developing world nearly 20% of cancers are due to infections such as hepatitis B, hepatitis C and human papillomavirus infection. These factors act, at least partly, by changing the genes of a cell.
Typically many genetic changes are required before cancer develops. Approximately 5–10% of cancers are due to inherited genetic defects from a person's parents. Cancer can be detected by certain signs and symptoms or screening tests. It is then typically further investigated by medical imaging and confirmed by biopsy.
Many cancers can be prevented by not smoking, maintaining a healthy weight, not drinking too much alcohol, eating plenty of vegetables, fruits and whole grains, vaccination against certain infectious diseases, not eating too much processed and red meat, and avoiding too much sunlight exposure.
Early detection through screening is useful for cervical and colorectal cancer. The benefits of screening in breast cancer are controversial. Cancer is often treated with some combination of radiation therapy, surgery, chemotherapy, and targeted therapy.
Pain and symptom management are an important part of care. Palliative care is particularly important in people with advanced disease.
The chance of survival depends on the type of cancer and extent of disease at the start of treatment. In children under 15 at diagnosis the five-year survival rate in the developed world is on average 80%. For cancer in the United States the average five-year survival rate is 66%.
In 2015 about 90.5 million people had cancer. About 14.1 million new cases occur a year (not including skin cancer other than melanoma). It caused about 8.8 million deaths (15.7%) of human deaths.
The most common types of cancer in males are lung cancer, prostate cancer, colorectal cancer and stomach cancer.
In females, the most common types are breast cancer, colorectal cancer, lung cancer and cervical cancer.
If skin cancer other than melanoma were included in total new cancers each year it would account for around 40% of cases.
In children, acute lymphoblastic leukemia and brain tumors are most common except in Africa where non-Hodgkin lymphoma occurs more often. In 2012, about 165,000 children under 15 years of age were diagnosed with cancer.
The risk of cancer increases significantly with age and many cancers occur more commonly in developed countries. Rates are increasing as more people live to an old age and as lifestyle changes occur in the developing world. The financial costs of cancer were estimated at $1.16 trillion USD per year as of 2010.
Cancers are a large family of diseases that involve abnormal cell growth with the potential to invade or spread to other parts of the body. They form a subset of neoplasms. A neoplasm or tumor is a group of cells that have undergone unregulated growth and will often form a mass or lump, but may be distributed diffusely.
All tumor cells show the six hallmarks of cancer. These characteristics are required to produce a malignant tumor. They include:
Signs and Symptoms:
Main article: Cancer signs and symptoms
When cancer begins, it produces no symptoms. Signs and symptoms appear as the mass grows or ulcerates. The findings that result depend on the cancer's type and location. Few symptoms are specific. Many frequently occur in individuals who have other conditions.
Cancer is a "great imitator". Thus, it is common for people diagnosed with cancer to have been treated for other diseases, which were hypothesized to be causing their symptoms.
People may become anxious or depressed post-diagnosis. The risk of suicide in people with cancer is approximately double.
Click on any of the following blue hyperlinks for more about Cancer:
Treatment of Cancer:
Cancer can be treated by any of the following methods:
The choice of therapy depends upon the location and grade of the tumor and the stage of the disease, as well as the general state of the patient (performance status). A number of experimental cancer treatments are also under development. Under current estimates, two in five people will have cancer at some point in their lifetime.
Complete removal of the cancer without damage to the rest of the body (that is, achieving cure with near-zero adverse effects) is the ideal goal of treatment and is often the goal in practice.
Sometimes this can be accomplished by surgery, but the propensity of cancers to invade adjacent tissue or to spread to distant sites by microscopic metastasis often limits its effectiveness; and chemotherapy and radiotherapy can have a negative effect on normal cells.
Therefore, cure with nonnegligible adverse effects may be accepted as a practical goal in some cases; and besides curative intent, practical goals of therapy can also include (1) suppressing the cancer to a subclinical state and maintaining that state for years of good quality of life (that is, treating the cancer as a chronic disease), and (2) palliative care without curative intent (for advanced-stage metastatic cancers).
Because "cancer" refers to a class of diseases, it is unlikely that there will ever be a single "cure for cancer" any more than there will be a single treatment for all infectious diseases.
Angiogenesis inhibitors were once thought to have potential as a "silver bullet" treatment applicable to many types of cancer, but this has not been the case in practice.
Click on any of the following blue hyperlinks for more about Treatment of Cancer:
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. Not all tumors are cancerous; benign tumors do not spread to other parts of the body.
Possible signs and symptoms include a lump, abnormal bleeding, prolonged cough, unexplained weight loss, and a change in bowel movements. While these symptoms may indicate cancer, they may have other causes. Over 100 types of cancers affect humans.
Tobacco use is the cause of about 22% of cancer deaths. Another 10% is due to obesity, poor diet, lack of physical activity, and excessive drinking of alcohol.
Other factors include certain infections, exposure to ionizing radiation and environmental pollutants.
In the developing world nearly 20% of cancers are due to infections such as hepatitis B, hepatitis C and human papillomavirus infection. These factors act, at least partly, by changing the genes of a cell.
Typically many genetic changes are required before cancer develops. Approximately 5–10% of cancers are due to inherited genetic defects from a person's parents. Cancer can be detected by certain signs and symptoms or screening tests. It is then typically further investigated by medical imaging and confirmed by biopsy.
Many cancers can be prevented by not smoking, maintaining a healthy weight, not drinking too much alcohol, eating plenty of vegetables, fruits and whole grains, vaccination against certain infectious diseases, not eating too much processed and red meat, and avoiding too much sunlight exposure.
Early detection through screening is useful for cervical and colorectal cancer. The benefits of screening in breast cancer are controversial. Cancer is often treated with some combination of radiation therapy, surgery, chemotherapy, and targeted therapy.
Pain and symptom management are an important part of care. Palliative care is particularly important in people with advanced disease.
The chance of survival depends on the type of cancer and extent of disease at the start of treatment. In children under 15 at diagnosis the five-year survival rate in the developed world is on average 80%. For cancer in the United States the average five-year survival rate is 66%.
In 2015 about 90.5 million people had cancer. About 14.1 million new cases occur a year (not including skin cancer other than melanoma). It caused about 8.8 million deaths (15.7%) of human deaths.
The most common types of cancer in males are lung cancer, prostate cancer, colorectal cancer and stomach cancer.
In females, the most common types are breast cancer, colorectal cancer, lung cancer and cervical cancer.
If skin cancer other than melanoma were included in total new cancers each year it would account for around 40% of cases.
In children, acute lymphoblastic leukemia and brain tumors are most common except in Africa where non-Hodgkin lymphoma occurs more often. In 2012, about 165,000 children under 15 years of age were diagnosed with cancer.
The risk of cancer increases significantly with age and many cancers occur more commonly in developed countries. Rates are increasing as more people live to an old age and as lifestyle changes occur in the developing world. The financial costs of cancer were estimated at $1.16 trillion USD per year as of 2010.
Cancers are a large family of diseases that involve abnormal cell growth with the potential to invade or spread to other parts of the body. They form a subset of neoplasms. A neoplasm or tumor is a group of cells that have undergone unregulated growth and will often form a mass or lump, but may be distributed diffusely.
All tumor cells show the six hallmarks of cancer. These characteristics are required to produce a malignant tumor. They include:
- Cell growth and division absent the proper signals
- Continuous growth and division even given contrary signals
- Avoidance of programmed cell death
- Limitless number of cell divisions
- Promoting blood vessel construction
- Invasion of tissue and formation of metastases
Signs and Symptoms:
Main article: Cancer signs and symptoms
When cancer begins, it produces no symptoms. Signs and symptoms appear as the mass grows or ulcerates. The findings that result depend on the cancer's type and location. Few symptoms are specific. Many frequently occur in individuals who have other conditions.
Cancer is a "great imitator". Thus, it is common for people diagnosed with cancer to have been treated for other diseases, which were hypothesized to be causing their symptoms.
People may become anxious or depressed post-diagnosis. The risk of suicide in people with cancer is approximately double.
Click on any of the following blue hyperlinks for more about Cancer:
- Local symptoms
- Systemic symptoms
- Metastasis
- Causes
- Pathophysiology
- Diagnosis
- Classification
- Prevention
- Screening
- Management
- Prognosis
- Epidemiology
- History
- Society and culture
- Research
- Pregnancy
Treatment of Cancer:
Cancer can be treated by any of the following methods:
- surgery,
- chemotherapy,
- radiation therapy,
- hormonal therapy,
- targeted therapy (including immunotherapy such as monoclonal antibody therapy)
- and synthetic lethality.
The choice of therapy depends upon the location and grade of the tumor and the stage of the disease, as well as the general state of the patient (performance status). A number of experimental cancer treatments are also under development. Under current estimates, two in five people will have cancer at some point in their lifetime.
Complete removal of the cancer without damage to the rest of the body (that is, achieving cure with near-zero adverse effects) is the ideal goal of treatment and is often the goal in practice.
Sometimes this can be accomplished by surgery, but the propensity of cancers to invade adjacent tissue or to spread to distant sites by microscopic metastasis often limits its effectiveness; and chemotherapy and radiotherapy can have a negative effect on normal cells.
Therefore, cure with nonnegligible adverse effects may be accepted as a practical goal in some cases; and besides curative intent, practical goals of therapy can also include (1) suppressing the cancer to a subclinical state and maintaining that state for years of good quality of life (that is, treating the cancer as a chronic disease), and (2) palliative care without curative intent (for advanced-stage metastatic cancers).
Because "cancer" refers to a class of diseases, it is unlikely that there will ever be a single "cure for cancer" any more than there will be a single treatment for all infectious diseases.
Angiogenesis inhibitors were once thought to have potential as a "silver bullet" treatment applicable to many types of cancer, but this has not been the case in practice.
Click on any of the following blue hyperlinks for more about Treatment of Cancer:
- Types of treatments
- Symptom control and palliative care
- Research
- Complementary and alternative
- Special circumstances
- See also:
Eating Disorders including Types of Eating Disorders and Any Impact on Development
YouTube Video: A First-Person Account of Binge Eating Disorder
by WebMD
Pictured: Comparison of Anoxeria and Bulimia Treatments
YouTube Video: A First-Person Account of Binge Eating Disorder
by WebMD
Pictured: Comparison of Anoxeria and Bulimia Treatments
Click here for a List of Eating Disorders.
An eating disorder is a mental disorder defined by abnormal eating habits that negatively affect a person's physical or mental health. They include:
Anxiety disorders, depression, and substance abuse are common among people with eating disorders. These disorders do not include obesity.
The cause of eating disorders is not clear. Both biological and environmental factors appear to play a role. Cultural idealization of thinness is believed to contribute. Eating disorders affect about 12 percent of dancers.Those who have experienced sexual abuse are also more likely to develop eating disorders. Some disorders such as pica and rumination disorder occur more often in people with intellectual disabilities. Only one eating disorder can be diagnosed at a given time.
Treatment can be effective for many eating disorders. This typically involves counselling, a proper diet, a normal amount of exercise, and the reduction of efforts to eliminate food.
Hospitalization is occasionally needed. Medications may be used to help with some of the associated symptoms. At five years about 70% of people with anorexia and 50% of people with bulimia recover. Recovery from binge eating disorder is less clear and estimated at 20% to 60%. Both anorexia and bulimia increase the risk of death.
In the developed world binge eating disorder affects about 1.6% of women and 0.8% of men in a given year. Anorexia affects about 0.4% and bulimia affects about 1.3% of young women in a given year.
During the entire life up to 4% of women have anorexia, 2% have bulimia, and 2% have binge eating disorder. Anorexia and bulimia occur nearly ten times more often in females than males. Typically they begin in late childhood or early adulthood. Rates of other eating disorders are not clear. Rates of eating disorders appear to be lower in less developed countries.
Click on any of the following blue hyperlinks for more about Eating Disorders:
Eating disorders and development:
Eating disorders typically peak at specific periods in development, notably sensitive and transitional periods such as puberty.
Feeding and eating disorders in childhood are often the result of a complex interplay of organic and non-organic factors. Medical conditions, developmental problems and temperament are all strongly correlated with feeding disorders, but important contextual features of the environment and parental behavior have also been found to influence the development of childhood eating disorders. Given the complexity of early childhood eating problems, consideration of both biological and behavioral factors is warranted for diagnosis and treatment.
Revisions in the DSM-5 (see next topic) have attempted to improve diagnostic utility for clinicians working with feeding and eating disorder patients. In the DSM-5, diagnostic categories are less defined by age of patient, and guided more by developmental differences in presentation and expression of eating problems.
Click on any of the following blue hyperlinks for more about Eating Disorders & Development:
An eating disorder is a mental disorder defined by abnormal eating habits that negatively affect a person's physical or mental health. They include:
- binge eating disorder where people eat a large amount in a short period of time,
- anorexia nervosa where people eat very little and thus have a low body weight,
- bulimia nervosa where people eat a lot and then try to rid themselves of the food,
- pica where people eat non-food items,
- rumination disorder where people regurgitate food,
- avoidant/restrictive food intake disorder where people have a lack of interest in food,
- and a group of other specified feeding or eating disorders.
Anxiety disorders, depression, and substance abuse are common among people with eating disorders. These disorders do not include obesity.
The cause of eating disorders is not clear. Both biological and environmental factors appear to play a role. Cultural idealization of thinness is believed to contribute. Eating disorders affect about 12 percent of dancers.Those who have experienced sexual abuse are also more likely to develop eating disorders. Some disorders such as pica and rumination disorder occur more often in people with intellectual disabilities. Only one eating disorder can be diagnosed at a given time.
Treatment can be effective for many eating disorders. This typically involves counselling, a proper diet, a normal amount of exercise, and the reduction of efforts to eliminate food.
Hospitalization is occasionally needed. Medications may be used to help with some of the associated symptoms. At five years about 70% of people with anorexia and 50% of people with bulimia recover. Recovery from binge eating disorder is less clear and estimated at 20% to 60%. Both anorexia and bulimia increase the risk of death.
In the developed world binge eating disorder affects about 1.6% of women and 0.8% of men in a given year. Anorexia affects about 0.4% and bulimia affects about 1.3% of young women in a given year.
During the entire life up to 4% of women have anorexia, 2% have bulimia, and 2% have binge eating disorder. Anorexia and bulimia occur nearly ten times more often in females than males. Typically they begin in late childhood or early adulthood. Rates of other eating disorders are not clear. Rates of eating disorders appear to be lower in less developed countries.
Click on any of the following blue hyperlinks for more about Eating Disorders:
- Classification
- Signs and symptoms
- Causes
- Mechanisms
- Diagnosis
- Prevention
- Treatment
- Outcomes
- Epidemiology
- Economics
- See also:
Eating disorders and development:
Eating disorders typically peak at specific periods in development, notably sensitive and transitional periods such as puberty.
Feeding and eating disorders in childhood are often the result of a complex interplay of organic and non-organic factors. Medical conditions, developmental problems and temperament are all strongly correlated with feeding disorders, but important contextual features of the environment and parental behavior have also been found to influence the development of childhood eating disorders. Given the complexity of early childhood eating problems, consideration of both biological and behavioral factors is warranted for diagnosis and treatment.
Revisions in the DSM-5 (see next topic) have attempted to improve diagnostic utility for clinicians working with feeding and eating disorder patients. In the DSM-5, diagnostic categories are less defined by age of patient, and guided more by developmental differences in presentation and expression of eating problems.
Click on any of the following blue hyperlinks for more about Eating Disorders & Development:
- Avoidant/Restrictive Intake Disorder (ARFID)
- Pica
- Rumination disorder
- Anorexia nervosa
- Bulimia nervosa
- Binge eating disorder
Human Emotions, including Categories of Emotion
YouTube Video of an Emotional Acting Scene by Marlon Brando in the 1951 Movie "A Streetcar Named Desire" (1951 film)
Pictured Below: Examples of the different type of emotions
YouTube Video of an Emotional Acting Scene by Marlon Brando in the 1951 Movie "A Streetcar Named Desire" (1951 film)
Pictured Below: Examples of the different type of emotions
Click here for a List of Emotions by Category (alphabetical A-Z)
Emotion is any conscious experience characterized by intense mental activity and a high degree of pleasure or displeasure. Scientific discourse has drifted to other meanings and there is no consensus on a definition.
Emotion is often intertwined with mood, temperament, personality, disposition, and motivation. In some theories, cognition is an important aspect of emotion. Those acting primarily on the emotions they are feeling may seem as if they are not thinking, but mental processes are still essential, particularly in the interpretation of events. For example, the realization of our believing that we are in a dangerous situation and the subsequent arousal of our body's nervous system (rapid heartbeat and breathing, sweating, muscle tension) is integral to the experience of our feeling afraid.
Other theories, however, claim that emotion is separate from and can precede cognition.
Emotions are complex. According to some theories, they are states of feeling that result in physical and psychological changes that influence our behavior.The physiology of emotion is closely linked to arousal of the nervous system with various states and strengths of arousal relating, apparently, to particular emotions.
Emotion is also linked to behavioral tendency. Extroverted people are more likely to be social and express their emotions, while introverted people are more likely to be more socially withdrawn and conceal their emotions.
Emotion is often the driving force behind motivation, positive or negative. According to other theories, emotions are not causal forces but simply syndromes of components, which might include motivation, feeling, behavior, and physiological changes, but no one of these components is the emotion. Nor is the emotion an entity that causes these components.
Emotions involve different components, such as subjective experience, cognitive processes, expressive behavior, psychophysiological changes, and instrumental behavior. At one time, academics attempted to identify the emotion with one of the components: William James with a subjective experience, behaviorists with instrumental behavior, psychophysiologists with physiological changes, and so on.
More recently, emotion is said to consist of all the components. The different components of emotion are categorized somewhat differently depending on the academic discipline.
In psychology and philosophy, emotion typically includes a subjective, conscious experience characterized primarily by psychophysiological expressions, biological reactions, and mental states.
A similar multi-componential description of emotion is found in sociology. For example, Peggy Thoits described emotions as involving physiological components, cultural or emotional labels (anger, surprise, etc.), expressive body actions, and the appraisal of situations and contexts.
Research on emotion has increased significantly over the past two decades with many fields contributing including psychology, neuroscience, endocrinology, medicine, history, sociology, and computer science.
The numerous theories that attempt to explain the origin, neurobiology, experience, and function of emotions have only fostered more intense research on this topic. Current areas of research in the concept of emotion include the development of materials that stimulate and elicit emotion. In addition PET scans and fMRI scans help study the affecting processes in the brain.
Emotions can be defined as a positive or negative experience that is associated with a particular pattern of physiological activity. Emotions produce different physiological, behavioral and cognitive changes. The original role of emotions was to motivate adaptive behaviors that in the past would have contributed to the survival of humans. Emotions are responses to significant internal and external events.
Click on any of the following blue hyperlinks for more about Human Emotions:
Emotion is any conscious experience characterized by intense mental activity and a high degree of pleasure or displeasure. Scientific discourse has drifted to other meanings and there is no consensus on a definition.
Emotion is often intertwined with mood, temperament, personality, disposition, and motivation. In some theories, cognition is an important aspect of emotion. Those acting primarily on the emotions they are feeling may seem as if they are not thinking, but mental processes are still essential, particularly in the interpretation of events. For example, the realization of our believing that we are in a dangerous situation and the subsequent arousal of our body's nervous system (rapid heartbeat and breathing, sweating, muscle tension) is integral to the experience of our feeling afraid.
Other theories, however, claim that emotion is separate from and can precede cognition.
Emotions are complex. According to some theories, they are states of feeling that result in physical and psychological changes that influence our behavior.The physiology of emotion is closely linked to arousal of the nervous system with various states and strengths of arousal relating, apparently, to particular emotions.
Emotion is also linked to behavioral tendency. Extroverted people are more likely to be social and express their emotions, while introverted people are more likely to be more socially withdrawn and conceal their emotions.
Emotion is often the driving force behind motivation, positive or negative. According to other theories, emotions are not causal forces but simply syndromes of components, which might include motivation, feeling, behavior, and physiological changes, but no one of these components is the emotion. Nor is the emotion an entity that causes these components.
Emotions involve different components, such as subjective experience, cognitive processes, expressive behavior, psychophysiological changes, and instrumental behavior. At one time, academics attempted to identify the emotion with one of the components: William James with a subjective experience, behaviorists with instrumental behavior, psychophysiologists with physiological changes, and so on.
More recently, emotion is said to consist of all the components. The different components of emotion are categorized somewhat differently depending on the academic discipline.
In psychology and philosophy, emotion typically includes a subjective, conscious experience characterized primarily by psychophysiological expressions, biological reactions, and mental states.
A similar multi-componential description of emotion is found in sociology. For example, Peggy Thoits described emotions as involving physiological components, cultural or emotional labels (anger, surprise, etc.), expressive body actions, and the appraisal of situations and contexts.
Research on emotion has increased significantly over the past two decades with many fields contributing including psychology, neuroscience, endocrinology, medicine, history, sociology, and computer science.
The numerous theories that attempt to explain the origin, neurobiology, experience, and function of emotions have only fostered more intense research on this topic. Current areas of research in the concept of emotion include the development of materials that stimulate and elicit emotion. In addition PET scans and fMRI scans help study the affecting processes in the brain.
Emotions can be defined as a positive or negative experience that is associated with a particular pattern of physiological activity. Emotions produce different physiological, behavioral and cognitive changes. The original role of emotions was to motivate adaptive behaviors that in the past would have contributed to the survival of humans. Emotions are responses to significant internal and external events.
Click on any of the following blue hyperlinks for more about Human Emotions:
- Etymology, definitions, and differentiation
- Components
- Classification
- Basic emotions
Multi-dimensional analysis
- Basic emotions
- Theories
- Ancient Greece, Ancient China, and the Middle Ages
Evolutionary theories
Somatic theories
Cognitive theories
Situated perspective on emotion
- Ancient Greece, Ancient China, and the Middle Ages
- Genetics
- Neurocircuitry
- Prefrontal cortex
Homeostatic/primordial emotion
- Prefrontal cortex
- Disciplinary approaches
- History
Sociology
Psychotherapy and regulation
Cross-cultural research
Computer science
- History
- Notable theorists
- See also:
- Affect measures
- Affective Computing
- Affective forecasting
- Affective neuroscience
- Affective science
- Cannon–Bard theory
- Contrasting and categorization of emotions
- CyberEmotions
- Donald B. Lindsley
- Emoticons
- Emotion classification
- Emotions and culture
- Emotion and memory
- Emotional expression
- Emotional climate
- Emotions in virtual communication
- Empathy
- Endocrinology
- Facial feedback hypothesis
- Facial Action Coding System
- Fear
- Feeling
- Fuzzy-trace theory
- Group emotion
- International Affective Picture System
- James–Lange theory
- List of emotions
- Measuring Emotions
- Neuroendocrinology
- Two-factor theory of emotion
- Sociology of emotions
- Social emotion
- Social neuroscience
- Social sharing of emotions
- Somatic markers hypothesis
- Yerkes–Dodson law
- The Internet Encyclopedia of Philosophy: Theories of Emotion
- The Stanford Encyclopedia of Philosophy: Emotion
Suicides including a List of Suicides by Well-known Individuals
YouTube Video: The Warning Signs of Suicide
Pictured (L-R): Kurt Cobain (suicide by shotgun) and Robin Williams (suicide by hanging)
YouTube Video: The Warning Signs of Suicide
Pictured (L-R): Kurt Cobain (suicide by shotgun) and Robin Williams (suicide by hanging)
Click here for a list of Suicides by well known people.
Suicide is the act of intentionally causing one's own death. Risk factors include mental disorders such as depression, bipolar disorder, schizophrenia, personality disorders, and substance abuse, including alcoholism and use of benzodiazepines.
Other suicides are impulsive acts due to stress such as from financial difficulties, troubles with relationships, or from bullying. Those who have previously attempted suicide are at higher risk for future attempts. Suicide prevention efforts include limiting access to methods of suicide, such as firearms, drugs, and poisons, treating mental disorders and substance misuse, proper media reporting of suicide, and improving economic conditions.
Although crisis hotlines are common, there is little evidence for their effectiveness.
The most commonly used method of suicide varies between countries, and is partly related to the availability of effective means. Common methods include hanging, pesticide poisoning, and firearms. Suicide resulted in 828,000 deaths globally in 2015 (up from 712,000 deaths in 1990). This makes it the 10th leading cause of death worldwide.
Approximately 0.5% to 1.4% of people die by suicide, about 12 per 100,000 persons per year. Three quarters of suicides globally occur in the developing world. Rates of completed suicides are generally higher in men than in women, ranging from 1.5 times as much in the developing world to 3.5 times in the developed world.
Suicide is generally most common among those over the age of 70; however, in certain countries those aged between 15 and 30 are at highest risk. There are an estimated 10 to 20 million non-fatal attempted suicides every year. Non-fatal suicide attempts may lead to injury and long-term disabilities. In the Western world, attempts are more common in young people and females.
Views on suicide have been influenced by broad existential themes such as religion, honor, and the meaning of life. The Abrahamic religions traditionally consider suicide an offense towards God due to the belief in the sanctity of life.
During the samurai era in Japan, a form of suicide known as seppuku (harakiri) was respected as a means of making up for failure or as a form of protest. Sati, a practice outlawed by the British Raj, expected the Indian widow to kill herself on her husband's funeral fire, either willingly or under pressure from the family and society.
Suicide and attempted suicide, while previously illegal, are no longer so in most Western countries. It remains a criminal offense in many countries.
In the 20th and 21st centuries, suicide has been used on rare occasions as a form of protest, and kamikaze and suicide bombings have been used as a military or terrorist tactic.
Click on any of the following blue hyperlinks for more about Suicide:
Suicide is the act of intentionally causing one's own death. Risk factors include mental disorders such as depression, bipolar disorder, schizophrenia, personality disorders, and substance abuse, including alcoholism and use of benzodiazepines.
Other suicides are impulsive acts due to stress such as from financial difficulties, troubles with relationships, or from bullying. Those who have previously attempted suicide are at higher risk for future attempts. Suicide prevention efforts include limiting access to methods of suicide, such as firearms, drugs, and poisons, treating mental disorders and substance misuse, proper media reporting of suicide, and improving economic conditions.
Although crisis hotlines are common, there is little evidence for their effectiveness.
The most commonly used method of suicide varies between countries, and is partly related to the availability of effective means. Common methods include hanging, pesticide poisoning, and firearms. Suicide resulted in 828,000 deaths globally in 2015 (up from 712,000 deaths in 1990). This makes it the 10th leading cause of death worldwide.
Approximately 0.5% to 1.4% of people die by suicide, about 12 per 100,000 persons per year. Three quarters of suicides globally occur in the developing world. Rates of completed suicides are generally higher in men than in women, ranging from 1.5 times as much in the developing world to 3.5 times in the developed world.
Suicide is generally most common among those over the age of 70; however, in certain countries those aged between 15 and 30 are at highest risk. There are an estimated 10 to 20 million non-fatal attempted suicides every year. Non-fatal suicide attempts may lead to injury and long-term disabilities. In the Western world, attempts are more common in young people and females.
Views on suicide have been influenced by broad existential themes such as religion, honor, and the meaning of life. The Abrahamic religions traditionally consider suicide an offense towards God due to the belief in the sanctity of life.
During the samurai era in Japan, a form of suicide known as seppuku (harakiri) was respected as a means of making up for failure or as a form of protest. Sati, a practice outlawed by the British Raj, expected the Indian widow to kill herself on her husband's funeral fire, either willingly or under pressure from the family and society.
Suicide and attempted suicide, while previously illegal, are no longer so in most Western countries. It remains a criminal offense in many countries.
In the 20th and 21st centuries, suicide has been used on rare occasions as a form of protest, and kamikaze and suicide bombings have been used as a military or terrorist tactic.
Click on any of the following blue hyperlinks for more about Suicide:
Metabolism including Aging, Basal Metabolic Rate, and Nutrition*
* -- Article by The National Center for Biotechnology Information (NCBI)
YouTube Video: Losing Weight Over 50 - How To Get Thin Now That Life Has Changed
Pictured: Diagrammatic overview of molecular and cellular changes during skeletal muscle aging. The flowchart summarizes major age-related changes in contractile patterns and muscle metabolism as revealed by proteomic analyses of young adult vs. middle-aged vs. aged human vastus lateralis muscle. (Courtesy of Spandidos Publications)
* -- Article by The National Center for Biotechnology Information (NCBI)
YouTube Video: Losing Weight Over 50 - How To Get Thin Now That Life Has Changed
Pictured: Diagrammatic overview of molecular and cellular changes during skeletal muscle aging. The flowchart summarizes major age-related changes in contractile patterns and muscle metabolism as revealed by proteomic analyses of young adult vs. middle-aged vs. aged human vastus lateralis muscle. (Courtesy of Spandidos Publications)
Article by NCBI: Aging, basal metabolic rate, and nutrition
"Age is one of the most important factor of changes in energy metabolism. The basal metabolic rate decreases almost linearly with age. Skeletal musculature is a fundamental organ that consumes the largest part of energy in the normal human body.
The total volume of skeletal muscle can be estimated by 24-hours creatinine excretion. The volume of skeletal musculature decreases and the percentage of fat tissue increases with age.
It is shown that the decrease in muscle mass relative to total body may be wholly responsible for the age-related decreases in basal metabolic rate. Energy consumption by physical activity also decreases with atrophic changes of skeletal muscle. Thus, energy requirement in the elderly decreases.
With decrease of energy intake, intake of essential nutrients also decreases. If energy intake, on the other hand, exceeds individual energy needs, fat accumulates in the body. Body fat tends to accumulate in the abdomen in the elderly.
Fat tissue in the abdominal cavity is connected directly with the liver through portal vein. Accumulation of abdominal fat causes disturbance in glucose and lipid metabolism. It is shown that glucose tolerance decreases with age.
Although age contributes independently to the deterioration in glucose tolerance, the decrease in glucose tolerance may be partly prevented through changes of life-style variables, energy metabolism is essential for the physiological functions. It may also be possible to delay the aging process of various physiological functions by change of dietary habits, stopping smoking, and physical activity."
[End of Article]
___________________________________________________________________________
Metabolism is the set of life-sustaining chemical transformations within the cells of living organisms.
The three main purposes of metabolism are the conversion of food/fuel to energy to run cellular processes, the conversion of food/fuel to building blocks for proteins, lipids, nucleic acids, and some carbohydrates, and the elimination of nitrogenous wastes.
These enzyme-catalyzed reactions allow organisms to grow and reproduce, maintain their structures, and respond to their environments. The word metabolism can also refer to the sum of all chemical reactions that occur in living organisms, including digestion and the transport of substances into and between different cells, in which case the set of reactions within the cells is called intermediary metabolism or intermediate metabolism.
Metabolism is usually divided into two categories: catabolism, the breaking down of organic matter for example, the breaking down of glucose to pyruvate, by cellular respiration, and anabolism, the building up of components of cells such as proteins and nucleic acids.
Usually, breaking down releases energy and building up consumes energy.
The chemical reactions of metabolism are organized into metabolic pathways, in which one chemical is transformed through a series of steps into another chemical, by a sequence of enzymes.
Enzymes are crucial to metabolism because they allow organisms to drive desirable reactions that require energy that will not occur by themselves, by coupling them to spontaneous reactions that release energy. Enzymes act as catalysts that allow the reactions to proceed more rapidly. Enzymes also allow the regulation of metabolic pathways in response to changes in the cell's environment or to signals from other cells.
The metabolic system of a particular organism determines which substances it will find nutritious and which poisonous. For example, some prokaryotes use hydrogen sulfide as a nutrient, yet this gas is poisonous to animals.The speed of metabolism, the metabolic rate, influences how much food an organism will require, and also affects how it is able to obtain that food.
A striking feature of metabolism is the similarity of the basic metabolic pathways and components between even vastly different species. For example, the set of carboxylic acids that are best known as the intermediates in the citric acid cycle are present in all known organisms, being found in species as diverse as the unicellular bacterium Escherichia coli and huge multi-cellular organisms like elephants. These striking similarities in metabolic pathways are likely due to their early appearance in evolutionary history, and their retention because of their efficacy.
Click on any of the following blue hyperlinks for more about Metabolism:
"Age is one of the most important factor of changes in energy metabolism. The basal metabolic rate decreases almost linearly with age. Skeletal musculature is a fundamental organ that consumes the largest part of energy in the normal human body.
The total volume of skeletal muscle can be estimated by 24-hours creatinine excretion. The volume of skeletal musculature decreases and the percentage of fat tissue increases with age.
It is shown that the decrease in muscle mass relative to total body may be wholly responsible for the age-related decreases in basal metabolic rate. Energy consumption by physical activity also decreases with atrophic changes of skeletal muscle. Thus, energy requirement in the elderly decreases.
With decrease of energy intake, intake of essential nutrients also decreases. If energy intake, on the other hand, exceeds individual energy needs, fat accumulates in the body. Body fat tends to accumulate in the abdomen in the elderly.
Fat tissue in the abdominal cavity is connected directly with the liver through portal vein. Accumulation of abdominal fat causes disturbance in glucose and lipid metabolism. It is shown that glucose tolerance decreases with age.
Although age contributes independently to the deterioration in glucose tolerance, the decrease in glucose tolerance may be partly prevented through changes of life-style variables, energy metabolism is essential for the physiological functions. It may also be possible to delay the aging process of various physiological functions by change of dietary habits, stopping smoking, and physical activity."
[End of Article]
___________________________________________________________________________
Metabolism is the set of life-sustaining chemical transformations within the cells of living organisms.
The three main purposes of metabolism are the conversion of food/fuel to energy to run cellular processes, the conversion of food/fuel to building blocks for proteins, lipids, nucleic acids, and some carbohydrates, and the elimination of nitrogenous wastes.
These enzyme-catalyzed reactions allow organisms to grow and reproduce, maintain their structures, and respond to their environments. The word metabolism can also refer to the sum of all chemical reactions that occur in living organisms, including digestion and the transport of substances into and between different cells, in which case the set of reactions within the cells is called intermediary metabolism or intermediate metabolism.
Metabolism is usually divided into two categories: catabolism, the breaking down of organic matter for example, the breaking down of glucose to pyruvate, by cellular respiration, and anabolism, the building up of components of cells such as proteins and nucleic acids.
Usually, breaking down releases energy and building up consumes energy.
The chemical reactions of metabolism are organized into metabolic pathways, in which one chemical is transformed through a series of steps into another chemical, by a sequence of enzymes.
Enzymes are crucial to metabolism because they allow organisms to drive desirable reactions that require energy that will not occur by themselves, by coupling them to spontaneous reactions that release energy. Enzymes act as catalysts that allow the reactions to proceed more rapidly. Enzymes also allow the regulation of metabolic pathways in response to changes in the cell's environment or to signals from other cells.
The metabolic system of a particular organism determines which substances it will find nutritious and which poisonous. For example, some prokaryotes use hydrogen sulfide as a nutrient, yet this gas is poisonous to animals.The speed of metabolism, the metabolic rate, influences how much food an organism will require, and also affects how it is able to obtain that food.
A striking feature of metabolism is the similarity of the basic metabolic pathways and components between even vastly different species. For example, the set of carboxylic acids that are best known as the intermediates in the citric acid cycle are present in all known organisms, being found in species as diverse as the unicellular bacterium Escherichia coli and huge multi-cellular organisms like elephants. These striking similarities in metabolic pathways are likely due to their early appearance in evolutionary history, and their retention because of their efficacy.
Click on any of the following blue hyperlinks for more about Metabolism:
- Key biochemicals
- Amino acids and proteins
Lipids
Carbohydrates
Nucleotides
Coenzymes
Minerals and cofactors
- Amino acids and proteins
- Catabolism
- Digestion
Energy from organic compounds
- Digestion
- Energy transformations
- Oxidative phosphorylation
Energy from inorganic compounds
Energy from light
- Oxidative phosphorylation
- Anabolism
- Carbon fixation
Carbohydrates and glycans
Fatty acids, isoprenoids and steroids
Proteins
Nucleotide synthesis and salvage
- Carbon fixation
- Xenobiotics and redox metabolism
- Thermodynamics of living organisms
- Regulation and control
- Evolution
- Investigation and manipulation
- History
- See also:
- Anthropogenic metabolism
- Antimetabolite
- Basal metabolic rate
- Calorimetry
- Isothermal microcalorimetry
- Inborn error of metabolism
- Iron-sulfur world theory, a "metabolism first" theory of the origin of life
- Metabolic disorder
- Primary nutritional groups
- Respirometry
- Stream metabolism
- Sulfur metabolism
- Thermic effect of food
- Urban metabolism
- Water metabolism
- General information
- Sparknotes SAT biochemistry Overview of biochemistry. School level.
- MIT Biology Hypertextbook Undergraduate-level guide to molecular biology.
- Human metabolism
- Topics in Medical Biochemistry Guide to human metabolic pathways. School level.
- THE Medical Biochemistry Page Comprehensive resource on human metabolism.
- Databases
- Metabolic pathways
- Metabolism reference Pathway
- The Nitrogen cycle and Nitrogen fixation at the Wayback Machine (archive index)
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)
YouTube Video: What DSM-5 Means for Diagnosing Mental Health Patients by PBS Hour
Pictured: Book cover of DSM-5, Copyright owned by the American Psychiatric Association
YouTube Video: What DSM-5 Means for Diagnosing Mental Health Patients by PBS Hour
Pictured: Book cover of DSM-5, Copyright owned by the American Psychiatric Association
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) is the 2013 update to the American Psychiatric Association's (APA) classification and diagnostic tool. In the United States the DSM serves as a universal authority for psychiatric diagnoses. Treatment recommendations, as well as payment by health care providers, are often determined by DSM classifications, so the appearance of a new version has significant practical importance.
The DSM-5 was published on May 18, 2013, superseding the DSM-IV-TR, which was published in 2000. The development of the new edition began with a conference in 1999, and proceeded with the formation of a Task Force in 2007, which developed and field-tested a variety of new classifications.
In most respects DSM-5 is not greatly changed from DSM-IV-TR. Notable changes include the following:
In addition, the DSM-5 is the first "living document" version of a DSM.
Various authorities criticized the fifth edition both before and after it was formally published.
Critics assert, for example, that many DSM-5 revisions or additions lack empirical support; inter-rater reliability is low for many disorders; several sections contain poorly written, confusing, or contradictory information; and the psychiatric drug industry unduly influenced the manual's content.
Many of the members of work groups for the DSM-5 had conflicting interests, including ties to pharmaceutical companies.
Various scientists have argued that the DSM-5 forces clinicians to make distinctions that are not supported by solid evidence, distinctions that have major treatment implications, including drug prescriptions and the availability of health insurance coverage.
General criticism of the DSM-5 ultimately resulted in a petition, signed by many mental health organizations, which called for outside review of DSM-5.
Click here for more about The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
The DSM-5 was published on May 18, 2013, superseding the DSM-IV-TR, which was published in 2000. The development of the new edition began with a conference in 1999, and proceeded with the formation of a Task Force in 2007, which developed and field-tested a variety of new classifications.
In most respects DSM-5 is not greatly changed from DSM-IV-TR. Notable changes include the following:
- dropping Asperger syndrome as a distinct classification;
- loss of subtype classifications for variant forms of schizophrenia;
- dropping the "bereavement exclusion" for depressive disorders;
- a revised treatment and naming of gender identity disorder to gender dysphoria,
- and removing the A2 criterion for posttraumatic stress disorder (PTSD) because its requirement for specific emotional reactions to trauma did not apply to combat veterans and first responders with PTSD.
In addition, the DSM-5 is the first "living document" version of a DSM.
Various authorities criticized the fifth edition both before and after it was formally published.
Critics assert, for example, that many DSM-5 revisions or additions lack empirical support; inter-rater reliability is low for many disorders; several sections contain poorly written, confusing, or contradictory information; and the psychiatric drug industry unduly influenced the manual's content.
Many of the members of work groups for the DSM-5 had conflicting interests, including ties to pharmaceutical companies.
Various scientists have argued that the DSM-5 forces clinicians to make distinctions that are not supported by solid evidence, distinctions that have major treatment implications, including drug prescriptions and the availability of health insurance coverage.
General criticism of the DSM-5 ultimately resulted in a petition, signed by many mental health organizations, which called for outside review of DSM-5.
Click here for more about The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
Diabetes
- YouTube Video: The Myth about Blood Sugars and Diabetes
- YouTube Video: How to Reverse Type 2 Diabetes
- YouTube Video: Symptoms and Signs of Diabetes
Diabetes mellitus (DM), commonly referred to as diabetes, is a group of metabolic disorders in which there are high blood sugar levels over a prolonged period. Symptoms of high blood sugar include frequent urination, increased thirst, and increased hunger. If left untreated, diabetes can cause many complications.
Acute complications can include diabetic ketoacidosis, hyperosmolar hyperglycemic state, or death. Serious long-term complications include cardiovascular disease, stroke, chronic kidney disease, foot ulcers, and damage to the eyes.
Diabetes is due to either the pancreas not producing enough insulin or the cells of the body not responding properly to the insulin produced.
There are three main types of diabetes mellitus:
Prevention and treatment involve maintaining a healthy diet, regular physical exercise, a normal body weight, and avoiding use of tobacco. Control of blood pressure and maintaining proper foot care are important for people with the disease. Type 1 DM must be managed with insulin injections. Type 2 DM may be treated with medications with or without insulin. Insulin and some oral medications can cause low blood sugar. Weight loss surgery in those with obesity is sometimes an effective measure in those with type 2 DM.
Gestational diabetes usually resolves after the birth of the baby.
As of 2015, an estimated 415 million people had diabetes worldwide, with type 2 DM making up about 90% of the cases. This represents 8.3% of the adult population, with equal rates in both women and men.
As of 2014, trends suggested the rate would continue to rise. Diabetes at least doubles a person's risk of early death. From 2012 to 2015, approximately 1.5 to 5.0 million deaths each year resulted from diabetes. The global economic cost of diabetes in 2014 was estimated to be US$612 billion. In the United States, diabetes cost $245 billion in 2012.
Click on any of the following blue hyperlinks for more about Diabetes:
Acute complications can include diabetic ketoacidosis, hyperosmolar hyperglycemic state, or death. Serious long-term complications include cardiovascular disease, stroke, chronic kidney disease, foot ulcers, and damage to the eyes.
Diabetes is due to either the pancreas not producing enough insulin or the cells of the body not responding properly to the insulin produced.
There are three main types of diabetes mellitus:
- Type 1 DM results from the pancreas's failure to produce enough insulin. This form was previously referred to as "insulin-dependent diabetes mellitus" (IDDM) or "juvenile diabetes". The cause is unknown.
- Type 2 DM begins with insulin resistance, a condition in which cells fail to respond to insulin properly. As the disease progresses a lack of insulin may also develop. This form was previously referred to as "non insulin-dependent diabetes mellitus" (NIDDM) or "adult-onset diabetes". The most common cause is excessive body weight and not enough exercise.
- Gestational diabetes is the third main form and occurs when pregnant women without a previous history of diabetes develop high blood sugar levels.
Prevention and treatment involve maintaining a healthy diet, regular physical exercise, a normal body weight, and avoiding use of tobacco. Control of blood pressure and maintaining proper foot care are important for people with the disease. Type 1 DM must be managed with insulin injections. Type 2 DM may be treated with medications with or without insulin. Insulin and some oral medications can cause low blood sugar. Weight loss surgery in those with obesity is sometimes an effective measure in those with type 2 DM.
Gestational diabetes usually resolves after the birth of the baby.
As of 2015, an estimated 415 million people had diabetes worldwide, with type 2 DM making up about 90% of the cases. This represents 8.3% of the adult population, with equal rates in both women and men.
As of 2014, trends suggested the rate would continue to rise. Diabetes at least doubles a person's risk of early death. From 2012 to 2015, approximately 1.5 to 5.0 million deaths each year resulted from diabetes. The global economic cost of diabetes in 2014 was estimated to be US$612 billion. In the United States, diabetes cost $245 billion in 2012.
Click on any of the following blue hyperlinks for more about Diabetes:
- Signs and symptoms
- Causes
- Pathophysiology
- Diagnosis
- Prevention
- Management
- Epidemiology
- History
- Society and culture
- Research
- See Also:
Infectious Diseases including a List of Infectious Diseases
- YouTube Video: What You Need To Know About Infectious Disease
- YouTube Video: How Pandemics Spread (TedEd)
- Left: Culex mosquitos (Culex quinquefasciatus shown) are biological vectors that transmit West Nile Virus;
- Right: About Meningitis
Infection is the invasion of an organism's body tissues by disease-causing agents, their multiplication, and the reaction of host tissues to these organisms and the toxins they produce. Infectious disease, also known as transmissible disease or communicable disease, is illness resulting from an infection.
Infections are caused by:
Hosts can fight infections using their immune system. Mammalian hosts react to infections with an innate response, often involving inflammation, followed by an adaptive response.
Specific medications used to treat infections include antibiotics, antivirals, antifungals, antiprotozoals, and antihelminthics.
Infectious diseases resulted in 9.2 million deaths in 2013 (about 17% of all deaths). The branch of medicine that focuses on infections is referred to as infectious disease.
Click on any of the following blue hyperlinks for more about Infections:
Click here for an alphabetical List of Infectious Diseases.
A disease is a particular abnormal condition that affects part or all of an organism and that consists of a disorder of a structure or function. The study of disease is called pathology, which includes the study of cause.
Disease is often construed as a medical condition associated with specific symptoms and signs. It may be caused by external factors such as pathogens or by internal dysfunctions, particularly of the immune system, such as an immunodeficiency, or by a hypersensitivity, including allergies and autoimmunity.
When caused by pathogens (e.g. malaria by Plasmodium ssp.), the term disease is often misleadingly used even in the scientific literature in place of its causal agent, the pathogen.
This language habit can cause confusion in the communication of the cause-effect principle in epidemiology, and as such it should be strongly discouraged.
In humans, disease is often used more broadly to refer to any condition that causes pain, dysfunction, distress, social problems, or death to the person afflicted, or similar problems for those in contact with the person.
In this broader sense, it sometimes includes injuries, disabilities, disorders, syndromes, infections, isolated symptoms, deviant behaviors, and atypical variations of structure and function, while in other contexts and for other purposes these may be considered distinguishable categories.
Diseases can affect people not only physically, but also emotionally, as contracting and living with a disease can alter the affected person's perspective on life.
Death due to disease is called death by natural causes.
There are four main types of disease:
Diseases can also be classified as communicable and non-communicable. The deadliest diseases in humans are coronary artery disease (blood flow obstruction), followed by cerebrovascular disease and lower respiratory infections.
Click on any of the following blue hyperlinks for more about Diseases impacting Humans:
Infections are caused by:
- infectious agents including
- nematodes such as
- parasitic roundworms and pinworms,
- arthropods such as
- fungi such as ringworm,
- and other macroparasites such as tapeworms and other helminths.
Hosts can fight infections using their immune system. Mammalian hosts react to infections with an innate response, often involving inflammation, followed by an adaptive response.
Specific medications used to treat infections include antibiotics, antivirals, antifungals, antiprotozoals, and antihelminthics.
Infectious diseases resulted in 9.2 million deaths in 2013 (about 17% of all deaths). The branch of medicine that focuses on infections is referred to as infectious disease.
Click on any of the following blue hyperlinks for more about Infections:
- Classification
- Signs and symptoms
- Pathophysiology
- Diagnosis
- Prevention
- Treatments
- Epidemiology
- History
- Society and culture
- Fossil record
- See also:
- infectious disease (medical specialty)
- Host-pathogen interface
- Bioinformatics Resource Centers for Infectious Diseases
- Biological contamination
- Blood-borne disease
- Coinfection
- Copenhagen Consensus
- Cordon sanitaire
- Disease diffusion mapping
- Foodborne illness
- Globalization and disease
- Human microbiome project
- Infection control
- Infectious disease dynamics
- Isolation (health care)
- Membrane vesicle trafficking
- Infectious disease eradication
- Infectious disease in the 20th century
- List of causes of death by rate
- List of diseases caused by insects
- List of epidemics
- List of bacterial vaginosis microbiota
- Multiplicity of infection
- Neglected tropical diseases
- Nosocomial infection
- Quarantine
- Spatiotemporal Epidemiological Modeler (STEM)
- Social distancing
- Spillover infection
- Threshold host density
- Transmission (medicine)
- Tropical disease
- Ubi pus, ibi evacua (Latin: "where there is pus, there evacuate it")
- Vaccine-preventable diseases
- Waterborne diseases
- European Center for Disease Prevention and Control
- U.S. Centers for Disease Control and Prevention,
- Infectious Disease Society of America (IDSA)
- Infectious Disease Index of the Public Health Agency of Canada (PHAC)
- Infection Information Resource
- Microbes & Infection (Journal)
- Table: Global deaths from communicable diseases, 2010 - Canadian Broadcasting Corp.
Click here for an alphabetical List of Infectious Diseases.
A disease is a particular abnormal condition that affects part or all of an organism and that consists of a disorder of a structure or function. The study of disease is called pathology, which includes the study of cause.
Disease is often construed as a medical condition associated with specific symptoms and signs. It may be caused by external factors such as pathogens or by internal dysfunctions, particularly of the immune system, such as an immunodeficiency, or by a hypersensitivity, including allergies and autoimmunity.
When caused by pathogens (e.g. malaria by Plasmodium ssp.), the term disease is often misleadingly used even in the scientific literature in place of its causal agent, the pathogen.
This language habit can cause confusion in the communication of the cause-effect principle in epidemiology, and as such it should be strongly discouraged.
In humans, disease is often used more broadly to refer to any condition that causes pain, dysfunction, distress, social problems, or death to the person afflicted, or similar problems for those in contact with the person.
In this broader sense, it sometimes includes injuries, disabilities, disorders, syndromes, infections, isolated symptoms, deviant behaviors, and atypical variations of structure and function, while in other contexts and for other purposes these may be considered distinguishable categories.
Diseases can affect people not only physically, but also emotionally, as contracting and living with a disease can alter the affected person's perspective on life.
Death due to disease is called death by natural causes.
There are four main types of disease:
- infectious diseases,
- deficiency diseases,
- genetic diseases (both hereditary and non-hereditary),
- and physiological diseases.
Diseases can also be classified as communicable and non-communicable. The deadliest diseases in humans are coronary artery disease (blood flow obstruction), followed by cerebrovascular disease and lower respiratory infections.
Click on any of the following blue hyperlinks for more about Diseases impacting Humans:
- Terminology
- Concepts
- Types by body system
- Stages
- Extent
- Classifications
- Causes including Types of causes
- Prevention
- Treatments
- Epidemiology
- Society and culture
- See also:
- Cryptogenic disease, a disease whose cause is currently unknown
- Developmental disability, severe, lifelong disabilities attributable to mental or physical impairments
- Environmental disease
- Host-pathogen interface
- List of incurable diseases
- Mitochondrial disease
- Plant pathology
- Rare disease, a disease that affects very few people
- Sociology of health and illness
- Health Topics, MedlinePlus descriptions of most diseases, with access to current research articles.
- OMIM Comprehensive information on genes that cause disease at Online Mendelian Inheritance in Man
- CTD The Comparative Toxicogenomics Database is a scientific resource connecting chemicals, genes, and human diseases.
- NLM Comprehensive database from the US National Library of Medicine
- Health Topics A-Z, fact sheets about many common diseases at Centers for Disease Control
- The Merck Manual containing detailed description of most diseases
- Report: The global burden of disease from World Health Organization (WHO), 2004
- Free online health-risk assessment by Your Disease Risk at Washington University in St Louis
Congenital Disorders ("Birth Defects"), including a List of Congenital Disorders.
Click here for a List of Congenital Disorders.
A congenital disorder, also known as birth defect, is a condition existing at or before birth regardless of cause. Of these disorders, those characterized by structural deformities are termed "congenital anomalies" and involve defects in a developing fetus.
Birth defects vary widely in cause and symptoms. Any substance that causes birth defects is known as a teratogen. Some disorders can be detected before birth through prenatal diagnosis (prophecy).
Birth defects may be the result of genetic or environmental factors. This includes errors of morphogenesis, infection, epigenetic modifications on a parental germline, or a chromosomal abnormality.
The outcome of the disorder will depend on complex interactions between the pre-natal deficit and the post-natal environment.
Animal studies indicate that the mother's (and likely the father's) diet, vitamin intake, and glucose levels prior to ovulation and conception have long-term effects on fetal growth and adolescent and adult disease.
Animal studies have shown that paternal exposures prior to conception and during pregnancy result in increased risk of certain birth defects and cancers. This research suggests that paternal food deprivation, germ line mutations, alcohol use, chemical mutagens, age, smoking habits and epigenetic alterations can affect birth outcomes.
However, the relationship between offspring health and paternal exposures, age, and lifestyle are still relatively weak. This is likely because paternal exposures and their effects on the fetus are studied far less extensively than maternal exposures.
Birth defects are present in about 3% of newborns in USA. Congenital anomalies resulted in about 632,000 deaths per year in 2013 down from 751,000 in 1990.
The type with the greatest numbers of deaths are congenital heart disease (323,000), followed by neural tube defects (69,000)
Click on any of the following blue hyperlinks for more about Congenital Disorders:
A congenital disorder, also known as birth defect, is a condition existing at or before birth regardless of cause. Of these disorders, those characterized by structural deformities are termed "congenital anomalies" and involve defects in a developing fetus.
Birth defects vary widely in cause and symptoms. Any substance that causes birth defects is known as a teratogen. Some disorders can be detected before birth through prenatal diagnosis (prophecy).
Birth defects may be the result of genetic or environmental factors. This includes errors of morphogenesis, infection, epigenetic modifications on a parental germline, or a chromosomal abnormality.
The outcome of the disorder will depend on complex interactions between the pre-natal deficit and the post-natal environment.
Animal studies indicate that the mother's (and likely the father's) diet, vitamin intake, and glucose levels prior to ovulation and conception have long-term effects on fetal growth and adolescent and adult disease.
Animal studies have shown that paternal exposures prior to conception and during pregnancy result in increased risk of certain birth defects and cancers. This research suggests that paternal food deprivation, germ line mutations, alcohol use, chemical mutagens, age, smoking habits and epigenetic alterations can affect birth outcomes.
However, the relationship between offspring health and paternal exposures, age, and lifestyle are still relatively weak. This is likely because paternal exposures and their effects on the fetus are studied far less extensively than maternal exposures.
Birth defects are present in about 3% of newborns in USA. Congenital anomalies resulted in about 632,000 deaths per year in 2013 down from 751,000 in 1990.
The type with the greatest numbers of deaths are congenital heart disease (323,000), followed by neural tube defects (69,000)
Click on any of the following blue hyperlinks for more about Congenital Disorders:
- Classification
- Primarily structural
Primarily metabolic
Other
- Primarily structural
- Causes
- Epidemiology
- United States
- See also:
- Malformative syndrome
- ICD-10 Chapter Q: Congenital malformations, deformations and chromosomal abnormalities
- Idiopathic
- List of ICD-9 codes 740-759: Congenital anomalies
- March of Dimes
- Mitochondrial disease
- Supernumerary body part
- CDC’s National Center on Birth Defects and Developmental Disabilities
- Birth Defect Research for Children
Genetic Disorders, including a List of Genetic Disorders
Click here for a List of Genetic Disorders.
A genetic disorder is a genetic problem caused by one or more abnormalities in the genome, especially a condition that is present from birth (congenital).
Most genetic disorders are quite rare and affect one person in every several thousands or millions.
Genetic disorders may be hereditary, passed down from the parents' genes. In other genetic disorders, defects may be caused by new mutations or changes to the DNA. In such cases, the defect will only be passed down if it occurs in the germ line.
The same disease, such as some forms of cancer, may be caused by an inherited genetic condition in some people, by new mutations in other people, and mainly by environmental causes in other people.
Whether, when and to what extent a person with the genetic defect or abnormality will actually suffer from the disease is almost always affected by the environmental factors and events in the person's development.
Some types of recessive gene disorders confer an advantage in certain environments when only one copy of the gene is present.
Click on any of the following blue hyperlinks for more about Genetic Disorders:
A genetic disorder is a genetic problem caused by one or more abnormalities in the genome, especially a condition that is present from birth (congenital).
Most genetic disorders are quite rare and affect one person in every several thousands or millions.
Genetic disorders may be hereditary, passed down from the parents' genes. In other genetic disorders, defects may be caused by new mutations or changes to the DNA. In such cases, the defect will only be passed down if it occurs in the germ line.
The same disease, such as some forms of cancer, may be caused by an inherited genetic condition in some people, by new mutations in other people, and mainly by environmental causes in other people.
Whether, when and to what extent a person with the genetic defect or abnormality will actually suffer from the disease is almost always affected by the environmental factors and events in the person's development.
Some types of recessive gene disorders confer an advantage in certain environments when only one copy of the gene is present.
Click on any of the following blue hyperlinks for more about Genetic Disorders:
- Single-gene
- Autosomal dominant
Autosomal recessive
X-linked dominant
X-linked recessive
Y-linked
Mitochondrial
- Autosomal dominant
- Many genes
- Diagnosis
- Prognosis
- Treatment
- See also:
- FINDbase (the Frequency of Inherited Disorders database)
- Genetic epidemiology
- Inborn errors of metabolism
- Population groups in biomedicine
- Mendelian error
- Public Health Genomics at CDC
- OMIM — Online Mendelian Inheritance in Man, a catalog of human genes and genetic disorders
- Genetic and Rare Diseases Information Center (GARD) Office of Rare Diseases (ORD), National Institutes of Health (NIH)
- CDC’s National Center on Birth Defects and Developmental Disabilities
- Genetic Disease Information from the Human Genome Project
- Global Genes Project, Genetic and Rare Diseases Organization
American Medical Association (AMA) including the Journal of the American Medical Association (JAMA) AMA Web Site Pictured below: Logos for the (L-R) AMA and JAMA
The American Medical Association (AMA), founded in 1847 and incorporated in 1897, is the largest association of physicians—both MDs and DOs—and medical students in the United States.
The AMA's stated mission is "to bring together physicians and communities to improve the nation’s health."
The Association also publishes the Journal of the American Medical Association (JAMA), which has the largest circulation of any weekly medical journal in the world.
The AMA also publishes a list of Physician Specialty Codes which are the standard method in the U.S. for identifying physician and practice specialties.
Click on any of the following blue hyperlinks for more about the American Medical Association:
The AMA's stated mission is "to bring together physicians and communities to improve the nation’s health."
The Association also publishes the Journal of the American Medical Association (JAMA), which has the largest circulation of any weekly medical journal in the world.
The AMA also publishes a list of Physician Specialty Codes which are the standard method in the U.S. for identifying physician and practice specialties.
Click on any of the following blue hyperlinks for more about the American Medical Association:
- History
- Criticisms and historical controversies
- Structure
- Membership
- Charitable activities
- See also:
- JAMA Pediatrics
- AMA Foundation Leadership Award
- AMA Manual of Style
- AMA Scientific Achievement Award
- American Association of Physicians and Surgeons
- American College of Physicians
- American Dental Association
- American Medical Student Association
- American Osteopathic Association
- List of journals published by the American Medical Association
- National Physicians Alliance
- Physicians for a National Health Program
- American Medical Association annual meetings collection (1866-1890)—National Library of Medicine finding aid
- AMA Deceased Physicians Masterfile (1906-1969)—National Library of Medicine finding aid
The Study of Medicine, including Medical Degrees in the United States along with Medical Schools including a List of Medical Schools
- YouTube Video: M.D. vs. D.O. | Allopathic and Osteopathic Medical School Comparison
- YouTube Video: Mayo Clinic in Rochester's Internal Medicine Residency Overview
- YouTube Video: Tips For Foreign Medical Grads To Practice In The United States
Medicine is the science and practice of the diagnosis, treatment, and prevention of disease. Medicine encompasses a variety of health care practices evolved to maintain and restore health by the prevention and treatment of illness.
Contemporary medicine applies biomedical sciences, biomedical research, genetics, and medical technology to diagnose, treat, and prevent injury and disease, typically through pharmaceuticals or surgery, but also through therapies as diverse as psychotherapy, external splints and traction, medical devices, biologics, and ionizing radiation, amongst others.
Medicine has existed for thousands of years, during most of which it was an art (an area of skill and knowledge) frequently having connections to the religious and philosophical beliefs of local culture.
For example, a medicine man would apply herbs and say prayers for healing, or an ancient philosopher and physician would apply bloodletting according to the theories of humorism.
In recent centuries, since the advent of modern science, most medicine has become a combination of art and science (both basic and applied, under the umbrella of medical science). While stitching technique for sutures is an art learned through practice, the knowledge of what happens at the cellular and molecular level in the tissues being stitched arises through science.
Prescientific forms of medicine are now known as traditional medicine and folk medicine. They remain commonly used with or instead of scientific medicine and are thus called alternative medicine. For example, evidence on the effectiveness of acupuncture is "variable and inconsistent" for any condition, but is generally safe when done by an appropriately trained practitioner. In contrast, treatments outside the bounds of safety and efficacy are termed quackery.
Click on any of the following blue hyperlinks for more about Medicine:
Medical education in the United States:
Medical education in the United States includes educational activities involved in the education and training of physicians in the United States, from entry-level training through to continuing education of qualified specialists.
A typical outline of the medical education pathway is presented below; however, medicine is a diverse profession with many options available.
For example, some physicians work in pharmaceutical research, occupational medicine (within a company), public health medicine (working for the general health of a population in an area), or join the armed forces.
Medical School:
Main article: Medical school in the United States
In the United States a medical school is an institution with the purpose of educating physicians in the United States in the field of medicine. Admission into medical school may not technically require completion of a previous degree; however, applicants are usually required to complete at least 3 years of "pre-med" courses at the university level because in the US medical degrees are classified as Second entry degrees.
Once enrolled in a medical school the four years progressive study is divided into two roughly equal components: pre-clinical (consisting of didactic courses in the basic sciences) and clinical (clerkships consisting of rotations through different wards of a teaching hospital).
The degree granted at the conclusion of these four years of study is Doctor of Medicine (M.D.) or, less commonly, Doctor of Osteopathic Medicine (D.O.) depending on the medical school; both degrees allow the holder to practice medicine after completing an accredited residency program.
Further information: Comparison of MD and DO in the United States
Internship:
Main article: Internship (medicine)
During the last year of graduate medical education, students apply for postgraduate residencies in their chosen field of specialization. These vary in competitiveness depending upon the desirability of the specialty, prestige of the program, and the number of applicants relative to the number of available positions. All but a few positions are granted via a national computer match which pairs an applicant's preference with the programs' preference for applicants.
Historically, post-graduate medical education began with a free-standing, one-year internship. Completion of this year continues to be the minimum training requirement for obtaining a general license to practice medicine in most states. However, because of the gradual lengthening of post-graduate medical education, and the decline of its use as the terminal stage in training, most new physicians complete the internship requirement as their first year of residency.
Not withstanding the trend toward internships integrated into categorical residencies, the one-year "traditional rotating internship" (sometimes called a "transitional year") continues to exist. Some residency training programs, such as in neurology and ophthalmology, do not include an internship year and begin after completion of an internship or transitional year.
Some use it to re-apply to programs into which they were not accepted, while others use it as a year to decide upon a specialty. In addition, osteopathic physicians "are required to have completed an American Osteopathic Association (AOA)-approved first year of training in order to be licensed in Florida, Michigan, Oklahoma and Pennsylvania.
Residency:
Main article: Residency (medicine)
Each of the specialties in medicine has established its own curriculum, which defines the length and content of residency training necessary to practice in that specialty.
Programs range from 3 years after medical school for internal medicine and pediatrics, to 5 years for general surgery, to 7 years for neurosurgery. Each specialty training program either incorporates an internship year to satisfy the requirements of state licensure, or stipulates that an internship year be completed before starting the program at the second post-graduate year (PGY-2).
Fellowship:
Main article: Fellowship (medicine)
A fellowship is a formal, full-time training program that focuses on a particular area within the specialty, with requirements beyond the related residency. Many highly specialized fields require formal training beyond residency. Examples of these include the following:
There are many others for each field of study. In some specialties such as pathology and radiology, a majority of graduating residents go on to further their training. The training programs for these fields are known as fellowships and their participants are fellows, to denote that they already have completed a residency and are board eligible or board certified in their basic specialty.
Fellowships range in length from one to three years and are granted by application to the individual program or sub-specialty organizing board. Fellowships often contain a research component.
Board Certification:
Main article: Board certification
The physician or surgeon who has completed his or her residency and possibly fellowship training and is in the practice of his or her specialty is known as an attending physician.
Physicians then must pass written and oral exams in their specialty in order to become board certified. Each of the 26 medical specialties has different requirements for practitioners to undertake continuing medical education activities.
See Also:
Contemporary medicine applies biomedical sciences, biomedical research, genetics, and medical technology to diagnose, treat, and prevent injury and disease, typically through pharmaceuticals or surgery, but also through therapies as diverse as psychotherapy, external splints and traction, medical devices, biologics, and ionizing radiation, amongst others.
Medicine has existed for thousands of years, during most of which it was an art (an area of skill and knowledge) frequently having connections to the religious and philosophical beliefs of local culture.
For example, a medicine man would apply herbs and say prayers for healing, or an ancient philosopher and physician would apply bloodletting according to the theories of humorism.
In recent centuries, since the advent of modern science, most medicine has become a combination of art and science (both basic and applied, under the umbrella of medical science). While stitching technique for sutures is an art learned through practice, the knowledge of what happens at the cellular and molecular level in the tissues being stitched arises through science.
Prescientific forms of medicine are now known as traditional medicine and folk medicine. They remain commonly used with or instead of scientific medicine and are thus called alternative medicine. For example, evidence on the effectiveness of acupuncture is "variable and inconsistent" for any condition, but is generally safe when done by an appropriately trained practitioner. In contrast, treatments outside the bounds of safety and efficacy are termed quackery.
Click on any of the following blue hyperlinks for more about Medicine:
- Etymology
- Clinical practice
- Institutions including Delivery
- Branches
- Education and legal controls
- Medical ethics
- History
- Traditional medicine
- See also:
Medical education in the United States:
Medical education in the United States includes educational activities involved in the education and training of physicians in the United States, from entry-level training through to continuing education of qualified specialists.
A typical outline of the medical education pathway is presented below; however, medicine is a diverse profession with many options available.
For example, some physicians work in pharmaceutical research, occupational medicine (within a company), public health medicine (working for the general health of a population in an area), or join the armed forces.
Medical School:
Main article: Medical school in the United States
In the United States a medical school is an institution with the purpose of educating physicians in the United States in the field of medicine. Admission into medical school may not technically require completion of a previous degree; however, applicants are usually required to complete at least 3 years of "pre-med" courses at the university level because in the US medical degrees are classified as Second entry degrees.
Once enrolled in a medical school the four years progressive study is divided into two roughly equal components: pre-clinical (consisting of didactic courses in the basic sciences) and clinical (clerkships consisting of rotations through different wards of a teaching hospital).
The degree granted at the conclusion of these four years of study is Doctor of Medicine (M.D.) or, less commonly, Doctor of Osteopathic Medicine (D.O.) depending on the medical school; both degrees allow the holder to practice medicine after completing an accredited residency program.
Further information: Comparison of MD and DO in the United States
Internship:
Main article: Internship (medicine)
During the last year of graduate medical education, students apply for postgraduate residencies in their chosen field of specialization. These vary in competitiveness depending upon the desirability of the specialty, prestige of the program, and the number of applicants relative to the number of available positions. All but a few positions are granted via a national computer match which pairs an applicant's preference with the programs' preference for applicants.
Historically, post-graduate medical education began with a free-standing, one-year internship. Completion of this year continues to be the minimum training requirement for obtaining a general license to practice medicine in most states. However, because of the gradual lengthening of post-graduate medical education, and the decline of its use as the terminal stage in training, most new physicians complete the internship requirement as their first year of residency.
Not withstanding the trend toward internships integrated into categorical residencies, the one-year "traditional rotating internship" (sometimes called a "transitional year") continues to exist. Some residency training programs, such as in neurology and ophthalmology, do not include an internship year and begin after completion of an internship or transitional year.
Some use it to re-apply to programs into which they were not accepted, while others use it as a year to decide upon a specialty. In addition, osteopathic physicians "are required to have completed an American Osteopathic Association (AOA)-approved first year of training in order to be licensed in Florida, Michigan, Oklahoma and Pennsylvania.
Residency:
Main article: Residency (medicine)
Each of the specialties in medicine has established its own curriculum, which defines the length and content of residency training necessary to practice in that specialty.
Programs range from 3 years after medical school for internal medicine and pediatrics, to 5 years for general surgery, to 7 years for neurosurgery. Each specialty training program either incorporates an internship year to satisfy the requirements of state licensure, or stipulates that an internship year be completed before starting the program at the second post-graduate year (PGY-2).
Fellowship:
Main article: Fellowship (medicine)
A fellowship is a formal, full-time training program that focuses on a particular area within the specialty, with requirements beyond the related residency. Many highly specialized fields require formal training beyond residency. Examples of these include the following:
- after internal medicine:
- after anesthesiology:
- after general surgery:
- after obstetrics/gynecology:
There are many others for each field of study. In some specialties such as pathology and radiology, a majority of graduating residents go on to further their training. The training programs for these fields are known as fellowships and their participants are fellows, to denote that they already have completed a residency and are board eligible or board certified in their basic specialty.
Fellowships range in length from one to three years and are granted by application to the individual program or sub-specialty organizing board. Fellowships often contain a research component.
Board Certification:
Main article: Board certification
The physician or surgeon who has completed his or her residency and possibly fellowship training and is in the practice of his or her specialty is known as an attending physician.
Physicians then must pass written and oral exams in their specialty in order to become board certified. Each of the 26 medical specialties has different requirements for practitioners to undertake continuing medical education activities.
See Also:
- The Flexner Report
- Combined internal medicine and psychiatry residency
- Integrated Medical Curriculum
- List of medical schools in the United States
The United States Department of Health and Human Services (HHS), also known as the Health Department, is a cabinet-level department of the U.S. federal government with the goal of protecting the health of all Americans and providing essential human services.
Its motto is "Improving the health, safety, and well-being of America".
Before the separate federal Department of Education was created in 1979, it was called the Department of Health, Education, and Welfare (HEW).
Department of Health and Human Services
The Department of Health, Education, and Welfare was renamed the Department of Health and Human Services (HHS) in 1979, when its education functions were transferred to the newly created United States Department of Education under the Department of Education Organization Act.
HHS was left in charge of the Social Security Administration, agencies constituting the Public Health Service, and Family Support Administration.
In 1995, the Social Security Administration was removed from the Department of Health and Human Services, and established as an independent agency of the executive branch of the United States Government.
HHS is administered by the Secretary of Health and Human Services, who is appointed by the President with the advice and consent of the Senate. The United States Public Health Service (PHS) is the main division of the HHS and is led by the Assistant Secretary for Health. The current Secretary, Alex Azar, assumed office on January 29, 2018, upon his appointment by President Trump and confirmation by the Senate.
The United States Public Health Service Commissioned Corps, the uniformed service of the PHS, is led by the Surgeon General who is responsible for addressing matters concerning public health as authorized by the Secretary or by the Assistant Secretary of Health in addition to his or her primary mission of administering the Commissioned Corps.
Federal, state, and local health departments:
There are three tiers of health departments, the federal health department, state health department and local health department. In relation with state and local government, the federal government provides states with funding to ensure that states are able to retain current programs and are able to implement new programs.
The coordination between all three health departments is critical to ensure the programs being implemented are well structured and suited to the corresponding level of health department. The health department at state level needs to safeguard good relations with legislators as well as governors in order to acquire legal and financial aid to guarantee the development and enhancements of the programs.
Assemblies are set up to guide the relationships between state and local health departments. The state sets up the regulations and health policies whereas the local health departments are the ones implementing the health policies and services.
Office of Inspector General:
The Office of the Inspector General (OIG) investigates criminal activity for HHS. The special agents who work for OIG have the same title series "1811", training and authority as other federal criminal investigators, such as the FBI, ATF, DEA and Secret Service. However, OIG Special Agents have special skills in investigating white collar crime related to Medicare and Medicaid fraud and abuse. Organized crime has dominated the criminal activity relative to this type of fraud.
HHS-OIG investigates tens of millions of dollars in Medicare fraud each year. In addition, OIG will continue its coverage of all 50 states and the District of Columbia by its multi-agency task forces (PSOC Task Forces) that identify, investigate, and prosecute individuals who willfully avoid payment of their child support obligations under the Child Support Recovery Act.
HHS-OIG agents also provide protective services to the Secretary of HHS, and other department executives as necessary.
In 2002, the department released Healthy People 2010, a national strategic initiative for improving the health of Americans.
With the passage of the Fraud Enforcement and Recovery Act of 2009, and the Affordable Care Act of 2010, the Office of the Inspector General has taken an emboldened stance against healthcare related non-compliance, most notably for violations of Stark Law and the Anti-Kickback Statute.
In 2015, the OIG issued a fraud alert as a warning to hospitals and healthcare systems to monitor and comply with their physician compensation arrangements.
Recent years have seen dramatic increases in both the number and the amounts of Stark Law violation settlements, prompting healthcare experts to identify a need for automated solutions that manage physician arrangements by centralizing necessary information with regard to physician-hospital integration.
Contract management software companies such as Meditract provide options for health systems to organize and store physician contracts. Ludi Inc introduced DocTime Log®, an SaaS solution that specifically addresses this growing concern, automating physician time logging in compliance with contract terms to eliminate Stark Law and Anti-Kickback Statute violations.
Click on any of the following blue hyperlinks for more about the United States Department of Health & Human Services:
Its motto is "Improving the health, safety, and well-being of America".
Before the separate federal Department of Education was created in 1979, it was called the Department of Health, Education, and Welfare (HEW).
Department of Health and Human Services
The Department of Health, Education, and Welfare was renamed the Department of Health and Human Services (HHS) in 1979, when its education functions were transferred to the newly created United States Department of Education under the Department of Education Organization Act.
HHS was left in charge of the Social Security Administration, agencies constituting the Public Health Service, and Family Support Administration.
In 1995, the Social Security Administration was removed from the Department of Health and Human Services, and established as an independent agency of the executive branch of the United States Government.
HHS is administered by the Secretary of Health and Human Services, who is appointed by the President with the advice and consent of the Senate. The United States Public Health Service (PHS) is the main division of the HHS and is led by the Assistant Secretary for Health. The current Secretary, Alex Azar, assumed office on January 29, 2018, upon his appointment by President Trump and confirmation by the Senate.
The United States Public Health Service Commissioned Corps, the uniformed service of the PHS, is led by the Surgeon General who is responsible for addressing matters concerning public health as authorized by the Secretary or by the Assistant Secretary of Health in addition to his or her primary mission of administering the Commissioned Corps.
Federal, state, and local health departments:
There are three tiers of health departments, the federal health department, state health department and local health department. In relation with state and local government, the federal government provides states with funding to ensure that states are able to retain current programs and are able to implement new programs.
The coordination between all three health departments is critical to ensure the programs being implemented are well structured and suited to the corresponding level of health department. The health department at state level needs to safeguard good relations with legislators as well as governors in order to acquire legal and financial aid to guarantee the development and enhancements of the programs.
Assemblies are set up to guide the relationships between state and local health departments. The state sets up the regulations and health policies whereas the local health departments are the ones implementing the health policies and services.
Office of Inspector General:
The Office of the Inspector General (OIG) investigates criminal activity for HHS. The special agents who work for OIG have the same title series "1811", training and authority as other federal criminal investigators, such as the FBI, ATF, DEA and Secret Service. However, OIG Special Agents have special skills in investigating white collar crime related to Medicare and Medicaid fraud and abuse. Organized crime has dominated the criminal activity relative to this type of fraud.
HHS-OIG investigates tens of millions of dollars in Medicare fraud each year. In addition, OIG will continue its coverage of all 50 states and the District of Columbia by its multi-agency task forces (PSOC Task Forces) that identify, investigate, and prosecute individuals who willfully avoid payment of their child support obligations under the Child Support Recovery Act.
HHS-OIG agents also provide protective services to the Secretary of HHS, and other department executives as necessary.
In 2002, the department released Healthy People 2010, a national strategic initiative for improving the health of Americans.
With the passage of the Fraud Enforcement and Recovery Act of 2009, and the Affordable Care Act of 2010, the Office of the Inspector General has taken an emboldened stance against healthcare related non-compliance, most notably for violations of Stark Law and the Anti-Kickback Statute.
In 2015, the OIG issued a fraud alert as a warning to hospitals and healthcare systems to monitor and comply with their physician compensation arrangements.
Recent years have seen dramatic increases in both the number and the amounts of Stark Law violation settlements, prompting healthcare experts to identify a need for automated solutions that manage physician arrangements by centralizing necessary information with regard to physician-hospital integration.
Contract management software companies such as Meditract provide options for health systems to organize and store physician contracts. Ludi Inc introduced DocTime Log®, an SaaS solution that specifically addresses this growing concern, automating physician time logging in compliance with contract terms to eliminate Stark Law and Anti-Kickback Statute violations.
Click on any of the following blue hyperlinks for more about the United States Department of Health & Human Services:
- Official website
- Department of Health and Human Services in the Federal Register
- National Archives, RG 235, General Records of the Department of Health, Education and Welfare
- History
- Criticisms and controversies
- Strengthening Communities Fund
- Organization
- Budget and finances
- Former operating divisions and agencies
- Programs
- Freedom of Information Act processing performance
- Health care reform
- Related legislation
- See also
- American Recovery and Reinvestment Act (ARRA)
- Early Head Start
- Emergency Care Coordination Center
- Global Health Security Initiative
- Head Start
- Health information technology
- Health professional
- Healthy People 2010
- Human experimentation in the United States
- Rural health
- Supporting Healthy Marriage Project
- William R. Steiger
Within the following five topics, we will comprehensively cover Healthcare in the United States in all its facets.
Healthcare in the United States including a List of Hospitals and Medical Centers
YouTube Video: A History of Health Care in the United States.
(Dr. Valerie Arkoosh explains how the employer-based heathcare system came about in the United States and why it is no longer adequate to meet the needs of many Americans.)
YouTube Video: George Halvorson* talks differences in health care between U.S. and world
*- George Halvorson
Pictured: U.S. healthcare costs exceed those of other countries, relative to the size of the economy or GDP. Courtesy of Council of Economic Advisers to the President of the United States - Council of Economic Advisers (2009-06). 10. Executive Office of the President of the United States.
Healthcare in the United States including a List of Hospitals and Medical Centers
YouTube Video: A History of Health Care in the United States.
(Dr. Valerie Arkoosh explains how the employer-based heathcare system came about in the United States and why it is no longer adequate to meet the needs of many Americans.)
YouTube Video: George Halvorson* talks differences in health care between U.S. and world
*- George Halvorson
Pictured: U.S. healthcare costs exceed those of other countries, relative to the size of the economy or GDP. Courtesy of Council of Economic Advisers to the President of the United States - Council of Economic Advisers (2009-06). 10. Executive Office of the President of the United States.
Click Here for a List of Hospitals in the United States
Click Here for a List of Medical Centers in the United States
Health care in the United States is provided by many distinct organizations. Health care facilities are largely owned and operated by private sector businesses. 58% of US community hospitals are non-profit, 21% are government owned, and 21% are for-profit.
According to the World Health Organization (WHO), the United States spent more on health care per capita ($8,608), and more on health care as percentage of its GDP (17.2%), than any other nation in 2011.
64.3% of health spending was paid for by the government in 2013, funded via programs such as Medicare, Medicaid, the Children's Health Insurance Program, and the Veterans Health Administration. People aged under 67 acquire insurance via their or a family member's employer, by purchasing health insurance on their own, or are uninsured. Health insurance for public sector employees is primarily provided by the government.
The United States life expectancy of 78.4 years at birth, up from 75.2 years in 1990, ranks it 50th among 221 nations, and 27th out of the 34 industrialized OECD countries, down from 20th in 1990.
Of 17 high-income countries studied by the National Institutes of Health in 2013, the United States had the highest or near-highest prevalence of obesity, car accidents, infant mortality, heart and lung disease, sexually transmitted infections, adolescent pregnancies, injuries, and homicides.
On average, a U.S. male can be expected to live almost four fewer years than those in the top-ranked country, though notably Americans aged 75 live longer than those who reach that age in other developed nations.
A 2014 survey of the healthcare systems of 11 developed countries found the US healthcare system to be the most expensive and worst-performing in terms of health access, efficiency, and equity.
Americans undergo cancer screenings at significantly higher rates than people in other developed countries, and access MRI and CT scans at the highest rate of any OECD nation.
People in the U.S. diagnosed with high cholesterol or hypertension access pharmaceutical treatments at higher rates than those diagnosed in other developed nations, and are more likely to successfully control the conditions. Diabetics are more likely to receive treatment and meet treatment targets in the U.S. than in Canada, England, or Scotland. A study showed that the U.S., Japan, and France recorded the highest survival rates among 31 nations for four types of cancer.
Gallup recorded that the uninsured rate among U.S. adults was 11.9% for the first quarter of 2015, continuing the decline of the uninsured rate outset by the Affordable Care Act. A 2004 Institute of Medicine (IOM) report said: "The United States is among the few industrialized nations in the world that does not guarantee access to health care for its population."
A 2004 OECD report said: "With the exception of Mexico, Turkey, and the United States, all OECD countries had achieved universal or near-universal (at least 98.4% insured) coverage of their populations by 1990." Recent evidence demonstrates that lack of health insurance causes some 45,000 to 48,000 unnecessary deaths every year in the United States.
In 2007, 62.1% of filers for bankruptcies claimed high medical expenses. A 2013 study found that about 25% of all senior citizens declare bankruptcy due to medical expenses, and 43% are forced to mortgage or sell their primary residence.
In 2010 the Patient Protection and Affordable Care Act (PPACA) became law, providing for major changes in health insurance. Under the act, hospitals and primary physicians would transform their practices financially, technologically, and clinically to drive better health outcomes, lower costs, and improve their methods of distribution and accessibility.
The Supreme Court upheld the constitutionality of most of the law in June 2012 and affirmed insurance exchange subsidies in all states in June 2015.
Click on any of the following blue hyperlinks for further amplification:
Click Here for a List of Medical Centers in the United States
Health care in the United States is provided by many distinct organizations. Health care facilities are largely owned and operated by private sector businesses. 58% of US community hospitals are non-profit, 21% are government owned, and 21% are for-profit.
According to the World Health Organization (WHO), the United States spent more on health care per capita ($8,608), and more on health care as percentage of its GDP (17.2%), than any other nation in 2011.
64.3% of health spending was paid for by the government in 2013, funded via programs such as Medicare, Medicaid, the Children's Health Insurance Program, and the Veterans Health Administration. People aged under 67 acquire insurance via their or a family member's employer, by purchasing health insurance on their own, or are uninsured. Health insurance for public sector employees is primarily provided by the government.
The United States life expectancy of 78.4 years at birth, up from 75.2 years in 1990, ranks it 50th among 221 nations, and 27th out of the 34 industrialized OECD countries, down from 20th in 1990.
Of 17 high-income countries studied by the National Institutes of Health in 2013, the United States had the highest or near-highest prevalence of obesity, car accidents, infant mortality, heart and lung disease, sexually transmitted infections, adolescent pregnancies, injuries, and homicides.
On average, a U.S. male can be expected to live almost four fewer years than those in the top-ranked country, though notably Americans aged 75 live longer than those who reach that age in other developed nations.
A 2014 survey of the healthcare systems of 11 developed countries found the US healthcare system to be the most expensive and worst-performing in terms of health access, efficiency, and equity.
Americans undergo cancer screenings at significantly higher rates than people in other developed countries, and access MRI and CT scans at the highest rate of any OECD nation.
People in the U.S. diagnosed with high cholesterol or hypertension access pharmaceutical treatments at higher rates than those diagnosed in other developed nations, and are more likely to successfully control the conditions. Diabetics are more likely to receive treatment and meet treatment targets in the U.S. than in Canada, England, or Scotland. A study showed that the U.S., Japan, and France recorded the highest survival rates among 31 nations for four types of cancer.
Gallup recorded that the uninsured rate among U.S. adults was 11.9% for the first quarter of 2015, continuing the decline of the uninsured rate outset by the Affordable Care Act. A 2004 Institute of Medicine (IOM) report said: "The United States is among the few industrialized nations in the world that does not guarantee access to health care for its population."
A 2004 OECD report said: "With the exception of Mexico, Turkey, and the United States, all OECD countries had achieved universal or near-universal (at least 98.4% insured) coverage of their populations by 1990." Recent evidence demonstrates that lack of health insurance causes some 45,000 to 48,000 unnecessary deaths every year in the United States.
In 2007, 62.1% of filers for bankruptcies claimed high medical expenses. A 2013 study found that about 25% of all senior citizens declare bankruptcy due to medical expenses, and 43% are forced to mortgage or sell their primary residence.
In 2010 the Patient Protection and Affordable Care Act (PPACA) became law, providing for major changes in health insurance. Under the act, hospitals and primary physicians would transform their practices financially, technologically, and clinically to drive better health outcomes, lower costs, and improve their methods of distribution and accessibility.
The Supreme Court upheld the constitutionality of most of the law in June 2012 and affirmed insurance exchange subsidies in all states in June 2015.
Click on any of the following blue hyperlinks for further amplification:
- History
- Statistics
- Nobel Prize
- Providers
- Facilities
- Spending
- Regulation and oversight
- Overall system effectiveness
- System efficiency and equity
- Drug efficiency and safety
- Political issues
- Reform
- Health insurance coverage for immigrants
- Health insurance coverage for visitors to the U.S.
- See also:
- Canadian and American health care systems compared
- Centers for Disease Control and Prevention timeline
- Key person insurance
- Health care compared – tabular comparisons of the US, Canada, and other countries not shown above.
- Health care industry
- Health care politics
- Health care systems (including comparisons)
- Health insurance cooperative
- Healthy people
- HIV/AIDS in the United States
- List of healthcare accreditation organizations in the United States
- List of countries by health care expenditures
- Medical centers in the United States
- Medical debt
- Medicare Rights Center
- Medicare Sustainable Growth Rate
- Military Health System
- School health services
- United States National Health Care Act
- Universal Health Care Foundation of Connecticut
- Water fluoridation in the United States
Healthcare reform in the United States
YouTube Video About Health Care Reform in America: A History*
*-- CNN's Sanjay Gupta gives us a brief history of health care reform in America.
Pictured: Health spending per capita, in US$ PPP-adjusted, compared amongst various first world nations.
YouTube Video About Health Care Reform in America: A History*
*-- CNN's Sanjay Gupta gives us a brief history of health care reform in America.
Pictured: Health spending per capita, in US$ PPP-adjusted, compared amongst various first world nations.
Health care reform in the United States has a long history. Reforms have often been proposed but have rarely been accomplished. In 2010, landmark reform was passed through two federal statutes enacted in 2010: the Patient Protection and Affordable Care Act (PPACA), signed March 23, 2010, and the Health Care and Education Reconciliation Act of 2010 (H.R. 4872), which amended the PPACA and became law on March 30, 2010.
Future reforms of the American health care system continue to be proposed, with notable proposals including a single-payer system and a reduction in fee-for-service medical care The PPACA includes a new agency, the Center for Medicare and Medicaid Innovation, which is intended to research reform ideas through pilot projects.
Click on any of the following blue hyperlinks for more about Healthcare reform in the United States:
Future reforms of the American health care system continue to be proposed, with notable proposals including a single-payer system and a reduction in fee-for-service medical care The PPACA includes a new agency, the Center for Medicare and Medicaid Innovation, which is intended to research reform ideas through pilot projects.
Click on any of the following blue hyperlinks for more about Healthcare reform in the United States:
- History of national reform efforts
- Motivation
- Public opinion
- Patient Protection and Affordable Care Act
- Alternatives and research directions
- Trump administration efforts
- See also:
Healthcare Spending in the United States
YouTube Video: PBS* Documentary: Why Does U.S. Health Care Cost So Much?
* -- PBS News Hour
Pictured:
TOP PHOTO: U.S. Healthcare Costs as a Percentage of GDP 2000-2011 (Courtesy of Farcaster - Data from Centers for Medicare and Medicaid Services, CC BY-SA 3.0,
BOTTOM PHOTO: Health care cost rise in the U.S. relative to other countries, as measured by total expenditure on health as percent of GDP.
YouTube Video: PBS* Documentary: Why Does U.S. Health Care Cost So Much?
* -- PBS News Hour
Pictured:
TOP PHOTO: U.S. Healthcare Costs as a Percentage of GDP 2000-2011 (Courtesy of Farcaster - Data from Centers for Medicare and Medicaid Services, CC BY-SA 3.0,
BOTTOM PHOTO: Health care cost rise in the U.S. relative to other countries, as measured by total expenditure on health as percent of GDP.
Health care spending in the United States is characterized as the most costly compared to all OECD (developed) countries, measured both per person and as a share of GDP. Despite this spending, the quality of health care overall is low by some measures.
The Centers for Medicare and Medicaid reported in 2014 that U.S. healthcare costs were 17.4% GDP in 2013, similar to 2009-2012 but up from 13.4% GDP in 2000. Healthcare costs per capita have risen steadily from $4,881 in 2000 to $9,255 in 2013, a 5% average annual increase. The annual rate of increase in total healthcare costs has been declining, falling steadily from a 9.6% increase in 2002 to 3.8% for 2009 and has been steady since, to a 3.6% increase in 2013.
The Congressional Budget Office reported in January 2015 that:
CBO projected in June 2015 that federal spending on healthcare programs will rise from 5.2% GDP in 2015 to 8.0% GDP by 2040. This would be driven by a significant increase in the number of program beneficiaries due to the retirement of the Baby Boomers and expanded coverage under the Affordable Care Act, along with healthcare cost inflation.
According to the World Health Organization (WHO), total health care spending in the U.S. was 17% of its GDP in 2012, the highest in the world. The Health and Human Services Department expects that the health share of GDP will continue its historical upward trend, reaching 19.6% of GDP by 2024.
Of each dollar spent on health care in the United States:
The Commonwealth Fund ranked the United States last in the quality of health care among similar countries, while U.S. care costs the most.
Around 84.7% of Americans have some form of health insurance; either through their employer or the employer of their spouse or parent (59.3%), purchased individually (8.9%), or provided by government programs (27.8%; there is some overlap in these figures).
All government health care programs have restricted eligibility, and there is no government health insurance company which covers all Americans. Americans without health insurance coverage in 2007 totaled 15.3% of the population, or 45.7 million people.
Among those whose employer pays for health insurance, the employee may be required to contribute part of the cost of this insurance, while the employer usually chooses the insurance company and, for large groups, negotiates with the insurance company.
Government programs directly cover 27.8% of the population (83 million), including the elderly, disabled, children, veterans, and some of the poor, and federal law mandates public access to emergency services regardless of ability to pay. Public spending accounts for between 45% and 56.1% of U.S. health care spending.
Some Americans do not qualify for government-provided health insurance, are not provided health insurance by an employer, and are unable to afford, cannot qualify for, or choose not to purchase, private health insurance. When charity or "uncompensated" care is not available, they sometimes simply go without needed medical treatment. This problem has become a source of considerable political controversy on a national level.
Click here for being taken to the last topic about Healthcare in the United States: Health Insurance Cover.
Or, click on any of the following blue hyperlinks for more about Healthcare Spending in the United States:
The Centers for Medicare and Medicaid reported in 2014 that U.S. healthcare costs were 17.4% GDP in 2013, similar to 2009-2012 but up from 13.4% GDP in 2000. Healthcare costs per capita have risen steadily from $4,881 in 2000 to $9,255 in 2013, a 5% average annual increase. The annual rate of increase in total healthcare costs has been declining, falling steadily from a 9.6% increase in 2002 to 3.8% for 2009 and has been steady since, to a 3.6% increase in 2013.
The Congressional Budget Office reported in January 2015 that:
- Medicare costs were 3.5% GDP in 2014, steady from 2009 but up from 2.1% GDP in 2000;
- Medicaid costs were 1.7% GDP in 2014, steady from 2009 but up from 1.2% GDP in 2000.
CBO projected in June 2015 that federal spending on healthcare programs will rise from 5.2% GDP in 2015 to 8.0% GDP by 2040. This would be driven by a significant increase in the number of program beneficiaries due to the retirement of the Baby Boomers and expanded coverage under the Affordable Care Act, along with healthcare cost inflation.
According to the World Health Organization (WHO), total health care spending in the U.S. was 17% of its GDP in 2012, the highest in the world. The Health and Human Services Department expects that the health share of GDP will continue its historical upward trend, reaching 19.6% of GDP by 2024.
Of each dollar spent on health care in the United States:
- 31% goes to hospital care,
- 21% goes to physician/clinical services,
- 10% to pharmaceuticals,
- 4% to dental,
- 6% to nursing homes and 3% to home health care,
- 3% for other retail products, 3% for government public health activities,
- 7% to administrative costs,
- 7% to investment,
- and 6% to other professional services (physical therapists, optometrists, etc.).
The Commonwealth Fund ranked the United States last in the quality of health care among similar countries, while U.S. care costs the most.
Around 84.7% of Americans have some form of health insurance; either through their employer or the employer of their spouse or parent (59.3%), purchased individually (8.9%), or provided by government programs (27.8%; there is some overlap in these figures).
All government health care programs have restricted eligibility, and there is no government health insurance company which covers all Americans. Americans without health insurance coverage in 2007 totaled 15.3% of the population, or 45.7 million people.
Among those whose employer pays for health insurance, the employee may be required to contribute part of the cost of this insurance, while the employer usually chooses the insurance company and, for large groups, negotiates with the insurance company.
Government programs directly cover 27.8% of the population (83 million), including the elderly, disabled, children, veterans, and some of the poor, and federal law mandates public access to emergency services regardless of ability to pay. Public spending accounts for between 45% and 56.1% of U.S. health care spending.
Some Americans do not qualify for government-provided health insurance, are not provided health insurance by an employer, and are unable to afford, cannot qualify for, or choose not to purchase, private health insurance. When charity or "uncompensated" care is not available, they sometimes simply go without needed medical treatment. This problem has become a source of considerable political controversy on a national level.
Click here for being taken to the last topic about Healthcare in the United States: Health Insurance Cover.
Or, click on any of the following blue hyperlinks for more about Healthcare Spending in the United States:
- Spending
- Cost forecasts
- Payment
- The uninsured
- Role of government in health care market
- Impact on U.S. economic productivity
- Proposed solutions
Health Insurance Coverage in the United States,
- YouTube Video: The Basics of Health Insurance 101
- YouTube Video: How Health Insurance Works
- YouTube Video: Congressional Budget Office: 24M more will be uninsured under GOP health plan
The number of people without health insurance coverage in the United States is one of the primary concerns raised by advocates of health care reform. A person without health insurance is commonly termed uninsured (regardless of insurance of objects unrelated to health), and this article uses the term in this sense as well.
Multiple surveys indicate the number of uninsured has fallen due to expanded Medicaid eligibility and health insurance exchanges established due to the Patient Protection and Affordable Care Act, also known as PPACA or "Obamacare". These changes took effect March 23, 2012. The Commonwealth Fund reported in July 2014 that an additional 9.5 million people aged 19–64 had obtained health insurance, roughly 5% of the working-aged population. Gallup reported in July 2014 that the uninsured rate among adults 18 and over fell from 18.0% in Q3 2013 to 13.4% by Q2 2014. Rand Corporation had similar findings.
According to the United States Census Bureau, in 2012 there were 48.0 million people in the US (15.4% of the population) who were without health insurance. The causes of this rate of uninsurance remain a matter of political debate. Rising insurance costs have contributed to a trend in which fewer employers are offering health insurance, and many employers are managing costs by requiring higher employee contributions.
Many of the uninsured are the working poor or are unemployed. Others are healthy and choose to go without it. Some have been rejected by insurance companies and are considered "uninsurable". Some are without health insurance only temporarily. Some choose faith-based alternatives to health insurance.
Click on any of the following blue hyperlinks for more about Health Insurance Coverage in the United States:
Multiple surveys indicate the number of uninsured has fallen due to expanded Medicaid eligibility and health insurance exchanges established due to the Patient Protection and Affordable Care Act, also known as PPACA or "Obamacare". These changes took effect March 23, 2012. The Commonwealth Fund reported in July 2014 that an additional 9.5 million people aged 19–64 had obtained health insurance, roughly 5% of the working-aged population. Gallup reported in July 2014 that the uninsured rate among adults 18 and over fell from 18.0% in Q3 2013 to 13.4% by Q2 2014. Rand Corporation had similar findings.
According to the United States Census Bureau, in 2012 there were 48.0 million people in the US (15.4% of the population) who were without health insurance. The causes of this rate of uninsurance remain a matter of political debate. Rising insurance costs have contributed to a trend in which fewer employers are offering health insurance, and many employers are managing costs by requiring higher employee contributions.
Many of the uninsured are the working poor or are unemployed. Others are healthy and choose to go without it. Some have been rejected by insurance companies and are considered "uninsurable". Some are without health insurance only temporarily. Some choose faith-based alternatives to health insurance.
Click on any of the following blue hyperlinks for more about Health Insurance Coverage in the United States:
- Estimates of the number of uninsured
- Uninsured demographic
- Downturn effects
- Types of insurance
- Causes
- Consequences
- Emergency Medical Treatment and Active Labor Act (EMTALA)
- Uninsured rates by state
- Assisting programs for uninsured
- See also:
The Quality of Healthcare in the United States compared to Other Nations
YouTube Video: Bernie Sanders* proposing "Medicare for ALL Americans"
* - Bernie Sanders
Pictured: How the U.S. Health Care System Compares Internationally according to the Commonwealth Fund.
YouTube Video: Bernie Sanders* proposing "Medicare for ALL Americans"
* - Bernie Sanders
Pictured: How the U.S. Health Care System Compares Internationally according to the Commonwealth Fund.
Click here for list of countries by quality of healthcare as published by the Organisation for Economic Co-operation and Development (OECD).
Click on any of the following blue hyperlinks covering Healthcare in the United States vs. Other Countries:
Click on any of the following blue hyperlinks covering Healthcare in the United States vs. Other Countries:
Medical Specialties
- YouTube Video: Minimally Invasive Vascular Surgery
- YouTube Video: Cardiothoracic surgery
- YouTube Video: Surgical Video - Posterior Total Hip Replacement
A medical speciality is a branch of medical practice that is focused on a defined group of patients, diseases, skills, or philosophy. Examples include children (paediatrics), cancer (oncology), laboratory medicine (pathology), or primary care (family medicine). After completing medical school, physicians or surgeons usually further their medical education in a specific specialty of medicine by completing a multiple-year residency to become a medical specialist.
History of medical specialization:
Medical practitioners have long been specialized. According to Galen, specialization was common among Roman physicians. The particular system of modern medical specialties evolved gradually during the 19th century. Informal social recognition of medical specialization evolved before the formal legal system. The particular subdivision of the practice of medicine into various specialties varies from country to country, and is somewhat arbitrary.
Classification of medical specialization:
Medical specialties can be classified along several axes. These are:
Throughout history, the most important has been the division into surgical and internal medicine specialties:
In some countries, anesthesiology is classified as a surgical discipline, since it is vital in the surgical process, though anesthesiologists never perform major surgery themselves.
Many specialties are organ-based. Many symptoms and diseases come from a particular organ. Others are based mainly around a set of techniques, such as radiology, which was originally based around X-rays.
The age range of patients seen by any given specialist can be quite variable. Pediatricians handle most complaints and diseases in children that do not require surgery, and there are several sub-specialties (formally or informally) in pediatrics that mimic the organ-based specialties in adults.
Pediatric surgery may or may not be a separate specialty that handles some kinds of surgical complaints in children.
A further subdivision is the diagnostic versus therapeutic specialties. While the diagnostic process is of great importance in all specialties, some specialists perform mainly or only diagnostic examinations, such as pathology, clinical neurophysiology, and radiology. This line is becoming somewhat blurred with interventional radiology, an evolving field that uses image expertise to perform minimally invasive procedures.
Specialties that are common worldwide: Click on any of the following blue hyperlinks for more about that specialty:
Click on any of the following blue hyperlinks for more about Medical Specialties:
History of medical specialization:
Medical practitioners have long been specialized. According to Galen, specialization was common among Roman physicians. The particular system of modern medical specialties evolved gradually during the 19th century. Informal social recognition of medical specialization evolved before the formal legal system. The particular subdivision of the practice of medicine into various specialties varies from country to country, and is somewhat arbitrary.
Classification of medical specialization:
Medical specialties can be classified along several axes. These are:
- Surgical or internal medicine
- Age range of patients
- Diagnostic or therapeutic
- Organ-based or technique-based
Throughout history, the most important has been the division into surgical and internal medicine specialties:
- The surgical specialties are those in which an important part of diagnosis and treatment is achieved through major surgical techniques.
- The internal medicine specialties are the specialties in which the main diagnosis and treatment is never major surgery.
In some countries, anesthesiology is classified as a surgical discipline, since it is vital in the surgical process, though anesthesiologists never perform major surgery themselves.
Many specialties are organ-based. Many symptoms and diseases come from a particular organ. Others are based mainly around a set of techniques, such as radiology, which was originally based around X-rays.
The age range of patients seen by any given specialist can be quite variable. Pediatricians handle most complaints and diseases in children that do not require surgery, and there are several sub-specialties (formally or informally) in pediatrics that mimic the organ-based specialties in adults.
Pediatric surgery may or may not be a separate specialty that handles some kinds of surgical complaints in children.
A further subdivision is the diagnostic versus therapeutic specialties. While the diagnostic process is of great importance in all specialties, some specialists perform mainly or only diagnostic examinations, such as pathology, clinical neurophysiology, and radiology. This line is becoming somewhat blurred with interventional radiology, an evolving field that uses image expertise to perform minimally invasive procedures.
Specialties that are common worldwide: Click on any of the following blue hyperlinks for more about that specialty:
- Allergy and immunology
- Adolescent medicine
- Anesthesiology
- Aerospace medicine
- Cardiology
- Cardiothoracic surgery
- Clinical neurophysiology
- Colorectal surgery
- Dermatology
- Emergency medicine
- Endocrinology
- Family Medicine
- Forensic pathology
- Forensic psychiatry
- Gastroenterology
- General surgery
- Geriatrics
- Geriatric psychiatry
- Gynecologic oncology
- Hematology
- Infectious disease
- Internal medicine
- Interventional radiology
- Intensive care medicine
- Maternal-fetal medicine
- Medical biochemistry
- Medical genetics
- Medical oncology
- Neonatology
- Nephrology
- Neurology
- Neuropathology
- Neurosurgery
- Nuclear medicine
- Obstetrics and gynecology
- Occupational medicine
- Ophthalmology
- Orthopedic surgery
- Oral and maxillofacial surgery
- Otorhinolaryngology
- Palliative care
- Pathology
- Pediatrics
- Pediatric emergency medicine
- Pediatric surgery
- Physical medicine and rehabilitation
- Plastic, reconstructive and aesthetic surgery
- Psychiatry
- Public health
- Radiation oncology
- Radiology
- Respiratory medicine
- Rheumatology
- Sports medicine
- Neuroradiology
- Urology
- Vascular surgery
Click on any of the following blue hyperlinks for more about Medical Specialties:
- List of North American medical specialties and others
- Salaries
- Specialties by country
- United States
- Demography
- Satisfaction and burnout
- See also:
- Interdisciplinary sub-specialties of medicine, including
- Occupational medicine – branch of clinical medicine that provides health advice to organizations and individuals concerning work-related health and safety issues and standards. See occupational safety and health.
- Disaster medicine – branch of medicine that provides healthcare services to disaster survivors; guides medically related:
- throughout the disaster life cycle and serves as a liaison between and partner to:
- the medical contingency planner,
- the emergency management professional,
- the incident command system,
- government and policy makers.
- Preventive medicine – part of medicine engaged with preventing disease rather than curing it. It can be contrasted not only with curative medicine, but also with public health methods (which work at the level of population health rather than individual health).
- Medical genetics – the application of genetics to medicine. Medical genetics is a broad and varied field. It encompasses many different individual fields, including:
- clinical genetics,
- biochemical genetics,
- cytogenetics,
- molecular genetics,
- the genetics of common diseases (such as neural tube defects),
- and genetic counseling.
- Specialty Registrar
- Society of General Internal Medicine
- Interdisciplinary sub-specialties of medicine, including
Emergency Room, including 9-1-1 Operator and Emergency Medical Technicians (EMT)
- YouTube Video: Paramedics: Emergency Response - Catch Your Breath
- YouTube Video: A Day in the Life of 9-1-1 Operators
- YouTube Video: 24 Hours in the ER: Health care's front lines
Below we will present the three arms of emergency healthcare in the order that a patient requiring immediate healthcare would need incur them]
9-1-1, also written 911, is an emergency telephone number for the North American Numbering Plan (NANP), one of eight N11 codes.
Like other emergency numbers around the world, this number is intended for use in emergency circumstances only, and using it for any other purpose (such as making false or prank calls) is a crime in certain jurisdictions.
In over 98% of locations in the United States and Canada, dialing "9-1-1" from any telephone will link the caller to an emergency dispatch office—called a public-safety answering point (PSAP) by the telecommunications industry—which can send emergency responders to the caller's location in an emergency.
In approximately 96 percent of the U.S., the enhanced 9-1-1 system automatically pairs caller numbers with a physical address.
In the US, some carriers, including AT&T, map the number 112 to the emergency number 9-1-1.
Click on any of the following blue hyperlinks for more about the Emergency 9-1-1 Dispatcher:
Emergency medical technician (EMT), paramedic and ambulance technician are terms used in some countries to denote a health care provider of emergency medical services. EMTs are clinicians, trained to respond quickly to emergency situations regarding medical issues, traumatic injuries and accident scenes.
EMTs are most commonly found working in ambulances, but should not be confused with "ambulance drivers" or "ambulance attendants" – ambulance staff who in the past were not trained in emergency care or driving.
EMTs are often employed by private ambulance services, governments, and hospitals, but are also often employed by fire departments (and seen on fire apparatus), in police departments (and seen on police vehicles), and there are many firefighter/EMTs and police officer/EMTs. EMTs operate under a limited scope of practice. EMTs are normally supervised by a medical director, who is a physician.
Some EMTs are paid employees, while others (particularly those in rural areas) are volunteers.
Click on any of the following blue hyperlinks for more about EMTs:
An emergency department (ED), also known as an accident & emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine, the acute care of patients who present without prior appointment; either by their own means or by that of an ambulance.
The emergency department is usually found in a hospital or other primary care center.
Due to the unplanned nature of patient attendance, the department must provide initial treatment for a broad spectrum of illnesses and injuries, some of which may be life-threatening and require immediate attention.
In some countries, emergency departments have become important entry points for those without other means of access to medical care.
The emergency departments of most hospitals operate 24 hours a day, although staffing levels may be varied in an attempt to reflect patient volume.
Click on any of the following blue hyperlinks for more about Hospital Emergency Rooms:
9-1-1, also written 911, is an emergency telephone number for the North American Numbering Plan (NANP), one of eight N11 codes.
Like other emergency numbers around the world, this number is intended for use in emergency circumstances only, and using it for any other purpose (such as making false or prank calls) is a crime in certain jurisdictions.
In over 98% of locations in the United States and Canada, dialing "9-1-1" from any telephone will link the caller to an emergency dispatch office—called a public-safety answering point (PSAP) by the telecommunications industry—which can send emergency responders to the caller's location in an emergency.
In approximately 96 percent of the U.S., the enhanced 9-1-1 system automatically pairs caller numbers with a physical address.
In the US, some carriers, including AT&T, map the number 112 to the emergency number 9-1-1.
Click on any of the following blue hyperlinks for more about the Emergency 9-1-1 Dispatcher:
- History
- Enhanced 9-1-1
- Computer-aided dispatch
- Funding 9-1-1 services
- Problems with 9-1-1
- See also:
- 3-1-1, non-emergency number
- 911 Tapping Protocol
- eCall
- Emergency Medical Dispatcher
- Emergency telephone
- Emergency telephone number
- Enhanced 9-1-1
- In case of emergency
- Next Generation 9-1-1
- Reverse 911
- Wireless 9-1-1 Services Guide Federal Communications Commission (FCC)
- How to Use 9-1-1 from KidsHealth
- Emergency Numbers Around the World from 911dispatch.com
Emergency medical technician (EMT), paramedic and ambulance technician are terms used in some countries to denote a health care provider of emergency medical services. EMTs are clinicians, trained to respond quickly to emergency situations regarding medical issues, traumatic injuries and accident scenes.
EMTs are most commonly found working in ambulances, but should not be confused with "ambulance drivers" or "ambulance attendants" – ambulance staff who in the past were not trained in emergency care or driving.
EMTs are often employed by private ambulance services, governments, and hospitals, but are also often employed by fire departments (and seen on fire apparatus), in police departments (and seen on police vehicles), and there are many firefighter/EMTs and police officer/EMTs. EMTs operate under a limited scope of practice. EMTs are normally supervised by a medical director, who is a physician.
Some EMTs are paid employees, while others (particularly those in rural areas) are volunteers.
Click on any of the following blue hyperlinks for more about EMTs:
- United States
- See also:
An emergency department (ED), also known as an accident & emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine, the acute care of patients who present without prior appointment; either by their own means or by that of an ambulance.
The emergency department is usually found in a hospital or other primary care center.
Due to the unplanned nature of patient attendance, the department must provide initial treatment for a broad spectrum of illnesses and injuries, some of which may be life-threatening and require immediate attention.
In some countries, emergency departments have become important entry points for those without other means of access to medical care.
The emergency departments of most hospitals operate 24 hours a day, although staffing levels may be varied in an attempt to reflect patient volume.
Click on any of the following blue hyperlinks for more about Hospital Emergency Rooms:
- History
- Nomenclature in English
- Signage
- United States
- Critical conditions handled
- Special facilities, training, and equipment
- Non-emergency use
- Overcrowding
- In the military
- Violence against health care workers
- Medication errors
- See also:
- Acute Assessment Unit
- Walk-in clinic
- Morgue
- Overuse of Emergency Departments Among Insured Californians (US) (California HealthCare Foundation, October 2006)
- ED visits (US) (National Center for Health Statistics)
- Academic Emergency Medicine, ISSN 1069-6563, Elsvier
- Physicians on Call: California's Patchwork Approach to Emergency Department Coverage
- Wait Time for Treatment in Hospital Emergency Departments, 2009. Hyattsville, Md.: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, 2012.
- Friday Night at the ER (Simulation game and education program about Emergency Department crowding)
Nursing, including in the United States, along with Nursing Degrees, List of Nursing Schools, and the History of Nursing
- YouTube Video: A Day in the Life - Laurie (ER Nurse)
- YouTube Video: A Day in the Life - Tanisha (Oncology Nurse)
- YouTube Video: Patient says 'thank you' to nurse who saved her life
Click here for an alphabetical list of nursing schools by state in the United States.
Nursing is a profession within the health care sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life.
Nurses may be differentiated from other health care providers by their approach to patient care and training, and scope of practice. Nurses practice in many specialties with differing levels of prescription authority.
Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. However, nurse practitioners are permitted by most jurisdictions to practice independently in a variety of settings.
Since the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient's family and other team members, that focuses on treating illness to improve quality of life. In the United States and the United Kingdom, advanced practice nurses, such as clinical nurse specialists and nurse practitioners, diagnose health problems and prescribe medications and other therapies, depending on individual state regulations.
Nurses may help coordinate the patient care performed by other members of a multidisciplinary health care team such as therapists, medical practitioners and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
Although nursing practice varies both through its various specialties and countries, these nursing organizations offer the following definitions:
Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups and communities, sick or well, and in all settings. Nursing includes the promotion of health, prevention of illness, and the care of ill, disabled and dying people.
Advocacy, promotion of a safe environment, research, participation in shaping health policy and in patient and health systems management, and education are also key nursing roles.
(The above by Virginia Avenel Henderson (November 30, 1897 – March 19, 1996) was an influential nurse, researcher, theorist and author.)
As a Profession:
The authority for the practice of nursing is based upon a social contract that delineates professional rights and responsibilities as well as mechanisms for public accountability. In almost all countries, nursing practice is defined and governed by law, and entrance to the profession is regulated at the national or state level.
The aim of the nursing community worldwide is for its professionals to ensure quality care for all, while maintaining their credentials, code of ethics, standards, and competencies, and continuing their education.
There are a number of educational paths to becoming a professional nurse, which vary greatly worldwide; all involve extensive study of nursing theory and practice as well as training in clinical skills.
Nurses care for individuals of all ages and cultural backgrounds who are healthy and ill in a holistic manner based on the individual's physical, emotional, psychological, intellectual, social, and spiritual needs. The profession combines physical science, social science, nursing theory, and technology in caring for those individuals.
To work in the nursing profession, all nurses hold one or more credentials depending on their scope of practice and education. In the United States, a Licensed Practical Nurse (LPN) works independently or with a Registered Nurse (RN). The most significant difference between an LPN and RN is found in the requirements for entry to practice, which determines entitlement for their scope of practice.
RNs provide scientific, psychological, and technological knowledge in the care of patients and families in many health care settings. RNs may earn additional credentials or degrees.
In the United States, multiple educational paths will qualify a candidate to sit for the licensure examination as a RN. The Associate Degree in Nursing (ADN) is awarded to the nurse who has completed a two-year undergraduate academic degree awarded by community colleges, junior colleges, technical colleges, and bachelor's degree-granting colleges and universities upon completion of a course of study usually lasting two years.
It is also referred to as Associate in Nursing (AN), Associate of Applied Science in Nursing (AAS), or Associate of Science in Nursing (ASN). The Bachelor of Science in Nursing (BSN) is awarded to the nurse who has earned an American four-year academic degree in the science and principles of nursing, granted by a tertiary education university or similarly accredited school.
After completing either the LPN or either RN education programs in the United States, graduates are eligible to sit for a licensing examination to become a nurse, the passing of which is required for the nursing license. The National Licensure Examination (NCLEX) test is a standardized exam (including multiple choice, select all that apply, fill in the blank and "hot spot" questions) that nurses take to become licensed.
It costs two-hundred dollars to take the NCLEX. It examines a nurses ability to properly care for a client. Study books and practice tests are available for purchase.
Some nurses follow the traditional role of working in a hospital setting. Other options include: pediatrics, neonatal, maternity, OBGYN, geriatrics, ambulatory, and nurse anesthetists and informatics (eHealth). There are many other options nurses can explore depending on the type of degree and education acquired. RNs may also pursue different roles as advanced practice nurses.
Nurses are not doctors' assistants. This is possible in certain situations, but nurses more often are independently caring for their patients or assisting other nurses. RNs treat patients, record their medical history, provide emotional support, and provide follow-up care. Nurses also help doctors perform diagnostic tests. Nurses are almost always working on their own or with other nurses. Nurses will assist doctors in the emergency room or in trauma care when help is needed.
Gender issues:
Main article: Men in nursing
Despite equal opportunity legislation, nursing has continued to be a female-dominated profession. For instance, the male-to-female ratio of nurses is approximately 1:19 in Canada and the United States. This ratio is represented around the world.
Notable exceptions include Francophone Africa, which includes the countries of Benin, Burkina Faso, Cameroon, Chad, Congo, Côte d'Ivoire, the Democratic Republic of Congo, Djibouti, Guinea, Gabon, Mali, Mauritania, Niger, Rwanda, Senegal, and Togo, which all have more male than female nurses.
In Europe, in countries such as Spain, Portugal, Czech Republic and Italy, over 20% of nurses are male. In the United Kingdom, 11% of nurses and midwives registered with the Nursing and Midwifery Council (NMC) are male. The number of male registered nurses in the United States between 1980 and 2000s doubled.
Although females are more common, male nurses receive the same pay.
Click here for more about Nursing as applied world-wide.
___________________________________________________________________________
Nursing in the United States practice nursing in a wide variety of specialized products .
Types of Nurses:
Nursing in the United States is provided by several levels of professional and paraprofessional staff:
Nursing is a profession within the health care sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life.
Nurses may be differentiated from other health care providers by their approach to patient care and training, and scope of practice. Nurses practice in many specialties with differing levels of prescription authority.
Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. However, nurse practitioners are permitted by most jurisdictions to practice independently in a variety of settings.
Since the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient's family and other team members, that focuses on treating illness to improve quality of life. In the United States and the United Kingdom, advanced practice nurses, such as clinical nurse specialists and nurse practitioners, diagnose health problems and prescribe medications and other therapies, depending on individual state regulations.
Nurses may help coordinate the patient care performed by other members of a multidisciplinary health care team such as therapists, medical practitioners and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
Although nursing practice varies both through its various specialties and countries, these nursing organizations offer the following definitions:
Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups and communities, sick or well, and in all settings. Nursing includes the promotion of health, prevention of illness, and the care of ill, disabled and dying people.
Advocacy, promotion of a safe environment, research, participation in shaping health policy and in patient and health systems management, and education are also key nursing roles.
- International Council of Nurses. The use of clinical judgment in the provision of care to enable people to improve, maintain, or recover health, to cope with health problems, and to achieve the best possible quality of life, whatever their disease or disability, until death.
- Royal College of Nursing (2003) Nursing is the protection, promotion, and optimization of health and abilities; prevention of illness and injury; alleviation of suffering through the diagnosis and treatment of human responses; and advocacy in health care for individuals, families, communities, and populations.
- American Nurses Association The unique function of the nurse is to assist the individual, sick or well, in the performance of those activities contributing to health or its recovery (or to peaceful death) that he would perform unaided if he had the necessary strength, will or knowledge.
(The above by Virginia Avenel Henderson (November 30, 1897 – March 19, 1996) was an influential nurse, researcher, theorist and author.)
As a Profession:
The authority for the practice of nursing is based upon a social contract that delineates professional rights and responsibilities as well as mechanisms for public accountability. In almost all countries, nursing practice is defined and governed by law, and entrance to the profession is regulated at the national or state level.
The aim of the nursing community worldwide is for its professionals to ensure quality care for all, while maintaining their credentials, code of ethics, standards, and competencies, and continuing their education.
There are a number of educational paths to becoming a professional nurse, which vary greatly worldwide; all involve extensive study of nursing theory and practice as well as training in clinical skills.
Nurses care for individuals of all ages and cultural backgrounds who are healthy and ill in a holistic manner based on the individual's physical, emotional, psychological, intellectual, social, and spiritual needs. The profession combines physical science, social science, nursing theory, and technology in caring for those individuals.
To work in the nursing profession, all nurses hold one or more credentials depending on their scope of practice and education. In the United States, a Licensed Practical Nurse (LPN) works independently or with a Registered Nurse (RN). The most significant difference between an LPN and RN is found in the requirements for entry to practice, which determines entitlement for their scope of practice.
RNs provide scientific, psychological, and technological knowledge in the care of patients and families in many health care settings. RNs may earn additional credentials or degrees.
In the United States, multiple educational paths will qualify a candidate to sit for the licensure examination as a RN. The Associate Degree in Nursing (ADN) is awarded to the nurse who has completed a two-year undergraduate academic degree awarded by community colleges, junior colleges, technical colleges, and bachelor's degree-granting colleges and universities upon completion of a course of study usually lasting two years.
It is also referred to as Associate in Nursing (AN), Associate of Applied Science in Nursing (AAS), or Associate of Science in Nursing (ASN). The Bachelor of Science in Nursing (BSN) is awarded to the nurse who has earned an American four-year academic degree in the science and principles of nursing, granted by a tertiary education university or similarly accredited school.
After completing either the LPN or either RN education programs in the United States, graduates are eligible to sit for a licensing examination to become a nurse, the passing of which is required for the nursing license. The National Licensure Examination (NCLEX) test is a standardized exam (including multiple choice, select all that apply, fill in the blank and "hot spot" questions) that nurses take to become licensed.
It costs two-hundred dollars to take the NCLEX. It examines a nurses ability to properly care for a client. Study books and practice tests are available for purchase.
Some nurses follow the traditional role of working in a hospital setting. Other options include: pediatrics, neonatal, maternity, OBGYN, geriatrics, ambulatory, and nurse anesthetists and informatics (eHealth). There are many other options nurses can explore depending on the type of degree and education acquired. RNs may also pursue different roles as advanced practice nurses.
Nurses are not doctors' assistants. This is possible in certain situations, but nurses more often are independently caring for their patients or assisting other nurses. RNs treat patients, record their medical history, provide emotional support, and provide follow-up care. Nurses also help doctors perform diagnostic tests. Nurses are almost always working on their own or with other nurses. Nurses will assist doctors in the emergency room or in trauma care when help is needed.
Gender issues:
Main article: Men in nursing
Despite equal opportunity legislation, nursing has continued to be a female-dominated profession. For instance, the male-to-female ratio of nurses is approximately 1:19 in Canada and the United States. This ratio is represented around the world.
Notable exceptions include Francophone Africa, which includes the countries of Benin, Burkina Faso, Cameroon, Chad, Congo, Côte d'Ivoire, the Democratic Republic of Congo, Djibouti, Guinea, Gabon, Mali, Mauritania, Niger, Rwanda, Senegal, and Togo, which all have more male than female nurses.
In Europe, in countries such as Spain, Portugal, Czech Republic and Italy, over 20% of nurses are male. In the United Kingdom, 11% of nurses and midwives registered with the Nursing and Midwifery Council (NMC) are male. The number of male registered nurses in the United States between 1980 and 2000s doubled.
Although females are more common, male nurses receive the same pay.
Click here for more about Nursing as applied world-wide.
___________________________________________________________________________
Nursing in the United States practice nursing in a wide variety of specialized products .
Types of Nurses:
Nursing in the United States is provided by several levels of professional and paraprofessional staff:
There is currently two Doctorial Nurses- Doctor of Nursing Practice, DNP (usually involved in community projects and professional nursing academia) Doctorate of Philosophy, PhD
(usually involved in the fundamentals and theory of nursing and research)
Education:
Registered nurses generally receive their basic preparation through one of four basic avenues:
There are also special programs for "LPN to RN", for LPNs seeking an RN degree. There are also accelerated baccalaureate nursing programs that take 1.5 to 2 years for people who hold undergraduate degrees in other disciplines, such as respiratory therapists and paramedics/military medics.
Graduates of all programs, once licensed, are eligible for employment as entry-level staff nurses.
Prerequisites for nursing school depend on the school, with baccalaureate programs requiring more courses, in general, than associate degree programs. Usual courses include three years of math, three years of science, including biology and chemistry, four years of English and two years of language.
Additionally, human development, human anatomy with lab, human physiology with lab, microbiology with lab, nutritional science and English composition may be required. Applicants are usually expected to have a high grade point average, especially in the core prerequisites of anatomy, microbiology, chemistry and physiology.
A typical course of study at any level typically includes such topics as:
All pathways into practice require that the candidate receive clinical training in nursing. Care is delivered by the student nurses under academic supervision in hospital and in other practice settings. Clinical courses typically include:
While in clinical training, student nurses are identified by a special uniform to distinguish them from licensed professionals.
In many nursing programs in the United States, a computerized exam is given before, during, and upon completion to evaluate the student and nursing program outcomes. This exam, upon completion of the nursing program, measures a student's readiness for the NCLEX-RN or NCLEX-PN state board license exam.
The exam identifies strengths and weaknesses and areas for remediation prior to taking the state board exam. This is not a requirement of all nursing programs in the United States, but has increased its usage in the past three to four years.
It is common for RNs to seek additional education to earn a Master of Science in Nursing or Doctor of Nursing Science to prepare for leadership or advanced practice roles within nursing. Management and teaching positions increasingly require candidates to hold an advanced degree in nursing.
Many hospitals offer tuition reimbursement or assistance to nurses who want to continue their education beyond their basic preparation.
Many nurses pursue voluntary specialty certification through professional organizations and certifying bodies in order to demonstrate advanced knowledge and skills in their area of expertise.
Most U.S. states and territories require RNs to graduate from an accredited nursing program which allows the candidate to sit for the NCLEX-RN, a standardized examination administered through the National Council of State Nursing Boards. Successful completion of the NCLEX-RN is required for state licensure as an RN.
Nurses from other countries are required to be proficient in English and have their educational credentials evaluated by an association known as the Commission on Graduates of Foreign Nursing Schools prior to being permitted to take the U.S. licensing exam.
Legal regulation:
Government regulates the profession of nursing to protect the public.
The individual states have authority over nursing practice. The scope of practice is defined by state laws and by regulations administered by State Nursing Boards.
Many states have adopted the Model Nursing Practice Act and Model Nursing Administrative Rules created by the National Council of State Nursing Boards (NCSNB).
In addition, many state nursing boards model their licensure requirements on the Uniform Core Licensure Requirements which set forth competency development and competency assessment principles.
Nurses may be licensed in more than one state, either by examination or endorsement of a license issued by another state. In addition, the states which have adopted the Nurse Licensure Compact allow nurses licensed in one of the states to practice in all of them through mutual recognition of licensing.
Licenses must be periodically renewed. Some states require continuing education in order to renew licenses.
Demand for nurses in the US:
The demand for nurses has been on the rise for several years, spurred by various economic and demographic factors. Demand for nurses is projected to increase for the foreseeable future (an increase of 23% between 2006 and 2016, according to the US Department of Labor).
Candidates for nursing jobs that are in highest demand include registered nurses, licensed practical nurses, certified nurse assistants, and certified medical assistants.
The Department of Labor's estimated increase percentage per nurse employer type is:
Nursing degrees in the United States:
In the United States, Nursing is the largest healthcare profession, with more than 3.1 million registered nurses.
Between 2012 and 2022, employment for nurses is projected to grow by 19 percent, which is more than any other profession.
Nurses make up the largest component of staff in hospitals but are also able to provide care in clinic settings, patient's homes, schools, nursing homes, public health agencies, and mental health centers. In addition, nurses can be found in the military, in industry, nursing education, and do health care research.
Nurses in these various roles and settings can provide direct patient care and case management, but also develop and establish nursing practice and quality standards within complex healthcare systems.
As each degree can provide a different level of care for patients and function in vastly different roles, it is important to differentiate between them. The levels of nursing degrees have different educational requirements, licensing, and credentialing that can vary state to state.
Licensed Practical Nurse:
The education required for a Licensed Practical Nurse/Licensed Vocational Nurse is the completion of a 12-18 month program, typically at a technical college. The program focuses on task activities and prepares the nurse for the National Council Licensure Examination for Licensed Practical Nurses (NCLEX). Requirements for taking the NCLEX-PN include having a high school diploma or equivalent and successful completion of an accredited practical/vocational nursing program.
LPN/LVNs work in a variety of settings including hospitals, clinics, nursing homes, rehabilitation centers, schools, and individual or group homes. Scope of practice for LPN/LVNs is defined by individual states, but each organization may narrow the scope of the LPN/LVN.
Hospital-Based Diploma Nurse:
Hospital-based diplomas were historically the primary form of nursing education, first appearing in the early 20th century. The number of facilities offering this degree as well as the number of nurses obtaining their education through them have declined since the 1970s due to the growth of Associate Degree in Nursing and Bachelor of Science in Nursing programs at colleges and universities, as well as increasing financial constraints on hospitals and the healthcare systems.
Diploma programs were the most abundant in the 1950s and 1960s, with nearly 1,300 diploma programs active nationwide. Presently, less than 10 percent of nursing degree programs are diploma programs, which produce less than 6 percent of registered nurses.
The majority of the remaining diploma programs in the United States are concentrated in the Midwest and on the East Coast. Programs for hospital diplomas are traditionally sponsored and run by hospitals in the community, as their name implies.
Courses are taught proximal to and in conjunction with the hospital, where students have practical application of their skills on the units and wards in the sponsoring facility.
Diploma programs typically have a strong focus on practical application of skills, with a larger percentage of time spent on the “hands-on” component of learning. Students attend classes for two to three years, at the completion of which they take the National Council Licensure Examination for Registered Nurses (NCLEX-RN) certifying exam, a standard exam for all practicing registered nurses.
Students graduate with a diploma in nursing, and passing of the NCLEX-RN allows for certification and state licensure, which permits the graduate to practice as a full registered nurse within his or her state's statutes. Coursework taken in a diploma nursing program can frequently be used for credits toward nursing degrees such as a BSN or ADN.
Associate Degree in Nursing:
An Associate Degree in Nursing (ADN) is the minimum educational requirement to become a registered nurse in the United States. All ADN prepared nurses are credentialed through individual state nursing boards after passing the NCLEX-RN. In order to be eligible to take the NCLEX-RN exam, candidates must have a high school diploma or its equivalent and a degree from a board of nursing approved nursing program.
ADN nursing programs typically take two years to complete but courses required differ by state. The standard course requirement includes anatomy, physiology, microbiology, chemistry, nutrition, psychology. Background checks are also performed on all candidates prior to granting license. Associate degree nurses are able to work in both outpatient and inpatient settings.
Of the almost 3.1 million registered nurses in the United States, 36.1 percent of them have an associate degrees in nursing.
Bachelor of Science Degree in Nursing:
Bachelor of Science in Nursing (BSN) degrees prepare nurses for a wide variety of professional roles and graduate study within nursing. It is typically acquired through a four-year program at a college or university.
Baccalaureate programs include a variety of liberal arts courses and professional education and training in the nursing field. It contains additional education beyond that of an ADN that often includes physical and social sciences, communication, leadership, and critical thinking.
There are 674 BSN programs in the United States. BSN programs are approved by each state's individual board of nursing that allows students to sit for the NCLEX-RN examination to obtain a license as a registered nurse.
Some states have accelerated programs called “RN-to-BSN” or “BSN completion” for registered nurses with associate degrees wanting to obtain their bachelor's degree in nursing.
In 2010, the Institute of Medicine called for 80 percent of nurses in the U.S. to be baccalaureate trained by the year 2020, and this has created a push for healthcare organizations to make a BSN a hiring requirement for registered nurses and instituting education assistance programs for those with associate degrees.
Master of Science Degree in Nursing:
The Master of Science in Nursing (MSN) is an advanced degree that allows for a more specialized role in nursing. The master's prepared nurse has a wide array of careers that he or she might aspire to fill. Career paths include certified nurse practitioner (CNP), certified nurse anesthetist (CRNA), clinical nurse specialist (CNS) or certified nurse midwife (CNM).
Some other areas the MSN prepared nurse might focus are in public health, business administration or health administration. Education curriculum may vary between 18 and 24 months of full-time graduate level studies, with program length determined by the specified field.
The certification exams for a master's prepared nurse are dependent upon the role being pursued. For example, the CNM takes the American Midwifery Certification Board exam and nurse administrators may receive their certification from the American Nurses Credentialing Center (ANCC).
Master's prepared nurses are trained in advanced assessment, counseling of patients, management, leadership, research and education. They may work in both inpatient and outpatient settings as well as educational institutions, and scope of practice may vary state-by-state.
Doctor of Nursing Practice Degree:
The scope of practice for a Doctor of Nursing Practice (DNP) includes assessing, diagnosing, prescribing, consulting, screening, educating, initiating referrals and the coordination of patient care.
There are numerous specialties DNPs may pursue including:
Specific practice guidelines can vary by state and area of practice. In order to become a DNP, one would need to obtain his or her doctorate in nursing practice. Specific program requirements vary with each program.
After completing the doctorate program, one must pass the specific certification exam that corresponds to his or her specialty prior to initiating practice. In 2014 there were 3,065 DNP graduates.
Doctor of Philosophy in Nursing:
Nurses who hold a Doctor of Philosophy Degree in Nursing (PhD), are less about hands-on patient care and more about the abstract thinking that helps move the profession forward. A nurse with a PhD has the training needed to conduct research aimed at changing nursing science or practice.
The education for a PhD in nursing includes courses in scientific research methodologies and statistics and philosophy of science. Either a BSN or MSN degree are required for entry into a PhD program. Credit requirements vary by program and state and typically take anywhere from three to five years to complete.
PhD programs do not have clinical practice hour requirements like DNP programs. PhD prepared nurses teach as academic faculty, conduct research, evaluate programs, hold academic and leadership positions, write books, and lead health care organizations.
See also:
History of nursing in the United States:
The History of nursing in the United States focuses on the professionalization of nursing since the Civil War.
Click on any of the following blue hyperlinks for more about the History of Nursing:
(usually involved in the fundamentals and theory of nursing and research)
Education:
Registered nurses generally receive their basic preparation through one of four basic avenues:
- Diploma in Nursing: Graduation with a three-year certificate from a hospital-based school of nursing. Few of these programs remain in the U.S. and the proportion of nurses practicing with a diploma is rapidly decreasing.
- Associate of Science in Nursing: Graduation from a degree-granting nursing program conferring the degree of ASN/AAS or ADN in nursing. This involves two to three years of college level study with a strong emphasis on clinical knowledge and skills.
- Bachelor of Science in Nursing: Graduation from a university, from a four- or five-year program conferring the BSN or BN degree with enhanced emphasis on leadership and research as well as clinically focused courses.
- Generic-entry Master of Science in Nursing: Graduation from a university, one to three-year program conferring the MS/MSN degree with emphasis on leadership and research as well as clinically focused courses for students who hold a bachelor's degree or higher in an academic field other than nursing.
There are also special programs for "LPN to RN", for LPNs seeking an RN degree. There are also accelerated baccalaureate nursing programs that take 1.5 to 2 years for people who hold undergraduate degrees in other disciplines, such as respiratory therapists and paramedics/military medics.
Graduates of all programs, once licensed, are eligible for employment as entry-level staff nurses.
Prerequisites for nursing school depend on the school, with baccalaureate programs requiring more courses, in general, than associate degree programs. Usual courses include three years of math, three years of science, including biology and chemistry, four years of English and two years of language.
Additionally, human development, human anatomy with lab, human physiology with lab, microbiology with lab, nutritional science and English composition may be required. Applicants are usually expected to have a high grade point average, especially in the core prerequisites of anatomy, microbiology, chemistry and physiology.
A typical course of study at any level typically includes such topics as:
- anatomy and physiology,
- epidemiology,
- pharmacology and medication administration,
- psychology,
- ethics,
- nursing theory
- and legal issues in nursing.
All pathways into practice require that the candidate receive clinical training in nursing. Care is delivered by the student nurses under academic supervision in hospital and in other practice settings. Clinical courses typically include:
- Maternal-child nursing.
- Pediatric nursing.
- Adult medical-surgical nursing.
- Geriatric nursing.
- Psychiatric nursing.
While in clinical training, student nurses are identified by a special uniform to distinguish them from licensed professionals.
In many nursing programs in the United States, a computerized exam is given before, during, and upon completion to evaluate the student and nursing program outcomes. This exam, upon completion of the nursing program, measures a student's readiness for the NCLEX-RN or NCLEX-PN state board license exam.
The exam identifies strengths and weaknesses and areas for remediation prior to taking the state board exam. This is not a requirement of all nursing programs in the United States, but has increased its usage in the past three to four years.
It is common for RNs to seek additional education to earn a Master of Science in Nursing or Doctor of Nursing Science to prepare for leadership or advanced practice roles within nursing. Management and teaching positions increasingly require candidates to hold an advanced degree in nursing.
Many hospitals offer tuition reimbursement or assistance to nurses who want to continue their education beyond their basic preparation.
Many nurses pursue voluntary specialty certification through professional organizations and certifying bodies in order to demonstrate advanced knowledge and skills in their area of expertise.
Most U.S. states and territories require RNs to graduate from an accredited nursing program which allows the candidate to sit for the NCLEX-RN, a standardized examination administered through the National Council of State Nursing Boards. Successful completion of the NCLEX-RN is required for state licensure as an RN.
Nurses from other countries are required to be proficient in English and have their educational credentials evaluated by an association known as the Commission on Graduates of Foreign Nursing Schools prior to being permitted to take the U.S. licensing exam.
Legal regulation:
Government regulates the profession of nursing to protect the public.
The individual states have authority over nursing practice. The scope of practice is defined by state laws and by regulations administered by State Nursing Boards.
Many states have adopted the Model Nursing Practice Act and Model Nursing Administrative Rules created by the National Council of State Nursing Boards (NCSNB).
In addition, many state nursing boards model their licensure requirements on the Uniform Core Licensure Requirements which set forth competency development and competency assessment principles.
Nurses may be licensed in more than one state, either by examination or endorsement of a license issued by another state. In addition, the states which have adopted the Nurse Licensure Compact allow nurses licensed in one of the states to practice in all of them through mutual recognition of licensing.
Licenses must be periodically renewed. Some states require continuing education in order to renew licenses.
Demand for nurses in the US:
The demand for nurses has been on the rise for several years, spurred by various economic and demographic factors. Demand for nurses is projected to increase for the foreseeable future (an increase of 23% between 2006 and 2016, according to the US Department of Labor).
Candidates for nursing jobs that are in highest demand include registered nurses, licensed practical nurses, certified nurse assistants, and certified medical assistants.
The Department of Labor's estimated increase percentage per nurse employer type is:
- 25% - Offices of physicians
- 23% - Home health care services
- 34% - Outpatient care centers, except mental health and substance abuse
- 33% - Employment services
- 23% - General medical and surgical hospitals, public and private
- 23% - Nursing care facilities
Nursing degrees in the United States:
In the United States, Nursing is the largest healthcare profession, with more than 3.1 million registered nurses.
Between 2012 and 2022, employment for nurses is projected to grow by 19 percent, which is more than any other profession.
Nurses make up the largest component of staff in hospitals but are also able to provide care in clinic settings, patient's homes, schools, nursing homes, public health agencies, and mental health centers. In addition, nurses can be found in the military, in industry, nursing education, and do health care research.
Nurses in these various roles and settings can provide direct patient care and case management, but also develop and establish nursing practice and quality standards within complex healthcare systems.
As each degree can provide a different level of care for patients and function in vastly different roles, it is important to differentiate between them. The levels of nursing degrees have different educational requirements, licensing, and credentialing that can vary state to state.
Licensed Practical Nurse:
The education required for a Licensed Practical Nurse/Licensed Vocational Nurse is the completion of a 12-18 month program, typically at a technical college. The program focuses on task activities and prepares the nurse for the National Council Licensure Examination for Licensed Practical Nurses (NCLEX). Requirements for taking the NCLEX-PN include having a high school diploma or equivalent and successful completion of an accredited practical/vocational nursing program.
LPN/LVNs work in a variety of settings including hospitals, clinics, nursing homes, rehabilitation centers, schools, and individual or group homes. Scope of practice for LPN/LVNs is defined by individual states, but each organization may narrow the scope of the LPN/LVN.
Hospital-Based Diploma Nurse:
Hospital-based diplomas were historically the primary form of nursing education, first appearing in the early 20th century. The number of facilities offering this degree as well as the number of nurses obtaining their education through them have declined since the 1970s due to the growth of Associate Degree in Nursing and Bachelor of Science in Nursing programs at colleges and universities, as well as increasing financial constraints on hospitals and the healthcare systems.
Diploma programs were the most abundant in the 1950s and 1960s, with nearly 1,300 diploma programs active nationwide. Presently, less than 10 percent of nursing degree programs are diploma programs, which produce less than 6 percent of registered nurses.
The majority of the remaining diploma programs in the United States are concentrated in the Midwest and on the East Coast. Programs for hospital diplomas are traditionally sponsored and run by hospitals in the community, as their name implies.
Courses are taught proximal to and in conjunction with the hospital, where students have practical application of their skills on the units and wards in the sponsoring facility.
Diploma programs typically have a strong focus on practical application of skills, with a larger percentage of time spent on the “hands-on” component of learning. Students attend classes for two to three years, at the completion of which they take the National Council Licensure Examination for Registered Nurses (NCLEX-RN) certifying exam, a standard exam for all practicing registered nurses.
Students graduate with a diploma in nursing, and passing of the NCLEX-RN allows for certification and state licensure, which permits the graduate to practice as a full registered nurse within his or her state's statutes. Coursework taken in a diploma nursing program can frequently be used for credits toward nursing degrees such as a BSN or ADN.
Associate Degree in Nursing:
An Associate Degree in Nursing (ADN) is the minimum educational requirement to become a registered nurse in the United States. All ADN prepared nurses are credentialed through individual state nursing boards after passing the NCLEX-RN. In order to be eligible to take the NCLEX-RN exam, candidates must have a high school diploma or its equivalent and a degree from a board of nursing approved nursing program.
ADN nursing programs typically take two years to complete but courses required differ by state. The standard course requirement includes anatomy, physiology, microbiology, chemistry, nutrition, psychology. Background checks are also performed on all candidates prior to granting license. Associate degree nurses are able to work in both outpatient and inpatient settings.
Of the almost 3.1 million registered nurses in the United States, 36.1 percent of them have an associate degrees in nursing.
Bachelor of Science Degree in Nursing:
Bachelor of Science in Nursing (BSN) degrees prepare nurses for a wide variety of professional roles and graduate study within nursing. It is typically acquired through a four-year program at a college or university.
Baccalaureate programs include a variety of liberal arts courses and professional education and training in the nursing field. It contains additional education beyond that of an ADN that often includes physical and social sciences, communication, leadership, and critical thinking.
There are 674 BSN programs in the United States. BSN programs are approved by each state's individual board of nursing that allows students to sit for the NCLEX-RN examination to obtain a license as a registered nurse.
Some states have accelerated programs called “RN-to-BSN” or “BSN completion” for registered nurses with associate degrees wanting to obtain their bachelor's degree in nursing.
In 2010, the Institute of Medicine called for 80 percent of nurses in the U.S. to be baccalaureate trained by the year 2020, and this has created a push for healthcare organizations to make a BSN a hiring requirement for registered nurses and instituting education assistance programs for those with associate degrees.
Master of Science Degree in Nursing:
The Master of Science in Nursing (MSN) is an advanced degree that allows for a more specialized role in nursing. The master's prepared nurse has a wide array of careers that he or she might aspire to fill. Career paths include certified nurse practitioner (CNP), certified nurse anesthetist (CRNA), clinical nurse specialist (CNS) or certified nurse midwife (CNM).
Some other areas the MSN prepared nurse might focus are in public health, business administration or health administration. Education curriculum may vary between 18 and 24 months of full-time graduate level studies, with program length determined by the specified field.
The certification exams for a master's prepared nurse are dependent upon the role being pursued. For example, the CNM takes the American Midwifery Certification Board exam and nurse administrators may receive their certification from the American Nurses Credentialing Center (ANCC).
Master's prepared nurses are trained in advanced assessment, counseling of patients, management, leadership, research and education. They may work in both inpatient and outpatient settings as well as educational institutions, and scope of practice may vary state-by-state.
Doctor of Nursing Practice Degree:
The scope of practice for a Doctor of Nursing Practice (DNP) includes assessing, diagnosing, prescribing, consulting, screening, educating, initiating referrals and the coordination of patient care.
There are numerous specialties DNPs may pursue including:
- Acute Care Nurse Practitioner,
- Adult Nurse Practitioner,
- Adult-gerontology nurse practitioner (acute or primary care),
- Adult Psychiatric- Mental Health Nurse Practitioner,
- Family Nurse Practitioner,
- Gerontological Nurse Practitioner,
- Pediatric Nurse Practitioner (acute or primary care),
- and School Nurse Practitioner.
Specific practice guidelines can vary by state and area of practice. In order to become a DNP, one would need to obtain his or her doctorate in nursing practice. Specific program requirements vary with each program.
After completing the doctorate program, one must pass the specific certification exam that corresponds to his or her specialty prior to initiating practice. In 2014 there were 3,065 DNP graduates.
Doctor of Philosophy in Nursing:
Nurses who hold a Doctor of Philosophy Degree in Nursing (PhD), are less about hands-on patient care and more about the abstract thinking that helps move the profession forward. A nurse with a PhD has the training needed to conduct research aimed at changing nursing science or practice.
The education for a PhD in nursing includes courses in scientific research methodologies and statistics and philosophy of science. Either a BSN or MSN degree are required for entry into a PhD program. Credit requirements vary by program and state and typically take anywhere from three to five years to complete.
PhD programs do not have clinical practice hour requirements like DNP programs. PhD prepared nurses teach as academic faculty, conduct research, evaluate programs, hold academic and leadership positions, write books, and lead health care organizations.
See also:
- National Council of State Boards of Nursing/NCLEX
- American Association of Colleges of Nursing
- Institute of Medicine
History of nursing in the United States:
The History of nursing in the United States focuses on the professionalization of nursing since the Civil War.
Click on any of the following blue hyperlinks for more about the History of Nursing:
- Origins
- Hospitals including Religious hospitals
- Public health
- Military nursing
- American Nurses Association
- World War II
- Postwar transformation
- Since 1964
- See also:
mHealth: Solutions for Medical Care involving your Mobile Device Pictured below: MyCareLink Monitor for Cardiac Pacemakers: see YouTube Video above
[Your WebHost: when researching this topic, I quickly realized that I have been a beneficiary of mHealth technology for some time: my Cardiologist had installed a cardiac pacemaker a couple of years ago, and I use the Medtronic MyCareLink Monitor along with my smartphone (as mentioned in the first YouTube Video above), to track its performance!]
mHealth (also written as m-health or mhealth) is an abbreviation for mobile health, a term used for the practice of medicine and public health supported by mobile devices. The term is most commonly used in reference to using mobile communication devices, such as mobile phones, tablet computers and PDAs, and wearable devices such as smart watches, for health services, information, and data collection.
The mHealth field has emerged as a sub-segment of eHealth, the use of information and communication technology (ICT), such as computers, mobile phones, communications satellite, patient monitors, etc., for health services and information.
mHealth applications include the use of mobile devices in collecting community and clinical health data, delivery of healthcare information to practitioners, researchers and patients, real-time monitoring of patient vital signs, the direct provision of care (via mobile telemedicine) as well as training and collaboration of health workers.
While mHealth certainly has application for industrialized nations, the field has emerged in recent years as largely an application for developing countries, stemming from the rapid rise of mobile phone penetration in low-income nations. The field, then, largely emerges as a means of providing greater access to larger segments of a population in developing countries, as well as improving the capacity of health systems in such countries to provide quality healthcare.
Within the mHealth space, projects operate with a variety of objectives, including increased access to healthcare and health-related information (particularly for hard-to-reach populations); improved ability to diagnose and track diseases; timelier, more actionable public health information; and expanded access to ongoing medical education and training for health workers.
According to an analyst firm, around 2.8 million patients worldwide were using a home monitoring service based on equipment with integrated connectivity at the end of 2012. The figure does not include patients that use monitoring devices connected to a PC or mobile phone. It only includes systems that rely on monitors with integrated connectivity or systems that use monitoring hubs with integrated cellular or fixed-line modems.
It forecast that the number of home monitoring systems with integrated communication capabilities will grow at a compound annual growth rate (CAGR) of 26.9 percent between 2011 and 2017 reaching 9.4 million connections globally by the end of the forecast period.
The number of these devices that have integrated cellular connectivity increased from 0.73 million in 2011 to about 1.03 million in 2012, and is projected to grow at a CAGR of 46.3 percent to 7.10 million in 2017.
A growing percentage of health-related smartphone apps are available, and some estimates predicted that 500 million patients would be using such apps by the year 2015.
While there are concerns about the accuracy and unregulated status of health apps, mHealth broadly encompasses the use of mobile telecommunication and multimedia technologies as they are integrated within increasingly mobile and wireless health care delivery systems.
The field broadly encompasses the use of mobile telecommunication and multimedia technologies in health care delivery. The term mHealth was coined by Robert Istepanian as use of "emerging mobile communications and network technologies for healthcare".
A definition used at the 2010 mHealth Summit of the Foundation for the National Institutes of Health (FNIH) was "the delivery of healthcare services via mobile communication devices".
While there are some projects that are considered solely within the field of mHealth, the linkage between mHealth and eHealth is unquestionable. For example, an mHealth project that uses mobile phones to access data on HIV/AIDS rates would require an eHealth system in order to manage, store, and assess the data. Thus, eHealth projects many times operate as the backbone of mHealth projects.
In a similar vein, while not clearly bifurcated by such a definition, eHealth can largely be viewed as technology that supports the functions and delivery of healthcare, while mHealth rests largely on providing healthcare access.
Because mHealth is by definition based on mobile technology such as smartphones, healthcare, through information and delivery, can better reach areas, people, and/or healthcare practitioners with previously limited exposure to certain aspects of healthcare.
Motivation:
mHealth is one aspect of eHealth that is pushing the limits of how to acquire, transport, store, process, and secure the raw and processed data to deliver meaningful results. mHealth offers the ability of remote individuals to participate in the health care value matrix, which may not have been possible in the past.
Participation does not imply just consumption of health care services. In many cases remote users are valuable contributors to gather data regarding disease and public health concerns such as outdoor pollution, drugs and violence.
The motivation behind the development of the mHealth field arises from two factors. The first factor concerns the myriad constraints felt by healthcare systems of developing nations.
These constraints include high population growth, a high burden of disease prevalence, low health care workforce, large numbers of rural inhabitants, and limited financial resources to support healthcare infrastructure and health information systems.
The second factor is the recent rapid rise in mobile phone penetration in developing countries to large segments of the healthcare workforce, as well as the population of a country as a whole. With greater access to mobile phones to all segments of a country, including rural areas, the potential of lowering information and transaction costs in order to deliver healthcare improves.
The combination of these two factors has motivated much discussion of how greater access to mobile phone technology can be leveraged to mitigate the numerous pressures faced by developing countries' healthcare systems. Both factors are discussed here.
Healthcare in low- and middle-income countries:
Middle income and especially low-income countries face a plethora of constraints in their healthcare systems. These countries face a severe lack of human and physical resources, as well as some of the largest burdens of disease, extreme poverty, and large population growth rates. Additionally, healthcare access to all reaches of society is generally low in these countries.
According to a World Health Organization (WHO) report from June 2011, higher-income countries show more mHealth activity than do lower-income countries (as consistent with eHealth trends in general).
Countries in the European Region are currently the most active and those in the African Region the least active. The WHO report findings also included that mHealth is most easily incorporated into processes and services that historically use voice communication through conventional telephone networks. The report was the result of a mHealth survey module designed by researchers at the Earth Institute's Center for Global Health and Economic Development, Columbia University.
The WHO notes an extreme deficit within the global healthcare workforce. The WHO notes critical healthcare workforce shortages in 57 countries—most of which are characterized as developing countries—and a global deficit of 2.4 million doctors, nurses, and midwives.
The WHO, in a study of the healthcare workforce in 12 countries of Africa, finds an average density of physicians, nurses and midwives per 1000 population of 0.64. The density of the same metric is four times as high in the United States, at 2.6.
The burden of disease is additionally much higher in low- and middle-income countries than high-income countries. The burden of disease, measured in disability-adjusted life year (DALY), which can be thought of as a measurement of the gap between current health status and an ideal situation where everyone lives into old age, free of disease and disability, is about five times higher in Africa than in high-income countries.
In addition, low- and middle-income countries are forced to face the burdens of both extreme poverty and the growing incidence of chronic diseases, such as diabetes and heart disease, an effect of new-found (relative) affluence.
Considering poor infrastructure and low human resources, the WHO notes that the healthcare workforce in sub-Saharan Africa would need to be scaled up by as much as 140% to attain international health development targets such as those in the Millennium Declaration.
The WHO, in reference to the healthcare condition in sub-saharan Africa, states:
Mobile technology has made a recent and rapid appearance into low- and middle-income nations. While, in the mHealth field, mobile technology usually refers to mobile phone technology, the entrance of other technologies into these nations to facilitate healthcare are also discussed here.
Health and development:
The link between health and development can be found in three of the Millennium Development Goals (MDGs), as set forth by the United Nations Millennium Declaration in 2000. The MDGs that specifically address health include reducing child mortality; improving maternal health; combating HIV and AIDS, malaria, and other diseases; and increasing access to safe drinking water.
A progress report published in 2006 indicates that childhood immunization and deliveries by skilled birth attendants are on the rise, while many regions continue to struggle to achieve reductions in the prevalence of the diseases of poverty including malaria, HIV and AIDS and tuberculosis.
Healthcare in developed countries:
In developed countries, healthcare systems have different policies and goals in relation to the personal and population health care goals.
In US and EU many patients and consumers use their cell phones and tablets to access health information and look for healthcare services. In parallel the number of mHealth applications grew significantly the last years.
Doctors, nurses and clinicians use mobile devices to access patient information and other databases and resources.
Technology and Market:
Basic SMS functions and real-time voice communication serve as the backbone and the current most common use of mobile phone technology. The broad range of potential benefits to the health sector that the simple functions of mobile phones can provide should not be understated.
The appeal of mobile communication technologies is that they enable communication in motion, allowing individuals to contact each other irrespective of time and place. This is particularly beneficial for work in remote areas where the mobile phone, and now increasingly wireless infrastructure, is able to reach more people, faster. As a result of such technological advances, the capacity for improved access to information and two-way communication becomes more available at the point of need.
Mobile phones:
With the global mobile phone penetration rate drastically increasing over the last decade, mobile phones have made a recent and rapid entrance into many parts of the low- and middle-income world. Improvements in telecommunications technology infrastructure, reduced costs of mobile handsets, and a general increase in non-food expenditure have influenced this trend.
Low- and middle-income countries are utilizing mobile phones as "leapfrog technology" (see leapfrogging). That is, mobile phones have allowed many developing countries, even those with relatively poor infrastructure, to bypass 20th century fixed-line technology and jump to modern mobile technology.
The number of global mobile phone subscribers in 2007 was estimated at 3.1 billion of an estimated global population of 6.6 billion (47%). These figures are expected to grow to 4.5 billion by 2012, or a 64.7% mobile penetration rate. The greatest growth is expected in Asia, the Middle East, and Africa.
In many countries, the number of mobile phone subscribers has bypassed the number of fixed-line telephones; this is particularly true in developing countries. Globally, there were 4.1 billion mobile phones in use in December 2008. See List of countries by number of mobile phones in use.
While mobile phone penetration rates are on the rise, globally, the growth within countries is not generally evenly distributed. In India, for example, while mobile penetration rates have increased markedly, by far the greatest growth rates are found in urban areas. Mobile penetration, in September 2008, was 66% in urban areas, while only 9.4% in rural areas.
The all India average was 28.2% at the same time. So, while mobile phones may have the potential to provide greater healthcare access to a larger portion of a population, there are certainly within-country equity issues to consider.
Mobile phones are spreading because the cost of mobile technology deployment is dropping and people are, on average, getting wealthier in low- and middle-income nations.
Vendors, such as Nokia, are developing cheaper infrastructure technologies (CDMA) and cheaper phones (sub $50–100, such as Sun's Java phone). Non-food consumption expenditure is increasing in many parts of the developing world, as disposable income rises, causing a rapid increase spending on new technology, such as mobile phones.
In India, for example, consumers have become and continue to become wealthier. Consumers are shifting their expenditure from necessity to discretionary. For example, on average, 56% of Indian consumers' consumption went towards food in 1995, compared to 42% in 2005.
The number is expected to drop to 34% by 2015. That being said, although total share of consumption has declined, total consumption of food and beverages increased 82% from 1985 to 2005, while per-capita consumption of food and beverages increased 24%. Indian consumers are getting wealthier and they are spending more and more, with a greater ability to spend on new technologies.
Smartphones:
More advanced mobile phone technologies are enabling the potential for further healthcare delivery. Smartphone technologies are in now in the hands of a large number of physicians and other healthcare workers in low- and middle-income countries.
Although far from ubiquitous, the spread of smartphone technologies opens up doors for mHealth projects such as technology-based diagnosis support, remote diagnostics and telemedicine, web browsing, GPS navigation, access to web-based patient information, post-visit patient surveillance, and decentralized health management information systems (HMIS).
While uptake of smartphone technology by the medical field has grown in low- and middle-income countries, it is worth noting that the capabilities of mobile phones in low- and middle-income countries has not reached the sophistication of those in high-income countries.
The infrastructure that enables web browsing, GPS navigation, and email through smartphones is not as well developed in much of the low- and middle-income countries. Increased availability and efficiency in both voice and data-transfer systems in addition to rapid deployment of wireless infrastructure will likely accelerate the deployment of mobile-enabled health systems and services throughout the world.
Other technologies:
Beyond mobile phones, wireless-enabled laptops and specialized health-related software applications are currently being developed, tested, and marketed for use in the mHealth field.
Many of these technologies, while having some application to low- and middle-income nations, are developing primarily in high-income countries. However, with broad advocacy campaigns for free and open source software (FOSS), applications are beginning to be tailored for and make inroads in low- and middle-income countries.
Some other mHealth technologies include:
Mobile device operating system technology:
Technologies relate to the operating systems that orchestrate mobile device hardware while maintaining confidentiality, integrity and availability are required to build trust. This may foster greater adoption of mHealth technologies and services, by exploiting lower cost multi purpose mobile devices such as tablets, PCs, and smartphones.
Operating systems that control these emerging classes of devices include Google's Android, Apple's iPhone OS, Microsoft's Windows Mobile, and RIM's BlackBerry OS.
Operating systems must be agile and evolve to effectively balance and deliver the desired level of service to an application and end user, while managing display real estate, power consumption and security posture. As advances in capabilities such as integrating voice, video and Web 2.0 collaboration tools into mobile devices, significant benefits can be achieved in the delivery of health care services.
New sensor technologies such as HD video and audio capabilities, accelerometers, GPS, ambient light detectors, barometers and gyroscopes can enhance the methods of describing and studying cases, close to the patient or consumer of the health care service. This could include diagnosis, education, treatment and monitoring.
Air quality sensing technologies:
Environmental conditions have a significant impact to public health. Per the World Health Organization, outdoor air pollution accounts for about 1.4% of total mortality. Utilizing Participatory sensing technologies in mobile telephone, public health research can exploit the wide penetration of mobile devices to collect air measurements, which can be utilized to assess the impact of pollution.
Projects such as the Urban Atmospheres are utilizing embedded technologies in mobile phones to acquire real time conditions from millions of user mobile phones. By aggregating this data, public health policy shall be able to craft initiatives to mitigate risk associated with outdoor air pollution.
Data:
Data has become an especially important aspect of mHealth. Data collection requires both the collection device (mobile phones, computer, or portable device) and the software that houses the information. Data is primarily focused on visualizing static text but can also extend to interactive decision support algorithms, other visual image information, and also communication capabilities through the integration of e-mail and SMS features.
Integrating use of GIS and GPS with mobile technologies adds a geographical mapping component that is able to "tag" voice and data communication to a particular location or series of locations. These combined capabilities have been used for emergency health services as well as for disease surveillance, health facilities and services mapping, and other health-related data collection.
Applications:
While others exist, the 2009 UN Foundation and Vodafone Foundation report presents seven application categories within the mHealth field:
Each application category as well as a specific project within the category will be described.
Education and awareness:
Education and awareness programs within the mHealth field are largely about the spreading of mass information from source to recipient through short message services (SMS). In education and awareness applications, SMS messages are sent directly to users' phones to offer information about various subjects, including testing and treatment methods, availability of health services, and disease management.
SMSs provide an advantage of being relatively unobtrusive, offering patients confidentiality in environments where disease (especially HIV/AIDS) is often taboo. Additionally, SMSs provide an avenue to reach far-reaching areas—such as rural areas—which may have limited access to public health information and education, health clinics, and a deficit of healthcare workers.
Helpline:
Helpline typically consists of a specific phone number that any individual is able to call to gain access to a range of medical services. These include phone consultations, counseling, service complaints, and information on facilities, drugs, equipment, and/or available mobile health clinics.
Diagnostic support, treatment support, communication and training for healthcare workers:
Diagnostic and treatment support systems are typically designed to provide healthcare workers in remote areas advice about diagnosis and treatment of patients. While some projects may provide mobile phone applications—such as a step-by-step medical decision tree systems—to help healthcare workers diagnosis, other projects provide direct diagnosis to patients themselves.
In such cases, known as telemedicine, patients might take a photograph of a wound or illness and allow a remote physician diagnose to help treat the medical problem. Both diagnosis and treatment support projects attempt to mitigate the cost and time of travel for patients located in remote areas.
mHealth projects within the communication and training for healthcare workers subset involve connecting healthcare workers to sources of information through their mobile phone. This involves connecting healthcare workers to other healthcare workers, medical institutions, ministries of health, or other houses of medical information. Such projects additionally involve using mobile phones to better organize and target in-person training.
Improved communication projects attempt to increase knowledge transfer among healthcare workers and improve patient outcomes through such programs as patient referral processes. For example, the systematic use of mobile instant messaging for the training and empowerment of health professionals has resulted in higher levels of clinical knowledge and fewer feelings of professional isolation.
Projects within this area operate to utilize mobile phones' ability to collect and transmit data quickly, cheaply, and relatively efficiently. Data concerning the location and levels of specific diseases (such as malaria, HIV/AIDS, TB, Avian Flu) can help medical systems or ministries of health or other organizations identify outbreaks and better target medical resources to areas of greatest need. Such projects can be particularly useful during emergencies, in order to identify where the greatest medical needs are within a country.
Policymakers and health providers at the national, district, and community level need accurate data in order to gauge the effectiveness of existing policies and programs and shape new ones. In the developing world, collecting field information is particularly difficult since many segments of the population are rarely able to visit a hospital, even in the case of severe illness.
A lack of patient data creates an arduous environment in which policy makers can decide where and how to spend their (sometimes limited) resources. While some software within this area is specific to a particular content or area, other software can be adapted to any data collection purpose.
Treatment support and medication compliance for patients, including chronic disease management:
Remote monitoring and treatment support allows for greater involvement in the continued care of patients. Recent studies seem to show also the efficacy of inducing positive and negative affective states, using smart phones.
Within environments of limited resources and beds—and subsequently a 'outpatient' culture—remote monitoring allows healthcare workers to better track patient conditions, medication regimen adherence, and follow-up scheduling. Such projects can operate through either one- or two-way communications systems.
Remote monitoring has been used particularly in the area of medication adherence for AIDS, cardiovascular disease, chronic lung disease, diabetes, antenatal mental health, mild anxiety, and tuberculosis. Technical process evaluations have confirmed the feasibility of deploying dynamically tailored, SMS-based interventions designed to provide ongoing behavioral reinforcement for persons living with HIV. among others.
In conclusion, the use of the mobile phone technology (in combination with a web-based interface) in health care results in an increase in convenience and efficiency of data collection, transfer, storage and analysis management of data as compared with paper-based systems.
Formal studies and preliminary project assessments demonstrate this improvement of efficiency of healthcare delivery by mobile technology. Nevertheless, mHealth should not be considered as a panacea for healthcare. Possible organizational issues include the ensuring of appropriate use and proper care of the handset, lost or stolen phones, and the important consideration of costs related to the purchase of equipment.
There is therefore a difficulty in comparison in weighing up mHealth interventions against other priority and evidence-based interventions.
Emerging trends and areas of interest:
According to Vodafone Group Foundation on February 13, 2008, a partnership for emergency communications was created between the group and United Nations Foundation. Such partnership will increase the effectiveness of the information and communications technology response to major emergencies and disasters around the world.
Criticism and concerns:
The extensive practice of mhealth research has sparked criticism, for example on the proliferation of fragmented pilot studies in low- and middle-income countries, which is also referred to as "pilotitis."
The extent of uncoordindated pilot studies prompted for instance the Ugandan Director General Health Services Dr Jane Ruth Aceng in 2012 to issue a notice that, "in order to jointly ensure that all eHealth efforts are harmonized and coordinated, I am directing that ALL eHealth projects/Initiatives be put to halt."
The assumptions that justify mhealth initiatives have also been challenged in recent sociological research. For examples:
Mhealth has also been argued to alter the practice of healthcare and patient-physician relationships as well as how bodies and health are being represented.
Another widespread concern relates to privacy and data protection, for example in the context of electronic health records.
See also:
mHealth (also written as m-health or mhealth) is an abbreviation for mobile health, a term used for the practice of medicine and public health supported by mobile devices. The term is most commonly used in reference to using mobile communication devices, such as mobile phones, tablet computers and PDAs, and wearable devices such as smart watches, for health services, information, and data collection.
The mHealth field has emerged as a sub-segment of eHealth, the use of information and communication technology (ICT), such as computers, mobile phones, communications satellite, patient monitors, etc., for health services and information.
mHealth applications include the use of mobile devices in collecting community and clinical health data, delivery of healthcare information to practitioners, researchers and patients, real-time monitoring of patient vital signs, the direct provision of care (via mobile telemedicine) as well as training and collaboration of health workers.
While mHealth certainly has application for industrialized nations, the field has emerged in recent years as largely an application for developing countries, stemming from the rapid rise of mobile phone penetration in low-income nations. The field, then, largely emerges as a means of providing greater access to larger segments of a population in developing countries, as well as improving the capacity of health systems in such countries to provide quality healthcare.
Within the mHealth space, projects operate with a variety of objectives, including increased access to healthcare and health-related information (particularly for hard-to-reach populations); improved ability to diagnose and track diseases; timelier, more actionable public health information; and expanded access to ongoing medical education and training for health workers.
According to an analyst firm, around 2.8 million patients worldwide were using a home monitoring service based on equipment with integrated connectivity at the end of 2012. The figure does not include patients that use monitoring devices connected to a PC or mobile phone. It only includes systems that rely on monitors with integrated connectivity or systems that use monitoring hubs with integrated cellular or fixed-line modems.
It forecast that the number of home monitoring systems with integrated communication capabilities will grow at a compound annual growth rate (CAGR) of 26.9 percent between 2011 and 2017 reaching 9.4 million connections globally by the end of the forecast period.
The number of these devices that have integrated cellular connectivity increased from 0.73 million in 2011 to about 1.03 million in 2012, and is projected to grow at a CAGR of 46.3 percent to 7.10 million in 2017.
A growing percentage of health-related smartphone apps are available, and some estimates predicted that 500 million patients would be using such apps by the year 2015.
While there are concerns about the accuracy and unregulated status of health apps, mHealth broadly encompasses the use of mobile telecommunication and multimedia technologies as they are integrated within increasingly mobile and wireless health care delivery systems.
The field broadly encompasses the use of mobile telecommunication and multimedia technologies in health care delivery. The term mHealth was coined by Robert Istepanian as use of "emerging mobile communications and network technologies for healthcare".
A definition used at the 2010 mHealth Summit of the Foundation for the National Institutes of Health (FNIH) was "the delivery of healthcare services via mobile communication devices".
While there are some projects that are considered solely within the field of mHealth, the linkage between mHealth and eHealth is unquestionable. For example, an mHealth project that uses mobile phones to access data on HIV/AIDS rates would require an eHealth system in order to manage, store, and assess the data. Thus, eHealth projects many times operate as the backbone of mHealth projects.
In a similar vein, while not clearly bifurcated by such a definition, eHealth can largely be viewed as technology that supports the functions and delivery of healthcare, while mHealth rests largely on providing healthcare access.
Because mHealth is by definition based on mobile technology such as smartphones, healthcare, through information and delivery, can better reach areas, people, and/or healthcare practitioners with previously limited exposure to certain aspects of healthcare.
Motivation:
mHealth is one aspect of eHealth that is pushing the limits of how to acquire, transport, store, process, and secure the raw and processed data to deliver meaningful results. mHealth offers the ability of remote individuals to participate in the health care value matrix, which may not have been possible in the past.
Participation does not imply just consumption of health care services. In many cases remote users are valuable contributors to gather data regarding disease and public health concerns such as outdoor pollution, drugs and violence.
The motivation behind the development of the mHealth field arises from two factors. The first factor concerns the myriad constraints felt by healthcare systems of developing nations.
These constraints include high population growth, a high burden of disease prevalence, low health care workforce, large numbers of rural inhabitants, and limited financial resources to support healthcare infrastructure and health information systems.
The second factor is the recent rapid rise in mobile phone penetration in developing countries to large segments of the healthcare workforce, as well as the population of a country as a whole. With greater access to mobile phones to all segments of a country, including rural areas, the potential of lowering information and transaction costs in order to deliver healthcare improves.
The combination of these two factors has motivated much discussion of how greater access to mobile phone technology can be leveraged to mitigate the numerous pressures faced by developing countries' healthcare systems. Both factors are discussed here.
Healthcare in low- and middle-income countries:
Middle income and especially low-income countries face a plethora of constraints in their healthcare systems. These countries face a severe lack of human and physical resources, as well as some of the largest burdens of disease, extreme poverty, and large population growth rates. Additionally, healthcare access to all reaches of society is generally low in these countries.
According to a World Health Organization (WHO) report from June 2011, higher-income countries show more mHealth activity than do lower-income countries (as consistent with eHealth trends in general).
Countries in the European Region are currently the most active and those in the African Region the least active. The WHO report findings also included that mHealth is most easily incorporated into processes and services that historically use voice communication through conventional telephone networks. The report was the result of a mHealth survey module designed by researchers at the Earth Institute's Center for Global Health and Economic Development, Columbia University.
The WHO notes an extreme deficit within the global healthcare workforce. The WHO notes critical healthcare workforce shortages in 57 countries—most of which are characterized as developing countries—and a global deficit of 2.4 million doctors, nurses, and midwives.
The WHO, in a study of the healthcare workforce in 12 countries of Africa, finds an average density of physicians, nurses and midwives per 1000 population of 0.64. The density of the same metric is four times as high in the United States, at 2.6.
The burden of disease is additionally much higher in low- and middle-income countries than high-income countries. The burden of disease, measured in disability-adjusted life year (DALY), which can be thought of as a measurement of the gap between current health status and an ideal situation where everyone lives into old age, free of disease and disability, is about five times higher in Africa than in high-income countries.
In addition, low- and middle-income countries are forced to face the burdens of both extreme poverty and the growing incidence of chronic diseases, such as diabetes and heart disease, an effect of new-found (relative) affluence.
Considering poor infrastructure and low human resources, the WHO notes that the healthcare workforce in sub-Saharan Africa would need to be scaled up by as much as 140% to attain international health development targets such as those in the Millennium Declaration.
The WHO, in reference to the healthcare condition in sub-saharan Africa, states:
- The problem is so serious that in many instances there is simply not enough human capacity even to absorb, deploy and efficiently use the substantial additional funds that are considered necessary to improve health in these countries.
Mobile technology has made a recent and rapid appearance into low- and middle-income nations. While, in the mHealth field, mobile technology usually refers to mobile phone technology, the entrance of other technologies into these nations to facilitate healthcare are also discussed here.
Health and development:
The link between health and development can be found in three of the Millennium Development Goals (MDGs), as set forth by the United Nations Millennium Declaration in 2000. The MDGs that specifically address health include reducing child mortality; improving maternal health; combating HIV and AIDS, malaria, and other diseases; and increasing access to safe drinking water.
A progress report published in 2006 indicates that childhood immunization and deliveries by skilled birth attendants are on the rise, while many regions continue to struggle to achieve reductions in the prevalence of the diseases of poverty including malaria, HIV and AIDS and tuberculosis.
Healthcare in developed countries:
In developed countries, healthcare systems have different policies and goals in relation to the personal and population health care goals.
In US and EU many patients and consumers use their cell phones and tablets to access health information and look for healthcare services. In parallel the number of mHealth applications grew significantly the last years.
Doctors, nurses and clinicians use mobile devices to access patient information and other databases and resources.
Technology and Market:
Basic SMS functions and real-time voice communication serve as the backbone and the current most common use of mobile phone technology. The broad range of potential benefits to the health sector that the simple functions of mobile phones can provide should not be understated.
The appeal of mobile communication technologies is that they enable communication in motion, allowing individuals to contact each other irrespective of time and place. This is particularly beneficial for work in remote areas where the mobile phone, and now increasingly wireless infrastructure, is able to reach more people, faster. As a result of such technological advances, the capacity for improved access to information and two-way communication becomes more available at the point of need.
Mobile phones:
With the global mobile phone penetration rate drastically increasing over the last decade, mobile phones have made a recent and rapid entrance into many parts of the low- and middle-income world. Improvements in telecommunications technology infrastructure, reduced costs of mobile handsets, and a general increase in non-food expenditure have influenced this trend.
Low- and middle-income countries are utilizing mobile phones as "leapfrog technology" (see leapfrogging). That is, mobile phones have allowed many developing countries, even those with relatively poor infrastructure, to bypass 20th century fixed-line technology and jump to modern mobile technology.
The number of global mobile phone subscribers in 2007 was estimated at 3.1 billion of an estimated global population of 6.6 billion (47%). These figures are expected to grow to 4.5 billion by 2012, or a 64.7% mobile penetration rate. The greatest growth is expected in Asia, the Middle East, and Africa.
In many countries, the number of mobile phone subscribers has bypassed the number of fixed-line telephones; this is particularly true in developing countries. Globally, there were 4.1 billion mobile phones in use in December 2008. See List of countries by number of mobile phones in use.
While mobile phone penetration rates are on the rise, globally, the growth within countries is not generally evenly distributed. In India, for example, while mobile penetration rates have increased markedly, by far the greatest growth rates are found in urban areas. Mobile penetration, in September 2008, was 66% in urban areas, while only 9.4% in rural areas.
The all India average was 28.2% at the same time. So, while mobile phones may have the potential to provide greater healthcare access to a larger portion of a population, there are certainly within-country equity issues to consider.
Mobile phones are spreading because the cost of mobile technology deployment is dropping and people are, on average, getting wealthier in low- and middle-income nations.
Vendors, such as Nokia, are developing cheaper infrastructure technologies (CDMA) and cheaper phones (sub $50–100, such as Sun's Java phone). Non-food consumption expenditure is increasing in many parts of the developing world, as disposable income rises, causing a rapid increase spending on new technology, such as mobile phones.
In India, for example, consumers have become and continue to become wealthier. Consumers are shifting their expenditure from necessity to discretionary. For example, on average, 56% of Indian consumers' consumption went towards food in 1995, compared to 42% in 2005.
The number is expected to drop to 34% by 2015. That being said, although total share of consumption has declined, total consumption of food and beverages increased 82% from 1985 to 2005, while per-capita consumption of food and beverages increased 24%. Indian consumers are getting wealthier and they are spending more and more, with a greater ability to spend on new technologies.
Smartphones:
More advanced mobile phone technologies are enabling the potential for further healthcare delivery. Smartphone technologies are in now in the hands of a large number of physicians and other healthcare workers in low- and middle-income countries.
Although far from ubiquitous, the spread of smartphone technologies opens up doors for mHealth projects such as technology-based diagnosis support, remote diagnostics and telemedicine, web browsing, GPS navigation, access to web-based patient information, post-visit patient surveillance, and decentralized health management information systems (HMIS).
While uptake of smartphone technology by the medical field has grown in low- and middle-income countries, it is worth noting that the capabilities of mobile phones in low- and middle-income countries has not reached the sophistication of those in high-income countries.
The infrastructure that enables web browsing, GPS navigation, and email through smartphones is not as well developed in much of the low- and middle-income countries. Increased availability and efficiency in both voice and data-transfer systems in addition to rapid deployment of wireless infrastructure will likely accelerate the deployment of mobile-enabled health systems and services throughout the world.
Other technologies:
Beyond mobile phones, wireless-enabled laptops and specialized health-related software applications are currently being developed, tested, and marketed for use in the mHealth field.
Many of these technologies, while having some application to low- and middle-income nations, are developing primarily in high-income countries. However, with broad advocacy campaigns for free and open source software (FOSS), applications are beginning to be tailored for and make inroads in low- and middle-income countries.
Some other mHealth technologies include:
- Patient monitoring devices
- Mobile telemedicine/telecare devices
- Microcomputers
- Data collection software
- Mobile Operating System Technology
- Mobile applications (e.g., game/social wellness solutions)
- Chatterbots
Mobile device operating system technology:
Technologies relate to the operating systems that orchestrate mobile device hardware while maintaining confidentiality, integrity and availability are required to build trust. This may foster greater adoption of mHealth technologies and services, by exploiting lower cost multi purpose mobile devices such as tablets, PCs, and smartphones.
Operating systems that control these emerging classes of devices include Google's Android, Apple's iPhone OS, Microsoft's Windows Mobile, and RIM's BlackBerry OS.
Operating systems must be agile and evolve to effectively balance and deliver the desired level of service to an application and end user, while managing display real estate, power consumption and security posture. As advances in capabilities such as integrating voice, video and Web 2.0 collaboration tools into mobile devices, significant benefits can be achieved in the delivery of health care services.
New sensor technologies such as HD video and audio capabilities, accelerometers, GPS, ambient light detectors, barometers and gyroscopes can enhance the methods of describing and studying cases, close to the patient or consumer of the health care service. This could include diagnosis, education, treatment and monitoring.
Air quality sensing technologies:
Environmental conditions have a significant impact to public health. Per the World Health Organization, outdoor air pollution accounts for about 1.4% of total mortality. Utilizing Participatory sensing technologies in mobile telephone, public health research can exploit the wide penetration of mobile devices to collect air measurements, which can be utilized to assess the impact of pollution.
Projects such as the Urban Atmospheres are utilizing embedded technologies in mobile phones to acquire real time conditions from millions of user mobile phones. By aggregating this data, public health policy shall be able to craft initiatives to mitigate risk associated with outdoor air pollution.
Data:
Data has become an especially important aspect of mHealth. Data collection requires both the collection device (mobile phones, computer, or portable device) and the software that houses the information. Data is primarily focused on visualizing static text but can also extend to interactive decision support algorithms, other visual image information, and also communication capabilities through the integration of e-mail and SMS features.
Integrating use of GIS and GPS with mobile technologies adds a geographical mapping component that is able to "tag" voice and data communication to a particular location or series of locations. These combined capabilities have been used for emergency health services as well as for disease surveillance, health facilities and services mapping, and other health-related data collection.
Applications:
While others exist, the 2009 UN Foundation and Vodafone Foundation report presents seven application categories within the mHealth field:
- Education and awareness
- Helpline
- Diagnostic and treatment support
- Communication and training for healthcare workers
- Disease and epidemic outbreak tracking
- Remote monitoring
- Remote data collection
Each application category as well as a specific project within the category will be described.
Education and awareness:
Education and awareness programs within the mHealth field are largely about the spreading of mass information from source to recipient through short message services (SMS). In education and awareness applications, SMS messages are sent directly to users' phones to offer information about various subjects, including testing and treatment methods, availability of health services, and disease management.
SMSs provide an advantage of being relatively unobtrusive, offering patients confidentiality in environments where disease (especially HIV/AIDS) is often taboo. Additionally, SMSs provide an avenue to reach far-reaching areas—such as rural areas—which may have limited access to public health information and education, health clinics, and a deficit of healthcare workers.
Helpline:
Helpline typically consists of a specific phone number that any individual is able to call to gain access to a range of medical services. These include phone consultations, counseling, service complaints, and information on facilities, drugs, equipment, and/or available mobile health clinics.
Diagnostic support, treatment support, communication and training for healthcare workers:
Diagnostic and treatment support systems are typically designed to provide healthcare workers in remote areas advice about diagnosis and treatment of patients. While some projects may provide mobile phone applications—such as a step-by-step medical decision tree systems—to help healthcare workers diagnosis, other projects provide direct diagnosis to patients themselves.
In such cases, known as telemedicine, patients might take a photograph of a wound or illness and allow a remote physician diagnose to help treat the medical problem. Both diagnosis and treatment support projects attempt to mitigate the cost and time of travel for patients located in remote areas.
mHealth projects within the communication and training for healthcare workers subset involve connecting healthcare workers to sources of information through their mobile phone. This involves connecting healthcare workers to other healthcare workers, medical institutions, ministries of health, or other houses of medical information. Such projects additionally involve using mobile phones to better organize and target in-person training.
Improved communication projects attempt to increase knowledge transfer among healthcare workers and improve patient outcomes through such programs as patient referral processes. For example, the systematic use of mobile instant messaging for the training and empowerment of health professionals has resulted in higher levels of clinical knowledge and fewer feelings of professional isolation.
Projects within this area operate to utilize mobile phones' ability to collect and transmit data quickly, cheaply, and relatively efficiently. Data concerning the location and levels of specific diseases (such as malaria, HIV/AIDS, TB, Avian Flu) can help medical systems or ministries of health or other organizations identify outbreaks and better target medical resources to areas of greatest need. Such projects can be particularly useful during emergencies, in order to identify where the greatest medical needs are within a country.
Policymakers and health providers at the national, district, and community level need accurate data in order to gauge the effectiveness of existing policies and programs and shape new ones. In the developing world, collecting field information is particularly difficult since many segments of the population are rarely able to visit a hospital, even in the case of severe illness.
A lack of patient data creates an arduous environment in which policy makers can decide where and how to spend their (sometimes limited) resources. While some software within this area is specific to a particular content or area, other software can be adapted to any data collection purpose.
Treatment support and medication compliance for patients, including chronic disease management:
Remote monitoring and treatment support allows for greater involvement in the continued care of patients. Recent studies seem to show also the efficacy of inducing positive and negative affective states, using smart phones.
Within environments of limited resources and beds—and subsequently a 'outpatient' culture—remote monitoring allows healthcare workers to better track patient conditions, medication regimen adherence, and follow-up scheduling. Such projects can operate through either one- or two-way communications systems.
Remote monitoring has been used particularly in the area of medication adherence for AIDS, cardiovascular disease, chronic lung disease, diabetes, antenatal mental health, mild anxiety, and tuberculosis. Technical process evaluations have confirmed the feasibility of deploying dynamically tailored, SMS-based interventions designed to provide ongoing behavioral reinforcement for persons living with HIV. among others.
In conclusion, the use of the mobile phone technology (in combination with a web-based interface) in health care results in an increase in convenience and efficiency of data collection, transfer, storage and analysis management of data as compared with paper-based systems.
Formal studies and preliminary project assessments demonstrate this improvement of efficiency of healthcare delivery by mobile technology. Nevertheless, mHealth should not be considered as a panacea for healthcare. Possible organizational issues include the ensuring of appropriate use and proper care of the handset, lost or stolen phones, and the important consideration of costs related to the purchase of equipment.
There is therefore a difficulty in comparison in weighing up mHealth interventions against other priority and evidence-based interventions.
Emerging trends and areas of interest:
- Emergency response systems (e.g., road traffic accidents, emergency obstetric care).
- Human resources coordination, management, and supervision.
- Mobile synchronous (voice) and asynchronous (SMS) telemedicine diagnostic and decision support to remote clinicians.
- Clinician-focused, evidence-based formulary, database and decision support information available at the point of care.
- Pharmaceutical supply chain integrity and patient safety systems (e.g. Sproxil and mPedigree).
- Clinical care and remote patient monitoring.
- Health extension services.
- Inpatient monitoring.
- Health services monitoring and reporting.
- Health-related mLearning for the general public.
- Mental health promotion.
- Training and continuing professional development for health care workers.
- Health promotion and community mobilization.
- Support of long-term conditions, for example medication reminders and diabetes self-management.
- Peer-to-peer personal health management for telemedicine.
- Social mobilization for infectious disease prevention.
- Surgical follow-up, such as for major joint arthroplasty patients.
- Mobile social media for global health personnel; for example, the capacity to facilitate professional connectedness, and to empower health workforce.
According to Vodafone Group Foundation on February 13, 2008, a partnership for emergency communications was created between the group and United Nations Foundation. Such partnership will increase the effectiveness of the information and communications technology response to major emergencies and disasters around the world.
Criticism and concerns:
The extensive practice of mhealth research has sparked criticism, for example on the proliferation of fragmented pilot studies in low- and middle-income countries, which is also referred to as "pilotitis."
The extent of uncoordindated pilot studies prompted for instance the Ugandan Director General Health Services Dr Jane Ruth Aceng in 2012 to issue a notice that, "in order to jointly ensure that all eHealth efforts are harmonized and coordinated, I am directing that ALL eHealth projects/Initiatives be put to halt."
The assumptions that justify mhealth initiatives have also been challenged in recent sociological research. For examples:
- mobile phones have been argued to be less widely accessible and usable than is often portrayed in mhealth-related publications;
- people integrate mobile phones into their health behaviour without external intervention;
- and the spread of mobile phones in low- and middle-income countries itself can create new forms of digital and healthcare exclusion, which mhealth interventions (using mobile phones as a platform) cannot overcome and potentially accentuate.
Mhealth has also been argued to alter the practice of healthcare and patient-physician relationships as well as how bodies and health are being represented.
Another widespread concern relates to privacy and data protection, for example in the context of electronic health records.
See also:
- Health informatics
- Health 2.0
- Open source software packages for mHealth
- Telehealth
- Healthcare workforce information systems
United States National Health Care Act, ("Medicare for All") including Universal Health Care
- YouTube Video: The Story of Medicare: A Timeline
- YouTube Video: Medicare for All: What does it Mean?
- YouTube Video: Medicare Explained (2019) Medicare Part B & Medicare Part A (and Supplements)
The United States National Health Care Act or Expanded and Improved Medicare for All Act is a bill first introduced in the United States House of Representatives by former Representative John Conyers (D-MI) in 2003, with 25 cosponsors.
As of October 1, 2017, it had 120 cosponsors, a majority of the Democratic caucus in the House of Representatives, and the highest level of support the bill has received since Conyers began annually introducing the bill in 2003.
The act would establish a universal single-payer health care system in the United States, the rough equivalent of Canada's Medicare and Taiwan's Bureau of National Health Insurance, among other examples.
Under a single-payer system, most medical care would be paid for by the federal government, ending the need for private health insurance and premiums, and recasting private insurance companies as providing purely supplemental coverage, to be used when non-essential care is sought.
The national system would be paid for in part through taxes replacing insurance premiums, but also by savings realized through the provision of preventative universal healthcare and the elimination of insurance company overhead and hospital billing costs. An analysis of the bill by Physicians for a National Health Program estimated the immediate savings at $350 billion per year.
Others have estimated a long-term savings amounting to 40% of all national health expenditures due to preventative health care. Preventative care can save several hundreds of billions of dollars per year in the U.S., because for example cancer patients are more likely to be diagnosed at Stage I where curative treatment is typically a few outpatient visits, instead of at Stage III or later in an emergency room where treatment can involve years of hospitalization and is often terminal.
During the 2009 health care debates over the bill that became the Patient Protection and Affordable Care Act, H.R. 676 was expected to be debated and voted upon by the House in September 2009, but was never debated.
On September 13, 2017, Senator Bernie Sanders introduced a parallel bill in the United States Senate with 16 cosponsors. The act would establish a universal single-payer health care system in the United States.
In 2019, the original 16 year old proposal was renumbered and Pramila Jayapal (D-WA) introduced a broadly similar but more detailed as HR 1384 for the 116th United States Congress.
Click on any of the following blue hyperlinks for more about "Medicare for All":
Universal healthcare (also called universal health coverage, universal coverage, or universal care) is a health care system that provides health care and financial protection to all residents of a particular country or region. It is organized around providing a specified package of benefits to all members of a society with the end goal of providing financial risk protection, improved access to health services, and improved health outcomes.
Universal healthcare does not imply coverage for all people for everything, only that all people have access to healthcare. Some universal healthcare systems are government funded, while others are based on a requirement that all citizens purchase private health insurance. Universal healthcare can be determined by three critical dimensions: who is covered, what services are covered, and how much of the cost is covered.
It is described by the World Health Organization as a situation where citizens can access health services without incurring financial hardship. The Director General of WHO describes universal health coverage as the “single most powerful concept that public health has to offer” since it unifies “services and delivers them in a comprehensive and integrated way”.
One of the goals with universal healthcare is to create a system of protection which provides equality of opportunity for people to enjoy the highest possible level of health.
As part of Sustainable Development Goals, United Nations member states have agreed to work toward worldwide universal health coverage by 2030.
Click on any of the following blue hyperlinks for more about Universal Healthcare:
As of October 1, 2017, it had 120 cosponsors, a majority of the Democratic caucus in the House of Representatives, and the highest level of support the bill has received since Conyers began annually introducing the bill in 2003.
The act would establish a universal single-payer health care system in the United States, the rough equivalent of Canada's Medicare and Taiwan's Bureau of National Health Insurance, among other examples.
Under a single-payer system, most medical care would be paid for by the federal government, ending the need for private health insurance and premiums, and recasting private insurance companies as providing purely supplemental coverage, to be used when non-essential care is sought.
The national system would be paid for in part through taxes replacing insurance premiums, but also by savings realized through the provision of preventative universal healthcare and the elimination of insurance company overhead and hospital billing costs. An analysis of the bill by Physicians for a National Health Program estimated the immediate savings at $350 billion per year.
Others have estimated a long-term savings amounting to 40% of all national health expenditures due to preventative health care. Preventative care can save several hundreds of billions of dollars per year in the U.S., because for example cancer patients are more likely to be diagnosed at Stage I where curative treatment is typically a few outpatient visits, instead of at Stage III or later in an emergency room where treatment can involve years of hospitalization and is often terminal.
During the 2009 health care debates over the bill that became the Patient Protection and Affordable Care Act, H.R. 676 was expected to be debated and voted upon by the House in September 2009, but was never debated.
On September 13, 2017, Senator Bernie Sanders introduced a parallel bill in the United States Senate with 16 cosponsors. The act would establish a universal single-payer health care system in the United States.
In 2019, the original 16 year old proposal was renumbered and Pramila Jayapal (D-WA) introduced a broadly similar but more detailed as HR 1384 for the 116th United States Congress.
Click on any of the following blue hyperlinks for more about "Medicare for All":
- Elements
- Cost
- Version history
- See also
- Other countries
- PNHP.org — Physicians for a National Health Program
- Healthcare-now.org — Healthcare-NOW!
- SinglePayerNow.net — Single Payer Now!
- MedicareForAll.org — "Single-payer for the USA."
Universal healthcare (also called universal health coverage, universal coverage, or universal care) is a health care system that provides health care and financial protection to all residents of a particular country or region. It is organized around providing a specified package of benefits to all members of a society with the end goal of providing financial risk protection, improved access to health services, and improved health outcomes.
Universal healthcare does not imply coverage for all people for everything, only that all people have access to healthcare. Some universal healthcare systems are government funded, while others are based on a requirement that all citizens purchase private health insurance. Universal healthcare can be determined by three critical dimensions: who is covered, what services are covered, and how much of the cost is covered.
It is described by the World Health Organization as a situation where citizens can access health services without incurring financial hardship. The Director General of WHO describes universal health coverage as the “single most powerful concept that public health has to offer” since it unifies “services and delivers them in a comprehensive and integrated way”.
One of the goals with universal healthcare is to create a system of protection which provides equality of opportunity for people to enjoy the highest possible level of health.
As part of Sustainable Development Goals, United Nations member states have agreed to work toward worldwide universal health coverage by 2030.
Click on any of the following blue hyperlinks for more about Universal Healthcare:
- History
- Funding models
- Implementation and comparisons
- See also:
- Global health
- Healthcare reform debate in the United States
- Health insurance cooperative
- List of countries by health insurance coverage
- National health insurance
- Primary healthcare
- Public health
- Publicly funded health care
- Right to health
- Single-payer healthcare
- Socialized medicine
- Two-tier healthcare
- Achieving Universal Health Care (July 2011). MEDICC Review: International Journal of Cuban Health and Medicine 13 (3). Theme issue: authors from 19 countries on dimensions of the challenges of providing universal access to health care.
- Catalyzing Change: The System Reform Costs of Universal Health Coverage (November 15, 2010). New York: The Rockefeller Foundation. Report on the feasibility of establishing the systems and institutions needed to pursue UHC.
- Physicians for a National Health Program Chicago: PNHP. A group of physicians and health professionals who support single-payer reform.
- UHC Forward Washington, D.C.: Results for Development Institute. Portal on universal health coverage.
Epilepsy and Epileptic Seizures
- YouTube Video: What is Epilepsy?
- YouTube Video: What would you do if someone has an epileptic seizure in front of You?
- YouTube Video: Children First Aid: Seizure (epilepsy)
Epilepsy is a group of neurological disorders characterized by recurrent epileptic seizures. Epileptic seizures are episodes that can vary from brief and nearly undetectable periods to long periods of vigorous shaking.
These episodes can result in physical injuries, including occasionally broken bones. In epilepsy, seizures have a tendency to recur and, as a rule, have no immediate underlying cause. Isolated seizures that are provoked by a specific cause such as poisoning are not deemed to represent epilepsy.
People with epilepsy may be treated differently in various areas of the world and experience varying degrees of social stigma due to their condition.
The cause of most cases of epilepsy is unknown. Some cases occur as the result of brain injury, stroke, brain tumors, infections of the brain, or birth defects through a process known as epileptogenesis.
Known genetic mutations are directly linked to a small proportion of cases. Epileptic seizures are the result of excessive and abnormal neuronal activity in the cortex of the brain.
The diagnosis involves ruling out other conditions that might cause similar symptoms, such as fainting, and determining if another cause of seizures is present, such as alcohol withdrawal or electrolyte problems. This may be partly done by imaging the brain and performing blood tests. Epilepsy can often be confirmed with an electroencephalogram (EEG), but a normal test does not rule out the condition.
Epilepsy that occurs as a result of other issues may be preventable. Seizures are controllable with medication in about 70% of cases; inexpensive anti-seizure medications are often available. In those whose seizures do not respond to medication, surgery, neurostimulation or dietary changes may then be considered. Not all cases of epilepsy are lifelong, and many people improve to the point that treatment is no longer needed.
As of 2015, about 39 million people have epilepsy. Nearly 80% of cases occur in the developing world. In 2015, it resulted in 125,000 deaths, an increase from 112,000 in 1990. Epilepsy is more common in older people.
In the developed world, onset of new cases occurs most frequently in babies and the elderly. In the developing world, onset is more common in older children and young adults due to differences in the frequency of the underlying causes. About 5–10% of people will have an unprovoked seizure by the age of 80, and the chance of experiencing a second seizure is between 40 and 50%.
In many areas of the world, those with epilepsy either have restrictions placed on their ability to drive or are not permitted to drive until they are free of seizures for a specific length of time. The word epilepsy is from Ancient Greek ἐπιλαμβάνειν, "to seize, possess, or afflict".
Click on any of the following blue hyperlinks for more about Epilepsy:
These episodes can result in physical injuries, including occasionally broken bones. In epilepsy, seizures have a tendency to recur and, as a rule, have no immediate underlying cause. Isolated seizures that are provoked by a specific cause such as poisoning are not deemed to represent epilepsy.
People with epilepsy may be treated differently in various areas of the world and experience varying degrees of social stigma due to their condition.
The cause of most cases of epilepsy is unknown. Some cases occur as the result of brain injury, stroke, brain tumors, infections of the brain, or birth defects through a process known as epileptogenesis.
Known genetic mutations are directly linked to a small proportion of cases. Epileptic seizures are the result of excessive and abnormal neuronal activity in the cortex of the brain.
The diagnosis involves ruling out other conditions that might cause similar symptoms, such as fainting, and determining if another cause of seizures is present, such as alcohol withdrawal or electrolyte problems. This may be partly done by imaging the brain and performing blood tests. Epilepsy can often be confirmed with an electroencephalogram (EEG), but a normal test does not rule out the condition.
Epilepsy that occurs as a result of other issues may be preventable. Seizures are controllable with medication in about 70% of cases; inexpensive anti-seizure medications are often available. In those whose seizures do not respond to medication, surgery, neurostimulation or dietary changes may then be considered. Not all cases of epilepsy are lifelong, and many people improve to the point that treatment is no longer needed.
As of 2015, about 39 million people have epilepsy. Nearly 80% of cases occur in the developing world. In 2015, it resulted in 125,000 deaths, an increase from 112,000 in 1990. Epilepsy is more common in older people.
In the developed world, onset of new cases occurs most frequently in babies and the elderly. In the developing world, onset is more common in older children and young adults due to differences in the frequency of the underlying causes. About 5–10% of people will have an unprovoked seizure by the age of 80, and the chance of experiencing a second seizure is between 40 and 50%.
In many areas of the world, those with epilepsy either have restrictions placed on their ability to drive or are not permitted to drive until they are free of seizures for a specific length of time. The word epilepsy is from Ancient Greek ἐπιλαμβάνειν, "to seize, possess, or afflict".
Click on any of the following blue hyperlinks for more about Epilepsy:
- Signs and symptoms
- Causes
- Mechanism
- Diagnosis
- Prevention
- Management
- Prognosis
- Epidemiology
- History
- Society and culture
- Research
- Other animals
- See also:
Could Decreasing Inflammation Be the Cure for Everything? (AARP November, 2019 Article); Inflammation (Wikipedia) and "What is Inflammation?" (WebMD)
- YouTube Video: Chronic Inflammation | Impact of Inflammation on Your Body
- YouTube Video: Inflammatory response | Human anatomy and physiology | Health & Medicine | Khan Academy
- YouTube Video: The Inflammatory Response HD Animation
[Your WebHost: I have included these three articles after receiving my November issue of AARP magazine. The possibility of a cure for the causes of inflammation will likely see continuing progress at increasing the longevity of life for mankind!]
Continued from image above by Harvard Medical School: "Chronic inflammation plays a central role in some of the most challenging diseases of our time, including rheumatoid arthritis, cancer, heart disease, diabetes, asthma, and even Alzheimer’s.
This report will examine the role that chronic inflammation plays in these conditions, and will also provide information on the breadth of drugs currently available to alleviate symptoms.
Drug choices range from simple aspirin, a nonsteroidal anti-inflammatory drug that’s been available for more than a century, to disease-modifying drugs and so-called biologics that promise more targeted treatments.
Click here to be taken to link for purchasing the book "Understanding Inflammation":
___________________________________________________________________________
"Could Decreasing Inflammation Be the Cure for Everything?" (AARP November 1, 2019 by Mike Zimmerman, AARP, November 1, 2019
It hardly sounds serious at all. An inconvenience, perhaps, like maybe a mild fever or a creaky joint. In the lexicon of aging and disease, there are far more worrisome words: cancer, heart disease, dementia, diabetes. But researchers have suspected for years that all of these health issues, and more, have at their heart one common trigger: low-grade inflammation.
And now they may finally have proof.
Cardiologists in Boston have reported on a clinical trial with more than 10,000 patients in 39 countries (mean age: 61) that tested to see if an anti-inflammatory drug could lower rates of heart disease. They discovered that it could. But they also found that the same drug, canakinumab, reduced lung cancer mortality more than 77 percent, and reports of gout and arthritis (conditions linked to inflammation) also fell.
"Inflammation plays a role in everyone's health,” says Dana DiRenzo, a rheumatologist and instructor of medicine at Johns Hopkins University School of Medicine in Baltimore. When inflammation levels increase, so does the risk of disease. But understanding inflammation can be tricky because, when you get a disease, inflammation levels naturally increase as your body fights the condition.
Inflammation, in other words, is both good and bad.
Given how crucial this issue is to your health, AARP spoke with some of America's top experts in the field, pored over the latest studies and created this guide to understanding — and overcoming — inflammation.
What exactly is inflammation?Think about when you catch the flu and your body temperature rises to fight the virus. That's a form of inflammation. So is the redness and swelling that occur when you sprain your ankle; it's the process your body uses to provide the healing chemicals and nutrients needed to help repair the damage.
These are examples of acute inflammation, a temporary, helpful response to an injury or illness. Once the danger goes away, so does the inflammation.
Chronic inflammation, on the other hand, is a slow, creeping condition caused by a misfiring of the immune system that keeps your body in a constant, long-term state of high alert, says Robert H. Shmerling, clinic chief in the department of rheumatology at Beth Israel Deaconess Medical
Why is chronic low-grade inflammation a problem?"Over time, inflammation damages healthy cells,” says Roma Pahwa, a researcher for the National Institutes of Health who specializes in the inflammatory response.
Here's why: When cells are in distress, they release chemicals that alert the immune system. White blood cells then flood the scene, where they work to eat up bacteria, viruses, damaged cells and debris from an infection or injury.
If the damage is too great, they call in backup cells known as neutrophils, which are the hand grenades of the immune system — they blow up everything in sight, healthy or not.
Each neutrophil has a short life span, but in chronic inflammation, they continue to be sent in long after the real threat is gone, causing damage to the healthy tissue that remains. The inflammation can start attacking the linings of your arteries or intestines, the cells in your liver and brain, or the tissues of your muscles and joints. This inflammation-caused cellular damage can trigger diseases like diabetes, cancer, dementia, heart disease, arthritis and depression.
And because it's low grade, “its slow and secret nature makes it hard to diagnose in day-to-day life,” Pahwa says. “You have no idea it's even happening until those conditions show symptoms."
How can something natural to our bodies be so toxic to our health?"It can be complicated to figure out if inflammation is friend or foe,” Pahwa says. Looking at the four main causes of chronic inflammation, however, sheds some light.
And getting older increases inflammation, too?
Unfortunately, yes. The older we are, the more exposure we've had to stuff like environmental toxins, stress, alcohol, bad foods and chronic diseases. Plus, aging makes it more difficult for our bodies to properly manage our immune systems, to extract nutrients from food and to shed extra pounds.
“There are thousands of articles in the science literature related to aging and inflammation,” says Thomas Buford, an associate professor with the University of Alabama at Birmingham School of Medicine's division of gerontology.
So what makes chronic inflammation happen?Chronic inflammation is a cascading effect of reactions in the body, Pahwa says. Here's a (very) basic breakdown of what's going on.
There are “pro-inflammatory foods"?
Yes, and they're the same foods you've been warned about by everyone from your dentist to your cardiologist. (And that's no surprise, because gingivitis and sclerotic arteries are both inflammatory conditions.) Foods high in sugar or high in unhealthy fats (think deli meats and fried foods) are top of the list.
"We don't fully understand it yet,” Buford says, “but now we know our gut microbiome, made up of trillions of bacteria, influences physiologic processes throughout the body.” We're born with a balance between good and bad bacteria in the gut. When that balance is thrown off — known as dysbiosis — it can lead to trouble. “A disregulated microbiome has been associated with metabolic diseases, pulmonary diseases, nervous system conditions, Alzheimer's — and these associations grow as we learn more and more,” Buford says.
What Causes? What Soothes?
Foods and activities that spark — and help reduce — inflammation:
We're still learning how these processes work, but one thing we do know is that foods high in sugar and fats, and low in fiber, feed the “unhealthy” bacteria in our digestive tract.
When the bad gut bacteria become too numerous, they can damage the lining of the digestive tract. “The intestinal barrier that separates the microorganisms from the rest of your body can become permeable, allowing particles to escape into the body circulation,” Buford says. This is known as leaky gut.
The immune system recognizes these particles as foreign invaders and attacks. But since the gut keeps leaking, the immune system keeps attacking, and — boom — you have chronic inflammation. High-fiber foods like whole grains, fruits and vegetables help to restore gut balance.
How do I know if I have chronic inflammation?
First, it's not that you either have it or don't have it. By a certain age, we all have some degree of inflammation in our bodies; the key is to keep it at a flickering ember and not let it erupt into a forest fire.
If you smoke, drink a lot, carry a lot of extra weight (especially in your belly), never exercise, eat poorly or constantly feel agitated by stress, your chances of having some level of chronic, elevated inflammation are high. If you are lean, are healthy and lead a balanced lifestyle? You should have less of it. “But it's tricky,” says Shmerling. Inflammation can be measured only by a blood test and interpreted by your doctor.
Did you say that my being overweight is causing inflammation?
Yes, we did. “Fat, especially belly fat, is a highly inflammatory tissue,” DiRenzo says. Every day, your belly fat is creating and releasing inflammatory compounds with Bond-villain names such as interleukin 6 and tumor necrosis factor-alpha. It's why lifestyle factors such as not sleeping well can cause weight gain; it's not just about calories, but about inflammation as well.
Remember, inflammation is a response to cell damage — and fat cells are the body's damsels in distress. They're bloated with triglycerides (a substance similar to diesel fuel) and as a result, they are very fragile and can easily burst and die. When they do, they trigger an inflammatory response as the immune system sends white blood cells to clean up the spilled fuel.
Is there a connection between stress and inflammation?There sure is. Chronic stress causes an increase in hormones like cortisol and adrenaline, which directly trigger a rise in inflammation. If you have an autoimmunity-based skin condition like psoriasis, you've probably witnessed this phenomenon yourself, says DiRenzo, who often sees it in her autoimmune patients. “They'll say, ‘Oh, I had a big stress week that triggered a flare-up,’ “ DiRenzo says. “And I say, ‘I believe you.’ “
Sounds like I should be asking my doctor to test me for inflammation.Here's the problem with testing: First, remember that we all have a certain amount of inflammation in our bodies. In fact, our levels fluctuate constantly, so a reading at 8 a.m. will be different from one at 8 p.m. Also, even something harmless like the common cold will spike the levels of disease-fighting chemicals in our blood, DiRenzo says.
Plus, if you're a generally healthy person with no diagnosed issues and you test high for inflammation, what are you going to do about it? For starters: Eat better, reduce stress, exercise more and lose weight. And that's what you should be doing regardless.
That's why doctors don't routinely test for inflammation, DiRenzo says: “Testing should come as a result of certain symptoms like swollen joints.” For example, if you have heart disease, your doctor may test for C-reactive protein (C-RP), an inflammation marker that's been linked to cardiac issues. But just chasing inflammation itself, without specific indicators, can open a Pandora's box of unnecessary testing for patients, DiRenzo says.
“Instead of trying to pin down this nebulous term ‘chronic inflammation,’ work closely with your doctor to ID specific-enough symptoms that may lead to a diagnosis of an inflammatory issue."
How about I just take anti-inflammatories like ibuprofen?Nice try, but no. While researchers continue to experiment with anti-inflammatory drugs, none has been approved for use in fighting chronic low-grade inflammation. “Ibuprofen has side effects such as stomach bleeding and increased blood pressure,” says physician Elizabeth Boham, medical director at the Ultrawellness Center in Lenox, Massachusetts. “There are much more effective ways to address chronic inflammation."
I assume that would be lifestyle changes.
Bingo. Lifestyle is the thing you can change fastest and the one thing you can control. The easy steps are to stay up to date on your vaccinations and wash your hands regularly, because infections trigger inflammation, Shmerling says. Beyond that, food, exercise, sleep and
The antioxidants in fruits and vegetables help to mitigate the cellular damage created by inflammation.
I already eat my veggies.
Brilliant. From an anti-inflammatory food perspective, eating a wide variety of colorful fruits and vegetables is about as good as it gets, because the antioxidants found in fruits and vegetables help to mitigate the cellular damage created by inflammation.
Cutting down on pro-inflammatory foods like processed flour, sugar and anything high in fat will also help, even if you can't stand the sight of cauliflower, DiRenzo says.
What else should I eat?
If all else fails, fiber. High-fiber foods feed the good microbes in your gut during digestion, helping to correct dysbiosis. “There's a lot of evidence that a high-fiber diet provides a positive balance of microbes and can potentially down-regulate inflammation,” Buford says. Also important: Avoid unhealthy fats because, he says, “even one high-fat meal can change the micro-environment."
So, less bacon, more broccoli. Is a vegetarian diet the answer?
Nope, unless that's what you want to do. It's true, plant-based foods pack the strongest anti-inflammatory punch. It's also true that red and processed meats can cause inflammation, but you don't have to banish meats from your diet, Boham says.
This is particularly important for older adults because protein consumption may help prevent age-related muscle loss. “I recommend a balance between plant — nuts, seeds, beans, grains — and animal protein,” she says. She recommends organic, grass-fed meats and wild-caught fish, which have a lower inflammation factor because they feed on plants and animals that are high in phytonutrients. Try to eat one food from every color of the rainbow every day.
I'm not much of an exerciser. How problematic is that?Well, research has shown that you don't have to be a marathoner to lower inflammation. In fact, a University of California, San Diego, study found that just 20 minutes of moderate exercise suppressed the inflammatory response. One reason, Buford says, is that exercise can positively affect your gut health (yes, that again). Maybe DiRenzo puts it best: “The difference between someone feeling OK and feeling great is exercise."
But exercise to me is unpleasant and uncomfortable.So is heart surgery. Which would you prefer? Ultimately, the anti-inflammatory benefits of exercise are worth the temporary discomfort. Even if you have physical limitations — bad knees, for example — exercise will most likely improve them.
To get started, DiRenzo suggests picking an activity you can do for five minutes a day. Next week, do it for seven minutes. It could be as simple as a brisk walk. “Yeah, you're gonna be sore,” she says, “but this is a good sore. Build and build and you will start to feel better."
If I'm going to be sore, doesn't that mean my muscles and joints have more inflammation?Sore muscles would be acute inflammation that'll go away in a day or two. (Good try, though.)
You make it sound like wholesale lifestyle changes are easy. They're not, you know.True. But isn't attacking one enemy — inflammation — a lot easier than worrying about dozens of them? Here's an idea: If you have to pick one lifestyle area to improve, focus on sleep, both the quantity and quality. It not only lowers your inflammation levels, it also helps you do everything else better. “I find when people give their body time to rest and lower stress, they have an easier time making smart food choices and getting exercise the next day,” Boham says.
Mike Zimmerman is the author of more than a dozen health books, including The 14-Day Anti-Inflammatory Diet.
More on Inflammation
[End of AARP Article]
___________________________________________________________________________
Inflammation (Wikipedia)
Inflammation is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants, and is a protective response involving immune cells, blood vessels, and molecular mediators.
The function of inflammation is to eliminate the initial cause of cell injury, clear out necrotic cells and tissues damaged from the original insult and the inflammatory process, and initiate tissue repair.
The five classical signs of inflammation are heat, pain, redness, swelling, and loss of function. Inflammation is a generic response, and therefore it is considered as a mechanism of innate immunity, as compared to adaptive immunity, which is specific for each pathogen.
Too little inflammation could lead to progressive tissue destruction by the harmful stimulus (e.g. bacteria) and compromise the survival of the organism. In contrast, chronic inflammation is associated with various diseases, such as hay fever, periodontal disease, atherosclerosis, and osteoarthritis.
Inflammation can be classified as either acute or chronic. Acute inflammation is the initial response of the body to harmful stimuli and is achieved by the increased movement of plasma and leukocytes (especially granulocytes) from the blood into the injured tissues. A series of biochemical events propagates and matures the inflammatory response, involving the local vascular system, the immune system, and various cells within the injured tissue.
Prolonged inflammation, known as chronic inflammation, leads to a progressive shift in the type of cells present at the site of inflammation, such as mononuclear cells, and is characterized by simultaneous destruction and healing of the tissue from the inflammatory process.
Inflammation is not a synonym for infection. Infection describes the interaction between the action of microbial invasion and the reaction of the body's inflammatory response—the two components are considered together when discussing an infection, and the word is used to imply a microbial invasive cause for the observed inflammatory reaction.
Inflammation on the other hand describes purely the body's immunovascular response, whatever the cause may be. But because of how often the two are correlated, words ending in the suffix -itis (which refers to inflammation) are sometimes informally described as referring to infection. For example, the word urethritis strictly means only "urethral inflammation", but clinical health care providers usually discuss urethritis as a urethral infection because urethral microbial invasion is the most common cause of urethritis.
It is useful to differentiate inflammation and infection because there are typical situations in pathology and medical diagnosis where inflammation is not driven by microbial invasion – for example, atherosclerosis, trauma, ischemia, and autoimmune diseases including type III hypersensitivity. Conversely, there is pathology where microbial invasion does not cause the classic inflammatory response – for example, parasitosis or eosinophilia.
Click on any of the following blue hyperlinks for more about Inflammation:
What Is Inflammation? (WebMD)
Inflammation is a process by which the body's white blood cells and substances they produce protect us from infection with foreign organisms, such as bacteria and viruses.
However, in some diseases, like arthritis, the body's defense system -- the immune system -- triggers an inflammatory response when there are no foreign invaders to fight off. In these diseases, called autoimmune diseases, the body's normally protective immune system causes damage to its own tissues. The body responds as if normal tissues are infected or somehow abnormal.
What Diseases Are Associated With Inflammation?
Some, but not all, types of arthritis are the result of misdirected inflammation. Arthritis is a general term that describes inflammation in the joints. Some types of arthritis associated with inflammation include the following:
Other painful conditions of the joints and musculoskeletal system that may not be associated with inflammation include osteoarthritis, fibromyalgia, muscular low back pain, and muscular neck pain.
What Are the Symptoms of Inflammation?
Symptoms of inflammation include:
Often, only a few of these symptoms are present.
Inflammation may also be associated with general flu-like symptoms including:
What Causes Inflammation and What Are Its Effects?
When inflammation occurs, chemicals from the body's white blood cells are released into the blood or affected tissues to protect your body from foreign substances. This release of chemicals increases the blood flow to the area of injury or infection, and may result in redness and warmth. Some of the chemicals cause a leak of fluid into the tissues, resulting in swelling. This protective process may stimulate nerves and cause pain.
The increased number of cells and inflammatory substances within the joint cause irritation, swelling of the joint lining and, eventually, wearing down of cartilage (cushions at the end of bones).
How Are Inflammatory Diseases Diagnosed?
Inflammatory diseases are diagnosed after careful evaluation of the following:
Can Inflammation Affect Internal Organs?
Yes. Inflammation can affect organs as part of an autoimmune disorder. The type of symptoms depend on which organs are affected. For example:
Pain may not be a primary symptom of an inflammatory disease, since many organs do not have many pain-sensitive nerves. Treatment of organ inflammation is directed at the cause of inflammation whenever possible.
How Are Inflammatory Joint Diseases Treated?
There are a number of treatment options for inflammatory diseases, like arthritis, including medications, rest, exercise, and surgery to correct joint damage. The type of treatment prescribed will depend on several factors, including the type of disease, the person's age, type of medications he or she is taking, overall health, medical history, and severity of symptoms.
The goals of treatment are the following:
What Drugs Are Used to Treat Inflammatory Diseases?
There are many drugs available to decrease joint pain, swelling and inflammation, and possibly prevent or minimize the progression of the inflammatory disease. They are often used in combination due to their differing effects.
The medications include:
Some of these medications are also used to treat other conditions such as cancer or inflammatory bowel disease, or to reduce the risk of rejection of a transplanted organ.
However, when "chemotherapy" types of medications (such as methotrexate or cyclophosphamide) are used to treat inflammatory diseases, the doses are sometimes significantly lower and the risks of side effects tend to be less than when prescribed in higher doses for cancer treatment.
When you are prescribed any medication, it is important to meet with your doctor regularly so he or she can detect the development of any side effects.
Continued from image above by Harvard Medical School: "Chronic inflammation plays a central role in some of the most challenging diseases of our time, including rheumatoid arthritis, cancer, heart disease, diabetes, asthma, and even Alzheimer’s.
This report will examine the role that chronic inflammation plays in these conditions, and will also provide information on the breadth of drugs currently available to alleviate symptoms.
Drug choices range from simple aspirin, a nonsteroidal anti-inflammatory drug that’s been available for more than a century, to disease-modifying drugs and so-called biologics that promise more targeted treatments.
Click here to be taken to link for purchasing the book "Understanding Inflammation":
___________________________________________________________________________
"Could Decreasing Inflammation Be the Cure for Everything?" (AARP November 1, 2019 by Mike Zimmerman, AARP, November 1, 2019
It hardly sounds serious at all. An inconvenience, perhaps, like maybe a mild fever or a creaky joint. In the lexicon of aging and disease, there are far more worrisome words: cancer, heart disease, dementia, diabetes. But researchers have suspected for years that all of these health issues, and more, have at their heart one common trigger: low-grade inflammation.
And now they may finally have proof.
Cardiologists in Boston have reported on a clinical trial with more than 10,000 patients in 39 countries (mean age: 61) that tested to see if an anti-inflammatory drug could lower rates of heart disease. They discovered that it could. But they also found that the same drug, canakinumab, reduced lung cancer mortality more than 77 percent, and reports of gout and arthritis (conditions linked to inflammation) also fell.
"Inflammation plays a role in everyone's health,” says Dana DiRenzo, a rheumatologist and instructor of medicine at Johns Hopkins University School of Medicine in Baltimore. When inflammation levels increase, so does the risk of disease. But understanding inflammation can be tricky because, when you get a disease, inflammation levels naturally increase as your body fights the condition.
Inflammation, in other words, is both good and bad.
Given how crucial this issue is to your health, AARP spoke with some of America's top experts in the field, pored over the latest studies and created this guide to understanding — and overcoming — inflammation.
What exactly is inflammation?Think about when you catch the flu and your body temperature rises to fight the virus. That's a form of inflammation. So is the redness and swelling that occur when you sprain your ankle; it's the process your body uses to provide the healing chemicals and nutrients needed to help repair the damage.
These are examples of acute inflammation, a temporary, helpful response to an injury or illness. Once the danger goes away, so does the inflammation.
Chronic inflammation, on the other hand, is a slow, creeping condition caused by a misfiring of the immune system that keeps your body in a constant, long-term state of high alert, says Robert H. Shmerling, clinic chief in the department of rheumatology at Beth Israel Deaconess Medical
Why is chronic low-grade inflammation a problem?"Over time, inflammation damages healthy cells,” says Roma Pahwa, a researcher for the National Institutes of Health who specializes in the inflammatory response.
Here's why: When cells are in distress, they release chemicals that alert the immune system. White blood cells then flood the scene, where they work to eat up bacteria, viruses, damaged cells and debris from an infection or injury.
If the damage is too great, they call in backup cells known as neutrophils, which are the hand grenades of the immune system — they blow up everything in sight, healthy or not.
Each neutrophil has a short life span, but in chronic inflammation, they continue to be sent in long after the real threat is gone, causing damage to the healthy tissue that remains. The inflammation can start attacking the linings of your arteries or intestines, the cells in your liver and brain, or the tissues of your muscles and joints. This inflammation-caused cellular damage can trigger diseases like diabetes, cancer, dementia, heart disease, arthritis and depression.
And because it's low grade, “its slow and secret nature makes it hard to diagnose in day-to-day life,” Pahwa says. “You have no idea it's even happening until those conditions show symptoms."
How can something natural to our bodies be so toxic to our health?"It can be complicated to figure out if inflammation is friend or foe,” Pahwa says. Looking at the four main causes of chronic inflammation, however, sheds some light.
- An outside infection that's hard to kill: You contract a chronic infection like hepatitis C or Lyme disease that lingers in the body for a long time. Your body responds with inflammation that also lingers a long time. In fact, it's often the chronic inflammation, not the viruses themselves, that causes much of the long-term damage related to these diseases.
- Genetics: You inherit a genetic propensity toward a health issue. In some cases, the genes related to these health issues can be turned on by inflammation: Diabetes and cancer are two genetically related diseases that can be triggered by inflammation. In other cases, the gene itself causes a misfiring of the immune system that causes the inflammation in rheumatoid arthritis, multiple sclerosis, lupus and other diseases.
- Environment: Pollution, air and water quality, environmental allergies and a host of other environmental factors can trigger and sustain inflammation.
- Lifestyle: Obesity, unregulated stress, tobacco use, drinking too much, lack of physical activity, lousy sleep and, of course, poor diet are all linked to chronic inflammation.
And getting older increases inflammation, too?
Unfortunately, yes. The older we are, the more exposure we've had to stuff like environmental toxins, stress, alcohol, bad foods and chronic diseases. Plus, aging makes it more difficult for our bodies to properly manage our immune systems, to extract nutrients from food and to shed extra pounds.
“There are thousands of articles in the science literature related to aging and inflammation,” says Thomas Buford, an associate professor with the University of Alabama at Birmingham School of Medicine's division of gerontology.
So what makes chronic inflammation happen?Chronic inflammation is a cascading effect of reactions in the body, Pahwa says. Here's a (very) basic breakdown of what's going on.
- Something triggers the immune system. Whether it's a chronic disease, an autoimmune disorder, weight gain, psychological stress, poor nutrition, exposure to chemicals or allergens — something puts your body in a state of stress and keeps it there.
- The immune system responds. The body goes into attack mode with its inflammatory response, which also includes blood vessel expansion to increase blood flow to the problem areas. Blood is the primary delivery system for all these substances.
- And responds … and responds … and responds. An endless cycle of pro-inflammatory foods, rampant stress, bad sleep and more keeps this process in constant motion because we never give the body a break.
There are “pro-inflammatory foods"?
Yes, and they're the same foods you've been warned about by everyone from your dentist to your cardiologist. (And that's no surprise, because gingivitis and sclerotic arteries are both inflammatory conditions.) Foods high in sugar or high in unhealthy fats (think deli meats and fried foods) are top of the list.
"We don't fully understand it yet,” Buford says, “but now we know our gut microbiome, made up of trillions of bacteria, influences physiologic processes throughout the body.” We're born with a balance between good and bad bacteria in the gut. When that balance is thrown off — known as dysbiosis — it can lead to trouble. “A disregulated microbiome has been associated with metabolic diseases, pulmonary diseases, nervous system conditions, Alzheimer's — and these associations grow as we learn more and more,” Buford says.
What Causes? What Soothes?
Foods and activities that spark — and help reduce — inflammation:
- White bread: A diet low in fiber can allow unhealthy bacteria to gain the upper hand in your digestive system, contributing to a leaky gut, in which toxins are allowed to pass through into your body rather than being swept away by the digestive system. Better: Whole-grain bread: As the body digests fiber, like that found in whole grains, it creates butyrate, a beneficial fatty acid with anti-inflammatory powers. Butyrate seems to cross the blood-brain barrier and may help prevent neurological decline.
- Deep fryers: Advanced glycation end products (AGEs) are inflammation-causing compounds produced when meats and grains are cooked at high heat — think doughnuts, french fries and fried chicken. Better: Fruit bowls: Dark-colored fruits, vegetables and beans contain polyphenols, plant compounds with antioxidant and anti-inflammatory properties. Examples you may have heard of: resveratrol (wine, grapes), catechins (tea, apples, berries).
- Bad attitudes: If you handle stress poorly, or feel helpless or put-upon, your body goes into fight-or-flight mode and releases cortisol, a hormone associated with inflammation. Better: Yoga: In one small study, women who were experienced at yoga were 4.75 times less likely to have detectable levels of C-reactive protein as those who were novices, showing that regular yoga seems to reduce inflammation.
- Pudding: Most processed foods, especially desserts, are low in fiber, high in sugar and packed with chemicals, all of which are bad for the gut. The more you cook at home with unprocessed food, the better. Better: Yogurt: Live culture yogurts contain healthy bacteria called probiotics, which help keep the bad gut bacteria in check.
- Roadhouses: The dancing and socializing at your favorite bar are healthy, but the smoking and drinking aren’t. Alcohol and tobacco mean party time for free radicals, compounds that cause cell damage and premature aging. And leave those fried chicken wings alone! Better: Church: Mindfulness techniques such as prayer and meditation have been shown to reduce some markers of inflammation and can help people suffering from chronic inflammatory conditions.
- Belly fat: Having a big belly means you have an excess of visceral fat, which builds up near your intestines and other internal organs. Visceral fat has been shown to secrete molecules that increase inflammation. Better: Healthy fats: Monounsaturated fats (olive oil, avocado, nuts) have been shown to lower the risk of heart disease, while polyunsaturated fats (fish, flax, oils) include an inflammation-busting mix of omega-6 and omega-3.
- Bottled salad dressings: Look at the label of your favorite dressing. The first three ingredients are probably water, sugar and soybean oil. Soy and vegetable oils are high in omega-6 fatty acids — which we tend to eat a lot of. Make your own salad dressings with inflammation-fighting olive oil, lemon or vinegar, and spices. Better: Big, colorful salads: The vitamins and minerals that are found in fruits and vegetables help prevent cell damage via oxidative stress — in other words, they fight inflammation. There are hundreds of antioxidants, such as vitamins A, C and E, as well as lycopene and selenium.
We're still learning how these processes work, but one thing we do know is that foods high in sugar and fats, and low in fiber, feed the “unhealthy” bacteria in our digestive tract.
When the bad gut bacteria become too numerous, they can damage the lining of the digestive tract. “The intestinal barrier that separates the microorganisms from the rest of your body can become permeable, allowing particles to escape into the body circulation,” Buford says. This is known as leaky gut.
The immune system recognizes these particles as foreign invaders and attacks. But since the gut keeps leaking, the immune system keeps attacking, and — boom — you have chronic inflammation. High-fiber foods like whole grains, fruits and vegetables help to restore gut balance.
How do I know if I have chronic inflammation?
First, it's not that you either have it or don't have it. By a certain age, we all have some degree of inflammation in our bodies; the key is to keep it at a flickering ember and not let it erupt into a forest fire.
If you smoke, drink a lot, carry a lot of extra weight (especially in your belly), never exercise, eat poorly or constantly feel agitated by stress, your chances of having some level of chronic, elevated inflammation are high. If you are lean, are healthy and lead a balanced lifestyle? You should have less of it. “But it's tricky,” says Shmerling. Inflammation can be measured only by a blood test and interpreted by your doctor.
Did you say that my being overweight is causing inflammation?
Yes, we did. “Fat, especially belly fat, is a highly inflammatory tissue,” DiRenzo says. Every day, your belly fat is creating and releasing inflammatory compounds with Bond-villain names such as interleukin 6 and tumor necrosis factor-alpha. It's why lifestyle factors such as not sleeping well can cause weight gain; it's not just about calories, but about inflammation as well.
Remember, inflammation is a response to cell damage — and fat cells are the body's damsels in distress. They're bloated with triglycerides (a substance similar to diesel fuel) and as a result, they are very fragile and can easily burst and die. When they do, they trigger an inflammatory response as the immune system sends white blood cells to clean up the spilled fuel.
Is there a connection between stress and inflammation?There sure is. Chronic stress causes an increase in hormones like cortisol and adrenaline, which directly trigger a rise in inflammation. If you have an autoimmunity-based skin condition like psoriasis, you've probably witnessed this phenomenon yourself, says DiRenzo, who often sees it in her autoimmune patients. “They'll say, ‘Oh, I had a big stress week that triggered a flare-up,’ “ DiRenzo says. “And I say, ‘I believe you.’ “
Sounds like I should be asking my doctor to test me for inflammation.Here's the problem with testing: First, remember that we all have a certain amount of inflammation in our bodies. In fact, our levels fluctuate constantly, so a reading at 8 a.m. will be different from one at 8 p.m. Also, even something harmless like the common cold will spike the levels of disease-fighting chemicals in our blood, DiRenzo says.
Plus, if you're a generally healthy person with no diagnosed issues and you test high for inflammation, what are you going to do about it? For starters: Eat better, reduce stress, exercise more and lose weight. And that's what you should be doing regardless.
That's why doctors don't routinely test for inflammation, DiRenzo says: “Testing should come as a result of certain symptoms like swollen joints.” For example, if you have heart disease, your doctor may test for C-reactive protein (C-RP), an inflammation marker that's been linked to cardiac issues. But just chasing inflammation itself, without specific indicators, can open a Pandora's box of unnecessary testing for patients, DiRenzo says.
“Instead of trying to pin down this nebulous term ‘chronic inflammation,’ work closely with your doctor to ID specific-enough symptoms that may lead to a diagnosis of an inflammatory issue."
How about I just take anti-inflammatories like ibuprofen?Nice try, but no. While researchers continue to experiment with anti-inflammatory drugs, none has been approved for use in fighting chronic low-grade inflammation. “Ibuprofen has side effects such as stomach bleeding and increased blood pressure,” says physician Elizabeth Boham, medical director at the Ultrawellness Center in Lenox, Massachusetts. “There are much more effective ways to address chronic inflammation."
I assume that would be lifestyle changes.
Bingo. Lifestyle is the thing you can change fastest and the one thing you can control. The easy steps are to stay up to date on your vaccinations and wash your hands regularly, because infections trigger inflammation, Shmerling says. Beyond that, food, exercise, sleep and
The antioxidants in fruits and vegetables help to mitigate the cellular damage created by inflammation.
I already eat my veggies.
Brilliant. From an anti-inflammatory food perspective, eating a wide variety of colorful fruits and vegetables is about as good as it gets, because the antioxidants found in fruits and vegetables help to mitigate the cellular damage created by inflammation.
Cutting down on pro-inflammatory foods like processed flour, sugar and anything high in fat will also help, even if you can't stand the sight of cauliflower, DiRenzo says.
What else should I eat?
If all else fails, fiber. High-fiber foods feed the good microbes in your gut during digestion, helping to correct dysbiosis. “There's a lot of evidence that a high-fiber diet provides a positive balance of microbes and can potentially down-regulate inflammation,” Buford says. Also important: Avoid unhealthy fats because, he says, “even one high-fat meal can change the micro-environment."
So, less bacon, more broccoli. Is a vegetarian diet the answer?
Nope, unless that's what you want to do. It's true, plant-based foods pack the strongest anti-inflammatory punch. It's also true that red and processed meats can cause inflammation, but you don't have to banish meats from your diet, Boham says.
This is particularly important for older adults because protein consumption may help prevent age-related muscle loss. “I recommend a balance between plant — nuts, seeds, beans, grains — and animal protein,” she says. She recommends organic, grass-fed meats and wild-caught fish, which have a lower inflammation factor because they feed on plants and animals that are high in phytonutrients. Try to eat one food from every color of the rainbow every day.
I'm not much of an exerciser. How problematic is that?Well, research has shown that you don't have to be a marathoner to lower inflammation. In fact, a University of California, San Diego, study found that just 20 minutes of moderate exercise suppressed the inflammatory response. One reason, Buford says, is that exercise can positively affect your gut health (yes, that again). Maybe DiRenzo puts it best: “The difference between someone feeling OK and feeling great is exercise."
But exercise to me is unpleasant and uncomfortable.So is heart surgery. Which would you prefer? Ultimately, the anti-inflammatory benefits of exercise are worth the temporary discomfort. Even if you have physical limitations — bad knees, for example — exercise will most likely improve them.
To get started, DiRenzo suggests picking an activity you can do for five minutes a day. Next week, do it for seven minutes. It could be as simple as a brisk walk. “Yeah, you're gonna be sore,” she says, “but this is a good sore. Build and build and you will start to feel better."
If I'm going to be sore, doesn't that mean my muscles and joints have more inflammation?Sore muscles would be acute inflammation that'll go away in a day or two. (Good try, though.)
You make it sound like wholesale lifestyle changes are easy. They're not, you know.True. But isn't attacking one enemy — inflammation — a lot easier than worrying about dozens of them? Here's an idea: If you have to pick one lifestyle area to improve, focus on sleep, both the quantity and quality. It not only lowers your inflammation levels, it also helps you do everything else better. “I find when people give their body time to rest and lower stress, they have an easier time making smart food choices and getting exercise the next day,” Boham says.
Mike Zimmerman is the author of more than a dozen health books, including The 14-Day Anti-Inflammatory Diet.
More on Inflammation
[End of AARP Article]
___________________________________________________________________________
Inflammation (Wikipedia)
Inflammation is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants, and is a protective response involving immune cells, blood vessels, and molecular mediators.
The function of inflammation is to eliminate the initial cause of cell injury, clear out necrotic cells and tissues damaged from the original insult and the inflammatory process, and initiate tissue repair.
The five classical signs of inflammation are heat, pain, redness, swelling, and loss of function. Inflammation is a generic response, and therefore it is considered as a mechanism of innate immunity, as compared to adaptive immunity, which is specific for each pathogen.
Too little inflammation could lead to progressive tissue destruction by the harmful stimulus (e.g. bacteria) and compromise the survival of the organism. In contrast, chronic inflammation is associated with various diseases, such as hay fever, periodontal disease, atherosclerosis, and osteoarthritis.
Inflammation can be classified as either acute or chronic. Acute inflammation is the initial response of the body to harmful stimuli and is achieved by the increased movement of plasma and leukocytes (especially granulocytes) from the blood into the injured tissues. A series of biochemical events propagates and matures the inflammatory response, involving the local vascular system, the immune system, and various cells within the injured tissue.
Prolonged inflammation, known as chronic inflammation, leads to a progressive shift in the type of cells present at the site of inflammation, such as mononuclear cells, and is characterized by simultaneous destruction and healing of the tissue from the inflammatory process.
Inflammation is not a synonym for infection. Infection describes the interaction between the action of microbial invasion and the reaction of the body's inflammatory response—the two components are considered together when discussing an infection, and the word is used to imply a microbial invasive cause for the observed inflammatory reaction.
Inflammation on the other hand describes purely the body's immunovascular response, whatever the cause may be. But because of how often the two are correlated, words ending in the suffix -itis (which refers to inflammation) are sometimes informally described as referring to infection. For example, the word urethritis strictly means only "urethral inflammation", but clinical health care providers usually discuss urethritis as a urethral infection because urethral microbial invasion is the most common cause of urethritis.
It is useful to differentiate inflammation and infection because there are typical situations in pathology and medical diagnosis where inflammation is not driven by microbial invasion – for example, atherosclerosis, trauma, ischemia, and autoimmune diseases including type III hypersensitivity. Conversely, there is pathology where microbial invasion does not cause the classic inflammatory response – for example, parasitosis or eosinophilia.
Click on any of the following blue hyperlinks for more about Inflammation:
- Causes
- Types
- Vascular component
- Cellular component
- Morphologic patterns
- Inflammatory disorders
- Systemic effects
- Outcomes
- Examples
- Diet and inflammation
- Exercise and inflammation
- See also:
- Anaphylatoxin
- Anti-inflammatories
- Essential fatty acid interactions
- Healing
- Inflammaging
- Inflammatory reflex
- Interleukin
- Lipoxin
- Neurogenic inflammation
- Substance P
- Inflammation at the US National Library of Medicine Medical Subject Headings (MeSH)
What Is Inflammation? (WebMD)
Inflammation is a process by which the body's white blood cells and substances they produce protect us from infection with foreign organisms, such as bacteria and viruses.
However, in some diseases, like arthritis, the body's defense system -- the immune system -- triggers an inflammatory response when there are no foreign invaders to fight off. In these diseases, called autoimmune diseases, the body's normally protective immune system causes damage to its own tissues. The body responds as if normal tissues are infected or somehow abnormal.
What Diseases Are Associated With Inflammation?
Some, but not all, types of arthritis are the result of misdirected inflammation. Arthritis is a general term that describes inflammation in the joints. Some types of arthritis associated with inflammation include the following:
- Rheumatoid arthritis
- Psoriatic arthritis
- Gouty arthritis
Other painful conditions of the joints and musculoskeletal system that may not be associated with inflammation include osteoarthritis, fibromyalgia, muscular low back pain, and muscular neck pain.
What Are the Symptoms of Inflammation?
Symptoms of inflammation include:
- Redness
- Swollen joint that's sometimes warm to the touch
- Joint pain
- Joint stiffness
- Loss of joint function
Often, only a few of these symptoms are present.
Inflammation may also be associated with general flu-like symptoms including:
What Causes Inflammation and What Are Its Effects?
When inflammation occurs, chemicals from the body's white blood cells are released into the blood or affected tissues to protect your body from foreign substances. This release of chemicals increases the blood flow to the area of injury or infection, and may result in redness and warmth. Some of the chemicals cause a leak of fluid into the tissues, resulting in swelling. This protective process may stimulate nerves and cause pain.
The increased number of cells and inflammatory substances within the joint cause irritation, swelling of the joint lining and, eventually, wearing down of cartilage (cushions at the end of bones).
How Are Inflammatory Diseases Diagnosed?
Inflammatory diseases are diagnosed after careful evaluation of the following:
- Complete medical history and physical exam with attention to:
- The pattern of painful joints and whether there is evidence of inflammation
- Presence of joint stiffness in the morning
- Evaluation of other symptoms
- Results of X-rays and blood tests
Can Inflammation Affect Internal Organs?
Yes. Inflammation can affect organs as part of an autoimmune disorder. The type of symptoms depend on which organs are affected. For example:
- Inflammation of the heart (myocarditis) may cause shortness of breath or fluid retention.
- Inflammation of the small tubes that transport air to the lungs may cause shortness of breath.
- Inflammation of the kidneys (nephritis) may cause high blood pressure or kidney failure.
Pain may not be a primary symptom of an inflammatory disease, since many organs do not have many pain-sensitive nerves. Treatment of organ inflammation is directed at the cause of inflammation whenever possible.
How Are Inflammatory Joint Diseases Treated?
There are a number of treatment options for inflammatory diseases, like arthritis, including medications, rest, exercise, and surgery to correct joint damage. The type of treatment prescribed will depend on several factors, including the type of disease, the person's age, type of medications he or she is taking, overall health, medical history, and severity of symptoms.
The goals of treatment are the following:
- Correct, control, or slow down the underlying disease process
- Avoid or modify activities that aggravate pain
- Relieve pain through pain medications and anti-inflammatory drugs
- Maintain joint movement and muscle strength through physical therapy
- Decrease stress on the joints by using braces, splints, or canes as needed
What Drugs Are Used to Treat Inflammatory Diseases?
There are many drugs available to decrease joint pain, swelling and inflammation, and possibly prevent or minimize the progression of the inflammatory disease. They are often used in combination due to their differing effects.
The medications include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs such as aspirin, ibuprofen, or naproxen)
- Corticosteroids (such as prednisone)
- Antimalarial medications (such as hydroxychloroquine)
- Other oral drugs known as DMARDs (disease-modifying antirheumatic drugs), including methotrexate, sulfasalazine, leflunomide, azathioprine, and cyclophosphamide
- Biologic drugs such as infliximab, etanercept, adalimumab, certolizumab, golimumab, abatacept, tocilizumab, and rituximab
Some of these medications are also used to treat other conditions such as cancer or inflammatory bowel disease, or to reduce the risk of rejection of a transplanted organ.
However, when "chemotherapy" types of medications (such as methotrexate or cyclophosphamide) are used to treat inflammatory diseases, the doses are sometimes significantly lower and the risks of side effects tend to be less than when prescribed in higher doses for cancer treatment.
When you are prescribed any medication, it is important to meet with your doctor regularly so he or she can detect the development of any side effects.
Emergency Medical Services
- YouTube Video: A Day in the Life of EMS (Emergency Medical Services)
- YouTube Video: Future of First Response: Vision for Emergency Medical Services
- YouTube Video: Emergency Medical Services: Inside the Ambulance
Emergency medical services (EMS), also known as ambulance services or paramedic services, are emergency services which treat illnesses and injuries that require an urgent medical response, providing out-of-hospital treatment and transport to definitive care. They may also be known as a first aid squad, FAST squad, emergency squad, rescue squad, ambulance squad, ambulance corps, life squad or by other acronyms such as EMAS or EMARS.
In most places, the EMS can be summoned by members of the public (as well as medical facilities, other emergency services, businesses and authorities) via an emergency telephone number which puts them in contact with a control facility, which will then dispatch a suitable resource to deal with the situation. Ambulances are the primary vehicles for delivering EMS, though some also use cars, motorcycles, aircraft or boats.
EMS agencies may also operate the non-emergency patient transport service, and some have units for technical rescue operations such as extrication, water rescue, and search and rescue.
As a first resort, the EMS provide treatment on the scene to those in need of urgent medical care. If it is deemed necessary, they are tasked with transferring the patient to the next point of care. This is most likely an emergency department of a hospital. Historically, ambulances only transported patients to care, and this remains the case in parts of the developing world.
The term "emergency medical service" was popularized when these services began to emphasize diagnosis and treatment at the scene. In some countries, a substantial portion of EMS calls do not result in a patient being taken to hospital.
Training and qualification levels for members and employees of emergency medical services vary widely throughout the world. In some systems, members may be present who are qualified only to drive ambulances, with no medical training.
In contrast, most systems have personnel who retain at least basic first aid certifications, such as basic life support (BLS). In English-speaking countries, they are known as emergency medical technicians (EMTs) and paramedics, with the latter having additional training such as advanced life support (ALS) skills. Physicians and nurses also provide pre-hospital care to varying degrees in different countries.
Click on any of the following blue hyperlinks for more about Emergency Medical Services:
In most places, the EMS can be summoned by members of the public (as well as medical facilities, other emergency services, businesses and authorities) via an emergency telephone number which puts them in contact with a control facility, which will then dispatch a suitable resource to deal with the situation. Ambulances are the primary vehicles for delivering EMS, though some also use cars, motorcycles, aircraft or boats.
EMS agencies may also operate the non-emergency patient transport service, and some have units for technical rescue operations such as extrication, water rescue, and search and rescue.
As a first resort, the EMS provide treatment on the scene to those in need of urgent medical care. If it is deemed necessary, they are tasked with transferring the patient to the next point of care. This is most likely an emergency department of a hospital. Historically, ambulances only transported patients to care, and this remains the case in parts of the developing world.
The term "emergency medical service" was popularized when these services began to emphasize diagnosis and treatment at the scene. In some countries, a substantial portion of EMS calls do not result in a patient being taken to hospital.
Training and qualification levels for members and employees of emergency medical services vary widely throughout the world. In some systems, members may be present who are qualified only to drive ambulances, with no medical training.
In contrast, most systems have personnel who retain at least basic first aid certifications, such as basic life support (BLS). In English-speaking countries, they are known as emergency medical technicians (EMTs) and paramedics, with the latter having additional training such as advanced life support (ALS) skills. Physicians and nurses also provide pre-hospital care to varying degrees in different countries.
Click on any of the following blue hyperlinks for more about Emergency Medical Services:
- History
- Organization
- Purpose
- Strategies for delivering care
- Personnel
- Specialist EMS
- Organization in different countries
- See also:
- Emergency Medical Services at Curlie
- "Emergency Medical Services in the European Union: report of an assessment project co-ordinated by the European Union"
- World Health Organization: Department of Violence and Injury Prevention "Prehospital Trauma Care Systems"
- In case of emergency, a program that enables EMS workers to identify victims and contact their next of kin to obtain important medical information
- Public utility model, a model for organizing Emergency Medical Services
- Battlefield medicine
- Wilderness medicine
- Mass Gathering Medicine
- Good Samaritan law
- CEN 1789
- The White Paper (Official title "Accidental Death and Disability: The Neglected Disease of Modern Society" – a 1966 report that prompted the development of organized EMS in the US)
- Medical amnesty policy
- Star of Life
- List of EMS provider credentials
Managing HIV/AIDS including HIV and HIV/AIDS
Pictured below: Managing HIV: Schematic description of the mechanism of the four classes of currently available antiretroviral drugs against HIV (Courtesy of Thomas Splettstoesser (www.scistyle.com) - Own work, CC BY 3.0.
Schematic description of the mechanism of the four classes of currently available antiviral drugs against HIV: fusion inhibitors ( interfere with the binding, fusion or entry of an HIV virion), reverse-transcriptase inhibitors (interfere with the translation of viral RNA into DNA), integrase inhibitors (block the viral enzyme integrase, that inserts the viral genome into the DNA of the host cell), protease inhibitors (block proteolytic cleavage of protein precursors that are necessary for the production of infectious viral particles)
- YouTube Video: What Causes HIV/AIDS?
- YouTube Video: The Science of HIV/AIDS
- YouTube Video: Famous People Who Died of HIV/AIDS
Pictured below: Managing HIV: Schematic description of the mechanism of the four classes of currently available antiretroviral drugs against HIV (Courtesy of Thomas Splettstoesser (www.scistyle.com) - Own work, CC BY 3.0.
Schematic description of the mechanism of the four classes of currently available antiviral drugs against HIV: fusion inhibitors ( interfere with the binding, fusion or entry of an HIV virion), reverse-transcriptase inhibitors (interfere with the translation of viral RNA into DNA), integrase inhibitors (block the viral enzyme integrase, that inserts the viral genome into the DNA of the host cell), protease inhibitors (block proteolytic cleavage of protein precursors that are necessary for the production of infectious viral particles)
___________________________________________________________________________
Pictured below: HIV
Scanning electron micrograph of HIV-1 (in green) budding from cultured lymphocyte. Multiple round bumps on cell surface represent sites of assembly and budding of virions.
Pictured below: HIV
Scanning electron micrograph of HIV-1 (in green) budding from cultured lymphocyte. Multiple round bumps on cell surface represent sites of assembly and budding of virions.
___________________________________________________________________________
Pictured below: HIV/AIDS
Left picture: Main symptoms of acute HIV infection
Right picture: Main symptoms of AIDS.
Pictured below: HIV/AIDS
Left picture: Main symptoms of acute HIV infection
Right picture: Main symptoms of AIDS.
Management of HIV/AIDS:
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs in an attempt to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle.
The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same sex and opposite sex partners so long as the HIV-positive partner maintains an undetectable viral load.
Treatment has been so successful that in many parts of the world, HIV has become a chronic condition in which progression to AIDS is increasingly rare. Anthony Fauci, head of the United States National Institute of Allergy and Infectious Diseases, has written, "With collective and resolute action now and a steadfast commitment for years to come, an AIDS-free generation is indeed within reach." In the same paper, he noted that an estimated 700,000 lives were saved in 2010 alone by antiretroviral therapy.
As another commentary in The Lancet noted, "Rather than dealing with acute and potentially life-threatening complications, clinicians are now confronted with managing a chronic disease that in the absence of a cure will persist for many decades."
The United States Department of Health and Human Services and the World Health Organization recommend offering antiretroviral treatment to all patients with HIV (see next topic below about HIV). Because of the complexity of selecting and following a regimen, the potential for side effects, and the importance of taking medications regularly to prevent viral resistance, such organizations emphasize the importance of involving patients in therapy choices and recommend analyzing the risks and the potential benefits.
The World Health Organization has defined health as more than the absence of disease. For this reason, many researchers have dedicated their work to better understanding the effects of HIV-related stigma, the barriers it creates for treatment interventions, and the ways in which those barriers can be circumvented.
Click on any of the following blue hyperlinks for more about Managing HIV:
The human immunodeficiency viruses (HIV) are two species of Lentivirus (a subgroup of retrovirus) that infect humans. Over time they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the immune system allows life-threatening opportunistic infections and cancers to thrive.
Without treatment, average survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype In most cases, HIV is a sexually transmitted infection and occurs by contact with or transfer of blood, pre-ejaculate, semen, and vaginal fluids.
Research has shown (for both same-sex and opposite-sex couples) that HIV is untransmittable through condomless sexual intercourse if the HIV-positive partner has a consistently undetectable viral load. Non-sexual transmission can occur from an infected mother to her infant during pregnancy, during childbirth by exposure to her blood or vaginal fluid, and through breast milk. Within these bodily fluids, HIV is present as both free virus particles and virus within infected immune cells.
HIV infects vital cells in the human immune system, such as helper T cells (specifically CD4+ T cells), macrophages, and dendritic cells. HIV infection leads to low levels of CD4+ T cells through a number of mechanisms, including pyroptosis of abortively infected T cells, apoptosis of uninfected bystander cells, direct viral killing of infected cells, and killing of infected CD4+ T cells by CD8+ cytotoxic lymphocytes that recognize infected cells. When CD4+ T cell numbers decline below a critical level, cell-mediated immunity is lost, and the body becomes progressively more susceptible to opportunistic infections, leading to the development of AIDS.
Click on any of the following blue hyperlinks for more about HIV: ___________________________________________________________________________
HIV/AIDS:
Human immunodeficiency virus infection and acquired immune deficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV). Following initial infection a person may not notice any symptoms, or may experience a brief period of influenza-like illness.
Typically, this is followed by a prolonged period with no symptoms. If the infection progresses, it interferes more with the immune system, increasing the risk of developing common infections such as tuberculosis, as well as other opportunistic infections, and tumors which are otherwise rare in people who have normal immune function. These late symptoms of infection are referred to as acquired immunodeficiency syndrome (AIDS). This stage is often also associated with unintended weight loss.
HIV is spread primarily by unprotected sex (including anal and oral sex), contaminated blood transfusions, hypodermic needles, and from mother to child during pregnancy, delivery, or breastfeeding. Some bodily fluids, such as saliva, sweat and tears, do not transmit the virus. HIV is a member of the group of viruses known as retroviruses.
Methods of prevention include:
Disease in a baby can often be prevented by giving both the mother and child antiretroviral medication. There is no cure or vaccine; however, antiretroviral treatment can slow the course of the disease and may lead to a near-normal life expectancy. Treatment is recommended as soon as the diagnosis is made. Without treatment, the average survival time after infection is 11 years.
In 2018 about 37.9 million people were living with HIV and it resulted in 770,000 deaths.
An estimated 20.6 million of these live in eastern and southern Africa. Between the time that AIDS was identified (in the early 1980s) and 2018, the disease caused an estimated 32 million deaths worldwide.
HIV/AIDS is considered a pandemic—a disease outbreak which is present over a large area and is actively spreading. HIV originated in west-central Africa during the late 19th or early 20th century. AIDS was first recognized by the United States Centers for Disease Control and Prevention (CDC) in 1981 and its cause—HIV infection—was identified in the early part of the decade.
HIV/AIDS has had a large impact on society, both as an illness and as a source of discrimination. The disease also has large economic impacts. There are many misconceptions about HIV/AIDS, such as the belief that it can be transmitted by casual non-sexual contact.
The disease has become subject to many controversies involving religion, including the Catholic Church's position not to support condom use as prevention. It has attracted international medical and political attention as well as large-scale funding since it was identified in the 1980s.
Click on any of the following blue hyperlinks for more about HIV/AIDS:
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs in an attempt to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle.
The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same sex and opposite sex partners so long as the HIV-positive partner maintains an undetectable viral load.
Treatment has been so successful that in many parts of the world, HIV has become a chronic condition in which progression to AIDS is increasingly rare. Anthony Fauci, head of the United States National Institute of Allergy and Infectious Diseases, has written, "With collective and resolute action now and a steadfast commitment for years to come, an AIDS-free generation is indeed within reach." In the same paper, he noted that an estimated 700,000 lives were saved in 2010 alone by antiretroviral therapy.
As another commentary in The Lancet noted, "Rather than dealing with acute and potentially life-threatening complications, clinicians are now confronted with managing a chronic disease that in the absence of a cure will persist for many decades."
The United States Department of Health and Human Services and the World Health Organization recommend offering antiretroviral treatment to all patients with HIV (see next topic below about HIV). Because of the complexity of selecting and following a regimen, the potential for side effects, and the importance of taking medications regularly to prevent viral resistance, such organizations emphasize the importance of involving patients in therapy choices and recommend analyzing the risks and the potential benefits.
The World Health Organization has defined health as more than the absence of disease. For this reason, many researchers have dedicated their work to better understanding the effects of HIV-related stigma, the barriers it creates for treatment interventions, and the ways in which those barriers can be circumvented.
Click on any of the following blue hyperlinks for more about Managing HIV:
- Classes of medication
- Combination therapy
- Treatment guidelines
- Concerns
- Response to therapy
- Salvage therapy
- Structured treatment interruptions
- Adverse effects
- HIV postexposure prophylaxis (PEP)
- Pregnancy planning
- History
- Research
- Drug advertisements
- Beyond Medical Management
- See also:
- Antiviral drug
- Discovery and development of HIV-protease inhibitors
- Discovery and development of non-nucleoside reverse-transcriptase inhibitors
- Discovery and development of nucleoside and nucleotide reverse-transcriptase inhibitors AIDSinfo – Comprehensive resource for HIV/AIDS treatment and clinical trial information from the U. S. Department of Health and Human Services
- ASHM – Australian Commentary on HHS Guidelines for the use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents
- Origins of antiretroviral combination therapy
- Viral Load research papers, including effectiveness of HAART on reducing viral load
- Current status of gene therapy strategies to treat HIV/AIDS
The human immunodeficiency viruses (HIV) are two species of Lentivirus (a subgroup of retrovirus) that infect humans. Over time they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the immune system allows life-threatening opportunistic infections and cancers to thrive.
Without treatment, average survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype In most cases, HIV is a sexually transmitted infection and occurs by contact with or transfer of blood, pre-ejaculate, semen, and vaginal fluids.
Research has shown (for both same-sex and opposite-sex couples) that HIV is untransmittable through condomless sexual intercourse if the HIV-positive partner has a consistently undetectable viral load. Non-sexual transmission can occur from an infected mother to her infant during pregnancy, during childbirth by exposure to her blood or vaginal fluid, and through breast milk. Within these bodily fluids, HIV is present as both free virus particles and virus within infected immune cells.
HIV infects vital cells in the human immune system, such as helper T cells (specifically CD4+ T cells), macrophages, and dendritic cells. HIV infection leads to low levels of CD4+ T cells through a number of mechanisms, including pyroptosis of abortively infected T cells, apoptosis of uninfected bystander cells, direct viral killing of infected cells, and killing of infected CD4+ T cells by CD8+ cytotoxic lymphocytes that recognize infected cells. When CD4+ T cell numbers decline below a critical level, cell-mediated immunity is lost, and the body becomes progressively more susceptible to opportunistic infections, leading to the development of AIDS.
Click on any of the following blue hyperlinks for more about HIV: ___________________________________________________________________________
HIV/AIDS:
Human immunodeficiency virus infection and acquired immune deficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV). Following initial infection a person may not notice any symptoms, or may experience a brief period of influenza-like illness.
Typically, this is followed by a prolonged period with no symptoms. If the infection progresses, it interferes more with the immune system, increasing the risk of developing common infections such as tuberculosis, as well as other opportunistic infections, and tumors which are otherwise rare in people who have normal immune function. These late symptoms of infection are referred to as acquired immunodeficiency syndrome (AIDS). This stage is often also associated with unintended weight loss.
HIV is spread primarily by unprotected sex (including anal and oral sex), contaminated blood transfusions, hypodermic needles, and from mother to child during pregnancy, delivery, or breastfeeding. Some bodily fluids, such as saliva, sweat and tears, do not transmit the virus. HIV is a member of the group of viruses known as retroviruses.
Methods of prevention include:
- safe sex,
- needle exchange programs,
- treating those who are infected,
- pre- and post-exposure prophylaxis,
- and male circumcision.
Disease in a baby can often be prevented by giving both the mother and child antiretroviral medication. There is no cure or vaccine; however, antiretroviral treatment can slow the course of the disease and may lead to a near-normal life expectancy. Treatment is recommended as soon as the diagnosis is made. Without treatment, the average survival time after infection is 11 years.
In 2018 about 37.9 million people were living with HIV and it resulted in 770,000 deaths.
An estimated 20.6 million of these live in eastern and southern Africa. Between the time that AIDS was identified (in the early 1980s) and 2018, the disease caused an estimated 32 million deaths worldwide.
HIV/AIDS is considered a pandemic—a disease outbreak which is present over a large area and is actively spreading. HIV originated in west-central Africa during the late 19th or early 20th century. AIDS was first recognized by the United States Centers for Disease Control and Prevention (CDC) in 1981 and its cause—HIV infection—was identified in the early part of the decade.
HIV/AIDS has had a large impact on society, both as an illness and as a source of discrimination. The disease also has large economic impacts. There are many misconceptions about HIV/AIDS, such as the belief that it can be transmitted by casual non-sexual contact.
The disease has become subject to many controversies involving religion, including the Catholic Church's position not to support condom use as prevention. It has attracted international medical and political attention as well as large-scale funding since it was identified in the 1980s.
Click on any of the following blue hyperlinks for more about HIV/AIDS:
- Signs and symptoms
- Transmission
- Virology
- Pathophysiology
- Diagnosis
- Prevention
- Treatment
- Prognosis
- Epidemiology
- History
- Society and culture
- Research
- See also:
- HIV/AIDS at Curlie
- UNAIDS – Joint United Nations Program on HIV/AIDS.
- AIDSinfo – Information on HIV/AIDS treatment, prevention, and research, U.S. Department of Health and Human Services.
- 2018 Recommendations of the International Antiviral Society
John Hopkins School of Medicine
- YouTube Video: 125 Years of the Johns Hopkins School of Medicine
- YouTube Video: M.D. vs. D.O. | Allopathic and Osteopathic Medical School Comparison
- YouTube Video: 10 Top Stories from Johns Hopkins Medicine
The Johns Hopkins University School of Medicine (JHUSOM), located in Baltimore, Maryland, is the research-intensive medical school of Johns Hopkins University.
Founded in 1893, the School of Medicine shares a campus with the Johns Hopkins Hospital, established in 1889. Johns Hopkins has consistently ranked among the top medical schools in the United States, in terms of the number of competitive research grants awarded by the National Institutes of Health, among other measures.
Overview:
The Johns Hopkins School of Medicine is located off Broadway in the East Baltimore campus of the Johns Hopkins University together with the Johns Hopkins Hospital, the Johns Hopkins Bloomberg School of Public Health, and the School of Nursing.
Known collectively as the "Johns Hopkins Medical Institutions" (JHMI) Campus, it spans several city blocks, radiating outwards from the 1889 original landmark red brick Billings building of the Johns Hopkins Hospital with its historic dome (cupola).
The founding physicians (the "Four Doctors") of the Johns Hopkins School of Medicine included:
The Johns Hopkins School of Medicine, which was finally begun 17 years after its original visionary benefactor Johns Hopkins (1795–1873), died and opened only with the large financial help offered by several wealthy daughters of the city's business elite on condition that the medical school be open equally to students of both sexes, consequently one of the first co-educational medical colleges.
The School of Medicine is affiliated with the Johns Hopkins Hospital, its main teaching hospital, as well as several other regional medical centers, including:
Together, they form an academic health science center.
The Johns Hopkins School of Medicine is the home of many medical advancements and contributions, including the first of many to admit women and to introduce rubber gloves, which provided a sterile approach to conducting surgical procedures. Johns Hopkins has also published The Harriet Lane Handbook, an indispensable tool for pediatricians, for over 60 years. The Lieber Institute for Brain Development is an affiliate of the School.
Reputation:
For years, Johns Hopkins has been among the nation's top medical schools in the number of competitive research grants awarded by the National Institutes of Health.
According to U.S. News and World Report, Johns Hopkins ranks #2 among research-oriented medical schools and has always ranked in the top 3. Its major teaching hospital, the Johns Hopkins Hospital, was ranked the top hospital in the United States every year from 1991 to 2011 by U.S. News & World Report.
International Business Times named an MD from Johns Hopkins one of the five most prestigious degrees in the world. Some achievements attributed to the school include the development of CPR, the discovery of the first effective treatments for severe forms of sickle cell disease, the development of the first biological pacemaker for the heart, and the planning and performance of one of the most challenging double arm transplants to date.
According to the Flexner Report, Hopkins has served as the model for American medical education. It was the first medical school to require its students to have an undergraduate degree and was also the first graduate-level medical school to admit women on an equal basis as men.
Mary Elizabeth Garrett, head of the Women's Medical School Fund, was a driving force behind both of these firsts. Sir William Osler became the first Professor of Medicine at Johns Hopkins and the first Physician-in-Chief at the Johns Hopkins Hospital. Osler was responsible for establishing the residency system of postgraduate medical training, where young physicians were required to reside within the hospital to better care for their patients.
Colleges Advising Program:
Upon matriculation, medical students at the Johns Hopkins School of Medicine are divided into four Colleges named after famous Hopkins faculty members who have had an impact in the history of medicine (Florence Sabin, Vivien Thomas, Daniel Nathans and Helen Taussig).
The Colleges were established to "foster camaraderie, networking, advising, mentoring, professionalism, clinical skills, and scholarship" in 2005. In each incoming class, 30 students are assigned to each College, and each College is further subdivided into six molecules of five students each.
Each molecule is advised and taught by a faculty advisor, who instructs them in Clinical Foundations of Medicine, a core first-year course, and continue advising them throughout their 4 years of medical school. The family within each college of each molecule across the four years who belong to a given advisor is referred to as a macromolecule.
Every year, the Colleges compete in the “College Olympics” in late October, a competition that includes athletic events and sports as well as art battles and dance-offs. Sabin College is the defending Olympics champion from both 2017 and 2018. Taussig College has held the Spirit Award each consecutive Olympics since 2016.
Governance:
The Johns Hopkins School of Medicine is led by :
The CFO of Johns Hopkins Medicine is Richard A. Grossi, who is also the Senior Associate Dean for Finance and Administration and executive vice president of Johns Hopkins Medicine.
Vice deans preside over specific administrative task areas. The vice deans are:
The dean's office also includes over twenty administrators in the position of associate or assistant dean.
Click on any of the following blue hyperlinks for more about John Hopkins School of Medicine:
Founded in 1893, the School of Medicine shares a campus with the Johns Hopkins Hospital, established in 1889. Johns Hopkins has consistently ranked among the top medical schools in the United States, in terms of the number of competitive research grants awarded by the National Institutes of Health, among other measures.
Overview:
The Johns Hopkins School of Medicine is located off Broadway in the East Baltimore campus of the Johns Hopkins University together with the Johns Hopkins Hospital, the Johns Hopkins Bloomberg School of Public Health, and the School of Nursing.
Known collectively as the "Johns Hopkins Medical Institutions" (JHMI) Campus, it spans several city blocks, radiating outwards from the 1889 original landmark red brick Billings building of the Johns Hopkins Hospital with its historic dome (cupola).
The founding physicians (the "Four Doctors") of the Johns Hopkins School of Medicine included:
- pathologist William Henry Welch (1850–1934), the first dean of the school and a mentor to generations of research scientists;
- a Canadian, internist Sir William Osler (1849–1919), regarded as the Father of Modern Medicine, having been perhaps the most influential physician of the late 19th and early 20th centuries as author of The Principles and Practice of Medicine (1892), written at the Johns Hopkins Hospital and published for more than a century;
- surgeon William Stewart Halsted (1852–1922), who revolutionized surgery by insisting on subtle skill and technique, as well as strict adherence to sanitary procedures;
- and gynecologist Howard Atwood Kelly (1858–1943), a superb gynecological surgeon credited with establishing gynecology as a specialty and being among the first to use radium to treat cancer.
The Johns Hopkins School of Medicine, which was finally begun 17 years after its original visionary benefactor Johns Hopkins (1795–1873), died and opened only with the large financial help offered by several wealthy daughters of the city's business elite on condition that the medical school be open equally to students of both sexes, consequently one of the first co-educational medical colleges.
The School of Medicine is affiliated with the Johns Hopkins Hospital, its main teaching hospital, as well as several other regional medical centers, including:
- the Johns Hopkins Bayview Medical Center on Eastern Avenue in East Baltimore;
- the Howard County General Hospital, near Ellicott City, southwest of Baltimore;
- Suburban Hospital in Bethesda in suburban Montgomery County, (northwest of Washington, D.C.);
- Sibley Memorial Hospital in Washington, D.C.;
- and Johns Hopkins All Children's Hospital in St. Petersburg, Florida.
Together, they form an academic health science center.
The Johns Hopkins School of Medicine is the home of many medical advancements and contributions, including the first of many to admit women and to introduce rubber gloves, which provided a sterile approach to conducting surgical procedures. Johns Hopkins has also published The Harriet Lane Handbook, an indispensable tool for pediatricians, for over 60 years. The Lieber Institute for Brain Development is an affiliate of the School.
Reputation:
For years, Johns Hopkins has been among the nation's top medical schools in the number of competitive research grants awarded by the National Institutes of Health.
According to U.S. News and World Report, Johns Hopkins ranks #2 among research-oriented medical schools and has always ranked in the top 3. Its major teaching hospital, the Johns Hopkins Hospital, was ranked the top hospital in the United States every year from 1991 to 2011 by U.S. News & World Report.
International Business Times named an MD from Johns Hopkins one of the five most prestigious degrees in the world. Some achievements attributed to the school include the development of CPR, the discovery of the first effective treatments for severe forms of sickle cell disease, the development of the first biological pacemaker for the heart, and the planning and performance of one of the most challenging double arm transplants to date.
According to the Flexner Report, Hopkins has served as the model for American medical education. It was the first medical school to require its students to have an undergraduate degree and was also the first graduate-level medical school to admit women on an equal basis as men.
Mary Elizabeth Garrett, head of the Women's Medical School Fund, was a driving force behind both of these firsts. Sir William Osler became the first Professor of Medicine at Johns Hopkins and the first Physician-in-Chief at the Johns Hopkins Hospital. Osler was responsible for establishing the residency system of postgraduate medical training, where young physicians were required to reside within the hospital to better care for their patients.
Colleges Advising Program:
Upon matriculation, medical students at the Johns Hopkins School of Medicine are divided into four Colleges named after famous Hopkins faculty members who have had an impact in the history of medicine (Florence Sabin, Vivien Thomas, Daniel Nathans and Helen Taussig).
The Colleges were established to "foster camaraderie, networking, advising, mentoring, professionalism, clinical skills, and scholarship" in 2005. In each incoming class, 30 students are assigned to each College, and each College is further subdivided into six molecules of five students each.
Each molecule is advised and taught by a faculty advisor, who instructs them in Clinical Foundations of Medicine, a core first-year course, and continue advising them throughout their 4 years of medical school. The family within each college of each molecule across the four years who belong to a given advisor is referred to as a macromolecule.
Every year, the Colleges compete in the “College Olympics” in late October, a competition that includes athletic events and sports as well as art battles and dance-offs. Sabin College is the defending Olympics champion from both 2017 and 2018. Taussig College has held the Spirit Award each consecutive Olympics since 2016.
Governance:
The Johns Hopkins School of Medicine is led by :
- Ronald J. Daniels, the president of the Johns Hopkins University,
- Paul B. Rothman, CEO and dean of the medical faculty,
- and Ronald R. Peterson, president of the Johns Hopkins Hospital and health system.
The CFO of Johns Hopkins Medicine is Richard A. Grossi, who is also the Senior Associate Dean for Finance and Administration and executive vice president of Johns Hopkins Medicine.
Vice deans preside over specific administrative task areas. The vice deans are:
- William A Baumgartner, Vice Dean for Clinical Affairs;
- Janice E. Clements, Vice Dean for Faculty Affairs;
- Landon King, Vice Dean for Research;
- Daniel E. Ford, Vice Dean for Clinical Investigation;
- David G. Nichols, Vice Dean for Education;
- and David Hellmann, Vice Dean for the Johns Hopkins Bayview Medical Center.
The dean's office also includes over twenty administrators in the position of associate or assistant dean.
Click on any of the following blue hyperlinks for more about John Hopkins School of Medicine:
- Nobel laureates
- Notable faculty and alumni
- In popular culture
- See also:
- Official website
- Media related to Johns Hopkins School of Medicine at Wikimedia Commons
Healthcare Occupations in the United States, including a List of Healthcare Occupations
- YouTube Video: Is Med School Right for Me? | Deciding on a Career in Medicine
- YouTube Video: Night Shift On Trauma Surgery During COVID | VLOG: Day in the Life of a Surgery Resident
- YouTube Video: Everyday Heroes | Essential Hospital Workers
Healthcare Occupations:
By the U.S. Bureau of Labor Statistics
Employment in healthcare occupations is projected to grow 15 percent from 2019 to 2029, much faster than the average for all occupations, adding about 2.4 million new jobs.
Healthcare occupations are projected to add more jobs than any of the other occupational groups. This projected growth is mainly due to an aging population, leading to greater demand for healthcare services.
The median annual wage for healthcare practitioners and technical occupations (such as registered nurses, physicians and surgeons, and dental hygienists) was $68,190 in May 2019, which was higher than the median annual wage for all occupations in the economy of $39,810.
Healthcare support occupations (such as home health aides, occupational therapy assistants, and medical transcriptionists) had a median annual wage of $28,470 in May 2019, lower than the median annual wage for all occupations in the economy.
Occupation: Athletic Trainers
Occupation: Audiologists
Occupation: Chiropractors
Occupation: Clinical Laboratory Technologists and Technicians
Occupation: Dental Assistants
Occupation: Dental Hygienists
Occupation: Dentists
Occupation: Diagnostic Medical Sonographers and Cardiovascular Technologists and Technicians, Including Vascular Technologists
Occupation: Dietitians and Nutritionists
Occupation: EMTs and Paramedics
Occupation: Exercise Physiologists
Occupation: Genetic Counselors
Occupation: Home Health Aides and Personal Care Aides
Occupation: Licensed Practical and Licensed Vocational Nurses
Occupation: Massage Therapists
Occupation: Medical Assistants
Occupation: Medical Records and Health Information Technicians
Occupation: Medical Transcriptionists
Occupation: Nuclear Medicine Technologists
Occupation: Nurse Anesthetists, Nurse Midwives, and Nurse Practitioners
Occupation: Nursing Assistants and Orderlies
Occupation: Occupational Health and Safety Specialists and Technicians
Occupation: Occupational Therapists
Occupation: Occupational Therapy Assistants and Aides
Occupation: Opticians
Occupation: Optometrists
Occupation: Orthotists and Prosthetists
Occupation: Pharmacists
Occupation Pharmacy Technicians
Occupation: Phlebotomists
Occupation: Physical Therapist Assistants and Aides
Occupation: Physical Therapists
Occupation: Physician Assistants
Occupation: Physicians and Surgeons
Occupation: Podiatrists
Occupation: Psychiatric Technicians and Aides
Occupation: Radiation Therapists
Occupation Radiologic and MRI Technologists
Occupation: Recreational Therapists
Occupation: Registered Nurses
Occupation: Respiratory Therapists
Occupation: Speech-Language Pathologists
Occupation: Surgical Technologists
Occupation Veterinarians
Occupation Veterinary Assistants and Laboratory Animal Caretakers
Occupation Veterinary Technologists and Technicians
List of healthcare occupations (by Wikipedia)
Below, a listing of health care professions by medical discipline.
Anesthesiology:
See also: Media related to Healthcare occupations at Wikimedia Commons
By the U.S. Bureau of Labor Statistics
Employment in healthcare occupations is projected to grow 15 percent from 2019 to 2029, much faster than the average for all occupations, adding about 2.4 million new jobs.
Healthcare occupations are projected to add more jobs than any of the other occupational groups. This projected growth is mainly due to an aging population, leading to greater demand for healthcare services.
The median annual wage for healthcare practitioners and technical occupations (such as registered nurses, physicians and surgeons, and dental hygienists) was $68,190 in May 2019, which was higher than the median annual wage for all occupations in the economy of $39,810.
Healthcare support occupations (such as home health aides, occupational therapy assistants, and medical transcriptionists) had a median annual wage of $28,470 in May 2019, lower than the median annual wage for all occupations in the economy.
Occupation: Athletic Trainers
- Job Summary: Athletic trainers specialize in preventing, diagnosing, and treating muscle and bone injuries and illnesses.
- Entry Level Education: Bachelor's degree
- 2019 Median Pay: $48,440
Occupation: Audiologists
- Job Summary: Audiologists diagnose, manage, and treat a patient’s hearing, balance, or ear problems.
- Entry Level Education: Doctoral or professional degree
- 2019 Median Pay: $77,600
Occupation: Chiropractors
- Job Summary: Chiropractors treat patients with health problems of the neuromusculoskeletal system, which includes nerves, bones, muscles, ligaments, and tendons.
- Entry Level Education: Doctoral or professional degree
- 2019 Median Pay: $70,340
Occupation: Clinical Laboratory Technologists and Technicians
- Job Summary: Clinical laboratory technologists and technicians collect samples and perform tests to analyze body fluids, tissue, and other substances.
- Entry Level Education: Bachelor's degree
- 2019 Median Pay: $53,120
Occupation: Dental Assistants
- Job Summary: Dental assistants provide patient care, take x rays, keep records, and schedule appointments.
- Entry Level Education: Postsecondary nondegree award
- 2019 Median Pay: $40,080
Occupation: Dental Hygienists
- Job Summary: Dental hygienists examine patients for signs of oral diseases, such as gingivitis, and provide preventive care, including oral hygiene.
- Entry Level Education: Associate's degree
- 2019 Median Pay: $76,220
Occupation: Dentists
- Job Summary: Dentists diagnose and treat problems with patients’ teeth, gums, and related parts of the mouth.
- Entry Level Education: Doctoral or professional degree
- 2019 Median Pay: $159,200
Occupation: Diagnostic Medical Sonographers and Cardiovascular Technologists and Technicians, Including Vascular Technologists
- Job Summary: Diagnostic medical sonographers and cardiovascular technologists and technicians, including vascular technologists operate special imaging equipment to create images or to conduct tests
- Entry Level Education: Associate's degree
- 2019 Median Pay: $68,750
Occupation: Dietitians and Nutritionists
- Job Summary: Dietitians and nutritionists advise people on what to eat in order to lead a healthy lifestyle or achieve a specific health-related goal.
- Entry Level Education: Bachelor's degree
- 2019 Median Pay: $61,270
Occupation: EMTs and Paramedics
- Job Summary: Emergency medical technicians (EMTs) and paramedics respond to emergency calls, performing medical services and transporting patients to medical facilities.
- Entry Level Education: Postsecondary nondegree award
- 2019 Median Pay: $35,400
Occupation: Exercise Physiologists
- Job Summary: Exercise physiologists develop fitness and exercise programs that help injured or sick patients recover.
- Entry Level Education: Bachelor's degree
- 2019 Median Pay $49,170
Occupation: Genetic Counselors
- Job Summary: Genetic counselors assess individual or family risk for a variety of inherited conditions, such as genetic disorders and birth defects.
- Entry Level Education: Master's degree
- 2019 Median Pay: $81,880
Occupation: Home Health Aides and Personal Care Aides
- Job Summary: Home health aides and personal care aides help people with disabilities, chronic illnesses, or cognitive impairment by assisting in their daily living activities.
- Entry Level Education: High school diploma or equivalent
- 2019 Median Pay: $25,280
Occupation: Licensed Practical and Licensed Vocational Nurses
- Job Summary: Licensed practical nurses (LPNs) and licensed vocational nurses (LVNs) provide basic nursing care.
- Entry Level Education: Postsecondary nondegree award
- 2019 Median Pay: $47,480
Occupation: Massage Therapists
- Job Summary: Massage therapists treat clients by using touch to manipulate the muscles and other soft tissues of the body.
- Entry Level Education: Postsecondary nondegree award
- 2019 Median Pay: $42,820
Occupation: Medical Assistants
- Job Summary: Medical assistants complete administrative and clinical tasks in hospitals, offices of physicians, and other healthcare facilities.
- Entry Level Education: Postsecondary nondegree award
- 2019 Median Pay: $34,800
Occupation: Medical Records and Health Information Technicians
- Job Summary: Medical records and health information technicians organize and manage health information data.
- Entry Level Education: Postsecondary nondegree award
- 2019 Median Pay: $42,630
Occupation: Medical Transcriptionists
- Job Summary: Medical transcriptionists listen to voice recordings that physicians and other healthcare workers make and convert them into written reports.
- Entry Level Education: Postsecondary nondegree award
- 2019 Median Pay: $33,380
Occupation: Nuclear Medicine Technologists
- Job Summary: Nuclear medicine technologists prepare radioactive drugs and administer them to patients for imaging or therapeutic purposes.
- Entry Level Education: Associate's degree
- 2019 Median Pay: $77,950
Occupation: Nurse Anesthetists, Nurse Midwives, and Nurse Practitioners
- Job Summary: Nurse anesthetists, nurse midwives, and nurse practitioners coordinate patient care and may provide primary and specialty healthcare.
- Entry Level Education: Master's degree
- 2019 Median Pay: $115,800
Occupation: Nursing Assistants and Orderlies
- Job Summary: Nursing assistants provide basic care and help patients with activities of daily living. Orderlies transport patients and clean treatment areas.
- See How to Become One
- 2019 Median Pay: $29,640
Occupation: Occupational Health and Safety Specialists and Technicians
- Job Summary: Occupational health and safety specialists and technicians collect data on and analyze many types of work environments and work procedures.
- See How to Become One
- 2019 Median Pay: $70,480
Occupation: Occupational Therapists
- Job Summary:Occupational therapists treat patients who have injuries, illnesses, or disabilities through the therapeutic use of everyday activities.
- Entry Level education: Master's degree
- 2019 Median Pay: $84,950
Occupation: Occupational Therapy Assistants and Aides
- Job Summary: Occupational therapy assistants and aides help patients develop, recover, improve, as well as maintain the skills needed for daily living and working.
- See How to Become One
- $2019 Median Pay: $59,200
Occupation: Opticians
- Job Summary: Opticians help fit eyeglasses and contact lenses, following prescriptions from ophthalmologists and optometrists.
- Entry Level Education: High school diploma or equivalent
- 2019 Median Pay: $37,840
Occupation: Optometrists
- Job Summary: Optometrists diagnose and treat visual problems and manage diseases, injuries, and other disorders of the eyes.
- Entry Level Education: Doctoral or professional degree
- 2019 Median Pay: $115,250
Occupation: Orthotists and Prosthetists
- Job Summary: Orthotists and prosthetists design and fabricate medical supportive devices and measure and fit patients for them.
- Entry Level Education: Master's degree
- 2019 Median Pay: $68,410
Occupation: Pharmacists
- Job Summary: Pharmacists dispense prescription medications to patients and offer expertise in the safe use of prescriptions.
- Entry Level Education: Doctoral or professional degree
- 2019 Median Pay: $128,090
Occupation Pharmacy Technicians
- Job Summary: Pharmacy technicians help pharmacists dispense prescription medication to customers or health professionals.
- Entry Level education: High school diploma or equivalent
- 2019 Median Pay: $33,950
Occupation: Phlebotomists
- Job Summary: Phlebotomists draw blood for tests, transfusions, research, or blood donations.
- Entry Level Education: Postsecondary nondegree award
- 2019 Median Pay: $35,510
Occupation: Physical Therapist Assistants and Aides
- Job Summary: Physical therapist assistants and aides are supervised by physical therapists to help patients regain movement and manage pain after injuries and illnesses.
- See How to Become One
- 2019 Median Pay: $48,990
Occupation: Physical Therapists
- Job Summary: Physical therapists help injured or ill people improve movement and manage pain.
- Entry Level Education: Doctoral or professional degree
- 2019 Median Pay: $89,440
Occupation: Physician Assistants
- Job Summary: Physician assistants practice medicine on teams with physicians, surgeons, and other healthcare workers.
- Entry Level Education: Master's degree
- 2019 Median Pay: $112,260
Occupation: Physicians and Surgeons
- Job Summary: Physicians and surgeons diagnose and treat injuries or illnesses.
- Entry Level Education: Doctoral or professional degree
- 2019 Median Pay: is equal to or greater than $208,000 per year.
Occupation: Podiatrists
- Job Summary: Podiatrists provide medical and surgical care for people with foot, ankle, and lower leg problems.
- Entry Level Education: Doctoral or professional degree
- 2019 Median Pay: $126,240
Occupation: Psychiatric Technicians and Aides
- Job Summary: Psychiatric technicians and aides care for people who have mental illness and developmental disabilities.
- See How to Become One
- 2019 Median Pay: $32,020
Occupation: Radiation Therapists
- Job Summary: Radiation therapists treat cancer and other diseases in patients by administering radiation treatments.
- Entry Level Education: Associate's degree
- 2019 Median Pay: $85,560
Occupation Radiologic and MRI Technologists
- Job Summary: Radiologic technologists perform diagnostic imaging examinations on patients. MRI technologists operate magnetic resonance imaging (MRI) scanners to create diagnostic images.
- Entry Level Education: Associate's degree
- 2019 Median Pay: $62,280
Occupation: Recreational Therapists
- Job Summary: Recreational therapists plan, direct, and coordinate recreation-based treatment programs for people with disabilities, injuries, or illnesses.
- Entry Level Education: Bachelor's degree
- 2019 Median Pay: $48,220
Occupation: Registered Nurses
- Job Summary: Registered nurses (RNs) provide and coordinate patient care and educate patients and the public about various health conditions.
- Entry Level Education: Bachelor's degree
- 2019 Median Pay: $73,300
Occupation: Respiratory Therapists
- Job Summary: Respiratory therapists care for patients who have trouble breathing—for example, from a chronic respiratory disease, such as asthma or emphysema.
- Entry Level Education: Associate's degree
- 2019 Median Pay: $61,330
Occupation: Speech-Language Pathologists
- Job Summary: Speech-language pathologists assess, diagnose, treat, and help to prevent communication and swallowing disorders in children and adults.
- Entry Level Education: Master's degree
- 2019 Median Pay: $79,120
Occupation: Surgical Technologists
- Job Summary: Surgical technologists assist in surgical operations.
- Entry Level Education: Postsecondary nondegree award
- 2019 Median Pay: $48,300
Occupation Veterinarians
- Job Summary: Veterinarians care for the health of animals and work to protect public health.
- Entry Level Education: Doctoral or professional degree
- 2019 Median Pay: $95,460
Occupation Veterinary Assistants and Laboratory Animal Caretakers
- Job Summary: Veterinary assistants and laboratory animal caretakers handle routine animal care and help scientists, veterinarians, and others with their daily tasks.
- Entry Level Education: High school diploma or equivalent
- 2019 Median Pay: $28,590
Occupation Veterinary Technologists and Technicians
- Job Summary: Veterinary technologists and technicians do medical tests that help diagnose animals’ injuries and illnesses.
- Entry Level Education: Associate's degree
- 2019 Median Pay: $35,320
List of healthcare occupations (by Wikipedia)
Below, a listing of health care professions by medical discipline.
Anesthesiology:
- Anesthesiologist
- Anesthesiology Fellow
- Certified Registered Nurse Anesthetist
- Registered Respiratory Therapist
- Anesthesiologist Assistant
- Cardiologist
- Cardiology Fellow
- Cardiology Physician Assistant
- Cardiac Scientist
- Cardiovascular Technologist
- Intensivist
- Neonatologist
- Critical Care Medicine Physician Assistant
- Critical Care Nurse Practitioner
- Critical Care Registered Nurse
- Critical Care Respiratory Therapist
- Dermatologist
- Dermatology Physician Assistant
- Emergency physician
- Emergency Physician Assistant
- Emergency Nurse Practitioner
- Flight Nurse
- Certified Emergency Registered Nurse
- Certified Emergency Registered Respiratory Therapist
- Emergency Medical Technician - Critical Care Paramedic
- Emergency Medical Technician - Paramedic
- Emergency Medical Technician - Intermediate 99
- Emergency Medical Technician - Intermediate 85
- Emergency Medical Technician - Basic
- Endocrinologist
- Endocrinology Physician Assistant
- Gastroenterologist
- Gastroenterology Physician Assistant
- Genetic Counselor/Counsellor
- Geriatrician
- Geriatric Medicine Physician Assistant
- Gerontological Nurse Practitioner
- Occupational Therapist
- Nephrologist
- Nephrology Physician Assistant
- Dialysis Technician
- Neurologist
- Neurology Physician assistant
- Occupational Therapist
- Speech Language Pathologist
- Audiologist
- Neuropsychologist
- Oncologist
- Oncology Physician Assistant
- Radiation Therapist
- Otolaryngologist (Ear, Nose and Throat physician)
- Otorhinolaryngology Physician assistant
- Healthcare Chaplain
- Pulmonologist
- Pulmonology/Respirology Physician Assistant
- Registered Respiratory Therapist
- General practitioner
- Primary care physician
- Internist
- Physician assistant
- Family nurse practitioner
- Pharmacist
- Neonatalologist
- Pediatrician
- Pediatric Physician Assistant
- Neonatal Nurse Practitioner
- Pediatric Nurse Practitioner
- Occupational Therapist- Neonatal/ Pediatric
- Pediatric Nurse
- Pediatric Respiratory Therapist
- Psychiatrist
- Psychiatry Physician Assistant
- Psychologist
- Psychiatric Nurse Practitioner
- Mental Health Nurse Practitioner
- Occupational Therapist
- Social Worker
- Mental Health Counselor
- Orthopedic Physician
- Orthopedic Physician Assistant
- Sport Psychologist
- Physical Therapist
- Occupational Therapist
- Physical Therapy Assistant
- Occupational Therapy Assistant
- Orthopaedic Technologist or Prosthetist & Orthotist
- Chiropractor
- Biokineticist
- Athletic Trainer
- Yoga Instructor
- Radiologist
- Radiology Physician Assistant
- Radiotherapist also known as a Radiation Therapist or Therapeutic Radiographer
- Radiographer, also known as a Radiologic Technologist
- Obstetrician
- Gynaecologist
- OB/GYN Physician Assistant
- Women's Health Nurse Practitioner
- Nurse-Midwife
- Midwife
- Lactation consultant
- General Doctor
- Bariatric Surgeon
- Cardiothoracic surgeon
- Cardiac Surgeon
- Hepatic Biliary Pancreatic Surgeon
- Neurosurgeon
- Podiatric Surgeon
- Surgery Physician Assistant
- Urologist
- Urology Physician Assistant
See also: Media related to Healthcare occupations at Wikimedia Commons
Drug Development, focusing on Covid-19 Vaccines
- YouTube Video: How safe is the Pfizer COVID-19 vaccine? (Good Morning America)
- YouTube Video: Inside the Lab That Invented the COVID-19 Vaccine
- YouTube Video: How COVID Kills Some People But Not Others - I'm a Lung Doctor (MEDICAL TRUTH) | Coronavirus
Drug Development:
Drug development is the process of bringing a new pharmaceutical drug to the market once a lead compound has been identified through the process of drug discovery. It includes preclinical research on microorganisms and animals, filing for regulatory status, such as via the United States Food and Drug Administration for an investigational new drug to initiate clinical trials on humans, and may include the step of obtaining regulatory approval with a new drug application to market the drug.
Click on any of the following blue hyperlinks for more about the Drug Development Process:
Below: a color-coded map by Covid-19 Approval Process:
Drug development is the process of bringing a new pharmaceutical drug to the market once a lead compound has been identified through the process of drug discovery. It includes preclinical research on microorganisms and animals, filing for regulatory status, such as via the United States Food and Drug Administration for an investigational new drug to initiate clinical trials on humans, and may include the step of obtaining regulatory approval with a new drug application to market the drug.
Click on any of the following blue hyperlinks for more about the Drug Development Process:
- New chemical entity development
- Cost
- Valuation
- Success rate
- Computing initiatives
- See also:
- Council for International Organizations of Medical Sciences
- Drug design
- Drug repositioning
- Pharmaceutical engineering
- Pharmaceutical manufacturing
- Generic drug
- International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use, a consensus between the U.S. Food and Drug Administration (FDA), EU, and Japan.
- List of pharmaceutical companies International Union of Basic and Clinical Pharmacology
Below: a color-coded map by Covid-19 Approval Process:
A COVID‑19 vaccine is any of several different vaccine technologies intended to provide acquired immunity against coronavirus disease 2019 (COVID‑19).
Previous work to develop a vaccine against the coronavirus diseases SARS and MERS established knowledge about the structure and function of coronaviruses, which accelerated development during early 2020 of varied technology platforms for a COVID‑19 vaccine.
As of mid-December 2020, 57 vaccine candidates were in clinical research: namely, 40 in Phase I–II trials and 17 in Phase II–III trials. No vaccine candidate had fully completed a Phase III trial or obtained licensure, as of 13 December.
In November 2020, Pfizer Inc and BioNTech, Moderna, the University of Oxford (in collaboration with AstraZeneca), and the Gamaleya Institute announced positive results from interim analyses of their Phase III vaccine trials.
As of 15 December, the following 11 countries have approved the Pfizer-BioNTech COVID-19 vaccine for emergency use:
Furthermore, Bahrain gave emergency marketing authorization for the vaccine manufactured by Sinopharm, followed by the United Arab Emirates.
By December, more than 10 billion vaccine doses had been preordered by countries. The manufacturers of three vaccines closest to global distribution – Pfizer, Moderna, and AstraZeneca – predicted a manufacturing capacity of 5.3 billion doses in 2021, which could be used to vaccinate about 3 billion people (as the vaccines require two doses for a protective effect against COVID-19).
Due to the high demand in preorders for 2021, people in low-income developing countries may not receive vaccinations from these manufacturers until 2023 or 2024, increasing the use of the COVAX initiative to supply vaccines equitably.
Click on any of the following blue hyperlinks for more about the Covid-19 Vaccines Approval Process:
Previous work to develop a vaccine against the coronavirus diseases SARS and MERS established knowledge about the structure and function of coronaviruses, which accelerated development during early 2020 of varied technology platforms for a COVID‑19 vaccine.
As of mid-December 2020, 57 vaccine candidates were in clinical research: namely, 40 in Phase I–II trials and 17 in Phase II–III trials. No vaccine candidate had fully completed a Phase III trial or obtained licensure, as of 13 December.
In November 2020, Pfizer Inc and BioNTech, Moderna, the University of Oxford (in collaboration with AstraZeneca), and the Gamaleya Institute announced positive results from interim analyses of their Phase III vaccine trials.
As of 15 December, the following 11 countries have approved the Pfizer-BioNTech COVID-19 vaccine for emergency use:
- United Kingdom,
- Bahrain,
- United Arab Emirates,
- Canada,
- Saudi Arabia,
- USA,
- Mexico,
- Kuwait,
- Singapore,
- Jordan,
- and Oman
Furthermore, Bahrain gave emergency marketing authorization for the vaccine manufactured by Sinopharm, followed by the United Arab Emirates.
By December, more than 10 billion vaccine doses had been preordered by countries. The manufacturers of three vaccines closest to global distribution – Pfizer, Moderna, and AstraZeneca – predicted a manufacturing capacity of 5.3 billion doses in 2021, which could be used to vaccinate about 3 billion people (as the vaccines require two doses for a protective effect against COVID-19).
Due to the high demand in preorders for 2021, people in low-income developing countries may not receive vaccinations from these manufacturers until 2023 or 2024, increasing the use of the COVAX initiative to supply vaccines equitably.
Click on any of the following blue hyperlinks for more about the Covid-19 Vaccines Approval Process:
- Synopsis and history
- Global development
- WHO COVID-19 trials
- Partnerships, competition, and distribution
- Compressed timelines
- Technology platforms
- Vaccine candidates
- Potential limitations
- Proposed challenge studies
- Emergency use authorization
- Licensure
- Commercialization and equitable access
- Supply chain
- Liability
- Misinformation
- See also:
- 2009 swine flu pandemic vaccine
- COVID-19 drug development
- COVID-19 drug repurposing research
- COVID-19 pandemic
- Phases of clinical research
- Respiratory disease
- "Coronavirus Vaccine Tracker". The New York Times.
- COVID-19 vaccine tracker, Regulatory Focus
- "STAT's Covid-19 Drugs and Vaccines Tracker". Stat.
- "Biopharma Leaders Unite to Stand with Science" (Press release). 8 September 2020 – via Business Wire.
- "Protocol mRNA-1273-P301" (PDF). Moderna.
- "Protocol C4591001 PF-07302048 (BNT162 RNA-Based COVID-19 Vaccines)" (PDF). Pfizer.
- "Protocol AZD1222 – D8110C00001" (PDF). AstraZeneca.
- Levine, Hallie (23 September 2020). "The 5 Stages of COVID-19 Vaccine Development: What You Need to Know About How a Clinical Trial Works". Johnson & Johnson.
- "COVID-19 vaccines: development, evaluation, approval and monitoring". European Medicines Agency.
- "Vaccine Development – 101". U.S. Food and Drug Administration (FDA).
Dentistry, including Dental Specialties
- YouTube Video: So, YouWant to be a Dentist?
- YouTube Video: The Ten Dental Specialties
- YouTube Video: Invisalign vs Braces: Tips from a Board Certified Orthodontist
Dentistry, also known as dental medicine and oral medicine, is a branch of medicine that consists of the study, diagnosis, prevention, and treatment of diseases, disorders, and conditions of the oral cavity, commonly in the dentition but also the oral mucosa, and of adjacent and related structures and tissues, particularly in the maxillofacial (jaw and facial) area.
Although primarily associated with teeth among the general public, the field of dentistry or dental medicine is not limited to teeth but includes other aspects of the craniofacial complex including the temporomandibular joint and other supporting, muscular, lymphatic, nervous, vascular, and anatomical structures.
Dentistry is often also understood to subsume the now largely defunct medical specialty of stomatology (the study of the mouth and its disorders and diseases) for which reason the two terms are used interchangeably in certain regions.
Dental treatments are carried out by a dental team, which often consists of a dentist and dental auxiliaries (dental assistants, dental hygienists, dental technicians, as well as dental therapists). Most dentists either work in private practices (primary care), dental hospitals or (secondary care) institutions (prisons, armed forces bases, etc.).
The history of dentistry is almost as ancient as the history of humanity and civilization with the earliest evidence dating from 7000 BC to 5500 BC. Skeletal remains from Mehgarh (now in Pakistan) dated to that time show evidence of teeth having been drilled with flint tools to remove decay, a method found to be "surprisingly effective".
Dentistry is thought to have been the first specialization in medicine. The modern movement of evidence-based dentistry calls for the use of high-quality scientific evidence to guide decision-making.
Terminology:
The term dentistry comes from dentist, which comes from French dentiste, which comes from the French and Latin words for tooth. The term for the associated scientific study of teeth is odontology – the study of the structure, development, and abnormalities of the teeth.
Dental treatment:
Dentistry usually encompasses practices related to the oral cavity. According to the World Health Organization, oral diseases are major public health problems due to their high incidence and prevalence across the globe, with the disadvantaged affected more than other socio-economic groups.
The majority of dental treatments are carried out to prevent or treat the two most common oral diseases which are dental caries (tooth decay) and periodontal disease (gum disease or pyorrhea).
Common treatments involve the restoration of teeth, extraction or surgical removal of teeth, scaling and root planing, endodontic root canal treatment and cosmetic dentistry
All dentists in the United States undergo at least three years of undergraduate studies, but nearly all complete a bachelor's degree. This schooling is followed by four years of dental school to qualify as a "Doctor of Dental Surgery" (DDS) or "Doctor of Dental Medicine" (DMD).
Specialization in dentistry is available in the fields of Anesthesiology, Dental Public Health, Endodontics, Oral Radiology, Oral Maxillofacial Surgery, Oral Medicine, Orofacial Pain, Pathology, Orthodontics, Pediatric Dentistry, Periodontics, and Prosthodontics. (SEE BELOW)
By nature of their general training they can carry out the majority of dental treatments such as restorative (fillings, crowns, bridges), prosthetic (dentures), endodontic (root canal) therapy, periodontal (gum) therapy, and extraction of teeth, as well as performing examinations, radiographs (x-rays), and diagnosis.
Dentists can also prescribe medications such as antibiotics, sedatives, and any other drugs used in patient management. Depending on their licensing boards, general dentists may be required to complete additional training to perform sedation, dental implants, etc.
Dentists also encourage prevention of oral diseases through proper hygiene and regular, twice or more yearly, checkups for professional cleaning and evaluation. Oral infections and inflammations may affect overall health and conditions in the oral cavity may be indicative of systemic diseases, such as osteoporosis, diabetes, celiac disease or cancer.
Many studies have also shown that gum disease is associated with an increased risk of diabetes, heart disease, and preterm birth. The concept that oral health can affect systemic health and disease is referred to as "oral-systemic health".
Education and licensing:
Main article: Dentistry throughout the world
John M. Harris started the world's first dental school in Bainbridge, Ohio, and helped to establish dentistry as a health profession. It opened on 21 February 1828, and today is a dental museum. The first dental college, Baltimore College of Dental Surgery, opened in Baltimore, Maryland, US in 1840. The second in the United States was the Ohio College of Dental Surgery, established in Cincinnati, Ohio, in 1845. The Philadelphia College of Dental Surgery followed in 1852. In 1907, Temple University accepted a bid to incorporate the school.
Studies show that dentists that graduated from different countries,[ or even from different dental schools in one country, may make different clinical decisions for the same clinical condition. For example, dentists that graduated from Israeli dental schools may recommend the removal of asymptomatic impacted third molar (wisdom teeth) more often than dentists that graduated from Latin American or Eastern European dental schools.
In the United Kingdom, the 1878 British Dentists Act and 1879 Dentists Register limited the title of "dentist" and "dental surgeon" to qualified and registered practitioners. However, others could legally describe themselves as "dental experts" or "dental consultants". The practice of dentistry in the United Kingdom became fully regulated with the 1921 Dentists Act, which required the registration of anyone practising dentistry.
The British Dental Association, formed in 1880 with Sir John Tomes as president, played a major role in prosecuting dentists practicing illegally. Dentists in the United Kingdom are now regulated by the General Dental Council.
In Korea, Taiwan, Japan, Finland, Sweden, Brazil, Chile, the United States, and Canada, a dentist is a healthcare professional qualified to practice dentistry after graduating with a degree of either Doctor of Dental Surgery (DDS) or Doctor of Dental Medicine (DMD). This is equivalent to the Bachelor of Dental Surgery/Baccalaureus Dentalis Chirurgiae (BDS, BDent, BChD, BDSc) that is awarded in the UK and British Commonwealth countries.
In most western countries, to become a qualified dentist one must usually complete at least four years of postgraduate study; within the European Union the education has to be at least five years. Dentists usually complete between five and eight years of post-secondary education before practicing. Though not mandatory, many dentists choose to complete an internship or residency focusing on specific aspects of dental care after they have received their dental degree.
Specialties:
Main article: Specialty (dentistry)
Some dentists undertake further training after their initial degree in order to specialize. Exactly which subjects are recognized by dental registration bodies varies according to location. Examples include:
Modern Denistry:
It was between 1650 and 1800 that the science of modern dentistry developed. The English physician Thomas Browne in his A Letter to a Friend (c. 1656 pub. 1690) made an early dental observation with characteristic humor:
"The Egyptian Mummies that I have seen, have had their Mouths open, and somewhat gaping, which affordeth a good opportunity to view and observe their Teeth, wherein 'tis not easy to find any wanting or decayed: and therefore in Egypt, where one Man practiced but one Operation, or the Diseases but of single Parts, it must needs be a barren Profession to confine unto that of drawing of Teeth, and little better than to have been Tooth-drawer unto King Pyrrhus, who had but two in his Head."
The French surgeon Pierre Fauchard became known as the "father of modern dentistry". Despite the limitations of the primitive surgical instruments during the late 17th and early 18th century, Fauchard was a highly skilled surgeon who made remarkable improvisations of dental instruments, often adapting tools from watchmakers, jewelers and even barbers, that he thought could be used in dentistry. He introduced dental fillings as treatment for dental cavities. He asserted that sugar-derived acids like tartaric acid were responsible for dental decay, and also suggested that tumors surrounding the teeth and in the gums could appear in the later stages of tooth decay.
Fauchard was the pioneer of dental prosthesis, and he invented many methods to replace lost teeth. He suggested that substitutes could be made from carved blocks of ivory or bone. He also introduced dental braces, although they were initially made of gold, he discovered that the teeth position could be corrected as the teeth would follow the pattern of the wires.
Waxed linen or silk threads were usually employed to fasten the braces. His contributions to the world of dental science consist primarily of his 1728 publication Le chirurgien dentiste or The Surgeon Dentist. The French text included "basic oral anatomy and function, dental construction, and various operative and restorative techniques, and effectively separated dentistry from the wider category of surgery".
After Fauchard, the study of dentistry rapidly expanded. Two important books, Natural History of Human Teeth (1771) and Practical Treatise on the Diseases of the Teeth (1778), were published by British surgeon John Hunter. In 1763 he entered into a period of collaboration with the London-based dentist James Spence.
Hunter began to theorize about the possibility of tooth transplants from one person to another. He realized that the chances of a successful tooth transplant (initially, at least) would be improved if the donor tooth was as fresh as possible and was matched for size with the recipient. These principles are still used in the transplantation of internal organs. Hunter conducted a series of pioneering operations, in which he attempted a tooth transplant.
Although the donated teeth never properly bonded with the recipients' gums, one of Hunter's patients stated that he had three which lasted for six years, a remarkable achievement for the period.
Major advances were made in the 19th century, and dentistry evolved from a trade to a profession. The profession came under government regulation by the end of the 19th century.
In the UK the Dentist Act was passed in 1878 and the British Dental Association formed in 1879. In the same year, Francis Brodie Imlach was the first ever dentist to be elected President of the Royal College of Surgeons (Edinburgh), raising dentistry onto a par with clinical surgery for the first time.
Hazards in modern dentistry:
Main article: Occupational hazards in dentistry
Long term occupational noise exposure can contribute to permanent hearing loss, which is referred to as noise-induced hearing loss (NIHL) and tinnitus. Noise exposure can cause excessive stimulation of the hearing mechanism, which damages the delicate structures of the inner ear.
NIHL can occur when an individual is exposed to sound levels above 90 dBA according to the Occupational Safety and Health Administration (OSHA). Regulations state that the permissible noise exposure levels for individuals is 90 dBA.
For the National Institute for Occupational Safety and Health (NIOSH), exposure limits are set to 85 dBA. Exposures below 85 dBA are not considered to be hazardous. Time limits are placed on how long an individual can stay in an environment above 85 dBA before it causes hearing loss. OSHA places that limitation at 8 hours for 85 dBA. The exposure time becomes shorter as the dBA level increases.
Within the field of dentistry, a variety of cleaning tools are used including piezoelectric and sonic scalers, and ultrasonic scalers and cleaners. While a majority of the tools do not exceed 75 dBA, prolonged exposure over many years can lead to hearing loss or complaints of tinnitus. Few dentists have reported using personal hearing protective devices, which could offset any potential hearing loss or tinnitus.
Evidence-based dentistry:
Main article: Evidence-based Dentistry
There is a movement in modern dentistry to place a greater emphasis on high-quality scientific evidence in decision-making. Evidence-based dentistry (EBD) uses current scientific evidence to guide decisions. It is an approach to oral health that requires the application and examination of relevant scientific data related to the patient's oral and medical health.
Along with the dentist's professional skill and expertise, EBD allows dentists to stay up to date on the latest procedures and patients to receive improved treatment.
A new paradigm for medical education designed to incorporate current research into education and practice was developed to help practitioners provide the best care for their patients.
It was first introduced by Gordon Guyatt and the Evidence-Based Medicine Working Group at McMaster University in Ontario, Canada in the 1990s. It is part of the larger movement toward evidence-based medicine and other evidence-based practices.
Ethical and medicolegal issues:
Dentistry is unique in that it requires dental students to have competence-based clinical skills that can only be acquired through specialized laboratory training and direct patient care. This necessitates the need for a scientific and professional basis of care with a foundation of research-based education. The accreditation of dental schools plays a role in enhancing the quality of dental education.
There are controversial articles that are not evidence based and rely on opinions that are published and attract attention.
See also:
Although primarily associated with teeth among the general public, the field of dentistry or dental medicine is not limited to teeth but includes other aspects of the craniofacial complex including the temporomandibular joint and other supporting, muscular, lymphatic, nervous, vascular, and anatomical structures.
Dentistry is often also understood to subsume the now largely defunct medical specialty of stomatology (the study of the mouth and its disorders and diseases) for which reason the two terms are used interchangeably in certain regions.
Dental treatments are carried out by a dental team, which often consists of a dentist and dental auxiliaries (dental assistants, dental hygienists, dental technicians, as well as dental therapists). Most dentists either work in private practices (primary care), dental hospitals or (secondary care) institutions (prisons, armed forces bases, etc.).
The history of dentistry is almost as ancient as the history of humanity and civilization with the earliest evidence dating from 7000 BC to 5500 BC. Skeletal remains from Mehgarh (now in Pakistan) dated to that time show evidence of teeth having been drilled with flint tools to remove decay, a method found to be "surprisingly effective".
Dentistry is thought to have been the first specialization in medicine. The modern movement of evidence-based dentistry calls for the use of high-quality scientific evidence to guide decision-making.
Terminology:
The term dentistry comes from dentist, which comes from French dentiste, which comes from the French and Latin words for tooth. The term for the associated scientific study of teeth is odontology – the study of the structure, development, and abnormalities of the teeth.
Dental treatment:
Dentistry usually encompasses practices related to the oral cavity. According to the World Health Organization, oral diseases are major public health problems due to their high incidence and prevalence across the globe, with the disadvantaged affected more than other socio-economic groups.
The majority of dental treatments are carried out to prevent or treat the two most common oral diseases which are dental caries (tooth decay) and periodontal disease (gum disease or pyorrhea).
Common treatments involve the restoration of teeth, extraction or surgical removal of teeth, scaling and root planing, endodontic root canal treatment and cosmetic dentistry
All dentists in the United States undergo at least three years of undergraduate studies, but nearly all complete a bachelor's degree. This schooling is followed by four years of dental school to qualify as a "Doctor of Dental Surgery" (DDS) or "Doctor of Dental Medicine" (DMD).
Specialization in dentistry is available in the fields of Anesthesiology, Dental Public Health, Endodontics, Oral Radiology, Oral Maxillofacial Surgery, Oral Medicine, Orofacial Pain, Pathology, Orthodontics, Pediatric Dentistry, Periodontics, and Prosthodontics. (SEE BELOW)
By nature of their general training they can carry out the majority of dental treatments such as restorative (fillings, crowns, bridges), prosthetic (dentures), endodontic (root canal) therapy, periodontal (gum) therapy, and extraction of teeth, as well as performing examinations, radiographs (x-rays), and diagnosis.
Dentists can also prescribe medications such as antibiotics, sedatives, and any other drugs used in patient management. Depending on their licensing boards, general dentists may be required to complete additional training to perform sedation, dental implants, etc.
Dentists also encourage prevention of oral diseases through proper hygiene and regular, twice or more yearly, checkups for professional cleaning and evaluation. Oral infections and inflammations may affect overall health and conditions in the oral cavity may be indicative of systemic diseases, such as osteoporosis, diabetes, celiac disease or cancer.
Many studies have also shown that gum disease is associated with an increased risk of diabetes, heart disease, and preterm birth. The concept that oral health can affect systemic health and disease is referred to as "oral-systemic health".
Education and licensing:
Main article: Dentistry throughout the world
John M. Harris started the world's first dental school in Bainbridge, Ohio, and helped to establish dentistry as a health profession. It opened on 21 February 1828, and today is a dental museum. The first dental college, Baltimore College of Dental Surgery, opened in Baltimore, Maryland, US in 1840. The second in the United States was the Ohio College of Dental Surgery, established in Cincinnati, Ohio, in 1845. The Philadelphia College of Dental Surgery followed in 1852. In 1907, Temple University accepted a bid to incorporate the school.
Studies show that dentists that graduated from different countries,[ or even from different dental schools in one country, may make different clinical decisions for the same clinical condition. For example, dentists that graduated from Israeli dental schools may recommend the removal of asymptomatic impacted third molar (wisdom teeth) more often than dentists that graduated from Latin American or Eastern European dental schools.
In the United Kingdom, the 1878 British Dentists Act and 1879 Dentists Register limited the title of "dentist" and "dental surgeon" to qualified and registered practitioners. However, others could legally describe themselves as "dental experts" or "dental consultants". The practice of dentistry in the United Kingdom became fully regulated with the 1921 Dentists Act, which required the registration of anyone practising dentistry.
The British Dental Association, formed in 1880 with Sir John Tomes as president, played a major role in prosecuting dentists practicing illegally. Dentists in the United Kingdom are now regulated by the General Dental Council.
In Korea, Taiwan, Japan, Finland, Sweden, Brazil, Chile, the United States, and Canada, a dentist is a healthcare professional qualified to practice dentistry after graduating with a degree of either Doctor of Dental Surgery (DDS) or Doctor of Dental Medicine (DMD). This is equivalent to the Bachelor of Dental Surgery/Baccalaureus Dentalis Chirurgiae (BDS, BDent, BChD, BDSc) that is awarded in the UK and British Commonwealth countries.
In most western countries, to become a qualified dentist one must usually complete at least four years of postgraduate study; within the European Union the education has to be at least five years. Dentists usually complete between five and eight years of post-secondary education before practicing. Though not mandatory, many dentists choose to complete an internship or residency focusing on specific aspects of dental care after they have received their dental degree.
Specialties:
Main article: Specialty (dentistry)
Some dentists undertake further training after their initial degree in order to specialize. Exactly which subjects are recognized by dental registration bodies varies according to location. Examples include:
- Cosmetic dentistry- Focuses on improving the appearance of the mouth,teeth and smile.
- Anesthesiology – The specialty of dentistry that deals with the advanced use of general anesthesia, sedation and pain management to facilitate dental procedures.
- Dental public health – The study of epidemiology and social health policies relevant to oral health.
- Endodontics (also called endodontology) – Root canal therapy and study of diseases of the dental pulp and periapical tissues.
- Forensic odontology – The gathering and use of dental evidence in law. This may be performed by any dentist with experience or training in this field. The function of the forensic dentist is primarily documentation and verification of identity.
- Geriatric dentistry or geriodontics – The delivery of dental care to older adults involving the diagnosis, prevention, and treatment of problems associated with normal aging and age-related diseases as part of an interdisciplinary team with other health care professionals.
- Oral and maxillofacial pathology – The study, diagnosis, and sometimes the treatment of oral and maxillofacial related diseases.
- Oral and maxillofacial radiology – The study and radiologic interpretation of oral and maxillofacial diseases.
- Oral and maxillofacial surgery (also called oral surgery) – Extractions, implants, and surgery of the jaws, mouth and face.
- Oral biology – Research in dental and craniofacial biology
- Oral Implantology – The art and science of replacing extracted teeth with dental implants.
- Oral medicine – The clinical evaluation and diagnosis of oral mucosal diseases
- Orthodontics and dentofacial orthopedics – The straightening of teeth and modification of midface and mandibular growth.
- Pediatric dentistry (also called pedodontics) – Dentistry for children
- Periodontology (also called periodontics) – The study and treatment of diseases of the periodontium (non-surgical and surgical) as well as placement and maintenance of dental implants
- Prosthodontics (also called prosthetic dentistry) – Dentures, bridges and the restoration of implants.
- Some prosthodontists super-specialize in Maxillofacial Prosthetics, which is the discipline originally concerned with the rehabilitation of patients with congenital facial and oral defects such as cleft lip and palate or patients born with an underdeveloped ear (microtia). Today, most Maxillofacial Prosthodontists return function and esthetics to patients with acquired defects secondary to surgical removal of head and neck tumors, or secondary to trauma from war or motor vehicle accidents.
- Special needs dentistry (also called special care dentistry) – Dentistry for those with developmental and acquired disabilities.
- Sports dentistry – the branch of sports medicine dealing with prevention and treatment of dental injuries and oral diseases associated with sports and exercise. The sports dentist works as an individual consultant or as a member of the Sports Medicine Team.
- Veterinary dentistry – The field of dentistry applied to the care of animals. It is a specialty of veterinary medicine.
Modern Denistry:
It was between 1650 and 1800 that the science of modern dentistry developed. The English physician Thomas Browne in his A Letter to a Friend (c. 1656 pub. 1690) made an early dental observation with characteristic humor:
"The Egyptian Mummies that I have seen, have had their Mouths open, and somewhat gaping, which affordeth a good opportunity to view and observe their Teeth, wherein 'tis not easy to find any wanting or decayed: and therefore in Egypt, where one Man practiced but one Operation, or the Diseases but of single Parts, it must needs be a barren Profession to confine unto that of drawing of Teeth, and little better than to have been Tooth-drawer unto King Pyrrhus, who had but two in his Head."
The French surgeon Pierre Fauchard became known as the "father of modern dentistry". Despite the limitations of the primitive surgical instruments during the late 17th and early 18th century, Fauchard was a highly skilled surgeon who made remarkable improvisations of dental instruments, often adapting tools from watchmakers, jewelers and even barbers, that he thought could be used in dentistry. He introduced dental fillings as treatment for dental cavities. He asserted that sugar-derived acids like tartaric acid were responsible for dental decay, and also suggested that tumors surrounding the teeth and in the gums could appear in the later stages of tooth decay.
Fauchard was the pioneer of dental prosthesis, and he invented many methods to replace lost teeth. He suggested that substitutes could be made from carved blocks of ivory or bone. He also introduced dental braces, although they were initially made of gold, he discovered that the teeth position could be corrected as the teeth would follow the pattern of the wires.
Waxed linen or silk threads were usually employed to fasten the braces. His contributions to the world of dental science consist primarily of his 1728 publication Le chirurgien dentiste or The Surgeon Dentist. The French text included "basic oral anatomy and function, dental construction, and various operative and restorative techniques, and effectively separated dentistry from the wider category of surgery".
After Fauchard, the study of dentistry rapidly expanded. Two important books, Natural History of Human Teeth (1771) and Practical Treatise on the Diseases of the Teeth (1778), were published by British surgeon John Hunter. In 1763 he entered into a period of collaboration with the London-based dentist James Spence.
Hunter began to theorize about the possibility of tooth transplants from one person to another. He realized that the chances of a successful tooth transplant (initially, at least) would be improved if the donor tooth was as fresh as possible and was matched for size with the recipient. These principles are still used in the transplantation of internal organs. Hunter conducted a series of pioneering operations, in which he attempted a tooth transplant.
Although the donated teeth never properly bonded with the recipients' gums, one of Hunter's patients stated that he had three which lasted for six years, a remarkable achievement for the period.
Major advances were made in the 19th century, and dentistry evolved from a trade to a profession. The profession came under government regulation by the end of the 19th century.
In the UK the Dentist Act was passed in 1878 and the British Dental Association formed in 1879. In the same year, Francis Brodie Imlach was the first ever dentist to be elected President of the Royal College of Surgeons (Edinburgh), raising dentistry onto a par with clinical surgery for the first time.
Hazards in modern dentistry:
Main article: Occupational hazards in dentistry
Long term occupational noise exposure can contribute to permanent hearing loss, which is referred to as noise-induced hearing loss (NIHL) and tinnitus. Noise exposure can cause excessive stimulation of the hearing mechanism, which damages the delicate structures of the inner ear.
NIHL can occur when an individual is exposed to sound levels above 90 dBA according to the Occupational Safety and Health Administration (OSHA). Regulations state that the permissible noise exposure levels for individuals is 90 dBA.
For the National Institute for Occupational Safety and Health (NIOSH), exposure limits are set to 85 dBA. Exposures below 85 dBA are not considered to be hazardous. Time limits are placed on how long an individual can stay in an environment above 85 dBA before it causes hearing loss. OSHA places that limitation at 8 hours for 85 dBA. The exposure time becomes shorter as the dBA level increases.
Within the field of dentistry, a variety of cleaning tools are used including piezoelectric and sonic scalers, and ultrasonic scalers and cleaners. While a majority of the tools do not exceed 75 dBA, prolonged exposure over many years can lead to hearing loss or complaints of tinnitus. Few dentists have reported using personal hearing protective devices, which could offset any potential hearing loss or tinnitus.
Evidence-based dentistry:
Main article: Evidence-based Dentistry
There is a movement in modern dentistry to place a greater emphasis on high-quality scientific evidence in decision-making. Evidence-based dentistry (EBD) uses current scientific evidence to guide decisions. It is an approach to oral health that requires the application and examination of relevant scientific data related to the patient's oral and medical health.
Along with the dentist's professional skill and expertise, EBD allows dentists to stay up to date on the latest procedures and patients to receive improved treatment.
A new paradigm for medical education designed to incorporate current research into education and practice was developed to help practitioners provide the best care for their patients.
It was first introduced by Gordon Guyatt and the Evidence-Based Medicine Working Group at McMaster University in Ontario, Canada in the 1990s. It is part of the larger movement toward evidence-based medicine and other evidence-based practices.
Ethical and medicolegal issues:
Dentistry is unique in that it requires dental students to have competence-based clinical skills that can only be acquired through specialized laboratory training and direct patient care. This necessitates the need for a scientific and professional basis of care with a foundation of research-based education. The accreditation of dental schools plays a role in enhancing the quality of dental education.
There are controversial articles that are not evidence based and rely on opinions that are published and attract attention.
See also:
Organ Transplantation from a Donor using Transplantable Human Organs, including a List of Human Organs
TOP: Internal Organs of the human body
BOTTOM: Heart Transplant Procedure courtesy of Mayo Clinic
- YouTube Video of Lung Transplant Surgery at Henry Ford Hospital, Detroit MI
- YouTube Video of Kidney Transplant Surgery at UCLA, Los Angeles CA
- YouTube Video of Mayo Clinic’s First Face Transplant: The Surgery
TOP: Internal Organs of the human body
BOTTOM: Heart Transplant Procedure courtesy of Mayo Clinic
Click Here For A List of Transplantable organs and tissues
Organ Transplantation
Organ transplantation is a medical procedure in which an organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ. The donor and recipient may be at the same location, or organs may be transported from a donor site to another location.
Organs and/or tissues that are transplanted within the same person's body are called autografts. Transplants that are recently performed between two subjects of the same species are called allografts. Allografts can either be from a living or cadaveric source.
Organs that have been successfully transplanted include the heart, kidneys, liver, lungs, pancreas, intestine, thymus and uterus. Tissues include bones, tendons (both referred to as musculoskeletal grafts), corneae, skin, heart valves, nerves and veins.
Worldwide, the kidneys are the most commonly transplanted organs, followed by the liver and then the heart. Corneae and musculoskeletal grafts are the most commonly transplanted tissues; these outnumber organ transplants by more than tenfold.
Organ donors may be living, brain dead, or dead via circulatory death. Tissue may be recovered from donors who die of circulatory death, as well as of brain death – up to 24 hours past the cessation of heartbeat. Unlike organs, most tissues (with the exception of corneas) can be preserved and stored for up to five years, meaning they can be "banked".
Transplantation raises a number of bioethical issues, including the definition of death, when and how consent should be given for an organ to be transplanted, and payment for organs for transplantation. Other ethical issues include transplantation tourism (medical tourism) and more broadly the socio-economic context in which organ procurement or transplantation may occur. A particular problem is organ trafficking. There is also the ethical issue of not holding out false hope to patients.
Transplantation medicine is one of the most challenging and complex areas of modern medicine. Some of the key areas for medical management are the problems of transplant rejection, during which the body has an immune response to the transplanted organ, possibly leading to transplant failure and the need to immediately remove the organ from the recipient.
When possible, transplant rejection can be reduced through serotyping to determine the most appropriate donor-recipient match and through the use of immunosuppressant drugs.
Click on any of the following blue hyperlinks for more about Organ Transplantation:
Organ donation:
Organ donation is the process when a person allows an organ of their own to be removed and transplanted to another person, legally, either by consent while the donor is alive or dead with the assent of the next of kin.
Donation may be for research or, more commonly, healthy transplantable organs and tissues may be donated to be transplanted into another person.
Common transplantations include:
Some organs and tissues can be donated by living donors, such as a kidney or part of the liver, part of the pancreas, part of the lungs or part of the intestines, but most donations occur after the donor has died.
In 2019, Spain had the highest donor rate in the world at 46.91 per million people, followed by the US (36.88 per million), Croatia (34.63 per million), Portugal (33.8 per million), and France (33.25 per million).
As of February 2, 2019, there were 120,000 people waiting for life-saving organ transplants in the US. Of these, 74,897 people were active candidates waiting for a donor. While views of organ donation are positive, there is a large gap between the numbers of registered donors compared to those awaiting organ donations on a global level.
To increase the number of organ donors, especially among underrepresented populations, current approaches include the use of optimized social network interventions, exposing tailored educational content about organ donation to target social media users.
Process in the United States:
Organ donors are usually dead at the time of donation, but may be living. For living donors, organ donation typically involves extensive testing before the donation, including psychological evaluation to determine whether the would-be donor understands and consents to the donation.
On the day of the donation, the donor and the recipient arrive at the hospital, just like they would for any other major surgery.
For dead donors, the process begins with verifying that the person is undoubtedly deceased, determining whether any organs could be donated, and obtaining consent for the donation of any usable organs.
Normally, nothing is done until the person has already died, although if death is inevitable, it is possible to check for consent and to do some simple medical tests shortly beforehand, to help find a matching recipient.
The verification of death is normally done by a neurologist (a physician specializing in brain function) that is not involved in the previous attempts to save the patient's life. This physician has nothing to do with the transplantation process.
Verification of death is often done multiple times, to prevent doctors from overlooking any remaining sign of life, however small. After death, the hospital may keep the body on a mechanical ventilator and use other methods to keep the organs in good condition. Donors and their families are not charged for any expenses related to the donation.
The surgical process depends upon which organs are being donated.
The body is normally restored to as normal an appearance as possible, so that the family can proceed with funeral rites and either cremation or burial.
The lungs are highly vulnerable to injury and thus the most difficult to preserve, with only 15–25% of donated organs utilized.
History:
Further information: List of organ transplant donors and recipients
The first living organ donor in a successful transplant was Ronald Lee Herrick (1931–2010), who donated a kidney to his identical twin brother in 1954. The lead surgeon, Joseph Murray, won the Nobel Prize in Physiology or Medicine in 1990 for advances in organ transplantation.
The youngest organ donor was a baby with anencephaly, born in 2014, who lived for only 100 minutes and donated his kidneys to an adult with renal failure.
The oldest known cornea donor was a 107-year-old Scottish woman, whose corneas were donated after her death in 2016. The oldest known organ donor for an internal organ was a 95-year-old West Virginia man, who donated his liver after he died.
The oldest altruistic living organ donor was an 85-year-old woman in Britain, who donated a kidney to a stranger in 2014 after hearing how many people needed to receive a transplant.
Researchers were able to develop a novel way to transplant human fetal kidneys into anephric rats to overcome a significant obstacle in impeding human fetal organ transplantations. The human fetal kidneys demonstrated both growth and function within the rats.
Brain donation:
Donated brain tissue is a valuable resource for research into brain function, neurodiversity, neuropathology and possible treatments. Both divergent and healthy control brains are needed for comparison. Brain banks typically source tissue from donors that had directly registered with them before their passing, since organ donor registries focus on tissue meant for transplantation.
In the United States the nonprofit Brain Donor Project facilitates this process.
Legislation and global perspectives:
The laws of different countries allow potential donors to permit or refuse donation, or give this choice to relatives. The frequency of donations varies among countries.
Consent process:
The term consent is typically defined as a subject adhering to an agreement of principles and regulations; however, the definition becomes difficult to execute concerning the topic of organ donation, mainly because the subject is incapable of consent due to death or mental impairment.
There are two types of consent being reviewed; explicit consent and presumed consent. Explicit consent consists of the donor giving direct consent through proper registration depending on the country.
The second consent process is presumed consent, which does not need direct consent from the donor or the next of kin. Presumed consent assumes that donation would have been permitted by the potential donor if permission was pursued. Of possible donors an estimated twenty-five percent of families refuse to donate a loved one's organs.
Opt-in versus opt-out:
See also: Mandated choice
As medical science advances, the number of people who could be helped by organ donors increases continuously. As opportunities to save lives increase with new technologies and procedures, the demand for organ donors rises faster than the actual number of donors. In order to respect individual autonomy, voluntary consent must be determined for the individual's disposition of their remains following death.
There are two main methods for determining voluntary consent: "opt in" (only those who have given explicit consent are donors) and "opt out" (anyone who has not refused consent to donate is a donor). In terms of an opt-out or presumed consent system, it is assumed that individuals do intend to donate their organs to medical use when they expire. Opt-out legislative systems dramatically increase effective rates of consent for donation as a consequence of the default effect.
For example, Germany, which uses an opt-in system, has an organ donation consent rate of 12% among its population, while Austria, a country with a very similar culture and economic development, but which uses an opt-out system, has a consent rate of 99.98%.
Opt-out consent, otherwise known as "deemed" consent, support refers to the notion that the majority of people support organ donation, but only a small percentage of the population are actually registered, because they fail to go through the actual step of registration, even if they want to donate their organs at the time of death. This could be resolved with an opt-out system, where many more people would be registered as donors when only those who object consent to donation have to register to be on the non-donation list.
For these reasons, countries, such as Wales, have adopted a "soft opt-out" consent, meaning if a citizen has not clearly made a decision to register, then they will be treated as a registered citizen and participate in the organ donation process. Likewise, opt-in consent refers to the consent process of only those who are registered to participate in organ donation.
Currently, the United States has an opt-in system, but studies show that countries with an opt-out system save more lives due to more availability of donated organs. The current opt-in consent policy assumes that individuals are not willing to become organ donors at the time of their death, unless they have documented otherwise through organ donation registration.
Because of public policies, cultural, infrastructural and other factors, presumed consent or opt-out models do not always translate directly into increased effective rates of donation.
The United Kingdom has several different laws and policies for the organ donation process, such as consent of a witness or guardian must be provided to participate in organ donation. This policy is currently being consulted on by Department of Health and Social Care.
In terms of effective organ donations, in some systems like Australia (14.9 donors per million, 337 donors in 2011), family members are required to give consent or refusal, or may veto a potential recovery even if the donor has consented.
Some countries with an opt-out system like Spain (40.2 donors per million inhabitants), Croatia (40.2 donors/million) or Belgium (31.6 donors/million) have high donor rates, however some countries such as Greece (6 donors/million) maintain low donor rates even with this system.
The president of the Spanish National Transplant Organisation has acknowledged Spain's legislative approach is likely not the primary reason for the country's success in increasing the donor rates, starting in the 1990s.
Looking to the example of Spain, which has successfully adopted the presumed consent donation system, intensive care units (ICUs) must be equipped with enough doctors to maximize the recognition of potential donors and maintain organs while families are consulted for donation.
The characteristic that enables the Spanish presumed consent model to be successful is the resource of transplant coordinators; it is recommended to have at least one at each hospital where opt-out donation is practiced to authorize organ procurement efficiently.
Public views are crucial to the success of opt-out or presumed consent donation systems. In a study done to determine if health policy change to a presumed consent or opt-out system would help to increase donors, an increase of 20 to 30 percent was seen among countries who changed their policies from some type of opt-in system to an opt-out system. Of course, this increase must have a great deal to do with the health policy change, but also may be influenced by other factors that could have impacted donor increases.
Transplant Priority for Willing Donors, also known as the "donor-priority rule," is a newer method and the first to incorporate a "non-medical" criteria into the priority system to encourage higher donation rates in the opt-in system.
Initially implemented in Israel, it allows an individual in need of an organ to move up the recipient list. Moving up the list is contingent on the individual opting-in prior to their need for an organ donation. The policy applies nonmedical criteria when allowing the individual who has previously registered as an organ donor, or family has previously donated an organ, priority over another possible recipient. It must be determined that both recipients have identical medical needs prior to moving a recipient up the list.
While incentives like this in the opt-in system do help raise donation rates, they are not as successful in doing so as the opt-out, presumed consent default policies for donation.
United States:
Over 121,000 people in need of an organ are on the U.S. government waiting list. This crisis within the United States is growing rapidly because on average there are only 30,000 transplants performed each year. More than 8,000 people die each year from lack of a donor organ, an average of 22 people a day. Between the years 1988 and 2006 the number of transplants doubled, but the number of patients waiting for an organ grew six times as large.
In the past presumed consent was urged to try to decrease the need for organs. The Uniform Anatomical Gift Act of 1987 was adopted in several states, and allowed medical examiners to determine if organs and tissues of cadavers could be donated.
By the 1980s, several states adopted different laws that allowed only certain tissues or organs to be retrieved and donated, some allowed all, and some did not allow any without consent of the family. In 2006 when the UAGA was revised, the idea of presumed consent was abandoned. In the United States today, organ donation is done only with consent of the family or donator themselves.
According to economist Alex Tabarrok, the shortage of organs has increased the use of so-called expanded criteria organs, or organs that used to be considered unsuitable for transplant. Five patients that received kidney transplants at the University of Maryland School of Medicine developed cancerous or benign tumors which had to be removed. The head surgeon, Dr. Michael Phelan, explained that "the ongoing shortage of organs from deceased donors, and the high risk of dying while waiting for a transplant, prompted five donors and recipients to push ahead with the surgery."
Several organizations such as the American Kidney Fund are pushing for opt-out organ donation in the United States.
Donor Leave Laws:
In addition to their sick and annual leave, federal executive agency employees are entitled to 30 days paid leave for organ donation. Thirty-two states (excluding only Alabama, Connecticut, Florida, Kentucky, Maine, Michigan, Montana, Nebraska, Nevada, New Hampshire, New Jersey, North Carolina, Pennsylvania, Rhode Island, South Dakota, Tennessee, Vermont, and Wyoming) and the District of Columbia also offer paid leave for state employees.
Five states (California, Hawaii, Louisiana, Minnesota, and Oregon) require certain private employers to provide paid leave for employees for organ or bone marrow donation, and seven others (Arkansas, Connecticut, Maine, Nebraska, New York, South Carolina, and West Virginia) either require employers to provide unpaid leave, or encourage employers to provide leave, for organ or bone marrow donation.
A bill in the US House of Representatives, the Living Donor Protection Act (introduced in 2016, then reintroduced in 2017, would amend the Family and Medical Leave Act of 1993 to provide leave under the act for an organ donor. If successful, this new law would permit "eligible employee" organ donors to receive up to 12 work weeks of leave in a 12-month period.
Tax incentives:
Nineteen US states and the District of Columbia provide tax incentives for organ donation. The most generous state tax incentive is Utah's tax credit, which covers up to $10,000 of unreimbursed expenses (travel, lodging, lost wages, and medical expenses) associated with organ or tissue donation. Idaho (up to $5,000 of unreimbursed expenses) and Louisiana (up to $7,500 of 72% of unreimbursed expenses) also provide donor tax credits.
Arkansas, the District of Columbia, Louisiana and Pennsylvania provide tax credits to employers for wages paid to employees on leave for organ donation.
Thirteen states (Arkansas, Georgia, Iowa, Massachusetts, Mississippi, New Mexico, New York, North Dakota, Ohio, Oklahoma, Rhode Island and Wisconsin) have a tax deduction for up to $10,000 of unreimbursed costs, and Kansas and Virginia offer a tax deduction for up to $5,000 of unreimbursed costs.
States have focused their tax incentives on unreimbursed costs associated with organ donation to ensure compliance with the National Organ Transplant Act of 1984. NOTA prohibits, "any person to knowingly acquire, receive, or otherwise transfer any human organ for valuable consideration for use in human transplantation."
However, NOTA exempts, "the expenses of travel, housing, and lost wages incurred by the donor of a human organ in connection with the donation of the organ," from its definition of "valuable consideration."
While offering income tax deductions has been the preferred method of providing tax incentives, some commentators have expressed concern that these incentives provide disproportionate benefits to wealthier donors. Tax credits, on the other hand, are perceived as more equitable since the after tax benefit of the incentive is not tied to the marginal tax rate of the donor.
Additional tax favored approaches have been proposed for organ donation, including providing: tax credits to the families of deceased donors (seeking to encourage consent), refundable tax credits (similar to the earned income credit) to provide greater tax equity among potential donors, and charitable deductions for the donation of blood or organs.
Other financial incentives:
As stated above, under the National Organ Transplant Act of 1984, granting monetary incentives for organ donation is illegal in the United States. However, there has been some discussion about providing fixed payment for potential live donors. In 1988, regulated paid organ donation was instituted in Iran and, as a result, the renal transplant waiting list was eliminated.
Critics of paid organ donation argue that the poor and vulnerable become susceptible to transplant tourism. Travel for transplantation becomes transplant tourism if the movement of organs, donors, recipients or transplant professionals occurs across borders and involves organ trafficking or transplant commercialism.
Poor and underserved populations in underdeveloped countries are especially vulnerable to the negative consequences of transplant tourism because they have become a major source of organs for the 'transplant tourists' that can afford to travel and purchase organs.
In 1994 a law was passed in Pennsylvania which proposed to pay $300 for room and board and $3,000 for funeral expenses to an organ donor's family. Developing the program was an eight-year process; it is the first of its kind. Procurement directors and surgeons across the nation await the outcomes of Pennsylvania's program.
There have been at least nineteen families that have signed up for the benefit. Due to investigation of the program, however, there has been some concern whether the money collected is being used to assist families.
Some organizations, such as the National Kidney Foundation, oppose financial incentives associated with organ donation claiming, "Offering direct or indirect economic benefits in exchange for organ donation is inconsistent with our values as a society."
One argument is it will disproportionately affect the poor. The $300–3,000 reward may act as an incentive for poorer individuals, as opposed to the wealthy who may not find the offered incentives significant. The National Kidney Foundation has noted that financial incentives, such as this Pennsylvania statute, diminish human dignity.
Bioethical issues:
Deontological:
Deontological issues are issues about whether a person has an ethical duty or responsibility to take an action. Nearly all scholars and societies around the world agree that voluntarily donating organs to sick people is ethically permissible.
Although nearly all scholars encourage organ donation, fewer scholars believe that all people are ethically required to donate their organs after death. Similarly, nearly all religions support voluntary organ donation as a charitable act of great benefit to the community.
Certain small faiths such as Jehovah Witnesses and Shinto are opposed to organ donation based upon religious teachings; for Jehovah Witnesses this opposition is absolute whereas there exists increasing flexibility amongst Shinto scholars.
The Roma People, are also often opposed to organ donation based on prevailing spiritual beliefs and not religious views per se. Issues surrounding patient autonomy, living wills, and guardianship make it nearly impossible for involuntary organ donation to occur.
From the standpoint of deontological ethics, the primary issues surrounding the morality of organ donation are semantic in nature. The debate over the definitions of life, death, human, and body is ongoing. For example, whether or not a brain-dead patient ought to be kept artificially animate in order to preserve organs for donation is an ongoing problem in clinical bioethics.
In addition, some have argued that organ donation constitutes an act of self-harm, even when an organ is donated willingly.
Further, the use of cloning to produce organs with a genotype identical to the recipient is a controversial topic, especially considering the possibility for an entire person to be brought into being for the express purpose of being destroyed for organ procurement. While the benefit of such a cloned organ would be a zero-percent chance of transplant rejection, the ethical issues involved with creating and killing a clone may outweigh these benefits.
However, it may be possible in the future to use cloned stem-cells to grow a new organ without creating a new human being.
A relatively new field of transplantation has reinvigorated the debate. Xenotransplantation, or the transfer of animal (usually pig) organs into human bodies, promises to eliminate many of the ethical issues, while creating many of its own.
While xenotransplantation promises to increase the supply of organs considerably, the threat of organ transplant rejection and the risk of xenozoonosis, coupled with general anathema to the idea, decreases the functionality of the technique. Some animal rights groups oppose the sacrifice of an animal for organ donation and have launched campaigns to ban them.
Teleological:
On teleological or utilitarian grounds, the moral status of "black market organ donation" relies upon the ends, rather than the means. Insofar as those who donate organs are often impoverished and those who can afford black market organs are typically well-off, it would appear that there is an imbalance in the trade. In many cases, those in need of organs are put on waiting lists for legal organs for indeterminate lengths of time—many die while still on a waiting list.
Organ donation is fast becoming an important bioethical issue from a social perspective as well. While most first-world nations have a legal system of oversight for organ transplantation, the fact remains that demand far outstrips supply. Consequently, there has arisen a black market trend often referred to as transplant tourism. The issues are weighty and controversial.
On the one hand are those who contend that those who can afford to buy organs are exploiting those who are desperate enough to sell their organs. Many suggest this results in a growing inequality of status between the rich and the poor.
On the other hand, are those who contend that the desperate should be allowed to sell their organs and that preventing them from doing so is merely contributing to their status as impoverished. Further, those in favor of the trade hold that exploitation is morally preferable to death, and in so far as the choice lies between abstract notions of justice on the one hand and a dying person whose life could be saved on the other hand, the organ trade should be legalized.
Conversely, surveys conducted among living donors postoperatively and in a period of five years following the procedure have shown extreme regret in a majority of the donors, who said that given the chance to repeat the procedure, they would not. Additionally, many study participants reported a decided worsening of economic condition following the procedure. These studies looked only at people who sold a kidney in countries where organ sales are already legal.
A consequence of the black market for organs has been a number of cases and suspected cases of organ theft, including murder for the purposes of organ theft. Proponents of a legal market for organs say that the black-market nature of the current trade allows such tragedies and that regulation of the market could prevent them. Opponents say that such a market would encourage criminals by making it easier for them to claim that their stolen organs were legal.
Legalization of the organ trade carries with it its own sense of justice as well. Continuing black-market trade creates further disparity on the demand side: only the rich can afford such organs. Legalization of the international organ trade could lead to increased supply, lowering prices so that persons outside the wealthiest segments could afford such organs as well.
Exploitation arguments generally come from two main areas:
The New Cannibalism is a phrase coined by anthropologist Nancy Scheper-Hughes in 1998 for an article written for The New Internationalist. Her argument was that the actual exploitation is an ethical failing, a human exploitation; a perception of the poor as organ sources which may be used to extend the lives of the wealthy.
Economic drivers leading to increased donation are not limited to areas such as India and Africa, but also are emerging in the United States. Increasing funeral expenses combined with decreasing real value of investments such as homes and retirement savings which took place in the 2000s have purportedly led to an increase in citizens taking advantage of arrangements where funeral costs are reduced or eliminated.
Brain death versus cardiac death:
Brain death may result in legal death, but still with the heart beating and with mechanical ventilation, keeping all other vital organs alive and functional for a certain period of time.
Given long enough, patients who do not fully die in the complete biological sense, but who are declared brain dead, will usually start to build up toxins and wastes in the body. In this way, the organs can eventually dysfunction due to coagulopathy, fluid or electrolyte and nutrient imbalances, or even fail.
Thus, the organs will usually only be sustainable and viable for acceptable use up until a certain length of time. This may depend on factors such as how well the patient is maintained, any comorbidities, the skill of the healthcare teams and the quality their facilities.
A major point of contention is whether transplantation should be allowed at all if the patient is not yet fully biologically dead, and if brain death is acceptable, whether the person's whole brain needs to have died, or if the death of a certain part of the brain is enough for legal and ethical and moral purposes.
Most organ donation for organ transplantation is done in the setting of brain death. However, in Japan this is a fraught point, and prospective donors may designate either brain death or cardiac death – see organ transplantation in Japan.
In some nations such as Belgium, France, Netherlands, New Zealand, Poland, Portugal, Singapore and Spain, everyone is automatically an organ donor unless they opt out of the system. Elsewhere, consent from family members or next-of-kin is required for organ donation. The non-living donor is kept on ventilator support until the organs have been surgically removed. If a brain-dead individual is not an organ donor, ventilator and drug support is discontinued and cardiac death is allowed to occur.
In the United States, where since the 1980s the Uniform Determination of Death Act has defined death as the irreversible cessation of the function of either the brain or the heart and lungs, the 21st century has seen an order-of-magnitude increase of donation following cardiac death.
In 1995, only one out of 100 dead donors in the nation gave their organs following the declaration of cardiac death. That figure grew to almost 11 percent in 2008, according to the Scientific Registry of Transplant Recipients. That increase has provoked ethical concerns about the interpretation of "irreversible" since "patients may still be alive five or even 10 minutes after cardiac arrest because, theoretically, their hearts could be restarted, [and thus are] clearly not dead because their condition was reversible."
Gender inequality:
The majority of organ donors are women. For example, in the United States, 62% of kidney donors and 53% of liver donors are women. In India, women constitute 74% of kidney donors and 60.5% of liver donors. Additionally, the number of female organ recipients is conspicuously lower than that of male recipients. In the U.S., 35% of liver recipients and 39% of kidney recipients are women. In India, the figures are 24% and 19% respectively.
Political issues:
There are also controversial issues regarding how organs are allocated to recipients. For example, some believe that livers should not be given to alcoholics in danger of reversion, while others view alcoholism as a medical condition like diabetes. Faith in the medical system is important to the success of organ donation.
Brazil switched to an opt-out system and ultimately had to withdraw it because it further alienated patients who already distrusted the country's medical system. Adequate funding, strong political will to see transplant outcomes improve, and the existence of specialized training, care and facilities also increase donation rates.
Expansive legal definitions of death, such as Spain uses, also increase the pool of eligible donors by allowing physicians to declare a patient to be dead at an earlier stage, when the organs are still in good physical condition. Allowing or forbidding payment for organs affects the availability of organs. Generally, where organs cannot be bought or sold, quality and safety are high, but supply is not adequate to the demand. Where organs can be purchased, the supply increases.
Iran adopted a system of paying kidney donors in 1988 and within 11 years it became the only country in the world to clear its waiting list for transplants — The Economist
Healthy humans have two kidneys, a redundancy that enables living donors (inter vivos) to give a kidney to someone who needs it. The most common transplants are to close relatives, but people have given kidneys to other friends. The rarest type of donation is the undirected donation whereby a donor gives a kidney to a stranger. Less than a few hundred of such kidney donations have been performed.
In recent years, searching for altruistic donors via the internet has also become a way to find life saving organs. However, internet advertising for organs is a highly controversial practice, as some scholars believe it undermines the traditional list-based allocation system.
The National Transplant Organization of Spain is one of the most successful in the world (Spain has been the world leader in organ donation for decades), but it still cannot meet the demand, as 10% of those needing a transplant die while still on the transplant list. Donations from corpses are anonymous, and a network for communication and transport allows fast extraction and transplant across the country.
Under Spanish law, every corpse can provide organs unless the deceased person had expressly rejected it. Because family members still can forbid the donation, carefully trained doctors ask the family for permission, making it very similar in practice to the United States system.
In the overwhelming majority of cases, organ donation is not possible for reasons of recipient safety, match failures, or organ condition. Even in Spain, which has the highest organ donation rate in the world, there are only 35.1 actual donors per million people, and there are hundreds of patients on the waiting list.
This rate compares to 24.8 per million in Austria, where families are rarely asked to donate organs, and 22.2 per million in France, which—like Spain—has a presumed-consent system.
Prison inmates:
See also: Organ donation in the United States prison population
In the United States, prisoners are not discriminated against as organ recipients and are equally eligible for organ transplants along with the general population.
A 1976 U.S. Supreme Court case ruled that withholding health care from prisoners constituted "cruel and unusual punishment". United Network for Organ Sharing, the organization that coordinates available organs with recipients, does not factor a patient's prison status when determining suitability for a transplant.
An organ transplant and follow-up care can cost the prison system up to one million dollars.
If a prisoner qualifies, a state may allow compassionate early release to avoid high costs associated with organ transplants. However, an organ transplant may save the prison system substantial costs associated with dialysis and other life-extending treatments required by the prisoner with the failing organ. For example, the estimated cost of a kidney transplant is about $111,000.
A prisoner's dialysis treatments are estimated to cost a prison $120,000 per year. Because donor organs are in short supply, there are more people waiting for a transplant than available organs. When a prisoner receives an organ, there is a high probability that someone else will die waiting for the next available organ.
A response to this ethical dilemma states that felons who have a history of violent crime, who have violated others’ basic rights, have lost the right to receive an organ transplant, though it is noted that it would be necessary "to reform our justice system to minimize the chance of an innocent person being wrongly convicted of a violent crime and thus being denied an organ transplant"
Prisons typically do not allow inmates to donate organs to anyone but immediate family members. There is no law against prisoner organ donation; however, the transplant community has discouraged use of prisoner's organs since the early 1990s due to concern over prisons' high-risk environment for infectious diseases.
Physicians and ethicists also criticize the idea because a prisoner is not able to consent to the procedure in a free and non-coercive environment, especially if given inducements to participate.
However, with modern testing advances to more safely rule out infectious disease and by ensuring that there are no incentives offered to participate, some have argued that prisoners can now voluntarily consent to organ donation just as they can now consent to medical procedures in general. With careful safeguards, and with over 2 million prisoners in the U.S., they reason that prisoners can provide a solution for reducing organ shortages in the U.S.
While some have argued that prisoner participation would likely be too low to make a difference, one Arizona program started by former Maricopa County Sheriff Joe Arpaio encourages inmates to voluntarily sign up to donate their heart and other organs. As of 2015, there have been over 16,500 participants.
Similar initiatives have been started in other US states. In 2013, Utah became the first state to allow prisoners to sign up for organ donation upon death.
Religious viewpoints:
Main article: Religious views on organ donation
See also: Organ donation in Jewish law
There are several different religions that have different perspectives. Islam has a conflicting view regarding the issue, with half believing that it is against the religion. Muslims are commanded to seek medical attention when in need and saving life is a very important factor of the Islamic religion. Christianity is lenient on the topic of organ donation, and believe it is a service of life.
All major religions accept organ donation in at least some form on either utilitarian grounds (i.e., because of its life-saving capabilities) or deontological grounds (e.g., the right of an individual believer to make his or her own decision). Most religions, among them the Roman Catholic Church, support organ donation on the grounds that it constitutes an act of charity and provides a means of saving a life.
One religious group, The Jesus Christians, became known as "The Kidney Cult" because more than half its members had donated their kidneys altruistically. Jesus Christians claim altruistic kidney donation is a great way to "Do unto others what they would want you to do unto them."
Some religions impose certain restrictions on the types of organs that may be donated and/or on the means by which organs may be harvested and/or transplanted. For example, Jehovah's Witnesses require that organs be drained of any blood due to their interpretation of the Hebrew Bible/Christian Old Testament as prohibiting blood transfusion, and Muslims require that the donor have provided written consent in advance. A few groups disfavor organ transplantation or donation; notably, these include Shinto and those who follow the customs of the Gypsies.
Orthodox Judaism considers organ donation obligatory if it will save a life, as long as the donor is considered dead as defined by Jewish law. In both Orthodox Judaism and non-Orthodox Judaism, the majority view holds that organ donation is permitted in the case of irreversible cardiac rhythm cessation. In some cases, rabbinic authorities believe that organ donation may be mandatory, whereas a minority opinion considers any donation of a live organ as forbidden.
Organ shortfall:
The demand for organs significantly surpasses the number of donors everywhere in the world. There are more potential recipients on organ donation waiting lists than organ donors.
In particular, due to significant advances in dialysis techniques, patients suffering from end-stage renal disease (ESRD) can survive longer than ever before. Because these patients don't die as quickly as they used to, and as kidney failure increases with the rising age and prevalence of high blood pressure and diabetes in a society, the need especially for kidneys rises every year.
As of March 2014, about 121,600 people in the United States are on the waiting list, although about a third of those patients are inactive and could not receive a donated organ. Wait times and success rates for organs differ significantly between organs due to demand and procedure difficulty.
As of 2007, three-quarters of patients in need of an organ transplant were waiting for a kidney, and as such kidneys have much longer waiting times. As stated by the Gift of Life Donor Program website, the median patient who ultimately received an organ waited 4 months for a heart or lung—but 18 months for a kidney, and 18–24 months for a pancreas because demand for these organs substantially outstrips supply.
An increased prevalence of self-driving cars could exacerbate this problem: In the US, 13% of organ donations come from car crash victims, and autonomous vehicles are projected to reduce the frequency of car crashes.
In Australia, there are 10.8 transplants per million people, about a third of the Spanish rate. The Lions Eye Institute, in Western Australia, houses the Lions Eye Bank. The Bank was established in 1986 and coordinates the collection, processing and distribution of eye tissue for transplantation.
The Lions Eye Bank also maintains a waitlist of patients who require corneal graft operations. About 100 corneas are provided by the Bank for transplant each year, but there is still a waiting list for corneas."To an economist, this is a basic supply-and-demand gap with tragic consequences."
Approaches to addressing this shortfall include:
In hospitals, organ network representatives routinely screen patient records to identify potential donors shortly in advance of their deaths.
Distribution:
The United States has two agencies that govern organ procurement and distribution within the country. The United Network for Organ Sharing and the Organ Procurement and Transplant Network (OPTN) regulate Organ Procurement Organizations (OPO) with regard to procurement and distribution ethics and standards.
OPOs are non-profit organizations charged with the evaluation, procurement and allocation of organs within their Designated Service Area (DSA). Once a donor has been evaluated and consent obtained, provisional allocation of organs commences.
UNOS developed a computer program that automatically generates donor specific match lists for suitable recipients based on the criteria that the patient was listed with. OPO coordinators enter donor information into the program and run the respective lists. Organ offers to potential recipients are made to transplant centers to make them aware of a potential organ.
The surgeon will evaluate the donor information and make a provisional determination of medical suitability to their recipient. Distribution varies slightly between different organs but is essentially very similar.
When lists are generated, many factors are taken into consideration; these factors include: distance of transplant center from the donor hospital, blood type, medical urgency, wait time, donor size and tissue typing.
For heart recipients medical urgency is denoted by a recipients "Status" (Status 1A, 1B and status 2).
Lungs are allocated based on a recipients Lung Allocation Score (LAS) that is determined based on the urgency of clinical need as well as the likelihood of benefit from the transplant.
Livers are allocated using both a status system and MELD/PELD score (Model for End-stage Liver Disease/Pediatric End-stage Liver Disease).
Kidney and pancreas lists are based on location, blood type, Human Leukocyte Antigen (HLA) typing and wait time. When a recipient for a kidney or pancreas has no direct antibodies to the donor HLA the match is said to be a 0 ABDR mismatch or zero antigen mismatch.
A zero mismatch organ has a low rate of rejection and allows a recipient to be on lower doses of immunosuppressive drugs. Since zero mismatches have such high graft survival these recipients are afforded priority regardless of location and wait time. UNOS has in place a "Payback" system to balance organs that are sent out of a DSA because of a zero mismatch.
Location of a transplant center with respect to a donor hospital is given priority due to the effects of Cold Ischemic Time (CIT). Once the organ is removed from the donor, blood no longer perfuses through the vessels and begins to starve the cells of oxygen (ischemia).
Each organ tolerates different ischemic times. Hearts and lungs need to be transplanted within 4–6 hours from recovery, liver about 8–10 hours and pancreas about 15 hours; kidneys are the most resilient to ischemia. Kidneys packaged on ice can be successfully transplanted 24–36 hours after recovery.
Developments in kidney preservation have yielded a device that pumps cold preservation solution through the kidneys vessels to prevent Delayed Graft Function (DGF) due to ischemia. Perfusion devices, often called kidney pumps, can extend graft survival to 36–48 hours post recovery for kidneys.
Recently similar devices have been developed for the heart and lungs, in an effort to increase distances procurement teams may travel to recover an organ.
Suicide:
People committing suicide have a higher rate of donating organs than average. One reason is lower negative response or refusal rate by the family and relatives, but the explanation for this remains to be clarified. In addition, donation consent is higher than average from people committing suicide.
Attempted suicide is a common cause of brain death (3.8%), mainly among young men. Organ donation is more common in this group compared to other causes of death.
Brain death may result in legal death, but still with the heart beating, and with mechanical ventilation all other vital organs may be kept completely alive and functional, providing optimal opportunities for organ transplantation.
Controversies:
In 2008, California transplant surgeon Hootan Roozrokh was charged with dependent adult abuse for prescribing what prosecutors alleged were excessive doses of morphine and sedatives to hasten the death of a man with adrenal leukodystrophy and irreversible brain damage, in order to procure his organs for transplant.
The case brought against Roozrokh was the first criminal case against a transplant surgeon in the US, and resulted in his acquittal. Further, Dr. Roozrokh successfully sued for defamation stemming from the incident.
At California's Emanuel Medical Center, neurologist Narges Pazouki, MD, said an organ-procurement organization representative pressed her to declare a patient brain-dead before the appropriate tests had been done.
In September 1999, eBay blocked an auction for "one functional human kidney" which had reached a highest bid of $5.7 million. Under United States federal laws, eBay was obligated to dismiss the auction for the selling of human organs which is punishable by up to five years in prison and a $50,000 fine.
On June 27, 2008, Indonesian Sulaiman Damanik, 26, pleaded guilty in a Singapore court for sale of his kidney to CTang's executive chair, Mr. Tang Wee Sung, 55, for 150 million rupiah (US$17,000). The Transplant Ethics Committee must approve living donor kidney transplants.
Organ trading is banned in Singapore and in many other countries to prevent the exploitation of "poor and socially disadvantaged donors who are unable to make informed choices and suffer potential medical risks." Toni, 27, the other accused, donated a kidney to an Indonesian patient in March, alleging he was the patient's adopted son, and was paid 186 million rupiah (US$21,000).
Public service announcements:
Marketing for organ donation must walk a fine line between stressing the need for organ donation and not being too forceful. If the marketing agent is too forceful, then the target of the message will react defensively to the request. According to psychological reactance theory, a person will perceive their freedom threatened and will react to restore the freedom.
According to Ashley Anker, the use of transportation theory has a positive effect on target reactions by marketing attempts. When public service announcements use recipient-focused messages, targets were more transported. Individuals who watched recipient-focused messages were more transported because potential donors experience empathy for the potential recipient.
Future public service announcements should use recipient-focused stories to elicit relationship formation between potential donors and recipients.
Awareness about organ donation leads to greater social support for organ donation, in turn leading to greater registration. By starting with promoting college students’ awareness of organ donation and moving to increasing social support for organ donation, the more likely people will be to register as organ donors.
The United States Department of Health funded a study by the University of Wisconsin Hospital to increase efforts to increase awareness and the number of registered donors by pursuing members of the university and their family and friends through social media. The results of the study showed a 20% increase in organ donation by creating support and awareness through social media.
See also:
Organ Transplantation
Organ transplantation is a medical procedure in which an organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ. The donor and recipient may be at the same location, or organs may be transported from a donor site to another location.
Organs and/or tissues that are transplanted within the same person's body are called autografts. Transplants that are recently performed between two subjects of the same species are called allografts. Allografts can either be from a living or cadaveric source.
Organs that have been successfully transplanted include the heart, kidneys, liver, lungs, pancreas, intestine, thymus and uterus. Tissues include bones, tendons (both referred to as musculoskeletal grafts), corneae, skin, heart valves, nerves and veins.
Worldwide, the kidneys are the most commonly transplanted organs, followed by the liver and then the heart. Corneae and musculoskeletal grafts are the most commonly transplanted tissues; these outnumber organ transplants by more than tenfold.
Organ donors may be living, brain dead, or dead via circulatory death. Tissue may be recovered from donors who die of circulatory death, as well as of brain death – up to 24 hours past the cessation of heartbeat. Unlike organs, most tissues (with the exception of corneas) can be preserved and stored for up to five years, meaning they can be "banked".
Transplantation raises a number of bioethical issues, including the definition of death, when and how consent should be given for an organ to be transplanted, and payment for organs for transplantation. Other ethical issues include transplantation tourism (medical tourism) and more broadly the socio-economic context in which organ procurement or transplantation may occur. A particular problem is organ trafficking. There is also the ethical issue of not holding out false hope to patients.
Transplantation medicine is one of the most challenging and complex areas of modern medicine. Some of the key areas for medical management are the problems of transplant rejection, during which the body has an immune response to the transplanted organ, possibly leading to transplant failure and the need to immediately remove the organ from the recipient.
When possible, transplant rejection can be reduced through serotyping to determine the most appropriate donor-recipient match and through the use of immunosuppressant drugs.
Click on any of the following blue hyperlinks for more about Organ Transplantation:
- Types of transplant
- Organs and tissues transplanted
- Types of donor
- Allocation of organs
- Reasons for donation and ethical issues
- Proliferation
- History
- Society and culture
- Research
- See also:
- Artificial organ
- Beating heart cadaver
- Blood transfusion
- Laboratory-grown organ
- Organ donation
- Regenerative medicine
- Transplant rejection
- Xenotransplantation
- Organ Transplant survival rates from the Scientific Registry of Transplant Recipients: The Gift of a Lifetime – Online Educational Documentary
- The short film A Science of Miracles (2009) is available for free download at the Internet Archive.
- "Overcoming the Rejection Factor: MUSC's First Organ Transplant" online exhibit at Waring Historical Library
Organ donation:
Organ donation is the process when a person allows an organ of their own to be removed and transplanted to another person, legally, either by consent while the donor is alive or dead with the assent of the next of kin.
Donation may be for research or, more commonly, healthy transplantable organs and tissues may be donated to be transplanted into another person.
Common transplantations include:
- kidneys,
- heart,
- liver,
- pancreas,
- intestines,
- lungs,
- bones,
- bone marrow,
- skin,
- and corneas.
Some organs and tissues can be donated by living donors, such as a kidney or part of the liver, part of the pancreas, part of the lungs or part of the intestines, but most donations occur after the donor has died.
In 2019, Spain had the highest donor rate in the world at 46.91 per million people, followed by the US (36.88 per million), Croatia (34.63 per million), Portugal (33.8 per million), and France (33.25 per million).
As of February 2, 2019, there were 120,000 people waiting for life-saving organ transplants in the US. Of these, 74,897 people were active candidates waiting for a donor. While views of organ donation are positive, there is a large gap between the numbers of registered donors compared to those awaiting organ donations on a global level.
To increase the number of organ donors, especially among underrepresented populations, current approaches include the use of optimized social network interventions, exposing tailored educational content about organ donation to target social media users.
Process in the United States:
Organ donors are usually dead at the time of donation, but may be living. For living donors, organ donation typically involves extensive testing before the donation, including psychological evaluation to determine whether the would-be donor understands and consents to the donation.
On the day of the donation, the donor and the recipient arrive at the hospital, just like they would for any other major surgery.
For dead donors, the process begins with verifying that the person is undoubtedly deceased, determining whether any organs could be donated, and obtaining consent for the donation of any usable organs.
Normally, nothing is done until the person has already died, although if death is inevitable, it is possible to check for consent and to do some simple medical tests shortly beforehand, to help find a matching recipient.
The verification of death is normally done by a neurologist (a physician specializing in brain function) that is not involved in the previous attempts to save the patient's life. This physician has nothing to do with the transplantation process.
Verification of death is often done multiple times, to prevent doctors from overlooking any remaining sign of life, however small. After death, the hospital may keep the body on a mechanical ventilator and use other methods to keep the organs in good condition. Donors and their families are not charged for any expenses related to the donation.
The surgical process depends upon which organs are being donated.
The body is normally restored to as normal an appearance as possible, so that the family can proceed with funeral rites and either cremation or burial.
The lungs are highly vulnerable to injury and thus the most difficult to preserve, with only 15–25% of donated organs utilized.
History:
Further information: List of organ transplant donors and recipients
The first living organ donor in a successful transplant was Ronald Lee Herrick (1931–2010), who donated a kidney to his identical twin brother in 1954. The lead surgeon, Joseph Murray, won the Nobel Prize in Physiology or Medicine in 1990 for advances in organ transplantation.
The youngest organ donor was a baby with anencephaly, born in 2014, who lived for only 100 minutes and donated his kidneys to an adult with renal failure.
The oldest known cornea donor was a 107-year-old Scottish woman, whose corneas were donated after her death in 2016. The oldest known organ donor for an internal organ was a 95-year-old West Virginia man, who donated his liver after he died.
The oldest altruistic living organ donor was an 85-year-old woman in Britain, who donated a kidney to a stranger in 2014 after hearing how many people needed to receive a transplant.
Researchers were able to develop a novel way to transplant human fetal kidneys into anephric rats to overcome a significant obstacle in impeding human fetal organ transplantations. The human fetal kidneys demonstrated both growth and function within the rats.
Brain donation:
Donated brain tissue is a valuable resource for research into brain function, neurodiversity, neuropathology and possible treatments. Both divergent and healthy control brains are needed for comparison. Brain banks typically source tissue from donors that had directly registered with them before their passing, since organ donor registries focus on tissue meant for transplantation.
In the United States the nonprofit Brain Donor Project facilitates this process.
Legislation and global perspectives:
The laws of different countries allow potential donors to permit or refuse donation, or give this choice to relatives. The frequency of donations varies among countries.
Consent process:
The term consent is typically defined as a subject adhering to an agreement of principles and regulations; however, the definition becomes difficult to execute concerning the topic of organ donation, mainly because the subject is incapable of consent due to death or mental impairment.
There are two types of consent being reviewed; explicit consent and presumed consent. Explicit consent consists of the donor giving direct consent through proper registration depending on the country.
The second consent process is presumed consent, which does not need direct consent from the donor or the next of kin. Presumed consent assumes that donation would have been permitted by the potential donor if permission was pursued. Of possible donors an estimated twenty-five percent of families refuse to donate a loved one's organs.
Opt-in versus opt-out:
See also: Mandated choice
As medical science advances, the number of people who could be helped by organ donors increases continuously. As opportunities to save lives increase with new technologies and procedures, the demand for organ donors rises faster than the actual number of donors. In order to respect individual autonomy, voluntary consent must be determined for the individual's disposition of their remains following death.
There are two main methods for determining voluntary consent: "opt in" (only those who have given explicit consent are donors) and "opt out" (anyone who has not refused consent to donate is a donor). In terms of an opt-out or presumed consent system, it is assumed that individuals do intend to donate their organs to medical use when they expire. Opt-out legislative systems dramatically increase effective rates of consent for donation as a consequence of the default effect.
For example, Germany, which uses an opt-in system, has an organ donation consent rate of 12% among its population, while Austria, a country with a very similar culture and economic development, but which uses an opt-out system, has a consent rate of 99.98%.
Opt-out consent, otherwise known as "deemed" consent, support refers to the notion that the majority of people support organ donation, but only a small percentage of the population are actually registered, because they fail to go through the actual step of registration, even if they want to donate their organs at the time of death. This could be resolved with an opt-out system, where many more people would be registered as donors when only those who object consent to donation have to register to be on the non-donation list.
For these reasons, countries, such as Wales, have adopted a "soft opt-out" consent, meaning if a citizen has not clearly made a decision to register, then they will be treated as a registered citizen and participate in the organ donation process. Likewise, opt-in consent refers to the consent process of only those who are registered to participate in organ donation.
Currently, the United States has an opt-in system, but studies show that countries with an opt-out system save more lives due to more availability of donated organs. The current opt-in consent policy assumes that individuals are not willing to become organ donors at the time of their death, unless they have documented otherwise through organ donation registration.
Because of public policies, cultural, infrastructural and other factors, presumed consent or opt-out models do not always translate directly into increased effective rates of donation.
The United Kingdom has several different laws and policies for the organ donation process, such as consent of a witness or guardian must be provided to participate in organ donation. This policy is currently being consulted on by Department of Health and Social Care.
In terms of effective organ donations, in some systems like Australia (14.9 donors per million, 337 donors in 2011), family members are required to give consent or refusal, or may veto a potential recovery even if the donor has consented.
Some countries with an opt-out system like Spain (40.2 donors per million inhabitants), Croatia (40.2 donors/million) or Belgium (31.6 donors/million) have high donor rates, however some countries such as Greece (6 donors/million) maintain low donor rates even with this system.
The president of the Spanish National Transplant Organisation has acknowledged Spain's legislative approach is likely not the primary reason for the country's success in increasing the donor rates, starting in the 1990s.
Looking to the example of Spain, which has successfully adopted the presumed consent donation system, intensive care units (ICUs) must be equipped with enough doctors to maximize the recognition of potential donors and maintain organs while families are consulted for donation.
The characteristic that enables the Spanish presumed consent model to be successful is the resource of transplant coordinators; it is recommended to have at least one at each hospital where opt-out donation is practiced to authorize organ procurement efficiently.
Public views are crucial to the success of opt-out or presumed consent donation systems. In a study done to determine if health policy change to a presumed consent or opt-out system would help to increase donors, an increase of 20 to 30 percent was seen among countries who changed their policies from some type of opt-in system to an opt-out system. Of course, this increase must have a great deal to do with the health policy change, but also may be influenced by other factors that could have impacted donor increases.
Transplant Priority for Willing Donors, also known as the "donor-priority rule," is a newer method and the first to incorporate a "non-medical" criteria into the priority system to encourage higher donation rates in the opt-in system.
Initially implemented in Israel, it allows an individual in need of an organ to move up the recipient list. Moving up the list is contingent on the individual opting-in prior to their need for an organ donation. The policy applies nonmedical criteria when allowing the individual who has previously registered as an organ donor, or family has previously donated an organ, priority over another possible recipient. It must be determined that both recipients have identical medical needs prior to moving a recipient up the list.
While incentives like this in the opt-in system do help raise donation rates, they are not as successful in doing so as the opt-out, presumed consent default policies for donation.
United States:
Over 121,000 people in need of an organ are on the U.S. government waiting list. This crisis within the United States is growing rapidly because on average there are only 30,000 transplants performed each year. More than 8,000 people die each year from lack of a donor organ, an average of 22 people a day. Between the years 1988 and 2006 the number of transplants doubled, but the number of patients waiting for an organ grew six times as large.
In the past presumed consent was urged to try to decrease the need for organs. The Uniform Anatomical Gift Act of 1987 was adopted in several states, and allowed medical examiners to determine if organs and tissues of cadavers could be donated.
By the 1980s, several states adopted different laws that allowed only certain tissues or organs to be retrieved and donated, some allowed all, and some did not allow any without consent of the family. In 2006 when the UAGA was revised, the idea of presumed consent was abandoned. In the United States today, organ donation is done only with consent of the family or donator themselves.
According to economist Alex Tabarrok, the shortage of organs has increased the use of so-called expanded criteria organs, or organs that used to be considered unsuitable for transplant. Five patients that received kidney transplants at the University of Maryland School of Medicine developed cancerous or benign tumors which had to be removed. The head surgeon, Dr. Michael Phelan, explained that "the ongoing shortage of organs from deceased donors, and the high risk of dying while waiting for a transplant, prompted five donors and recipients to push ahead with the surgery."
Several organizations such as the American Kidney Fund are pushing for opt-out organ donation in the United States.
Donor Leave Laws:
In addition to their sick and annual leave, federal executive agency employees are entitled to 30 days paid leave for organ donation. Thirty-two states (excluding only Alabama, Connecticut, Florida, Kentucky, Maine, Michigan, Montana, Nebraska, Nevada, New Hampshire, New Jersey, North Carolina, Pennsylvania, Rhode Island, South Dakota, Tennessee, Vermont, and Wyoming) and the District of Columbia also offer paid leave for state employees.
Five states (California, Hawaii, Louisiana, Minnesota, and Oregon) require certain private employers to provide paid leave for employees for organ or bone marrow donation, and seven others (Arkansas, Connecticut, Maine, Nebraska, New York, South Carolina, and West Virginia) either require employers to provide unpaid leave, or encourage employers to provide leave, for organ or bone marrow donation.
A bill in the US House of Representatives, the Living Donor Protection Act (introduced in 2016, then reintroduced in 2017, would amend the Family and Medical Leave Act of 1993 to provide leave under the act for an organ donor. If successful, this new law would permit "eligible employee" organ donors to receive up to 12 work weeks of leave in a 12-month period.
Tax incentives:
Nineteen US states and the District of Columbia provide tax incentives for organ donation. The most generous state tax incentive is Utah's tax credit, which covers up to $10,000 of unreimbursed expenses (travel, lodging, lost wages, and medical expenses) associated with organ or tissue donation. Idaho (up to $5,000 of unreimbursed expenses) and Louisiana (up to $7,500 of 72% of unreimbursed expenses) also provide donor tax credits.
Arkansas, the District of Columbia, Louisiana and Pennsylvania provide tax credits to employers for wages paid to employees on leave for organ donation.
Thirteen states (Arkansas, Georgia, Iowa, Massachusetts, Mississippi, New Mexico, New York, North Dakota, Ohio, Oklahoma, Rhode Island and Wisconsin) have a tax deduction for up to $10,000 of unreimbursed costs, and Kansas and Virginia offer a tax deduction for up to $5,000 of unreimbursed costs.
States have focused their tax incentives on unreimbursed costs associated with organ donation to ensure compliance with the National Organ Transplant Act of 1984. NOTA prohibits, "any person to knowingly acquire, receive, or otherwise transfer any human organ for valuable consideration for use in human transplantation."
However, NOTA exempts, "the expenses of travel, housing, and lost wages incurred by the donor of a human organ in connection with the donation of the organ," from its definition of "valuable consideration."
While offering income tax deductions has been the preferred method of providing tax incentives, some commentators have expressed concern that these incentives provide disproportionate benefits to wealthier donors. Tax credits, on the other hand, are perceived as more equitable since the after tax benefit of the incentive is not tied to the marginal tax rate of the donor.
Additional tax favored approaches have been proposed for organ donation, including providing: tax credits to the families of deceased donors (seeking to encourage consent), refundable tax credits (similar to the earned income credit) to provide greater tax equity among potential donors, and charitable deductions for the donation of blood or organs.
Other financial incentives:
As stated above, under the National Organ Transplant Act of 1984, granting monetary incentives for organ donation is illegal in the United States. However, there has been some discussion about providing fixed payment for potential live donors. In 1988, regulated paid organ donation was instituted in Iran and, as a result, the renal transplant waiting list was eliminated.
Critics of paid organ donation argue that the poor and vulnerable become susceptible to transplant tourism. Travel for transplantation becomes transplant tourism if the movement of organs, donors, recipients or transplant professionals occurs across borders and involves organ trafficking or transplant commercialism.
Poor and underserved populations in underdeveloped countries are especially vulnerable to the negative consequences of transplant tourism because they have become a major source of organs for the 'transplant tourists' that can afford to travel and purchase organs.
In 1994 a law was passed in Pennsylvania which proposed to pay $300 for room and board and $3,000 for funeral expenses to an organ donor's family. Developing the program was an eight-year process; it is the first of its kind. Procurement directors and surgeons across the nation await the outcomes of Pennsylvania's program.
There have been at least nineteen families that have signed up for the benefit. Due to investigation of the program, however, there has been some concern whether the money collected is being used to assist families.
Some organizations, such as the National Kidney Foundation, oppose financial incentives associated with organ donation claiming, "Offering direct or indirect economic benefits in exchange for organ donation is inconsistent with our values as a society."
One argument is it will disproportionately affect the poor. The $300–3,000 reward may act as an incentive for poorer individuals, as opposed to the wealthy who may not find the offered incentives significant. The National Kidney Foundation has noted that financial incentives, such as this Pennsylvania statute, diminish human dignity.
Bioethical issues:
Deontological:
Deontological issues are issues about whether a person has an ethical duty or responsibility to take an action. Nearly all scholars and societies around the world agree that voluntarily donating organs to sick people is ethically permissible.
Although nearly all scholars encourage organ donation, fewer scholars believe that all people are ethically required to donate their organs after death. Similarly, nearly all religions support voluntary organ donation as a charitable act of great benefit to the community.
Certain small faiths such as Jehovah Witnesses and Shinto are opposed to organ donation based upon religious teachings; for Jehovah Witnesses this opposition is absolute whereas there exists increasing flexibility amongst Shinto scholars.
The Roma People, are also often opposed to organ donation based on prevailing spiritual beliefs and not religious views per se. Issues surrounding patient autonomy, living wills, and guardianship make it nearly impossible for involuntary organ donation to occur.
From the standpoint of deontological ethics, the primary issues surrounding the morality of organ donation are semantic in nature. The debate over the definitions of life, death, human, and body is ongoing. For example, whether or not a brain-dead patient ought to be kept artificially animate in order to preserve organs for donation is an ongoing problem in clinical bioethics.
In addition, some have argued that organ donation constitutes an act of self-harm, even when an organ is donated willingly.
Further, the use of cloning to produce organs with a genotype identical to the recipient is a controversial topic, especially considering the possibility for an entire person to be brought into being for the express purpose of being destroyed for organ procurement. While the benefit of such a cloned organ would be a zero-percent chance of transplant rejection, the ethical issues involved with creating and killing a clone may outweigh these benefits.
However, it may be possible in the future to use cloned stem-cells to grow a new organ without creating a new human being.
A relatively new field of transplantation has reinvigorated the debate. Xenotransplantation, or the transfer of animal (usually pig) organs into human bodies, promises to eliminate many of the ethical issues, while creating many of its own.
While xenotransplantation promises to increase the supply of organs considerably, the threat of organ transplant rejection and the risk of xenozoonosis, coupled with general anathema to the idea, decreases the functionality of the technique. Some animal rights groups oppose the sacrifice of an animal for organ donation and have launched campaigns to ban them.
Teleological:
On teleological or utilitarian grounds, the moral status of "black market organ donation" relies upon the ends, rather than the means. Insofar as those who donate organs are often impoverished and those who can afford black market organs are typically well-off, it would appear that there is an imbalance in the trade. In many cases, those in need of organs are put on waiting lists for legal organs for indeterminate lengths of time—many die while still on a waiting list.
Organ donation is fast becoming an important bioethical issue from a social perspective as well. While most first-world nations have a legal system of oversight for organ transplantation, the fact remains that demand far outstrips supply. Consequently, there has arisen a black market trend often referred to as transplant tourism. The issues are weighty and controversial.
On the one hand are those who contend that those who can afford to buy organs are exploiting those who are desperate enough to sell their organs. Many suggest this results in a growing inequality of status between the rich and the poor.
On the other hand, are those who contend that the desperate should be allowed to sell their organs and that preventing them from doing so is merely contributing to their status as impoverished. Further, those in favor of the trade hold that exploitation is morally preferable to death, and in so far as the choice lies between abstract notions of justice on the one hand and a dying person whose life could be saved on the other hand, the organ trade should be legalized.
Conversely, surveys conducted among living donors postoperatively and in a period of five years following the procedure have shown extreme regret in a majority of the donors, who said that given the chance to repeat the procedure, they would not. Additionally, many study participants reported a decided worsening of economic condition following the procedure. These studies looked only at people who sold a kidney in countries where organ sales are already legal.
A consequence of the black market for organs has been a number of cases and suspected cases of organ theft, including murder for the purposes of organ theft. Proponents of a legal market for organs say that the black-market nature of the current trade allows such tragedies and that regulation of the market could prevent them. Opponents say that such a market would encourage criminals by making it easier for them to claim that their stolen organs were legal.
Legalization of the organ trade carries with it its own sense of justice as well. Continuing black-market trade creates further disparity on the demand side: only the rich can afford such organs. Legalization of the international organ trade could lead to increased supply, lowering prices so that persons outside the wealthiest segments could afford such organs as well.
Exploitation arguments generally come from two main areas:
- Physical exploitation suggests that the operations in question are quite risky, and, taking place in third-world hospitals or "back-alleys", even more risky. Yet, if the operations in question can be made safe, there is little threat to the donor.
- Financial exploitation suggests that the donor (especially in the Indian subcontinent and Africa) are not paid enough. Commonly, accounts from persons who have sold organs in both legal and black market circumstances put the prices at between $150 and $5,000, depending on the local laws, supply of ready donors and scope of the transplant operation. In Chennai, India where one of the largest black markets for organs is known to exist, studies have placed the average sale price at little over $1,000. Many accounts also exist of donors being postoperatively denied their promised pay.
The New Cannibalism is a phrase coined by anthropologist Nancy Scheper-Hughes in 1998 for an article written for The New Internationalist. Her argument was that the actual exploitation is an ethical failing, a human exploitation; a perception of the poor as organ sources which may be used to extend the lives of the wealthy.
Economic drivers leading to increased donation are not limited to areas such as India and Africa, but also are emerging in the United States. Increasing funeral expenses combined with decreasing real value of investments such as homes and retirement savings which took place in the 2000s have purportedly led to an increase in citizens taking advantage of arrangements where funeral costs are reduced or eliminated.
Brain death versus cardiac death:
Brain death may result in legal death, but still with the heart beating and with mechanical ventilation, keeping all other vital organs alive and functional for a certain period of time.
Given long enough, patients who do not fully die in the complete biological sense, but who are declared brain dead, will usually start to build up toxins and wastes in the body. In this way, the organs can eventually dysfunction due to coagulopathy, fluid or electrolyte and nutrient imbalances, or even fail.
Thus, the organs will usually only be sustainable and viable for acceptable use up until a certain length of time. This may depend on factors such as how well the patient is maintained, any comorbidities, the skill of the healthcare teams and the quality their facilities.
A major point of contention is whether transplantation should be allowed at all if the patient is not yet fully biologically dead, and if brain death is acceptable, whether the person's whole brain needs to have died, or if the death of a certain part of the brain is enough for legal and ethical and moral purposes.
Most organ donation for organ transplantation is done in the setting of brain death. However, in Japan this is a fraught point, and prospective donors may designate either brain death or cardiac death – see organ transplantation in Japan.
In some nations such as Belgium, France, Netherlands, New Zealand, Poland, Portugal, Singapore and Spain, everyone is automatically an organ donor unless they opt out of the system. Elsewhere, consent from family members or next-of-kin is required for organ donation. The non-living donor is kept on ventilator support until the organs have been surgically removed. If a brain-dead individual is not an organ donor, ventilator and drug support is discontinued and cardiac death is allowed to occur.
In the United States, where since the 1980s the Uniform Determination of Death Act has defined death as the irreversible cessation of the function of either the brain or the heart and lungs, the 21st century has seen an order-of-magnitude increase of donation following cardiac death.
In 1995, only one out of 100 dead donors in the nation gave their organs following the declaration of cardiac death. That figure grew to almost 11 percent in 2008, according to the Scientific Registry of Transplant Recipients. That increase has provoked ethical concerns about the interpretation of "irreversible" since "patients may still be alive five or even 10 minutes after cardiac arrest because, theoretically, their hearts could be restarted, [and thus are] clearly not dead because their condition was reversible."
Gender inequality:
The majority of organ donors are women. For example, in the United States, 62% of kidney donors and 53% of liver donors are women. In India, women constitute 74% of kidney donors and 60.5% of liver donors. Additionally, the number of female organ recipients is conspicuously lower than that of male recipients. In the U.S., 35% of liver recipients and 39% of kidney recipients are women. In India, the figures are 24% and 19% respectively.
Political issues:
There are also controversial issues regarding how organs are allocated to recipients. For example, some believe that livers should not be given to alcoholics in danger of reversion, while others view alcoholism as a medical condition like diabetes. Faith in the medical system is important to the success of organ donation.
Brazil switched to an opt-out system and ultimately had to withdraw it because it further alienated patients who already distrusted the country's medical system. Adequate funding, strong political will to see transplant outcomes improve, and the existence of specialized training, care and facilities also increase donation rates.
Expansive legal definitions of death, such as Spain uses, also increase the pool of eligible donors by allowing physicians to declare a patient to be dead at an earlier stage, when the organs are still in good physical condition. Allowing or forbidding payment for organs affects the availability of organs. Generally, where organs cannot be bought or sold, quality and safety are high, but supply is not adequate to the demand. Where organs can be purchased, the supply increases.
Iran adopted a system of paying kidney donors in 1988 and within 11 years it became the only country in the world to clear its waiting list for transplants — The Economist
Healthy humans have two kidneys, a redundancy that enables living donors (inter vivos) to give a kidney to someone who needs it. The most common transplants are to close relatives, but people have given kidneys to other friends. The rarest type of donation is the undirected donation whereby a donor gives a kidney to a stranger. Less than a few hundred of such kidney donations have been performed.
In recent years, searching for altruistic donors via the internet has also become a way to find life saving organs. However, internet advertising for organs is a highly controversial practice, as some scholars believe it undermines the traditional list-based allocation system.
The National Transplant Organization of Spain is one of the most successful in the world (Spain has been the world leader in organ donation for decades), but it still cannot meet the demand, as 10% of those needing a transplant die while still on the transplant list. Donations from corpses are anonymous, and a network for communication and transport allows fast extraction and transplant across the country.
Under Spanish law, every corpse can provide organs unless the deceased person had expressly rejected it. Because family members still can forbid the donation, carefully trained doctors ask the family for permission, making it very similar in practice to the United States system.
In the overwhelming majority of cases, organ donation is not possible for reasons of recipient safety, match failures, or organ condition. Even in Spain, which has the highest organ donation rate in the world, there are only 35.1 actual donors per million people, and there are hundreds of patients on the waiting list.
This rate compares to 24.8 per million in Austria, where families are rarely asked to donate organs, and 22.2 per million in France, which—like Spain—has a presumed-consent system.
Prison inmates:
See also: Organ donation in the United States prison population
In the United States, prisoners are not discriminated against as organ recipients and are equally eligible for organ transplants along with the general population.
A 1976 U.S. Supreme Court case ruled that withholding health care from prisoners constituted "cruel and unusual punishment". United Network for Organ Sharing, the organization that coordinates available organs with recipients, does not factor a patient's prison status when determining suitability for a transplant.
An organ transplant and follow-up care can cost the prison system up to one million dollars.
If a prisoner qualifies, a state may allow compassionate early release to avoid high costs associated with organ transplants. However, an organ transplant may save the prison system substantial costs associated with dialysis and other life-extending treatments required by the prisoner with the failing organ. For example, the estimated cost of a kidney transplant is about $111,000.
A prisoner's dialysis treatments are estimated to cost a prison $120,000 per year. Because donor organs are in short supply, there are more people waiting for a transplant than available organs. When a prisoner receives an organ, there is a high probability that someone else will die waiting for the next available organ.
A response to this ethical dilemma states that felons who have a history of violent crime, who have violated others’ basic rights, have lost the right to receive an organ transplant, though it is noted that it would be necessary "to reform our justice system to minimize the chance of an innocent person being wrongly convicted of a violent crime and thus being denied an organ transplant"
Prisons typically do not allow inmates to donate organs to anyone but immediate family members. There is no law against prisoner organ donation; however, the transplant community has discouraged use of prisoner's organs since the early 1990s due to concern over prisons' high-risk environment for infectious diseases.
Physicians and ethicists also criticize the idea because a prisoner is not able to consent to the procedure in a free and non-coercive environment, especially if given inducements to participate.
However, with modern testing advances to more safely rule out infectious disease and by ensuring that there are no incentives offered to participate, some have argued that prisoners can now voluntarily consent to organ donation just as they can now consent to medical procedures in general. With careful safeguards, and with over 2 million prisoners in the U.S., they reason that prisoners can provide a solution for reducing organ shortages in the U.S.
While some have argued that prisoner participation would likely be too low to make a difference, one Arizona program started by former Maricopa County Sheriff Joe Arpaio encourages inmates to voluntarily sign up to donate their heart and other organs. As of 2015, there have been over 16,500 participants.
Similar initiatives have been started in other US states. In 2013, Utah became the first state to allow prisoners to sign up for organ donation upon death.
Religious viewpoints:
Main article: Religious views on organ donation
See also: Organ donation in Jewish law
There are several different religions that have different perspectives. Islam has a conflicting view regarding the issue, with half believing that it is against the religion. Muslims are commanded to seek medical attention when in need and saving life is a very important factor of the Islamic religion. Christianity is lenient on the topic of organ donation, and believe it is a service of life.
All major religions accept organ donation in at least some form on either utilitarian grounds (i.e., because of its life-saving capabilities) or deontological grounds (e.g., the right of an individual believer to make his or her own decision). Most religions, among them the Roman Catholic Church, support organ donation on the grounds that it constitutes an act of charity and provides a means of saving a life.
One religious group, The Jesus Christians, became known as "The Kidney Cult" because more than half its members had donated their kidneys altruistically. Jesus Christians claim altruistic kidney donation is a great way to "Do unto others what they would want you to do unto them."
Some religions impose certain restrictions on the types of organs that may be donated and/or on the means by which organs may be harvested and/or transplanted. For example, Jehovah's Witnesses require that organs be drained of any blood due to their interpretation of the Hebrew Bible/Christian Old Testament as prohibiting blood transfusion, and Muslims require that the donor have provided written consent in advance. A few groups disfavor organ transplantation or donation; notably, these include Shinto and those who follow the customs of the Gypsies.
Orthodox Judaism considers organ donation obligatory if it will save a life, as long as the donor is considered dead as defined by Jewish law. In both Orthodox Judaism and non-Orthodox Judaism, the majority view holds that organ donation is permitted in the case of irreversible cardiac rhythm cessation. In some cases, rabbinic authorities believe that organ donation may be mandatory, whereas a minority opinion considers any donation of a live organ as forbidden.
Organ shortfall:
The demand for organs significantly surpasses the number of donors everywhere in the world. There are more potential recipients on organ donation waiting lists than organ donors.
In particular, due to significant advances in dialysis techniques, patients suffering from end-stage renal disease (ESRD) can survive longer than ever before. Because these patients don't die as quickly as they used to, and as kidney failure increases with the rising age and prevalence of high blood pressure and diabetes in a society, the need especially for kidneys rises every year.
As of March 2014, about 121,600 people in the United States are on the waiting list, although about a third of those patients are inactive and could not receive a donated organ. Wait times and success rates for organs differ significantly between organs due to demand and procedure difficulty.
As of 2007, three-quarters of patients in need of an organ transplant were waiting for a kidney, and as such kidneys have much longer waiting times. As stated by the Gift of Life Donor Program website, the median patient who ultimately received an organ waited 4 months for a heart or lung—but 18 months for a kidney, and 18–24 months for a pancreas because demand for these organs substantially outstrips supply.
An increased prevalence of self-driving cars could exacerbate this problem: In the US, 13% of organ donations come from car crash victims, and autonomous vehicles are projected to reduce the frequency of car crashes.
In Australia, there are 10.8 transplants per million people, about a third of the Spanish rate. The Lions Eye Institute, in Western Australia, houses the Lions Eye Bank. The Bank was established in 1986 and coordinates the collection, processing and distribution of eye tissue for transplantation.
The Lions Eye Bank also maintains a waitlist of patients who require corneal graft operations. About 100 corneas are provided by the Bank for transplant each year, but there is still a waiting list for corneas."To an economist, this is a basic supply-and-demand gap with tragic consequences."
Approaches to addressing this shortfall include:
- Donor registries and "primary consent" laws, to remove the burden of the donation decision from the legal next-of-kin. Illinois adopted a policy of "mandated choice" in 2006, which requires driver's license registrants to answer the question "Do you want to be an organ donor?" Illinois has a registration rate of 60 percent compared to 38 percent nationally. The added cost of adding a question to the registration form is minimal.
- Monetary incentives for signing up to be a donor. Some economists have advocated going as far as allowing the sale of organs. The New York Times reported that "Gary Becker and Julio Jorge Elias argued in a recent paper that 'monetary incentives would increase the supply of organs for transplant sufficiently to eliminate the very large queues in organ markets, and the suffering and deaths of many of those waiting, without increasing the total cost of transplant surgery by more than 12 percent.'" Iran allows the sale of kidneys and has no waiting list. Organ futures have been proposed to incentivise donation through direct or indirect compensation. The primary argument against such proposals is a moral one; as the article notes, many find such a suggestion repugnant. As the National Kidney Foundation puts it, "Offering direct or indirect economic benefits in exchange for organ donation is inconsistent with our values as a society. Any attempt to assign a monetary value to the human body, or body parts, either arbitrarily, or through market forces, diminishes human dignity."
- An opt-out system ("dissent solution"), in which a potential donor or his/her relatives must take specific action to be excluded from organ donation, rather than specific action to be included. This model is used in several European countries, such as Austria, which has a registration rate eight times that of Germany, which uses an opt-in system.
- Social incentive programs, wherein members sign a legal agreement to direct their organs first to other members who are on the transplant waiting list. One historical example of a private organization using this model is LifeSharers, which is free to join and whose members agree to sign a document giving preferred access to their organs. "The proposal [for an organ mutual insurance pool] can be easily summarized: An individual would receive priority for any needed transplant if that individual agrees that his or her organs will be available to other members of the insurance pool in the event of his or her death. … The main purpose [of this proposal] is to increase the supply of transplantable organs in order to save or improve more lives."
- Technical advances allow the use of donors that were previously rejected. For example, hepatitis C can be knowingly transplanted and treated in the organ recipient.
In hospitals, organ network representatives routinely screen patient records to identify potential donors shortly in advance of their deaths.
Distribution:
The United States has two agencies that govern organ procurement and distribution within the country. The United Network for Organ Sharing and the Organ Procurement and Transplant Network (OPTN) regulate Organ Procurement Organizations (OPO) with regard to procurement and distribution ethics and standards.
OPOs are non-profit organizations charged with the evaluation, procurement and allocation of organs within their Designated Service Area (DSA). Once a donor has been evaluated and consent obtained, provisional allocation of organs commences.
UNOS developed a computer program that automatically generates donor specific match lists for suitable recipients based on the criteria that the patient was listed with. OPO coordinators enter donor information into the program and run the respective lists. Organ offers to potential recipients are made to transplant centers to make them aware of a potential organ.
The surgeon will evaluate the donor information and make a provisional determination of medical suitability to their recipient. Distribution varies slightly between different organs but is essentially very similar.
When lists are generated, many factors are taken into consideration; these factors include: distance of transplant center from the donor hospital, blood type, medical urgency, wait time, donor size and tissue typing.
For heart recipients medical urgency is denoted by a recipients "Status" (Status 1A, 1B and status 2).
Lungs are allocated based on a recipients Lung Allocation Score (LAS) that is determined based on the urgency of clinical need as well as the likelihood of benefit from the transplant.
Livers are allocated using both a status system and MELD/PELD score (Model for End-stage Liver Disease/Pediatric End-stage Liver Disease).
Kidney and pancreas lists are based on location, blood type, Human Leukocyte Antigen (HLA) typing and wait time. When a recipient for a kidney or pancreas has no direct antibodies to the donor HLA the match is said to be a 0 ABDR mismatch or zero antigen mismatch.
A zero mismatch organ has a low rate of rejection and allows a recipient to be on lower doses of immunosuppressive drugs. Since zero mismatches have such high graft survival these recipients are afforded priority regardless of location and wait time. UNOS has in place a "Payback" system to balance organs that are sent out of a DSA because of a zero mismatch.
Location of a transplant center with respect to a donor hospital is given priority due to the effects of Cold Ischemic Time (CIT). Once the organ is removed from the donor, blood no longer perfuses through the vessels and begins to starve the cells of oxygen (ischemia).
Each organ tolerates different ischemic times. Hearts and lungs need to be transplanted within 4–6 hours from recovery, liver about 8–10 hours and pancreas about 15 hours; kidneys are the most resilient to ischemia. Kidneys packaged on ice can be successfully transplanted 24–36 hours after recovery.
Developments in kidney preservation have yielded a device that pumps cold preservation solution through the kidneys vessels to prevent Delayed Graft Function (DGF) due to ischemia. Perfusion devices, often called kidney pumps, can extend graft survival to 36–48 hours post recovery for kidneys.
Recently similar devices have been developed for the heart and lungs, in an effort to increase distances procurement teams may travel to recover an organ.
Suicide:
People committing suicide have a higher rate of donating organs than average. One reason is lower negative response or refusal rate by the family and relatives, but the explanation for this remains to be clarified. In addition, donation consent is higher than average from people committing suicide.
Attempted suicide is a common cause of brain death (3.8%), mainly among young men. Organ donation is more common in this group compared to other causes of death.
Brain death may result in legal death, but still with the heart beating, and with mechanical ventilation all other vital organs may be kept completely alive and functional, providing optimal opportunities for organ transplantation.
Controversies:
In 2008, California transplant surgeon Hootan Roozrokh was charged with dependent adult abuse for prescribing what prosecutors alleged were excessive doses of morphine and sedatives to hasten the death of a man with adrenal leukodystrophy and irreversible brain damage, in order to procure his organs for transplant.
The case brought against Roozrokh was the first criminal case against a transplant surgeon in the US, and resulted in his acquittal. Further, Dr. Roozrokh successfully sued for defamation stemming from the incident.
At California's Emanuel Medical Center, neurologist Narges Pazouki, MD, said an organ-procurement organization representative pressed her to declare a patient brain-dead before the appropriate tests had been done.
In September 1999, eBay blocked an auction for "one functional human kidney" which had reached a highest bid of $5.7 million. Under United States federal laws, eBay was obligated to dismiss the auction for the selling of human organs which is punishable by up to five years in prison and a $50,000 fine.
On June 27, 2008, Indonesian Sulaiman Damanik, 26, pleaded guilty in a Singapore court for sale of his kidney to CTang's executive chair, Mr. Tang Wee Sung, 55, for 150 million rupiah (US$17,000). The Transplant Ethics Committee must approve living donor kidney transplants.
Organ trading is banned in Singapore and in many other countries to prevent the exploitation of "poor and socially disadvantaged donors who are unable to make informed choices and suffer potential medical risks." Toni, 27, the other accused, donated a kidney to an Indonesian patient in March, alleging he was the patient's adopted son, and was paid 186 million rupiah (US$21,000).
Public service announcements:
Marketing for organ donation must walk a fine line between stressing the need for organ donation and not being too forceful. If the marketing agent is too forceful, then the target of the message will react defensively to the request. According to psychological reactance theory, a person will perceive their freedom threatened and will react to restore the freedom.
According to Ashley Anker, the use of transportation theory has a positive effect on target reactions by marketing attempts. When public service announcements use recipient-focused messages, targets were more transported. Individuals who watched recipient-focused messages were more transported because potential donors experience empathy for the potential recipient.
Future public service announcements should use recipient-focused stories to elicit relationship formation between potential donors and recipients.
Awareness about organ donation leads to greater social support for organ donation, in turn leading to greater registration. By starting with promoting college students’ awareness of organ donation and moving to increasing social support for organ donation, the more likely people will be to register as organ donors.
The United States Department of Health funded a study by the University of Wisconsin Hospital to increase efforts to increase awareness and the number of registered donors by pursuing members of the university and their family and friends through social media. The results of the study showed a 20% increase in organ donation by creating support and awareness through social media.
See also:
- Australian Organ Donor Register
- Organ transplantation in Israel
- Organ transplantation in China
- MOHAN Foundation
- Sri Lanka Eye Donation Society
- Donate Life America
- Klaus Schäfer: Organ donation in Germany
- National Institute of Health's MedLine on Organ Donation
- Organ Donation India
- UK Transplant, part of NHS Blood and Transplant
- OrganDonor.gov (US)
- Portal for Organ Donation After Execution
- Portal for The National Network of Organ Donors
- Human Tissue Donation – NPR News Investigation
- G.A.V.E Life Prisoner Organ Donation
- Organ and Tissue Donation What Every Nurse Needs to Know course on www.RN.org
Affordable Care Act (aka "Obamacare")
- YouTube Video: 5 Things About The Affordable Care Act (ACA) (U.S. Department of Health and Human Services)
- YouTube Video: How Does The Affordable Care Act Work?
- YouTube Video: Affordable Care Act 12th Anniversary | March 23, 2022
The Affordable Care Act (ACA), formally known as the Patient Protection and Affordable Care Act and colloquially known as Obamacare, is a landmark U.S. federal statute enacted by the 111th United States Congress and signed into law by President Barack Obama on March 23, 2010.
Together with the Health Care and Education Reconciliation Act of 2010 amendment, it represents the U.S. healthcare system's most significant regulatory overhaul and expansion of coverage since the enactment of Medicare and Medicaid in 1965.
The ACA's major provisions came into force in 2014. By 2016, the uninsured share of the population had roughly halved, with estimates ranging from 20 to 24 million additional people covered.
The law also enacted a host of delivery system reforms intended to constrain healthcare costs and improve quality. After it went into effect, increases in overall healthcare spending slowed, including premiums for employer-based insurance plans.
The increased coverage was due, roughly equally, to an expansion of Medicaid eligibility and to changes to individual insurance markets. Both received new spending, funded through a combination of new taxes and cuts to Medicare provider rates and Medicare Advantage.
Several Congressional Budget Office (CBO) reports said that overall these provisions reduced the budget deficit, that repealing ACA would increase the deficit, and that the law reduced income inequality by taxing primarily the top 1% to fund roughly $600 in benefits on average to families in the bottom 40% of the income distribution.
The act largely retained the existing structure of Medicare, Medicaid, and the employer market, but individual markets were radically overhauled. Insurers were made to accept all applicants without charging based on preexisting conditions or demographic status (except age). To combat the resultant adverse selection, the act mandated that individuals buy insurance (or pay a fine/tax) and that insurers cover a list of "essential health benefits".
Before and after enactment the ACA faced strong political opposition, calls for repeal and legal challenges. In National Federation of Independent Business v. Sebelius, the Supreme Court ruled that states could choose not to participate in the law's Medicaid expansion, but upheld the law as a whole.
The federal health insurance exchange, HealthCare.gov, faced major technical problems at the beginning of its rollout in 2013. Polls initially found that a plurality of Americans opposed the act, although its individual provisions were generally more popular. By 2017, the law had majority support.
The Tax Cuts and Jobs Act of 2017 set the individual mandate penalty at $0 starting in 2019. This raised questions about whether the ACA was still constitutional. In June 2021, the Supreme Court upheld the ACA for the third time in California v. Texas.
Provisions:
See also: Provisions of the Patient Protection and Affordable Care Act
ACA amended the Public Health Service Act of 1944 and inserted new provisions on affordable care into Title 42 of the United States Code. The individual insurance market was radically overhauled, and many of the law's regulations applied specifically to this market, while the structure of Medicare, Medicaid, and the employer market were largely retained.
Some regulations applied to the employer market, and the law also made delivery system changes that affected most of the health care system.
Further information: Commission on Key National Indicators
Insurance regulations: individual policies:
All new individual major medical health insurance policies sold to individuals and families faced new requirements. The requirements took effect on January 1, 2014. They include:
In determining essential benefits, the law required that standard benefits should offer at least that of a "typical employer plan". States may require additional services.
Individual mandate:
The individual mandate required everyone to have insurance or pay a penalty. The mandate and limits on open enrollment were designed to avoid the insurance death spiral, minimize the free rider problem and prevent the healthcare system from succumbing to adverse selection.
The mandate was intended to increase the size and diversity of the insured population, including more young and healthy participants to broaden the risk pool, spreading costs.
Among the groups who were not subject to the individual mandate are:
The Tax Cuts and Jobs Act of 2017, set to $0 the penalty for not complying with the individual mandate, starting in 2019.
Exchanges:
Main article: Health insurance marketplace
ACA mandated that health insurance exchanges be provided for each state. The exchanges are regulated, largely online marketplaces, administered by either federal or state governments, where individuals, families and small businesses can purchase private insurance plans.
Exchanges first offered insurance for 2014. Some exchanges also provide access to Medicaid.
States that set up their own exchanges have some discretion on standards and prices. For example, states approve plans for sale, and thereby influence (through negotiations) prices. They can impose additional coverage requirements—such as abortion. Alternatively, states can make the federal government responsible for operating their exchanges.
Premium subsidies:
Individuals whose household incomes are between 100% and 400% of the federal poverty level (FPL) are eligible to receive federal subsidies for premiums for policies purchased on an ACA exchange, provided they are not eligible for Medicare, Medicaid, the Children's Health Insurance Program, or other forms of public assistance health coverage, and do not have access to affordable coverage (no more than 9.86% of income for the employee's coverage) through their own or a family member's employer.
Households below the federal poverty level are not eligible to receive these subsidies. Lawful Residents and some other legally present immigrants whose household income is below 100% FPL and are not otherwise eligible for Medicaid are eligible for subsidies if they meet all other eligibility requirements.
Married people must file taxes jointly to receive subsidies. Enrollees must have U.S. citizenship or proof of legal residency to obtain a subsidy.
The subsidies for an ACA plan purchased on an exchange stop at 400% of the federal poverty level (FPL). According to the Kaiser Foundation, this results in a sharp "discontinuity of treatment" at 400% FPL, which is sometimes called the "subsidy cliff". After-subsidy premiums for the second lowest cost silver plan (SCLSP) just below the cliff are 9.86% of income in 2019.
Subsidies are provided as an advanceable, refundable tax credit.
The amount of subsidy is sufficient to reduce the premium for the second-lowest-cost silver plan (SCLSP) on an exchange cost a sliding-scale percentage of income. The percentage is based on the percent of federal poverty level (FPL) for the household, and varies slightly from year to year. In 2019, it ranged from 2.08% of income (100%-133% FPL) to 9.86% of income (300%-400% FPL).[70] The subsidy can be used for any plan available on the exchange, but not catastrophic plans. The subsidy may not exceed the premium for the purchased plan.
(In this section, the term "income" refers to modified adjusted gross income.
Small businesses are eligible for a tax credit provided they enroll in the SHOP Marketplace.
Double-click on figure below for additional information:
Together with the Health Care and Education Reconciliation Act of 2010 amendment, it represents the U.S. healthcare system's most significant regulatory overhaul and expansion of coverage since the enactment of Medicare and Medicaid in 1965.
The ACA's major provisions came into force in 2014. By 2016, the uninsured share of the population had roughly halved, with estimates ranging from 20 to 24 million additional people covered.
The law also enacted a host of delivery system reforms intended to constrain healthcare costs and improve quality. After it went into effect, increases in overall healthcare spending slowed, including premiums for employer-based insurance plans.
The increased coverage was due, roughly equally, to an expansion of Medicaid eligibility and to changes to individual insurance markets. Both received new spending, funded through a combination of new taxes and cuts to Medicare provider rates and Medicare Advantage.
Several Congressional Budget Office (CBO) reports said that overall these provisions reduced the budget deficit, that repealing ACA would increase the deficit, and that the law reduced income inequality by taxing primarily the top 1% to fund roughly $600 in benefits on average to families in the bottom 40% of the income distribution.
The act largely retained the existing structure of Medicare, Medicaid, and the employer market, but individual markets were radically overhauled. Insurers were made to accept all applicants without charging based on preexisting conditions or demographic status (except age). To combat the resultant adverse selection, the act mandated that individuals buy insurance (or pay a fine/tax) and that insurers cover a list of "essential health benefits".
Before and after enactment the ACA faced strong political opposition, calls for repeal and legal challenges. In National Federation of Independent Business v. Sebelius, the Supreme Court ruled that states could choose not to participate in the law's Medicaid expansion, but upheld the law as a whole.
The federal health insurance exchange, HealthCare.gov, faced major technical problems at the beginning of its rollout in 2013. Polls initially found that a plurality of Americans opposed the act, although its individual provisions were generally more popular. By 2017, the law had majority support.
The Tax Cuts and Jobs Act of 2017 set the individual mandate penalty at $0 starting in 2019. This raised questions about whether the ACA was still constitutional. In June 2021, the Supreme Court upheld the ACA for the third time in California v. Texas.
Provisions:
See also: Provisions of the Patient Protection and Affordable Care Act
ACA amended the Public Health Service Act of 1944 and inserted new provisions on affordable care into Title 42 of the United States Code. The individual insurance market was radically overhauled, and many of the law's regulations applied specifically to this market, while the structure of Medicare, Medicaid, and the employer market were largely retained.
Some regulations applied to the employer market, and the law also made delivery system changes that affected most of the health care system.
Further information: Commission on Key National Indicators
Insurance regulations: individual policies:
All new individual major medical health insurance policies sold to individuals and families faced new requirements. The requirements took effect on January 1, 2014. They include:
- Guaranteed issue prohibits insurers from denying coverage to individuals due to preexisting conditions.
- States were required to ensure the availability of insurance for individual children who did not have coverage via their families.
- A partial community rating allows premiums to vary only by age and location, regardless of preexisting conditions. Premiums for older applicants can be no more than three times those for the youngest.
- Essential health benefits must be provided. The National Academy of Medicine defines the law's "essential health benefits" as:
- "ambulatory patient services;
- emergency services;
- hospitalization;
- maternity and newborn care;
- mental health and substance use disorder services,
- including behavioral health treatment;
- prescription drugs;
- rehabilitative and habilitative services and devices;
- laboratory services;
- preventive and wellness services and chronic disease management;
- and pediatric services,
- including oral and vision care"
- and others rated Level A or B by the U.S. Preventive Services Task Force.
In determining essential benefits, the law required that standard benefits should offer at least that of a "typical employer plan". States may require additional services.
- Preventive care and screenings for women. "[A]ll Food and Drug Administration approved contraceptive methods, sterilization procedures, and patient education and counseling for all women with reproductive capacity". This mandate applies to all employers and educational institutions except for religious organizations. These regulations were included on the recommendations of the Institute of Medicine.
- Annual and lifetime coverage caps on essential benefits were banned.
- Insurers are forbidden from dropping policyholders when they become ill.
- All policies must provide an annual maximum out-of-pocket (MOOP) payment cap for an individual's or family's medical expenses (excluding premiums). After the MOOP payment is reached, all remaining costs must be paid by the insurer.
- Preventive care, vaccinations and medical screenings cannot be subject to co-payments, co-insurance or deductibles. Specific examples of covered services include:
- mammograms and colonoscopies,
- wellness visits,
- gestational diabetes screening,
- HPV testing,
- STI counseling,
- HIV screening and counseling,
- contraceptive methods,
- breastfeeding support/supplies
- and domestic violence screening and counseling.
- The law established four tiers of coverage: bronze, silver, gold and platinum. All categories offer essential health benefits. The categories vary in their division of premiums and out-of-pocket costs: bronze plans have the lowest monthly premiums and highest out-of-pocket costs, while platinum plans are the reverse. The percentages of health care costs that plans are expected to cover through premiums (as opposed to out-of-pocket costs) are, on average: 60% (bronze), 70% (silver), 80% (gold), and 90% (platinum).
- Insurers are required to implement an appeals process for coverage determination and claims on all new plans.
- Insurers must spend at least 80–85% of premium dollars on health costs; rebates must be issued if this is violated.
Individual mandate:
The individual mandate required everyone to have insurance or pay a penalty. The mandate and limits on open enrollment were designed to avoid the insurance death spiral, minimize the free rider problem and prevent the healthcare system from succumbing to adverse selection.
The mandate was intended to increase the size and diversity of the insured population, including more young and healthy participants to broaden the risk pool, spreading costs.
Among the groups who were not subject to the individual mandate are:
- Illegal immigrants, estimated at 8 million—or roughly a third of the 23 million projection—are ineligible for insurance subsidies and Medicaid. They remain eligible for emergency services.
- Medicaid-eligible citizens not enrolled in Medicaid.
- Citizens whose insurance coverage would cost more than 8% of household income.
- Citizens who live in states that opt-out of Medicaid expansion and who qualify for neither existing Medicaid coverage nor subsidized coverage.
The Tax Cuts and Jobs Act of 2017, set to $0 the penalty for not complying with the individual mandate, starting in 2019.
Exchanges:
Main article: Health insurance marketplace
ACA mandated that health insurance exchanges be provided for each state. The exchanges are regulated, largely online marketplaces, administered by either federal or state governments, where individuals, families and small businesses can purchase private insurance plans.
Exchanges first offered insurance for 2014. Some exchanges also provide access to Medicaid.
States that set up their own exchanges have some discretion on standards and prices. For example, states approve plans for sale, and thereby influence (through negotiations) prices. They can impose additional coverage requirements—such as abortion. Alternatively, states can make the federal government responsible for operating their exchanges.
Premium subsidies:
Individuals whose household incomes are between 100% and 400% of the federal poverty level (FPL) are eligible to receive federal subsidies for premiums for policies purchased on an ACA exchange, provided they are not eligible for Medicare, Medicaid, the Children's Health Insurance Program, or other forms of public assistance health coverage, and do not have access to affordable coverage (no more than 9.86% of income for the employee's coverage) through their own or a family member's employer.
Households below the federal poverty level are not eligible to receive these subsidies. Lawful Residents and some other legally present immigrants whose household income is below 100% FPL and are not otherwise eligible for Medicaid are eligible for subsidies if they meet all other eligibility requirements.
Married people must file taxes jointly to receive subsidies. Enrollees must have U.S. citizenship or proof of legal residency to obtain a subsidy.
The subsidies for an ACA plan purchased on an exchange stop at 400% of the federal poverty level (FPL). According to the Kaiser Foundation, this results in a sharp "discontinuity of treatment" at 400% FPL, which is sometimes called the "subsidy cliff". After-subsidy premiums for the second lowest cost silver plan (SCLSP) just below the cliff are 9.86% of income in 2019.
Subsidies are provided as an advanceable, refundable tax credit.
The amount of subsidy is sufficient to reduce the premium for the second-lowest-cost silver plan (SCLSP) on an exchange cost a sliding-scale percentage of income. The percentage is based on the percent of federal poverty level (FPL) for the household, and varies slightly from year to year. In 2019, it ranged from 2.08% of income (100%-133% FPL) to 9.86% of income (300%-400% FPL).[70] The subsidy can be used for any plan available on the exchange, but not catastrophic plans. The subsidy may not exceed the premium for the purchased plan.
(In this section, the term "income" refers to modified adjusted gross income.
Small businesses are eligible for a tax credit provided they enroll in the SHOP Marketplace.
Double-click on figure below for additional information:
Cost-sharing reduction subsidies:
Main article: Cost sharing reductions subsidy
As written, ACA mandated that insurers reduce copayments and deductibles for ACA exchange enrollees earning less than 250% of the FPL. Medicaid recipients were not eligible for the reductions.
So-called cost-sharing reduction (CSR) subsidies were to be paid to insurance companies to fund the reductions. During 2017, approximately $7 billion in CSR subsidies were to be paid, versus $34 billion for premium tax credits.
The latter was defined as mandatory spending that does not require an annual Congressional appropriation. CSR payments were not explicitly defined as mandatory. This led to litigation and disruption later.
Risk management:
ACA implemented multiple approaches to helping mitigate the disruptions to insurers that came with its many changes.
Risk corridors:
The risk-corridor program was a temporary risk management device. It was intended to encourage reluctant insurers into ACA insurance market from 2014 to 2016. For those years the Department of Health and Human Services (DHHS) would cover some of the losses for insurers whose plans performed worse than they expected.
Loss-making insurers would receive payments paid for in part by profit-making insurers. Similar risk corridors had been established for the Medicare prescription drug benefit.
While many insurers initially offered exchange plans, the program did not pay for itself as planned, losing up to $8.3 billion for 2014 and 2015. Authorization had to be given so DHHS could pay insurers from "general government revenues". However, the Consolidated Appropriations Act, 2014 (H.R. 3547) stated that no funds "could be used for risk-corridor payments". leaving the government in a potential breach of contract with insurers who offered qualified health plans.
Several insurers sued the government at the United States Court of Federal Claims to recover the funds believed owed to them under the Risk Corridors program. While several were summarily closed, in the case of Moda Health v the United States, Moda Health won a $214-million judgment in February 2017.
Federal Claims judge Thomas C. Wheeler stated, "the Government made a promise in the risk corridors program that it has yet to fulfill. Today, the court directs the Government to fulfill that promise. After all, to say to [Moda], 'The joke is on you. You shouldn't have trusted us,' is hardly worthy of our great government."
Moda Health's case was appealed by the government to the United States Court of Appeals for the Federal Circuit along with the appeals of the other insurers; here, the Federal Circuit reversed the Moda Health ruling and ruled across all the cases in favor of the government, that the appropriations riders ceded the government from paying out remain money due to the insurers.
The Supreme Court reversed this ruling in the consolidated case, Maine Community Health Options v. United States, reaffirming as with Judge Wheeler that the government had a responsibility to pay those funds under the ACA and the use of riders to de-obligate its from those payments was illegal.
Reinsurance:
The temporary reinsurance program is meant to stabilize premiums by reducing the incentive for insurers to raise premiums due to concerns about higher-risk enrollees. Reinsurance was based on retrospective costs rather than prospective risk evaluations. Reinsurance was available from 2014 through 2016.
Risk adjustment:
Risk adjustment involves transferring funds from plans with lower-risk enrollees to plans with higher-risk enrollees. It was intended to encourage insurers to compete based on value and efficiency rather than by attracting healthier enrollees. Of the three risk management programs, only risk adjustment was permanent. Plans with low actuarial risk compensate plans with high actuarial risk.
Medicaid expansion:
Main article: Medicaid coverage gap
ACA revised and expanded Medicaid eligibility starting in 2014. All U.S. citizens and legal residents with income up to 133% of the poverty line, including adults without dependent children, would qualify for coverage in any state that participated in the Medicaid program.
The federal government was to pay 100% of the increased cost in 2014, 2015 and 2016; 95% in 2017, 94% in 2018, 93% in 2019, and 90% in 2020 and all subsequent years.
A 5% "income disregard" made the effective income eligibility limit for Medicaid 138% of the poverty level. However, the Supreme Court ruled in NFIB v. Sebelius that this provision of ACA was coercive, and that states could choose to continue at pre-ACA eligibility levels.
Medicare savings:
Medicare reimbursements were reduced to insurers and drug companies for private Medicare Advantage policies that the Government Accountability Office and Medicare Payment Advisory Commission found to be excessively costly relative to standard Medicare; and to hospitals that failed standards of efficiency and care.
Taxes:
Medicare taxes:
Income from self-employment and wages of single individuals in excess of $200,000 annually are subjected to an additional tax of 0.9%. The threshold amount is $250,000 for a married couple filing jointly (threshold applies to their total compensation), or $125,000 for a married person filing separately.
In ACA's companion legislation, the Health Care and Education Reconciliation Act of 2010, an additional tax of 3.8% was applied to unearned income, specifically the lesser of net investment income and the amount by which adjusted gross income exceeds the above income limits.
Excise taxes:
ACA included an excise tax of 40% ("Cadillac tax") on total employer premium spending in excess of specified dollar amounts (initially $10,200 for single coverage and $27,500 for family coverage) indexed to inflation. This tax was originally scheduled to take effect in 2018, but was delayed until 2020 by the Consolidated Appropriations Act, 2016 and again to 2022.
Excise taxes totaling $3 billion were levied on importers and manufacturers of prescription drugs. An excise tax of 2.3% on medical devices and a 10% excise tax on indoor tanning services were applied as well. The tax was repealed in late 2019.
SCHIP:
The State Children's Health Insurance Program (CHIP) enrollment process was simplified.
Dependents:
Dependents were permitted to remain on their parents' insurance plan until their 26th birthday, including dependents who no longer lived with their parents, are not a dependent on a parent's tax return, are no longer a student, or are married.
Employer mandate:
Businesses that employ fifty or more people but do not offer health insurance to their full-time employees are assessed additional tax if the government has subsidized a full-time employee's healthcare through tax deductions or other means. This is commonly known as the employer mandate.
This provision was included to encourage employers to continue providing insurance once the exchanges began operating.
Delivery system reforms:
The act includes delivery system reforms intended to constrain costs and improve quality. These include Medicare payment changes to discourage hospital-acquired conditions and readmissions, bundled payment initiatives, the Center for Medicare and Medicaid Innovation, the Independent Payment Advisory Board, and accountable care organizations.
Hospital quality:
Health care cost/quality initiatives included incentives to reduce hospital infections, adopt electronic medical records, and to coordinate care and prioritize quality over quantity.
Bundled payments:
Medicare switched from fee-for-service to bundled payments. A single payment was to be paid to a hospital and a physician group for a defined episode of care (such as a hip replacement) rather than separate payments to individual service providers.
Accountable care organizations
Main article: Accountable care organization
The Medicare Shared Savings Program (MSSP) was established by section 3022 of the Affordable Care Act. It is the program by which an accountable care organization interacts with the federal government, and by which accountable care organizations can be created. It is a fee-for-service model.
The Act allowed the creation of accountable care organizations (ACOs), which are groups of doctors, hospitals and other providers that commit to give coordinated care to Medicare patients. ACOs were allowed to continue using fee-for-service billing.
They receive bonus payments from the government for minimizing costs while achieving quality benchmarks that emphasize prevention and mitigation of chronic disease. Missing cost or quality benchmarks subjected them to penalties.
Unlike health maintenance organizations, ACO patients are not required to obtain all care from the ACO. Also, unlike HMOs, ACOs must achieve quality-of-care goals.
Medicare drug benefit (Part D):
Medicare Part D participants received a 50% discount on brand name drugs purchased after exhausting their initial coverage and before reaching the catastrophic-coverage threshold.
By 2020, the "doughnut hole" would be completely filled.
State waivers:
From 2017 onwards, states can apply for a "waiver for state innovation" which allows them to conduct experiments that meet certain criteria. To obtain a waiver, a state must pass legislation setting up an alternative health system that provides insurance at least as comprehensive and as affordable as ACA, covers at least as many residents and does not increase the federal deficit.
These states can escape some of ACA's central requirements, including the individual and employer mandates and the provision of an insurance exchange. The state would receive compensation equal to the aggregate amount of any federal subsidies and tax credits for which its residents and employers would have been eligible under ACA, if they cannot be paid under the state plan.
Other insurance provisions:
The Community Living Assistance Services and Supports Act (or CLASS Act) established a voluntary and public long-term care insurance option for employees, The program was abolished as impractical without ever having taken effect.
Consumer Operated and Oriented Plans (CO-OP):
Member-governed non-profit insurers, could start providing health care coverage, based on a 5-year federal loan. As of 2017, only four of the original 23 co-ops were still in operation.
Nutrition labeling requirements:
Nutrition labeling requirements officially took effect in 2010, but implementation was delayed, and they actually took effect on May 7, 2018.
Legislative history:
Main articles:
ACA followed a long series of unsuccessful attempts by one party or the other to pass major insurance reforms. Innovations were limited to health savings accounts (2003), medical savings accounts (1996) or flexible spending accounts, which increased insurance options, but did not materially expand coverage.
Health care was a major factor in multiple elections, but until 2009, neither party had the votes to overcome the other's opposition.
Individual mandate:
The concept of an individual mandate goes back to at least 1989, when The Heritage Foundation, a conservative think-tank, proposed an individual mandate as an alternative to single-payer health care.
It was championed for a time by conservative economists and Republican senators as a market-based approach to healthcare reform on the basis of individual responsibility and avoidance of free rider problems. Specifically, because the 1986 Emergency Medical Treatment and Active Labor Act (EMTALA) requires any hospital participating in Medicare (nearly all do) to provide emergency care to anyone who needs it, the government often indirectly bore the cost of those without the ability to pay.
President Bill Clinton proposed a major healthcare reform bill in 1993 that ultimately failed. Clinton negotiated a compromise with the 105th Congress to instead enact the State Children's Health Insurance Program (SCHIP) in 1997.
The failed Clinton plan included a mandate for employers to provide health insurance to all employees through a regulated marketplace of health maintenance organizations. Republican senators proposed an alternative that would have required individuals, but not employers, to buy insurance.
The 1993 Republican Health Equity and Access Reform Today (HEART) Act, contained a "universal coverage" requirement with a penalty for noncompliance—an individual mandate—as well as subsidies to be used in state-based 'purchasing groups'.
Advocates included prominent Republican senators such as John Chafee, Orrin Hatch, Chuck Grassley, Bob Bennett and Kit Bond.
The 1994 Republican Consumer Choice Health Security Act, initially contained an individual mandate with a penalty provision; however, author Don Nickles subsequently removed the mandate, stating, "government should not compel people to buy health insurance".
At the time of these proposals, Republicans did not raise constitutional issues; Mark Pauly, who helped develop a proposal that included an individual mandate for George H. W. Bush, remarked, "I don't remember that being raised at all. The way it was viewed by the Congressional Budget Office in 1994 was, effectively, as a tax."
In 2006, an insurance expansion bill was enacted at the state level in Massachusetts. The bill contained both an individual mandate and an insurance exchange. Republican Governor Mitt Romney vetoed the mandate, but after Democrats overrode his veto, he signed it into law.
Romney's implementation of the 'Health Connector' exchange and individual mandate in Massachusetts was at first lauded by Republicans. During Romney's 2008 presidential campaign, Senator Jim DeMint praised Romney's ability to "take some good conservative ideas, like private health insurance, and apply them to the need to have everyone insured".
Romney said of the individual mandate: "I'm proud of what we've done. If Massachusetts succeeds in implementing it, then that will be the model for the nation."
In 2007 Republican Senator Bob Bennett and Democratic Senator Ron Wyden introduced the Healthy Americans Act, which featured an individual mandate and state-based, regulated insurance markets called "State Health Help Agencies". The bill attracted bipartisan support, but died in committee. Many of its sponsors and co-sponsors remained in Congress during the 2008 healthcare debate.
By 2008 many Democrats were considering this approach as the basis for healthcare reform. Experts said the legislation that eventually emerged from Congress in 2009 and 2010 bore similarities to the 2007 bill and that it took ideas from the Massachusetts reforms.
Academic foundation:
A driving force behind Obama's healthcare reform was Peter Orszag, Director of the Office of Management and Budget. Obama called Orszag his "healthcare czar" because of his knowledge of healthcare reform.
Orszag had previously been director of the Congressional Budget Office, and under his leadership the agency had focused on using cost analysis to create an affordable and effective approach to health care reform. Orszag claimed that healthcare reform became Obama's top agenda item because he wanted it to be his legacy.
According to an article by Ryan Lizza in The New Yorker, the core of "the Obama budget is Orszag's belief [in]...a government empowered with research on the most effective medical treatments". Obama bet "his presidency on Orszag's thesis of comparative effectiveness."
Orszag's policies were influenced by an article in The Annals of Internal Medicine co-authored by Elliott S. Fisher, David Wennberg and others. The article presented strong evidence based on the co-authors' research that numerous procedures, therapies and tests were being delivered with scant evidence of their medical value.
If those procedures and tests could be eliminated, this evidence suggested, medical costs might provide the savings to give healthcare to the uninsured population. After reading a The New Yorker article that used the "Dartmouth findings" to compare two counties in Texas with enormous variations in Medicare costs using hard data, Obama directed that his entire staff read it. More than anything else, the Dartmouth data intrigued Obama: Since it gave him an academic rationale for reshaping medicine.
The concept of comparing the effectiveness of healthcare options based on hard data ("comparative effectiveness" and "evidence-based medicine") was pioneered by John E. Wennberg, founder of The Dartmouth Institute, co-founder of The Foundation for Informed Medical Decision Making and senior advisor to Health Dialog Inc., a venture that he and his researchers created to help insurers implement the Dartmouth findings.
Healthcare debate, 2008–10
See also: Health care reforms proposed during the Obama administration
Healthcare reform was a major topic during the 2008 Democratic presidential primaries.
As the race narrowed, attention focused on the plans presented by the two leading candidates, Hillary Clinton and the eventual nominee, Barack Obama. Each candidate proposed a plan to cover the approximately 45 million Americans estimated to not have health insurance at some point each year.
Clinton's proposal would have required all Americans to obtain coverage (in effect, an individual mandate), while Obama's proposal provided a subsidy without a mandate.
During the general election, Obama said fixing healthcare would be one of his top four priorities as president. Obama and his opponent, Senator John McCain, both proposed health insurance reforms, though their plans differed.
McCain proposed tax credits for health insurance purchased in the individual market, which was estimated to reduce the number of uninsured people by about 2 million by 2018. Obama proposed private and public group insurance, income-based subsidies, consumer protections, and expansions of Medicaid and SCHIP, which was estimated at the time to reduce the number of uninsured people by 33.9 million by 2018 at a higher cost.
Obama announced to a joint session of Congress in February 2009 his intent to work with Congress to construct a plan for healthcare reform. By July, a series of bills were approved by committees within the House of Representatives.
On the Senate side, from June to September, the Senate Finance Committee held a series of 31 meetings to develop a proposal. This group—in particular, Democrats Max Baucus, Jeff Bingaman and Kent Conrad, along with Republicans Mike Enzi, Chuck Grassley and Olympia Snowe—met for more than 60 hours, and the principles they discussed, in conjunction with the other committees, became the foundation of a Senate bill.
Congressional Democrats and health policy experts, such as MIT economics professor Jonathan Gruber and David Cutler, argued that guaranteed issue would require both community rating and an individual mandate to ensure that adverse selection and/or "free riding" would not result in an insurance "death spiral".
They chose this approach after concluding that filibuster-proof support in the Senate was not present for more progressive plans such as single-payer. By deliberately drawing on bipartisan ideas—the same basic outline was supported by former Senate Majority Leaders Howard Baker, Bob Dole, Tom Daschle and George J. Mitchell—the bill's drafters hoped to garner the necessary votes.
However, following the incorporation of an individual mandate into the proposal, Republicans threatened to filibuster any bill that contained it. Senate Minority Leader Mitch McConnell, who led the Republican response, concluded Republicans should not support the bill.
Republican senators, including those who had supported earlier proposals with a similar mandate, began to describe the mandate as "unconstitutional". Journalist Ezra Klein wrote in The New Yorker, "a policy that once enjoyed broad support within the Republican Party suddenly faced unified opposition."
The reform attracted attention from lobbyists, including deals between lobby groups and the advocates to win the support of groups who had opposed past proposals
During the August 2009 summer congressional recess, many members went back to their districts and held town hall meetings on the proposals.
The nascent Tea Party movement organized protests and many conservative groups and individuals attended the meetings to oppose the proposed reforms. Threats were made against members of Congress over the course of the debate.
In September 2009 Obama delivered another speech to a joint session of Congress supporting the negotiations. On November 7, the House of Representatives passed the Affordable Health Care for America Act on a 220–215 vote and forwarded it to the Senate for passage.
Senate:
The Senate began work on its own proposals while the House was still working. The United States Constitution requires all revenue-related bills to originate in the House. To formally comply with this requirement, the Senate repurposed H.R. 3590, a bill regarding housing tax changes for service members. It had been passed by the House as a revenue-related modification to the Internal Revenue Code.
The bill became the Senate's vehicle for its healthcare reform proposal, discarding the bill's original content. The bill ultimately incorporated elements of proposals that were reported favorably by the Senate Health and Finance committees. With the Republican Senate minority vowing to filibuster, 60 votes would be necessary to pass the Senate.
At the start of the 111th Congress, Democrats had 58 votes. The Minnesota Senate election was ultimately won by Democrat Al Franken, making 59. Arlen Specter switched to the Democratic party in April 2009, giving them 60 seats, enough to end a filibuster.
Negotiations were undertaken attempting to satisfy moderate Democrats and to bring Republican senators aboard; particular attention was given to Republicans Bennett, Enzi, Grassley and Snowe.
After the Finance Committee vote on October 15, negotiations turned to moderate Democrats. Senate Majority Leader Harry Reid focused on satisfying centrists. The holdouts came down to Joe Lieberman of Connecticut, an independent who caucused with Democrats, and conservative Nebraska Democrat Ben Nelson.
Lieberman's demand that the bill not include a public option was met, although supporters won various concessions, including allowing state-based public options such as Vermont's failed Green Mountain Care.
The White House and Reid addressed Nelson's concerns during a 13-hour negotiation with two concessions: a compromise on abortion, modifying the language of the bill "to give states the right to prohibit coverage of abortion within their own insurance exchanges", which would require consumers to pay for the procedure out of pocket if the state so decided; and an amendment to offer a higher rate of Medicaid reimbursement for Nebraska. The latter half of the compromise was derisively termed the "Cornhusker Kickback" and was later removed.
On December 23, the Senate voted 60–39 to end debate on the bill: a cloture vote to end the filibuster. The bill then passed, also 60–39, on December 24, 2009, with all Democrats and two independents voting for it, and all Republicans against (except Jim Bunning, who did not vote). The bill was endorsed by the American Medical Association and AARP.
On January 19, 2010, Massachusetts Republican Scott Brown was elected to the Senate in a special election to replace the recently deceased Ted Kennedy, having campaigned on giving the Republican minority the 41st vote needed to sustain Republican filibusters.
Additionally, the symbolic importance of losing Kennedy's traditionally Democratic Massachusetts seat made many Congressional Democrats concerned about the political cost of the bill.
House:
With Democrats no longer able to get the 60 votes to break a filibuster in the Senate, White House Chief of Staff Rahm Emanuel argued that Democrats should scale back to a less ambitious bill, but House Speaker Nancy Pelosi pushed back, dismissing more moderate reform as "Kiddie Care".
Obama remained insistent on comprehensive reform. The news that Anthem in California intended to raise premium rates for its patients by as much as 39% gave him new evidence of the need for reform. On February 22, he laid out a "Senate-leaning" proposal to consolidate the bills. He held a meeting with both parties' leaders on February 25. The Democrats decided the House would pass the Senate's bill, to avoid another Senate vote.
House Democrats had expected to be able to negotiate changes in a House–Senate conference before passing a final bill. Since any bill that emerged from conference that differed from the Senate bill would have to pass the Senate over another Republican filibuster, most House Democrats agreed to pass the Senate bill on condition that it be amended by a subsequent bill.
They drafted the Health Care and Education Reconciliation Act, which could be passed by the reconciliation process.
Per the Congressional Budget Act of 1974, reconciliation cannot be subject to a filibuster. But reconciliation is limited to budget changes, which is why the procedure was not used to pass ACA in the first place; the bill had inherently non-budgetary regulations.
Although the already-passed Senate bill could not have been passed by reconciliation, most of House Democrats' demands were budgetary: "these changes—higher subsidy levels, different kinds of taxes to pay for them, nixing the Nebraska Medicaid deal—mainly involve taxes and spending. In other words, they're exactly the kinds of policies that are well-suited for reconciliation."
The remaining obstacle was a pivotal group of pro-life Democrats led by Bart Stupak who were initially reluctant to support the bill. The group found the possibility of federal funding for abortion significant enough to warrant opposition.
The Senate bill had not included language that satisfied their concerns, but they could not address abortion in the reconciliation bill as it would be non-budgetary. Instead, Obama issued Executive Order 13535, reaffirming the principles in the Hyde Amendment.
This won the support of Stupak and members of his group and assured the bill's passage. The House passed the Senate bill with a 219–212 vote on March 21, 2010, with 34 Democrats and all 178 Republicans voting against it. It passed the second bill, by 220–211, the same day (with the Senate passing this bill via reconciliation by 56-43 a few days later).
The day after the passage of ACA, March 22, Republicans introduced legislation to repeal it Obama signed ACA into law on March 23, 2010.
Click on any of the following blue hyperlinks for more about the Affordable Care Act:
Main article: Cost sharing reductions subsidy
As written, ACA mandated that insurers reduce copayments and deductibles for ACA exchange enrollees earning less than 250% of the FPL. Medicaid recipients were not eligible for the reductions.
So-called cost-sharing reduction (CSR) subsidies were to be paid to insurance companies to fund the reductions. During 2017, approximately $7 billion in CSR subsidies were to be paid, versus $34 billion for premium tax credits.
The latter was defined as mandatory spending that does not require an annual Congressional appropriation. CSR payments were not explicitly defined as mandatory. This led to litigation and disruption later.
Risk management:
ACA implemented multiple approaches to helping mitigate the disruptions to insurers that came with its many changes.
Risk corridors:
The risk-corridor program was a temporary risk management device. It was intended to encourage reluctant insurers into ACA insurance market from 2014 to 2016. For those years the Department of Health and Human Services (DHHS) would cover some of the losses for insurers whose plans performed worse than they expected.
Loss-making insurers would receive payments paid for in part by profit-making insurers. Similar risk corridors had been established for the Medicare prescription drug benefit.
While many insurers initially offered exchange plans, the program did not pay for itself as planned, losing up to $8.3 billion for 2014 and 2015. Authorization had to be given so DHHS could pay insurers from "general government revenues". However, the Consolidated Appropriations Act, 2014 (H.R. 3547) stated that no funds "could be used for risk-corridor payments". leaving the government in a potential breach of contract with insurers who offered qualified health plans.
Several insurers sued the government at the United States Court of Federal Claims to recover the funds believed owed to them under the Risk Corridors program. While several were summarily closed, in the case of Moda Health v the United States, Moda Health won a $214-million judgment in February 2017.
Federal Claims judge Thomas C. Wheeler stated, "the Government made a promise in the risk corridors program that it has yet to fulfill. Today, the court directs the Government to fulfill that promise. After all, to say to [Moda], 'The joke is on you. You shouldn't have trusted us,' is hardly worthy of our great government."
Moda Health's case was appealed by the government to the United States Court of Appeals for the Federal Circuit along with the appeals of the other insurers; here, the Federal Circuit reversed the Moda Health ruling and ruled across all the cases in favor of the government, that the appropriations riders ceded the government from paying out remain money due to the insurers.
The Supreme Court reversed this ruling in the consolidated case, Maine Community Health Options v. United States, reaffirming as with Judge Wheeler that the government had a responsibility to pay those funds under the ACA and the use of riders to de-obligate its from those payments was illegal.
Reinsurance:
The temporary reinsurance program is meant to stabilize premiums by reducing the incentive for insurers to raise premiums due to concerns about higher-risk enrollees. Reinsurance was based on retrospective costs rather than prospective risk evaluations. Reinsurance was available from 2014 through 2016.
Risk adjustment:
Risk adjustment involves transferring funds from plans with lower-risk enrollees to plans with higher-risk enrollees. It was intended to encourage insurers to compete based on value and efficiency rather than by attracting healthier enrollees. Of the three risk management programs, only risk adjustment was permanent. Plans with low actuarial risk compensate plans with high actuarial risk.
Medicaid expansion:
Main article: Medicaid coverage gap
ACA revised and expanded Medicaid eligibility starting in 2014. All U.S. citizens and legal residents with income up to 133% of the poverty line, including adults without dependent children, would qualify for coverage in any state that participated in the Medicaid program.
The federal government was to pay 100% of the increased cost in 2014, 2015 and 2016; 95% in 2017, 94% in 2018, 93% in 2019, and 90% in 2020 and all subsequent years.
A 5% "income disregard" made the effective income eligibility limit for Medicaid 138% of the poverty level. However, the Supreme Court ruled in NFIB v. Sebelius that this provision of ACA was coercive, and that states could choose to continue at pre-ACA eligibility levels.
Medicare savings:
Medicare reimbursements were reduced to insurers and drug companies for private Medicare Advantage policies that the Government Accountability Office and Medicare Payment Advisory Commission found to be excessively costly relative to standard Medicare; and to hospitals that failed standards of efficiency and care.
Taxes:
Medicare taxes:
Income from self-employment and wages of single individuals in excess of $200,000 annually are subjected to an additional tax of 0.9%. The threshold amount is $250,000 for a married couple filing jointly (threshold applies to their total compensation), or $125,000 for a married person filing separately.
In ACA's companion legislation, the Health Care and Education Reconciliation Act of 2010, an additional tax of 3.8% was applied to unearned income, specifically the lesser of net investment income and the amount by which adjusted gross income exceeds the above income limits.
Excise taxes:
ACA included an excise tax of 40% ("Cadillac tax") on total employer premium spending in excess of specified dollar amounts (initially $10,200 for single coverage and $27,500 for family coverage) indexed to inflation. This tax was originally scheduled to take effect in 2018, but was delayed until 2020 by the Consolidated Appropriations Act, 2016 and again to 2022.
Excise taxes totaling $3 billion were levied on importers and manufacturers of prescription drugs. An excise tax of 2.3% on medical devices and a 10% excise tax on indoor tanning services were applied as well. The tax was repealed in late 2019.
SCHIP:
The State Children's Health Insurance Program (CHIP) enrollment process was simplified.
Dependents:
Dependents were permitted to remain on their parents' insurance plan until their 26th birthday, including dependents who no longer lived with their parents, are not a dependent on a parent's tax return, are no longer a student, or are married.
Employer mandate:
Businesses that employ fifty or more people but do not offer health insurance to their full-time employees are assessed additional tax if the government has subsidized a full-time employee's healthcare through tax deductions or other means. This is commonly known as the employer mandate.
This provision was included to encourage employers to continue providing insurance once the exchanges began operating.
Delivery system reforms:
The act includes delivery system reforms intended to constrain costs and improve quality. These include Medicare payment changes to discourage hospital-acquired conditions and readmissions, bundled payment initiatives, the Center for Medicare and Medicaid Innovation, the Independent Payment Advisory Board, and accountable care organizations.
Hospital quality:
Health care cost/quality initiatives included incentives to reduce hospital infections, adopt electronic medical records, and to coordinate care and prioritize quality over quantity.
Bundled payments:
Medicare switched from fee-for-service to bundled payments. A single payment was to be paid to a hospital and a physician group for a defined episode of care (such as a hip replacement) rather than separate payments to individual service providers.
Accountable care organizations
Main article: Accountable care organization
The Medicare Shared Savings Program (MSSP) was established by section 3022 of the Affordable Care Act. It is the program by which an accountable care organization interacts with the federal government, and by which accountable care organizations can be created. It is a fee-for-service model.
The Act allowed the creation of accountable care organizations (ACOs), which are groups of doctors, hospitals and other providers that commit to give coordinated care to Medicare patients. ACOs were allowed to continue using fee-for-service billing.
They receive bonus payments from the government for minimizing costs while achieving quality benchmarks that emphasize prevention and mitigation of chronic disease. Missing cost or quality benchmarks subjected them to penalties.
Unlike health maintenance organizations, ACO patients are not required to obtain all care from the ACO. Also, unlike HMOs, ACOs must achieve quality-of-care goals.
Medicare drug benefit (Part D):
Medicare Part D participants received a 50% discount on brand name drugs purchased after exhausting their initial coverage and before reaching the catastrophic-coverage threshold.
By 2020, the "doughnut hole" would be completely filled.
State waivers:
From 2017 onwards, states can apply for a "waiver for state innovation" which allows them to conduct experiments that meet certain criteria. To obtain a waiver, a state must pass legislation setting up an alternative health system that provides insurance at least as comprehensive and as affordable as ACA, covers at least as many residents and does not increase the federal deficit.
These states can escape some of ACA's central requirements, including the individual and employer mandates and the provision of an insurance exchange. The state would receive compensation equal to the aggregate amount of any federal subsidies and tax credits for which its residents and employers would have been eligible under ACA, if they cannot be paid under the state plan.
Other insurance provisions:
The Community Living Assistance Services and Supports Act (or CLASS Act) established a voluntary and public long-term care insurance option for employees, The program was abolished as impractical without ever having taken effect.
Consumer Operated and Oriented Plans (CO-OP):
Member-governed non-profit insurers, could start providing health care coverage, based on a 5-year federal loan. As of 2017, only four of the original 23 co-ops were still in operation.
Nutrition labeling requirements:
Nutrition labeling requirements officially took effect in 2010, but implementation was delayed, and they actually took effect on May 7, 2018.
Legislative history:
Main articles:
ACA followed a long series of unsuccessful attempts by one party or the other to pass major insurance reforms. Innovations were limited to health savings accounts (2003), medical savings accounts (1996) or flexible spending accounts, which increased insurance options, but did not materially expand coverage.
Health care was a major factor in multiple elections, but until 2009, neither party had the votes to overcome the other's opposition.
Individual mandate:
The concept of an individual mandate goes back to at least 1989, when The Heritage Foundation, a conservative think-tank, proposed an individual mandate as an alternative to single-payer health care.
It was championed for a time by conservative economists and Republican senators as a market-based approach to healthcare reform on the basis of individual responsibility and avoidance of free rider problems. Specifically, because the 1986 Emergency Medical Treatment and Active Labor Act (EMTALA) requires any hospital participating in Medicare (nearly all do) to provide emergency care to anyone who needs it, the government often indirectly bore the cost of those without the ability to pay.
President Bill Clinton proposed a major healthcare reform bill in 1993 that ultimately failed. Clinton negotiated a compromise with the 105th Congress to instead enact the State Children's Health Insurance Program (SCHIP) in 1997.
The failed Clinton plan included a mandate for employers to provide health insurance to all employees through a regulated marketplace of health maintenance organizations. Republican senators proposed an alternative that would have required individuals, but not employers, to buy insurance.
The 1993 Republican Health Equity and Access Reform Today (HEART) Act, contained a "universal coverage" requirement with a penalty for noncompliance—an individual mandate—as well as subsidies to be used in state-based 'purchasing groups'.
Advocates included prominent Republican senators such as John Chafee, Orrin Hatch, Chuck Grassley, Bob Bennett and Kit Bond.
The 1994 Republican Consumer Choice Health Security Act, initially contained an individual mandate with a penalty provision; however, author Don Nickles subsequently removed the mandate, stating, "government should not compel people to buy health insurance".
At the time of these proposals, Republicans did not raise constitutional issues; Mark Pauly, who helped develop a proposal that included an individual mandate for George H. W. Bush, remarked, "I don't remember that being raised at all. The way it was viewed by the Congressional Budget Office in 1994 was, effectively, as a tax."
In 2006, an insurance expansion bill was enacted at the state level in Massachusetts. The bill contained both an individual mandate and an insurance exchange. Republican Governor Mitt Romney vetoed the mandate, but after Democrats overrode his veto, he signed it into law.
Romney's implementation of the 'Health Connector' exchange and individual mandate in Massachusetts was at first lauded by Republicans. During Romney's 2008 presidential campaign, Senator Jim DeMint praised Romney's ability to "take some good conservative ideas, like private health insurance, and apply them to the need to have everyone insured".
Romney said of the individual mandate: "I'm proud of what we've done. If Massachusetts succeeds in implementing it, then that will be the model for the nation."
In 2007 Republican Senator Bob Bennett and Democratic Senator Ron Wyden introduced the Healthy Americans Act, which featured an individual mandate and state-based, regulated insurance markets called "State Health Help Agencies". The bill attracted bipartisan support, but died in committee. Many of its sponsors and co-sponsors remained in Congress during the 2008 healthcare debate.
By 2008 many Democrats were considering this approach as the basis for healthcare reform. Experts said the legislation that eventually emerged from Congress in 2009 and 2010 bore similarities to the 2007 bill and that it took ideas from the Massachusetts reforms.
Academic foundation:
A driving force behind Obama's healthcare reform was Peter Orszag, Director of the Office of Management and Budget. Obama called Orszag his "healthcare czar" because of his knowledge of healthcare reform.
Orszag had previously been director of the Congressional Budget Office, and under his leadership the agency had focused on using cost analysis to create an affordable and effective approach to health care reform. Orszag claimed that healthcare reform became Obama's top agenda item because he wanted it to be his legacy.
According to an article by Ryan Lizza in The New Yorker, the core of "the Obama budget is Orszag's belief [in]...a government empowered with research on the most effective medical treatments". Obama bet "his presidency on Orszag's thesis of comparative effectiveness."
Orszag's policies were influenced by an article in The Annals of Internal Medicine co-authored by Elliott S. Fisher, David Wennberg and others. The article presented strong evidence based on the co-authors' research that numerous procedures, therapies and tests were being delivered with scant evidence of their medical value.
If those procedures and tests could be eliminated, this evidence suggested, medical costs might provide the savings to give healthcare to the uninsured population. After reading a The New Yorker article that used the "Dartmouth findings" to compare two counties in Texas with enormous variations in Medicare costs using hard data, Obama directed that his entire staff read it. More than anything else, the Dartmouth data intrigued Obama: Since it gave him an academic rationale for reshaping medicine.
The concept of comparing the effectiveness of healthcare options based on hard data ("comparative effectiveness" and "evidence-based medicine") was pioneered by John E. Wennberg, founder of The Dartmouth Institute, co-founder of The Foundation for Informed Medical Decision Making and senior advisor to Health Dialog Inc., a venture that he and his researchers created to help insurers implement the Dartmouth findings.
Healthcare debate, 2008–10
See also: Health care reforms proposed during the Obama administration
Healthcare reform was a major topic during the 2008 Democratic presidential primaries.
As the race narrowed, attention focused on the plans presented by the two leading candidates, Hillary Clinton and the eventual nominee, Barack Obama. Each candidate proposed a plan to cover the approximately 45 million Americans estimated to not have health insurance at some point each year.
Clinton's proposal would have required all Americans to obtain coverage (in effect, an individual mandate), while Obama's proposal provided a subsidy without a mandate.
During the general election, Obama said fixing healthcare would be one of his top four priorities as president. Obama and his opponent, Senator John McCain, both proposed health insurance reforms, though their plans differed.
McCain proposed tax credits for health insurance purchased in the individual market, which was estimated to reduce the number of uninsured people by about 2 million by 2018. Obama proposed private and public group insurance, income-based subsidies, consumer protections, and expansions of Medicaid and SCHIP, which was estimated at the time to reduce the number of uninsured people by 33.9 million by 2018 at a higher cost.
Obama announced to a joint session of Congress in February 2009 his intent to work with Congress to construct a plan for healthcare reform. By July, a series of bills were approved by committees within the House of Representatives.
On the Senate side, from June to September, the Senate Finance Committee held a series of 31 meetings to develop a proposal. This group—in particular, Democrats Max Baucus, Jeff Bingaman and Kent Conrad, along with Republicans Mike Enzi, Chuck Grassley and Olympia Snowe—met for more than 60 hours, and the principles they discussed, in conjunction with the other committees, became the foundation of a Senate bill.
Congressional Democrats and health policy experts, such as MIT economics professor Jonathan Gruber and David Cutler, argued that guaranteed issue would require both community rating and an individual mandate to ensure that adverse selection and/or "free riding" would not result in an insurance "death spiral".
They chose this approach after concluding that filibuster-proof support in the Senate was not present for more progressive plans such as single-payer. By deliberately drawing on bipartisan ideas—the same basic outline was supported by former Senate Majority Leaders Howard Baker, Bob Dole, Tom Daschle and George J. Mitchell—the bill's drafters hoped to garner the necessary votes.
However, following the incorporation of an individual mandate into the proposal, Republicans threatened to filibuster any bill that contained it. Senate Minority Leader Mitch McConnell, who led the Republican response, concluded Republicans should not support the bill.
Republican senators, including those who had supported earlier proposals with a similar mandate, began to describe the mandate as "unconstitutional". Journalist Ezra Klein wrote in The New Yorker, "a policy that once enjoyed broad support within the Republican Party suddenly faced unified opposition."
The reform attracted attention from lobbyists, including deals between lobby groups and the advocates to win the support of groups who had opposed past proposals
During the August 2009 summer congressional recess, many members went back to their districts and held town hall meetings on the proposals.
The nascent Tea Party movement organized protests and many conservative groups and individuals attended the meetings to oppose the proposed reforms. Threats were made against members of Congress over the course of the debate.
In September 2009 Obama delivered another speech to a joint session of Congress supporting the negotiations. On November 7, the House of Representatives passed the Affordable Health Care for America Act on a 220–215 vote and forwarded it to the Senate for passage.
Senate:
The Senate began work on its own proposals while the House was still working. The United States Constitution requires all revenue-related bills to originate in the House. To formally comply with this requirement, the Senate repurposed H.R. 3590, a bill regarding housing tax changes for service members. It had been passed by the House as a revenue-related modification to the Internal Revenue Code.
The bill became the Senate's vehicle for its healthcare reform proposal, discarding the bill's original content. The bill ultimately incorporated elements of proposals that were reported favorably by the Senate Health and Finance committees. With the Republican Senate minority vowing to filibuster, 60 votes would be necessary to pass the Senate.
At the start of the 111th Congress, Democrats had 58 votes. The Minnesota Senate election was ultimately won by Democrat Al Franken, making 59. Arlen Specter switched to the Democratic party in April 2009, giving them 60 seats, enough to end a filibuster.
Negotiations were undertaken attempting to satisfy moderate Democrats and to bring Republican senators aboard; particular attention was given to Republicans Bennett, Enzi, Grassley and Snowe.
After the Finance Committee vote on October 15, negotiations turned to moderate Democrats. Senate Majority Leader Harry Reid focused on satisfying centrists. The holdouts came down to Joe Lieberman of Connecticut, an independent who caucused with Democrats, and conservative Nebraska Democrat Ben Nelson.
Lieberman's demand that the bill not include a public option was met, although supporters won various concessions, including allowing state-based public options such as Vermont's failed Green Mountain Care.
The White House and Reid addressed Nelson's concerns during a 13-hour negotiation with two concessions: a compromise on abortion, modifying the language of the bill "to give states the right to prohibit coverage of abortion within their own insurance exchanges", which would require consumers to pay for the procedure out of pocket if the state so decided; and an amendment to offer a higher rate of Medicaid reimbursement for Nebraska. The latter half of the compromise was derisively termed the "Cornhusker Kickback" and was later removed.
On December 23, the Senate voted 60–39 to end debate on the bill: a cloture vote to end the filibuster. The bill then passed, also 60–39, on December 24, 2009, with all Democrats and two independents voting for it, and all Republicans against (except Jim Bunning, who did not vote). The bill was endorsed by the American Medical Association and AARP.
On January 19, 2010, Massachusetts Republican Scott Brown was elected to the Senate in a special election to replace the recently deceased Ted Kennedy, having campaigned on giving the Republican minority the 41st vote needed to sustain Republican filibusters.
Additionally, the symbolic importance of losing Kennedy's traditionally Democratic Massachusetts seat made many Congressional Democrats concerned about the political cost of the bill.
House:
With Democrats no longer able to get the 60 votes to break a filibuster in the Senate, White House Chief of Staff Rahm Emanuel argued that Democrats should scale back to a less ambitious bill, but House Speaker Nancy Pelosi pushed back, dismissing more moderate reform as "Kiddie Care".
Obama remained insistent on comprehensive reform. The news that Anthem in California intended to raise premium rates for its patients by as much as 39% gave him new evidence of the need for reform. On February 22, he laid out a "Senate-leaning" proposal to consolidate the bills. He held a meeting with both parties' leaders on February 25. The Democrats decided the House would pass the Senate's bill, to avoid another Senate vote.
House Democrats had expected to be able to negotiate changes in a House–Senate conference before passing a final bill. Since any bill that emerged from conference that differed from the Senate bill would have to pass the Senate over another Republican filibuster, most House Democrats agreed to pass the Senate bill on condition that it be amended by a subsequent bill.
They drafted the Health Care and Education Reconciliation Act, which could be passed by the reconciliation process.
Per the Congressional Budget Act of 1974, reconciliation cannot be subject to a filibuster. But reconciliation is limited to budget changes, which is why the procedure was not used to pass ACA in the first place; the bill had inherently non-budgetary regulations.
Although the already-passed Senate bill could not have been passed by reconciliation, most of House Democrats' demands were budgetary: "these changes—higher subsidy levels, different kinds of taxes to pay for them, nixing the Nebraska Medicaid deal—mainly involve taxes and spending. In other words, they're exactly the kinds of policies that are well-suited for reconciliation."
The remaining obstacle was a pivotal group of pro-life Democrats led by Bart Stupak who were initially reluctant to support the bill. The group found the possibility of federal funding for abortion significant enough to warrant opposition.
The Senate bill had not included language that satisfied their concerns, but they could not address abortion in the reconciliation bill as it would be non-budgetary. Instead, Obama issued Executive Order 13535, reaffirming the principles in the Hyde Amendment.
This won the support of Stupak and members of his group and assured the bill's passage. The House passed the Senate bill with a 219–212 vote on March 21, 2010, with 34 Democrats and all 178 Republicans voting against it. It passed the second bill, by 220–211, the same day (with the Senate passing this bill via reconciliation by 56-43 a few days later).
The day after the passage of ACA, March 22, Republicans introduced legislation to repeal it Obama signed ACA into law on March 23, 2010.
Click on any of the following blue hyperlinks for more about the Affordable Care Act:
- Impact
- Public opinion
- Political aspect
- Implementation
- In popular culture
- See also:
- Broccoli mandate
- Comparison of the healthcare systems in Canada and the United States
- Individual shared responsibility provision
- Massachusetts health care reform (sometimes called "Romneycare")
- Medicaid
- Medicare Access and CHIP Reauthorization Act of 2015 (Reform to the American Health Care system signed into law by President Obama)
- Single-payer health care
- Universal health care
- Universal health coverage by country
- U.S. health care compared with eight other countries (tabular form)
- ACA text
- Patient Protection and Affordable Care Act (PDF/details) as amended in the GPO Statute Compilations collection
- Full text, summary, background, provisions and more, via Democratic Policy Committee (Senate.gov)
END OF "Affordable Care Act" TOPIC
Healthcare Professional
- YouTube Video: Life as an allied health professional.
- YouTube Video: Health Features for Healthcare Professional Creators: What they are & How to apply
- YouTube Video: Allied Health Professionals - A Universe of Opportunities for your AHP career
See also: List of healthcare occupations
A health professional, healthcare professional, or healthcare worker (sometimes abbreviated HCW) is a provider of health care treatment and advice based on formal training and experience.
The field includes those who work as the following:
Experts in public health and community health are also health professionals.
Fields:
The healthcare workforce comprises a wide variety of professions and occupations who provide some type of healthcare service, including such direct care practitioners as:
They often work in hospitals, healthcare centers and other service delivery points, but also in academic training, research, and administration. Some provide care and treatment services for patients in private homes.
Many countries have a large number of community health workers who work outside formal healthcare institutions. Managers of healthcare services, health information technicians, and other assistive personnel and support workers are also considered a vital part of health care teams.
Healthcare practitioners are commonly grouped into health professions. Within each field of expertise, practitioners are often classified according to skill level and skill specialization.
"Health professionals" are highly skilled workers, in professions that usually require extensive knowledge including university-level study leading to the award of a first degree or higher qualification. This category includes:
Allied health professionals, also referred to as "health associate professionals" in the International Standard Classification of Occupations, support implementation of health care, treatment and referral plans usually established by medical, nursing, respiratory care, and other health professionals, and usually require formal qualifications to practice their profession.
In addition, unlicensed assistive personnel assist with providing health care services as permitted.
Another way to categorize healthcare practitioners is according to the sub-field in which they practice, such as mental health care, pregnancy and childbirth care, surgical care, rehabilitation care, or public health.
Mental health:
Main article: Mental health professional
A mental health professional is a health worker who offers services to improve the mental health of individuals or treat mental illness. These include:
These health care providers often deal with the same illnesses, disorders, conditions, and issues; however, their scope of practice often differs. The most significant difference across categories of mental health practitioners is education and training.
There are many damaging effects to the health care workers. Many have had diverse negative psychological symptoms ranging from emotional trauma to very severe anxiety. Health care workers have not been treated right and because of that their mental, physical, and emotional health has been affected by it.
The SAGE author's said that there were 94% of nurses that had experienced at least one PTSD after the traumatic experience. Others have experienced nightmares, flashbacks, and short and long term emotional reactions.
The abuse is causing detrimental effects on these health care workers. Violence is causing health care workers to have a negative attitude toward work tasks and patients, and because of that they are "feeling pressured to accept the order, dispense a product, or administer a medication".
Sometimes it can range from verbal to sexual to physical harassment, whether the abuser is a patient, patient's families, physician, supervisors, or nurses.
Obstetrics:
Main articles:
A maternal and newborn health practitioner is a health care expert who deals with the care of women and their children before, during and after pregnancy and childbirth. Such health practitioners include obstetricians, physician assistants, midwives, obstetrical nurses and many others.
One of the main differences between these professions is in the training and authority to provide surgical services and other life-saving interventions.
In some developing countries, traditional birth attendants, or traditional midwives, are the primary source of pregnancy and childbirth care for many women and families, although they are not certified or licensed.
Geriatrics:
Main articles: Geriatrics and Geriatric care management
A geriatric care practitioner plans and coordinates the care of the elderly and/or disabled to promote their health, improve their quality of life, and maintain their independence for as long as possible. They include:
Surgery:
A surgical practitioner is a healthcare professional and expert who specializes in the planning and delivery of a patient's perioperative care, including during the anaesthetic, surgical and recovery stages. They may include:
Rehabilitation:
A rehabilitation care practitioner is a health worker who provides care and treatment which aims to enhance and restore functional ability and quality of life to those with physical impairments or disabilities. These include:
Optometry:
Main article: Optometry
Optometry is a field traditionally associated with the correction of refractive errors using glasses or contact lenses, and treating eye diseases. Optometrists also provide general eye care, including screening exams for glaucoma and diabetic retinopathy and management of routine or eye conditions.
Optometrists may also undergo further training in order to specialize in various fields, including glaucoma, medical retina, low vision, or paediatrics.
In some countries, such as the United Kingdom, United States, and Canada, Optometrists may also undergo further training in order to be able to perform some surgical procedures.
Diagnostics:
Main article: Medical diagnosis
Medical diagnosis providers are health workers responsible for the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as diagnosis with the medical context being implicit. This usually involves a team of healthcare providers in various diagnostic units. These include:
Dentistry:
Main article: Dentistry
A dental care practitioner is a health worker and expert who provides care and treatment to promote and restore oral health. These include:
Podiatry:
Care and treatment for the foot, ankle, and lower leg may be delivered by podiatrists, chiropodists, pedorthists, foot health practitioners, podiatric medical assistants, podiatric nurse and others.
Public health:
A public health practitioner focuses on improving health among individuals, families and communities through the prevention and treatment of diseases and injuries, surveillance of cases, and promotion of healthy behaviors.
This category includes:
Alternative medicine:
In many societies, practitioners of alternative medicine have contact with a significant number of people, either as integrated within or remaining outside the formal health care system.
These include:
In some countries such as Canada, chiropractors and osteopaths (not to be confused with doctors of osteopathic medicine in the United States) are considered alternative medicine practitioners.
Occupational hazards:
See also: Occupational hazards in dentistry and Nursing § Occupational hazards
The healthcare workforce faces unique health and safety challenges and is recognized by the National Institute for Occupational Safety and Health (NIOSH) as a priority industry sector in the National Occupational Research Agenda (NORA) to identify and provide intervention strategies regarding occupational health and safety issues.
Biological hazards:
Exposure to respiratory infectious diseases like tuberculosis (caused by Mycobacterium tuberculosis) and influenza can be reduced with the use of respirators; this exposure is a significant occupational hazard for health care professionals. Healthcare workers are also at risk for diseases that are contracted through extended contact with a patient, including scabies.
Health professionals are also at risk for contracting blood-borne diseases like hepatitis B, hepatitis C, and HIV/AIDS through needlestick injuries or contact with bodily fluids. This risk can be mitigated with vaccination when there is a vaccine available, like with hepatitis B.
In epidemic situations, such as the 2014-2016 West African Ebola virus epidemic or the 2003 SARS outbreak, healthcare workers are at even greater risk, and were disproportionately affected in both the Ebola and SARS outbreaks.
In general, appropriate personal protective equipment (PPE) is the first-line mode of protection for healthcare workers from infectious diseases. For it to be effective against highly contagious diseases, personal protective equipment must be watertight and prevent the skin and mucous membranes from contacting infectious material.
Different levels of personal protective equipment created to unique standards are used in situations where the risk of infection is different.
Practices such as triple gloving and multiple respirators do not provide a higher level of protection and present a burden to the worker, who is additionally at increased risk of exposure when removing the PPE. Compliance with appropriate personal protective equipment rules may be difficult in certain situations, such as tropical environments or low-resource settings.
A 2020 Cochrane systematic review found low-quality evidence that using more breathable fabric in PPE, double gloving, and active training reduce the risk of contamination but that more randomized controlled trials are needed for how best to train healthcare workers in proper PPE use.
Tuberculosis screening, testing, and education:
Based on recommendations from The United States Center for Disease Control and Prevention (CDC) for TB screening and testing the following best practices should be followed when hiring and employing Health Care Personnel.
When hiring Health Care Personnel, the applicant should complete the following:
The CDC recommends either a blood test, also known as an interferon-gamma release assay (IGRA), or a skin test, also known as a Mantoux tuberculin skin test (TST). A TB blood test for baseline testing does not require two-step testing.
If the skin test method is used to test HCP upon hire, then two-step testing should be used. A one-step test is not recommended.
The CDC has outlined further specifics on recommended testing for several scenarios. In summary:
According to these recommended testing guidelines any two negative TST results within 12 months of each other constitute a two-step TST.
For annual screening, testing, and education, the only recurring requirement for all HCP is to receive TB education annually. While the CDC offers education materials, there is not a well defined requirement as to what constitutes a satisfactory annual education.
Annual TB testing is no longer recommended unless there is a known exposure or ongoing transmission at a healthcare facility. Should an HCP be considered at increased occupational risk for TB annual screening may be considered.
For HCP with a documented history of a positive TB test result do not need to be re-tested but should instead complete a TB symptom evaluation. It is assumed that any HCP who has undergone a chest x-ray test has had a previous positive test result. When considering mental health you may see your doctor to be evaluated at your digression. It is recommended to see someone at least once a year in order to make sure that there hasn't been any sudden changes.
Pyschosocial hazards:
Occupational stress and occupational burnout are highly prevalent among health professionals.
Some studies suggest that workplace stress is pervasive in the health care industry because of the following:
Other stressors include the emotional labor of caring for ill people and high patient loads.
The consequences of this stress can include substance abuse, suicide, major depressive disorder, and anxiety, all of which occur at higher rates in health professionals than the general working population.
Elevated levels of stress are also linked to high rates of burnout, absenteeism and diagnostic errors, and reduced rates of patient satisfaction.
In Canada, a national report (Canada's Health Care Providers) also indicated higher rates of absenteeism due to illness or disability among health care workers compared to the rest of the working population, although those working in health care reported similar levels of good health and fewer reports of being injured at work.
There is some evidence that cognitive-behavioral therapy, relaxation training and therapy (including meditation and massage), and modifying schedules can reduce stress and burnout among multiple sectors of health care providers. Research is ongoing in this area, especially with regards to physicians, whose occupational stress and burnout is less researched compared to other health professions.
Healthcare workers are at higher risk of on-the-job injury due to violence. Drunk, confused, and hostile patients and visitors are a continual threat to providers attempting to treat patients.
Frequently, assault and violence in a healthcare setting goes unreported and is wrongly assumed to be part of the job. Violent incidents typically occur during one-on-one care; being alone with patients increases healthcare workers' risk of assault.
In the United States, healthcare workers experience 2⁄3 of nonfatal workplace violence incidents. Psychiatric units represent the highest proportion of violent incidents, at 40%; they are followed by geriatric units (20%) and the emergency department (10%).
Workplace violence can also cause psychological trauma.
Health care professionals are also likely to experience sleep deprivation due to their jobs. Many health care professionals are on a shift work schedule, and therefore experience misalignment of their work schedule and their circadian rhythm.
In 2007, 32% of healthcare workers were found to get fewer than 6 hours of sleep a night. Sleep deprivation also predisposes healthcare professionals to make mistakes that may potentially endanger a patient.
COVID pandemic:
Especially in times like the present (2020), the hazards of health professional stem into the mental health. Research from the last few months highlights that COVID-19 has contributed greatly to the degradation of mental health in healthcare providers. This includes, but is not limited to, anxiety, depression/burnout, and insomnia.
A study done by Di Mattei et al. (2020) revealed that 12.63% of COVID nurses and 16.28% of other COVID healthcare workers reported extremely severe anxiety symptoms at the peak of the pandemic.
In addition, another study was conducted on 1,448 full time employees in Japan. The participants were surveyed at baseline in March 2020 and then again in May 2020. The result of the study showed that psychological distress and anxiety had increased more among healthcare workers during the COVID-19 outbreak.
Similarly, studies have also shown that following the pandemic, at least one in five healthcare professionals report symptoms of anxiety. Specifically, the aspect of "anxiety was assessed in 12 studies, with a pooled prevalence of 23.2%" following COVID. When considering all 1,448 participants that percentage makes up about 335 people.
Abuse by patients:
Physical and chemical hazards:
Slips, trips, and falls are the second-most common cause of worker's compensation claims in the US and cause 21% of work absences due to injury. These injuries most commonly result in strains and sprains; women, those older than 45, and those who have been working less than a year in a healthcare setting are at the highest risk.
An epidemiological study published in 2018 examined the hearing status of noise-exposed health care and social assistance (HSA) workers sector to estimate and compare the prevalence of hearing loss by subsector within the sector.
Most of the HSA subsector prevalence estimates ranged from 14% to 18%, but the Medical and Diagnostic Laboratories subsector had 31% prevalence and the Offices of All Other Miscellaneous Health Practitioners had a 24% prevalence. The Child Day Care Services subsector also had a 52% higher risk than the reference industry.
Exposure to hazardous drugs, including those for chemotherapy, is another potential occupational risk. These drugs can cause cancer and other health conditions.
Gender factors:
Female health care workers may face specific types of workplace-related health conditions and stress.
According to the World Health Organization, women predominate in the formal health workforce in many countries and are prone to musculoskeletal injury (caused by physically demanding job tasks such as lifting and moving patients) and burnout.
Female health workers are exposed to hazardous drugs and chemicals in the workplace which may cause adverse reproductive outcomes such as spontaneous abortion and congenital malformations.
In some contexts, female health workers are also subject to gender-based violence from coworkers and patients.
Workforce shortages:
See also:
Many jurisdictions report shortfalls in the number of trained health human resources to meet population health needs and/or service delivery targets, especially in medically underserved areas.
For example, in the United States, the 2010 federal budget invested $330 million to increase the number of physicians, physician assistants, nurse practitioners, nurses, and dentists practicing in areas of the country experiencing shortages of trained health professionals.
The Budget expands loan repayment programs for physicians, nurses, and dentists who agree to practice in medically underserved areas. This funding will enhance the capacity of nursing schools to increase the number of nurses. It will also allow states to increase access to oral health care through dental workforce development grants.
The Budget's new resources will sustain the expansion of the health care workforce funded in the Recovery Act. There were 15.7 million health care professionals in the US as of 2011.
In Canada, the 2011 federal budget announced a Canada Student Loan forgiveness program to encourage and support new family physicians, physician assistants, nurse practitioners and nurses to practice in underserved rural or remote communities of the country, including communities that provide health services to First Nations and Inuit populations.
In Uganda, the Ministry of Health reports that as many as 50% of staffing positions for health workers in rural and underserved areas remain vacant. As of early 2011, the Ministry was conducting research and costing analyses to determine the most appropriate attraction and retention packages for medical officers, nursing officers, pharmacists, and laboratory technicians in the country's rural areas.
At the international level, the World Health Organization estimates a shortage of almost 4.3 million doctors, midwives, nurses, and support workers worldwide to meet target coverage levels of essential primary health care interventions. The shortage is reported most severe in 57 of the poorest countries, especially in sub-Saharan Africa.
Nurses are the most common type of medical field worker to face shortages around the world. There are numerous reasons that the nursing shortage occurs globally. Some include: inadequate pay, a large percentage of working nurses are over the age of 45 and are nearing retirement age, burnout, and lack of recognition.
Incentive programs have been put in place to aid in the deficit of pharmacists and pharmacy students. The reason for the shortage of pharmacy students is unknown but one can infer that it is due to the level of difficulty in the program.
Results of nursing staff shortages can cause unsafe staffing levels that lead to poor patient care. Five or more incidents that occur per day in a hospital setting as a result of nurses who do not receive adequate rest or meal breaks is a common issue.
Regulation and registration:
Main article: Health professional requisites
Practicing without a license that is valid and current is typically illegal. In most jurisdictions, the provision of health care services is regulated by the government. Individuals found to be providing medical, nursing or other professional services without the appropriate certification or license may face sanctions and criminal charges leading to a prison term.
The number of professions subject to regulation, requisites for individuals to receive professional licensure, and nature of sanctions that can be imposed for failure to comply vary across jurisdictions.
In the United States, under Michigan state laws, an individual is guilty of a felony if identified as practicing in the health profession without a valid personal license or registration.
Health professionals can also be imprisoned if found guilty of practicing beyond the limits allowed by their licenses and registration. The state laws define the scope of practice for medicine, nursing, and a number of allied health professions.
In Florida, practicing medicine without the appropriate license is a crime classified as a third degree felony, which may give imprisonment up to five years. Practicing a health care profession without a license which results in serious bodily injury classifies as a second degree felony, providing up to 15 years' imprisonment.
In the United Kingdom, healthcare professionals are regulated by the state; the UK Health and Care Professions Council (HCPC) protects the 'title' of each profession it regulates. For example, it is illegal for someone to call himself an Occupational Therapist or Radiographer if they are not on the register held by the HCPC.
See also:
A health professional, healthcare professional, or healthcare worker (sometimes abbreviated HCW) is a provider of health care treatment and advice based on formal training and experience.
The field includes those who work as the following:
- nurse,
- physician
- (such as family physician,
- internist,
- obstetrician,
- psychiatrist,
- radiologist,
- surgeon etc.),
- (such as family physician,
- physician assistant,
- registered dietitian,
- veterinarian,
- veterinary technician,
- optometrist,
- pharmacist,
- pharmacy technician,
- medical assistant,
- physical therapist,
- occupational therapist,
- dentist,
- midwife,
- psychologist,
- or who perform services in allied health professions.
Experts in public health and community health are also health professionals.
Fields:
The healthcare workforce comprises a wide variety of professions and occupations who provide some type of healthcare service, including such direct care practitioners as:
- physicians,
- nurse practitioners,
- physician assistants,
- nurses,
- respiratory therapists,
- dentists,
- pharmacists,
- speech-language pathologist,
- physical therapists,
- occupational therapists,
- physical and behavior therapists,
- as well as allied health professionals such as
They often work in hospitals, healthcare centers and other service delivery points, but also in academic training, research, and administration. Some provide care and treatment services for patients in private homes.
Many countries have a large number of community health workers who work outside formal healthcare institutions. Managers of healthcare services, health information technicians, and other assistive personnel and support workers are also considered a vital part of health care teams.
Healthcare practitioners are commonly grouped into health professions. Within each field of expertise, practitioners are often classified according to skill level and skill specialization.
"Health professionals" are highly skilled workers, in professions that usually require extensive knowledge including university-level study leading to the award of a first degree or higher qualification. This category includes:
- physicians,
- physician assistants,
- registered nurses,
- veterinarians,
- veterinary technicians,
- veterinary assistants,
- dentists,
- midwives,
- radiographers,
- pharmacists,
- physiotherapists,
- optometrists,
- operating department practitioners
- and others.
Allied health professionals, also referred to as "health associate professionals" in the International Standard Classification of Occupations, support implementation of health care, treatment and referral plans usually established by medical, nursing, respiratory care, and other health professionals, and usually require formal qualifications to practice their profession.
In addition, unlicensed assistive personnel assist with providing health care services as permitted.
Another way to categorize healthcare practitioners is according to the sub-field in which they practice, such as mental health care, pregnancy and childbirth care, surgical care, rehabilitation care, or public health.
Mental health:
Main article: Mental health professional
A mental health professional is a health worker who offers services to improve the mental health of individuals or treat mental illness. These include:
- psychiatrists,
- psychiatry physician assistants,
- clinical, counseling, and school psychologists,
- occupational therapists,
- clinical social workers,
- psychiatric-mental health nurse practitioners,
- marriage and family therapists,
- mental health counselors,
- as well as other health professionals and allied health professions.
These health care providers often deal with the same illnesses, disorders, conditions, and issues; however, their scope of practice often differs. The most significant difference across categories of mental health practitioners is education and training.
There are many damaging effects to the health care workers. Many have had diverse negative psychological symptoms ranging from emotional trauma to very severe anxiety. Health care workers have not been treated right and because of that their mental, physical, and emotional health has been affected by it.
The SAGE author's said that there were 94% of nurses that had experienced at least one PTSD after the traumatic experience. Others have experienced nightmares, flashbacks, and short and long term emotional reactions.
The abuse is causing detrimental effects on these health care workers. Violence is causing health care workers to have a negative attitude toward work tasks and patients, and because of that they are "feeling pressured to accept the order, dispense a product, or administer a medication".
Sometimes it can range from verbal to sexual to physical harassment, whether the abuser is a patient, patient's families, physician, supervisors, or nurses.
Obstetrics:
Main articles:
A maternal and newborn health practitioner is a health care expert who deals with the care of women and their children before, during and after pregnancy and childbirth. Such health practitioners include obstetricians, physician assistants, midwives, obstetrical nurses and many others.
One of the main differences between these professions is in the training and authority to provide surgical services and other life-saving interventions.
In some developing countries, traditional birth attendants, or traditional midwives, are the primary source of pregnancy and childbirth care for many women and families, although they are not certified or licensed.
Geriatrics:
Main articles: Geriatrics and Geriatric care management
A geriatric care practitioner plans and coordinates the care of the elderly and/or disabled to promote their health, improve their quality of life, and maintain their independence for as long as possible. They include:
- geriatricians,
- occupational therapists,
- physician assistants,
- adult-gerontology nurse practitioners,
- clinical nurse specialists,
- geriatric clinical pharmacists,
- geriatric nurses,
- geriatric care managers,
- geriatric aides,
- nursing aides,
- caregivers
- and others who focus on the health and psychological care needs of older adults.
Surgery:
A surgical practitioner is a healthcare professional and expert who specializes in the planning and delivery of a patient's perioperative care, including during the anaesthetic, surgical and recovery stages. They may include:
- general and specialist surgeons,
- physician assistants,
- assistant surgeons,
- surgical assistants,
- veterinary surgeons,
- veterinary technicians.
- anesthesiologists,
- anesthesiologist assistants,
- nurse anesthetists,
- surgical nurses,
- clinical officers,
- operating department practitioners,
- anaesthetic technicians,
- perioperative nurses,
- surgical technologists,
- and others.
Rehabilitation:
A rehabilitation care practitioner is a health worker who provides care and treatment which aims to enhance and restore functional ability and quality of life to those with physical impairments or disabilities. These include:
- physiatrists,
- physician assistants,
- rehabilitation nurses,
- clinical nurse specialists,
- nurse practitioners,
- physiotherapists,
- chiropractors,
- orthotists,
- prosthetists,
- occupational therapists,
- recreational therapists,
- audiologists,
- speech and language pathologists,
- respiratory therapists,
- rehabilitation counsellors,
- physical rehabilitation therapists,
- athletic trainers,
- physiotherapy technicians,
- orthotic technicians,
- prosthetic technicians,
- personal care assistants,
- and others.
Optometry:
Main article: Optometry
Optometry is a field traditionally associated with the correction of refractive errors using glasses or contact lenses, and treating eye diseases. Optometrists also provide general eye care, including screening exams for glaucoma and diabetic retinopathy and management of routine or eye conditions.
Optometrists may also undergo further training in order to specialize in various fields, including glaucoma, medical retina, low vision, or paediatrics.
In some countries, such as the United Kingdom, United States, and Canada, Optometrists may also undergo further training in order to be able to perform some surgical procedures.
Diagnostics:
Main article: Medical diagnosis
Medical diagnosis providers are health workers responsible for the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as diagnosis with the medical context being implicit. This usually involves a team of healthcare providers in various diagnostic units. These include:
- radiographers,
- radiologists,
- Sonographers,
- medical laboratory scientists,
- pathologists,
- and related professionals.
Dentistry:
Main article: Dentistry
A dental care practitioner is a health worker and expert who provides care and treatment to promote and restore oral health. These include:
- dentists and dental surgeons,
- dental assistants,
- dental auxiliaries,
- dental hygienists,
- dental nurses,
- dental technicians,
- dental therapists or oral health therapists,
- and related professionals.
Podiatry:
Care and treatment for the foot, ankle, and lower leg may be delivered by podiatrists, chiropodists, pedorthists, foot health practitioners, podiatric medical assistants, podiatric nurse and others.
Public health:
A public health practitioner focuses on improving health among individuals, families and communities through the prevention and treatment of diseases and injuries, surveillance of cases, and promotion of healthy behaviors.
This category includes:
- community and preventive medicine specialists,
- physician assistants,
- public health nurses,
- pharmacist,
- clinical nurse specialists,
- dietitians,
- environmental health officers (public health inspectors),
- paramedics,
- epidemiologists,
- public health dentists,
- and others.
Alternative medicine:
In many societies, practitioners of alternative medicine have contact with a significant number of people, either as integrated within or remaining outside the formal health care system.
These include:
- practitioners in acupuncture,
- Ayurveda,
- herbalism,
- homeopathy,
- naturopathy,
- Reiki,
- Siddha medicine,
- traditional Chinese medicine,
- traditional Korean medicine,
- Unani,
- and Yoga.
In some countries such as Canada, chiropractors and osteopaths (not to be confused with doctors of osteopathic medicine in the United States) are considered alternative medicine practitioners.
Occupational hazards:
See also: Occupational hazards in dentistry and Nursing § Occupational hazards
The healthcare workforce faces unique health and safety challenges and is recognized by the National Institute for Occupational Safety and Health (NIOSH) as a priority industry sector in the National Occupational Research Agenda (NORA) to identify and provide intervention strategies regarding occupational health and safety issues.
Biological hazards:
Exposure to respiratory infectious diseases like tuberculosis (caused by Mycobacterium tuberculosis) and influenza can be reduced with the use of respirators; this exposure is a significant occupational hazard for health care professionals. Healthcare workers are also at risk for diseases that are contracted through extended contact with a patient, including scabies.
Health professionals are also at risk for contracting blood-borne diseases like hepatitis B, hepatitis C, and HIV/AIDS through needlestick injuries or contact with bodily fluids. This risk can be mitigated with vaccination when there is a vaccine available, like with hepatitis B.
In epidemic situations, such as the 2014-2016 West African Ebola virus epidemic or the 2003 SARS outbreak, healthcare workers are at even greater risk, and were disproportionately affected in both the Ebola and SARS outbreaks.
In general, appropriate personal protective equipment (PPE) is the first-line mode of protection for healthcare workers from infectious diseases. For it to be effective against highly contagious diseases, personal protective equipment must be watertight and prevent the skin and mucous membranes from contacting infectious material.
Different levels of personal protective equipment created to unique standards are used in situations where the risk of infection is different.
Practices such as triple gloving and multiple respirators do not provide a higher level of protection and present a burden to the worker, who is additionally at increased risk of exposure when removing the PPE. Compliance with appropriate personal protective equipment rules may be difficult in certain situations, such as tropical environments or low-resource settings.
A 2020 Cochrane systematic review found low-quality evidence that using more breathable fabric in PPE, double gloving, and active training reduce the risk of contamination but that more randomized controlled trials are needed for how best to train healthcare workers in proper PPE use.
Tuberculosis screening, testing, and education:
Based on recommendations from The United States Center for Disease Control and Prevention (CDC) for TB screening and testing the following best practices should be followed when hiring and employing Health Care Personnel.
When hiring Health Care Personnel, the applicant should complete the following:
- a TB risk assessment,
- a TB symptom evaluation for at least those listed on the Signs & Symptoms page,
- a TB test in accordance with the guidelines for Testing for TB Infection,
- and additional evaluation for TB disease as needed (e.g. chest x-ray for HCP with a positive TB test).
The CDC recommends either a blood test, also known as an interferon-gamma release assay (IGRA), or a skin test, also known as a Mantoux tuberculin skin test (TST). A TB blood test for baseline testing does not require two-step testing.
If the skin test method is used to test HCP upon hire, then two-step testing should be used. A one-step test is not recommended.
The CDC has outlined further specifics on recommended testing for several scenarios. In summary:
- Previous documented positive skin test (TST) then a further TST is not recommended
- Previous documented negative TST within 12 months before employment OR at least two documented negative TSTs ever then a single TST is recommended
- All other scenarios, with the exception of programs using blood tests, the recommended testing is a two-step TST
According to these recommended testing guidelines any two negative TST results within 12 months of each other constitute a two-step TST.
For annual screening, testing, and education, the only recurring requirement for all HCP is to receive TB education annually. While the CDC offers education materials, there is not a well defined requirement as to what constitutes a satisfactory annual education.
Annual TB testing is no longer recommended unless there is a known exposure or ongoing transmission at a healthcare facility. Should an HCP be considered at increased occupational risk for TB annual screening may be considered.
For HCP with a documented history of a positive TB test result do not need to be re-tested but should instead complete a TB symptom evaluation. It is assumed that any HCP who has undergone a chest x-ray test has had a previous positive test result. When considering mental health you may see your doctor to be evaluated at your digression. It is recommended to see someone at least once a year in order to make sure that there hasn't been any sudden changes.
Pyschosocial hazards:
Occupational stress and occupational burnout are highly prevalent among health professionals.
Some studies suggest that workplace stress is pervasive in the health care industry because of the following:
- inadequate staffing levels,
- long work hours,
- exposure to infectious diseases and hazardous substances leading to illness or death,
- and in some countries threat of malpractice litigation.
Other stressors include the emotional labor of caring for ill people and high patient loads.
The consequences of this stress can include substance abuse, suicide, major depressive disorder, and anxiety, all of which occur at higher rates in health professionals than the general working population.
Elevated levels of stress are also linked to high rates of burnout, absenteeism and diagnostic errors, and reduced rates of patient satisfaction.
In Canada, a national report (Canada's Health Care Providers) also indicated higher rates of absenteeism due to illness or disability among health care workers compared to the rest of the working population, although those working in health care reported similar levels of good health and fewer reports of being injured at work.
There is some evidence that cognitive-behavioral therapy, relaxation training and therapy (including meditation and massage), and modifying schedules can reduce stress and burnout among multiple sectors of health care providers. Research is ongoing in this area, especially with regards to physicians, whose occupational stress and burnout is less researched compared to other health professions.
Healthcare workers are at higher risk of on-the-job injury due to violence. Drunk, confused, and hostile patients and visitors are a continual threat to providers attempting to treat patients.
Frequently, assault and violence in a healthcare setting goes unreported and is wrongly assumed to be part of the job. Violent incidents typically occur during one-on-one care; being alone with patients increases healthcare workers' risk of assault.
In the United States, healthcare workers experience 2⁄3 of nonfatal workplace violence incidents. Psychiatric units represent the highest proportion of violent incidents, at 40%; they are followed by geriatric units (20%) and the emergency department (10%).
Workplace violence can also cause psychological trauma.
Health care professionals are also likely to experience sleep deprivation due to their jobs. Many health care professionals are on a shift work schedule, and therefore experience misalignment of their work schedule and their circadian rhythm.
In 2007, 32% of healthcare workers were found to get fewer than 6 hours of sleep a night. Sleep deprivation also predisposes healthcare professionals to make mistakes that may potentially endanger a patient.
COVID pandemic:
Especially in times like the present (2020), the hazards of health professional stem into the mental health. Research from the last few months highlights that COVID-19 has contributed greatly to the degradation of mental health in healthcare providers. This includes, but is not limited to, anxiety, depression/burnout, and insomnia.
A study done by Di Mattei et al. (2020) revealed that 12.63% of COVID nurses and 16.28% of other COVID healthcare workers reported extremely severe anxiety symptoms at the peak of the pandemic.
In addition, another study was conducted on 1,448 full time employees in Japan. The participants were surveyed at baseline in March 2020 and then again in May 2020. The result of the study showed that psychological distress and anxiety had increased more among healthcare workers during the COVID-19 outbreak.
Similarly, studies have also shown that following the pandemic, at least one in five healthcare professionals report symptoms of anxiety. Specifically, the aspect of "anxiety was assessed in 12 studies, with a pooled prevalence of 23.2%" following COVID. When considering all 1,448 participants that percentage makes up about 335 people.
Abuse by patients:
- The patients are selecting victims who are more vulnerable. For example, Cho said that these would be the nurses that are lacking experience or trying to get used to their new roles at work.
- Others authors that agree with this are Vento, Cainelli, & Vallone and they said that, the reason patients have caused danger to health care workers is because of insufficient communication between them, long waiting lines, and overcrowding in waiting areas. When patients are intrusive and/or violent toward the faculty, this makes the staff question what they should do about taking care of a patient.
- There have been many incidents from patients that have really caused some health care workers to be traumatized and have so much self doubt. Goldblatt and other authors said that there was a lady who was giving birth, her husband said, "Who is in charge around here"? "Who are these sluts you employ here". This was very avoidable to have been said to the people who are taking care of your wife and child.
Physical and chemical hazards:
Slips, trips, and falls are the second-most common cause of worker's compensation claims in the US and cause 21% of work absences due to injury. These injuries most commonly result in strains and sprains; women, those older than 45, and those who have been working less than a year in a healthcare setting are at the highest risk.
An epidemiological study published in 2018 examined the hearing status of noise-exposed health care and social assistance (HSA) workers sector to estimate and compare the prevalence of hearing loss by subsector within the sector.
Most of the HSA subsector prevalence estimates ranged from 14% to 18%, but the Medical and Diagnostic Laboratories subsector had 31% prevalence and the Offices of All Other Miscellaneous Health Practitioners had a 24% prevalence. The Child Day Care Services subsector also had a 52% higher risk than the reference industry.
Exposure to hazardous drugs, including those for chemotherapy, is another potential occupational risk. These drugs can cause cancer and other health conditions.
Gender factors:
Female health care workers may face specific types of workplace-related health conditions and stress.
According to the World Health Organization, women predominate in the formal health workforce in many countries and are prone to musculoskeletal injury (caused by physically demanding job tasks such as lifting and moving patients) and burnout.
Female health workers are exposed to hazardous drugs and chemicals in the workplace which may cause adverse reproductive outcomes such as spontaneous abortion and congenital malformations.
In some contexts, female health workers are also subject to gender-based violence from coworkers and patients.
Workforce shortages:
See also:
Many jurisdictions report shortfalls in the number of trained health human resources to meet population health needs and/or service delivery targets, especially in medically underserved areas.
For example, in the United States, the 2010 federal budget invested $330 million to increase the number of physicians, physician assistants, nurse practitioners, nurses, and dentists practicing in areas of the country experiencing shortages of trained health professionals.
The Budget expands loan repayment programs for physicians, nurses, and dentists who agree to practice in medically underserved areas. This funding will enhance the capacity of nursing schools to increase the number of nurses. It will also allow states to increase access to oral health care through dental workforce development grants.
The Budget's new resources will sustain the expansion of the health care workforce funded in the Recovery Act. There were 15.7 million health care professionals in the US as of 2011.
In Canada, the 2011 federal budget announced a Canada Student Loan forgiveness program to encourage and support new family physicians, physician assistants, nurse practitioners and nurses to practice in underserved rural or remote communities of the country, including communities that provide health services to First Nations and Inuit populations.
In Uganda, the Ministry of Health reports that as many as 50% of staffing positions for health workers in rural and underserved areas remain vacant. As of early 2011, the Ministry was conducting research and costing analyses to determine the most appropriate attraction and retention packages for medical officers, nursing officers, pharmacists, and laboratory technicians in the country's rural areas.
At the international level, the World Health Organization estimates a shortage of almost 4.3 million doctors, midwives, nurses, and support workers worldwide to meet target coverage levels of essential primary health care interventions. The shortage is reported most severe in 57 of the poorest countries, especially in sub-Saharan Africa.
Nurses are the most common type of medical field worker to face shortages around the world. There are numerous reasons that the nursing shortage occurs globally. Some include: inadequate pay, a large percentage of working nurses are over the age of 45 and are nearing retirement age, burnout, and lack of recognition.
Incentive programs have been put in place to aid in the deficit of pharmacists and pharmacy students. The reason for the shortage of pharmacy students is unknown but one can infer that it is due to the level of difficulty in the program.
Results of nursing staff shortages can cause unsafe staffing levels that lead to poor patient care. Five or more incidents that occur per day in a hospital setting as a result of nurses who do not receive adequate rest or meal breaks is a common issue.
Regulation and registration:
Main article: Health professional requisites
Practicing without a license that is valid and current is typically illegal. In most jurisdictions, the provision of health care services is regulated by the government. Individuals found to be providing medical, nursing or other professional services without the appropriate certification or license may face sanctions and criminal charges leading to a prison term.
The number of professions subject to regulation, requisites for individuals to receive professional licensure, and nature of sanctions that can be imposed for failure to comply vary across jurisdictions.
In the United States, under Michigan state laws, an individual is guilty of a felony if identified as practicing in the health profession without a valid personal license or registration.
Health professionals can also be imprisoned if found guilty of practicing beyond the limits allowed by their licenses and registration. The state laws define the scope of practice for medicine, nursing, and a number of allied health professions.
In Florida, practicing medicine without the appropriate license is a crime classified as a third degree felony, which may give imprisonment up to five years. Practicing a health care profession without a license which results in serious bodily injury classifies as a second degree felony, providing up to 15 years' imprisonment.
In the United Kingdom, healthcare professionals are regulated by the state; the UK Health and Care Professions Council (HCPC) protects the 'title' of each profession it regulates. For example, it is illegal for someone to call himself an Occupational Therapist or Radiographer if they are not on the register held by the HCPC.
See also:
- World Health Organization: Health workers
- Community health center
- Chronic care management
- Electronic superbill
- Geriatric care management
- Health human resources
Pembrolizumab (Brand Name =Keytruda)
- YouTube Video: Cancer Survivor Kathy Thomas Shares Her Keytruda Experience
- YouTube Video: How Keytruda Cancer Treatment Works (Update)
- YouTube Video: Understanding Immunotherapy for Lung Cancer
Pembrolizumab, sold under the brand name Keytruda, is a humanized antibody used in cancer immunotherapy that treats:
It is administered by slow intravenous injection.
Common side effects include:
It is an IgG4 isotype antibody that blocks a protective mechanism of cancer cells, allowing the immune system to destroy them. It targets the programmed cell death protein 1 (PD-1) receptor of lymphocytes
Pembrolizumab was approved for medical use in the United States in 2014 It is on the World Health Organization's List of Essential Medicines.
Medical uses:
As of 2019, pembrolizumab is used via intravenous infusion to treat:
For NSCLC, pembrolizumab is used:
Assessment of PD-L1 expression must be conducted with a validated and approved companion diagnostic.
In 2017, the US Food and Drug Administration (FDA) approved pembrolizumab for any unresectable or metastatic solid tumor with certain genetic anomalies (mismatch repair deficiency or microsatellite instability). This was the first time the FDA approved a cancer drug based on tumor genetics rather than tissue type or tumor site; therefore, pembrolizumab is a so-called tissue-agnostic drug.
In the European Union, pembrolizumab is indicated for:
In June 2020, the US FDA approved a new indication for pembrolizumab as the first-line treatment for people with unresectable or metastatic microsatellite instability-high (MSI‑H) or mismatch repair deficient (dMMR) colorectal cancer. The approval marks the first immunotherapy approved for that population in the US as a first-line treatment and which is administered to people without also giving chemotherapy.
In March 2021, the US FDA approved pembrolizumab in combination with platinum and fluoropyrimidine-based chemotherapy to treat metastatic or locally advanced esophageal or gastroesophageal (GEJ) (tumors with epicenter 1 to 5 centimeters above the gastroesophageal junction) carcinoma in people who are not candidates for surgical resection or definitive chemoradiation.
Efficacy was evaluated in KEYNOTE-590 (NCT03189719), a multicenter, randomized, placebo-controlled trial that enrolled 749 participants with metastatic or locally advanced esophageal or gastroesophageal junction carcinoma who were not candidates for surgical resection or definitive chemoradiation.
In May 2021, the US FDA approved pembrolizumab in combination with trastuzumab, fluoropyrimidine- and platinum-containing chemotherapy for the first-line treatment of people with locally advanced unresectable or metastatic HER2 positive gastric or gastroesophageal junction (GEJ) adenocarcinoma
Approval was based on the prespecified interim analysis of the first 264 participants of the ongoing KEYNOTE-811 (NCT03615326) trial, a multicenter, randomized, double‑blind, placebo‑controlled trial in people with HER2‑positive advanced gastric or gastroesophageal junction (GEJ) adenocarcinoma who had not previously received systemic therapy for metastatic disease.
In July 2021, the US FDA approved pembrolizumab for high-risk, early-stage, triple-negative breast cancer (TNBC) in combination with chemotherapy as neoadjuvant treatment, and then continued as a single agent as adjuvant treatment after surgery.
The FDA also granted regular approval to pembrolizumab in combination with chemotherapy for people with locally recurrent unresectable or metastatic TNBC whose tumors express PD-L1 (Combined Positive Score [CPS] ≥ 10) as determined by an FDA-approved test.
In November 2021, the US FDA approved pembrolizumab for the adjuvant treatment of people twelve years of age and older with stage IIB or IIC melanoma following complete resection.
In November 2021, the US FDA approved pembrolizumab for the adjuvant treatment of renal cell carcinoma for people at intermediate-high or high risk of recurrence following nephrectomy. Approval was based on KEYNOTE-564, a multicenter, randomized (1:1), double-blind, placebo-controlled trial in 994 patients with intermediate-high or high risk of recurrence of RCC, or M1 no evidence of disease.
In March 2022, the US FDA approved pembrolizumab for the treatment of advanced endometrial cancer.
In January 2023, the US FDA approved pembrolizumab for adjuvant treatment following resection and platinum-based chemotherapy for stage IB (T2a ≥ 4 cm), II, or IIIA non-small cell lung cancer.
In October 2023, the US FDA approved pembrolizumab to be used with gemcitabine and cisplatin for locally advanced unresectable or metastatic biliary tract cancer.
In January 2024, the US FDA approved pembrolizumab, in combination with chemoradiotherapy for the treatment of people with FIGO (International Federation of Gynecology and Obstetrics) 2014 Stage III-IVA cervical cancer.
Adverse effects:
People have had severe infusion-related reactions to pembrolizumab. There have also been severe immune-related adverse effects including lung inflammation (including fatal cases) and inflammation of endocrine organs that caused inflammation of the pituitary gland, of the thyroid (causing both hypothyroidism and hyperthyroidism in different people), and pancreatitis that caused Type 1 diabetes and diabetic ketoacidosis; some people have had to go on lifelong hormone therapy as a result (e.g. insulin therapy or thyroid hormones). Due to the drug,
People have also had:
The common adverse reactions have been:
Other adverse effects occurring in between 1% and 10% of people taking pembrolizumab have included:
Mechanism of action:
Pembrolizumab is a therapeutic antibody that binds to and blocks PD-1 located on lymphocytes. This receptor is generally responsible for preventing the immune system from attacking the body's own tissues; it is a so-called immune checkpoint
Normally, the PD-1 receptor on activated T-cells binds to the PD-L1 or PD-L2 ligands present on normal cells in the body, deactivating any potential cell-mediated immune response against these cells.
Many cancers make proteins such as PD-L1 that also bind to the PD-1 receptor, thus shutting down the ability of the body to kill the cancer. Pembrolizumab works by inhibiting lymphocytes' PD-1 receptors, blocking the ligands that would deactivate it and prevent an immune response.
This allows the immune system to target and destroy cancer cells, but also blocks a key mechanism preventing the immune system from attacking the body itself. This checkpoint inhibitor function of pembrolizumab thus has immune-dysfunction side effects as a result.
Tumors often have mutations that cause impaired DNA mismatch repair. This in turn often results in microsatellite instability allowing the tumor to generate numerous mutant proteins that could serve as tumor antigens, triggering an immune response against the tumor. By preventing the self-checkpoint system from blocking the T-cells, pembrolizumab appears to facilitate clearance of any such tumor by the immune system.
Pharmacology:
Since pembrolizumab is cleared from the circulation through non-specific catabolism, no metabolic drug interactions are expected and no studies were done on routes of elimination.
The systemic clearance [rate] is about 0.2 L/day and the terminal half-life is about 25 days.
Chemistry and manufacturing:
Pembrolizumab is an immunoglobulin G4, with a variable region against the human PD-1 receptor, a humanized mouse monoclonal [228-L-proline(H10-S>P)]γ4 heavy chain (134-218') disulfide and a humanized mouse monoclonal κ light chain dimer (226-226:229-229)-bisdisulfide.
It is recombinantly manufactured in Chinese hamster ovary (CHO) cells.
History:
Pembrolizumab was invented by scientists at Organon after which they worked with Medical Research Council Technology (which became LifeArc) starting in 2006, to humanize the antibody; Schering-Plough acquired Organon in 2007, and Merck & Co. acquired Schering-Plough two years later.
Inventors Gregory Carven, Hans van Eenennaam and Gradus Dulos were recognized as Inventors of the Year by the Intellectual Property Owners Education Foundation in 2016.
The development program for pembrolizumab was seen as high priority at Organon, but low at Schering and later Merck. In early 2010, Merck terminated development and began preparing to out-license it.
Later, in 2010, scientists from Bristol Myers Squibb published a paper in The New England Journal of Medicine showing that their checkpoint inhibitor, ipilimumab (Yervoy), had shown strong promise in treating metastatic melanoma and that a second Bristol Myers Squibb checkpoint inhibitor, nivolumab (Opdivo), was also promising.
Merck at that time had little commitment or expertise in either oncology or immunotherapy, but understood the opportunity and reacted strongly, reactivating the program and filing its IND by the end of 2010.
As one example, Martin Huber was one of the few senior people at Merck with strong experience in lung cancer drug development, but had been promoted to senior management and was no longer involved in product development. He stepped down from his role to lead clinical development of pembrolizumab for lung cancer.
Scientists at the company argued for developing a companion diagnostic and limiting testing of the drug only to patients with biomarkers showing they were likely to respond, and received agreement from management. Some people, including shareholders and analysts, criticized this decision as it limited the potential market size for the drug, while others argued it increased the chances of proving the drug would work and would make clinical trials faster.
(The trials would need fewer patients because of the likelihood of greater effect size.)
Moving quickly and reducing the risk of failure was essential for catching up with Bristol-Myers Squibb, which had an approximate five year lead over Merck. The phase I study started in early 2011, and Eric Rubin, who was running the melanoma trial, argued for and was able to win expansion of the trial until it reached around 1300 people.
This was the largest Phase I study ever run in oncology, with the patients roughly divided between melanoma and lung cancer.
In 2013, Merck quietly applied for and won a breakthrough therapy designation for the drug. This regulatory pathway was new at the time and not well understood. One of its advantages is that the US FDA holds more frequent meetings with drug developers, reducing the risk of developers of making mistakes or misunderstandings arising from the differences between regulators' expectations and what the developers want to do.
This was Merck's first use of the designation and the reduction in regulatory risk was one of the reasons management was willing to put company resources into development.
In 2013, the United States Adopted Name (USAN) name was changed from lambrolizumab to pembrolizumab. In that year clinical trial results in advanced melanoma were published in The New England Journal of Medicine. This was part of the large Phase I NCT01295827 trial.
In September 2014, the US Food and Drug Administration (FDA) approved pembrolizumab under the Fast Track Development Program. It is approved for use following treatment with ipilimumab, or after treatment with ipilimumab and a BRAF inhibitor in advanced melanoma patients who carry a BRAF mutation
As of 2015, the only PD-1/PD-L1 targeting drugs on the market are pembrolizumab and nivolumab, with clinical developments in the class of drugs receiving coverage in The New York Times.
By April 2016, Merck applied for approval to market the drug in Japan and signed an agreement with Taiho Pharmaceutical to co-promote it there.
In July 2015, pembrolizumab received marketing approval in the European Union.
In October 2015, the US FDA approved pembrolizumab for the treatment of metastatic non-small cell lung cancer (NSCLC) in people whose tumors express PD-L1 and who have failed treatment with other chemotherapeutic agents.
In July 2016, the US FDA accepted for priority review an application for recurrent or metastatic ub (HNSCC) after a platinum-based chemotherapy.
They granted accelerated approval to pembrolizumab as a treatment for patients with recurrent or metastatic (HNSCC) ("regardless of PD-L1 staining") following progression on a platinum-based chemotherapy, based on objective response rates (ORR) in the Phase Ib KEYNOTE-012 study in August of the same year.
In May 2017, pembrolizumab received an accelerated approval from the US FDA for use in any unresectable or metastatic solid tumor with DNA mismatch repair deficiencies or a microsatellite instability-high state (or, in the case of colon cancer, tumors that have progressed following chemotherapy).
This approval marked the first instance in which the FDA approved marketing of a drug based only on the presence of a genetic mutation, with no limitation on the site of the cancer or the kind of tissue in which it originated.
The approval was based on a clinical trial of 149 patients with microsatellite instability-high or mismatch repair deficient cancers who enrolled on one of five single-arm trials. Ninety patients had colorectal cancer, and 59 patients had one of 14 other cancer types.
The objective response rate for all patients was 39.6%. Response rates were similar across all cancer types, including 36% in colorectal cancer and 46% across the other tumor types.
Notably, there were 11 complete responses, with the remainder partial responses. Responses lasted for at least six months in 78% of responders. Because the clinical trial was fairly small, Merck is obligated to conduct further post-marketing studies to ensure that the results are valid. Pembrolizumab was granted orphan drug designation for SCLC in October 2017.
In June 2018, the US FDA approved pembrolizumab for use in both advanced cervical cancer for PD-L1 positive patients and for the treatment of adult and pediatric patients with refractory primary mediastinal large B-cell lymphoma (PMBCL), or who have relapsed after two or more prior lines of therapy.
In August 2018, the US FDA updated the prescribing information for pembrolizumab to require the use of an FDA-approved companion diagnostic test to determine PD-L1 levels in tumor tissue from patients with locally advanced or metastatic urothelial cancer who are cisplatin-ineligible.
On 16 August 2018, the FDA approved the Dako PD-L1 IHC 22C3 PharmDx Assay (Dako North America, Inc.) as a companion diagnostic to select patients with locally advanced or metastatic urothelial carcinoma who are cisplatin-ineligible for treatment with pembrolizumab.
The 22C3 assay determines PD-L1 expression by using a combined positive score (CPS) assessing PD-L1 staining in tumor and immune cells. As of August 2018, pembrolizumab is indicated for the treatment of those with locally advanced or metastatic urothelial carcinoma who are not eligible for cisplatin-containing chemotherapy and whose tumors express PD-L1 [Combined Positive Score (CPS) ≥ 10] as determined by an FDA-approved test, or in patients who are not eligible for any platinum-containing chemotherapy regardless of PD-L1 status.
In November 2018, the US FDA granted accelerated approval to pembrolizumab for those with hepatocellular carcinoma (HCC) who have been previously treated with sorafenib.
In February 2019, the US FDA approved pembrolizumab for the adjuvant treatment of patients with melanoma with involvement of lymph node(s) following complete resection.
The FDA granted the application orphan drug designation.
In June 2019, the US FDA granted accelerated approval to pembrolizumab for those with metastatic small cell lung cancer (SCLC) with disease progression on or after platinum-based chemotherapy and at least one other prior line of therapy, and the FDA approved pembrolizumab for the first-line treatment of patients with metastatic or unresectable recurrent head and neck squamous cell carcinoma (HNSCC).
Pembrolizumab was approved for use in combination with platinum and fluorouracil (FU) for all patients and as a single agent for patients whose tumors express PD‑L1 (Combined Positive Score [CPS] ≥ 1) as determined by an FDA‑approved test.
The FDA also expanded the intended use for the PD-L1 IHC 22C3 pharmDx kit to include use as a companion diagnostic device for selecting patients with HNSCC for treatment with pembrolizumab as a single agent.
In July 2019, the US FDA approved pembrolizumab for patients with recurrent, locally advanced or metastatic, squamous cell carcinoma of the esophagus (ESCC) whose tumors express PD-L1 (Combined Positive Score [CPS] ≥ 10), as determined by an FDA-approved test, with disease progression after one or more prior lines of systemic therapy.
The FDA also approved a new use for the PD-L1 IHC 22C3 pharmDx kit as a companion diagnostic device for selecting patients for the above indication.
In June 2020, the US FDA approved pembrolizumab as monotherapy for the treatment of adults and children with unresectable or metastatic tumor mutational burden-high (TMB-H) [≥ 10 mutations/megabase (mut/Mb)] solid tumors, as determined by an FDA-approved test, that have progressed following prior treatment and who have no satisfactory alternative treatment options.
In March 2021, the accelerated approval indication in the US for the treatment of people with metastatic small cell lung cancer (SCLC) was removed.
In January 2024, the FDA approved pembrolizumab, in combination with chemoradiotherapy, for people with FIGO 2014 Stage III-IVA cervical cancer. Efficacy was evaluated in KEYNOTE-A18 (NCT04221945), a multicenter, randomized, double-blind, placebo-controlled trial enrolling 1060 participants with cervical cancer who had not previously received definitive surgery, radiation, or systemic therapy.
The trial included 596 participants with FIGO 2014 Stage III-IVA disease and 462 participants with FIGO 2014 Stage IB2-IIB, node-positive disease.
Economics:
Pembrolizumab was priced at US$150,000 per year when it launched in 2014.
It was added to the Cancer Drugs Fund list of the English NHS in November 2022 after a "confidential" deal with manufacturer MSD.
Research:
In 2015, Merck reported results in 13 cancer types; much attention was given to early results in head and neck cancer.
As of May 2016, pembrolizumab was in Phase IB clinical trials for triple-negative breast cancer (TNBC), gastric cancer, urothelial cancer, and head and neck cancer (all under the "Keynote-012" trial) and in Phase II trial for TNBC (the "Keynote-086" trial).
At ASCO, in June 2016, Merck reported that the clinical development program was directed to around 30 cancers and that it was running over 270 clinical trials (around 100 in combination with other treatments) and had four registration-enabling studies in process.
Results of a Phase III clinical trial in triple-negative breast cancer were reported in Annals of Oncology in October 2019.
Results of a Phase II clinical trial in Merkel-cell carcinoma were reported in The New England Journal of Medicine in June 2016.
Results of a clinical trial in people with untreatable metastases arising from various solid tumors were published in Science in 2017.
A clinical Phase III trial in combination with epacadostat, an Indoleamine 2,3-dioxygenase (IDO1) inhibitor to treat melanoma was completed in 2019.
In 2021, researchers reported the results of a five-year follow-up study.
In January 2022, Neoleukin Therapeutics announced a collaboration with Merck for a combination clinical trial of Merck's Pembrolizumab and Neoleukin's NL-201, a de novo protein undergoing a Phase I clinical trial in patients with advanced, relapsed or refractory solid tumors.
In March 2023, Merck reported the results of NRG-GY018, a Phase III clinical trial in patients with stage 3 to 4 or recurrent endometrial carcinoma.
In 2022, Merck and Moderna tested Moderna's mRNA-4157/V940 drug candidate, a cancer vaccine, alongside pembrolizumab for treatment of skin and pancreatic cancers. mRNA-4157/V940 went on to win breakthrough status from the FDA.
See also:
- melanoma,
- lung cancer,
- head and neck cancer,
- Hodgkin lymphoma,
- stomach cancer,
- cervical cancer,
- and certain types of breast cancer.
It is administered by slow intravenous injection.
Common side effects include:
- fatigue,
- musculoskeletal pain,
- decreased appetite,
- itchy skin (pruritus),
- diarrhea,
- nausea,
- rash,
- fever (pyrexia),
- cough,
- difficulty breathing (dyspnea),
- constipation,
- pain,
- and abdominal pain.
It is an IgG4 isotype antibody that blocks a protective mechanism of cancer cells, allowing the immune system to destroy them. It targets the programmed cell death protein 1 (PD-1) receptor of lymphocytes
Pembrolizumab was approved for medical use in the United States in 2014 It is on the World Health Organization's List of Essential Medicines.
Medical uses:
As of 2019, pembrolizumab is used via intravenous infusion to treat:
- inoperable or metastatic melanoma,
- metastatic non-small cell lung cancer (NSCLC) in certain situations, as a first-line treatment for metastatic bladder cancer in patients who cannot receive cisplatin-based chemotherapy and have high levels of PD-L1,
- as a second-line treatment for head and neck squamous cell carcinoma (HNSCC),
- after platinum-based chemotherapy,
- for the treatment of adult and pediatric patients with refractory classic Hodgkin's lymphoma (cHL),
- and recurrent locally advanced or metastatic esophageal squamous cell carcinoma.
For NSCLC, pembrolizumab is used:
- in combination with chemotherapy (for all PD-L1, a PD-1 receptor ligand, levels)
- or by itself as a first-line treatment if the cancer expresses (≥ 1%) PD-L1 and the cancer has no mutations in EGFR or in ALK;
- if chemotherapy has already been administered, then pembrolizumab can be used as a second-line treatment, but if the cancer has EGFR or ALK mutations, agents targeting those mutations should be used first
Assessment of PD-L1 expression must be conducted with a validated and approved companion diagnostic.
In 2017, the US Food and Drug Administration (FDA) approved pembrolizumab for any unresectable or metastatic solid tumor with certain genetic anomalies (mismatch repair deficiency or microsatellite instability). This was the first time the FDA approved a cancer drug based on tumor genetics rather than tissue type or tumor site; therefore, pembrolizumab is a so-called tissue-agnostic drug.
In the European Union, pembrolizumab is indicated for:
- the treatment of advanced (unresectable or metastatic) melanoma in adults as monotherapy.
- the adjuvant treatment of adults with Stage III melanoma and lymph node involvement who have undergone complete resection as monotherapy.
- the first-line treatment of metastatic non-small cell lung carcinoma (NSCLC) in adults whose tumors express PD-L1 with a ≥ 50% tumor proportion score (TPS) with no EGFR or ALK positive tumor mutations as monotherapy.
- the first-line treatment of metastatic non-squamous NSCLC in adults whose tumors have no EGFR or ALK positive mutations in combination with pemetrexed and platinum chemotherapy.
- the first-line treatment of metastatic squamous NSCLC in adults in combination with carboplatin and either paclitaxel or nab-paclitaxel.
- the treatment of locally advanced or metastatic NSCLC in adults whose tumors express PD-L1 with a ≥ 1% TPS and who have received at least one prior chemotherapy regimen. People with EGFR or ALK positive tumor mutations should also have received targeted therapy before receiving Keytruda as monotherapy.
- the treatment of adults with relapsed or refractory classical Hodgkin lymphoma (cHL) who have failed autologous stem cell transplant (ASCT) and brentuximab vedotin (BV), or who are transplant-ineligible and have failed BV as monotherapy.
- the treatment of locally advanced or metastatic urothelial carcinoma in adults who have received prior platinum-containing chemotherapy as monotherapy.
- the treatment of locally advanced or metastatic urothelial carcinoma in adults who are not eligible for cisplatin-containing chemotherapy and whose tumors express PD L1 with a combined positive score (CPS) ≥ 10 as monotherapy.
- the first-line treatment of metastatic or unresectable recurrent head and neck squamous cell carcinoma (HNSCC) in adults whose tumors express PD-L1 with a CPS ≥ 1 as monotherapy or in combination with platinum and 5-fluorouracil (5-FU) chemotherapy.
- the treatment of recurrent or metastatic HNSCC in adults whose tumors express PD-L1 with a ≥ 50% TPS and progressing on or after platinum-containing chemotherapy as monotherapy.
- the first-line treatment of advanced renal cell carcinoma (RCC) in adults in combination with axitinib.
In June 2020, the US FDA approved a new indication for pembrolizumab as the first-line treatment for people with unresectable or metastatic microsatellite instability-high (MSI‑H) or mismatch repair deficient (dMMR) colorectal cancer. The approval marks the first immunotherapy approved for that population in the US as a first-line treatment and which is administered to people without also giving chemotherapy.
In March 2021, the US FDA approved pembrolizumab in combination with platinum and fluoropyrimidine-based chemotherapy to treat metastatic or locally advanced esophageal or gastroesophageal (GEJ) (tumors with epicenter 1 to 5 centimeters above the gastroesophageal junction) carcinoma in people who are not candidates for surgical resection or definitive chemoradiation.
Efficacy was evaluated in KEYNOTE-590 (NCT03189719), a multicenter, randomized, placebo-controlled trial that enrolled 749 participants with metastatic or locally advanced esophageal or gastroesophageal junction carcinoma who were not candidates for surgical resection or definitive chemoradiation.
In May 2021, the US FDA approved pembrolizumab in combination with trastuzumab, fluoropyrimidine- and platinum-containing chemotherapy for the first-line treatment of people with locally advanced unresectable or metastatic HER2 positive gastric or gastroesophageal junction (GEJ) adenocarcinoma
Approval was based on the prespecified interim analysis of the first 264 participants of the ongoing KEYNOTE-811 (NCT03615326) trial, a multicenter, randomized, double‑blind, placebo‑controlled trial in people with HER2‑positive advanced gastric or gastroesophageal junction (GEJ) adenocarcinoma who had not previously received systemic therapy for metastatic disease.
In July 2021, the US FDA approved pembrolizumab for high-risk, early-stage, triple-negative breast cancer (TNBC) in combination with chemotherapy as neoadjuvant treatment, and then continued as a single agent as adjuvant treatment after surgery.
The FDA also granted regular approval to pembrolizumab in combination with chemotherapy for people with locally recurrent unresectable or metastatic TNBC whose tumors express PD-L1 (Combined Positive Score [CPS] ≥ 10) as determined by an FDA-approved test.
In November 2021, the US FDA approved pembrolizumab for the adjuvant treatment of people twelve years of age and older with stage IIB or IIC melanoma following complete resection.
In November 2021, the US FDA approved pembrolizumab for the adjuvant treatment of renal cell carcinoma for people at intermediate-high or high risk of recurrence following nephrectomy. Approval was based on KEYNOTE-564, a multicenter, randomized (1:1), double-blind, placebo-controlled trial in 994 patients with intermediate-high or high risk of recurrence of RCC, or M1 no evidence of disease.
In March 2022, the US FDA approved pembrolizumab for the treatment of advanced endometrial cancer.
In January 2023, the US FDA approved pembrolizumab for adjuvant treatment following resection and platinum-based chemotherapy for stage IB (T2a ≥ 4 cm), II, or IIIA non-small cell lung cancer.
In October 2023, the US FDA approved pembrolizumab to be used with gemcitabine and cisplatin for locally advanced unresectable or metastatic biliary tract cancer.
In January 2024, the US FDA approved pembrolizumab, in combination with chemoradiotherapy for the treatment of people with FIGO (International Federation of Gynecology and Obstetrics) 2014 Stage III-IVA cervical cancer.
Adverse effects:
People have had severe infusion-related reactions to pembrolizumab. There have also been severe immune-related adverse effects including lung inflammation (including fatal cases) and inflammation of endocrine organs that caused inflammation of the pituitary gland, of the thyroid (causing both hypothyroidism and hyperthyroidism in different people), and pancreatitis that caused Type 1 diabetes and diabetic ketoacidosis; some people have had to go on lifelong hormone therapy as a result (e.g. insulin therapy or thyroid hormones). Due to the drug,
People have also had:
The common adverse reactions have been:
- fatigue (24%),
- rash (19%),
- itchiness (pruritus) (17%),
- diarrhea (12%),
- nausea (11%)
- and joint pain (arthralgia) (10%).
Other adverse effects occurring in between 1% and 10% of people taking pembrolizumab have included:
- anemia,
- decreased appetite,
- headache,
- dizziness,
- distortion of the sense of taste,
- dry eye,
- high blood pressure,
- abdominal pain,
- constipation,
- dry mouth,
- severe skin reactions,
- vitiligo,
- various kinds of:
- acne,
- dry skin,
- eczema,
- muscle pain,
- pain in a limb,
- arthritis,
- weakness,
- edema,
- fever,
- chills,
- myasthenia gravis,
- and flu-like symptoms.
Mechanism of action:
Pembrolizumab is a therapeutic antibody that binds to and blocks PD-1 located on lymphocytes. This receptor is generally responsible for preventing the immune system from attacking the body's own tissues; it is a so-called immune checkpoint
Normally, the PD-1 receptor on activated T-cells binds to the PD-L1 or PD-L2 ligands present on normal cells in the body, deactivating any potential cell-mediated immune response against these cells.
Many cancers make proteins such as PD-L1 that also bind to the PD-1 receptor, thus shutting down the ability of the body to kill the cancer. Pembrolizumab works by inhibiting lymphocytes' PD-1 receptors, blocking the ligands that would deactivate it and prevent an immune response.
This allows the immune system to target and destroy cancer cells, but also blocks a key mechanism preventing the immune system from attacking the body itself. This checkpoint inhibitor function of pembrolizumab thus has immune-dysfunction side effects as a result.
Tumors often have mutations that cause impaired DNA mismatch repair. This in turn often results in microsatellite instability allowing the tumor to generate numerous mutant proteins that could serve as tumor antigens, triggering an immune response against the tumor. By preventing the self-checkpoint system from blocking the T-cells, pembrolizumab appears to facilitate clearance of any such tumor by the immune system.
Pharmacology:
Since pembrolizumab is cleared from the circulation through non-specific catabolism, no metabolic drug interactions are expected and no studies were done on routes of elimination.
The systemic clearance [rate] is about 0.2 L/day and the terminal half-life is about 25 days.
Chemistry and manufacturing:
Pembrolizumab is an immunoglobulin G4, with a variable region against the human PD-1 receptor, a humanized mouse monoclonal [228-L-proline(H10-S>P)]γ4 heavy chain (134-218') disulfide and a humanized mouse monoclonal κ light chain dimer (226-226:229-229)-bisdisulfide.
It is recombinantly manufactured in Chinese hamster ovary (CHO) cells.
History:
Pembrolizumab was invented by scientists at Organon after which they worked with Medical Research Council Technology (which became LifeArc) starting in 2006, to humanize the antibody; Schering-Plough acquired Organon in 2007, and Merck & Co. acquired Schering-Plough two years later.
Inventors Gregory Carven, Hans van Eenennaam and Gradus Dulos were recognized as Inventors of the Year by the Intellectual Property Owners Education Foundation in 2016.
The development program for pembrolizumab was seen as high priority at Organon, but low at Schering and later Merck. In early 2010, Merck terminated development and began preparing to out-license it.
Later, in 2010, scientists from Bristol Myers Squibb published a paper in The New England Journal of Medicine showing that their checkpoint inhibitor, ipilimumab (Yervoy), had shown strong promise in treating metastatic melanoma and that a second Bristol Myers Squibb checkpoint inhibitor, nivolumab (Opdivo), was also promising.
Merck at that time had little commitment or expertise in either oncology or immunotherapy, but understood the opportunity and reacted strongly, reactivating the program and filing its IND by the end of 2010.
As one example, Martin Huber was one of the few senior people at Merck with strong experience in lung cancer drug development, but had been promoted to senior management and was no longer involved in product development. He stepped down from his role to lead clinical development of pembrolizumab for lung cancer.
Scientists at the company argued for developing a companion diagnostic and limiting testing of the drug only to patients with biomarkers showing they were likely to respond, and received agreement from management. Some people, including shareholders and analysts, criticized this decision as it limited the potential market size for the drug, while others argued it increased the chances of proving the drug would work and would make clinical trials faster.
(The trials would need fewer patients because of the likelihood of greater effect size.)
Moving quickly and reducing the risk of failure was essential for catching up with Bristol-Myers Squibb, which had an approximate five year lead over Merck. The phase I study started in early 2011, and Eric Rubin, who was running the melanoma trial, argued for and was able to win expansion of the trial until it reached around 1300 people.
This was the largest Phase I study ever run in oncology, with the patients roughly divided between melanoma and lung cancer.
In 2013, Merck quietly applied for and won a breakthrough therapy designation for the drug. This regulatory pathway was new at the time and not well understood. One of its advantages is that the US FDA holds more frequent meetings with drug developers, reducing the risk of developers of making mistakes or misunderstandings arising from the differences between regulators' expectations and what the developers want to do.
This was Merck's first use of the designation and the reduction in regulatory risk was one of the reasons management was willing to put company resources into development.
In 2013, the United States Adopted Name (USAN) name was changed from lambrolizumab to pembrolizumab. In that year clinical trial results in advanced melanoma were published in The New England Journal of Medicine. This was part of the large Phase I NCT01295827 trial.
In September 2014, the US Food and Drug Administration (FDA) approved pembrolizumab under the Fast Track Development Program. It is approved for use following treatment with ipilimumab, or after treatment with ipilimumab and a BRAF inhibitor in advanced melanoma patients who carry a BRAF mutation
As of 2015, the only PD-1/PD-L1 targeting drugs on the market are pembrolizumab and nivolumab, with clinical developments in the class of drugs receiving coverage in The New York Times.
By April 2016, Merck applied for approval to market the drug in Japan and signed an agreement with Taiho Pharmaceutical to co-promote it there.
In July 2015, pembrolizumab received marketing approval in the European Union.
In October 2015, the US FDA approved pembrolizumab for the treatment of metastatic non-small cell lung cancer (NSCLC) in people whose tumors express PD-L1 and who have failed treatment with other chemotherapeutic agents.
In July 2016, the US FDA accepted for priority review an application for recurrent or metastatic ub (HNSCC) after a platinum-based chemotherapy.
They granted accelerated approval to pembrolizumab as a treatment for patients with recurrent or metastatic (HNSCC) ("regardless of PD-L1 staining") following progression on a platinum-based chemotherapy, based on objective response rates (ORR) in the Phase Ib KEYNOTE-012 study in August of the same year.
In May 2017, pembrolizumab received an accelerated approval from the US FDA for use in any unresectable or metastatic solid tumor with DNA mismatch repair deficiencies or a microsatellite instability-high state (or, in the case of colon cancer, tumors that have progressed following chemotherapy).
This approval marked the first instance in which the FDA approved marketing of a drug based only on the presence of a genetic mutation, with no limitation on the site of the cancer or the kind of tissue in which it originated.
The approval was based on a clinical trial of 149 patients with microsatellite instability-high or mismatch repair deficient cancers who enrolled on one of five single-arm trials. Ninety patients had colorectal cancer, and 59 patients had one of 14 other cancer types.
The objective response rate for all patients was 39.6%. Response rates were similar across all cancer types, including 36% in colorectal cancer and 46% across the other tumor types.
Notably, there were 11 complete responses, with the remainder partial responses. Responses lasted for at least six months in 78% of responders. Because the clinical trial was fairly small, Merck is obligated to conduct further post-marketing studies to ensure that the results are valid. Pembrolizumab was granted orphan drug designation for SCLC in October 2017.
In June 2018, the US FDA approved pembrolizumab for use in both advanced cervical cancer for PD-L1 positive patients and for the treatment of adult and pediatric patients with refractory primary mediastinal large B-cell lymphoma (PMBCL), or who have relapsed after two or more prior lines of therapy.
In August 2018, the US FDA updated the prescribing information for pembrolizumab to require the use of an FDA-approved companion diagnostic test to determine PD-L1 levels in tumor tissue from patients with locally advanced or metastatic urothelial cancer who are cisplatin-ineligible.
On 16 August 2018, the FDA approved the Dako PD-L1 IHC 22C3 PharmDx Assay (Dako North America, Inc.) as a companion diagnostic to select patients with locally advanced or metastatic urothelial carcinoma who are cisplatin-ineligible for treatment with pembrolizumab.
The 22C3 assay determines PD-L1 expression by using a combined positive score (CPS) assessing PD-L1 staining in tumor and immune cells. As of August 2018, pembrolizumab is indicated for the treatment of those with locally advanced or metastatic urothelial carcinoma who are not eligible for cisplatin-containing chemotherapy and whose tumors express PD-L1 [Combined Positive Score (CPS) ≥ 10] as determined by an FDA-approved test, or in patients who are not eligible for any platinum-containing chemotherapy regardless of PD-L1 status.
In November 2018, the US FDA granted accelerated approval to pembrolizumab for those with hepatocellular carcinoma (HCC) who have been previously treated with sorafenib.
In February 2019, the US FDA approved pembrolizumab for the adjuvant treatment of patients with melanoma with involvement of lymph node(s) following complete resection.
The FDA granted the application orphan drug designation.
In June 2019, the US FDA granted accelerated approval to pembrolizumab for those with metastatic small cell lung cancer (SCLC) with disease progression on or after platinum-based chemotherapy and at least one other prior line of therapy, and the FDA approved pembrolizumab for the first-line treatment of patients with metastatic or unresectable recurrent head and neck squamous cell carcinoma (HNSCC).
Pembrolizumab was approved for use in combination with platinum and fluorouracil (FU) for all patients and as a single agent for patients whose tumors express PD‑L1 (Combined Positive Score [CPS] ≥ 1) as determined by an FDA‑approved test.
The FDA also expanded the intended use for the PD-L1 IHC 22C3 pharmDx kit to include use as a companion diagnostic device for selecting patients with HNSCC for treatment with pembrolizumab as a single agent.
In July 2019, the US FDA approved pembrolizumab for patients with recurrent, locally advanced or metastatic, squamous cell carcinoma of the esophagus (ESCC) whose tumors express PD-L1 (Combined Positive Score [CPS] ≥ 10), as determined by an FDA-approved test, with disease progression after one or more prior lines of systemic therapy.
The FDA also approved a new use for the PD-L1 IHC 22C3 pharmDx kit as a companion diagnostic device for selecting patients for the above indication.
In June 2020, the US FDA approved pembrolizumab as monotherapy for the treatment of adults and children with unresectable or metastatic tumor mutational burden-high (TMB-H) [≥ 10 mutations/megabase (mut/Mb)] solid tumors, as determined by an FDA-approved test, that have progressed following prior treatment and who have no satisfactory alternative treatment options.
In March 2021, the accelerated approval indication in the US for the treatment of people with metastatic small cell lung cancer (SCLC) was removed.
In January 2024, the FDA approved pembrolizumab, in combination with chemoradiotherapy, for people with FIGO 2014 Stage III-IVA cervical cancer. Efficacy was evaluated in KEYNOTE-A18 (NCT04221945), a multicenter, randomized, double-blind, placebo-controlled trial enrolling 1060 participants with cervical cancer who had not previously received definitive surgery, radiation, or systemic therapy.
The trial included 596 participants with FIGO 2014 Stage III-IVA disease and 462 participants with FIGO 2014 Stage IB2-IIB, node-positive disease.
Economics:
Pembrolizumab was priced at US$150,000 per year when it launched in 2014.
It was added to the Cancer Drugs Fund list of the English NHS in November 2022 after a "confidential" deal with manufacturer MSD.
Research:
In 2015, Merck reported results in 13 cancer types; much attention was given to early results in head and neck cancer.
As of May 2016, pembrolizumab was in Phase IB clinical trials for triple-negative breast cancer (TNBC), gastric cancer, urothelial cancer, and head and neck cancer (all under the "Keynote-012" trial) and in Phase II trial for TNBC (the "Keynote-086" trial).
At ASCO, in June 2016, Merck reported that the clinical development program was directed to around 30 cancers and that it was running over 270 clinical trials (around 100 in combination with other treatments) and had four registration-enabling studies in process.
Results of a Phase III clinical trial in triple-negative breast cancer were reported in Annals of Oncology in October 2019.
Results of a Phase II clinical trial in Merkel-cell carcinoma were reported in The New England Journal of Medicine in June 2016.
Results of a clinical trial in people with untreatable metastases arising from various solid tumors were published in Science in 2017.
A clinical Phase III trial in combination with epacadostat, an Indoleamine 2,3-dioxygenase (IDO1) inhibitor to treat melanoma was completed in 2019.
In 2021, researchers reported the results of a five-year follow-up study.
In January 2022, Neoleukin Therapeutics announced a collaboration with Merck for a combination clinical trial of Merck's Pembrolizumab and Neoleukin's NL-201, a de novo protein undergoing a Phase I clinical trial in patients with advanced, relapsed or refractory solid tumors.
In March 2023, Merck reported the results of NRG-GY018, a Phase III clinical trial in patients with stage 3 to 4 or recurrent endometrial carcinoma.
In 2022, Merck and Moderna tested Moderna's mRNA-4157/V940 drug candidate, a cancer vaccine, alongside pembrolizumab for treatment of skin and pancreatic cancers. mRNA-4157/V940 went on to win breakthrough status from the FDA.
See also:
- Pembrolizumab at the U.S. National Library of Medicine Medical Subject Headings (MeSH)